Submitted:
25 January 2024
Posted:
25 January 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
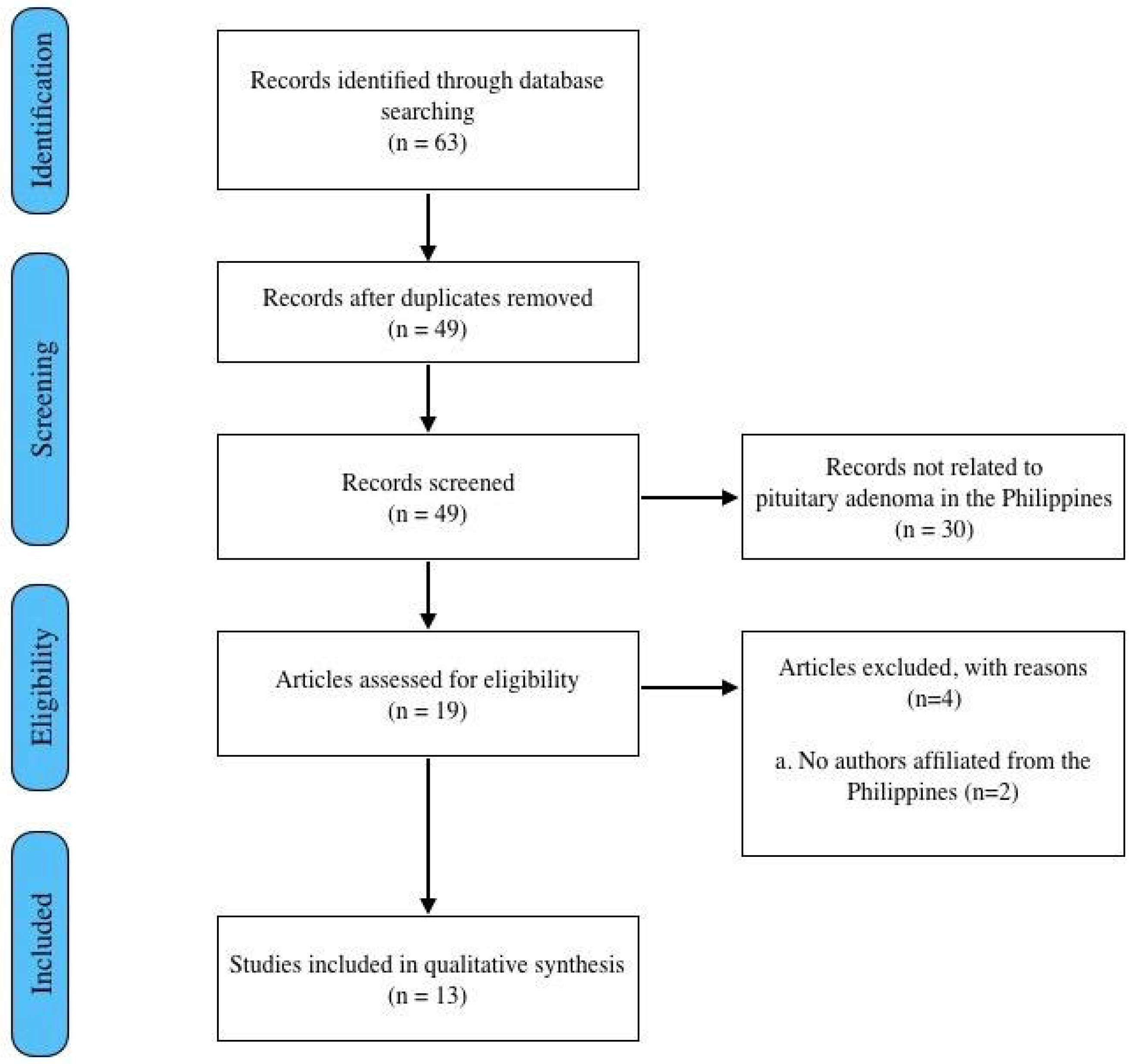
2. Materials and Methods
Protocol
Eligibility Criteria
Information/Data sources
Search and selection of sources
Charting of data and synthesis of results
3. Results
3.1. Search of studies
3.2. Epidemiology of Pituitary Adenoma in the Philippines
3.3. Local Research in Pituitary Adenoma
3.4. The Healthcare System of the Philippines
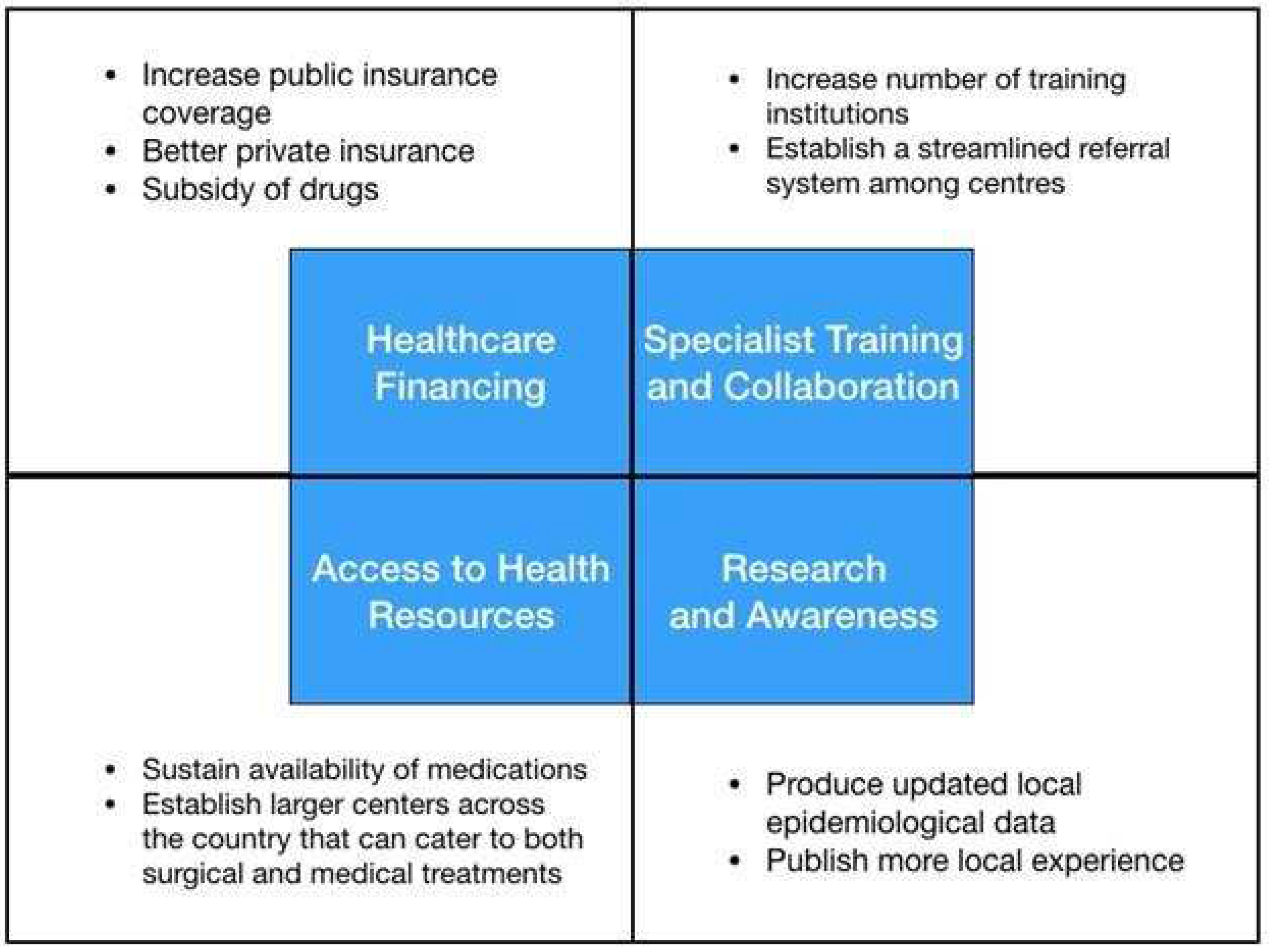
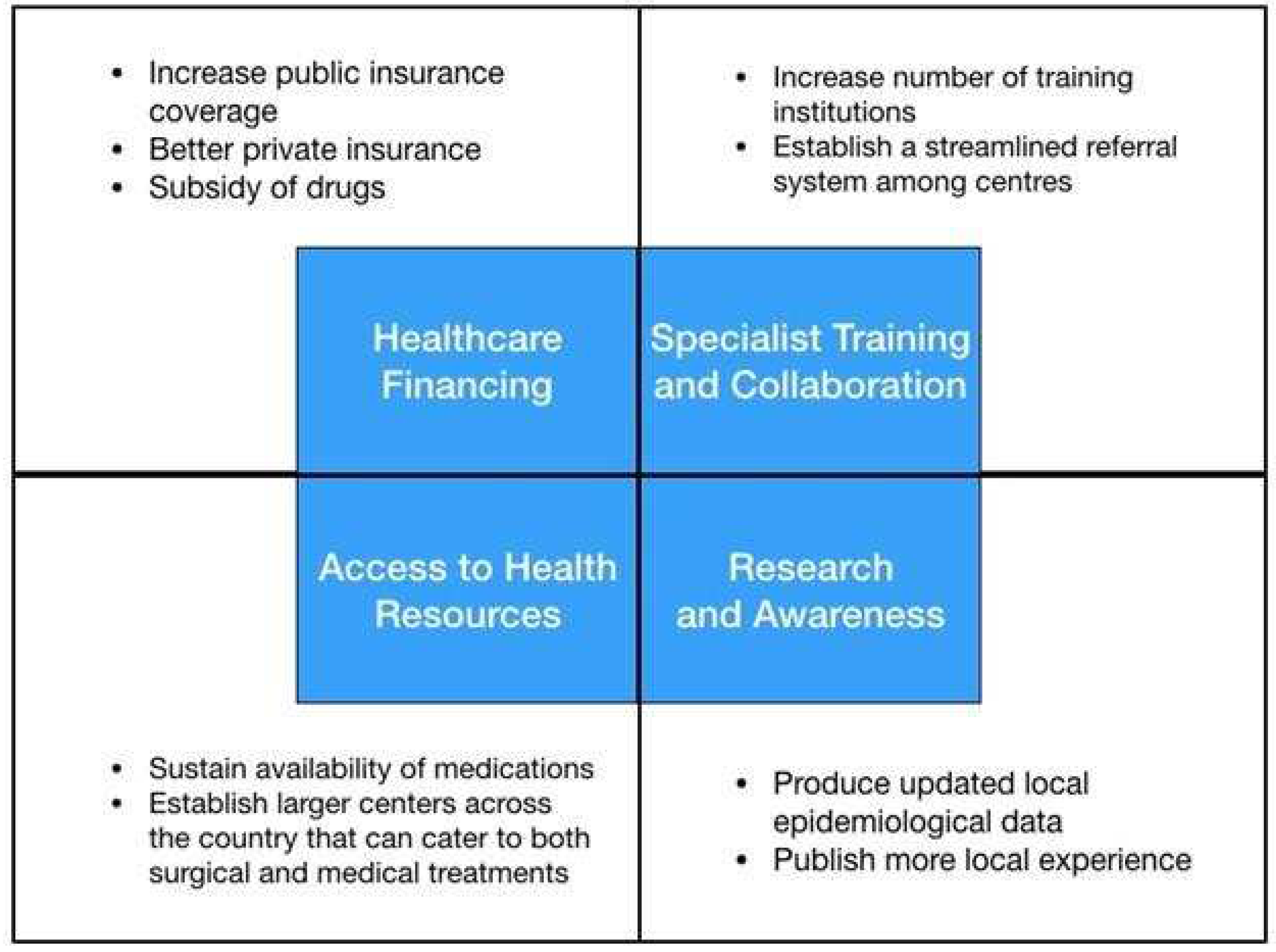
3.4. Healthcare Financing and Coverage in the Philippines
3.5. Specialist Training and Medical Education
3.6. Challenges on Diagnostics
3.6. Challenges on Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix
| Author | Age/ Sex |
Type of adenoma | Clinical Presentation | Imaging findings | Hormonal Profile | Surgical Treatment | Medical Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Bunoy et al., 2012 (4) | 38/M | Macro- adenoma |
Seizures, frontal headache, blurring of vision (bitemporal hemianopsia) | 4.0 x 5.0 x 4.5 cm sellar-suprasellar mass | Low cortisol, high TSH, normal ACTH | Cranioto- my with excision of the tumor |
Methima- zole, prednisone |
Improved |
| Mendo-za et al., 2015 (32) | 46/F | Macro- adenoma |
Amenorrhea, acromegaly | 2.1 x 3.3 x 2.4 cm sellar-suprasellar mass with foci of intratumoral hemorrhages suggestive of subclinical pituitary apoplexy | High GH, high prolactin | None | Cabergo- line 0.5 mg tablet once a week |
Improved |
| Tating et al., 2016 (30) | 13/M | Micro- adenoma |
Bilateral lower extremity weakness, hypertension | 0.8 x 0.9 x 0.8 cm anterior pituitary gland mass | High ACTH, high cortisol | Transphenoid-al adenomectom-y was indicated but deferred because dexamethasone suppression test revealed high serum cortisol and 24-hr free urine cortisol | None | Expired |
| Sandoval et al., 2020 (31) | 37/F | Macro- adenoma |
Amenorrhea, progressive weight gain, facial roundness, leg weakness, easy bruisability, blurring of vison (bitemporal hemianopsia), hyperpigmented fingernails | 4.6 x 4.1 x 7 cm lobulated, heterogeneously enhancing sellar-suprasellar mass with cystic and necrotic components | High ACTH | Transphenoid-al excision | None | Improved |
| Jordan et al., 2022 (39) | 40/F | Giant adenoma | Acromegaly, headache, blurring of vision (bitemporal hemianopsia) | 6.4 x 7.0 x 5.5 cm lobulated pituitary mass with cystic degeneration and necrosis | High GH, high IGF-1 | Surgical resection via transcranial approach | Bromocrip-tine, radiotherapy | Improved |
| Author | Title | Journal | Institution | Publication Year | Study Design |
|---|---|---|---|---|---|
| Villegas et al. (9) | A review of patients with pituitary tumors at St. Luke’s Medical Center from January 1997 to September 2000 | Philippine Journal of Internal Medicine | St. Luke’s Medical Center | 2002 | Retrospective study |
| Alinsonorin et al. (2) | Pituitary adenoma: clinical profile of 120 patients at the Philippine General Hospital | Philippine Journal of Internal Medicine | Philippine General Hospital | 2003 | Retrospective, descriptive |
| Fonte et al. (41) | Treatment outcomes of pituitary tumors at the University of Santo Tomas Hospital: 2004-2008 | Philippine Journal of Internal Medicine | University of Santo Tomas Hospital |
2009 | Retrospective cohort |
| Bunoy et al. (4) | Inappropriate secretion of thyroid stimulating hormone in a Filipino patient with a pituitary macroadenoma | Journal of ASEAN Federation of Endocrine Societies | St. Luke’s Medical Center | 2012 | Case report |
| Lo et al. (10) | Endogenous Cushing’s syndrome: the Philippine General Hospital experience | Journal of ASEAN Federation of Endocrine Societies | Philippine General Hospital | 2014 | Cross-sectional |
| Jordan et al. (39) | The sleeping giant: an atypical case of a giant pituitary adenoma presenting as acromegaly with minimal symptoms of mass effect | Journal of ASEAN Federation of Endocrine Societies | St. Luke’s Medical Center | 2014 | Case report |
| Mendoza et al. (32) | Acromegaly with cardiomegaly, cardiac thrombus and hemorrhagic cerebral infarct: a case report of therapeutic dilemma with review of literature | International Journal of Endocrinology and Metabolism | University of Santo Tomas Hospital |
2015 | Case report |
| Tating et al. (30) | Cushing’s syndrome from pituitary microadenoma and pulmonary nodules | Oncology Nursing Forum | Philippine General Hospital | 2016 | Case report |
| Faltado et al. (6) | Factors associated with postoperative diabetes insipidus after pituitary surgery | International Journal of Endocrinology and Metabolism | Philippine General Hospital | 2017 | Retrospective cohort |
| Carampatana-Jandug et al. (38) | In-hospital postoperative complications in patients with pituitary adenoma who underwent pituitary surgery from January 2010 to December 2015: a multicenter study | International Journal of Endocrinology and Metabolism | Chong Hua Hospital | 2017 | Retrospective cohort |
| Cudal et al. (37) | Postoperative complications of trans-sphenoidal surgery in a local tertiary hospital during hospital stay | Philippine Journal of Internal Medicine | Makati Medical Center | 2018 | Retrospective cross- sectional |
| Sandoval et al. (31) | Nail hyperpigmentation in ACTH-secreting pituitary adenoma (Cushing’s disease) and its resolution after successful trans-sphenoidal excision | BMJ Case Reports | Philippine General Hospital | 2020 | Case report |
| Seng et al. (3) | Extracapsular resection of pituitary adenomas: a systemic review | Asian Journal of Neurosurgery | Philippine General Hospital | 2023 | Systematic review |
| Laboratory Test/ Imaging | Cost Government- subsidized (USD) |
Cost No government no subsidy (USD) |
Cost Private (USD) |
|---|---|---|---|
| IGF-1 | NA | NA | 175.00 |
| ACTH | NA | NA | 136.90 |
| Cortisol | NA | NA | 52.80 |
| Prolactin | 5.80 | 8.50 | 9.10-31.20 |
| FSH | 6.10 | 9.70 | 11.50-24.20 |
| LH | 9.20 | 12.40 | 13.00-24.20 |
| Estradiol | 6.90 | 10.60 | 11.10-46.80 |
| Testosterone | 15.30 | 32.20 | 33.80-46.80 |
| TSH | 6.10 | 10.50 | 12.10-14.40 |
| FT3 | 8.30 | 12.90 | 13.60-49.90 |
| FT4 | 6.40 | 10.00 | 10.50-49.90 |
| Cranial MRI with contrast | 153.70 | 179.30 | 190.00-210.90 |
| Cranial MRI - plain | 75.60 | 91.30 | 96.60-107.30 |
| Cranial CT scan with contrast | 86.30 | 98.10 | 103.00-112.80 |
| Cranial CT scan - plain | 26.30 | 54.40 | 65.30-73.50 |
References
- Daly, A.F.; Beckers, A. The epidemiology of pituitary adenomas. Endocrinol Metab Clin North Am. 2020, 49, 347–55. [Google Scholar] [CrossRef]
- Alinsonorin, D.; Santos-Batongbacal, M.; Paz-Pacheco, E.; Trajano-Acampado, L. Pituitary adenoma: clinical profile of 120 patients at the Philippine General Hospital. Philipp J Int Med. 2003, 41, 323–29. [Google Scholar]
- Seng, K.S.; Malilay, O.R.M. Extracapsular resection of pituitary adenomas: a systematic review. Asian J Neurosurg. 2023, 18, 5–11. [Google Scholar] [CrossRef]
- Bunoy, L.S.; Co, J.M.I.O. Inappropriate secretion of thyroid stimulating hormone in a Filipino patient with a pituitary macroadenoma. J ASEAN Fed Endocr Soc. 2012, 27(1), 114–8. [Google Scholar] [CrossRef]
- Chavez, S.; Tan, C. Pituitary macroadenoma presenting as a synchronous occurrence of acromegaly and cushing’s disease. Rev Argent Endocrinol Metab. 2021, 58, 226. [Google Scholar]
- Faltado, A.L.; Macalalad-Josue, A.A.; Li, R.J.S.; Quisumbing, J.P.M.; Yu, M.G.Y.; Jimeno, C.A. Factors associated with postoperative diabetes insipidus after pituitary surgery. Endocrinol Metab. 2017, 32, 426. [Google Scholar] [CrossRef]
- Biermasz, N.R. The burden of disease for pituitary patients. Best Pract Res Clin Endocrinol Metab. 2019, 33, 101309. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and xxplanation. Ann Intern Med. 2018, 169, 467–73. [Google Scholar] [CrossRef] [PubMed]
- Villegas, M.; Quinto, G.; Quimpo, J. A Review of patients with pituitary tumors at St. Luke’s Medical Center from January 1997 to September 2000. Philipp J Intern Med. 2002, 40, 40–3. [Google Scholar]
- Lo, T.E.; Cabradilla, J.M.; Lim, S.A.; Jimeno, C.A. Endogenous Cushing’s syndrome: the Philippine General Hospital experience. J Solid Tumors. 2013, 4, 1–10. [Google Scholar]
- Dayrit, M.M.; Lagrada, L.P.; Picazo, O.F.; Pons, M.C.; Villaverde, M.C. The Philippines Health System Review; World Health Organization: New Delhi, India, 2018; Vol 8, No. 2; pp. 1–12. [Google Scholar]
- Pagaling, G.T.; Turalde, C.W.R.; Jamora, R.D.G. Autoimmune encephalitis in the Philippines: a scoping review on the treatment gaps, challenges, and current state of care. Front Neurol. 2022, 13, 788309. [Google Scholar] [CrossRef]
- Health expenses remain a big burden for Pinoys despite UHC. Philippines: Philippine Institute for Developmental Studies. Available online: https://www.pids.gov.ph/details/news/in-the-news/health-expenses-remain-a-big-burden-for-pinoys-despite-uhc# (accessed on 12 August 2023).
- World Health Organization Global health expenditure database. Available online: https://apps.who.int/nha/database/country_profile/Index/en (accessed on 18 August 2023).
- Philippine Health Insurance Corporation List of Medical Case Rates. Available online: https://www.philhealth.gov.ph/circulars/2017/annexes/0019/AnnexA-MedicalCaseRates (accessed on 12 August 2023).
- Official Gazette of the Republic of the Philippines Republic Act No. 11463. Available online: https://www.officialgazette.gov.ph/2019/12/03/republic-act-no-11463/ (accessed on 12 August 2023).
- Let’s Save The Brain. Available online: https://letssavethebrain.org/about-us/ (accessed on 16 August 2023).
- Philippine Cancer Resources Cancer Index. Available online: http://www.cancerindex.org/Philippines (accessed on 15 December 2023).
- Sagip Buhay Medical Foundation, Inc. UP-PGH Department of Medicine. Available online: https://uppghmedicine.com.ph/services/sagip/ (accessed on 15 December 2023).
- Russ, S.; Shafiq, I. Pituitary adenoma; StatPearls Publishing [Internet]: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554451/ (accessed on 22 August 2023).
- Tan, G.H. Diabetes care in the Philippines. Ann Glob Health. 2016, 81, 863. [Google Scholar] [CrossRef]
- World Health Organization The Global Health Observatory. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/medical-doctors-(per-10-000-population) (accessed on 15 December 2023).
- Mondia, M.W.L.; Espiritu, A.I.; Batara, J.M.F.; Jamora, R.D.G. Neuro-oncology in the Philippines: a scoping review on the state of medical practice, deterrents to care and therapeutic gaps. Ecancermedicalscience. 2021, 15, 1238. [Google Scholar] [CrossRef]
- Ignacio, K.H.D.; Espiritu, A.I.; Jamora, R.D.G. The current status and challenges in multiple sclerosis management in the Philippines. Mult Scler Relat Dis. 2020, 46, 102510. [Google Scholar] [CrossRef]
- PNA Fellows Philippine Neurological Association. Available online: https://www.philippineneurologicalassociation.com/pna-fellows (accessed on 15 December 2023).
- Academy of Filipino Neurosurgeons, Inc. Members. Available online: https://www.afninc.org/members-2/ (accessed on 26 October 2023).
- Training Institutions Philippine College of Endocrinology Diabetes and Metabolism. Available online: https://endo-society.org.ph/training-institutions/ (accessed on 5 December 2023).
- Division for Human Health: DIRAC (Directory of Radiotherapy Centres). Available online: https://dirac.iaea.org/Query/Countries (accessed on 5 December 2023).
- Facilities of Philippine Radiation Oncology Society. Available online: https://pros.org.ph/facilities/ (accessed on 5 December 2023).
- Tating, D.L.R.P.; Montevirgen, N.D.S.; Cajucom, L. Cushing’s syndrome from pituitary microadenoma and pulmonary nodules. Oncol Nurs Forum. 2016, 43, 136–40. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, M.A.S.; Bruno, R.G. Nail hyperpigmentation in ACTH-secreting pituitary adenoma (Cushing’s disease) and its resolution after successful trans-sphenoidal excision. BMJ Case Rep. 2020, 13, e234905. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, E.; Malong, C.L.; Tanchee-Ngo, M.J.; Mercado-Asis, L. Acromegaly with cardiomyopathy, cardiac thrombus and hemorrhagic cerebral infarct: a case report of therapeutic dilemma with review of literature. Int J Endocrinol Metab. 2015, 13, e18841. [Google Scholar] [CrossRef] [PubMed]
- Laboratory test prices. Available online: https://www.nwdi.com.ph/prices (accessed on 5 August 2023).
- Cudal, B.; Montano, C.; Pontillas, A.; Baraoidan, R. Post-operative complications of trans-sphenoidal surgery in a local tertiary hospital during hospital stay. Philipp J Int Med. 2018, 56(1), 15–8. [Google Scholar]
- Carampatana-Jandug, C.; Esguerra, J.M.; Panilagao, G.; Mejia, A.; Rama, J.; Bilocura, F.E. In-hospital postoperative complications in patients with pituitary adenoma who underwent pituitary surgery from January 2010 to December 2015: a multicenter study. J Endocr Metab. 2017, 7(4), 122–30. [Google Scholar] [CrossRef]
- Jordan, C.; Carmen, C.C.; Esposo, E.; Rosales, R.; Maravilla, R.D. The sleeping giant: an atypical case of a giant pituitary adenoma presenting as acromegaly with minimal symptoms of mass effect. J ASEAN Fed Endoc Soc. 2019, 34, 76. [Google Scholar]
- Te, J.; Pacia, E. Neuronavigation vs traditional C-arm fluoroscopy in transsphenoidal surgery for the excision of pituitary macroadenomas: a comparative study from the University of Santo Tomas Hospital, Philippines. J Am Coll Surg. 2018, 227, 1–2. [Google Scholar] [CrossRef]
- Fonte, J.; Matawaran, B.; Cunanan, E.; Mercado-Asis, L. Treatment outcomes of pituitary tumors at the University of Santo Tomas Hospital: 2004-2008. Philipp J Int Med. 2009, 47, 121–8. [Google Scholar] [CrossRef]
- De Roxas, R.C.; Pedro, K.M.; Rivera, J.P.; Batara, J.M.F. Current treatment status of adult brain tumors in the Philippine General Hospital. J Neurol Neurorehab Res. 2017, 2, 3–4. [Google Scholar] [CrossRef]
- Drug Price Reference Index Department of Health Philippines. Available online: https://dpri.doh.gov.ph/home/drug_2020_index/659 (accessed on 5 September 2023).
- Philippine Food and Drug Administration. Available online: https://verification.fda.gov.ph/drug_productsview.php?showdetail=®istration_number=DR-XY45172 (accessed on 18 December 2023).
| Author | Age/ Sex |
Type of adenoma | Clinical Presentation | Imaging findings | Hormonal Profile | Surgical Treatment | Medical Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Bunoy et al., 2012 (4) | 38/M | Macro- adenoma |
Seizures, frontal headache, blurring of vision (bitemporal hemianopsia) | 4.0 x 5.0 x 4.5 cm sellar-suprasellar mass | Low cortisol, high TSH, normal ACTH | Cranioto- my with excision of the tumor |
Methima- zole, prednisone |
Improved |
| Mendo-za et al., 2015 (32) | 46/F | Macro- adenoma |
Amenorrhea, acromegaly | 2.1 x 3.3 x 2.4 cm sellar-suprasellar mass with foci of intratumoral hemorrhages suggestive of subclinical pituitary apoplexy | High GH, high prolactin | None | Cabergo- line 0.5 mg tablet once a week |
Improved |
| Tating et al., 2016 (30) | 13/M | Micro- adenoma |
Bilateral lower extremity weakness, hypertension | 0.8 x 0.9 x 0.8 cm anterior pituitary gland mass | High ACTH, high cortisol | Transphenoid-al adenomectom-y was indicated but deferred because dexamethasone suppression test revealed high serum cortisol and 24-hr free urine cortisol | None | Expired |
| Sandoval et al., 2020 (31) | 37/F | Macro- adenoma |
Amenorrhea, progressive weight gain, facial roundness, leg weakness, easy bruisability, blurring of vison (bitemporal hemianopsia), hyperpigmented fingernails | 4.6 x 4.1 x 7 cm lobulated, heterogeneously enhancing sellar-suprasellar mass with cystic and necrotic components | High ACTH | Transphenoid-al excision | None | Improved |
| Jordan et al., 2022 (39) | 40/F | Giant adenoma | Acromegaly, headache, blurring of vision (bitemporal hemianopsia) | 6.4 x 7.0 x 5.5 cm lobulated pituitary mass with cystic degeneration and necrosis | High GH, high IGF-1 | Surgical resection via transcranial approach | Bromocrip-tine, radiotherapy | Improved |
| Author | Title | Journal | Institution | Publication Year | Study Design |
|---|---|---|---|---|---|
| Villegas et al. (9) | A review of patients with pituitary tumors at St. Luke’s Medical Center from January 1997 to September 2000 | Philippine Journal of Internal Medicine | St. Luke’s Medical Center | 2002 | Retrospective study |
| Alinsonorin et al. (2) | Pituitary adenoma: clinical profile of 120 patients at the Philippine General Hospital | Philippine Journal of Internal Medicine | Philippine General Hospital | 2003 | Retrospective, descriptive |
| Fonte et al. (41) | Treatment outcomes of pituitary tumors at the University of Santo Tomas Hospital: 2004-2008 | Philippine Journal of Internal Medicine | University of Santo Tomas Hospital |
2009 | Retrospective cohort |
| Bunoy et al. (4) | Inappropriate secretion of thyroid stimulating hormone in a Filipino patient with a pituitary macroadenoma | Journal of ASEAN Federation of Endocrine Societies | St. Luke’s Medical Center | 2012 | Case report |
| Lo et al. (10) | Endogenous Cushing’s syndrome: the Philippine General Hospital experience | Journal of ASEAN Federation of Endocrine Societies | Philippine General Hospital | 2014 | Cross-sectional |
| Jordan et al. (39) | The sleeping giant: an atypical case of a giant pituitary adenoma presenting as acromegaly with minimal symptoms of mass effect | Journal of ASEAN Federation of Endocrine Societies | St. Luke’s Medical Center | 2014 | Case report |
| Mendoza et al. (32) | Acromegaly with cardiomegaly, cardiac thrombus and hemorrhagic cerebral infarct: a case report of therapeutic dilemma with review of literature | International Journal of Endocrinology and Metabolism | University of Santo Tomas Hospital |
2015 | Case report |
| Tating et al. (30) | Cushing’s syndrome from pituitary microadenoma and pulmonary nodules | Oncology Nursing Forum | Philippine General Hospital | 2016 | Case report |
| Faltado et al. (6) | Factors associated with postoperative diabetes insipidus after pituitary surgery | International Journal of Endocrinology and Metabolism | Philippine General Hospital | 2017 | Retrospective cohort |
| Carampatana-Jandug et al. (38) | In-hospital postoperative complications in patients with pituitary adenoma who underwent pituitary surgery from January 2010 to December 2015: a multicenter study | International Journal of Endocrinology and Metabolism | Chong Hua Hospital | 2017 | Retrospective cohort |
| Cudal et al. (37) | Postoperative complications of trans-sphenoidal surgery in a local tertiary hospital during hospital stay | Philippine Journal of Internal Medicine | Makati Medical Center | 2018 | Retrospective cross- sectional |
| Sandoval et al. (31) | Nail hyperpigmentation in ACTH-secreting pituitary adenoma (Cushing’s disease) and its resolution after successful trans-sphenoidal excision | BMJ Case Reports | Philippine General Hospital | 2020 | Case report |
| Seng et al. (3) | Extracapsular resection of pituitary adenomas: a systemic review | Asian Journal of Neurosurgery | Philippine General Hospital | 2023 | Systematic review |
| Laboratory Test/Imaging | Cost Government- subsidized (USD) |
Cost No government no subsidy (USD) |
Cost Private (USD) |
|---|---|---|---|
| IGF-1 | NA | NA | 175.00 |
| ACTH | NA | NA | 136.90 |
| Cortisol | NA | NA | 52.80 |
| Prolactin | 5.80 | 8.50 | 9.10-31.20 |
| FSH | 6.10 | 9.70 | 11.50-24.20 |
| LH | 9.20 | 12.40 | 13.00-24.20 |
| Estradiol | 6.90 | 10.60 | 11.10-46.80 |
| Testosterone | 15.30 | 32.20 | 33.80-46.80 |
| TSH | 6.10 | 10.50 | 12.10-14.40 |
| FT3 | 8.30 | 12.90 | 13.60-49.90 |
| FT4 | 6.40 | 10.00 | 10.50-49.90 |
| Cranial MRI with contrast | 153.70 | 179.30 | 190.00-210.90 |
| Cranial MRI - plain | 75.60 | 91.30 | 96.60-107.30 |
| Cranial CT scan with contrast | 86.30 | 98.10 | 103.00-112.80 |
| Cranial CT scan - plain | 26.30 | 54.40 | 65.30-73.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





