1. Introduction
The first 1000 days of life are a critical period for the foundation of children’s lifelong health, learning, and well-being [
1]. Malnutrition during those first 1000 days of life is a serious public health problem that can have devastating consequences for health, development, and productivity over the life course [
2]. Malnutrition can manifest in stunting, wasting, micronutrient deficiencies, overweight or underweight status. It can also result in impaired cognitive development and learning, leading to lower academic achievement and lower earning potential in adulthood.
Breast milk is perfectly tailored to infants’ nutritional needs, containing the right balance of proteins, fats, carbohydrates, vitamins, and minerals, along with antibodies and other immune factors that help protect babies from infection and disease [
3]. It presents little to no risk of foodborne illness when delivered directly through breastfeeding. Despite those advantages, many caregivers are unable to breastfeed their infants due to a range of reasons such as insufficient milk supply, latching difficulties, lack of support, lack of maternal leave or other employment incompatibility, breast surgery, maternal medications, or medical conditions such as viral or bacterial infections [
4]. According to the Centers for Disease Control and Prevention (CDC), in 2019, 83% of infants born within the United States started out receiving some breast milk [
5]. At the age of 6 months, however, only 56% of infants were receiving any breast milk, and only 25% were receiving breast milk exclusively [
5]. Infant formula offers a good option for mothers who are unable or unwilling to breastfeed, and it provides some advantages, such as convenience, flexibility, shared feeding responsibilities, and the ability to provide consistent nutrition whenever needed. About 16% of infants born in the United States in 2019 were exclusively formula fed at 6 months, while 46% were combination-fed—receiving both breast milk and formula—at 6 months [
5]. Beyond the U.S., 37% of children aged 6 months or under are exclusively breastfed in low- and middle-income countries; there is a large and growing market for infant formula worldwide [
6].
While infant formula can provide a safe and nutritious way to feed infants, drawbacks compared to breastfeeding can include higher cost, higher risk of infection, and lower immune protection [
7]. Caregivers could potentially introduce additional risks for their infants during the preparation of infant formula by not following the instructions carefully, using unsanitary methods, or making substantial errors in the concentration or dilution of the formula [
8]. Under-diluting infant formula can result in short-term health problems such as hypernatremic dehydration, gastroenteritis, and other digestive problems or long-term excessive weight gain and obesity [
9]. Over-diluting infant formula could also lead to serious health problems for babies, including, diarrhea, water intoxication, nutrient deficiencies (potentially manifesting as stunting, wasting, or underweight) and even death [
9,
10].
Previous studies have assessed the measurement accuracy of caregivers’ infant formula preparations in relation to bottle characteristics, package instructions, caregiver experience, and target amount [
11,
12,
13,
14,
15]. In a systematic review published in 2003 by Renfrew and colleagues [
9], all five included studies showed substantial problems achieving the proper concentration by formula-feeding caregivers, with a tendency toward over-concentration (under-dilution) of formula. A more recent laboratory study of caregivers and non-caregivers showed consistent over-dispensation of powdered formula across 2oz, 4oz, 6oz, and 8oz preparations that was equivalent to 11% excess calories per bottle (under-dilution) [
11]. Few studies, however, have separately investigated the variability of hand-scooping infant formula powder and pouring water: 1) For both caregivers and expert measurers; 2) For the caregiver’s own personal formula products and a standardized set of products; 3) In relation to a variety of demographic variables. The purpose of the present study was to determine to what degree accurate powder and water measurements are made in accordance with the formula manufacturer specifications by caregivers and an expert measurer when preparing infant formula for feeding under multiple conditions. The study also aimed to determine the influences on the variability in hand scooping and liquid measurement during the caregivers’ preparation of powdered infant formula.
2. Materials and Methods
2.1. Study Design and Setting
This study employed a cross-over experimental design, wherein each participant measured formula powder and water under multiple conditions. Separately, a trained research assistant expertly measured infant formula powder and water 30 times each, under multiple highly controlled conditions. The research was approved by Institutional Review Boards for data collection in two locations: The Physical Activity and Nutrition Clinical Research Consortium (PAN-CRC) within Lafene Health Center at Kansas State University; and The Behavioral Nutrition and Physical Activity laboratory at the University of Nevada, Las Vegas.
Participants were contacted and recruited through various means, mainly through university announcements, email, text, referral, and social media. Interested caregivers were screened for eligibility criteria, provided with a general study description, and given an opportunity to ask questions before scheduling their study appointments. Eligibility criteria required participants to be: at least 18 years old; a mother or caregiver who was currently formula feeding an infant; fluent in English or Spanish; and willing to attend a research appointment in person for about 30–45 minutes.
2.2. Participants
A total of 84 participants were included in this study, 17 from Kansas and 67 from Nevada. Caregiver characteristics are summarized in
Table 1. The mean age of the participants was 31.1 years (SD = 7.36), and the mean age of participants’ infants was 7.2 months (SD = 5.16). A large majority of participants (n = 71) identified themselves as the infant’s primary caregiver and 30 participants indicated that they were simultaneously breastfeeding and supplementing with infant formula. More than one-third of participants (n = 32) were enrolled in the Special Supplemental Nutrition Program Women, Infants, and Children (WIC). Regarding the duration of breastfeeding, 39 participants reported never having breastfed their infant or breastfeeding for less than 1 month, 27 participants had breastfed for 1 to 5 months, and 18 participants had breastfed for 6 months or more. About one-third of participants (n = 29) reported bottle-feeding their infants one to three times daily, while nearly two-thirds (n = 54 participants) fed their infants four times or more daily. Only 5 participants reported preparing 2 ounces or less per feeding, while half (n = 42) reported preparing 3 to 5 ounces per feeding, and the remaining participants (n = 35) reported preparing 6 ounces or more per feeding, or did not report the amount (n=2). The sample was racially diverse, with a small majority (n = 44) of participants reporting their race as White. The remainder reported being Black or African American (n = 7), American Indian or Alaska Native (n = 1), Asian (n = 4), Mixed/other Race (n = 27), or did not report (n = 2). A sizable minority (n = 39) reported Hispanic ethnicity. There was also ample educational and household income diversity among participants (See
Table 1).
2.3. Measures and procedures
2.3.1. Bottles and Formula
Participants were instructed to bring up to five of their own baby bottles with them to the laboratory, including an 8oz bottle. They were also asked to bring a container of their usual powdered baby formula, complete with a scoop and intact label. In situations where participants did not bring their personal formula preparation products (hereafter referred to as products), researchers provided extras for them to use (Similac Advance infant formula and Evenflo Feeding Classic Clear Plastic Baby Bottles). Research assistants observed and recorded details of participants' bottles and formula powder, noting relevant information such as size, style, number of grams per scoop for formula, color, material, and volume scale for bottles. They also gathered information about the types and brands of formula and bottles typically used, including whether those differed from the products they brought with them. All bottles were marked with an identification sticker and then weighed to the one-hundredth of a gram while empty and dry, without any nipple or collar, on a calibrated Bonvoisin Lab Scale 5000g x 0.01g high precision electronic analytical balance.
2.3.2. Demographic Questionnaire
Participants completed a demographic questionnaire, providing information about themselves that included age, socioeconomic status, infant birthday, household characteristics, breastfeeding duration, and the amount and frequency of bottle feeding. Summary data are presented in
Table 1.
2.3.3. Infant Formula Preparation and Measurement
Participants were first asked to describe their typical steps for preparing infant formula. Research assistants recorded notes about these preparation steps, including any additional preparation products that were mentioned. Scooping of infant formula powder and pouring of water was not performed until after participants described their typical steps. Next, participants were instructed to take their own bottles and powder formula, then follow their typical steps of scooping powder and pouring water. Hand sanitizer and a leveling utensil were available within participants’ reach. They were first asked to scoop infant formula powder as they normally would if they were preparing a 4oz bottle. Researchers took a picture of the first scoop of powder, just before it was added to the bottle (see
supplement for a selection of images). Next, participants were asked to scoop infant formula for preparation of a 7oz bottle. This odd size (7oz) was specifically chosen because older infants often consume more than 6 ounces during a feeding and caregivers sometimes must choose between discarding costly unused formula, keeping leftover formula at the risk of contamination, or having to prepare additional formula for an unsated baby. We hypothesized that more error would result from an odd-size feeding because most infant formula scoops each hold enough powder when full and leveled for 2oz of prepared formula. For both 4oz and 7oz preparation, the steps were carefully documented, including spillage details, whether the formula was leveled or packed, plus any relevant notes about the process.
After powder was scooped and added to the bottle for either a 4oz or 7oz feeding, research assistants obtained weights from the Bonvoisin Lab Scale, meticulously recording them on a data sheet. Later, the previously recorded bottle dry weight was subtracted from the total bottle and powder weight to obtain the mass of formula powder that was scooped and poured into the bottle. Because this study was conducted during a time where there were formula shortages, once finished weighing was completed, researchers asked permission from the participants to return the measured dry powder formula back to the participant’s container, to prevent wasting valuable formula.
After measuring the powder formula, participants were asked to pour water as if they were preparing for a feeding. Although some caregivers reported using hot or boiling water in their usual preparations, the basic process of adding water to a target volume in the bottle is uniform. So, we standardized the water measurements for convenience by making room-temperature water available in a pitcher for participants to pour. Participants were asked to pour water first for a 4oz feeding, and then for a 7oz feeding, simulating their usual practices. Research assistants obtained weights of poured water within bottles from the Bonvoisin Lab Scale, recording them on a data sheet and subtracting empty bottle weight as described above.
Once finished with scooping powder and pouring water for the 4oz and 7oz feeding by using their own products (formula powder and bottles), we repeated the entire measuring process after providing participants with a standardized set of products. Those products consisted of researcher bottles and infant formula powder (Love and Care Infant Formula Powder and a second set of Evenflo Feeding Classic Clear Plastic Baby Bottles). Participants were invited to familiarize themselves with the bottles and infant formula powder instructions if they felt it necessary to do so.
After completing the scooping and pouring tasks using both their own products and those of the researchers, participants completed the second portion of a questionnaire related to their usual baby feeding practices. Those data are intended for a separate investigation and are not relevant to the present study. Before participants finished their research appointment, they were invited to review an infant formula preparation best practices information sheet from the Centers for Disease Control and Prevention, or to watch a video presenting infant formula preparation best practices from WIC. While participants reviewed those best practices materials, research assistants checked the completeness of data from questionnaires and observations.
2.3.4. Gold Standards
The weights, in grams, that were listed on the package label for each type of infant formula powder (either brought in by the caregivers or provided by the researchers) served as the theoretical gold standard for comparison. For the Love and Care formula, the theoretical value was 8.8g per scoop to prepare 2oz of formula, so 17.6g for a 4oz feeding and 30.8g for a 7oz feeding. For water at room temperature, a theoretical value of 29.57 grams per 1oz served as the basis for the gold standard values of 118.29g for 4oz and 207.015g for 7oz [
16].
After extensive training and measurement protocol development—consistent with the formula preparation instructions from the manufacturer—research assistant measurements were also evaluated as a practical gold standard. Separate from the research participant appointments, the research assistant performed a series of powder and water measurements under varying highly controlled conditions, according to the standardized measurement protocol. All practical gold standard measurements used the Love and Care Infant Formula powder, Evenflo Feeding Classic Clear Plastic bottles, and the water pitcher to conduct these careful measurements. Both powder and water were carefully measured, weighed, and recorded 30 times each for the 4oz and 7oz preparations. The research assistant scooped from the canister and leveled powder within the scoop using a straight-edged utensil before carefully adding the powder to a standard previously weighed bottle. Two level scoops were added for the 4oz preparation and 3 scoops for the 7oz preparation. For the last half-scoop of powder needed to prepare a 7oz feeding (3.5 scoops), the research assistant used and leveled a separate half-size scoop. In addition to 30 separate measurements that aligned with manufacturer specifications, they also scooped and packed formula powder 30 times for both 4oz and 7oz feedings to create a compacted measurement because some caregivers have been observed compacting the formula within the scoop. Last, the research assistant poured room temperature water at eye level until the bottom of the meniscus was at 4oz and then at 7oz within a standard previously weighed bottle. Each of the 30 pouring measurements for both 4oz and 7oz was carefully weighed and recorded using the Bonvoisin Lab Scale. The mean of each set of 30 non-compacted measurements served as the practical gold standard.
2.4. Statistical Analysis
For each participant’s measurement of 4oz and 7oz preparations, the mean absolute percent error (MAPE) was calculated by dividing the participant measurement in grams by the theoretical gold standard, subtracting 1.0 and then multiplying the absolute value of the result by 100. Initial examination of the formula and water MAPE demonstrated significant rightward skew; thus, they were log-transformed for parametric procedures. MAPE was also calculated for each set of combined powder and water measurements for 4oz and 7oz preparations, reflective of what error would be for each bottle of prepared formula.
Separate linear mixed effects models, one for formula and one for water, were used to estimate the primary fixed effects of the targeted amount (4oz versus 7oz) and products used (caregiver’s own versus researchers’ standardized set) on mean absolute percent error (MAPE) of measurement. Additional fixed effects used as statistical control variables comprised current breastfeeding status (yes/no), frequency of bottle feeding per day (ordinal 1–3), amount of bottle feeding (ounce ranges, ordinal 1–4), primary caregiver status (yes/no), age of the infant (interval), and scoop type (half- or full-size, only used for models of formula powder MAPE) with random intercepts of participant.
A generalized linear mixed effects model with binomial link function was used to examine the primary fixed effects of targeted amount (4oz versus 7oz) and bottle type (participant versus researcher) on the odds of the combination of powder and water MAPE being >10% for each set of measurements. Similar to the models above, additional fixed effects that were used as statistical control variables comprised current breastfeeding status, frequency of bottle feeding per day, amount of bottle feeding, primary caregiver status, age of the infant, and scoop type, with random intercepts of participant.
All fixed effect coefficients, and their respective 95% confidence intervals, were back-transformed using exponentiation for better interpretability. This resulted in an estimated coefficient that represents the multiplicative factor for every one-unit increase in the independent variable. For example, a back-transformed coefficient equal to 1.2 represents that for every one-unit increase in our independent variable, there was an increase in the dependent variable by a factor of 1.2, or 20% more than the original value.
A linear mixed effects model with a primary fixed effect of substance was used to examine differences in MAPE between formula versus water. Again, additional fixed effects included as statistical control variables were current breastfeeding status, frequency of bottle feeding per day, amount of bottle feeding, primary caregiver status, age of the infant, and scoop type, with random intercepts of participant.
One-sample t-tests were used to compare the practical gold standard (trained research assistant measurement results) to the theoretical gold standard. Thus, this test was used to assess presence or absence of a significant deviation between what the research assistant could carefully measure and what the infant formula label indicated. The family-wise alpha level for multiple comparisons in this study was set at 0.05, ensuring a controlled overall type I error rate across the various statistical tests conducted.
3. Results
3.1. Descriptive Statistics
Across 84 participants and conditions, the infant formula powder MAPE was 9.03% (SD=11.84%). This indicates that on average, measurements differed from the theoretical gold standard—either over or under—by more than 9%. Across participants and conditions, the water MAPE was 4.45% (SD=8.80%), indicating a difference of more than 4% from the theoretical gold standard. The combined MAPE for measuring powder and water was 13.04% (SD=19.55%), which means that the prepared formula would have differed from the theoretical gold standard by more than 13%.
Because indicators of central tendency such as MAPE often do not convey the prevalence of substantial errors in measurement, the proportion of measurements that differed from the theoretical gold standard by 10% or more was tallied and also used in binomial link function analyses (see below). Across participants and conditions, approximately one-fourth of infant formula powder measurements (25.6%) and one-fifteenth of water measurements (6.5%) showed substantial error. More than three-tenths of the combined powder and water measurements showed substantial error (30.6%). Last, two-thirds of participants (66.7%) made at least one measurement error that was 10% or greater.
3.2. Effects of substance, targeted amount, and products used
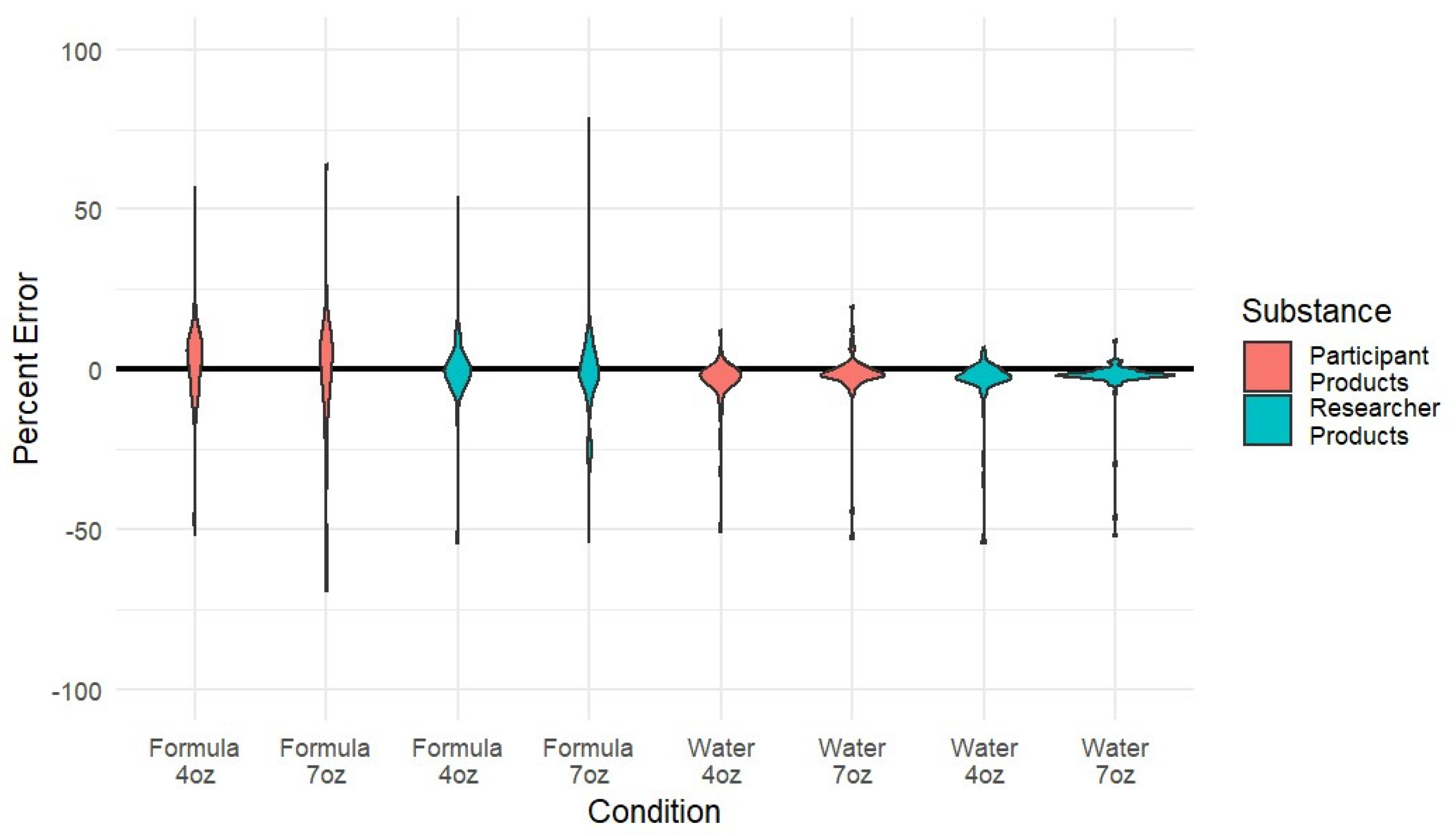
Figure 1 depicts variability in the MAPE of infant formula measurement by powder, water, size, and products used by participating caregivers. In linear mixed effects models that mutually adjusted for relevant caregiver characteristics (breastfeeding status, frequency of bottle feeding per day, amount of bottle feeding, primary caregiver status, age of the infant, and scoop type), significant differences in error were observed between measurements of infant formula powder and measurements of water (βWater =0.40, 95% CI=[0.33; 0.48],
p<0.001). This result indicates that—across the targeted amount and products used (caregiver’s own personal formula products or standardized set)—the participants’ measurements showed substantially less error for water, compared to infant formula powder.
Complete model results for powder MAPE can be viewed in table 2. In the linear mixed-effects models that mutually adjusted for relevant caregiver characteristics (breastfeeding status, frequency of bottle feeding per day, amount of bottle feeding, primary caregiver status, age of the infant, and scoop type), there was a significant effect of targeted amount (4oz vs 7 oz) on infant formula powder MAPE (β7ozP=1.36, 95% CI=[1.09; 1.69], p=0.006). This result indicates that powder MAPE during the preparation of a seven-ounce bottle was 36% higher than powder MAPE for the four-ounce bottle. In the linear mixed effects model, there was a significant effect of products used (caregiver’s own versus standardized set) on powder MAPE (βparticipantP=1.77, 95% CI=[1.43; 2.21], p<0.001). Specifically, there was 77% greater powder MAPE for the caregiver’s products, compared to the standardized set. There was no significant interaction of targeted amount by products used on powder MAPE, indicating that the error observed between infant formula powder targeted amount (4oz versus 7oz) did not vary by whose products were used.
Table 2.
Effects on mean average percent error of infant formula powder measurement.
Table 2.
Effects on mean average percent error of infant formula powder measurement.
| Variable Name |
MAPElog
estimate |
SE |
MAPE back-transformed
estimate |
DF |
t-value |
p-value |
| Intercept |
2.22 |
0.52 |
9.24 |
241 |
4.24 |
0.000 |
Caregiver’s own
products#
|
0.57 |
0.11 |
1.77 |
241 |
5.18 |
0.000 |
| Seven-ounce targeted amount1
|
0.31 |
0.11 |
1.36 |
241 |
2.79 |
0.006 |
| Currently breastfeeding2
|
-0.13 |
0.04 |
0.88 |
74 |
-3.43 |
0.001 |
Frequency of bottle
feeding3
|
-0.03 |
0.06 |
0.97 |
74 |
-0.61 |
0.547 |
| Amount of bottle feeding4
|
-0.33 |
0.14 |
0.72 |
74 |
-2.37 |
0.020 |
| Half-size scoop5
|
0.20 |
0.11 |
1.22 |
74 |
1.86 |
0.067 |
| Primary caregiver6
|
-0.01 |
0.24 |
0.99 |
74 |
-0.06 |
0.956 |
| Age of the infant7
|
-0.02 |
0.20 |
0.98 |
74 |
-0.11 |
0.913 |
Complete model results for water MAPE can be viewed in
Table 3. In the linear mixed-effects models that mutually adjusted for relevant caregiver characteristics, there was no significant effect of targeted amount on water MAPE (β7ozW=0.85, 95% CI=[0.66; 1.10],
p=0.22). Also, there was no significant effect of products used on water MAPE (βparticipantW = 0.89, 95% CI=[0.68; 1.15],
p= 0.36). There was no significant interaction of products used by targeted amount on water MAPE. This indicates that the level of error observed between products used did not vary due to water targeted amount (4oz versus 7oz).
3.3. Modeling large errors
As summarized in
Table 4, the binomial link function model was used to investigate effects on large errors (MAPE
> 10%) in the combined powder and water measurement. Results showed that when statistically controlling for other variables in the model (i.e., breastfeeding status, frequency of bottle feeding per day, amount of bottle feeding, primary caregiver status, age of the infant, and scoop type), there was a significant effect of products used (caregiver’s own versus standardized set) on the likelihood of large error (OR=4.23, 95% CI=[2.23; 8.04],
p<0.001). Specifically, participants were about four times more likely to measure amounts of formula powder and water that were at least 10% off target when using their own products, compared to the standardized set.
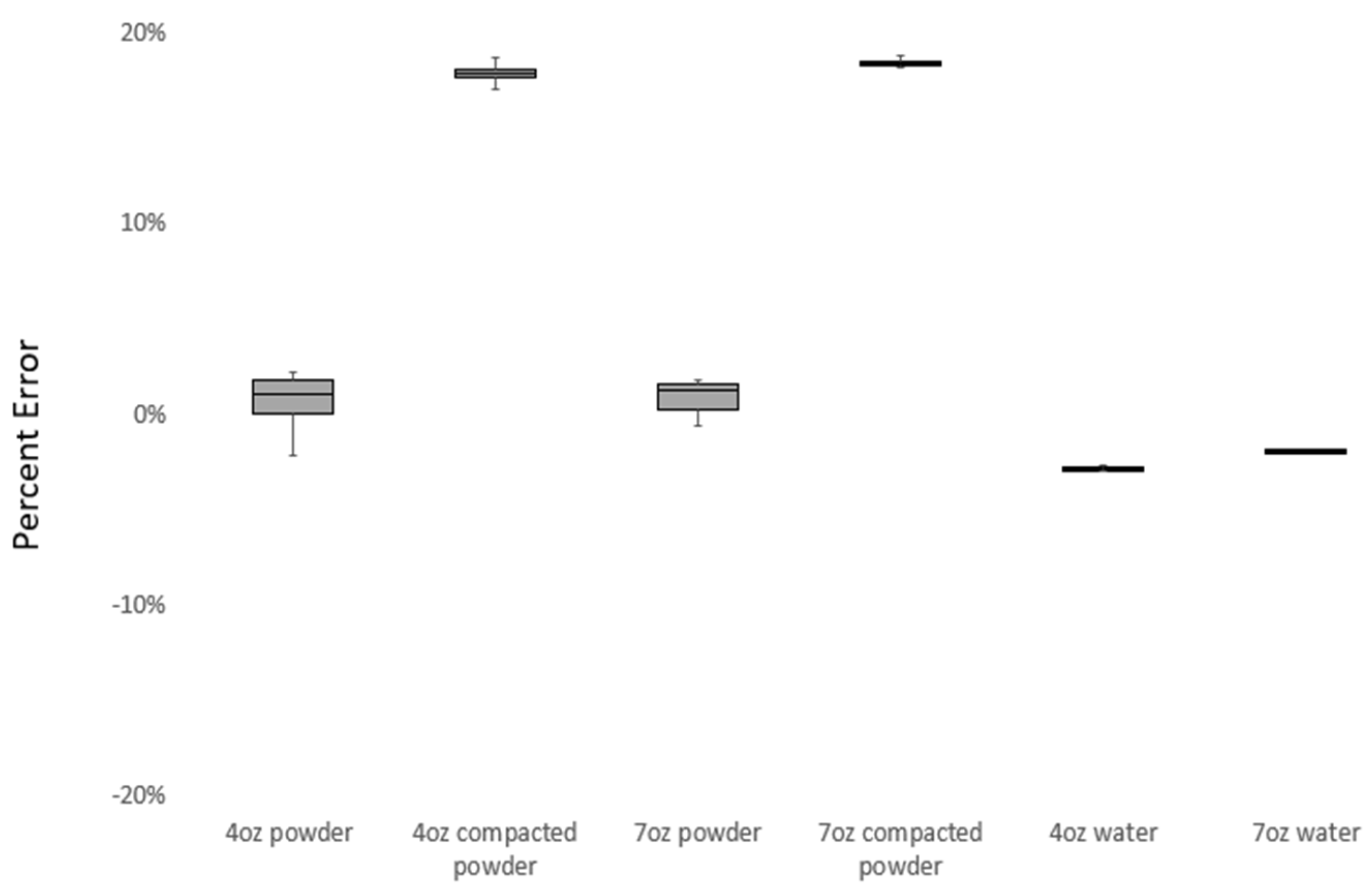
3.4. Practical gold standard error
Figure 2 displays the percentage of error in measurements performed by the trained research assistant under various conditions. Low percentage of error values were seen for the 4oz powder (1.05%), 7oz powder (1.27%), 4oz water (-2.70%) and 7oz water (-1.76%). In contrast, the 4oz compacted powder (17.87%) and 7oz compacted powder (18.39%) had the highest error measurements by the trained research assistant.
Table 5 presents comparisons between the theoretical gold standard (values expected from infant formula label) and the practical gold standard (measurement values obtained by the trained research assistant). For all conditions, the practical gold standard significantly differed from the theoretical gold standard (
p<0.001).
4. Discussion
Our study sought to determine to what degree accurate measurements are made in accordance with the formula manufacturer specifications mainly by caregivers—but also by expert measurers—when they prepare infant formula for feeding under multiple conditions. Although there was error both when participants hand-scooped infant formula and added it to their bottles (9%) and when participants poured water into bottles (4.4%), the largest magnitude of error was from the combined powder and water preparations (13%). There was wide variability in where participants made errors. Some participants were consistently higher or lower than the gold standard for both powder and water, which effectively would minimize the error for the combination. The general tendency, however, was for participants to over-dispense powdered formula and to under-pour water. This tendency exacerbated each of the individual component errors to result in a formula that was an average of 13% more concentrated than it should have been, surpassing the individual error contributions from powder or water alone. Put into caloric terms, a 13% error would add approximately 10kcals to each 4oz feeding or 18kcals to each 7oz feeding. Since most participants were feeding their infants four times or more times daily, many infants could be receiving substantial amounts of excess energy each day.
Photographs and observations that were made during this study revealed that many caregivers: failed to level a heaping scoop carefully; sometimes failed to fill the scoop; and often spilled some powder while adding powder to the bottle. Occasionally, caregivers compacted the formula by scooping powder into the side of the can. In a few cases, caregivers seemed to lose track of the number of scoops and either missed one or added an extra scoop of powdered formula. In contrast, the expert measurements made by the trained research assistant achieved a closer approximation of the target and theoretical gold standard, but still showed significant differences from the intended values that would result in under-diluted or over-concentrated formula.
Renfrew and colleagues [
9] described a general tendency in the scientific literature for under-dilution or over-concentration of formula. The present study supported that general tendency within the literature while investigating specific drivers of variability. Our results showed that the contribution of error from formula powder measurement was approximately twice the magnitude of error from water measurement. Given the complexity of the task of scooping powder from a can without compacting the powder, leveling the scooped powder, and then transferring it from the scoop into the bottle, there are multiple places where errors may accumulate. The present study was not equipped to investigate the individual contributions of each separate stage of powder measurement (scooping, leveling, transferring), but future studies should determine which of them contributes most to the total error. For the combined error of powder and water, we found an average of approximately13% under-dilution (over-concentration) in the present study, which is slightly higher than that reported by Altazan and colleagues [
11]. Notably, that 11% was seen in a study of both caregivers and non-caregivers, while our sample of all caregivers did no better, without any difference between primary caregivers and non-primary caregivers. Thus, being a primary caregiver does not appear to confer any particular advantage to infant formula measurement accuracy.
Contrary to what may have been expected, demographic variables were generally not significantly explanatory of error in measurements. There was some evidence that those who were currently breastfeeding and those feeding larger amounts made smaller errors during the measurement of formula powder, but those factors were not significant for water, nor for large errors in the combination of powder and water. Furthermore, frequency of bottle feeding, scoop size, and age of infant were not significant; neither were education nor income (data not shown). Overall, it appeared that error was not connected to any particular demographic, but was quite widespread across the sample. Indeed, one-quarter of the sample measurements had 10% or greater error for formula powder, almost one-third had >10% error for the combination of powder and water, and two-thirds of participants made at least one large error of >10% in their powder and/or water measurements.
The present study advances the current body of evidence, showing a substantial difference in error from formula powder measurement versus error from water measurement, and how the divergent directions of those errors combined to exacerbate under-dilution. Ostensibly, water measurement poses a less complex measurement problem, although extant literature has identified how even health professionals can have difficulty with liquid measurement accuracy [
17]. Furthermore, baby bottle manufacturers may contribute to measurement difficulties with difficult-to-read markings, irregularly shaped bottles, or inaccurate markings on the bottle contributing to barriers to preparing appropriate concentrations of infant formula [
14].
The most unexpected finding in the present study was that the caregivers made larger errors with their own products, as compared to with the standard researcher set that was provided. That is, caregivers made greater errors in powder measurement and were more likely to make substantial error (
>10%) in both preparation of powder and water when they were asked to prepare formula with their own powders, scoops, and bottles versus a presumably unfamiliar set of products. It is unclear why this occurred but it is unlikely due to an order effect as the order in which caregivers used each set of products was variable during their visit. One potential explanation may come from habit theory and dual process theory [
18]. According to those theories, frequently repeated actions may become automatic, rather than requiring focused attention and conscious deliberation. When caregivers used their own products in the preparation of formula, they may have been operating according to well-established habitual action patterns. When asked to use unfamiliar infant formulas, scoops, and bottles, caregivers may have moved from system 1 to system 2 thinking, bringing conscious awareness, deliberation, and a focused attention to the task of measuring accurately under those conditions. Related research has shown how the absence of attentional focus through maternal distraction can contribute to feeding problems [
19]. Although large errors were prevalent for the condition where caregivers were confronted with unfamiliar products, it was significantly less error-prone than when using their own familiar products.
The present study is limited in terms of a modest sample size and a short-term investigation of error during the measurement of formula powder and water. It is possible that the findings from this sample do not generalize to the wider population despite the diversity of participants and concordance with extant literature. The study is also limited in ecological validity in that participants were asked to come to a laboratory at a university, and that setting may be very different from where they usually prepare infant formula. Such differences could contribute to greater errors than normal. In contrast, participants who are being observed within a research study are often subject to the Hawthorne effect or demand characteristics that may have them acting more carefully or productively than if not being observed. Strengths of this study included the rigorous study protocol, multiple careful measurements made on a precision scale, investigation of many putative drivers of error, and the diversity of the sample.
5. Conclusions
In this study, participating caregivers demonstrated considerable variability and substantial error during infant formula preparation, particularly for hand-scooping of powder, which tended toward higher values than the theoretical gold standard. Greater measurement error was associated with the odd-sized 7oz preparation and—unexpectedly—with the participants’ own products. In combination, errors from powder and water often compounded, generally toward under-dilution of formula. Thus, this study’s results reveal that many caregivers could benefit from interventions to improve formula-feeding practices, with the eventual beneficiary being the infants under their care.
Caregivers were not uniquely error-prone in this study, as even trained research assistants in highly controlled conditions made significant and potentially meaningful errors in measuring powder and water. Their careful measurements of compacted powder also demonstrated one way that formula can be systematically under-diluted. For the non-compacted measurement conditions, the practical gold standard values that were achieved by research assistants may estimate the best-case scenario for what is possible among caregivers. It is unlikely that caregivers could achieve such a consistently lower level of error without additional technological tools, such as the implementation of a high precision scale during preparation. Clearly, the current tools provided in the form of powder formula, scoop, and bottles contribute to measurements being made that are rife with error. Additional factors, such as familiarity with the formula preparation products, may exacerbate those errors.
As much of the world begins to develop economically, this may lead to an increased reliance on formula feeding on a global level as there is a clear relationship between national income and breastfeeding [
6]. Thus, there is greater urgency to solve this problem as the proportion of infants globally that may be formula fed in the future may increase substantially. Future research on systematic error-reduction interventions is needed for what appears to be a persistent and widespread problem documented in the literature, particularly given that the problem of formula mis-measurement and under-dilution has potentially profound consequences for population health.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org, Figure S1: Figure S1: Visual images portraying the variability in hand scooping of powdered formula.
Author Contributions
Conceptualization was led by R.R. with input from A.G.A and S.R. Methodology was led by R.R. and S.R. Formal analysis was led by A.H. and R.R. Writing—original draft preparation was done by R.R. Writing—review and editing were conducted by A.G.A., S.R., A.H., C.B.P., C.A., and J.R.H. Supervision and project administration was provided by R.R. Data collection was performed by A.G.A., C.A., C.B.P., and J.R.H. Funding acquisition was led by R.R. All authors have read and agreed to the published version of the manuscript. All authors have contributed substantially to the work reported.
Funding
This research was funded by The Betesh Group. The APC was funded by The Betesh Group. The authors had full independence to design and conduct the study without interference or restriction regarding the publication of findings.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of University of Nevada, Las Vegas (#UNLV-2022-464, November 2022) and by the Institutional Review Board of Kansas State University (IRB-11215, June 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data supporting reported results can be shared. Interested parties should contact the author.
Acknowledgments
We would like to thank Nokwanda Hlophe, Fiza Maqsood, and Dawn Matusz for their contributions to data collection.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role: in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Karakochuk, C.D.; Whitfield, K.C.; Green, T.J.; Kraemer, K. The biology of the first 1,000 days. Taylor & Francis; 2018. [CrossRef]
- Schwarzenberg, S.J.; Georgieff, M.K.; Daniels, S.; Corkins, M.; Golden, N.H.; Kim, J.H.; Lindsey, C.; Magge, S.N. Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. 2018, 141(2). [CrossRef]
- Andreas, N.J.; Kampmann, B.; Le-Doare, K.M.; Human breast milk: A review on its composition and bioactivity. Early Hum Dev. 2015, 91(11), 629-35. [CrossRef]
- Odom, E.C.; Li, R.; Scanlon, K.S.; Perrine, C.G.; Grummer-Strawn, L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics. 2013, 131(3), e726-32. [CrossRef]
- Rupnicki, S. Breastfeeding Report Card United States, 2020. CDC: Atlanta, GA, USA. 2020.
- Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016, 387, 475-90. [CrossRef]
- McNiel, M.E.; Labbok, M.H.; Abrahams, S.W. What are the risks associated with formula feeding? A re-analysis and review. Birth. 2010, 37(1), 50-8. [CrossRef]
- Gibson, S.; Sahanggamu, D.; Fatmaningrum, D.; Curtis, V.; White, S. ‘Unfit for human consumption’: a study of the contamination of formula milk fed to young children in East Java, Indonesia. Trop Med Int Health. 2017, 22(10), 1275-82. [CrossRef]
- Renfrew, M.J.; Ansell, P.; Macleod, K.L. Formula feed preparation: helping reduce the risks; a systematic review. Arch Dis Child. 2003, 88(10), 855-8. [CrossRef]
- Fein, S.B.; Falci, C.D. Infant formula preparation, handling, and related practices in the United States. J Am Diet Assoc. 1999, 99(10), 1234-40. [CrossRef]
- Altazan, A.D.; Gilmore, L.A.; Guo, J.; Rosenberg, D.M.; Toupo, D.; Gowins, A.; Burton, J.H.; Beyl, R.A.; Chow, C.C.; Hall, K.D.; Redman, L.M. Unintentional error in formula preparation and its simulated impact on infant weight and adiposity. Pediatr Obes. 2019, 14(12), e12564. 12. [CrossRef]
- Ventura, A.K.; Golen, R.P. A pilot study comparing opaque, weighted bottles with conventional, clear bottles for infant feeding. Appetite. 2015, 85, 178-84. [CrossRef]
- Ventura, A.K.; Hernandez, A. Effects of opaque, weighted bottles on maternal sensitivity and infant intake. Matern Child Nutr. 2019, 15(2), e12737. 2. [CrossRef]
- Gribble, K.; Berry, N.; Kerac, M.; Challinor, M. Volume marker inaccuracies: A cross-sectional survey of infant feeding bottles. Matern Child Nutr. 2017, 13(3), e12388. 3. [CrossRef]
- Gilmore, L.A.; Altazan, A.D.; Flanagan, E.W.; Beyer, A.G.; Olson, K.N.; O’Connell, A.A.; Nguyen, T.H.; Beyl, R.A.; Redman, L.M. Modifications to infant formula instructions improve the accuracy of formula dispensing. Nutrients. 2020, 12(4), 1150. [CrossRef]
- Calculate weight of compounds and materials per volume. Available online: https://www.aqua-calc.com/calculate/volume-to-weight (accessed on 13 January 2024).
- Evans, S.; Ashmore, C.; Daly, A.; MacDonald, A. Accuracy of formula preparation equipment for liquid measurement. Mol Genet Metab Rep. 2014, 1, 141-7. [CrossRef]
- Wood, W.; Labrecque, J.S.; Lin, P.Y.; Rünger, D. Habits in dual process models. In Dual process theories of the social mind. United States, 2014, 1, 371-85.
- Golen, R.B.; Ventura, A.K. Mindless feeding: Is maternal distraction during bottle-feeding associated with overfeeding?. Appetite. 2015, 91, 385-92. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).