1. Introduction
Infections involving the Retzius space are rare clinical practice, often characterized by patients presenting with vague and atypical symptoms, before preceding substantial abscess involving various extraperitoneal spaces. The complex anatomical planes within the extraperitoneal space provide a conduit for disease dissemination from distant etiology, posing diagnostic challenges that may hinder the timely implementation of definitive treatment. Thus, a comprehensive understanding of anatomy and a heightened awareness of potential management pitfalls are essential in navigating such clinical scenarios.
This study presents a case analysis of a Retzius space infection originating from a complex perirectal abscess, effectively managed. In addition, we also review the intricacies of anatomy, pathophysiology, and optimal treatment strategies associated with perirectal abscesses extending into the extraperitoneum.
2. Case Report
A 68-year-old male presented to the emergency department with dizziness and diffuse pain located in the lower abdomen over the previous 24 hours. He remained awake and alert, with no reported pain in other areas. Past medical history revealed hyperlipidemia and hypertension. Notably, there was no history of constipation or perianal infection. However, traced back to his illness from this emergent episode, he had experienced intermittent perianal pain for approximately one month. Initial consultations at local medical clinics had led to an impression of hemorrhoids. Despite topical and oral forms of medication, the pain persisted and discomforted him for a while. This time, upon admission, he was febrile (body temperature, 38.5°C), hypotensive (blood pressure, 96/62 mmHg), and slightly tachycardic (heart rate, 102 beats/minute), necessitating immediate administration of inotropic agents.
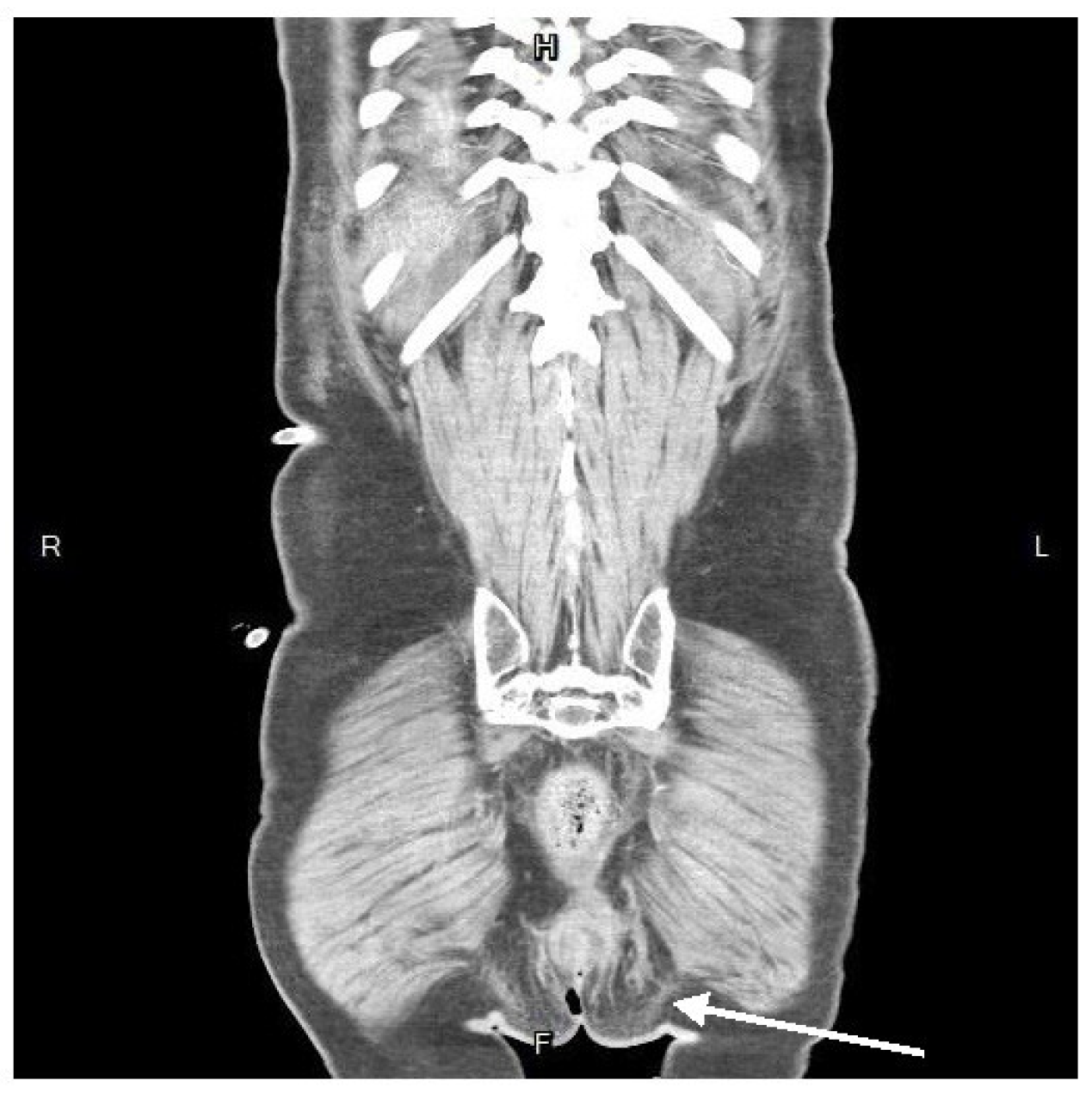
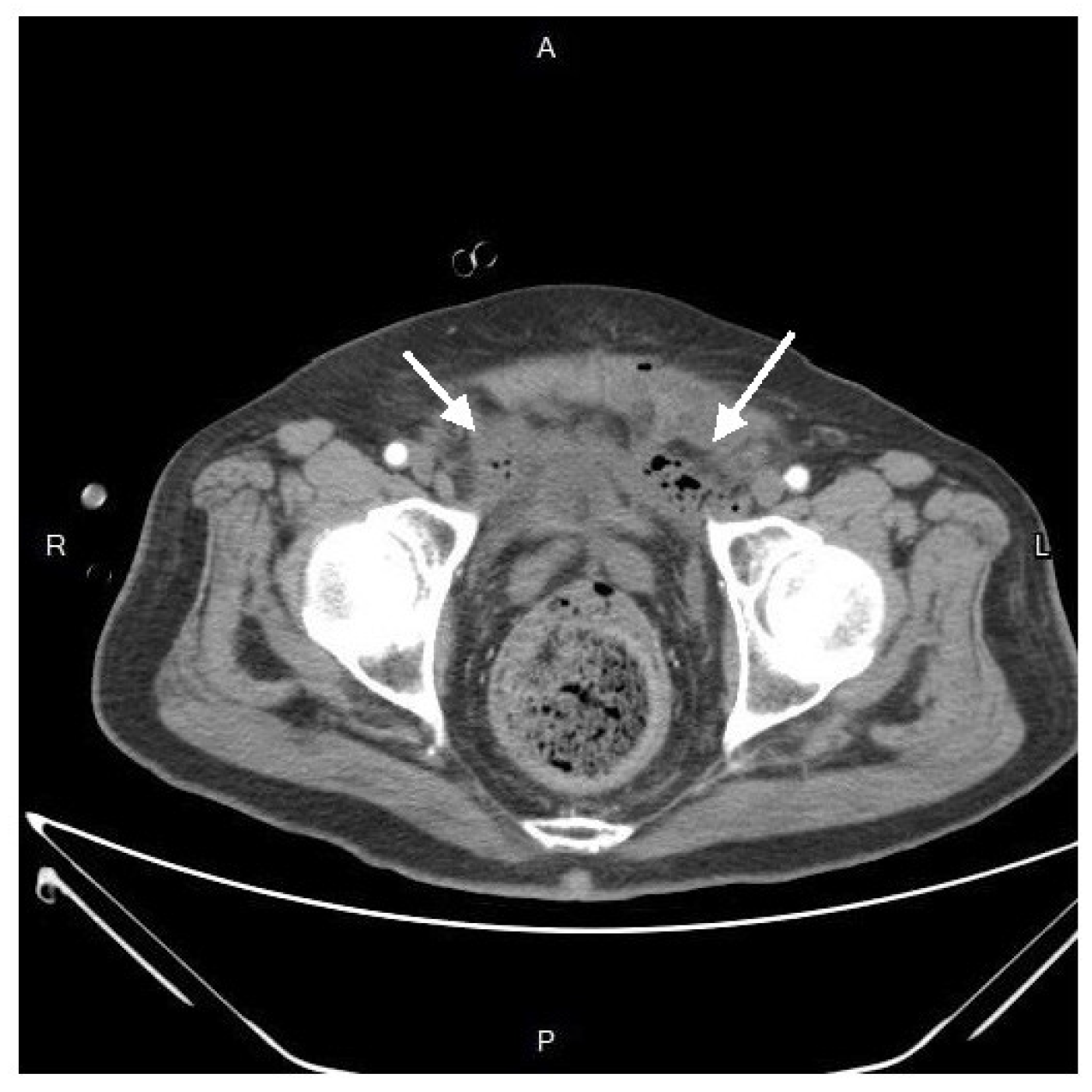
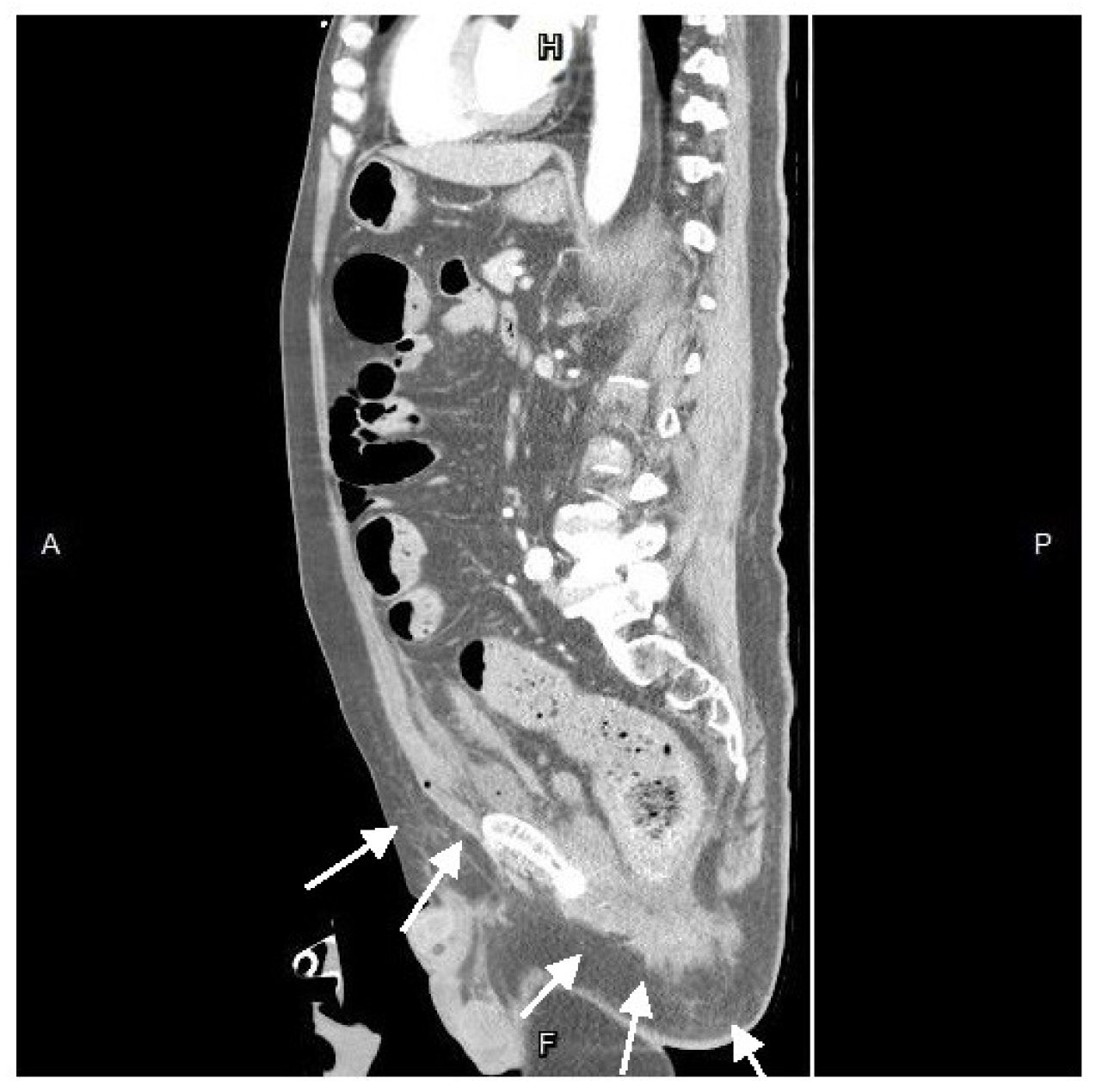
Physical examination revealed pain with deep palpation over the groin and suprapubic area, without rebounding tenderness or signs of deep vein thrombosis in the extremities. The digital rectal examination yielded negative of bloody discharge but noted mild nonspecific pain. The pain did not impact ambulation and normal gait and the strength testing was impaired. The patient did not report dysuria or increased urinary frequency. A plain abdominal radiograph was normal, and laboratory findings consisted of elevated white blood cell count and C-reactive protein (white blood cells, 27,830/μL; neutrophils, 90.6%; C-reactive protein, 21.65 mg/L). Abdominal contrast-enhanced computed tomography (CT) showed a heterogenous fluid-filled perianal abscess, 5.0x4.4x6.8 cm, (
Figure 1) in the left perianal region, with extraperitoneal air spreading through the abdominal wall fascia. (
Figure 2 and
Figure 3)
The blood cultures were drawn, and broad-spectrum empiric antibiotics were initiated. Following fluid resuscitation, the patient underwent incision and drainage in the 8 o’clock region, with the placement of a Foley tube for adequate drainage and irrigation. Subsequent dressing changes were performed regularly for proper hygiene. However, ten days later, the patient experienced sudden massive rectal bleeding with hypovolemic shock. Upon examination with an anal retractor, a bleeder was identified at the rectum in the 9 o’clock region, successfully managed by suturing ligation with 2-0 Vicryl. An emergent colonoscopy revealed no active bleeding or rectal ulcers. Simultaneously, an emergent abdomen and pelvic CT indicated no contrast medium extravasation in the bowel lumen or peritoneal space but identified an extraperitoneal abscess around the bladder.
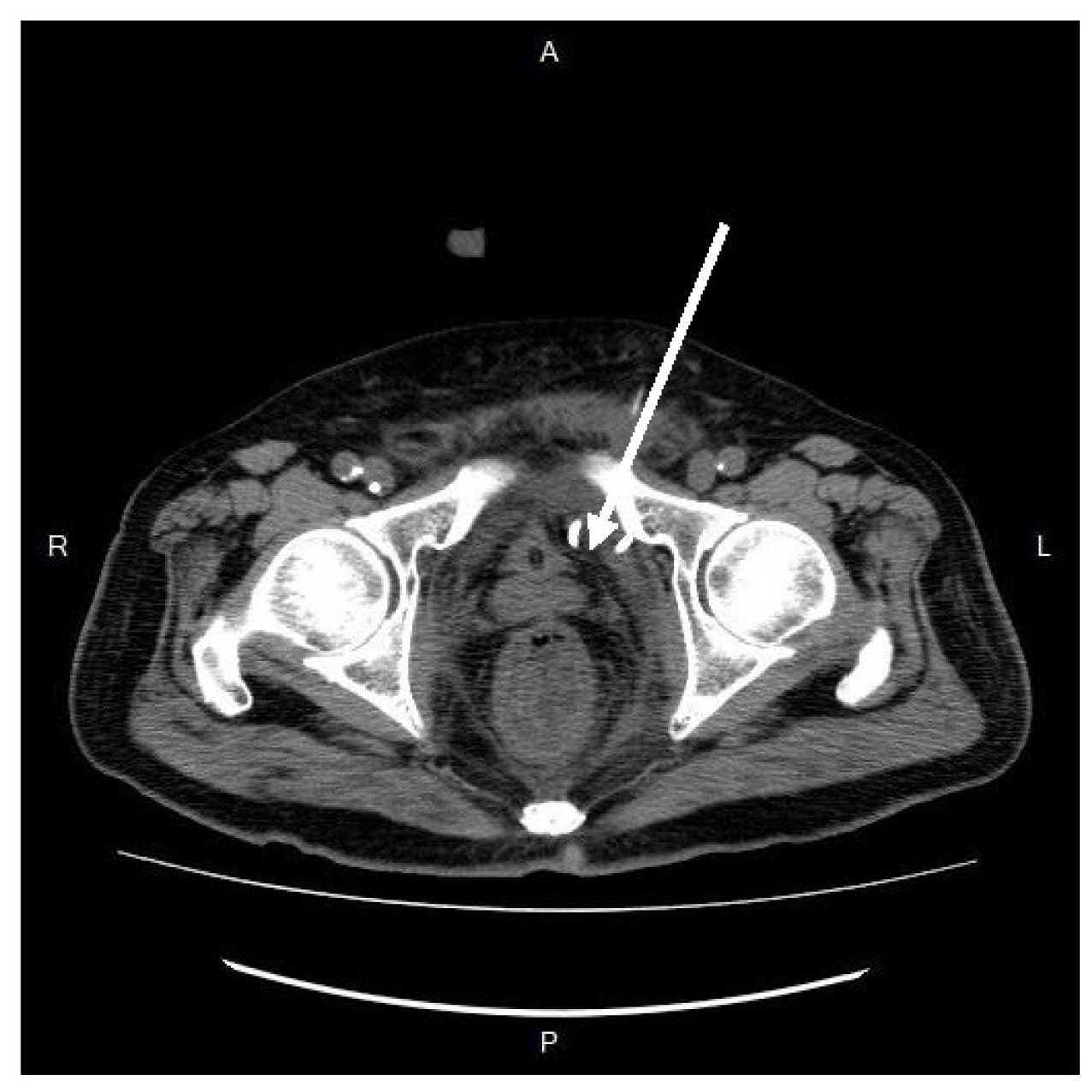
After resuscitation and blood transfusion, his vital signs stabilized, and the inotrope was tapered. Upon the next day, we consulted a radiologist for CT-guided extraperitoneal abscess drainage, (
Figure 4) collecting a considerable amount of turbid fluid. Cultures from the pus identified Klebsiella pneumoniae, Escherichia coli, Viridans streptococcus gr., and Bacteroides fragilis.
Within two weeks later, hypogastric pain and fever improved gradually. The patient became afebrile with normal laboratory values, letting him be discharged from the hospital. During the 3-month follow-up, there were no signs of recurrence or long-term complications. This study was approved by the Institutional Review Board of the Tri-Service General Hospital in Taiwan.
3. Discussion
The space of Retzius, also known as the prevesical or retropubic space, is delineated externally by the transversalis fascia and internally by the parietal peritoneum. Its lateral extension includes the space of Bogros below the inguinal ligament, housing iliofemoral vessels and iliopsoas muscles. Continuing posterolaterally, it is directly contiguous with the infrarenal retroperitoneal compartments and caudally extends to the supralevator extraperitoneal space. Also, anatomically, the supralevator space is a pelvic compartment above the levator ani muscle that communicates anteriorly with the space of Retzius, bilaterally with the retro-inguinal spaces, and posteriorly with the retroperitoneum. The puborectalis muscle may act as a barrier to inferior abscess expansion, although aggressive invasion may occur, facilitating infections spread through the anterior and posterior extraperitoneal abdominal compartments.
Via proofs of perfusion study and cadaver dissection, Chen et al1 demonstrated communication between the pararectal spaces and the vesical extraperitoneal space anteriorly. Owing to the umbilical-vesical fascia ending at the reflection of the vesical peritoneum, the bellowing adipose tissue connects between the side of the vesica and the pararectal space. The above findings are consistent with previous reports as well.2
Moreover, the space of Retzius is typically characterized by fat, loose fibrous tissue, and a perivesical venous plexus. Although abscess formation in this space is relatively rare,3-5 cases has been reported with various etiology, such as adjacent contacts or indirect spreading from nearby organs, including bladder infections, septic arthritis or osteomyelitis of the pubic symphysis, perianal abscesses, and Fournier’s gangrene. The bacterial etiology of the abscess often depends on the original inciting infection. For instance, perianal abscess extending to the prevesical space would be more likely to be secondary to polymicrobial including gram-negative anaerobes.
In our patient’s case, the original perirectal abscess likely extended cephalad through the supralevator space, progressed into the iliac space, and then advanced laterally to medially into the prevesical space.
Therapeutic strategies vary, with percutaneous drainage being the preferred method. Meanwhile, open surgical treatment and debridement may be necessary and inevitable, especially in cases of widespread abscesses and patients in septic state. Reported optimal treatments include extraperitoneal drainage with a lower midline abdominal incision6 and additional fistulectomy and diverting loop sigmoidostomy.7 And the wound could be closed primarily with drains or vacuum-assisted devices.8 Notably, in massive abscess with extraperitoneal extension, access to the peritoneal cavity or transperitoneal manipulation must be avoided due to high risk of contamination and secondary peritonitis. On the contrary, if the abscess is unilocular, relatively free of heterogenous particulate matter, and safely approachable, percutaneous drainage of the abscess seemed to be a favorable maneuver. Surgical debridement can always be instituted later if sepsis was not controlled prominently.
Moreover, upon abscess detection, blood cultures should be drawn, and broad-spectrum antibiotics, such as vancomycin and Piperacillin/tazobactam or a combination of vancomycin, cefepime, and metronidazole should be administrated early. The antibiotic regimen should cover methicillin-resistant Staphylococcus aureus and gram-negative anaerobes, considering possible hematogenous seeding and contiguous spread of infection. Prolonged course may be required if accompanying osteomyelitis is present.
Deep spreading perianal abscesses, particularly those with extraperitoneal invasion, puzzle physicians with diagnostic challenges due to their rarity and indolent clinical manifestations. Abdominal pain is indicative of an extraperitoneal spreading abscess as much portion of patients (86%) having that presentation.9 Associated medical illnesses, such as diabetes mellitus, alcoholism, end-stage renal disease, and immunocompromise, could predispose to higher complication rates, with pneumonia and respiratory failure being common.10 That is, a baseline frail status coupled with extensive infection may accelerate disease progression and severity. Furthermore, the number of days for fever to subside after drainage procedure is a significant prognostic indicator, related to mortality rate.10 In patients with preoperative fever, temperature fell below 100 °F in less than 3 days had an 89% mortality rate, compared to 71% in those remained febrile (p < 0.05).10 Meanwhile, the overall mortality rate for extraperitoneal abscesses ranges from 22% to 46%. If absent of rapid clinical improvement after initial drainage, the clinician must remain vigilant for signs of complicated condition. With increasing surgical manipulation in complex extraperitoneal abscesses, surgeons must be familiar with their potential interconnections, considering both source and intervention. With earlier diagnosis, more instant surgical drainage facilitated by CT imaging should decrease related morbidity and mortality risks.
4. Conclusions
This is a unique case of septic patient diagnosed of perirectal abscess with upward extension to the extraperitoneal space. Early consideration and identification of extraperitoneal abscesses are pivotal for timely intervention. More accurate and efficient diagnosis and treatment could reduce derived complications, reducing risks of morbidity and mortality.
Author Contributions
Hsiang Teng and Po-Hsien Wu conceived the study and conducted data collection. Hsiang Teng drafted the manuscript and all authors contributed substantially to the published vision of the manuscript. Po-Hsien Wu takes responsibility for the paper as a whole.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the Tri-Service General Hospital in Taiwan. (Protocol code C202415003 and date of approval: 2 January 2024).
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
All data are included in the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gittinger, J.W., Jr. Ocular involvement in Castleman’s disease. Response to radiotherapy. Ophthalmology. 1989, 96, 1646–1649. [Google Scholar] [CrossRef] [PubMed]
- Goel, R.; Raut, A.; Agarwal, A.; Raghav, S.; Kumar, S.; Chaudhary, S.; Golhait, P.; Kumar, S.; Saran, R. A rare presentation of orbital Castleman’s disease. Case Rep Ophthalmol Med. 2020, 2020, 1012759. [Google Scholar] [CrossRef] [PubMed]
- Dispenzieri, A.; Fajgenbaum, D.C. Overview of Castleman disease. Blood. 2020, 135, 1353–1364. [Google Scholar] [CrossRef] [PubMed]
- Stone, J.H.; Zen, Y.; Deshpande, V. IgG4-related disease. N Engl J Med. 2012, 366, 539–551. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, S.; Goyal, S.; Yadav, A.K.; Goyal, A. Multi-organ IgG4-related disease: demystifying the diagnostic enigma. J Postgrad Med. 2018, 64, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Martín-Nares, E.; Hernández-Molina, G.; Baenas, D.F.; Paira, S. IgG4-related disease: mimickers and diagnostic pitfalls. J Clin Rheumatol. 2022, 28, e596–e604. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, T.; Akiyama, M.; Kaneko, Y.; Takeuchi, T. Immunoglobulin G4-related disease and idiopathic multicentric Castleman’s disease: confusable immune-mediated disorders. Rheumatol (Oxf Engl). 2022, 61, 490–501. [Google Scholar] [CrossRef] [PubMed]
- Koppens, J.M.; Pon, J.A.; Allen, J.; Sloan, B.H. Castleman’s disease of the lacrimal gland. Clin Exp Ophthalmol. 2004, 32, 108–110. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Tang, D.; Sun, F. Clinical analysis of Castleman’s disease of the lacrimal gland. J Ophthalmol. 2020, 2020, 3718305. [Google Scholar] [CrossRef] [PubMed]
- Khosroshahi, A.; Wallace, Z.S.; Crowe, J.L.; Akamizu, T.; Azumi, A.; Carruthers, M.N.; Chari, S.T.; Della-Torre, E.; Frulloni, L.; Goto, H.; et al. International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol. 2015, 67, 1688–1699. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.K.; Kao, S.C.; Yang, C.F.; Lee, F.L.; Tsai, C.C. Ocular adnexal IgG4-related disease: clinical features, outcome, and factors associated with response to systemic steroids. Jpn J Ophthalmol. 2015, 59, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Otani, K.; Inoue, D.; Fujikura, K.; Komori, T.; Abe-Suzuki, S.; Tajiri, T.; Itoh, T.; Zen, Y. Idiopathic multicentric Castleman’s disease: a clinicopathologic study in comparison with IgG4-related disease. Oncotarget. 2018, 9, 6691–6706. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Wang, H.W.; Pittaluga, S.; Jaffe, E.S. Multicentric Castleman disease and the evolution of the concept. Pathologica. 2021, 113, 339–353. [Google Scholar] [CrossRef] [PubMed]
- González García, A.; Fernández-Martín, J.; Robles Marhuenda, Á. Idiopathic multicentric Castleman disease and associated autoimmune and autoinflammatory conditions: practical guidance for diagnosis. Rheumatol (Oxf Engl). 2023, 62, 1426–1435. [Google Scholar] [CrossRef] [PubMed]
- Mochizuki, H.; Kato, M.; Higuchi, T.; Koyamada, R.; Arai, S.; Okada, S.; Eto, H. Overlap of IgG4-related disease and multicentric Castleman’s disease in a patient with skin lesions. Intern Med. 2017, 56, 1095–1099. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).