1. Introduction
Over the last years, functional loading of implants immediately after their placement has been used with high success rates in both arches [
1]. This procedure reduces the number of surgical interventions, thus reducing the treatment time between surgical and prosthetic phases. Immediate loading was defined as the placement of an interim implant-supported structure up to 48 hours after implant insertion, and is often used in full-arch implant-supported rehabilitations, with great long-term results [
2,
3,
4]. There are several clinical and in vitro studies on full-arch immediate load treatments that have concluded that the placement of four implants , either two anterior parallel implants and two distally tilted, or four parallel implants, have similar stress distribution on the surrounding bone of the distal implants, leaving the choice of one or other depending on the preference of the operator and anatomical situation [
5,
6,
7,
8]. Recently, computed guided protocols for studying and planning the placement of these implants in the better possible position represents a viable therapeutic choice for implant-supported rehabilitations of edentulous dental arches specially [
9,
10,
11].
The conventional implant placement protocol includes incisions, complete detachment of the mucosa and periosteum, followed by exposure of the bone tissue for implant placement in a 1- or 2-stage approach and require longer surgical time, resulting in more uncomfortable postoperative healing as a consequence of pain, edema, and hematoma. Computer-guided flapless implant surgery, in contrast, provides a postoperative period with less trauma, systemic inflammation, bleeding, edema, and hematoma because of the shorter surgical time, leading to precision closer to that of the initial planning[
11,
12,
13,
14,
15]. Although flapless computer-guided surgery with virtual planning and the use of a prototype guide had some minimum angular and linear deviations, it has been considered acceptably safe and accurate[
16,
17,
18,
19]. But in order to be able to perform immediate load on these implants, some authors claim that installation torque values over 32Ncm are mandatory to provide sufficient primary stability for that purpose. Macrogeometry and microgeometry are directly related to primary stability, and after the healing period, the maintenance of the osseointegration of the implants [
20,
21,
22].
The transition from primary stability to secondary stability is characterized by bone remodeling around the implant during the healing process. Likewise, the characteristics of the implant surface influence this osseointegration process [
23]. The treatment of the surface of dental implants, that is, microgeometry, directly influences the retention of blood clots and migration of bone cells to stimulate the osseointegration process and, therefore, obtain greater bone/implant contact, especially in regions with low density bone [
24,
25,
26,
27]. The surface of implants with titanium powder direct laser-sintered has also been studied in humans [
28,
29]. The results of these studies suggest that osteoblasts are activated by direct contact with the sintered surface of the implant, leading to contact osteogenesis. The percentage of bone-implant contact in these previous studies was higher than that found in implants with a smooth surface, but still lower than that found in studies of implants with surfaces blasted by titanium oxide and washed with acids [
26,
30]. Recently, new technologies and advances in the additive manufacturing implants showed a great improvement in osseointegration and protein adsorption. Clinical studies on humans have also been carried out showing that implants produced entirely by additive manufacturing using the same process described previously, only carried out layer by layer, sintering titanium powder, also showed success rates compatible with conventional technologies of manufacturing dental implants for single cases [
31,
32].
Thus, we aim to report a clinical case of an immediate load full-arch screw retained over 4 implants produced by 3D printing manufacturing technology and installed by computed-guided surgery, with 24 months follow-up.
2. Case Report
A patient, EMZ, 72-year-old woman, with complete dentures on the upper and lower arches, came to our private practice complaining that she started to have discomfort when chewing, in the mental foramen region, on the left side. The alveolar mucosa seemed healthy (
Figure 1). The patient had just replaced her old pair of dentures, and these new ones were aesthetically and functionally satisfactory, with correct vertical dimensions, occlusion and good retention. Therefore, she was looking for some kind of fixed rehabilitation, that wouldn’t compress the nerves emergence and give her comfort on clenching. Along anamnesis she told us she had been using a prescribed anticoagulant because of a genetic heart condition. On clinical examination, it was possible to feel the alveolar nerve on the crest of the mandible. The patient was asked to get a computed tomography scan with the dentures in position, with 6 radiopaque points that we made (
Figure 2) on the lower denture, so we could digitally plan the best position for the possible implant for a fixed rehabilitation, and produce a computed guide accordingly to this project, in order to avoid incisions and so reduce the risk for excessive bleeding during surgery, due to her systemic condition. The images were sent to the Plenum planning center (Plenum
® Bioengenharia- Jundiaí, Brazil), where the project of the implants position and manufactory of the surgical guide would be 3D printed, after approval. Four implants were planned, two anterior in an axial position, and two distal slightly tilted, from a safe distance to the mentual foramen. Three fixation pins were planned also, to eliminate micromovements of the guide during the use and diminish possibility of errors (
Figure 3,
Figure 4 and
Figure 5). The patient approved our treatment plan for a flapless surgery. The computed surgical guide was tested for its adaptation before the surgery day (
Figure 6).
Pre-operatory medication consisted only on 2g of Amoxicillin one hour before the procedure, as suggested by her cardiologist. On surgery day, after anesthesia with Articaine 4% 1: 100,000 (DFL, Rio de Janeiro, Brazil), the computed surgical guide was placed in position, assured by the oclusal position on both sides and the stability over the patient’s mucosa, and in this position, fixed with the fixation pins after using their drills, assuring the guide immobilization (
Figure 7). After that, we followed the guided bone instrumentation protocol recommended by the Plenum implant system (Plenum
® Bioengenharia- Jundiaí, Brazil) to place 4 dental implants of 4.0x10mm with morse-tapper connection, produced by addtive manufacturing technology using titanium powder grade 23 (
Figure 8), without raising a flap (
Figure 9 and
Figure 10). Because of this detail, very little bleeding was noted during the surgery. All implants were inserted with insertion torque ranging from 45 to 60 N/cm, assuring us the possibility for immediate load. The guide was removed (
Figure 11) and four mini-conic abutments (Plenum
® Bioengenharia- Jundiaí, Brazil), with 2mm high were installed on the implants. No suture was necessary and minimum trauma was noted on the soft tissue (
Figure 12). Over these abutments, titanium cylinders were installed (
Figure 13) and the lower denture was prepared to capture the implants position, translating the removable prosthesis into a fixed one (
Figure 14 and
Figure 15). Pattern Resin was used to unite the denture to the cylinders, and over the red resin, pink acrylic resin was used to improve the aesthetic appearance of the prosthesis. The denture was worn out in order not to touch the patient’s mucosa, and to diminish the cantilever we removed the molars from both sides of the denture (
Figure 16) and installed the temporary fixed screw retained full-arch rehabilitation (
Figure 17 and
Figure 18). With this, the patient left the surgical appointment with an immediate load implant rehabilitation. Post operatory medication consisted on 600mg of Ibuprofen, twice a day during 3 days, if necessary. She was instructed to put ice bags on the surgical area during 48 hours, about 15 minutes every hour. On the day before surgery the patient suspended the medication because she had no pain. The patient was also instructed not to sleep with the opposing complete denture for 7 days and feed only with soft foods.
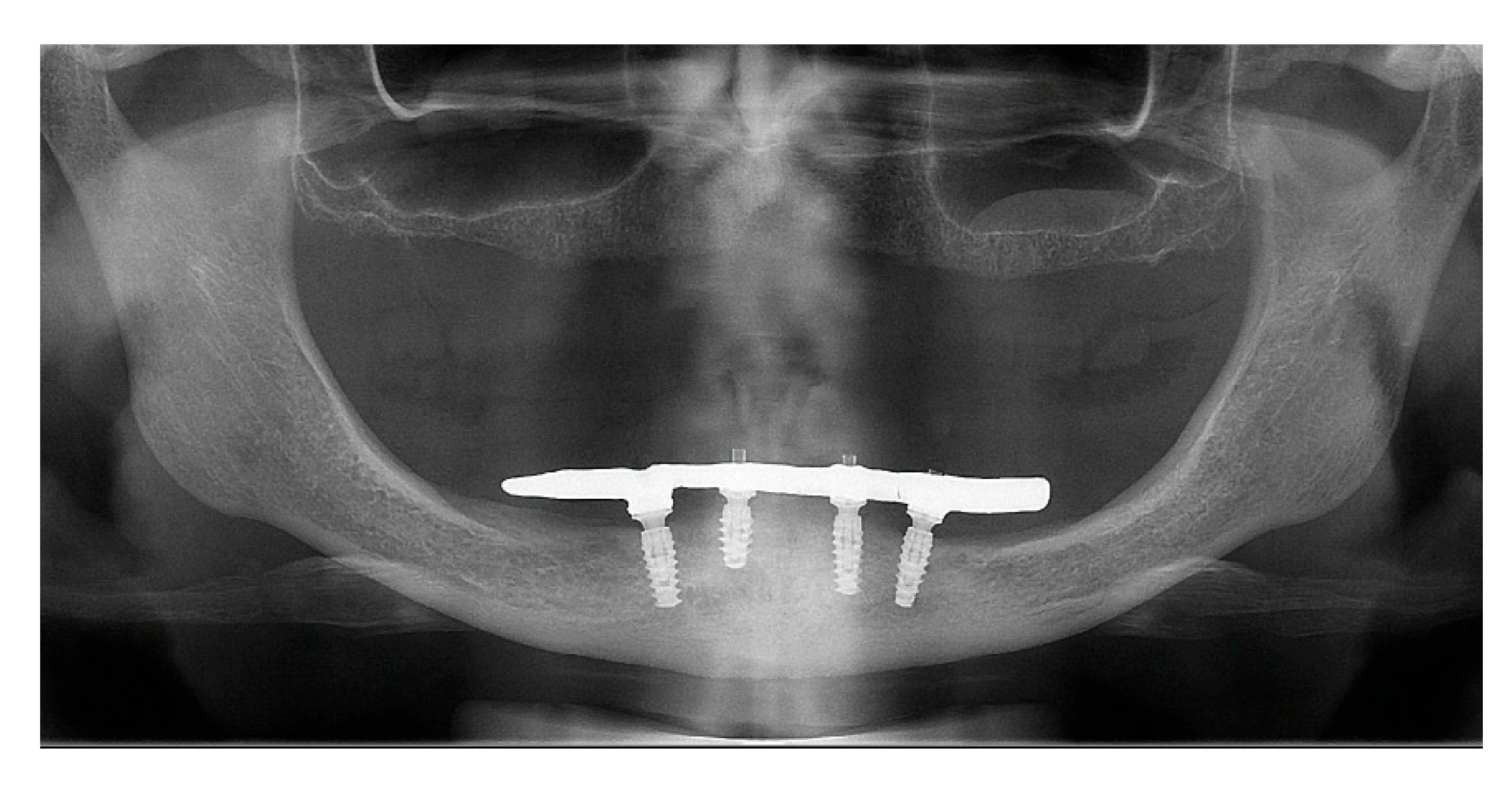
After a healing period of 3 months the patient returned to change que temporary fixed prothesis for a new one, more delicate and with a reinforced metallic bar for a better ferulization of the implants and better dissipation of the stress during function. After removal of the temporary prosthesis we could see the peri-implant mucosa was healthy (
Figure 19), without bleeding on probe nor peri-implant sulcus with more than 3mm depth, even around the implants were there were lack of a satisfactory keratinized tissue band, showing us that the patient was being able to maintain the cleansing of the region below the prosthesis. A new fixed rehabilitation over the implants was produced (
Figure 20,
Figure 21 and
Figure 22). 2 years after the surgery we could see on a control panoramic radiograph no signs of bone remodeling above the expected around the implants (
Figure 23).
3. Discussion
Full-arch fixed rehabilitation over 4 implants is not a new alternative to treat edentulous patients, and became very famous due to the “All-n-four concept”[
33,
34], with several studies showing excelent long term results[
3,
4,
5,
35]. In this case case we also choose with the patient’s consent to use only four implants for her lower jaw rehabilitation. Even that we didn’t tilted the disatl implants as much as the “All-on-four concept” precognize, at the 24 months follow-up it seems to be successful so far, corroborating with some studies that also claim that parallel implants may be as effective as tilted ones [
6,
7,
8] . The age of the patient also seemed not to interfere on the result, but because of her systemic condition[
36,
37,
38] we preferred to perform a flapless computed guided surgery, promoting more comfort during and after the procedure [
13,
14,
15,
16]. This modality of computed guided surgery with flapless approach has been proved to show good results for the ful-arch rehabilitation over implants [
15,
19,
39,
40] and encouraged us to use it in our clinical case.
The advances in digital dentistry and implantology are not exclusive for planning implant positions, producing computed surgical guides, or preparing prosthetic rehabilitation even before the surgery, with reliable accuracy [
41,
42,
43,
44,
45]. In this clinical report, we placed titanium dental implants produced by 3D printing or additive manufacturing technology. As we know at this moment, this is the only commercially available implant system that uses this kind of technology in the manufacturation of their implants. Direct laser sintering may improve the mechanical properties, accuracy, and material versatility in dental applications by the construction of the component or implant layer by layer, as in 3D printing [
46,
47]. The greater control in the production of micro and nano geometry in this process appears to balance the difference between the elastic moduli of the bone tissue and the titanium implant, thus reducing the stress on functional load and providing greater long-term tissue stability [
31,
32]. In fact, there are some studies published about implants produced by direct laser forming, showing excellent results on survival rates and osseointegration levels [
31,
32,
48,
49,
50]. Some studies have been published on this technology when used for implant surface treatment as well, with good results [
25,
26,
29,
48].
A recent systematic review of clinical trials compared the bone-to-implant interface of different implant surface treatments, aiming to asses histological healing outcomes of loaded and unloaded implants, on bone-to-implant contact, bone density in and outside the threaded area, and osteocyte index [
51]. They concluded that rough surfaces and load implants resulted in higher values of every parameter studied. Another recent review that aimed to analyze different implant surfaces and try to identify the ideal structure from a clinical and durability point of view [
52] concluded that treated surfaces allowed better osseointegration and better cell proliferation, as long as a better propensity for epithelial cell adhesion and attachment, proliferation, and differentiation of osteoblastic cells. They also suggest that 3D printed implants deserve further investigation to help improve biocompatibility. In the same direction, an in vitro study evaluated the interaction between 5 different implant surfaces and fibrinogen, because of it is the first step for the formation of the fibrin network [
53]. Among the specimens was the implant used in this clincal case report. They showed that Plenum
® surface had the best performance on coverage by the liquid fibrinogen, with a thick and dense fibrin layer with more cells trapped inside. According to the authors, the topography characteristics of this implant, such as the mimic of the microstructure of a trabecular bone, may stimulate cell adhesion and new bone formation because of the thicker fibrin fibers inserted and interconnected between its microroughness, shown in the study [
53]. Another in vitro study evaluated the impact of two different methods for titanium disc production, conventional and by direct laser metal sintering, and their influence on microbial profile using a subgingival multispecies biofilm in vitro model. The results showed that the direct laser metal sintering modified the in vitro biofilm profile, reducing the proportion of red complex and decreasing total counts of
Porphyromonas gingivalis which might be related to peri-implant disease. Finally, an animal study compared the sequential osseointegration between implants produced by 3D printing technology with conventional titanium implants after 2 and 6 weeks [
55]. Because of the 3D network of the trabecular structure of the 3D printed implants, the total surface available for the osseointegration process was higher than that of conventional implants, as shown statistically by higher bone-to-implant contact. So, the direct bone formation on the 3D-printed implant surface is by far adequate for functional stability. The authors concluded that implants manufactured by 3D printing had successfully osseointegrated, with adequate fractions of mineralized bone formation after 2 and 6 weeks. Also, it appears that the crystal bone height was maintained in an optimal way compared to the conventional implant systems [
55].
4. Conclusions
Within the limitations of this single case report, the fixed full-arch rehabilitation over 4 implants produced by 3D printing manufacturing and placed with a computed surgical guide seems to be effective, without any biological or mechanical complications, at the 24 months follow-up. Although this is a new implant system, studies on the field encourage clinicians to run clinical trials to evidence medium- and long-term results with these implants, ensuring that the good in vitro results may be translated to in vivo studies.
Author Contributions
Conceptualization, M.C.F.; J.A.S; methodology, M.C.F.; validation, M.C.F.; and R.F.; formal analysis, M.C.F.; investigation, M.C.F.; resources, M.C.F.; data curation, M.C.F.; writing—original draft preparation, M.C.F. J.A.S; writing—review and editing, M.C.F. J.A.S; visualization, M.C.F.; R.F.; supervision, M.C.F; project administration, M.C.F; funding acquisition, M.C.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
Jamil Shibli is founder and shareholder of Plenum Bioengenharia, Jundiai, SP, Brazil. The other authors declare no conflicts of interest.
References
- Del Fabbro, M.; Testori, T.; Kekovic, V.; Goker, F.; Tumedei, M.; Wang, H.L. A Systematic Review of Survival Rates of Osseointegrated Implants in Fully and Partially Edentulous Patients Following Immediate Loading. J Clin Med 2019, 8, 2142. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, G.S.Y.; de Magalhães, K.M.F.; Rocha, E.P.; Dos Santos, P.H.; Assunção, W.G. Oral health-related quality of life and satisfaction in edentulous patients rehabilitated with implant-supported full dentures all-on-four concept: a systematic review. Clin Oral Invest 2022, 26, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Agliardi, E.; Panigatti, S.; Clerico, M.; Villa, C.; Malo, P. Immediate rehabilitation of the edentulous jaws with full fixed prostheses supported by four implants: Interim results of a single cohort prospective study. Clin Oral Implant Res 2010, 21, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Agliardi, E.L.; Pozzi, A.; Romeo, D.; Del Fabbro, M. Clinical outcomes of full-arch immediate fixed prostheses supported by two axial and two tilted implants: A retrospective cohort study with 12-15 years of follow-up. Clin Oral Implants Res 2023, 34, 351–366. [Google Scholar] [CrossRef] [PubMed]
- Malò, P.; De Arauijo Norbre, M.; Lopes, A.; Ferro, A.; Botto, J. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: A longitudinal study with 10 to 18 years of follow-up. Clin Implant Dent Relat Res 2019, 21, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Baggi, L.; Pastore, S.; di Girolamo, M.; Vairo, G. Implantbone load transfer mechanisms in complete-arch prostheses supported by four implants: a three-dimensional finite element approach. J Prosthetc Dent 2013, 109, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Shimamura, I.; Sakurai, K. Influence of number and inclination angle of implants on stress distribution in mandibular cortical bone with All-on-4 concept. J Prost Res 2010, 54, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Agnini, A.; Agnini, A.M.; Romeo, D.; Chiesi, M.; Pariente, L.; Stappert, C.F.J. Clinical investigation on axial versus tilted implants for immediate fixed rehabilitation of edentulous arches: preliminary results of a single cohort study. Clinical Implant Dentistry and Related Research 2014, 16, 527–539. [Google Scholar] [CrossRef] [PubMed]
- Manacorda, M.; Poletti de Chaurand, B.; Merlone, A.; Tetè, G.; Mottola, F.; Vinci, R. Virtual Implant Rehabilitation of the Severely Atrophic Maxilla: A Radiographic Study. Dent J 2020, 8, 14. [Google Scholar] [CrossRef]
- Cattoni, F.; Chirico, L.; Merlone, A.; Manacorda, M.; Vinci, R.; Gherlone, E.F. Digital Smile Designed Computer-Aided Surgery versus Traditional Workflow in “All on Four” Rehabilitations: A Randomized Clinical Trial with 4-Years Follow Up. Int J Environ Res Public Health 2021, 18, 3449. [Google Scholar] [CrossRef]
- Vercruyssen, M.; Hultin, M.; Van Assche, N.; Svensson, K.; Naert, I.; Quirynen, M. Guided surgery: accuracy and efficacy. Periodontol 2000 2014, 66, 228–46. [Google Scholar] [CrossRef] [PubMed]
- Di Giacomo, G.A.; Cury, P.R.; de Araujo, N.S.; Sendyk, W.R.; Sendyk, C.L. Clinical application of stereolithographic surgical guides for implant placement: preliminary results. J Periodontol 2005, 76, 503–7. [Google Scholar] [CrossRef] [PubMed]
- Fortin, T.; Bosson, J.L.; Isidori, M.; Blanchet, E. Effect of flapless surgery on pain experienced in implant placement using an image-guided system. Int J Oral Maxillofac Implants 2006, 21, 298–304. [Google Scholar] [PubMed]
- D'haese, J.; Ackhurst, J.; Wismeijer, D.; De Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontol 2000 2017, 73, 121–133. [Google Scholar] [CrossRef]
- Naeini, E.N.; Atashkadeh, M.; De Bruyn, H.; D'Haese, J. Narrative review regarding the applicability, accuracy, and clinical outcome of flapless implant surgery with or without computer guidance. Clin Implant Dent Relat Res 2020, 22, 454–467. [Google Scholar] [CrossRef] [PubMed]
- Cunha, R.M.; Souza, F.A.; Hadad, H.; Poli, P.P.; Maiorana, C.; Carvalho, P.S.P. Accuracy evaluation of computer-guided implant surgery associated with prototyped surgical guides. J Prosthet Dent 2021, 125, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, A.; Komiyama, A.; Hultin, M.; Näsström, K.; Klinge, B. Accuracy of virtually planned and template guided implant surgery on edentate patients. Clin Implant Dent Relat Res 2012, 14, 527–37. [Google Scholar] [CrossRef]
- Arisan, V.; Karabuda, Z.C.; Ozdemir, T. Accuracy of two stereolithographic guide systems for computer-aided implant placement: a computed tomography-based clinical comparative study. J Periodontol 2010, 81, 43–51. [Google Scholar] [CrossRef] [PubMed]
- La Monaca, G.; Pranno, N.; Annibali, S.; Di Carlo, S.; Pompa, G.; Cristalli, M.P. Immediate flapless full-arch rehabilitation of edentulous jaws on 4 or 6 implants according to the prosthetic-driven planning and guided implant surgery: A retrospective study on clinical and radiographic outcomes up to 10 years of follow-up. Clin Implant Dent Relat Res 2022, 24, 831–844. [Google Scholar] [CrossRef]
- Tumedei, M.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. A Narrative Review of the Histological and Histomorphometrical Evaluation of the Peri-Implant Bone in Loaded and Unloaded Dental Implants. A 30-Year Experience (1988–2018). Int J Environ Res Public Health 2020, 17, 2088. [Google Scholar] [CrossRef]
- Sotto-Maior, B.S.; Rocha, E.P.; Almeida, E.O.; Freitas-Júnior, A.C.; Anchieta, R.B.; Del Bel Cury, A.A. Influence of high insertion torque on implant placement – an anisotropic bone stress analysis. Braz Dent J 2010, 21, 21,508–514. [Google Scholar] [CrossRef]
- Dos Santos, M.V.; Elias, C.N.; Lima, J.H.C. The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res 2011, 13, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Lahens, B.; Neiva, R.; Tovar, N.; Alifarag, A.M.; Jimbo, R.; Bonfante, E.A.; Bowers, M.M.; Cuppini, M.; Freitas, H.; Witek, L.; Coelho, P.G. Biomechanical and histologic basis of Osseodensification drilling for endosteal implant placement in low density bone. An experimental study in sheep. J Mech Behav Biomed Mater 2016, 63, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Coelho, P.G.; Granjeiro, J.M.; Romanos, G.E.; Suzuki, M.; Silva, N.R.; Cardaropoli, G.; Thompson, V.P.; Lemons, J.E. Basic research methods and current trends of dental implant surfaces. J Biomed Mater Res B Appl Biomater 2009, 88, 579–96. [Google Scholar] [CrossRef] [PubMed]
- Mangano, C.; Raspanti, M.; Traini, T.; Piattelli, A.; Sammons, R. Stereo imaging and cytocompatibility of a model dental implant surface formed by direct laser fabrication. J Biomed Mater Res A 2009, 88, 823–31. [Google Scholar] [CrossRef] [PubMed]
- Grassi, S.; Piattelli, A.; de Figueiredo, L.C.; Feres, M.; de Melo, L.; Iezzi, G.; Alba, R.C. Jr.; Shibli, J.A. Histologic evaluation of early human response to different implant surfaces. J Periodontol 2006, 77, 1736–1743. [Google Scholar] [CrossRef] [PubMed]
- Shibli, J.A.; Grassi, S.; de Figueiredo, L.C.; Feres, M.; Iezzi, G.; Piattelli, A. Human peri-implant bone response to turned and oxidized titanium implants inserted and retrieved after 2 months. Implant Dent 2007, 16, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Shibli, J.A.; Mangano, C.; D’avila, S.; Piattelli, A.; Pecora, G.E.; Mangano, F.; Onuma, T.; Cardoso, L.A.; Ferrari, D.S.; Aguiar, K.C.; Iezzi, G. Influence of direct laser fabrication implant topography on type IV bone: a histomorphometric study in humans. J Biomed Mater Res A 2010, 93, 607–614. [Google Scholar] [CrossRef]
- Mangano, C.; Piattelli, A.; Raspanti, M.; Mangano, F.; Cassoni, A.; Iezzi, G.; Shibli, J.A. Scanning eléctron microscopy (SEM) and X-ray dispersive spectrometry evaluation of direct laser metal sintering surface and human bone interface: a case series. Lasers Med Sci 2011, 26, 133–138. [Google Scholar] [CrossRef]
- Grassi, S.; Piattelli, A.; Ferrari, D.S.; Figueiredo, L.C.; Feres, M.; Iezzi, G.; Shibli, J.A. Histologic evaluation of human bone integration on machined and sandblasted acid-etched titanium surfaces in type IV bone. J Oral Implantol 2007, 33, 8–12. [Google Scholar] [CrossRef]
- Shibli, J.A.; Mangano, C.; Mangano, F.; Rodrigues, J.A.; Cassoni, A.; Bechara, K.; Ferreia, J.D.B.; Dottore, A.M.; Iezzi, G.; Piattelli, A. Bone-to-implant contact around immediately loaded direct laser metal-forming transitional implants in human posterior maxilla. J Periodontol 2013, 84, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Tunchel, S.; Blay, A.; Kolerman, R.; Mijirisky, E.; Shibli, J.A. 3D printing/additive manufacturing single titanium dental implants: a prospective multicenter study with 3 years of follow-up. Int J Dent 2016, 2016, 8590971. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Rangert, B.; Nobre, M. “All-on- four” immediate-function concept with Brånemark system implants for completely edentulous mandibles: A retrospective clinical study. Clinical Implant Dentistry and Related Research 2003, 5 (Suppl 1), 2–9. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Rangert, B.; Nobre, M. All-on- 4 immediate-function concept with Brånemark system implants for completely edentulous maxillae: A 1-year retrospective clinical study. Clinical Implant Dentistry and Related Research 2005, 7 (Suppl 1), S88–S94. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; de Araujo Nobre, M.; Lopes, A.; Ferro, A.; Nunes, M. The all-on- 4 concept for full-arch rehabilitation of the edentulous maxillae: A longitudinal study with 5-13 years of follow-up. Clinical Implant Dentistry and Related Research 2019, 21, 538–549. [Google Scholar] [CrossRef] [PubMed]
- Corbella, S.; Agliardi, E.; Basso, M.; Romeo, D.; Testori, T.; Francetti, L. Management of dental patients taking anticoagulant drugs. Dent Cadmos 2008, 76, 13–23. [Google Scholar]
- Tetè, G.; Polizzi, E.; D’orto, B.; Carinci, G.; Capparè, P. How to consider implant-prosthetic rehabilitation in elderly patients: A narrative review. J Biol Regul Homeost Agents 2021, 35 (Suppl. S1), 119–126. [Google Scholar] [PubMed]
- Kowar, J.; Eriksson, A.; Jemt, T. Fixed implant-supported prostheses in elderly patients: A 5-years retrospective comparison between partially and completely edentulous patients aged 80 years or older at iumplant surgery. Clin Implant Dent Relat Res 2013, 15, 37–46. [Google Scholar] [CrossRef]
- van Steenberghe, D.; Glauser, R.; Blombäck, U.; Andersson, M.; Schutyser, F.; Pettersson, A.; Wendelhag, I. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: a prospective multicenter study. Clin Implant Dent Relat Res 2005, 7, S111–S120. [Google Scholar] [CrossRef]
- Malo, P.; de Araujo, N.M.; Lopes, A. The use of computer-guided flapless implant surgery and four implants placed in immediate function to support a fixed denture: preliminary results after a mean follow-up period of thirteen months. J Prosthet Dent 2007, 97(6 Suppl), S26–S34. [Google Scholar] [CrossRef]
- Tallarico, M. Computerization and Digital Workflow in Medicine: Focus on Digital Dentistry. Materials 2020, 13, 2172 439. 440. [Google Scholar] [CrossRef]
- Todaro, C.; Cerri, M.; Isola, G.; Manazza, A.; Storelli, S.; Rodriguez y Baena, R.; Lupi, S.M. Computer-Guided Osteotomy with Simultaneous Implant Placement and Immediately Loaded Full-Arch Fixed Restoration: A Case Report. Prosthesis 2023, 5, 221–233. [Google Scholar] [CrossRef]
- Todaro, C.; Cerri, M.; Rodriguez, Y.; Baena, R.; Lupi, S.M. Full-Arch Guided Restoration and Bone Regeneration: A Complete Digital Workflow Case Report. Healthcare (Basel) 2023, 11, 1301. [Google Scholar] [CrossRef] [PubMed]
- Pesce, P.; Pera, F.; Setti, P.; Menini, M. Precision and Accuracy of a Digital Impression Scanner in Full-Arch 445 Implant Rehabilitation. Int J Prosthodont 2018, 31, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Park, J.M.; Kim, S.M.; Kim, M.J.; Lee, J.H.; Kim, M.J. An assessment of template-guided implant surgery in terms of accuracy and related factors. J Adv Prosthodont 2013, 5, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Huang, S. .; Wei, H., Ed.; Li, D. Additive manufacturing technologies in the oral implant clinic: A review of current 465 applications and progress. Front Bioeng Biotechnol 2023 11, 1100155. 466.
- Goguta, L.; Lungeanu, D.; Negru, R.; Birdeanu, M.; Jivanescu, A.; Sinescu, C.; Sinescu, C. Selective Laser Sintering versus Selective Laser Melting and Computer Aided Design - Computer 467 Aided Manufacturing in Double Crowns Retention. J Prosthodont Res 2021, 65, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Shibli, J.A.; Mangano, C.; Mangano, F.; Brasil, O.; Lins, B.; Cozzolino, F.; Tunchel, S.; Blay, A.; Iezzi, G.; Piattelli, A. Histomorphometric Evaluation of Direct Laser Metal Forming (DLMF) Implant Surface in the Type IV Bone: A Controlled Study in Human Jaw. POSEIDO 2013, 1, 45. [Google Scholar]
- Mangano, C.; Mangano, F.; Shibli, J.A.; Luongo, G.; De Franco, M.; Briguglio, F.; Figliuzzi, M.; Eccellente T, Rapani C, Piombino M. Macchi A. Prospective clinical evaluation of 201 direct laser metal forming implants: results from a 1-year multicenter study. Lasers Med Sci 2012, 27, 181-9. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Mangano, C.; Piattelli, A.; Iezzi, G. Histological Evidence of the Osseointegration of Fractured Direct Metal Laser Sintering Implants Retrieved after 5 Years of Function. Biomed Res Int 2017, 2017, 9732136. [Google Scholar] [CrossRef]
- Chambrone, L.; Rincón-Castro, M.V.; Poveda-Marín, A.E.; Diazgranados-Lozano, M.P.; Fajardo-Escolar, C.E.; Bocanegra-Puerta, M.C.; Palma, L.F. Histological healing outcomes at the bone-titanium interface of loaded and unloaded dental implants placed in humans: A systematic review of controlled clinical trials. Int J Oral Implantol (Berl) 2020, 13, 321–342. [Google Scholar] [PubMed]
- Inchingolo, A.M.; Malcangi, G.; Ferrante, L.; Del Vecchio, G.; Viapiano, F.; Inchingolo, A.D.; Mancini, A.; Annicchiarico, C.; Inchingolo, F.; Dipalma, G.; Minetti, E.; Palermo, A.; Patano, A. Surface Coatings of Dental Implants: A Review. J Funct Biomater 2023, 22, 287. [Google Scholar] [CrossRef] [PubMed]
- Andrade, C.X.; Quirynen, M.; Rosenberg, D.R.; Pinto, N.R. Interaction between Different Implant Surfaces and Liquid Fibrinogen: A Pilot In Vitro Experiment. Biomed Res Int 2021, 5, 2021:9996071. [Google Scholar] [CrossRef] [PubMed]
- Pingueiro, J.; Piattelli, A.; Paiva, J.; Figueiredo, L.C.; Feres, M.; Shibli, J.; Bueno-Silva, B. Additive manufacturing of titanium alloy could modify the pathogenic microbial profile: an in vitro study. Braz Oral Res 2019, 33(suppl 1), e065. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Imber, J.C.; Lang, K.N.; Schmid, B.; Muñoz, F.; Bosshardt, D.D.; Saulacic, N. Sequential osseointegration of a novel implant system based on 3D printing in comparison with conventional titanium implants. Clin Oral Implants Res 2023, 34, 627–638. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
Initial view of the patient’s lower mucosa.
Figure 1.
Initial view of the patient’s lower mucosa.
Figure 2.
Buccal view of the denture in position with radiopaque points inserted to guide the virtual planning after tomography.
Figure 2.
Buccal view of the denture in position with radiopaque points inserted to guide the virtual planning after tomography.
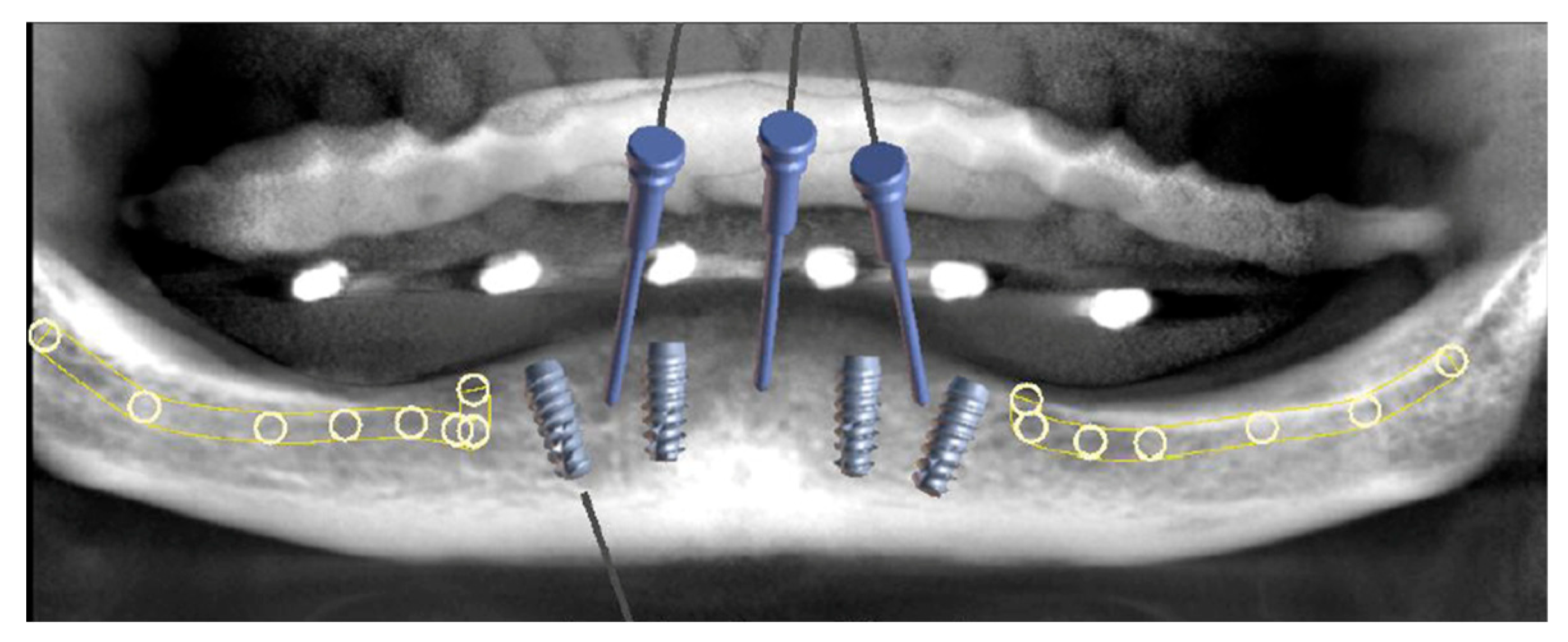
Figure 3.
Front view of the project, with the position of the four implants and the fixation pins.
Figure 3.
Front view of the project, with the position of the four implants and the fixation pins.
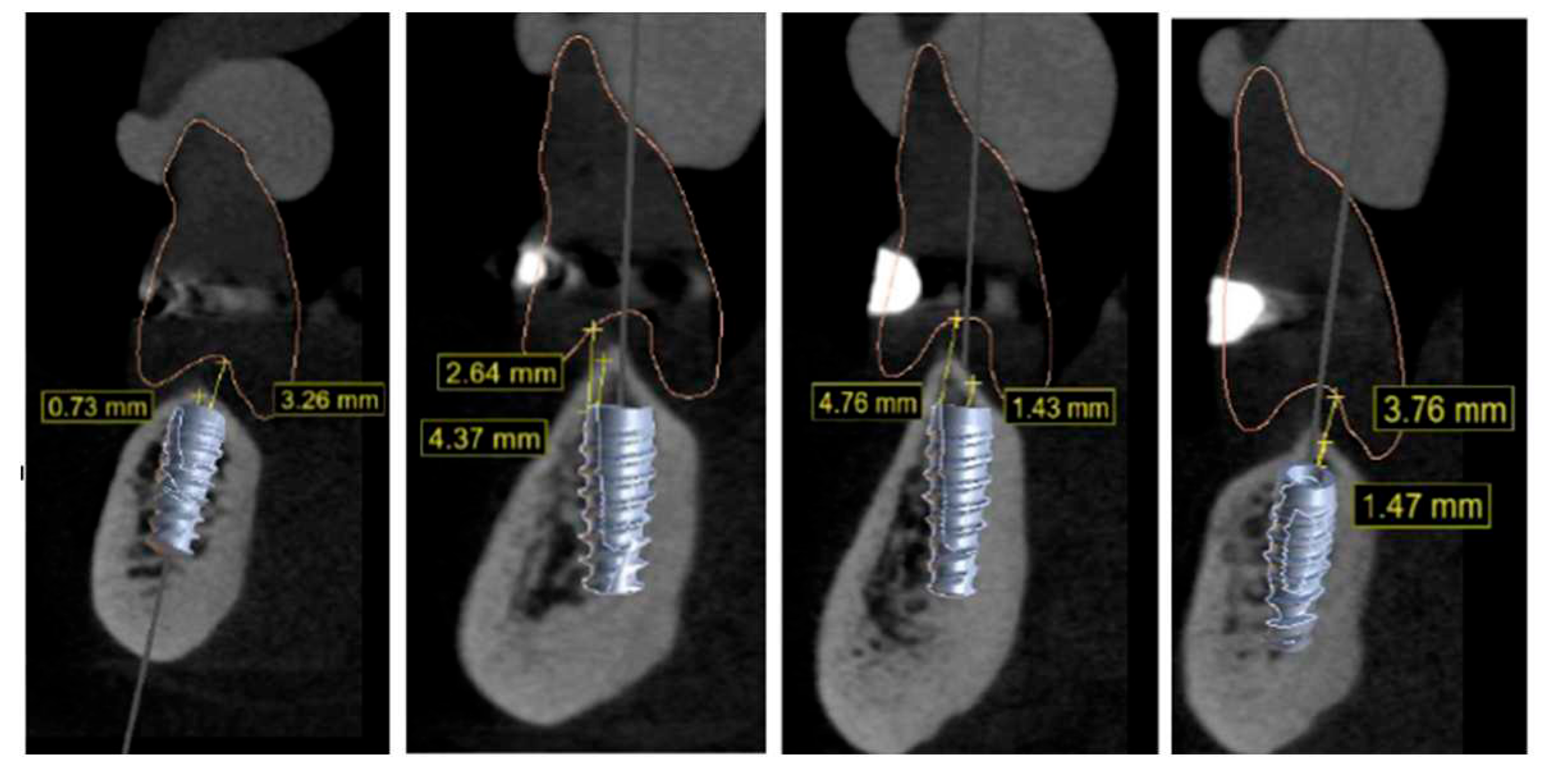
Figure 4.
Tomographic view of each implant position, accordingly to the prosthetic project.
Figure 4.
Tomographic view of each implant position, accordingly to the prosthetic project.
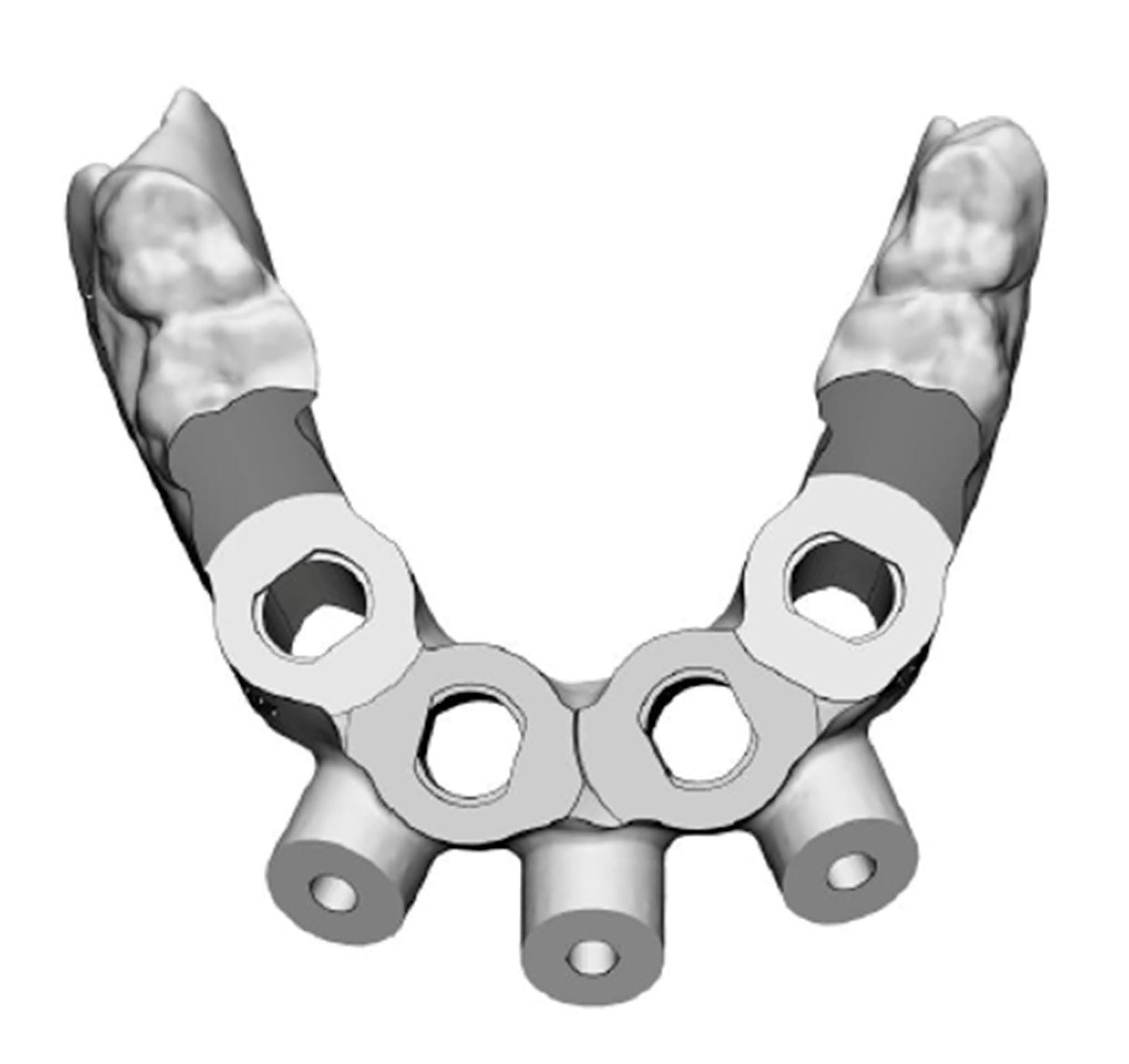
Figure 5.
Project of the computed surgical guide.
Figure 5.
Project of the computed surgical guide.
Figure 6.
Buccal view of the surgical guide test for adaptation and stability.
Figure 6.
Buccal view of the surgical guide test for adaptation and stability.
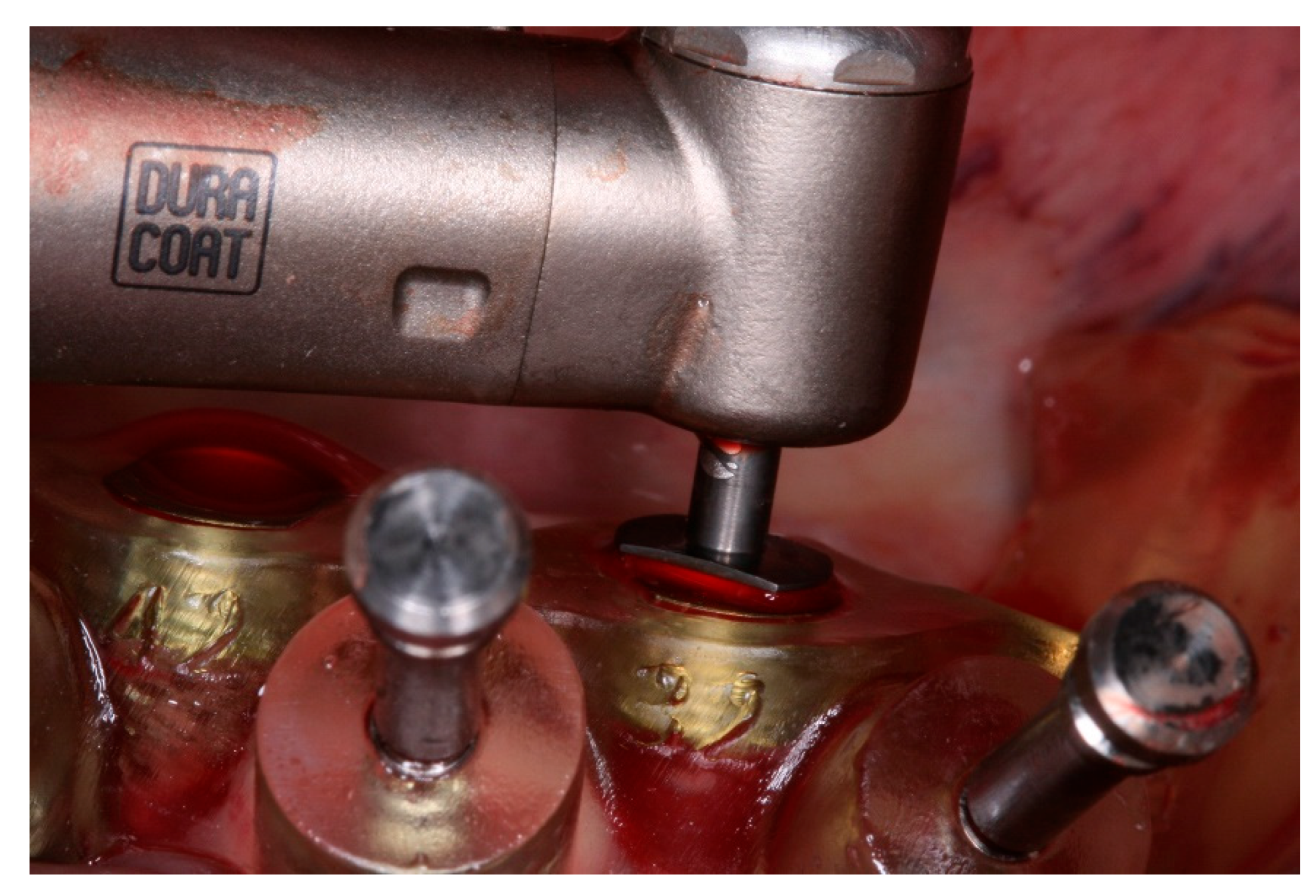
Figure 7.
Computed surgical guide fixed to the mandible with the fixation pins.
Figure 7.
Computed surgical guide fixed to the mandible with the fixation pins.
Figure 8.
Implant Plenum RE 4.0x10mm.
Figure 8.
Implant Plenum RE 4.0x10mm.
Figure 9.
Bone instrumentation through the surgical guide, as recommended by the manufacturer, with the bur with total length of the proposed implant.
Figure 9.
Bone instrumentation through the surgical guide, as recommended by the manufacturer, with the bur with total length of the proposed implant.
Figure 10.
Implant placement through the computed surgical guide.
Figure 10.
Implant placement through the computed surgical guide.
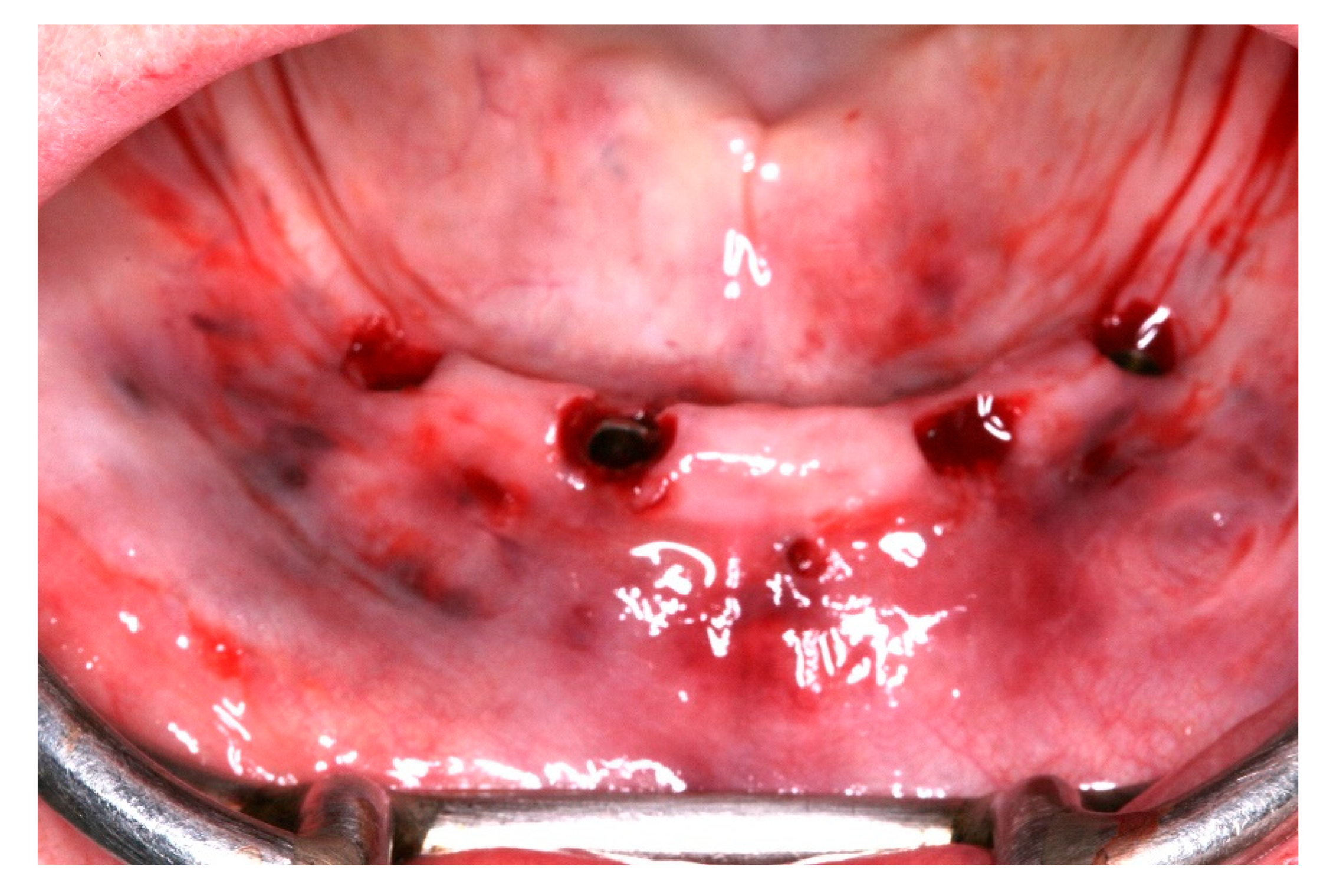
Figure 11.
View of the mucosa immediately after surgical guide removal and implants placement.
Figure 11.
View of the mucosa immediately after surgical guide removal and implants placement.
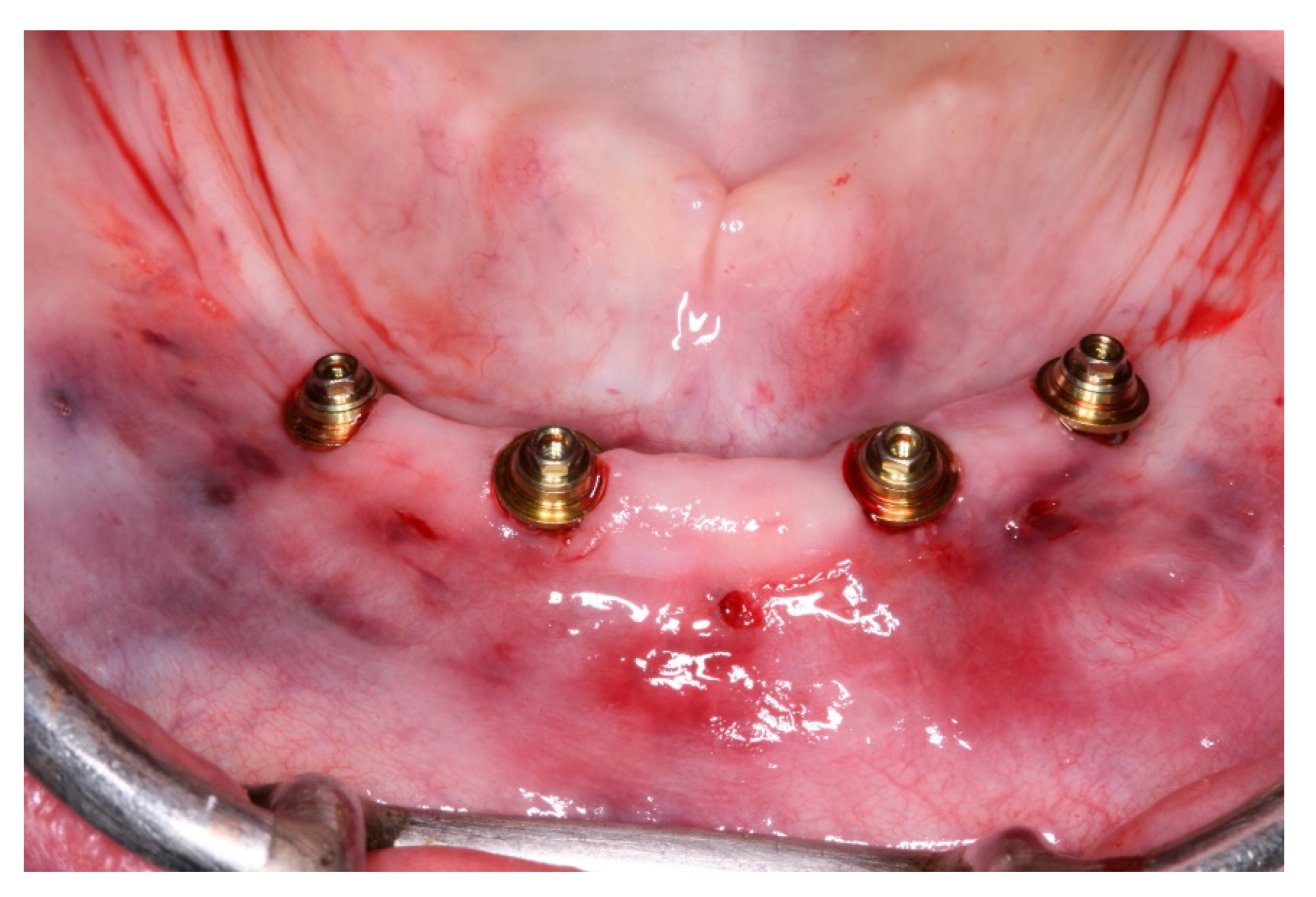
Figure 12.
View of the mini conic abutments installed.
Figure 12.
View of the mini conic abutments installed.
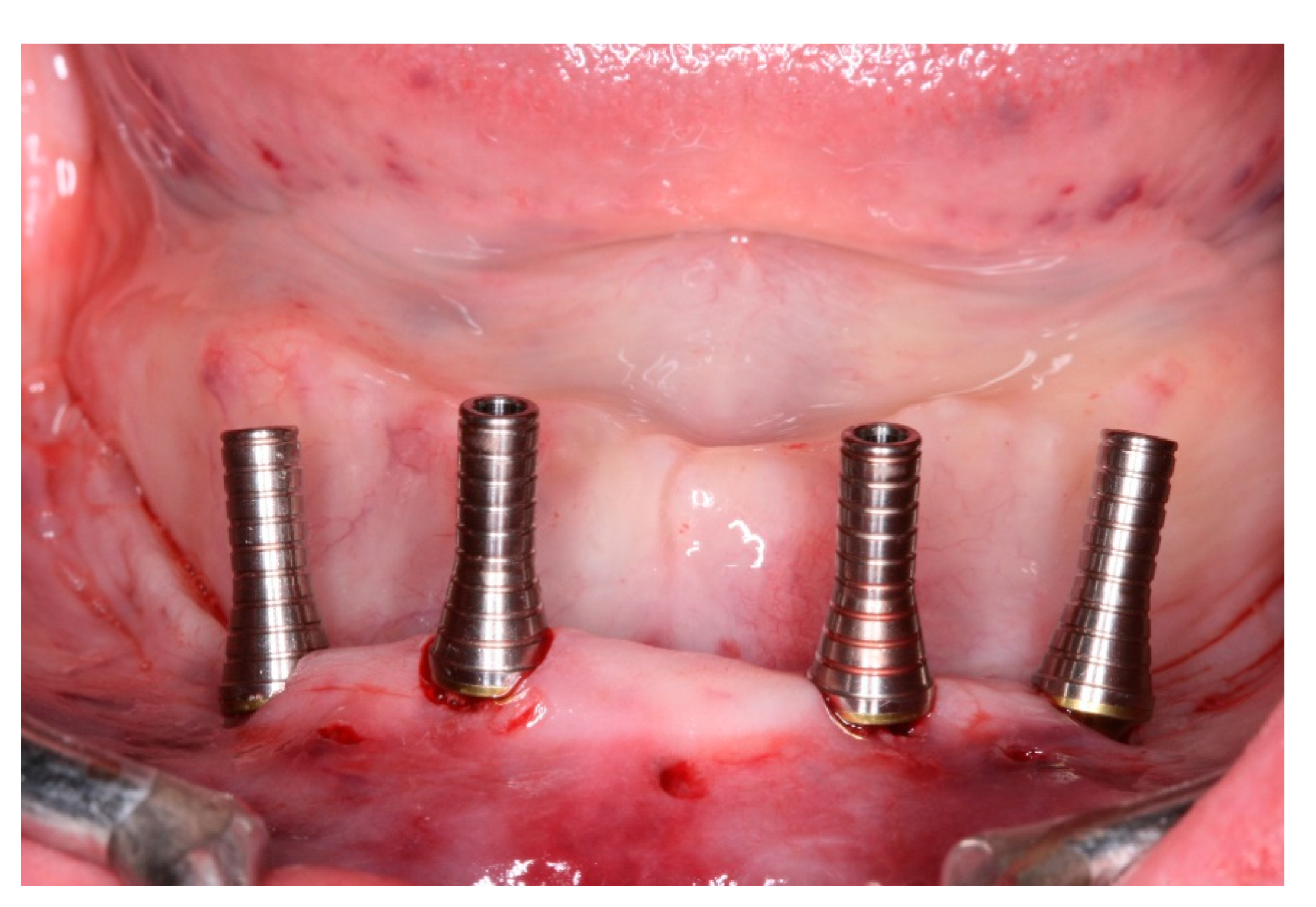
Figure 13.
View of the titanium cylinders screwed to the abutments.
Figure 13.
View of the titanium cylinders screwed to the abutments.
Figure 14.
Denture preparation for capturing the implant position.
Figure 14.
Denture preparation for capturing the implant position.
Figure 15.
Denture prepared and in position to capture the implants position through the opening windows.
Figure 15.
Denture prepared and in position to capture the implants position through the opening windows.
Figure 16.
Inferior denture translated into a fixed screw-retained temporary full-arch prosthesis after modifications.
Figure 16.
Inferior denture translated into a fixed screw-retained temporary full-arch prosthesis after modifications.
Figure 17.
View of the fixed screw-retained temporary full-arch prosthesis installed.
Figure 17.
View of the fixed screw-retained temporary full-arch prosthesis installed.
Figure 18.
Buccal view of the fixed screw-retained temporary full-arch prosthesis installed.
Figure 18.
Buccal view of the fixed screw-retained temporary full-arch prosthesis installed.
Figure 19.
View of the peri-implants mucosa after 3 months of healing.
Figure 19.
View of the peri-implants mucosa after 3 months of healing.
Figure 20.
Lingual view of the new fixed screw-retained full-arch rehabilitation.
Figure 20.
Lingual view of the new fixed screw-retained full-arch rehabilitation.
Figure 21.
Buccal view of the new fixed screw-retained full-arch rehabilitation in occlusion.
Figure 21.
Buccal view of the new fixed screw-retained full-arch rehabilitation in occlusion.
Figure 22.
Extra oral view of the patient with the new fixed screw-retained full-arch rehabilitation.
Figure 22.
Extra oral view of the patient with the new fixed screw-retained full-arch rehabilitation.
Figure 23.
Panoramic radiograph view with 24 months follow-up.
Figure 23.
Panoramic radiograph view with 24 months follow-up.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).