Submitted:
22 January 2024
Posted:
23 January 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Patient risk factors for Long Covid
Vaccination status/experience
Acute infection symptoms
Long-term symptoms
| Symptom | Time of onset | Duration | Plain language description |
|---|---|---|---|
| Cough | Day 2 of infection | 4 months | Month 1: wet and productive cough, month 2-4: unproductive, dry cough |
| Sore throat | Day 2 of infection | Ongoing | Dry, scratchy and painful throat, hurts to swallow |
| Pressure headache | Day 2 of infection | 5 months constant, then 2 days a week ongoing | It feels like a fork is being scraped over the front half of my brain while the back half of my brain is being squeezed in a vice |
| Extreme fatigue | Day 2 of infection | Ongoing | I slept for 16+ hours every day for the first 4 months post infection. If I try to fight or push through feeling tired, I will wind down like I'm running out of batteries and black out from exhaustion, no matter where I am or whether I am lying down. My current sleep baseline is 12 hours a day, with 3-4 days a month needing 16 hours of sleep a day. It feels like I am being drained and weakened, the longer I stay awake past my energy envelope. |
| Unrefreshing sleep | 3 weeks post infection | 22 months constant, then 3 days a week ongoing | No matter how much I sleep, or how well I sleep, I wake up feeling the same or worse as when I went to sleep |
| Joint pain | Day 2 of infection | Ongoing | Deep persistent ache within shoulder, elbow, wrist, and pelvic joints |
| Joint subluxations | 2 weeks post infection | Ongoing | My shoulders now pop out of place and back in if I lift my arm too quickly; it feels like a popping then crunching sensation at the shoulder joint, followed by increased muscle and joint pain in that joint. My ribs will slip out of place and I then have a stabbing sensation in my back every time I try to breathe or bend over, until the joint settles back into place |
| Muscle pain | Day 2 of infection | Ongoing | Burning and aching muscles, similar to the sensation following a hard workout, but present at all times |
| Sensory sensitivities | 3 weeks post infection | Ongoing | I have become extremely jumpy in response to any sudden noise or movement; it’s as if my brain has difficulty filtering out irrelevant stimuli. Listening to music, or fast speaking in television/movies, brings on a pressure headache and makes my brain feel like it’s full of static |
| Phantom sensations | 3 weeks post infection | Ongoing | Pinching and stinging sensations that feel like I am being bitten by a spider; these usually repeat every 10 minutes in the same body location over an hour or two |
| Cognitive deficits | 2 weeks post infection | Ongoing | Difficulty following conversations; video calls are overwhelming and bring on a pressure headache if they last past 15 minutes; constant mistakes while typing; having my brain "shut down" and feel like it's full of static if I try to engage in high level thinking or conversation for longer than 30 minutes at a time |
| Memory dysfunction | 2 weeks post infection | Ongoing | Complete loss of memory from the 2 months post infection; previous recall ability is severely reduced; reliant on lists and online calendars to remember anything where previously I was able to run science experiments, manage a household, and parent without difficulty |
| Speech issues | 2 weeks post infection | Ongoing | Losing words mid-sentence and being unable to recall them; saying the wrong word in a sentence and not realising, then being incapable of producing the right word even when corrected and making an effort to do so |
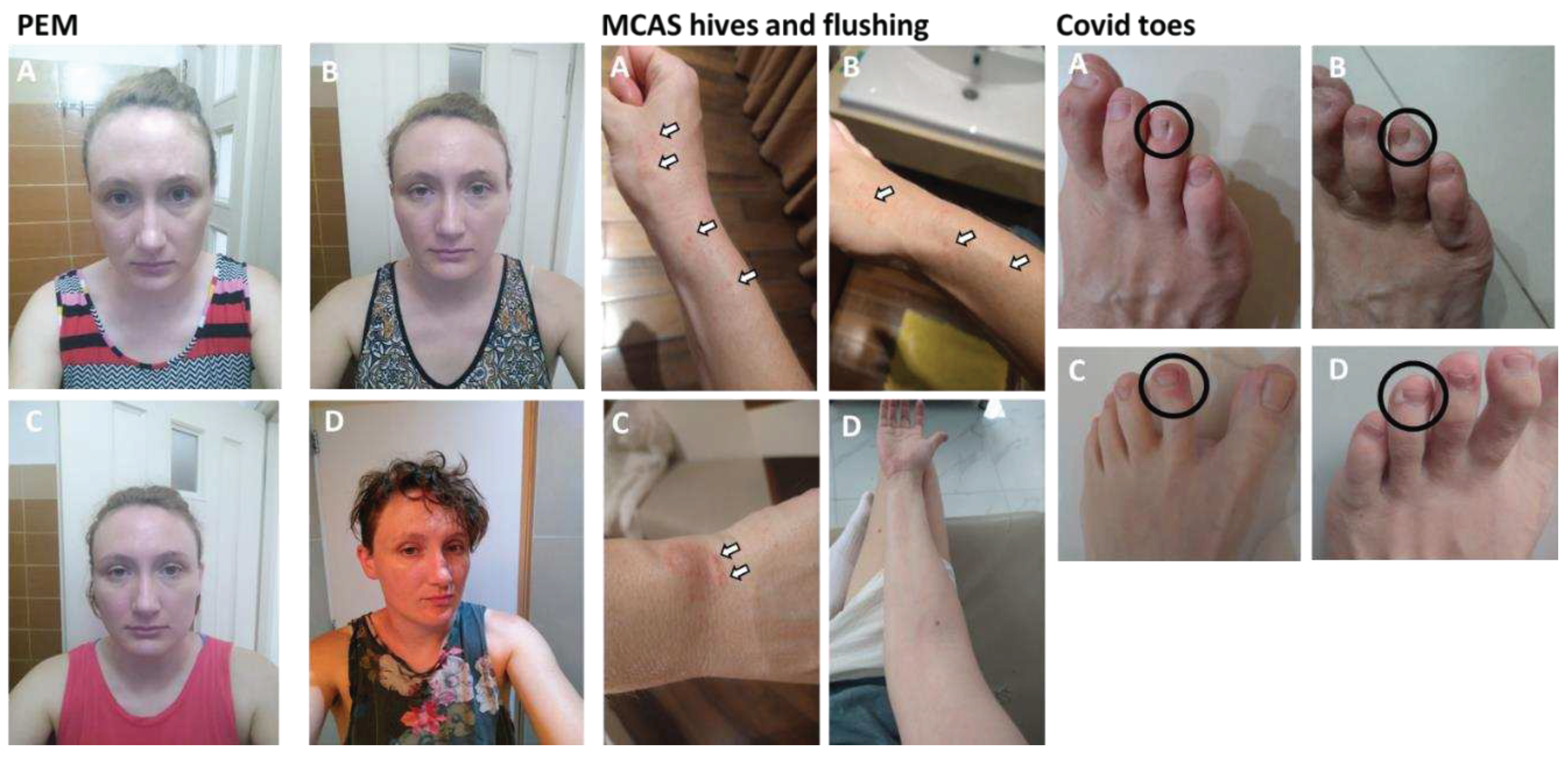
| Covid toes | 3 weeks post infection | Ongoing | Swollen, painful, red skin that appears on the edge of toenails and spreads down to the nearest knuckle; this skin then dies and forms a large white blister-like patch before peeling off |
| Muscle weakness | Day 2 of infection | Ongoing | Shaky and weak; unable to lift everyday objects, frequently dropping household items, burning myself on the oven or stove multiple times a day because my hands don't respond like they used to |
| Tachycardia | Day 2 of infection | Ongoing | During illness or times of stress, my heart rate increases to 120-130 bpm and stays there regardless of activity level or postural position |
| Palpitations | Day 2 of infection | 22 months constant, now in times of illness | My heart constantly skips beats, lurches and does half-beats, and pauses in the middle of beats so that it feels like it's not going to restart |
| Irregular menstruation | During acute infection | Ongoing | Despite taking the oral contraceptive pill; loss of period during acute illness, followed by extremely heavy 10 day long bleeds every month from March 2022 - September 2022; loss of menstruation starting in December 2022, with 4-6 month gaps between periods for the year of 2023 |
| Vertigo/dizziness | 2 weeks post infection | Ongoing | Brought on by sudden postural changes; at its worst I was unable to sit upright without the entire room tilting and spinning around me; daily occurrences of stumbling sideways due to sudden onset dizziness |
| Shortness of breath | During acute infection | Ongoing | Tightness around my ribs and chest, like an iron band is squeezing me and I can't ever draw in a full breath; worsens with physical exertion |
| Hives | 6 weeks post infection | 18 months | Dry, itchy and painful. I was scratching in my sleep until I bled |
| Severe hayfever reactions | 6 weeks post infection | Ongoing, occur every 2 weeks | Itchy deep within my sinuses and nostrils, uncontrollably sneezing every 90 seconds for 36 hours straight, streaming itchy eyes, sudden pressure headache, severe joint pain, muzzy headed and foggy brained. Feel like I’ve been hit by a truck full of pollen |
| Post-exertional malaise (PEM) | 3 weeks post infection | Ongoing | All of the above symptoms worsen when I over-exert myself mentally, physically or emotionally; PEM also feels like a combination of having a bad hangover, jetlag, coming down with the flu, and extreme exhaustion all at the same time, on top of the other symptoms worsening |
Management of long-term Long Covid symptoms
Discussion
Acknowledgements
Conflicts of Interest
References
- Greenhalgh, T., et al., Management of post-acute covid-19 in primary care. BMJ, 2020. 370: p. m3026. [CrossRef]
- Mohammed F. Islam, J.C.L.A.J., Post-viral fatigue and COVID-19: lessons from past epidemics. Fatigue: Biomedicine, Health & Behavior, 2020. 8(2): p. 61-69. [CrossRef]
- Davis, H.E., et al., Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol, 2023. 21(3): p. 133-146. [CrossRef]
- MEpedia. History of myalgic encephalomyelitis and chronic fatigue syndrome. 2023; Available from: https://me-pedia.org/wiki/History_of_myalgic_encephalomyelitis_and_chronic_fatigue_syndrome#:~:text=It%20was%20named%20myalgic%20encephalomyelitis,redefined%20as%20Chronic%20Fatigue%20Syndrome.
- Ballering, A.V., et al., Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet, 2022. 400(10350): p. 452-461. [CrossRef]
- Foundation, d.B., Poll: Physicians agree Long Covid is a problem but are unprepared to treat it. 2022.
- Bai, F., et al., Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect, 2022. 28(4): p. 611 e9-611 e16. [CrossRef]
- Torjesen, I., Covid-19: Middle aged women face greater risk of debilitating long term symptoms. BMJ, 2021. 372: p. n829. [CrossRef]
- Gavrilova, N., et al., New Clinical Phenotype of the Post-Covid Syndrome: Fibromyalgia and Joint Hypermobility Condition. Pathophysiology, 2022. 29(1): p. 24-29. [CrossRef]
- Wolff, D., et al., Allergic diseases as risk factors for Long-COVID symptoms: Systematic review of prospective cohort studies. Clin Exp Allergy, 2023. 53(11): p. 1162-1176. [CrossRef]
- Rivera, J., et al., Prevalence of post-COVID-19 in patients with fibromyalgia: a comparative study with other inflammatory and autoimmune rheumatic diseases. BMC Musculoskelet Disord, 2022. 23(1): p. 471. [CrossRef]
- Sapkota, H.R. and A. Nune, Long COVID from rheumatology perspective - a narrative review. Clin Rheumatol, 2022. 41(2): p. 337-348. [CrossRef]
- Raj, S.R., A. Fedorowski, and R.S. Sheldon, Diagnosis and management of postural orthostatic tachycardia syndrome. CMAJ, 2022. 194(10): p. E378-E385. [CrossRef]
- Afrin, L.B., et al., Diagnosis of mast cell activation syndrome: a global "consensus-2". Diagnosis (Berl), 2021. 8(2): p. 137-152. [CrossRef]
- Sommerfelt, K.S., T.; Seton, K.A.; Carding, S.R. Assessing Functional Capacity in ME/CFS: A Patient Informed Questionnaire. Preprints 2023. 2023092091. [CrossRef]
- Grach, S.L., et al., Diagnosis and Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Mayo Clin Proc, 2023. 98(10): p. 1544-1551. [CrossRef]
- Butterfield, J.H., Survey of aspirin administration in systemic mastocytosis. Prostaglandins Other Lipid Mediat, 2009. 88(3-4): p. 122-4. [CrossRef]
- Etheresia Pretorius, C.V., Gert Jacobus Laubscher et al. Combined triple treatment of fibrin amyloid microclots and platelet pathology in individuals with Long COVID/ Post-Acute Sequelae of COVID-19 (PASC) can resolve their persistent symptoms. Research Square, 28 December 2021. [CrossRef]
- Snapper, H. and W.P. Cheshire, Oral and intravenous hydration in the treatment of orthostatic hypotension and postural tachycardia syndrome. Auton Neurosci, 2022. 238: p. 102951. [CrossRef]
- Schloss, J.V., Nutritional deficiencies that may predispose to long COVID. Inflammopharmacology, 2023. 31(2): p. 573-583. [CrossRef]
- Ranisavljev, M., et al., Reduced tissue creatine levels in patients with long COVID-19: A cross-sectional study. J Postgrad Med, 2023. 69(3): p. 162-163. [CrossRef]
- Slankamenac, J., et al., Creatine supplementation combined with breathing exercises reduces respiratory discomfort and improves creatine status in patients with long-COVID. J Postgrad Med, 2023. [CrossRef]
- Hsu, R.L., et al., Amyloid-degrading ability of nattokinase from Bacillus subtilis natto. J Agric Food Chem, 2009. 57(2): p. 503-8. [CrossRef]
- Tanikawa, T., et al., Degradative Effect of Nattokinase on Spike Protein of SARS-CoV-2. Molecules, 2022. 27(17). [CrossRef]
- Chansaenroj, J., et al., Long-term persistence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein-specific and neutralizing antibodies in recovered COVID-19 patients. PLoS One, 2022. 17(4): p. e0267102. [CrossRef]
- Arman Fesharaki-Zadeh, N.L., Amy F.T. Arnsten, Clinical experience with the α2A-adrenoceptor agonist, guanfacine, and N-acetylcysteine for the treatment of cognitive deficits in “Long-COVID19”. Neuroimmunology Reports, 2023. 3(100154). [CrossRef]
- McPherson, R.A., et al., N -acetylcysteine is associated with reduction of postconcussive symptoms in elderly patients: A pilot study. J Trauma Acute Care Surg, 2022. 93(5): p. 644-649. [CrossRef]
- Zubchenko, S., et al., Herpesvirus infections and post-COVID-19 manifestations: a pilot observational study. Rheumatol Int, 2022. 42(9): p. 1523-1530. [CrossRef]
- German, E.R., M.K. Jairath, and J. Caston, Treatment of Long-Haul COVID Patients With Off-Label Acyclovir. Cureus, 2023. 15(4): p. e37926. [CrossRef]
- Bramante, C.T., et al., Outpatient treatment of COVID-19 and incidence of post-COVID-19 condition over 10 months (COVID-OUT): a multicentre, randomised, quadruple-blind, parallel-group, phase 3 trial. Lancet Infect Dis, 2023. 23(10): p. 1119-1129. [CrossRef]
- Andrzejewski, S., et al., Metformin directly acts on mitochondria to alter cellular bioenergetics. Cancer Metab, 2014. 2: p. 12. [CrossRef]
- Appelman, B., et al., Muscle abnormalities worsen after post-exertional malaise in long COVID. Nat Commun, 2024. 15(1): p. 17. [CrossRef]
- Chen, T.H., C.J. Chang, and P.H. Hung, Possible Pathogenesis and Prevention of Long COVID: SARS-CoV-2-Induced Mitochondrial Disorder. Int J Mol Sci, 2023. 24(9). [CrossRef]
- Cookson, H. and C. Grattan, An update on mast cell disorders. Clin Med (Lond), 2016. 16(6): p. 580-583. [CrossRef]
- Salvucci, F., et al., Antihistamines improve cardiovascular manifestations and other symptoms of long-COVID attributed to mast cell activation. Front Cardiovasc Med, 2023. 10: p. 1202696. [CrossRef]
- Heald, A., et al., Reducing fatigue-related symptoms in Long COVID-19: a preliminary report of a lymphatic drainage intervention. Cardiovasc Endocrinol Metab, 2022. 11(2): p. e0261. [CrossRef]
- Espejo, J.A., M. Garcia-Escudero, and E. Oltra, Unraveling the Molecular Determinants of Manual Therapy: An Approach to Integrative Therapeutics for the Treatment of Fibromyalgia and Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Int J Mol Sci, 2018. 19(9). [CrossRef]
- Li, H., et al., Chronic fatigue syndrome treated by the traditional Chinese procedure abdominal tuina: a randomized controlled clinical trial. J Tradit Chin Med, 2017. 37(6): p. 819-826. [CrossRef]
- Bourne, K.M., et al., Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients With Postural Orthostatic Tachycardia Syndrome. J Am Coll Cardiol, 2021. 77(3): p. 285-296. [CrossRef]
- Eastin E F, T.A., Quach T C, et al. New Alcohol Sensitivity in Patients With Post-acute Sequelae of SARS-CoV-2 (PASC): A Case Series. Cureus, 2023. 15. [CrossRef]
- Sher, L., Long COVID and the risk of suicide. Gen Hosp Psychiatry, 2023. 80: p. 66-67. [CrossRef]
| Intervention | Time of day | Dosage | Side effects | Symptoms alleviated | Rationale & references |
|---|---|---|---|---|---|
| Aspirin | 7am | 160mg | Nil | Cognitive and speech issues, joint pain, joint subluxations, extreme fatigue | Aspirin brings down MCAS symptoms [17], reduces incidence of blood clots, and breaks down Long Covid microclots [18] |
| Rehydration salts, berocca and creatine | 7am | 1 litre water with 1 pouch rehydration salts, 1 berocca tablet, 1 scoop creatine | Nil | Vertigo/dizziness, pressure headache, muscle weakness | Bolus fluids alleviate POTS symptoms [19], B vitamins are deficient in Long Covid [20], creatine relieves Long Covid symptoms [21,22] |
| Nattokinase | 9pm | 6000 units | Occasional nausea and heart burn sensation; taking 2 hours after dinner helps prevent this | Long and heavy menstruation, extreme fatigue, cognitive and speech issues, covid toes | Nattokinase breaks down amyloid clots [23] and also breaks down Covid-19 spike protein [24], which is known to persist in the body after Covid-19 infection [25] |
| N-acetylcysteine (NAC) | 9pm | 1 tablet | Nil | Cognitive and speech issues | NAC is known to reduce cognitive issues in Long Covid [26] and following concussion [27] |
| Acyclovir | 9pm every 2 days | 400mg | Upper left abdominal pain; lightheadedness; nausea; adjusting dosage helped stop these | Cognitive and speech issues, extreme fatigue | Herpes virus activation in Long Covid is known to contribute to health issues [28] and acyclovyr has been trialled as a treatment in a small group of Long Covid patients [29] |
| Metformin | 9pm | 500mg | Nausea and upset stomach alternating between diarrhea and constipation for the first 10 days | Cognitive, speech and memory issues, extreme fatigue, muscle weakness, muscle pain, covid toes, unrefreshing sleep, sensory sensitivities, palpitations, and tachycardia | Metformin reduces incidence of Long Covid if given during acute infection [30], and aids in mitochondrial repair and function [31] which are deficient in Long Covid [32,33] |
| Ibuprofen | 9pm | 400mg | Nil | Muscle pain and joint pain | Ibuprofen is an anti-inflammatory pain medication |
| Antihistamine (fexofenadine hydrochloride) | 9pm | 180mg | Nil | Hives, severe hayfever reactions, joint subluxations, extreme fatigue, cognitive issues, palpitations | Antihistamines are used for the management of MCAS [34] and alleviate Long Covid symptoms [35] |
| Multivitamin | 9pm | 1 tablet | Nil | Long Covid patients display vitamin deficiencies [20] | |
| Massage therapy | 9am | 90 minutes weekly | Increased fatigue immediately after, I usually sleep after a massage | Muscle pain, joint pain, muscle weakness, extreme fatigue, cognitive issues | Lymphatic drainage massage alleviates Long Covid symptoms [36], and full body massage alleviates ME symptoms [37,38] |
| Thuan Moc ointment | 9am and 9pm | Apply directly to hives | Nil | Hives (completely eliminated after a few weeks of use) | Most likely due to the willow bark extract in the cream |
| Compression socks | All day | Feeling spacey and light-headed | Extreme fatigue, PEM | Compression socks help to regulate blood pressure issues caused by POTS [39] | |
| Abstinence from alcohol | Constant | Extreme fatigue, joint pain, muscle pain, headache, vertigo/dizziness | Alcohol exacerbates Long Covid symptoms [40] | ||
| Resting and pacing | All the time | Scheduling rest before and after activity; making sure to sleep whenever I felt tired | Nil | Extreme fatigue, cognitive and speech issues, muscle pain, PEM | Resting and pacing is a well-established management technique for infection-associated chronic conditions (https://www.meaction.net/stoprestpace/) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





