Preprint
Article
Shock Absorption Capacity of High-Performance Polymers for Dental Implant Prosthesis: In Vitro Study
Altmetrics
Downloads
152
Views
59
Comments
0
A peer-reviewed article of this preprint also exists.
Submitted:
23 January 2024
Posted:
23 January 2024
You are already at the latest version
Alerts
Abstract
Background: Restorative materials might significantly affect load transmission at peri-implant bone. The aim of the present study is to evaluate the shock absorption capacity of two different polymeric materials to be used as frameworks for implant-supported prostheses.
Methods: A masticatory robot was used to compare the shock absorption capacity of polyether-ketoneketone (PEKK) Pekkton®ivory (Cendres+Mètaux) and glass fiber-reinforced composite (GFRC) TRINIATM (Bicon). Five identical sample crowns for each of the materials was tested un-der the same conditions described in previously published papers (Menini et al. 2013). Forces transmitted at the simulated periimplant bone were recorded and statistically analysed.
Results: The statistical analysis of forces transmitted at the simulated dental implant revealed significant differences between all the materials tested and significant differences with the mate-rials tested in a previously published paper (Menini et al. 2013: zirconia, glass ceramic, composite resin, acrylic resin). Only differences between PEKK and veneered PEKK and between PEKK and one of the previously tested composite resins were not statistically significant. PEKK samples demonstrated significantly greater shock absorption capacity compared to GFRC.
Conclusions: PEKK revealed optimal shock absorption capacity. Further studies are needed to evaluate its efficacy in case of long span prostheses with reduced prosthetic volume.
Keywords:
Subject: Medicine and Pharmacology - Dentistry and Oral Surgery
1. Introduction
The design and material of implant-supported prostheses greatly affect the long-term success of the rehabilitation contributing to the recovery of masticatory function as well as patients’ quality of life. Usually frameworks for implant-supported prostheses are made by casting metal or milling either titanium or zirconia [1,2]. As an alternative, polymeric materials might be also used as framework materials.
Previously published studies demonstrated the feasibility of using carbon fiber reinforced composites (CFRC) or glass fiber reinforced composites (GFRC) for the fabrication of full-arch implant-supported prostheses [1,2,3].
In addition, high performance polymers (HPPs) are available. The HPPs that have entered dentistry are the polyaryletherketones (PAEKs), a family of synthetic semi-crystalline thermoplastic polymers including different materials with varying chemical structures. PAEKs are commonly described in terms of an «E» and a «K» which means the sequence of ether and ketone group units in the polymer structure.
The most common PAEKs are polyetheretherketone (PEEK) and polyetherketoneketone (PEKK), although also other polymers such as polyetherketone (PEK), polyetherketoneetherketoneketone (PEKEKK), etc. exist. In their unaltered, unfilled state, these materials are ivory-greyish in color and they can be filled with pigments or reinforcing agents in order to improve their esthetic and mechanical performances.
In particular, biocompatible high-performance polymer (BioHPP) is a PEEK subgroup with an additional 20% of 0.3- to 0.5-mm ceramic fillers. It is currently being used in the fabrication of removable partial denture frameworks, removable dentures, obturators, crowns, fixed partial dentures, endocrowns, post-and-cores, and individual implant abutments [4,5,6].
On the other hand, polyetherketoneketone (PEKK) was first introduced by Bonner in 1962, and since then it has been used for different industrial and military purposes [7]. Thanks to its several qualities, it was introduced in the medical and dental field with a wide range of applications [8]. It has been used as an alternative to metal and ceramics in dentistry. It has excellent mechanical properties, low density, low weight, semiradiolucency, antibacterial activity, an ivory color similar to that of teeth, chemical and wear resistance, and excellent biocompatibility [7,8,9,10].
Regarding mechanical properties, PEKK demonstrated good strength-to-weight ratio and very closely resembles the characteristics of human mineralized tissues. In fact, its density (less than 2g/cm3), compressive strength (between 200 and 300 MPa) and modulus of elasticity (5.1 GPa) are comparable to those of dentin and bone. PEKK has an 80% greater compressive strength and better long-term fatigue properties than unreinforced PEEK, because of the extra ketone group [11,12].
Due to the above mentioned characteristics, PEKK has been taken into consideration as a restorative material for fixed prostheses in order to fabricate both monolithic and bi-layered structures, the latter veneered with composite resin, crowns and bridges on natural teeth, inlays-core with or without onlays and even monolithic posterior crowns [7].
Several applications have been documented, including: crown and bridges, endodontic posts, splinting devices, implant-supported prostheses, implant abutments, framework for overdentures and removable prostheses, etc. [13,14,15]. PEKK has been also used to fabricate dental implants [7].
PEKK can be manufactured in two different ways: injection molding (pressing) or CAD/CAM milling process. It must be underlined that the surface preparation of PEKK before bonding (a specific procedure combining mechanical retention and chemical bonding) is mandatory in order to obtain acceptable bonding values. According to an in vitro study by Fuhrmann et al., evaluating resin bonding to PAEKs, crystalline and amorphous PEKK exhibited lower values of tensile bond strength than fiber-reinforced PEEK, and highest values were achieved after conditioning PEKK and PEEK with silica coating and priming [16].
Ease of product and repair, resistance to corrosion, possible shock absorption capacity, good aesthetics, low costs, etc. make polymeric materials like PEKK particularly suitable also for implant prosthodontics when compared to other aesthetic materials such as ceramic and zirconia.
In addition, restorations made of radiolucent polymers such as PEEK or PEKK can significantly reduce CT artifacts and increase image quality compared to titanium and zirconia [17].
However, these new promising materials need in vitro and in vivo investigations to validate their effectiveness.
One of the most relevant mechanical properties related to the aspect of shock absorption is the flexural strength and elastic modulus. This aspect has to be considered when investigating the eventual application of PEKK as framework material in implant prosthodontics, especially for full-arch implant-supported rehabilitations and especially in case of immediate loading protocols where load control is mandatory to ensure an adequate osseointegration avoiding or minimizing implant micromovements. A proper load control is tied to patient-related factors and to prosthesis design and material. The presence of a stiff substructure, which rigidly splints the implants together, is supposed to provide a good distribution of occlusal stress more evenly to the abutments and implants. This would prevent high levels of compressive forces and strains on peri-implant bone, which is particularly important right after implants insertion in case of immediate loading [1,18] . At the same time the shock-absorption capacity of restorative materials might help to dampen occlusal loads [19].
Shock-absorption is supposed to be different for this innovative polymeric material, compared to competitor polymeric materials (fibre-reinforced composites) and traditional materials (acrylic resin, traditional resin composite, glass ceramic, gold alloy, zirconia).
Therefore, the aim of the present in vitro study was to compare the shock absorption capacity of a high-performance polymer with the shock absorption capacity of a glass fiber reinforced composite through the use of a masticatory robot.
In particular Pekkton®ivory, that is a polyetherketoneketone with titanium dioxide pigments, was tested and compared with TRINIA®, a high performance CAD/CAM glass fiber-reinforced composite. Both veneered and non-veneered crowns have been tested.
In addition, the outcomes were compared with those of previously tested materials (acrylic resin, composite resin, gold alloy, glass ceramic and zirconia) [19].
2. Materials and Methods
The masticatory robot set-up of the University of Genova (Italy) used in previously published papers [19,20,21] (Figure 1) was used to compare the shock absorption capacity of 2 polymeric materials: polyetherketoneketone Pekkton®ivory (Cendres+Mètaux SA, Biel/Bienne, CH) and glass fiber-reinforced nanohybrid composite resin TRINIATM (Bicon, Boston, USA) (Table 1).
The masticatory robot is able to simulate three-dimensionally the masticatory cycle and to reproduce the forces exerted during mastication. The movable part of the robot is constituted of a Stewart platform and it is equipped with a sensorized base which records the loads transmitted at the pin simulating the implant-abutment system. Sample crowns to be tested are placed on the pin [20,21].
2.1. Sample crowns
Five identical sample crowns were made of each of the materials to be tested: 5 Pekkton®ivory full contour samples (PI), 5 Pekkton®ivory veneered samples (PIV), and 5 TRINIATM full contour samples (TR) (n=15).
Both PI and TR sample crowns were milled. PIV crowns were realized using milled Pekkton®ivory as framework material with thickness in the range of IFU recommendations (i.e., 1 mm). The framework was veneered using the composite resin anaxBLEND Flow opaquer and dentin (anaxdent GmbH, Stuttgart, DE).
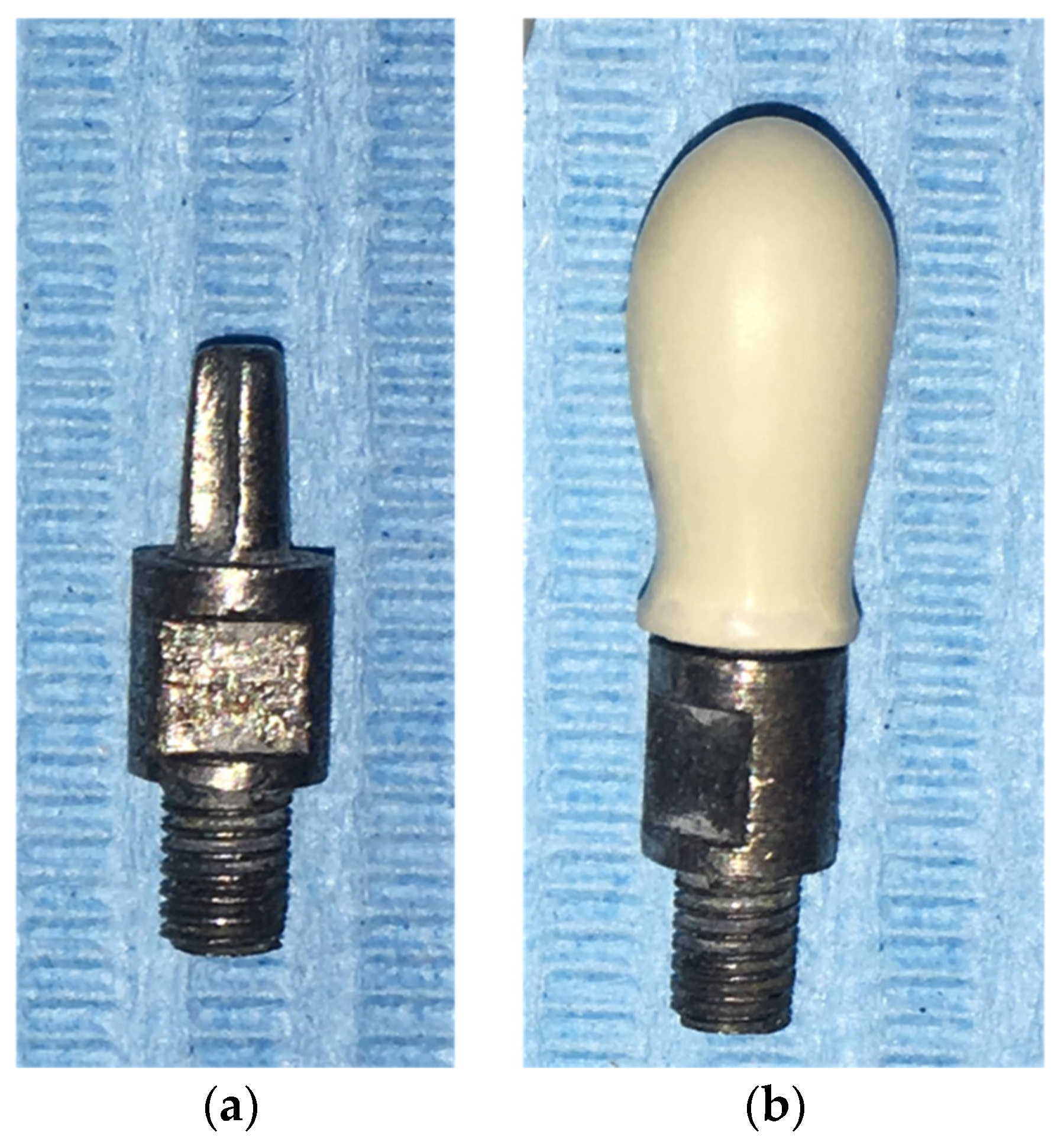
All the crowns had identical shape and dimensions (5 mm thick) to the ones tested in previously published studies in order to be fitted on the existing metal pin simulating the implant-abutment system to be screwed in the masticatory robot [19].
Figure 2.
(a) Pin simulating the implant-abutment system provided with a groove that matches with the sample crown; (b) PEKK crown inserted onto the pin.
Figure 2.
(a) Pin simulating the implant-abutment system provided with a groove that matches with the sample crown; (b) PEKK crown inserted onto the pin.
2.2. Test set-up
The samples were tested using the robotic chewing simulator of Genoa University under the same conditions described in previously published papers. The chewing robot was set to follow the same 3-dimensional trajectory used in previously published studies [19].
All the crowns were positioned in occlusion with the flat fixed upper part of the robot (start position=end position) and were placed under 100 consecutive chewing cycles.
2.3. Statistical analysis
Only vertical loads on z-axis were considered and then processed With MATLAB 6.1 software (MathWorks). The maximum values of the forces (N) for each chewing cycle were recorded and mean and standard deviation (SD) of the maximum values of the forces were calculated for each sample crown. These values underwent statistical analysis using the software SAS 9.4. Two-way analysis of variance (ANOVA) was used to compare maximum forces and Welch's t-test, considered in case of unequal variances, has been computed. The data recorded in the present investigation were also compared with data reported in the previously published study [19]. Alpha was set at .05.
3. Results
No fractures nor chippings of the samples occurred during the tests.
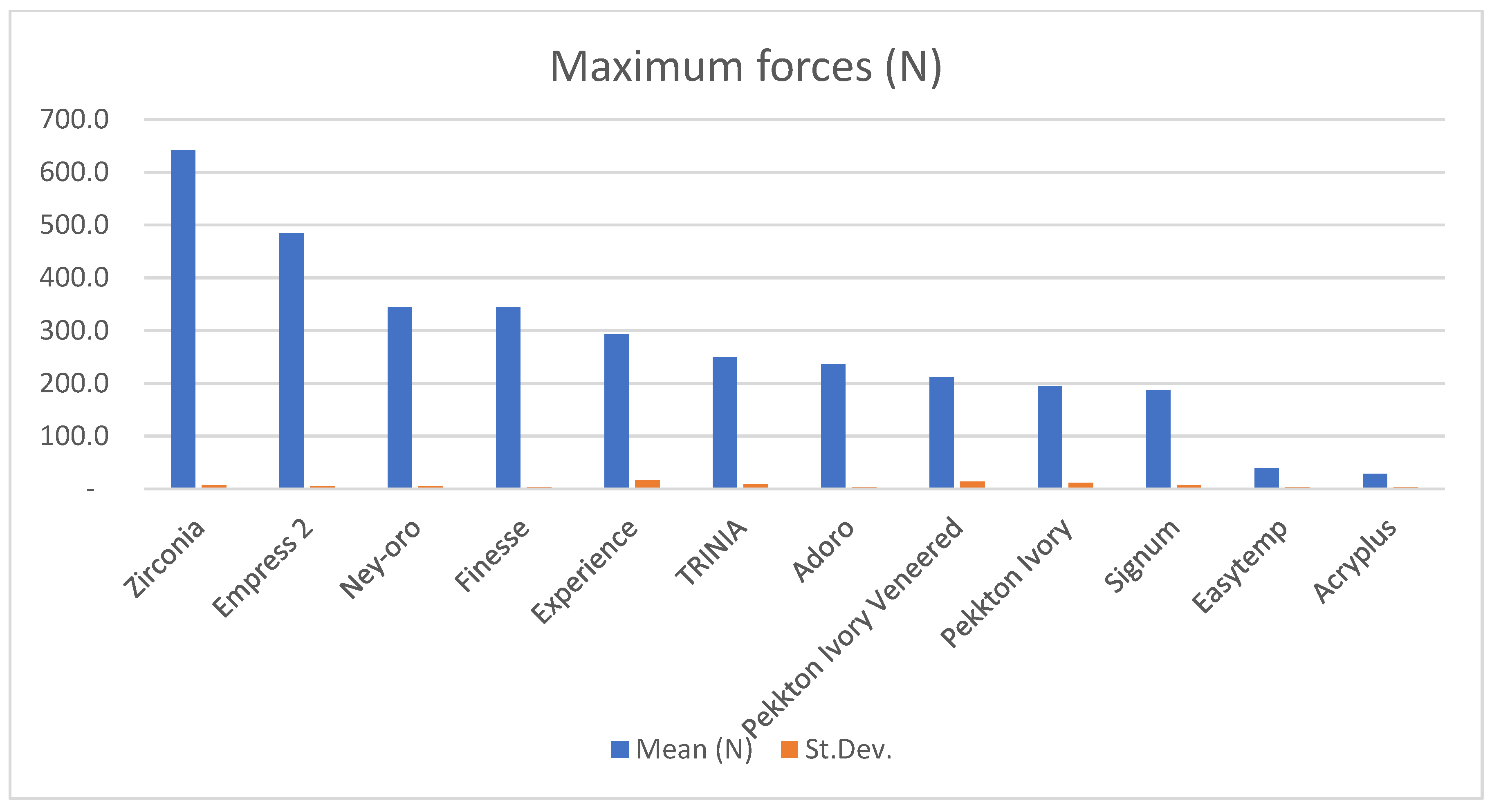
All the sample crowns showed a shock-absorption behaviour similar to composite resin materials tested in previously published studies [19]. The values of stresses transmitted to the simulated periimplant bone resulted far lower compared to zirconia, ceramic materials and metal alloys.
Resulting vertical loads expressed in Newton are resumed in Table 2.
The analysis of variance (ANOVA) revealed statistically significant differences with a p-value<.0001.
No considerable differences were found between Pekkton®ivory and Pekkton®ivory Veneered, within a significance level of 5% (p-value Pekkton Ivory vs Pekkton Ivory Veneered 6.45%).
On the contrary, TRINIATM showed higher values of force compared to Pekkton®ivory and Pekkton®ivory Veneered.
Both Pekkton Ivory vs TRINIATM and Pekkton Ivory Veneered vs TRINIATM presented significant statistical differences in forces transmitted at the simulated dental implant with p-values <1%.
Welch's t-test was applied to individually compare Pekkton Ivory, Pekkton Ivory Veneered, and TRINIATM with each of the materials tested in the previously published paper [19]. All the comparisons revealed statistically significant differences at 1% except the comparison between Pekkton Ivory and Signum composite resin (p-value: 0.2396).
Table 2.
Table resuming mean maximum occlusal forces (N) recorded during 100 masticatory cycles of the masticatory robot using sample crowns made of PEEK and of glass fiber-reinforced composite.
Table 2.
Table resuming mean maximum occlusal forces (N) recorded during 100 masticatory cycles of the masticatory robot using sample crowns made of PEEK and of glass fiber-reinforced composite.
| Sample | Pekkton® ivory | Pekkton® ivory veneered | TRINIATM | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD (N) | min (N) | MAX (N) | Mean ± SD (N) | min (N) | MAX (N) | Mean ± SD (N) | min (N) | MAX (N) | |
| 1 | 194.664 ± 2.037 | 191.547 | 207.656 | 214.274 ± 2.143 | 210.955 | 224.221 | 240.685 ± 1.890 | 237.622 | 251.655 |
| 2 | 201.490 ± 1.961 | 197.282 | 213.019 | 229.910 ± 1.777 | 226.891 | 239.053 | 257.446 ± 2.415 | 253.766 | 273.020 |
| 3 | 174.865 ± 4.254 | 169.962 | 194.329 | 216.873 ± 2.010 | 211.908 | 227.352 | 245.492 ± 3.960 | 240.717 | 274.793 |
| 4 | 198.381 ± 2.060 | 195.554 | 211.475 | 193.914 ± 1.951 | 189.975 | 205.977 | 260.094 ± 3.805 | 255.703 | 286.513 |
| 5 | 202.872 ± 2.306 | 199.964 | 217.816 | 203.231 ± 1.878 | 197.737 | 212.133 | 247.298 ± 2.254 | 243.770 | 262.483 |
| Mean | 194.454 ± 10.544 | 169.962 | 217.816 | 211.640 ± 12.437 | 189.975 | 239.053 | 250.203 ± 7.954 | 237.622 | 286.513 |
Figure 3.
Maximum vertical forces recorded for the materials tested in the present investigation and for the materials tested in the previously published paper [19].
Figure 3.
Maximum vertical forces recorded for the materials tested in the present investigation and for the materials tested in the previously published paper [19].
4. Discussion
The present investigation shed light on the shock-absorption capacity of two different polymers employed for implant-supported fixed prosthesis. Sample crowns were realized using PEKK (Pekkton®ivory), and a glass fibre-reinforced composite (TRINIATM). The use of different restorative materials significantly affected the forces transmitted at the simulation of the dental implant. Only the differences between PI and PIV and between PI and Signum composite resin were not statistically significant, probably due to the similar elastic modulus of the two polymers.
Tests have been performed using also veneered crowns using Pekkton®ivory as framework material and a composite resin as veneering material (anaxBLEND Flow opaquer and dentin) in order to be closer to real situations. In fact, PEKK requires veneering due to its low translucency and grayish color. The bond strength of composite veneering materials is one of the aspects of PEKK that needs further evaluation in future studies [8].
In fixed prosthesis, one of the crucial factors for long-term clinical success is the correct choice of the framework material that supports the artificial teeth, and transfers the loads to the substructures including implants and periimplant bone [22].
Frameworks for implant-supported prosthesis are typically made by casting metal or milling titanium or zirconia.
Metal reduced elastic modulus and consequent high stiffness allows distribution of masticatory loads at the periimplant bone. However, metal is less resistant to bending, less biocompatible, and entails high costs and process time. In addition, its adhesive affinity with acrylic resin is not optimal and often causes the chipping of dental aesthetic veneers from the framework, with consequential patient discomfort [1].
Titanium with its alloys is also rigid, more biocompatible, but has a high melting point and reactivity, making special equipment necessary for its processing [23].
Metal-free computer-aided design and computer-aided manufacturing (CAD-CAM) dental materials have been developed and include zirconia and also high-performance polymers and glass fiber-reinforced polymers such as the ones tested in the present study.
The use of zirconia prostheses in modern implantology have been proposed as a promising alternative to conventional metal-based restorations. Aesthetic concerns lead to the indication of zirconia, due to its favorable biocompatible, biological and mechanical properties [24].
The principal technical complication of zirconia implant-supported fixed dental prostheses is chipping or fracture of the layering porcelain [25]. A clinical study found a 31.25% porcelain chipping/fracture rate after 2-4 years of function [26]. In addition, some authors suggested caution in employing zirconia frameworks, especially in case of potential risk factors for mechanical complications (e.g., parafunctional habits), because of zirconia high rigidity and strain concentration [27].
According to two recent systematic reviews, high zirconia weight, its difficult adjustment and polishing, as well as complications such as ceramic veneer chipping and the less frequent framework failure still represent frequent and unsolved problems [1,28].
Since the 1980s, there has been an interest in fiber reinforced composites (CFRCs), a group of nonmetallic biomaterials consisting of a resin matrix incorporating fibers made of carbon, or in most cases they are glass fibers. CFRCs special features include biocompatibility, aesthetics, low weight, and good static and dynamic strength, especially breaking strength in relation to weight. They are also less expensive than metals. In addition to cohesion agents and coatings (which improve wettability of the fibers and their adhesion to the matrix) they possess fillers that provide dimensional stability, reducing their cost [2,18,29].
According to a study by Menini et al., prosthesis tested with a carbon fiber-reinforced framework showed an amount of stress transfer to the supporting implants that was intermediate between metal framework and full-acrylic prosthesis [18].
CFRCs demonstrated optimal biocompatibility and mechanical characteristics, and they now appear suitable for the fabrication of frameworks for implant-supported full-arch restorations. However, the manufacture technique strongly affects the material mechanical characteristics, therefore great care must be taken in the use of this material [30,31].
Glass fiber reinforced composites have been also proposed as framework material for implant-supported prostheses providing esthetic advantage compared to CFRC. In the present study TRINIATM (Bicon, Boston, USA) has been tested, which consists of 60% multi-directional interlacing glass fibers (woven configuration) and 40% epoxy resin in several layers [6,32,33,34]. TRINIATM is employed to fabricate copings, frameworks for anterior or posterior crowns and bridges, and for cemented or uncemented restorations, such as telescopic crowns.
Jovanovic et al reported that glass fiber-reinforced resin-based materials reduce the impact of functional load on implants up to 50% when compared with ceramic-reinforced resin-based materials, in fact the elastic modulus is similar (18.8 GPa) to that of dentin (18.6 GPa) [6].
In the in vitro study my Omaish et al., the microstrain values recorded around implants restored with TRINIATM were also significantly lower than those restored with bioactive high-performance polymer (BioHPP) when a static load was applied, with considerably higher microstrain when the implant abutment angulation increased [33].
On the other hand, non-reinforced acrylic resin, due to the reduced elastic modulus and low stiffness showed good flexural strength, but a higher degree of deformation resulting in more overload on the abutment closer to the loading point when multiunit prostheses are considered [30]. Thanks to their shock absorption potential, resilient veneering materials, such as acrylic or composite resin, have been proposed for coating rigid metal frameworks in traditional treatment protocols for full-arch implant supported rehabilitations [35].
Results previously reported by Menini et al. have shown that composite and acrylic resin absorb shocks from occlusal forces significantly better than ceramic and zirconia. This would allow to reduce loads at the bone-implant interface [19]. The presence of a rigid framework (so that loads are evenly distributed over the supporting implants), combined with a shock-absorbing effect of the veneering material, can be considered by the authors an optimal option for controlling occlusal loads.
PEKK, a synthetic methacrylate-free high-performance polymer (HPP) with a semicrystalline structure, could be a versatile material that resumes several of the cited characteristics that are sought in a restorative material. In fact, it shows excellent physical and mechanical properties, such as melting temperature, compressive and fracture strength, and, as demonstrated by the present study, optimal shock absorption capacity [11,12,36,37,38]. According to a study by Alsadon et al. the fatigue limit of PEKK composite-coated molar crowns was comparable to that of cobalt-chrome and polymethylmethacrylate (PMMA) (750 N) [39]. In addition, thanks to its excellent biocompatibility, it should be considered as an alternative to metal and ceramics for dental restorations [40]. In the present study, Pekkton®ivory (Cendres+Mètaux SA, Biel/Bienne, CH) has been used as PEKK material which demonstrated a significantly greater shock absorption capacity compared to TRINIATM. Pekkton®ivory was previously available both for pressing and milling. The pressing technology was taken off the market but CAD-CAM milling blanks are still available today and have been used in the present study.
It must be noted that in the present study only single crowns have been tested in order to evaluate the shock absorption capacity of the materials. However, the use of PEKK and glass fiber reinforced composites as framework material should be carefully considered based on the prosthetic volume available. In fact, the thinner the framework and the longer the bridge span, the greater its flexure and possible bending moments on implant-prosthodontic components. Therefore, in case of multi-unit rehabilitations the outcomes could be different in terms of load transmitted to the dental implant and periimplant bone.
In vitro studies and short-term clinical reports have evaluated the use of PEKK in dentistry for implant supported dental prostheses with favourable outcomes [41,42]. A recent in vitro study concluded that, although PEEK and PEKK implant abutments with titanium bases demonstrated adequate fracture resistance, before recommending PEKK or PEEK as alternative implant abutments materials, further studies are needed in order to evaluate their long-term performance [15].
The present study, using a masticatory robot, has the advantage of overcoming some of the limitations of other in vitro studies that rely, for example, on finite element analysis (undermined by the simplification of results inherent in the virtual simulation itself). However, as explained in detail in our previous study [19], even this in vitro model has a number of limitations in reproducing the three-dimensional clinical reality of masticatory function. First of all differences should be considered based on the type of restorations: different outcomes are expected when testing single crowns rather than multi-unit prostheses, due to the possible flexure of the bridge span.
Little is known yet about PEKK mechanical response as frameworks for implant-supported full-arch prosthesis. A finite element analysis by Shash et al. investigated the effect of polymeric frameworks (e.g., CFR-PEEK 30%, CFR-PEEK 60%, PEKK, and PEEK) as alternatives to titanium frameworks in implant-supported full-arch fixed prosthesis. PEKK frameworks slightly reduced the stresses on bone tissues, especially in low-density bone, however, it increased the mucosal stress (even if these values did not exceed the pain threshold value) [43]. CFR-PEEK 60% distributed the loads in a similar manner as the titanium framework. The authors concluded that polymeric frameworks can offer improved performance and aesthetics, greater design freedom, production of lighter prostheses, reduced overall cost, and reduced manufacturing and mechanical problems compared with titanium (Shash et al, 2023).
According to a 3D-FEA by Lee et al., simulating a full-arch prosthesis supported by 4 maxillary implants, PEKK structures showed lower implant and tissue stress under compressive strain and higher stress under tensile strain. Therefore, the authors suggested that PEKK structure, being a resilient structure, should be limited in some areas, conversely a more rigid material such as titanium and zirconia can provide favorable stress distribution and safety of the implant prosthodontic components. [44].
A recent study by Villefort et al. employed the finite element analysis to compare the behavior of PEKK and PEEK prosthetic frameworks used in the all-on-four concept. It was observed that PEKK, thanks to its superior shock absorbance, induced lower stress concentration on the prosthetic screw and on the prosthetic base. According to the authors this would clinically represent a lower fracture risk on the acrylic base and screw loosening [10].
In conclusion, according to the results of the present research PEKK, thanks to its structure, low elastic modulus (3-5 GPa), and high shock-absorption characteristics, might contribute to shock absorption of occlusal loads, reducing the stresses transferred to periimplant bone. This makes it a promising metal-free framework material for implant-supported prosthesis, particularly in case of fixed partial dentures.
However, based on the present outcomes and on data reported in the literature, further investigations and especially long-term clinical studies are needed before recommending its application as a restorative material for implant-supported full-arch prostheses, especially in case of long span prostheses with reduced prosthetic volume where the risk of prosthesis flexure might indicate the use of more rigid materials.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “Conceptualization, M.M. and P.P.; methodology, M.M. and D.B.; formal analysis, L.C. and D.B.; investigation, P.S. and F.B.; resources, M.M. and P.P.; data curation, P.S. and F.B.; writing—original draft preparation, M.M., F.D. and P.S.; writing—review and editing, M.M., F.D. and M.M.; supervision, M.M. and L.C.; project administration, M.M.; funding acquisition, M.M. and P.P.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, M. Menini, upon request.
Acknowledgments
The authors wish to thank Cendres+Métaux SA, which supported the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Delucchi, F.; De Giovanni, E.; Pesce, P.; Bagnasco, F.; Pera, F.; Baldi, D.; Menini, M. Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials (Basel) 2021, 14. [Google Scholar] [CrossRef]
- Pera, F.; Pesce, P.; Solimano, F.; Tealdo, T.; Pera, P.; Menini, M. Carbon fibre versus metal framework in full-arch immediate loading rehabilitations of the maxilla - a cohort clinical study. J Oral Rehabil 2017, 44, 392–397. [Google Scholar] [CrossRef]
- Collaert, B.; De Bruyn, H. Immediate functional loading of TiOblast dental implants in full-arch edentulous maxillae: a 3-year prospective study. Clin Oral Implants Res 2008, 19, 1254–1260. [Google Scholar] [CrossRef]
- Arshad, M.; Hassantash, S.; Chinian, S.; Sadr, A.; Habibzadeh, S. Fracture strength and three-dimensional marginal evaluation of biocompatible high-performance polymer versus pressed lithium disilicate crowns. J Prosthet Dent 2023, 130, 132 e131–132 e139. [Google Scholar] [CrossRef] [PubMed]
- Elashmawy, Y.; Elshahawy, W.; Seddik, M.; Aboushelib, M. Influence of fatigue loading on fracture resistance of endodontically treated teeth restored with endocrowns. J Prosthodont Res 2021, 65, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Jovanovic, M.; Zivic, M.; Milosavljevic, M. A potential application of materials based on a polymer and CAD/CAM composite resins in prosthetic dentistry. J Prosthodont Res 2021, 65, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Alqurashi, H.; Khurshid, Z.; Syed, A.U.Y.; Rashid Habib, S.; Rokaya, D.; Zafar, M.S. Polyetherketoneketone (PEKK): An emerging biomaterial for oral implants and dental prostheses. J Adv Res 2021, 28, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Han, K.H.; Lee, J.Y.; Shin, S.W. Implant- and Tooth-Supported Fixed Prostheses Using a High-Performance Polymer (Pekkton) Framework. Int J Prosthodont 2016, 29, 451–454. [Google Scholar] [CrossRef] [PubMed]
- Klur, T.; Hasan, I.; Ottersbach, K.; Stark, H.; Fichte, M.; Dirk, C.; Bourauel, C. PEKK-made indirect temporary crowns and bridges: a clinical pilot study. Clin Oral Investig 2019, 23, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Villefort, R.F.; Diamantino, P.J.S.; Zeidler, S.; Borges, A.L.S.; Silva-Concilio, L.R.; Saavedra, G.; Tribst, J.P.M. Mechanical Response of PEKK and PEEK As Frameworks for Implant-Supported Full-Arch Fixed Dental Prosthesis: 3D Finite Element Analysis. Eur J Dent 2022, 16, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Shin, J.H.; Kim, J.E.; Kim, J.H.; Lee, W.C.; Shin, S.W.; Lee, J.Y. Corrigendum to "Biomechanical Evaluation of a Tooth Restored with High Performance Polymer PEKK Post-Core System: A 3D Finite Element Analysis". Biomed Res Int 2017, 2017, 7196847. [Google Scholar] [CrossRef]
- Lee, K.S.; Shin, J.H.; Kim, J.E.; Kim, J.H.; Lee, W.C.; Shin, S.W.; Lee, J.Y. Biomechanical Evaluation of a Tooth Restored with High Performance Polymer PEKK Post-Core System: A 3D Finite Element Analysis. Biomed Res Int 2017, 2017, 1373127. [Google Scholar] [CrossRef]
- Qian, B.; Ji, K.; Lu, W.; Wu, G.; Tan, B.; Jing, J.; Ji, J. Polyetherketoneketone, a high-performance polymer for splinting mobile teeth: A clinical report. J Prosthet Dent 2023. [Google Scholar] [CrossRef]
- Salem, M.T.; El-Layeh, M.; El-Farag, S.A.A.; Salem, A.S.; Attia, A. Clinical assessment of different implant-supported esthetic crown systems fabricated with semi-digital workflow: Two-year prospective study. J Esthet Restor Dent 2022, 34, 1247–1262. [Google Scholar] [CrossRef]
- Turksayar, A.A.D.; Atsu, S.S. Fracture Resistance of Zirconia, Polyetheretherketone, and Polyetherketoneketone Implant Abutments After Aging. Int J Oral Maxillofac Implants 2021, 36, 332–340. [Google Scholar] [CrossRef]
- Fuhrmann, G.; Steiner, M.; Freitag-Wolf, S.; Kern, M. Resin bonding to three types of polyaryletherketones (PAEKs)-durability and influence of surface conditioning. Dent Mater 2014, 30, 357–363. [Google Scholar] [CrossRef]
- Lommen, J.; Schorn, L.; Sproll, C.; Haussmann, J.; Kubler, N.R.; Budach, W.; Rana, M.; Tamaskovics, B. Reduction of CT Artifacts Using Polyetheretherketone (PEEK), Polyetherketoneketone (PEKK), Polyphenylsulfone (PPSU), and Polyethylene (PE) Reconstruction Plates in Oral Oncology. J Oral Maxillofac Surg 2022, 80, 1272–1283. [Google Scholar] [CrossRef] [PubMed]
- Menini, M.; Pesce, P.; Bevilacqua, M.; Pera, F.; Tealdo, T.; Barberis, F.; Pera, P. Effect of Framework in an Implant-Supported Full-Arch Fixed Prosthesis: 3D Finite Element Analysis. Int J Prosthodont 2015, 28, 627–630. [Google Scholar] [CrossRef]
- Menini, M.; Conserva, E.; Tealdo, T.; Bevilacqua, M.; Pera, F.; Signori, A.; Pera, P. Shock absorption capacity of restorative materials for dental implant prostheses: an in vitro study. Int J Prosthodont 2013, 26, 549–556. [Google Scholar] [CrossRef]
- Conserva, E.; Menini, M.; Tealdo, T.; Bevilacqua, M.; Pera, F.; Ravera, G.; Pera, P. Robotic chewing simulator for dental materials testing on a sensor-equipped implant setup. Int J Prosthodont 2008, 21, 501–508. [Google Scholar] [PubMed]
- Conserva, E.; Menini, M.; Tealdo, T.; Bevilacqua, M.; Ravera, G.; Pera, F.; Pera, P. The use of a masticatory robot to analyze the shock absorption capacity of different restorative materials for prosthetic implants: a preliminary report. Int J Prosthodont 2009, 22, 53–55. [Google Scholar]
- Kelkar, K.C.; Bhat, V.; Hegde, C. Finite element analysis of the effect of framework materials at the bone-implant interface in the all-on-four implant system. Dent Res J (Isfahan) 2021, 18, 1. [Google Scholar] [PubMed]
- Hoque, M.E.; Showva, N.N.; Ahmed, M.; Rashid, A.B.; Sadique, S.E.; El-Bialy, T.; Xu, H. Titanium and titanium alloys in dentistry: current trends, recent developments, and future prospects. Heliyon 2022, 8, e11300. [Google Scholar] [CrossRef] [PubMed]
- Dantas, T.A.; Pinto, P.; Vaz, P.C.S.; Silva, F.S. Design and optimization of zirconia functional surfaces for dental implants applications. Ceramics International 2020, 46, 16328–16336. [Google Scholar] [CrossRef]
- Kondo, T.; Komine, F.; Honda, J.; Takata, H.; Moriya, Y. Effect of veneering materials on fracture loads of implant-supported zirconia molar fixed dental prostheses. J Prosthodont Res 2019, 63, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Papaspyridakos, P.; Lal, K. Computer-assisted design/computer-assisted manufacturing zirconia implant fixed complete prostheses: clinical results and technical complications up to 4 years of function. Clin Oral Implants Res 2013, 24, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Tiossi, R.; Gomes, E.A.; Faria, A.C.L.; Rodrigues, R.C.S.; Ribeiro, R.F. Biomechanical behavior of titanium and zirconia frameworks for implant-supported full-arch fixed dental prosthesis. Clin Implant Dent Relat Res 2017, 19, 860–866. [Google Scholar] [CrossRef] [PubMed]
- Abdulmajeed, A.A.; Lim, K.G.; Narhi, T.O.; Cooper, L.F. Complete-arch implant-supported monolithic zirconia fixed dental prostheses: A systematic review. J Prosthet Dent 2016, 115, 672–677 e671. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K. An overview of development and status of fiber-reinforced composites as dental and medical biomaterials. Acta Biomater Odontol Scand 2018, 4, 44–55. [Google Scholar] [CrossRef]
- Menini, M.; Pesce, P.; Pera, F.; Barberis, F.; Lagazzo, A.; Bertola, L.; Pera, P. Biological and mechanical characterization of carbon fiber frameworks for dental implant applications. Mater Sci Eng C Mater Biol Appl 2017, 70, 646–655. [Google Scholar] [CrossRef]
- Pesce, P.; Lagazzo, A.; Barberis, F.; Repetto, L.; Pera, F.; Baldi, D.; Menini, M. Mechanical characterisation of multi vs. uni-directional carbon fiber frameworks for dental implant applications. Mater Sci Eng C Mater Biol Appl 2019, 102, 186–191. [Google Scholar] [CrossRef]
- Liebermann, A.; Wimmer, T.; Schmidlin, P.R.; Scherer, H.; Loffler, P.; Roos, M.; Stawarczyk, B. Physicomechanical characterization of polyetheretherketone and current esthetic dental CAD/CAM polymers after aging in different storage media. J Prosthet Dent 2016, 115, 321–328 e322. [Google Scholar] [CrossRef]
- Omaish, H.H.M.; Abdelhamid, A.M.; Neena, A.F. Comparison of the strain developed around implants with angled abutments with two reinforced polymeric CAD-CAM superstructure materials: An in vitro comparative study. J Prosthet Dent 2022, 127, 634 e631–634 e638. [Google Scholar] [CrossRef]
- Suzaki, N.; Yamaguchi, S.; Hirose, N.; Tanaka, R.; Takahashi, Y.; Imazato, S.; Hayashi, M. Evaluation of physical properties of fiber-reinforced composite resin. Dent Mater 2020, 36, 987–996. [Google Scholar] [CrossRef]
- Gracis, S.E.; Nicholls, J.I.; Chalupnik, J.D.; Yuodelis, R.A. Shock-absorbing behavior of five restorative materials used on implants. Int J Prosthodont 1991, 4, 282–291. [Google Scholar] [CrossRef]
- Elkabbany, A.; Kern, M.; Elkhadem, A.H.; Wille, S.; Amer, A.A.; Chaar, M.S. Retention of metallic and non-metallic double-crown-retained mandibular overdentures on implants: An in-vitro study. J Prosthodont Res 2020, 64, 384–390. [Google Scholar] [CrossRef]
- Nishihara, H.; Haro Adanez, M.; Att, W. Current status of zirconia implants in dentistry: preclinical tests. J Prosthodont Res 2019, 63, 1–14. [Google Scholar] [CrossRef]
- Song, C.H.; Choi, J.W.; Jeon, Y.C.; Jeong, C.M.; Lee, S.H.; Kang, E.S.; Yun, M.J.; Huh, J.B. Comparison of the Microtensile Bond Strength of a Polyetherketoneketone (PEKK) Tooth Post Cemented with Various Surface Treatments and Various Resin Cements. Materials (Basel) 2018, 11. [Google Scholar] [CrossRef] [PubMed]
- Alsadon, O.; Wood, D.; Patrick, D.; Pollington, S. Fatigue behavior and damage modes of high performance poly-ether-ketone-ketone PEKK bilayered crowns. J Mech Behav Biomed Mater 2020, 110, 103957. [Google Scholar] [CrossRef] [PubMed]
- Schwitalla, A.D.; Spintig, T.; Kallage, I.; Muller, W.D. Flexural behavior of PEEK materials for dental application. Dent Mater 2015, 31, 1377–1384. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.H.; Hyde, B.; Hurst, M.; Harris, B.T.; Lin, W.S. Polyetherketoneketone (PEKK), a framework material for complete fixed and removable dental prostheses: A clinical report. J Prosthet Dent 2018, 119, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Katzenbach, A.; Dorsam, I.; Stark, H.; Bourauel, C.; Keilig, L. Fatigue behaviour of dental crowns made from a novel high-performance polymer PEKK. Clin Oral Investig 2021, 25, 4895–4905. [Google Scholar] [CrossRef]
- Shash, Y.H.; El-Wakad, M.T.; El-Dosoky, M.A.A.; Dohiem, M.M. Evaluation of stresses on mandible bone and prosthetic parts in fixed prosthesis by utilizing CFR-PEEK, PEKK and PEEK frameworks. Sci Rep 2023, 13, 11542. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Shin, S.W.; Lee, S.P.; Kim, J.E.; Kim, J.H.; Lee, J.Y. Comparative Evaluation of a Four-Implant-Supported Polyetherketoneketone Framework Prosthesis: A Three-Dimensional Finite Element Analysis Based on Cone Beam Computed Tomography and Computer-Aided Design. Int J Prosthodont 2017, 30, 581–585. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
The sensor-equipped masticatory robot employed in the present research.
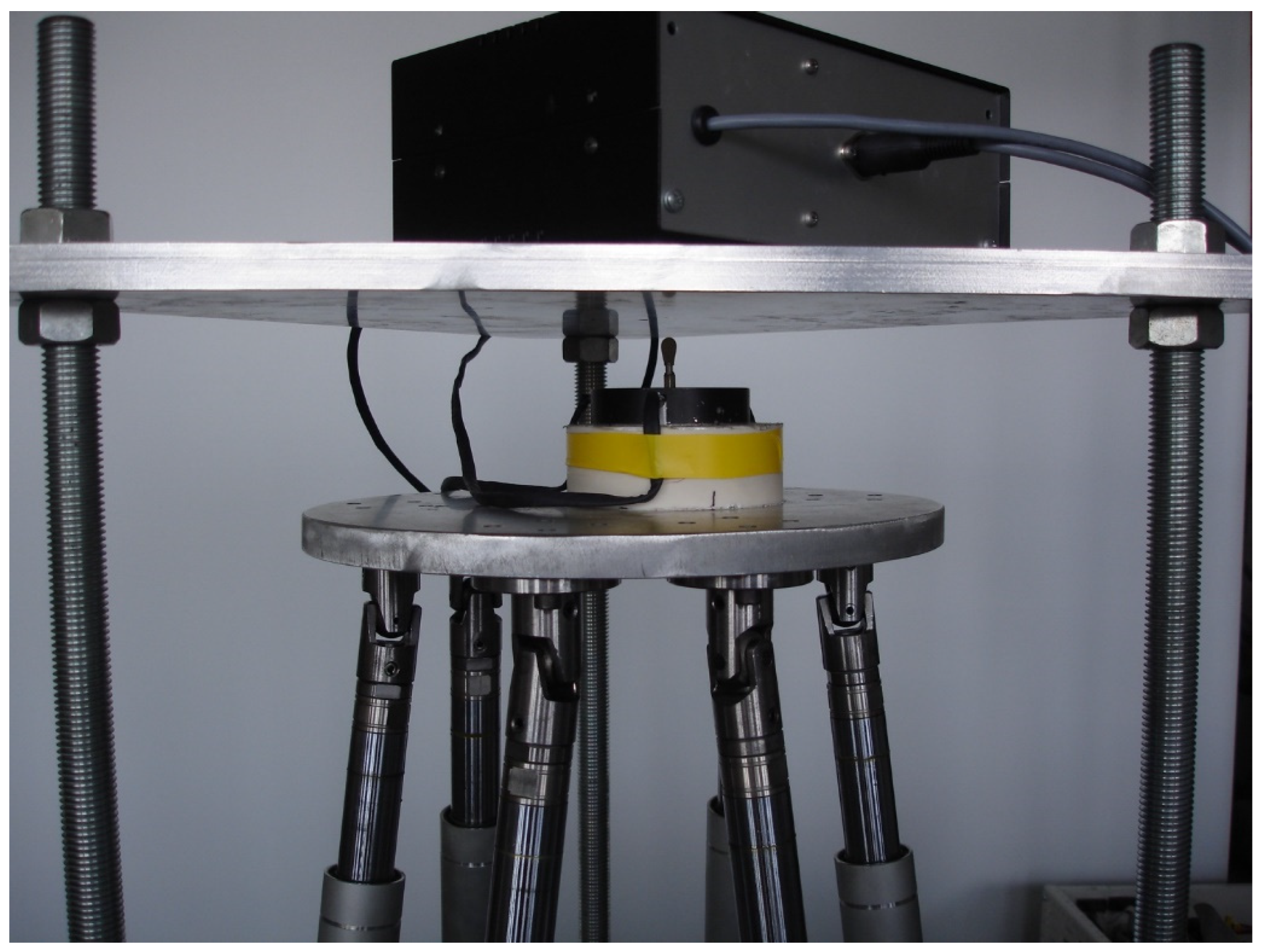
Table 1.
Resuming table of the properties of the materials tested.
| Material property | TRINIATM | Pekkton®ivory |
|---|---|---|
| Flexural Strength | 393 MPa | 200 MPa |
| Flexural Modulus of Elasticity | 18.8 GPa | 5.1 GPa |
| Tensile Strength | 169 MPa | 119 MPa |
| Compressive Strength | 339 MPa | 246 MPa |
| Rockwell Hardness (R-Scale) | 870 HV | 33 HV |
| Density | 1.68 g/cm3 | 1.4 g/cm3 |
| Fracture strength | 9.7 MPa m1/2 | 115 MPa |
| Water absorption | 0.03 % | 8.7 μg/mm3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated









