1. Introduction
Japan is facing a super-aged society, and the proportion of frail older adults is also on the rise. Frailty refers to a vulnerable state in which one's physiological reserve declines, and individuals with frailty become more susceptible to stress in later life [
1]. Physical frailty in particular is closely linked to the need for caregiving, and its presence increases the risk of various diseases [
2,
3,
4]. It is thus essential to identify factors and approaches that can reduce the risk of the development of physical frailty in community-dwelling older adults.
Physical activity is a factor that has been reported to contribute most significantly to reducing the risk of physical frailty [
5]. Numerous studies have explored the negative relationship between moderate-to-vigorous physical activity (MVPA) and physical frailty [
6,
7]. Our research has demonstrated that compared to community-dwelling older adults' exercise habits or social participation, there is a stronger association between their MVPA and their risk of physical frailty [
8]. Conversely, sleep is a critical component of daily life, and age-related declines in sleep quality have been reported. For example, Ohayon et al. observed a series of healthy adults and documented increased nocturnal awakenings and decreased deep sleep from the age of 55, indicating a relatively early decline in sleep quality [
9]. Although an association between poor sleep quality and an increased risk of physical frailty has been reported, the physical activity levels of the participants were not examined [
10,
11,
12].
Other investigations have suggested an association between poor sleep quality and slower maximal gait speed, even after adjusting for average physical activity (counts/min/day) evaluated by a triaxial accelerometer [
13]. Reduced sleep quality could thus be an independent factor that increases the risk of physical frailty. A positive association between the level of physical activity and the quality of sleep has been proposed [
14], but even among individuals who engage in sufficient physical activity, it is possible that some may experience poor sleep quality, and these individuals may potentially be at a higher risk of physical frailty. The combination of insufficient MVPA and poor sleep quality may also synergistically increase that risk.
The objective of this study was to determine the association between individual and combined effects of MVPA and sleep quality with physical frailty in community-dwelling older adults.
2. Materials and Methods
2.1. Study design
The study's design was cross-sectional. We used the baseline data obtained in the Itoshima Felix Study conducted in 2017 [
15].
2.2. Participants
Our initial study population comprised 10,000 citizens aged 65–75 years who lived in Itoshima City, Fukuoka, Japan and responded to the Community Needs Survey in 2016. None of the citizens were certified as requiring support or nursing care under Japan's Long-Term Care Insurance System [
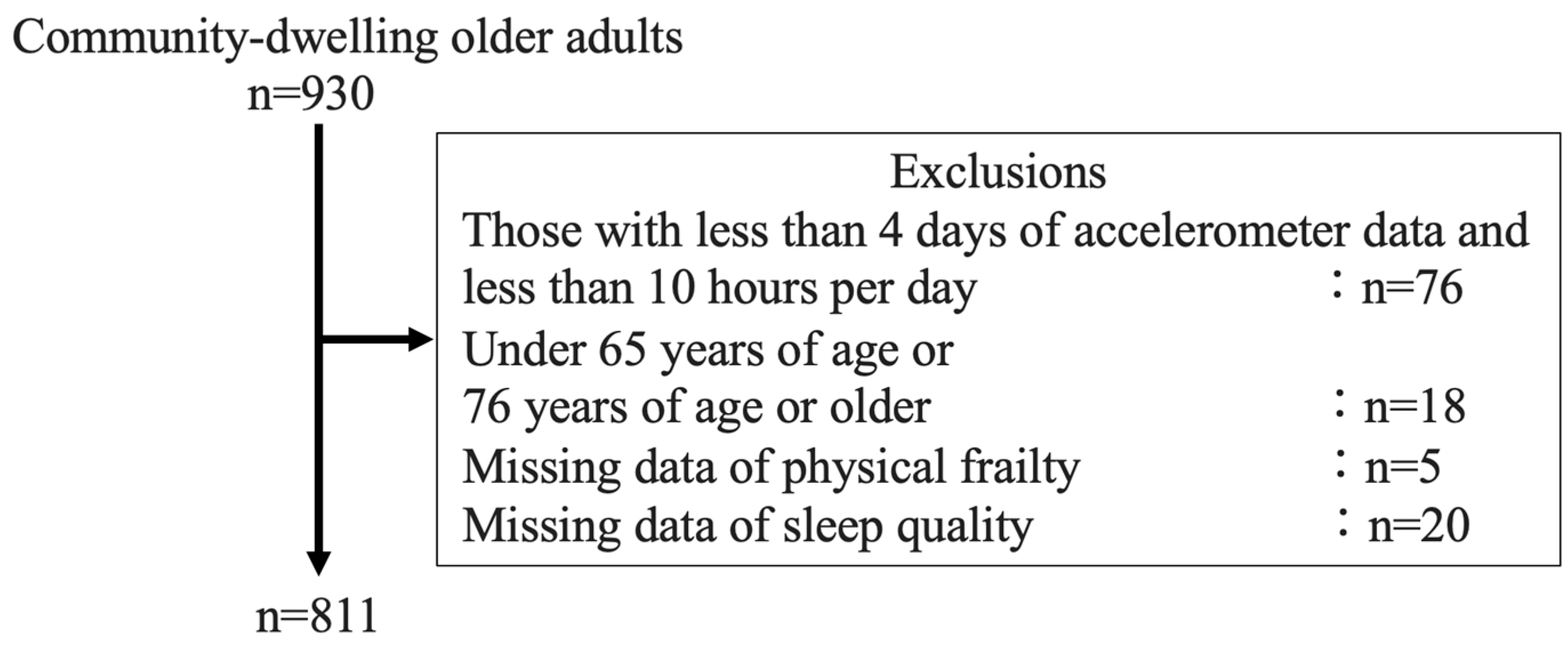
16]. Taking into account the size of the district, we randomly selected 5,000 of the citizens and sent them invitations to participate in the Itoshima Felix study and complete questionnaires. Among these individuals, 930 completed physical function tests and additional questionnaires at local community centers. Ultimately, in the final analysis, we analyzed the data of the 811 participants who met the criteria for valid data on physical activity measured by a triaxial accelerometer and had no missing data on sleep quality and physical frailty (
Figure 1).
This study was approved by the Institutional Review Board of Kyushu University (approval no. 201708), and informed consent was obtained from all of the participants.
2.3. Measurements
2.3.1. Physical frailty
The criteria that were used for assessing the participants' physical frailty were determined based on the frailty phenotype, specifically focusing on values in the bottom 20% of the population [
1,
17]. These criteria encompass five components: weight loss, low grip strength, psychological stress, slow gait speed, and low physical activity. In the present study, we defined 'frailty' as meeting three or more of these five criteria, 'pre-frailty' as meeting one or two of the criteria, and 'robust' as meeting none of the criteria.
Weight loss was defined as responding "yes" to the question, "Have you experienced unintentional weight loss exceeding 2–3 kg in the previous six months?"
Psychological stress was assessed using two items from the six-item method developed by Kessler et al. [
18]. Participants were asked about their feelings in the past month, specifically whether they felt that everything they did was an effort and whether they felt exhausted without any reason. Response options ranged from 'not at all' to 'always. ' If any of the responses fell into the categories of 'sometimes,' 'mostly,' or 'always, ' the participant was considered exhausted.
Low grip strength was defined based on grip strength, with individuals scoring in the lowest 20% of maximum grip strength stratified by gender and body mass index (BMI). Grip strength was measured using a Smedley grip strength meter (GRIP-D, T.K.K. 5401; Takei Scientific Instruments, Niigata, Japan) with a posture in a natural standing position where there is no bending of shoulders or elbows while standing. Measurements were taken for both hands, alternating between hands, and repeated. The greater values from both hands were averaged [
19].
Slow gait speed was identified based on gait speed, with individuals scoring in the slowest 20% of maximum gait speed determined by a 5-meter walking test. In the test, the participant walked an 11-m distance from a stationary standing position, and the time taken to walk was measured at the 5-m mark between the 3-m and 8-m points. The participants were allowed to use walking aids during the measurements. Gait speed was assessed twice, and the faster speed was recorded. The results were stratified by gender and height [
20].
Low physical activity was evaluated by measuring the participant's physical activity energy expenditure (PAEE, kcal) using the aforementioned triaxial accelerometer. Low physical activity was defined as scoring in the lowest 20% of energy expenditure from physical activity per day, stratified by sex. The quantification is expressed as kilocalories per kilogram of body weight expended per day (kcal/kg/day). We introduced an accelerometer (Active Style Pro HJA-350IT, Omron Healthcare, Kyoto, Japan). The accelerometer is a device that continuously measures exercise intensity using an algorithm derived from the relationship between data obtained by an acceleration sensor and energy consumption determined by expired gas analysis. Post-processing of the data followed established procedures from previous studies [
21]. Anteroposterior (x-axis), mediolateral (y-axis), and vertical (z-axis) acceleration measurements were collected during each activity at a rate of 32 Hz with 12-bit accuracy. The acceleration data range for each axis is ±6 G, resulting in a resolution of 3 mG. Each signal from the triaxial accelerometer underwent high-pass filtering with a cutoff frequency of 0.7 Hz to eliminate the gravitational acceleration component. The integral of the absolute value of the acceleration signals from all three axes was calculated over 10-second intervals. The researchers explained the method of wearing the activity monitor to each participant individually, both in written instructions and verbally, and assisted the participants in putting on the device. The participants wore this accelerometer continuously for 7 days. We defined 'valid data' as the accelerometer data recorded consistently for ≥10 hr/day on ≥4 days [
22]. Accelerometer data are known to be more accurate than self-reported questionnaire estimates, and the usage of accelerometers in general populations is increasing [
23]. The accuracy of the intensity estimation by the Active Style Pro accelerometer has been validated with the Douglas bag method [
24]. The use of a triaxial accelerometer to assess physical activity also allows for a more precise estimation of activity intensities compared to conventional uniaxial accelerometers [
24,
25].
2.3.2. Physical activity
According to the Physical Activity Guidelines proposed by the World Health Organization (WHO) in 2020, it is recommended that older adults engage in moderate-intensity physical activity (MPA) for 150–300 min/week or vigorous-intensity physical activity (VPA) for 75–150 min/week [
25]. To obtain even greater benefits, it is recommended that older adults engage in MPA for >300 min/week or VPA for >150 min/week [
26]. Our study participants were older adults who were living independently, and we thus defined 'meeting the MVPA criterion' as either engaging in MPA for ≥300 min/week, VPA for ≥150 min/week, or both.
2.3.3. Sleep quality
The Pittsburgh Sleep Quality Index (PSQI) was used to assess the study participants' sleep quality. The PSQI is a seven-item questionnaire, with each item being rated on a scale of 0 to 3, resulting in a total score ranging from 0 to 21. Higher scores indicate poorer sleep quality. Based on previous research, we used a score of ≥5.5 as the threshold to define decreased sleep quality and a score of <5.5 to define good sleep quality [
27].
2.4. Statistical analyses
We classified the participants into four groups: those who met the criteria for both MVPA and good sleep quality (MVA+SLP+), those who met the criteria for MVPA but had poor sleep quality (MVA+SLP−), those who did not meet the criteria for MVPA but had good sleep quality (MVA−SLP+), and those who did not meet the criteria for both MVPA and sleep quality (MVA−SLP−). The proportions of physical pre-frailty and frailty in these four groups combining MVPA status and sleep quality deterioration were compared by a one-way analysis of variance (ANOVA) or the Kruskal-Wallis test. Subsequently, multiple comparisons between groups were conducted using the Bonferroni method to investigate the differences in each item among the groups, specifically comparing the group that engaged in MVPA and had good sleep quality (MVA+SLP+) with the other three groups.
We also performed an ordinal logistic regression analysis using the MVPA status and poor sleep quality as exposure factors and three categories: robust, physical pre-frailty, and physical frailty as outcomes. The logistic regression analysis models included Model 1 without adjusted factors, and Model 2, adjusted for population demographic factors that have been reported to be associated with physical pre-frailty and frailty. The adjustment factors included age, sex, BMI, presence of disease (osteoporosis, hypertension, dyslipidemia, diabetes, stroke, cardiovascular disease, and other diseases), number of pain sites (shoulder, elbow, wrist, hip, knee, ankle, lower back, and neck), Mini-Mental State Examination (MMSE) score, years of education, presence of a tobacco-smoking habit (categorized as 'almost every day,' 'occasionally,' 'used to smoke but quit,' or "never smoked'; we considered the categories 'almost every day' and 'occasionally' as having a tobacco-smoking habit), alcohol consumption (categorized as 'almost every day,' "occasionally,' 'rarely,' or 'never drink'; we considered the categories 'almost every day' and 'occasionally' as having an alcohol consumption habit), sedentary time, which was assessed by the Omron Healthcare Active style Pro HJA-350IT triaxial accelerometer; we considered activity-intensity values below 1.5 metabolic equivalent of task (MET) units as sedentary time (ST). These factors were extracted from the questionnaires and measurement results. To examine the interaction between MVPA and sleep quality, the variables were dichotomized, that is, whether or not MVPA was met and whether sleep quality was good. A cross-product term was added to the logistic regression model to evaluate the statistical significance of the interaction between MVPA and sleep quality on physical frailty.
3. Results
3.1. Comparison of characteristics in the combination of MVPA and sleep quality
The participant response rate among the initially guided population was 930 participants (18.6%), which was low. Furthermore, out of this group, the final analyzable participants comprised 811 participants (87.2%). As shown in
Table 1, the number of participants in each group was as follows: 360 individuals (42.2%) in the MVA
+SLP
+ group, 105 individuals (12.3%) in the MVA
+SLP
− group, 301 individuals (35.3%) in the MVA
−SLP
+ group, and 88 individuals (10.3%) in the MVA
−SLP
− group. Compared to the MVA
+SLP
+ group, the proportion of individuals with age and illness was significantly higher in the MVA
−SLP
− group. Both the MVA
+SLP
− and MVA
−SLP
− groups exhibited a significantly higher number of pain locations. The MVA
−SLP
+ group had a higher prevalence of smokers. Both the MVA
−SLP
+ and MVA
−SLP
− groups had significantly lower levels of physical activity. Compared to the MVA
+SLP
+ group, the PSQI score was significantly higher in both the MVA
+SLP
− and MVA
−SLP
− groups.
The rate of individuals classified as having physical pre-frailty/frailty in each group was as follows: 42.8%/0.6% in the MVA+SLP+ group, 47.5%/2.0% in the MVA+SLP− group, 58.5%/8.2% in the MVA−SLP+ group, and 65.5%/12.6% in the MVA−SLP− group.
Table 1.
Characteristics of MVPA in combination with sleep quality.
Table 1.
Characteristics of MVPA in combination with sleep quality.
| |
MVA+SLP+
n=360
|
MVA+SLP−
n=105
|
MVA−SLP+
n=301
|
MVA−SLP−
n=88
|
p-value |
| Age, yrs |
70 [68–73] |
71 [68–73] |
70 [68–74] |
72 [69–75]* |
<0.01 |
| Men |
158 (46.3) |
42 (41.6) |
147 (52.1) |
39 (44.8) |
0.23 |
| BMI, kg/m2
|
22.6 ± 3.1 |
22.5 ± 3.2 |
23.2 ± 3.0 |
23.2 ± 3.6 |
0.08 |
| Presence of disease |
247 (72.4) |
76 (75.3) |
227 (80.5) |
81 (93.1)* |
<0.01 |
| No. of pain sites |
1 [0–2] |
2 [1–3]* |
1 [0–2] |
2 [1–3]* |
<0.01 |
| Education, yrs |
12.9 ± 2.3 |
12.8 ± 2.5 |
13.2 ± 2.5 |
12.5 ± 2.1 |
0.06 |
| Presence of tobacco smoking habit |
18 (5.3) |
2 (2.0) |
34 (12.1)* |
8 (9.2) |
<0.01 |
| Presence of alcohol habit |
181 (53.1) |
52 (51.5) |
140 (49.7) |
37 (42.5) |
0.36 |
| MMSE, score |
29 [26–30] |
28 [26–30] |
28 [26–30] |
28 [26–30] |
0.55 |
| Sedentary time, min/day |
412 ± 104.8 |
417.8 ± 102.7 |
486.9 ± 9.9* |
477.1 ± 99.6* |
<0.01 |
| MVPA, min/day |
66.0 [53.0–88.1] |
68.4 [55.7–87.1] |
28.6 [18.4–36.3]* |
25.7 [17.2–33.0]* |
<0.01 |
| PSQI, score |
3 [2–4] |
8 [6–10]* |
3 [2–4] |
8 [7–9]* |
<0.01 |
| Physical pre-frailty |
146 (42.8) |
48 (47.5) |
165 (58.5)* |
57 (65.5)* |
<0.01 |
| Physical frailty |
2 (0.6) |
2 (2.0) |
23 (8.2)* |
11 (12.6)* |
| Low grip strength |
63 (18.5) |
20 (19.8) |
62 (22.0) |
23 (26.4) |
0.38 |
| Slow gaiit speed |
47 (13.8) |
1 (10.9) |
74 (26.2)* |
27 (31.0)* |
<0.01 |
| Psychological stress |
28 (8.2) |
22 (21.8)* |
28 (9.9) |
24 (27.6)* |
<0.01 |
| Weight loss |
33 (9.7) |
8 (7.9) |
25 (8.9) |
11 (12.6) |
0.70 |
| Low physical activity |
9 (2.6) |
2 (2.0) |
105 (37.2)* |
35 (40.2)* |
<0.01 |
3.2. Association between the combination of MVPA + sleep quality and physical pre-frailty and frailty
Using an ordinal logistic regression analysis, we calculated and compared the odds ratios (OR) and 95% confidence intervals (CI) for physical pre-frailty and frailty, with the MVA
+SLP
+ group serving as the reference group. The MVA
−SLP
+ group and the MVA
−SLP
− group showed significantly higher ORs for physical pre-frailty and frailty. As shown in
Table 2, this association remained significant even after multivariate adjustment, with an OR of 2.56 (95%CI: 1.80–3.62) in the MVA
−SLP
+ group and an OR of 3.97 (95%CI: 2.33–6.74) in the MVA
−SLP
− group. The interaction between the MVPA and sleep quality was significant (p<0.0001).
3.3. Association between the combination of MVPA and sleep quality and components of physical frailty
Compared to the MVA
+SLP
+ group, the MVA
+SLP
− group showed a significantly higher OR for psychological stress, while the MVA
−SLP
+ group had a significantly higher OR for slow gait speed and low physical activity. These associations remained significant after adjustment (
Table 3). The MVA
−SLP
− group also had higher ORs for slow gait speed, psychological stress, and low physical activity; the significance of the association for slow gait speed disappeared after adjustment.
4. Discussion
The results of our analyses revealed that compared to the group of participants who met the MVPA criteria and had good sleep quality, there was a significant increase in the risk of physical pre-frailty and frailty among the group of participants who did not meet the criteria for MVPA but had good sleep quality, as well as the group who did not meet the MVPA criteria and had poor sleep quality. In addition, the prevalence of physical frailty in our participants was lower compared to a systematic review that included cross-sectional studies targeting community-dwelling older adults aged ≥65 years (21 papers, total of 61,500 individuals) [
28]. Moreover, in comparison to previous studies, we observed a higher proportion of older adults who met the criteria for MVPA, and a similar proportion of older adults with poor sleep quality compared to the reported values [
29,
30]. In the present participants, objective triaxial accelerometers were used to assess MVPA, which allowed for an accurate calculation of walking and other activities. This difference in assessment methods may have contributed to the discrepancy between the past and present results. When considering sleep quality, it is essential to acknowledge the potential disparities between objectively measured and reported results. Both previous studies and our study utilized the same PSQI for assessing sleep quality, resulting in similar prevalence rates. However, there is a need to consider the possibility of different proportions when objectively evaluating sleep quality.
As in earlier studies, our present findings demonstrated that individuals who did not meet the criteria for MVPA had a higher risk of physical pre-frailty and frailty. Cross-sectional studies have reported a negative association between MVPA and physical frailty in community-dwelling older adults, which aligns with the results of our study (15,31,32). On the other hand, regarding sleep quality, an investigation of community-dwelling older adults have reported a negative association between sleep quality as assessed by the PSQI and physical frailty assessed by the Fried phenotype [
10]; however, physical activity was not measured in that study. A novel finding from our present analyses is that when an individual's sleep quality is poor, not meeting the criteria for MVPA increases the risk of physical pre-frailty and frailty, but when the criteria for MVPA are met, poor sleep quality does not necessarily increase the risk of physical pre-frailty and frailty.
Although our results also revealed that individuals who met the criteria for MVPA were not independently at a higher risk of physical pre-frailty and frailty, even if they had poor sleep quality, the MVA
+SLP
− group had a higher risk of psychological stress. A novel finding of the present study is that individuals who meet the criteria for MVPA are not necessarily at a higher risk of physical pre-frailty and frailty, even if the quality of their sleep is poor. An investigation of 2,264 community-dwelling older adults indicated that poor sleep quality was associated with daytime fatigue [
33], which is consistent with our result, indicating a similar relationship. Although physical activity is effective for preventing frailty, a meta-analysis of randomized controlled trials (RCTs) reported adverse events such as muscle pain, fatigue, and shoulder stiffness in older adults [
5]. The possibility that meeting the criteria for MVPA also influenced the increased risk of psychological stress thus cannot be ruled out. Poor sleep quality may also contribute to insufficient performance and muscle recovery, leading to a decrease in the benefits of physical activity [
34,
35]. In a study of community-dwelling older adults (average age 82 yrs), a positive association between sleep quality and physical function was observed, even when the subjects' average physical activity (counts/min/day) was evaluated by a triaxial accelerometer [
13]. We detected no association between sleep quality and physical function measures such as grip strength, gait speed, and weight loss in the present participants, which suggests the possibility that sleep quality does not directly impact performance. The average age of the earlier study's subjects was higher, and the study's authors did not consider the influence of activity levels and exercise. The lack of a significant association with the risk of physical pre-frailty and frailty in the MVA
+SLP
− group can be attributed to the prominence of fatigue as the only risk factor. A study of community-dwelling older adults reported that compared to the group of subjects who had the 'usual' sleep pattern of 6–8 hr, the long-sleep group (≥8 hr) were at a higher risk of sarcopenia [
36]. Our present study included individuals with long sleep durations among those with good sleep quality, and their presence may have influenced the results. However, given the interaction between sleep quality and MVPA concerning physical frailty, it might not necessarily imply a higher probability of being frail for individuals meeting MVPA criteria and having poor sleep quality compared to those without poor sleep quality. The limited number of individuals in the group meeting both poor sleep quality and MVPA criteria could have affected the low statistical power, leading to non-significant findings.
We also observed that the present participants who had good sleep quality but did not meet the criteria for MVPA were at a higher risk of physical pre-frailty and frailty. Their group showed a higher risk of slow gait speed and low physical activity. MVPA as we defined it is recommended by the WHO to reduce the risk of diseases such as stroke, cardiovascular disease, cancer, and diabetes. Considering that the criteria for MVPA suggested by the WHO typically indicate higher levels of activity compared to the PAEE criteria, it is plausible that the reason why both groups meeting MVPA criteria did not exhibit a higher risk of physical frailty was due to meeting sufficient PAEE requirements. A positive association between physical activity levels and gait speed has been described [
37]. When physical activity levels are low, there is a decrease in high-intensity activities such as walking at a brisk pace and movements requiring lower-limb strength in exercise and daily activities. This leads to a decrease in lower-limb strength and balance, resulting in a higher risk of slow gait speed and low physical activity [
38]. Thus, despite good sleep quality, the association between slow gait speed and not meeting MVPA criteria might suggest a potential link with the risk of physical frailty.
Among the present participants, poor sleep quality and a failure to meet the MVPA criteria were associated with a higher risk of physical pre-frailty and frailty. An interaction between MVPA and sleep quality was also observed in relation to physical pre-frailty and frailty. When sleep quality declines, the basal metabolic rate decreases, leading to reduced energy expenditure. As energy expenditure decreases, there may be insufficient energy available for maintaining muscle mass and physical functions, resulting in muscle atrophy and decreased muscle strength [
1]. Moreover, the reduction in energy expenditure can impact immune function and decrease the body's resistance, potentially leading to increased susceptibility to illnesses and subsequent decline in physical function. Additionally, the decline in sleep quality might hinder muscle repair and growth during sleep, potentially contributing to a decrease in muscle mass and strength. Consequently, this decrease in physical activity may further contribute to a reduction in energy expenditure. As mentioned earlier, individuals who do not meet the criteria for MVPA are associated with a higher risk of slow gait speed and low physical activity, even if they have good sleep quality, and they are independently at a higher risk of physical frailty. Poor sleep quality is associated with a higher risk of psychological stress, which synergistically contributes to the increased risk of physical pre-frailty and frailty.
The strength of this study lies in our consideration of the influence of sleep quality on the association between MVPA and physical pre-frailty and frailty. Another strength of this study is that the participants' MVPA was assessed using accelerometers and defined based on moderate-to-vigorous physical activity (MPA and VPA), allowing for the objective measurement of activity levels rather than relying on self-report questionnaires.
Several study limitations must be addressed, however. Out of 5000 elderly residents in the region invited for this study, the response rate was low at 18.6%. Therefore, there are certain limitations to the generalizability of the research findings. The study's cross-sectional design prevents any conclusion regarding causality. The longitudinal relationship between the combination of MVPA plus sleep quality and the risk of physical frailty should be examined in future research. Our assessment of sleep quality relied on questionnaires, which may be subject to recall bias; objective measures of sleep quality should be employed in future studies. In this study, we classified physical activity and sleep quality based on cutoffs that have been considered important for health in previous research. However, whether these cutoffs are optimal as indicators for physical frailty remains a subject for future investigation. Both the PAEE, a component of the outcome physical frailty, and the exposure factor MVPA were assessed for activity intensity using the same physical activity monitor. Therefore, one possible explanation for the observation that both groups meeting MVPA criteria did not have a higher risk of physical frailty could be attributed to these groups meeting sufficient PAEE requirements. However, meeting the MVPA criteria recommended by the WHO is associated with the criteria for low physical activity (a component of physical frailty), suggesting the potential of meeting the MVPA criteria as a beneficial indicator for older adults. The characteristics of movements in older individuals have shown an underestimation of high-intensity physical activity compared to younger individuals. This suggests the potential presence of participants within the group meeting high MVPA criteria but not categorized as meeting MVPA. However, the authors believe that the results of this study remain consistent within the group meeting MVPA criteria.
5. Conclusions
The results of this study demonstrated that older adults who did not meet the criteria for MVPA levels is associated with higher odds of physical pre-frailty and frailty, regardless of whether or not their sleep quality was impaired. In the future, it is crucial to comprehend both aspects of physical activity levels and sleep quality among older adults in community settings. Furthermore, there is a need for ongoing investigations to longitudinally examine whether the status of MVPA and sleep quality heightens the risk of physical frailty.
Author Contributions
Conceptualization, T.Y., H.Y. T.C., X.L., W.L. and H.K.; methodology, T.Y. T.C., X.L., and H.K.; software, H.Y. and X. L.; validation, T.Y. and H.K.; formal analysis, T.Y.; investigation, T.Y., H.Y. T.C., X.L. and H.K.; resources, H.K.; data curation, T.Y., H.Y. T.C. and X.L.; writing—original draft preparation, T.Y.; writing—review and editing, T.Y., H.Y. T.C., X.L., W.L. and H.K.; visualization, T.Y.; supervision, H.K.; project administration, H.K.; funding acquisition, H.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported in part by Grants-in-Aid for Scientific Research (B) (JP 20H04016 and JP 20H04030) and (C) (JP23K10763 and JP 20K11446) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; by Itoshima City (j2023-65), Asanohi Orthopaedic Clinic (k2022-634). None of the funding sources had any role in the study design, data analysis, data interpretation, writing of the manuscript, or decision on the submission of this manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Kyushu University (approval no. 201708).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
We thank all of the study participants, the faculty and laboratory members who advised us on this research, and the staff of the Division of Health and Welfare of Itoshima City.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| ANOVA |
analysis of variance |
| BMI |
body mass index |
| CI |
confidence intervals |
| MET |
metabolic equivalent of task |
| MMSE |
Mini-Mental State Examination |
| MPA |
moderate physical activity |
| MVPA |
moderate-to-vigorous physical activity |
| OR |
odds ratios |
| PAEE |
physical activity energy expenditure |
| PSQI |
Pittsburgh Sleep Quality Index |
| ST |
sedentary time |
| VPA |
vigorous physical activity |
| WHO |
World Health Organization |
References
- Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:146-156. [CrossRef]
- Katsuya, I. Katsuya I. Older people and society (including oral frailty). The Japanese Society of Internal Medicine 2018;107:2469-2477. [in Japanese]. [CrossRef]
- Chen S, Honda T, Narazaki K, Chen T, Kishimoto H, Kumagai S. Physical frailty and risk of needing long-term care in community-dwelling older adults: A 6-year prospective study in Japan. J Nutr Health Aging 2019;23:856-861. [CrossRef]
- Matthew CL, Sonnega AJ, Resciniti NV, Leggett AN. Lohman. Frailty phenotype and cause-specific mortality in the United States. J Gerontol A Biol Sci Med Sci 2020;75:1935-1942. [CrossRef]
- Negm AM, Kennedy CC, Thabane L et al. Management of frailty: A systematic review and network meta-analysis of randomized controlled trials. JAMDA 2019;20:1190-1198. [CrossRef]
- Blodgett J, Theou O, Kirkland S, Andreou P, Rockwood K. The association between sedentary behaviour, moderate-vigorous physical activity and frailty in NHANES cohorts. Maturitas 2015;80:187-191. [CrossRef]
- Chen S, Chen T, Kishimoto H, Yatsugi H, Kumagai S. Associations of objectively measured patterns of sedentary behavior and physical activity with frailty status screened by The Frail Scale in Japanese community-dwelling older adults. J Sports Sci Med 2020;19:166-174. PMCID: PMC7039012.
- Yokote T. Associations between various perspectives of activity and physical frailty in older Japanese: A cross-sectional study. In press. [CrossRef]
- Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 2004;27:1255-1273. [CrossRef]
- Moreno-Tamayo K, Manrique-Espinoza B, Ortiz-Barrios LB, Cardenas-Bahena A, Ramirez-Garcia E, Sanchez-Garcia S. Insomnia, low sleep quality, and sleeping little are associated with frailty in Mexican women. Maturitas 2020;136:7-12. [CrossRef]
- Shih AC, Chen LH, Tsai CC, Chen JY. Correlation between sleep quality and frailty status among middle-aged and older Taiwanese people: A community-based, cross-sectional study. Int J Environ Res Public Health. 2020;17:9457. [CrossRef]
- Sun XH, Ma T, Yao S, Chen ZK, Xu WD, Jiang XY, Wang XF. Associations of sleep quality and sleep duration with frailty and pre-frailty in an elderly population Rugao longevity and ageing study. BMC Geriatr. 2020;20:9. [CrossRef]
- Kim M, Yoshida H, Sasai H, Kojima N, Kim H. Association between objectively measured sleep quality and physical function among community-dwelling oldest old Japanese: A cross-sectional study. Geriatr Gerontol Int 2015;15:1040-1048. [CrossRef]
- Kubala AG, Buysse DJ, Brindle RC et al. The association between physical activity and a composite measure of sleep health. Sleep Breath 2020;24:1207-1214. [CrossRef]
- Chen S, Chen T, Kishimoto H, Susaki Y, Kumagai S. Development of a Fried Frailty Phenotype Questionnaire for use in screening community-dwelling older adults. J Am Med Dir Assoc 2020;21:272-276. [CrossRef]
- Tsutsui T, Muramatsu N. Care-needs certification in the long-term care insurance system of Japan. J Am Geriatr Soc 2005;53:522-527. [CrossRef]
- Liu X, Chen T, Chen S, Yatsugi H, Chu T, Kishimoto H. The relationship between psychological distress and physical frailty in Japanese community-dwelling older adults: A cross-sectional study. J Frailty Aging 2023;12:43-48. [CrossRef]
- Kessler RC, Andrews G, Colpe LJ et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002;32:959-976. [CrossRef]
- Chen S, Honda T, Chen T et al. Screening for frailty phenotype with objectively-measured physical activity in a west Japanese suburban community: Evidence from the Sasaguri Genkimon Study. BMC Geriatr 2015;15:36. [CrossRef]
- Narazaki K, Matsuo E, Honda T, Nofuji Y, Yonemoto K, Kumagai S. Physical fitness measures as potential markers of low cognitive function in Japanese community-dwelling older adults without apparent cognitive problems. J Sports Sci Med 2014;13:590-596. PMCID: PMC4126296.
- Nagayoshi S, Yatsugi H, Xin L, Saito T, Yamatsu K, Kishimoto H. Evaluation of physical activity assessment using a triaxial activity monitor in community-dwelling older Japanese adults with and without lifestyle-related diseases. JMPB 2023;6:264-270. [CrossRef]
- Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc 2005;37:S531-S543. [CrossRef]
- Murphy, SL. Murphy SL. Review of physical activity measurement using accelerometers in older adults: Considerations for research design and conduct. Prev Med (Baltim) 2009;48:108-114. [CrossRef]
- Ohkawara K, Oshima Y, Hikihara Y, Ishikawa-Takata K, Tabata I, Tanaka S. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br J Nutr 2011;105:1681-1691. [CrossRef]
- Nagayoshi S, Oshima Y, Ando T, Aoyama T, Nakae S, Usui C, Kumagai S, Tanaka S. Validity of estimating physical activity intensity using a triaxial accelerometer in healthy adults and older adults. BMJ Open Sport Exerc Med. 2019;5:e000592. [CrossRef]
- World Health Organization. WHO guidelines on physical activity and sedentary behavior. 2020. https://www.who.int/publications/i/item/9789240015128. [accessed 3. 06. 2023].
- Doi Y, Minowa M, Uchiyama M, et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res 2000;97:165-172. [CrossRef]
- Collard RM, Boter H, Schoevers RA, Voshaar RCO. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012;60:1487-92. [CrossRef]
- Katewongsa P, Yousomboon C, Haemathulin N, RasriN, Widyastari DA. Prevalence of sufficient MVPA among Thai adults: Pooled panel data analysis from Thailand’s surveillance on physical activity 2012–2019. BMC Public Health 2021;21:665. [CrossRef]
- Zitser J, Allen IE, Falgas N, et al. Pittsburgh Sleep Quality Index (PSQI) responses are modulated by total sleep time and wake after sleep onset in healthy older adults. PLOS ONE 2022;17:e0270095. [CrossRef]
- Blodgett J, Theou O, Kirkland S, Andreou P, Rockwood K. The association between sedentary behaviour, moderate-vigorous physical activity and frailty in NHANES cohorts. Maturitas 2015;80:187-191. [CrossRef]
- Castaneda-Gameros D, Redwood S, Thompson JL. Physical activity, sedentary time, and frailty in older migrant women from ethnically diverse backgrounds: A mixed-methods study. J Aging Phys Act 2018;26:194-203. [CrossRef]
- Goldman SE, Ancoli-Israel S, Boudreau R, et al. Suzanne E Goldman. Sleep problems and associated daytime fatigue in community-dwelling older individuals. J Gerontol A Biol Sci Med Sci 2008;63:1069-1075. [CrossRef]
- Hita-Contreras F, Martínez-Amat A, Cruz-Díaz D, et al. Sleep quality and its association with postural stability and fear of falling among Spanish postmenopausal women. Menopause 2018;22:62-69. [CrossRef]
- Dattilo M, Antunes H K, Medeiros A, et al. Sleep and muscle recovery: Endocrinological and molecular basis for a new and promising hypothesis. Medical hypotheses. Med Hypotheses 2011;77:220-222. [CrossRef]
- Shibuki T, Iida M, Harada S, et al. The association between sleep parameters and sarcopenia in Japanese community-dwelling older adults. Arch Gerontol Geriatr 2023;109:104948. [CrossRef]
- Spartano NL, Lyass A, Larson MG, et al. Objective physical activity and physical performance in middle-aged and older adults. Exp Gerontol 2019;119:203-211. [CrossRef]
- Ramsey KA, Rojer AGM, D`Andrea L, et al. The association of objectively measured physical activity and sedentary behavior with skeletal muscle strength and muscle power in older adults: A systematic review and meta-analysis. Ageing Res Rev 2021;67:101266. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).