1. Introduction
The overall pattern of the coronavirus pandemic has been a series of COVID-19 waves: the number of infections increasing and decreasing repeatedly over time. People’s choice of protective measures changed accordingly. At the onset of the pandemic when COVID-19 vaccines were not available publicly, nonpharmaceutical interventions (NPIs) were the only effective measures to contain the pandemic [
2]. NPIs include personal measures, physical distancing, movement restrictions, and specific protection measures for vulnerable groups [
3], which serve as essential safeguards against direct contact with COVID-19 viruses. Previous research showed that although either vaccination or NPIs alone can provide a satisfactory protection, the best protection comes from the implementation of both measures together [
1]. However, people seemed to be less favorable to NPIs. This might be true for some NPIs, such as lockdowns, that have significant socioeconomic costs and may adversely affect individual well-being [
4,
5]. However, personal NPIs also appeared to be less favored [
6], despite their lower costs and their effectiveness in preventing COVID-19 transmission, such as mask-wearing [
7].
The reluctance to adopt personal NPIs may have something to do with individuals’ risk preferences. For instance, previous research found that people prone to risky decision-making performed less mask-wearing and social-distancing behaviors [
8]. However, a small proportion of risk-seeking individuals cannot fully explain the widespread resistance to personal NPIs (e.g., mask-wearing). Instead, the underlying reason why a majority of people do not adhere to the recommended personal NPIs may stem from an evaluation of their risk perception of COVID-19, and such an evaluation can be dynamic throughout the pandemic [
9].
Risk perception refers to an individual’s feeling and understanding of objective risks in the outside world [
10]. It is suggested that the risk perception of COVID-19 consists of two components. First, the cognitive component, such as understanding of the COVID-19 fatality rate and the perceived risk of being infected. Second, the emotional component, such as the fear of being infected and the scariness of COVID-19. These two components in the COVID-19 risk perception have been reported as positively correlated with each other in previous research [
11]. Also, previous research has indicated that individual’s willingness to receive the COVID-19 vaccination was correlated with their emotions, such as scariness and worry [
12,
13,
14]. In addition to vaccination, research has reported that people’s emotions about COVID-19, such as fear, anxiety, and worry can predict their willingness to adopt NPIs [
15,
16,
17]. These results are consistent with the risk-as-feelings model [
18]. In this model, when a risk is unknown and uncommon, our reaction to it is instinctive and intuitive [
19]. However, when people get used to a risk, such as being exposed to it for a long time, their perceived risk decreases [
20]. Thus, they may decrease protective reactions to maintain the risk.
At the time when we conducted this study, Taiwanese people had learned COVID-19 from mass media, social media, and/or other medium for two years. Thus, according to the risk-as-feelings model, people may decline to adopt personal NPIs because they got used to COVID-19, which is our first hypothesis. In addition to risk-as-feelings model, the Peltzman effect [
21] might also be the interpretation to the incline in adopting personal NPIs. This effect states that people are more likely to engage in risky behavior when security measures have been mandated. For instance, when the use of seatbelts is mandated, people would correspondingly drive with less attentiveness. Similarly, it is conceivable that a false sense of security resulting from vaccination could lead to risky behaviors in response to COVID-19, such as ceasing to wear masks. This is our second hypothesis. In order to clarify which hypothesis might be correct, two surveys were administered before and during the first outbreak of COVID-19 in Taiwan.
2. Materials and Methods
2.1. Study Sample
For Survey 1, data were collected by sharing the URL for access to the online questionnaire on the three most popular social media platforms in Taiwan: Facebook, PTT, and Dcard. The data collection period was from January 22 to February 28, 2022, during which three prize draws were conducted. Participants had the chance to win ten NT$300 (US$10), ten NT$200 (US$6.67), and five NT$200 as lottery prizes, respectively. To maximize the response rate upon questionnaire release, participants who did not win in one prize draw were automatically entered into the next prize draw. In total, 406 participants were recruited for the first survey.
Survey 2 was conducted from May 18 to June 29, 2022, using the same prize draw procedure as in Survey 1. A total of 505 participants were recruited for the second survey. All participants were adults (>18 years old) and gave written consent before attending the survey. Data collection was anonymous, and no personal information was collected, except age. A priori power analysis for SEM showed that our sample sizes were sufficiently large for both surveys. Details of the power analysis will be provided in the Results section.
The Taiwanese government had been implementing NPIs at a high stringency level since early 2020, resulting in a relatively flat curve of confirmed cases and deaths for about two years. However, during the Omicron outbreak in early 2022, the Taiwanese government shifted its prevention policy from zero-COVID-19 to coexisting with the virus, while still maintaining personal NPIs. The daily confirmed cases increased significantly from around 60 new cases (during Survey 1) to over 60,000 cases every day (during Survey 2) [
22]. The differences between the data of these two surveys could reveal changes in people’s risk perception to COVID-19 along the development of the Omicron wave.
2.2. Study Design
In this study, we administered two cross-sectional surveys with a same questionnaire to investigate different participants’ recognized severity of COVID-19, perceived worry of COVID-19, intention to adopt personal NPIs, and attitude toward COVID-19 vaccines.
2.3. Instruments
The questionnaire used in this study is listed in
Table 1, which consists of two parts. The first part aims to collect demographic data, including age and the number of COVID-19 vaccine doses taken. In Survey 2, as the daily confirmed case increased significantly, an additional question was included to inquire about how many times they had been tested positive for COVID-19.
The second part of the questionnaire was designed to investigate participants’ understanding of the severity of COVID-19, worry level about COVID-19, attitude toward COVID-19 vaccines, intention to adopt personal NPIs, and rating for specific events related to the pandemic to happen. Participants were asked to provide a number between 0 and 100 to represent their ratings for each item. For example, the question “What is the probability you think that you will get infected by Omicron?” allowed participants to respond with a number between 0% (indicating no chance) and 100% (indicating a firm belief of being infected). The descriptions of all items and their corresponding concepts are provided in
Table 1.
2.4. Statistical Analyses
First, comparisons on general characteristics of these two samples were described. Second, we used the R package {lavaan} [
23] to conduct multigroup SEM for the data of these two samples. We would test to what extent these two samples can be viewed as equal with different models from assuming that the structural models for these two samples have the same configure to assuming that even the parameters have the same values for these two samples. This check can help us explain the differences between the two samples.
3. Results
3.1. Comparisons on Demographic Characteristics between Two Samples
The age distributions in Survey 1 (M = 28.67 years, SD = 7.17 years) and Survey 2 (M = 28.41 years, SD = 7.79 years) were similar, and the difference between their mean ages was not significant [
,
]. More participants received three doses of COVID-19 vaccines in Survey 2 compared to Survey 1 (see
Table 2 for more details). The proportion of participants testing positive in Survey 2 was 6.93%, which was close to the COVID-19 prevalence rate of 7.99% in Taiwan at that time [
22].
3.2. Multigroup SEM
We conducted multigroup SEM to assess to what extent these two samples exhibit invariance by comparing four structural models. These models respectively assumed configural invariance for the two samples (i.e., only the configure of the structural model is the same for them), measurement invariance (i.e., the configure of the structural model and the factor loadings on observed items are the same), scalar invariance (i.e., the factor loadings and the intercepts of latent variables are the same), and residual invariance (i.e., the factor loadings, the intercepts of latent variables, and the residual of each regression formula are the same). Apparently, latter models set more constraints on invariance than previous ones do. Thus, we compared every two models sequentially from the model with the least constraint to the one with the most constraint.
The results showed that the modeling performance started to significantly drop in the model assuming scalar invariance, compared with the model assuming measurement invariance [AIC = 219 and BIC = 175, , ]. It is suggested that measurement invariance is held for these two samples. That is, these two samples are equivalent in terms of the constitution of the mental constructs of our interest, even though the data were collected in a cross-sectional design. This result also provides support for the construct validity of our questionnaire. In the model assuming measurement invariance, all parameters except the factor loadings on the observed items were estimated separately for each sample.
3.2.1. Measurement Model and Structural Model
The measurement model for the two samples consists of four latent variables. They are worry about COVID-19 (indicated by items Q2, Q3, Q4, and Q19 in the questionnaire), severity of COVID-19 (indicated by Q7, Q8, and Q9), attitudes toward COVID-19 vaccines (indicated by Q10, Q11, and Q12
2), and intention to adopt personal NPIs (indicated by Q16, Q17, and Q18). All item scores were transformed into z-scores before constructing the latent variables. The composite reliabilities of the four latent variables in the measurement model for Survey 1 are mostly satisfactory (i.e.,
, according to [
24]) [0.82, 0.66, 0.81, and 0.81, respectively, for the latent variables Worry, Severity, NPIs, and Vaccines]. The measurement model for Survey 2 also demonstrate good reliabilities for the four latent variables [0.81, 0.53, 0.83, and 0.81, respectively, for Worry, Severity, NPIs, and Vaccines]. The lower reliability for Severity might be due to the high skewness of the distributions for Q7, Q8, and Q9 (see
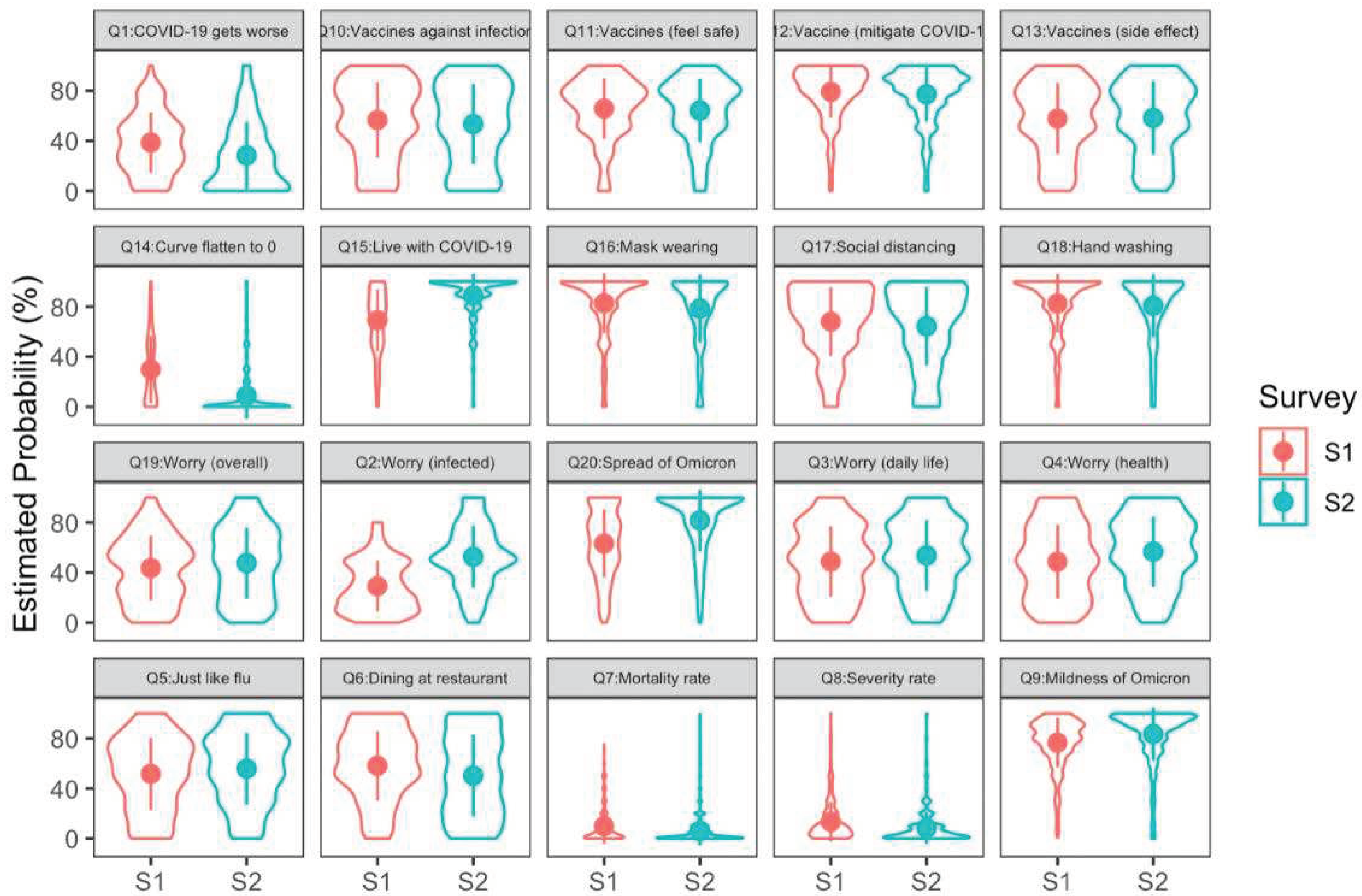
Figure 1). As a compensatory measure, we increased the reliability of Severity to 0.76 (in Survey 1) and 0.70 (in Survey 2) by using the square roots of these item scores. However, in order to maintain consistency across all items, we continued to use z-scores.
Both measurement models exhibit a good construct validity, as the average variance extracted for Worry, Severity, NPIs, and Vaccines are all > 0.5 [
25], with 0.56, 0.63, 0.58, and 0.61 for Worry, Severity, NPIs, and Vaccines in Survey 1, and 0.53, 0.53, 0.61, and 0.58 for the same latent variables in Survey 2. See
Table 3 for the statistics of the factor loadings, all of which are significant.
The optimal structural model performed pretty well, as shown by the goodness-of-fit indices [
,
,
,
,
, and
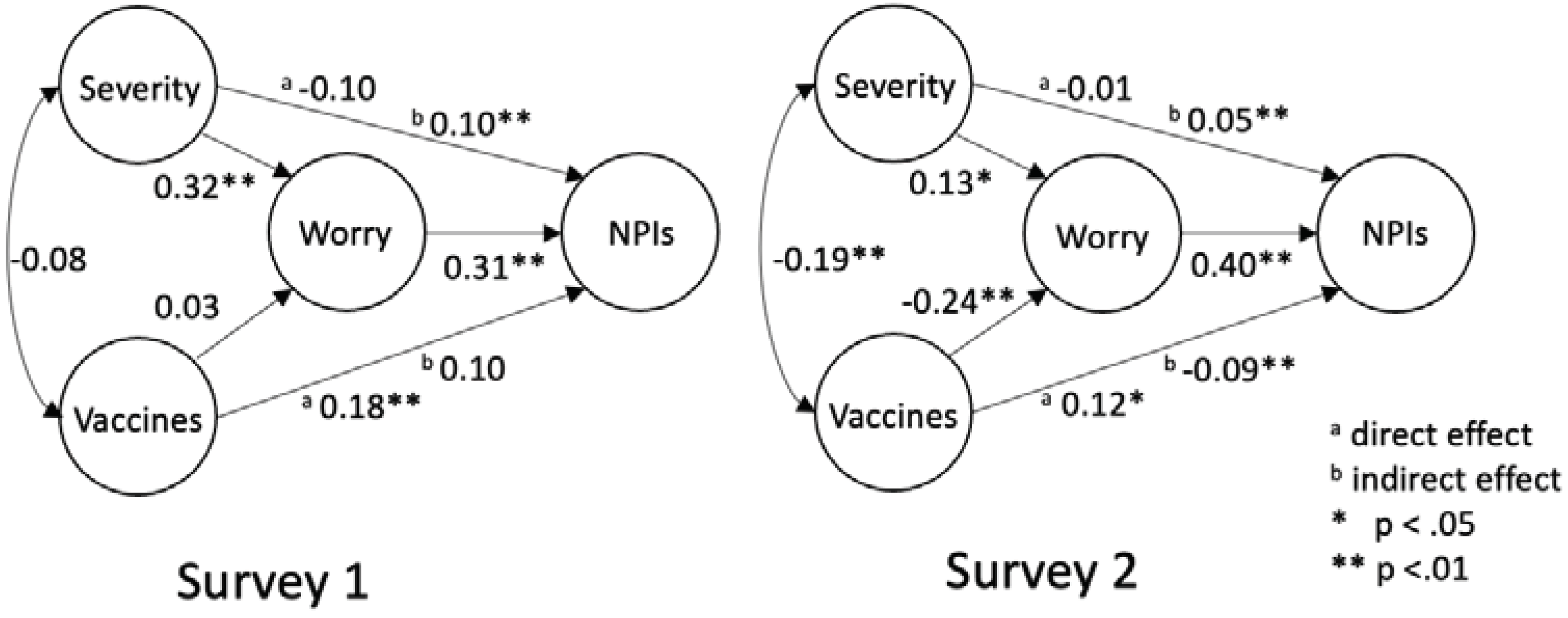
]. The scheme of this model can be seen in
Figure 2. This structural model consists of four latent variables and 13 observed items in total. A priori power analysis for this model, with the anticipated power set as 0.80, effect size set as 0.30, and type I error set as 0.05, suggested that the minimum sample size should be 166. Either of our surveys recruited more than 166 participants, guaranteeing the power of this structural model to be 0.80 at least.
3.2.2. Worry Fully Mediated the Influence of Severity on NPIs
The two latent variables Severity and Worry are treated as the cognitive and emotional components of the risk perception of COVID-19. In
Figure 2, for no matter which sample, Severity positively predicts Worry. This is consistent with the previous finding [
11]. NPIs representing the intention to adopt personal NPIs is predicted by Worry directly, but not by Severity directly, suggesting that the reaction to COVID-19 is driven by the emotional component of the risk perception of COVID-19. This finding supports the risk-as-feelings model. However, two points deserves attention. First, NPIs are driven by Worry in Survey 2. This result suggests that the participants in Survey 2 had not yet been habituated to COVID-19. Second, while there is no direct effect of Severity on NPIs, the indirect effect of Severity on NPIs is significant with Worry as the mediator for both samples. Thus, it is not appropriate to argue that the cognitive component of risk perception has nothing to do with the reaction to a risk. Instead, the effect of the cognitive component is fully mediated by the emotional component, hence elaborating the theoretical relationships between risk-as-analysis and risk-as-feelings models [
18] in a systematic view.
3.2.3. Worry Increased during the Outbreak
In order to examine if there is any change on people’s perceived severity of COVID-19, worry about COVID-19, attitude toward COVID-19 vaccines, and intention to adopt NPIs, we compared the means of the four latent variables between the two surveys. The results showed that compared with Survey 1, the participants in Survey 2 perceived COVID-19 as less severe [, ], were more worried about COVID-19 [, ], but would be less willing to adopt the personal NPIs [, ]. The attitude toward COVID-19 vaccines was not changed between these surveys [, ]. The decline in the intention to adopt NPIs might not result from the habituation to COVID-19, as the worry level in Survey 2 was higher than that in Survey 1 the other way around. If people got used to COVID-19, the worry level should have been lower in the second survey. Also, Worry can still predict NPIs in Survey 2, as does in Survey 1. These results converge toward rejection of the hypothesis that the incline in willingness to adopt personal NPIs results from people’s habituation to COVID-19.
3.2.4. Vaccine Attitudes Affected NPI Adoption, Implying the Peltzman Effect
Now we turn to verify the other hypothesis that the incline in adoption of NPIs might reflect the Peltzman effect brought by vaccines. As shown in
Figure 2, there are two regression paths from Vaccines to Worry and NPIs respectively. In Survey 1, the regression weight from Vaccines to Worry is not significant [
,
], suggesting that the participants’ worry about COVID-19 could not be predicted by their attitude toward vaccines. However, the direct effect of Vaccines on NPIs is significant [
,
], suggesting that a more positive attitude toward vaccines is associated with a greater willingness to adopt personal NPIs. This is not surprising, as vaccines and NPIs are both the prevention measures for COVID-19. One who believes the effect of vaccines on maintaining COVID-19 would more like to adopt personal NPIs to block the contact to COVID-19.
In Survey 2, Vaccines negatively predicted Worry [, ], meaning that a more positive attitude toward vaccines is associated with less worry about COVID-19. Perhaps, this is because people in Survey 2 realized the protective effect of vaccination (e.g., mild symptoms) during the outbreak. As Worry positively predict the intention to adopt NPIs [, ], a decreasing worry level leads to a lower intention to adopt NPIs. This inference is supported by the significant negative indirect effect of Vaccines on NPIs with the mediation of Worry [, ]. This negative effect suggests the occurrence of the Peltzman effect. Here in this case, people felt safer after having received COVID-19 vaccination, that in turn relaxed their alert and decreased their intention to adopt personal NPIs continuously. One important point to note is that the direct effect of Vaccines on NPIs is positive and significant [, ]. This indicates that the effect of Vaccines on NPIs is not entirely replaced by Worry. Thus, it suggests that worry about COVID-19 serves as a partial mediator in the path from the attitudes toward vaccines to the intention to adopt NPIs. However, the worry about COVID-19 acts as a full mediator in the path from the perceived severity of COVID-19 the intention to adopt NPIs.
4. Discussion
In this study, we conducted two cross-sectional surveys to investigate how people’s risk perception of COVID-19, attitudes toward COVID-19 vaccines, and intention to adopt personal NPIs changed in correspondence to the evolving COVID-19 pandemic. Specifically, we would like to examine why people declined to adopt personal NPIs. To this end, we conducted multigroup SEM for these two samples. The major results are summarized here. First, we replicated the previous finding that the cognitive component is positively correlated with the emotional component in people’s risk perception of COVID-19 [
11]. Second, we elaborated the risk-as-feelings model [
18] with the finding that the influence of Severity on NPIs was fully mediated by Worry rather than absent. Third, the decline in people’s willingness to adopt NPIs in Survey 2 was confirmed as the occurrence of the Peltzman effect, not people’s habituation to COVID-19.
Previous studies put emphasis on how people’s risk perception would influence their reaction to COVID-19, such that the worry about being infected raised people’s willingness to receive vaccination [
12], consistent with risk-as-feelings model, or that people would underestimate the likelihood of being infected for themselves [
26], consistent with optimism bias [
27]. However, most of these studies did not take into consideration the relationships between protective measures (e.g., cooperative or competitive). In this study, we found that receiving vaccination might lower people’s alert that in turn declines their intention to adopt personal NPIs, namely the Peltzman effect. In addition to ours, one preprint paper also mentioned the Peltzman effect on personal NPIs induced by vaccination [
28]. More than their study, we demonstrated through SEM the path how vaccination induces the laxity in personal NPIs via lowering people’s worry about COVID-19. Our model provides a more systematic view to understand how people generate their reactions to COVID-19.
Why did previous studies seldom mention the Peltzman effect? One reason might be that these studies were published in the early period of COVID-19. At that time, the coverage ratio of vaccination for COVID-19 was not up to a satisfactory level. Thus, it would be less likely to observe the effect, if any, of having received vaccination on willingness to adopt NPIs. Unlike most European countries, the Taiwanese government has implemented stringent border quarantine until early 2022, that bought time for Taiwanese people to have well prepared for real outbreaks of COVID-19 (i.e., more than 90% Taiwanese people have received at least two doses of COVID-19 vaccines before the Omicron wave). This coincidentally made Taiwan a perfect place for natural experiments to examine the effect of COVID-19 vaccines. Here in this study, we found that although people were more worried about being infected during the Omicron wave, their intention to adopt NPIs declined instead, because of the Peltzman effect brought by having received vaccination.
Is it possible to have a reversed Peltzman effect on receiving vaccination? For instance, would it happen that people feel safer with wearing masks or keeping social distance and then refuse receiving vaccination? Theoretically, it is not impossible. However, vaccines have been proved as an effective means to maintain pandemics for decades. It is not surprising that vaccination was mandated worldwide but not NPIs. This might be the reason why a reversed Peltzman on receiving vaccination has not been reported. Nonetheless, researchers have shown that both vaccination and NPIs together can provide the best protection from COVID-19 [
1]. In addition, variants of SARS-CoV-2 (i.e., the virus causes COVID-19) may evade protection from existing vaccines. Thus, NPIs should not be neglected, as they provide a physical separation between us and viruses whether known or unknown. We would like to treat the results of this study as a notice for the public to keep alert for the occurrence of the Peltzman effect when trying to maintain COVID-19.
Study Limitations
This study has a few limitations that should be considered when interpreting the results. Firstly, the current cross-sectional, time-sequential, survey design used in the current study may introduce potential sampling bias and alternative explanations for the observed differences between the two surveys, as two different groups of participants were recruited in two data collections. However, a few reasons indicated that these two datasets were comparable. First, the multigroup SEM results indicated that both survey groups shared the same mental constructs and processing routes. Moreover, there was no age difference between the two groups. In addition, we distributed questionnaires on the same platforms at two time points, thus the same user groups were accessed. Therefore, we believe that the current cross-sectional approach can still bring some useful insights into the dynamics of risk perception during the pandemic, just like previous studies employing cross-sectional and time-sequential surveys to study cohort’s attitudes toward and reactions to COVID-19 [12,29-31].
Secondly, the use of single items instead of developed questionnaires for each mental construct can be seen as a limitation. Each of the mental constructs was assessed using three to four questions. Although normally using single items has some disadvantages, such as reduced precision and reliability, it is worth noting that the composite reliabilities and the construct validities were satisfactory in both surveys. Moreover, using single items allows for quicker data collection and minimizes the burden on participants, which is crucial given the rapidly changing pandemic situations. Similar usage of single items has been also seen in previous research [10-12,32], which we believe the same reasons apply to these studies. In addition, as a majority of participants were recruited from social media and platforms, our samples are biased toward younger adults between the ages from 18 to 40s. Thus, caution should be exercised when applying the current findings to older populations.
Lastly, the current study focused on specific aspects of risk perception, attitudes toward vaccines, and intention to adopt personal NPIs in response to the evolving pandemic. Other factors, such as cultural, political, or socioeconomic influences, were not thoroughly examined in this research. These unmeasured factors could potentially contribute to the observed behaviors and attitudes, and further research is needed to explore their impact on risk perception and preventive behaviors during the pandemic.
5. Conclusions
In this study, we examined why people declined to adopt personal NPIs during the COVID-19 wave with two hypotheses: habituated to COVID-19 or the Peltzman effect. Our results support the Peltzman effect, that having received vaccination lowers people’s worry about COVID-19, that in turn decreases their willingness to adopt personal NPIs. Specifically, the structural model proposed in this study clearly explains through what mental paths the risk-as-feelings model and the Peltzman effect can be accommodated.
Supplementary Materials
The following supporting information can be downloaded at:
www.mdpi.com/xxx/s1, Figure S1: title; Table S1: title; Video S1: title.
Author Contributions
Conceptualization, L.Y. (Lee-Xieng Yang) and C.L. (Chia-Yuan Lin); methodology, L.Y. (Lee-Xieng Yang); formal analysis, L.Y. (Lee-Xieng Yang); data curation, W.Z. (Wan-Zhen Zhan), B.C. (Bo-An Chiang), and E.C. (En-Chi Chang); writing—original draft preparation, L.Y. (Lee-Xieng Yang); writing—review and editing, C.L. (Chia-Yuan Lin). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of National Chengchi University, Taiwan (NCCU-REC-202205-I030).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of Interest
The authors declare no conflict of interest.
Notes
| 1 |
June for Survey 2. |
| 2 |
Q13 was not included because the loading of it for constructing the latent variable of attitudes toward vaccines was not significant. |
References
- Ge, Y., Zhang, W. Bin, Wu, X., Ruktanonchai, C. W., Liu, H., Wang, J., Song, Y., Liu, M., Yan, W., Yang, J., Cleary, E., Qader, S. H., Atuhaire, F., Ruktanonchai, N. W., Tatem, A. J., & Lai, S. (2022). Untangling the changing impact of non-pharmaceutical interventions and vaccination on European COVID-19 trajectories. Nature Communications, 13(1). [CrossRef]
- Ge, Y., Zhang, W. Bin, Liu, H., Ruktanonchai, C. W., Hu, M., Wu, X., Song, Y., Ruktanonchai, N. W., Yan, W., Cleary, E., Feng, L., Li, Z., Yang, W., Liu, M., Tatem, A. J., Wang, J. F., & Lai, S. (2022). Impacts of worldwide individual non-pharmaceutical interventions on COVID-19 transmission across waves and space. International Journal of Applied Earth Observation and Geoinformation, 106. [CrossRef]
- World Health Organization. (2020). Calibrating long-term non-pharmaceutical interventions for COVID-19. In World Health Organization (Issue May).
- Barni, D., Danioni, F., Canzi, E., Ferrari, L., Ranieri, S., Lanz, M., Iafrate, R., Regalia, C., & Rosnati, R. (2020). Facing the COVID-19 Pandemic: The Role of Sense of Coherence. Frontiers in Psychology, 11. [CrossRef]
- Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., & Zheng, J. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research, 287. [CrossRef]
- Kollmann, J., Kocken, P. L., Syurina, E. V., & Hilverda, F. (2022). The role of risk perception and affective response in the COVID-19 preventive behaviours of young adults: A mixed methods study of university students in the Netherlands. BMJ Open, 12(1). [CrossRef]
- Wang, Y., Deng, Z., & Shi, D. (2021). How effective is a mask in preventing COVID-19 infection? MEDICAL DEVICES & SENSORS, 4(1). [CrossRef]
- Byrne, K. A., Six, S. G., Anaraky, R. G., Harris, M. W., & Winterlind, E. L. (2021). Risk-taking unmasked: Using risky choice and temporal discounting to explain COVID-19 preventative behaviors. PLOS ONE, 16(5), e0251073. [CrossRef]
- Xu, J., & Peng, Z. (2015). People at risk of influenza pandemics: The evolution of perception and behavior. PLoS ONE, 10(12). [CrossRef]
- Shen, Z., Zhong, Z., Xie, J., Ding, S., Li, S., & Li, C. (2021). Development and psychometric assessment of the public health emergency risk perception scale: Under the outbreak of COVID-19. International Journal of Nursing Sciences, 8(1), 87–94. [CrossRef]
- Yıldırım, M., & Güler, A. (2020). Factor analysis of the COVID-19 Perceived Risk Scale: A preliminary study. Death Studies. [CrossRef]
- Caserotti, M., Girardi, P., Rubaltelli, E., Tasso, A., Lotto, L., & Gavaruzzi, T. (2021). Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Social Science and Medicine, 272. [CrossRef]
- Hilverda, F., & Vollmann, M. (2022). The role of risk perception in students’ COVID-19 vaccine uptake: A longitudinal study. Vaccines, 10(1). [CrossRef]
- Vollmann, M., & Salewski, C. (2021). To get vaccinated, or not to get vaccinated, that is the question: Illness representations about covid-19 and perceptions about covid-19 vaccination as predictors of covid-19 vaccination willingness among young adults in the Netherlands. Vaccines, 9(9). [CrossRef]
- Harper, C. A., Satchell, L. P., Fido, D., & Latzman, R. D. (2021). Functional Fear Predicts Public Health Compliance in the COVID-19 Pandemic. International Journal of Mental Health and Addiction, 19(5). [CrossRef]
- Qin, H., Sanders, C., Prasetyo, Y., Syukron, M., & Prentice, E. (2021). Exploring the dynamic relationships between risk perception and behavior in response to the Coronavirus Disease 2019 (COVID-19) outbreak. Social Science and Medicine, 285. [CrossRef]
- Sobkow, A., Zaleskiewicz, T., Petrova, D., Garcia-Retamero, R., & Traczyk, J. (2020). Worry, Risk Perception, and Controllability Predict Intentions Toward COVID-19 Preventive Behaviors. Frontiers in Psychology, 11. [CrossRef]
- Slovic, P., Finucane, M. L., Peters, E., & MacGregor, D. G. (2004). Risk as Analysis and Risk as Feelings: Some Thoughts about Affect, Reason, Risk, and Rationality. In Risk Analysis (Vol. 24, Issue 2, pp. 311–322). [CrossRef]
- Slovic, P., Finucane, M. L., Peters, E., & MacGregor, D. G. (2007). The affect heuristic. European Journal of Operational Research, 177(3). [CrossRef]
- Slovic, P. (1987). Perception of risk. Science, 236, 280-285. [CrossRef]
- Peltzman, S. (1976). Toward a More General Theory of Regulation. The Journal of Law and Economics, 19(2). [CrossRef]
- Worldometer. (2023). [COVID-19 statistics in Taiwan]. https://www.worldometers.info/coronavirus/country/taiwan/#graph-deaths-daily.
- Rosseel, Y. (2012). Lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48. [CrossRef]
- Henseler, J., Dijkstra, T. K., Sarstedt, M., Ringle, C. M., Diamantopoulos, A., Straub, D. W., Ketchen, D. J., Hair, J. F., Hult, G. T. M., & Calantone, R. J. (2014). Common Beliefs and Reality About PLS: Comments on Rönkkö and Evermann (2013). Organizational Research Methods, 17(2). [CrossRef]
- Chan, S. H., & Lay, Y. F. (2018). Examining the reliability and validity of research instruments using partial least squares structural equation modeling (PLS-SEM). Journal of Baltic Science Education, 17(2). [CrossRef]
- Wise, T., Zbozinek, T. D., Michelini, G., Hagan, C. C., & Mobbs, D. (2020). Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States: COVID-19 risk perception and behavior. Royal Society Open Science, 7(9).
- Sharot, T. (2011). The optimism bias. Current Biology, 21, 941-945.
- Jia, J. S., Yuan Y., Jia, J., & Christakis, N. A. (2022). Risk perception and behaviour change after personal vaccination for COVID-19 in the USA. PsyArXiv.
- Attema, A. E., L’Haridon, O., Raude, J., & Seror, V. (2021). Beliefs and Risk Perceptions About COVID-19: Evidence From Two Successive French Representative Surveys During Lockdown. Frontiers in Psychology, 12. [CrossRef]
- Henk, K., Rosing, F., Wolff, F., Frenzel, S. B., van Dick, R., Erkens, V. A., Häusser, J. A., Mojzisch, A., & Boer, D. (2023). An examination and extension of the Peltzman effect during the Covid-19 pandemic. Current Research in Ecological and Social Psychology, 4. [CrossRef]
- Nguyen, Q. C., Yardi, I., Gutierrez, F. X. M., Mane, H., & Yue, X. (2022). Leveraging 13 million responses to the U.S. COVID-19 Trends and Impact Survey to examine vaccine hesitancy, vaccination, and mask wearing, January 2021-February 2022. BMC Public Health, 22(1). [CrossRef]
- Chen, Y., Feng, J., Chen, A., Lee, J. E., & An, L. (2021). Risk perception of COVID-19: A comparative analysis of China and South Korea. International Journal of Disaster Risk Reduction, 61. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).