Submitted:
25 January 2024
Posted:
26 January 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
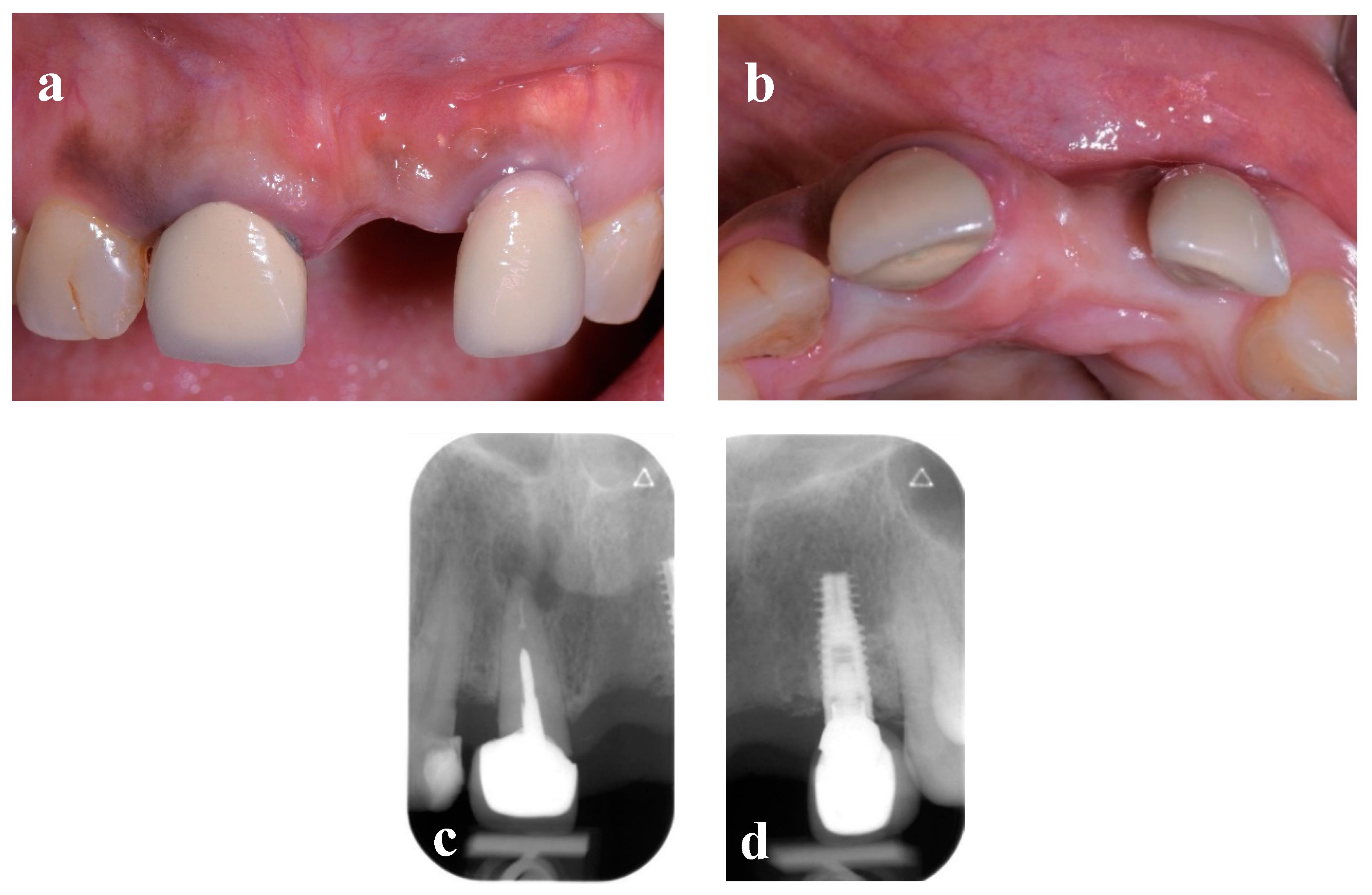
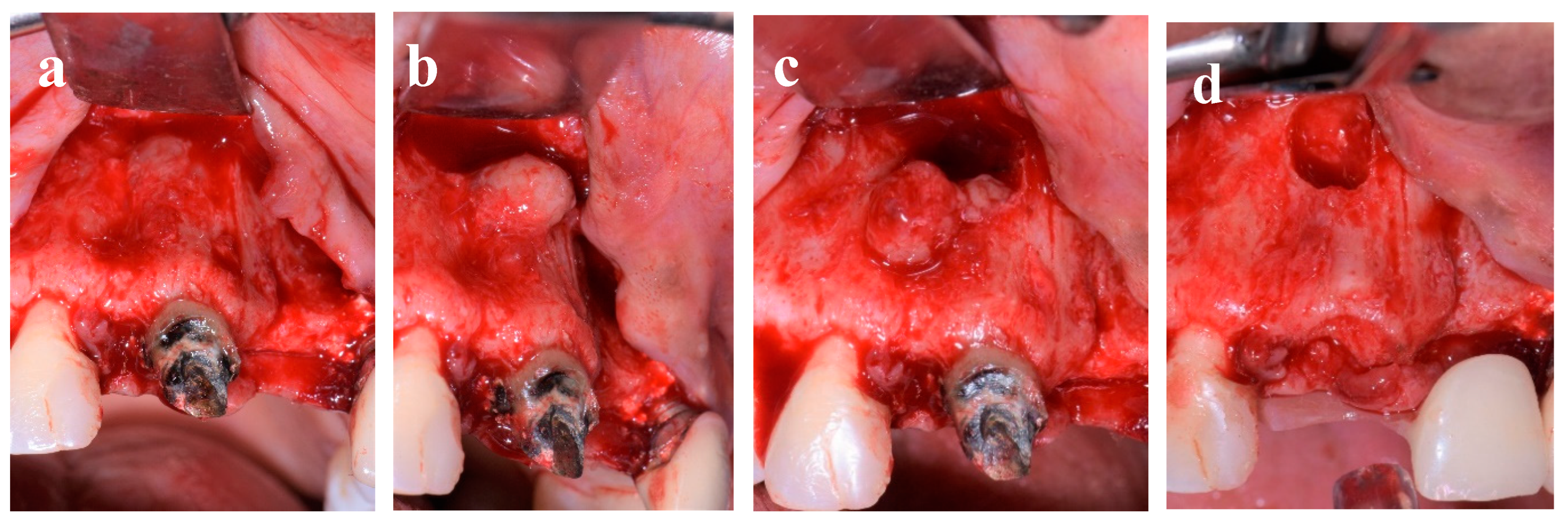
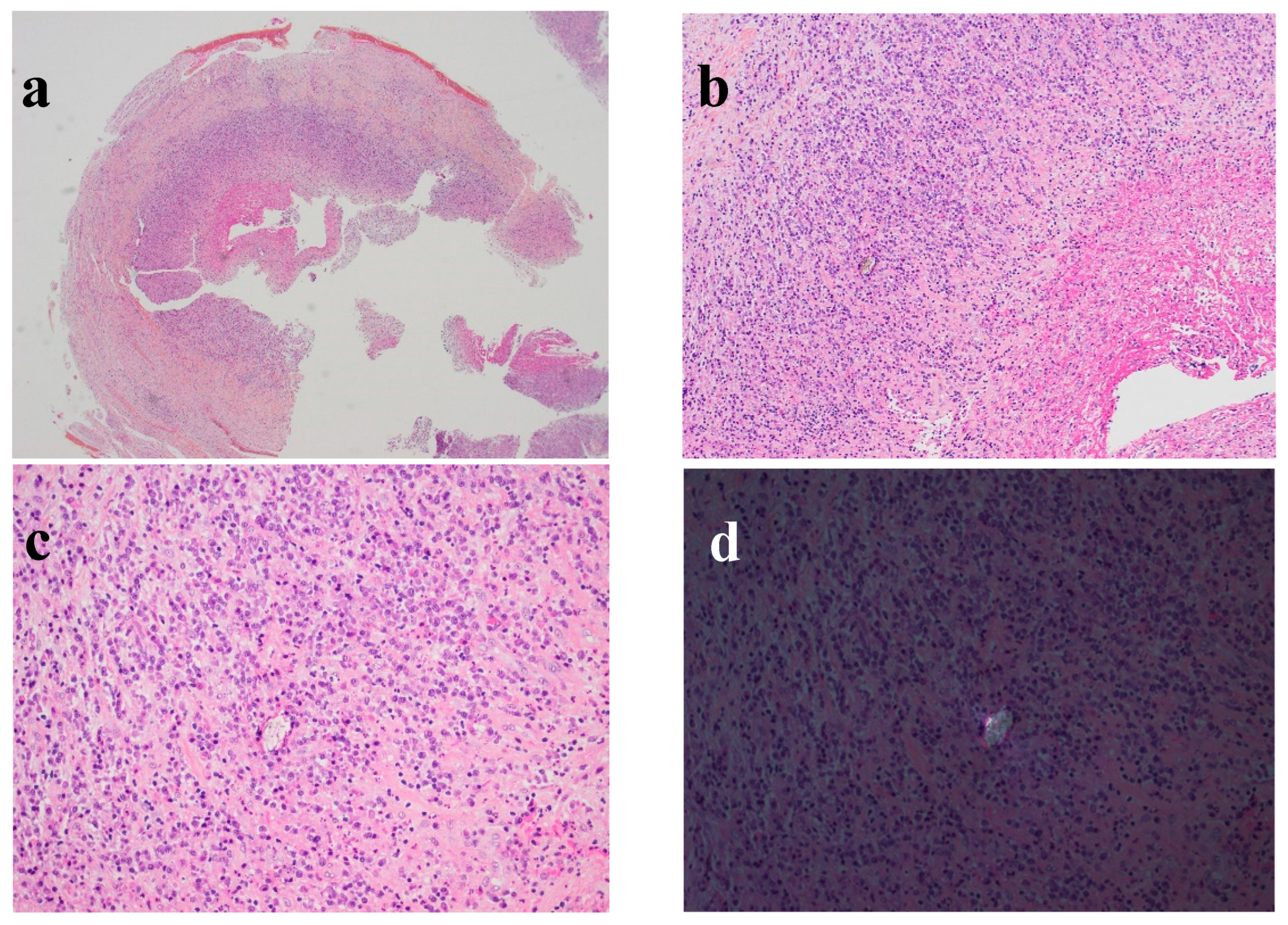
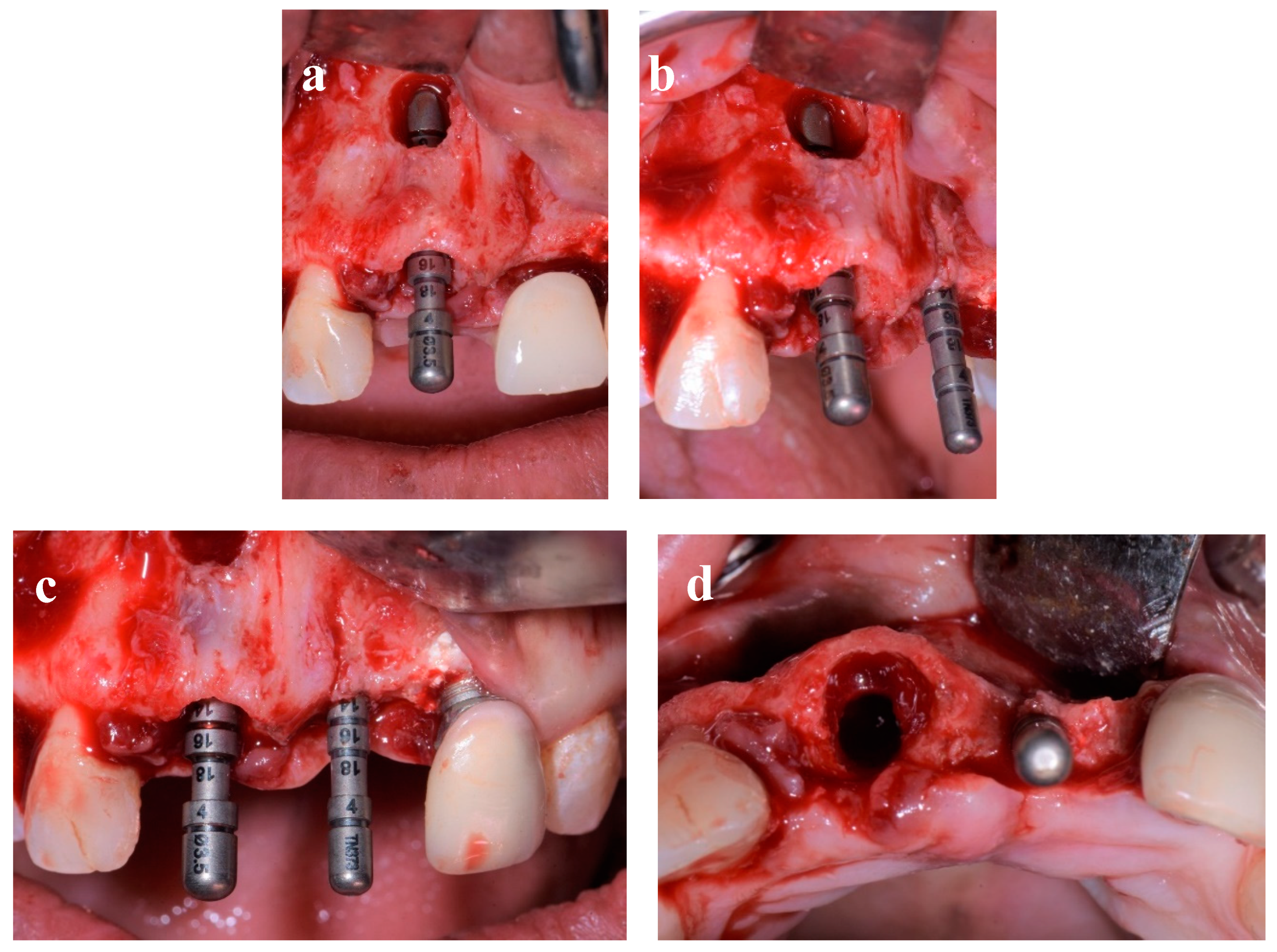
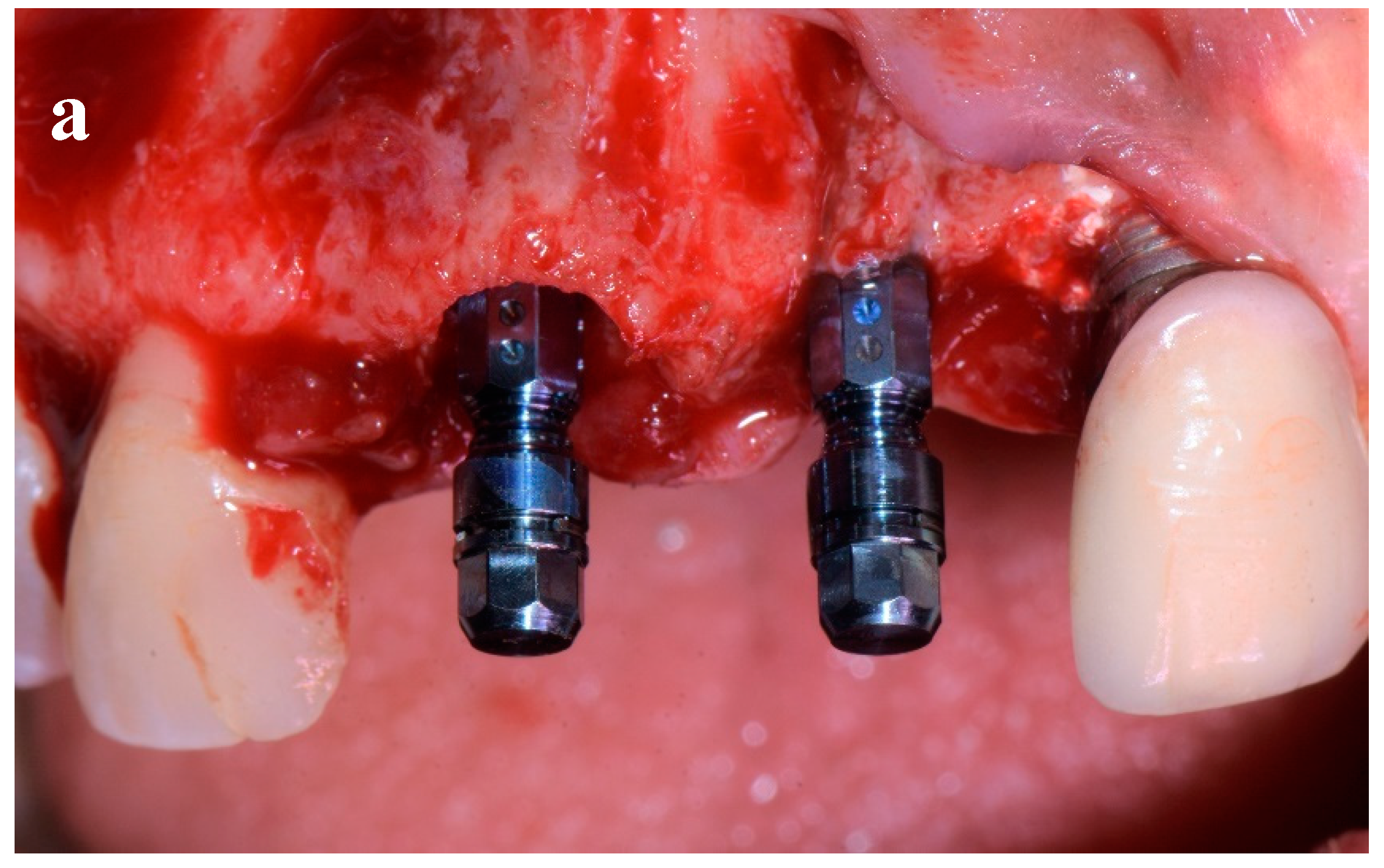
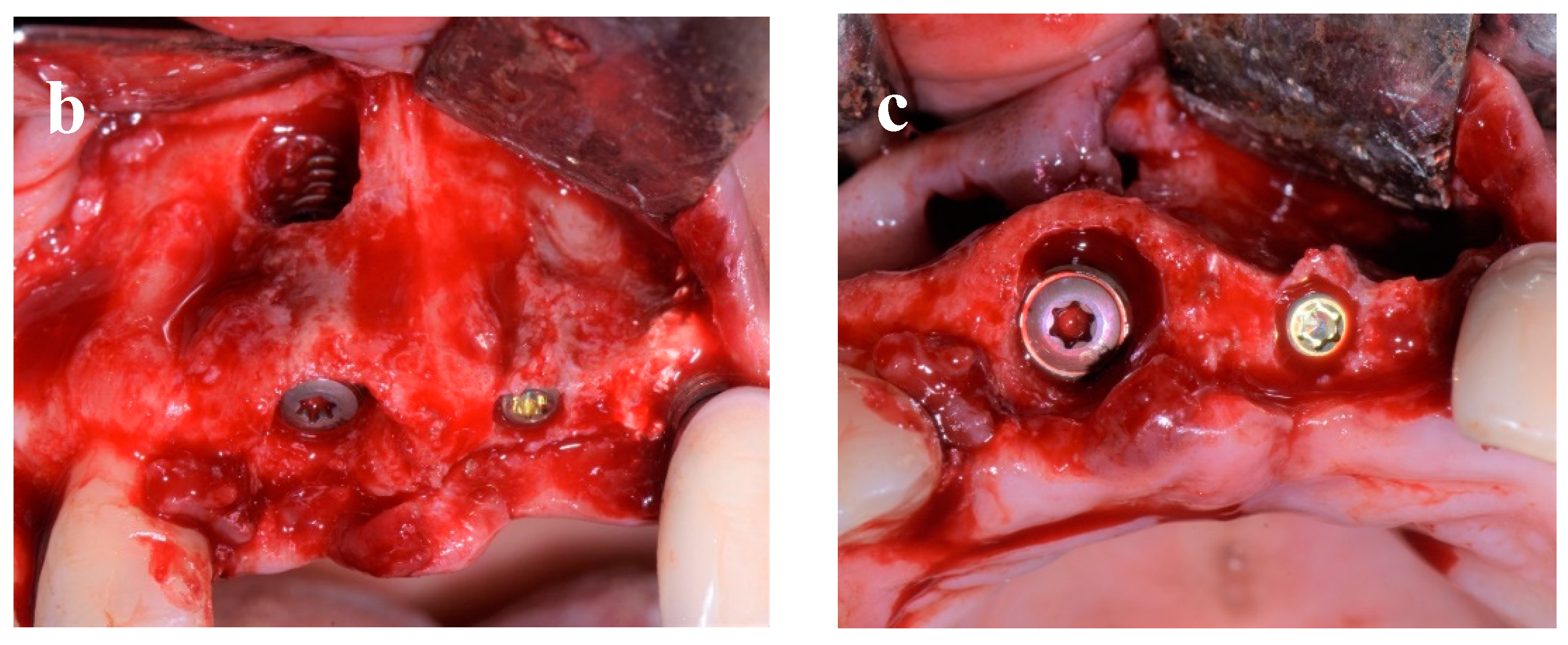
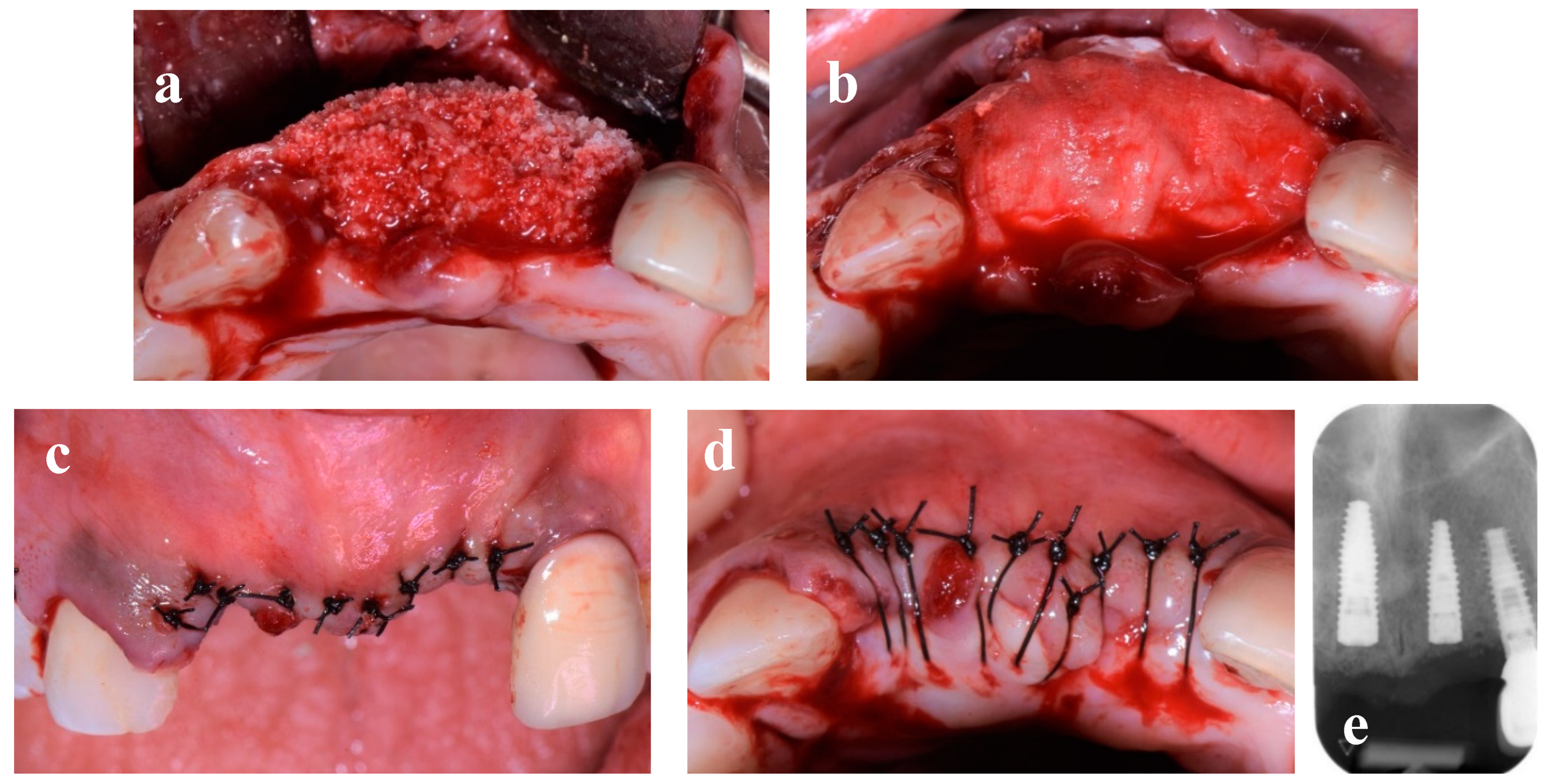
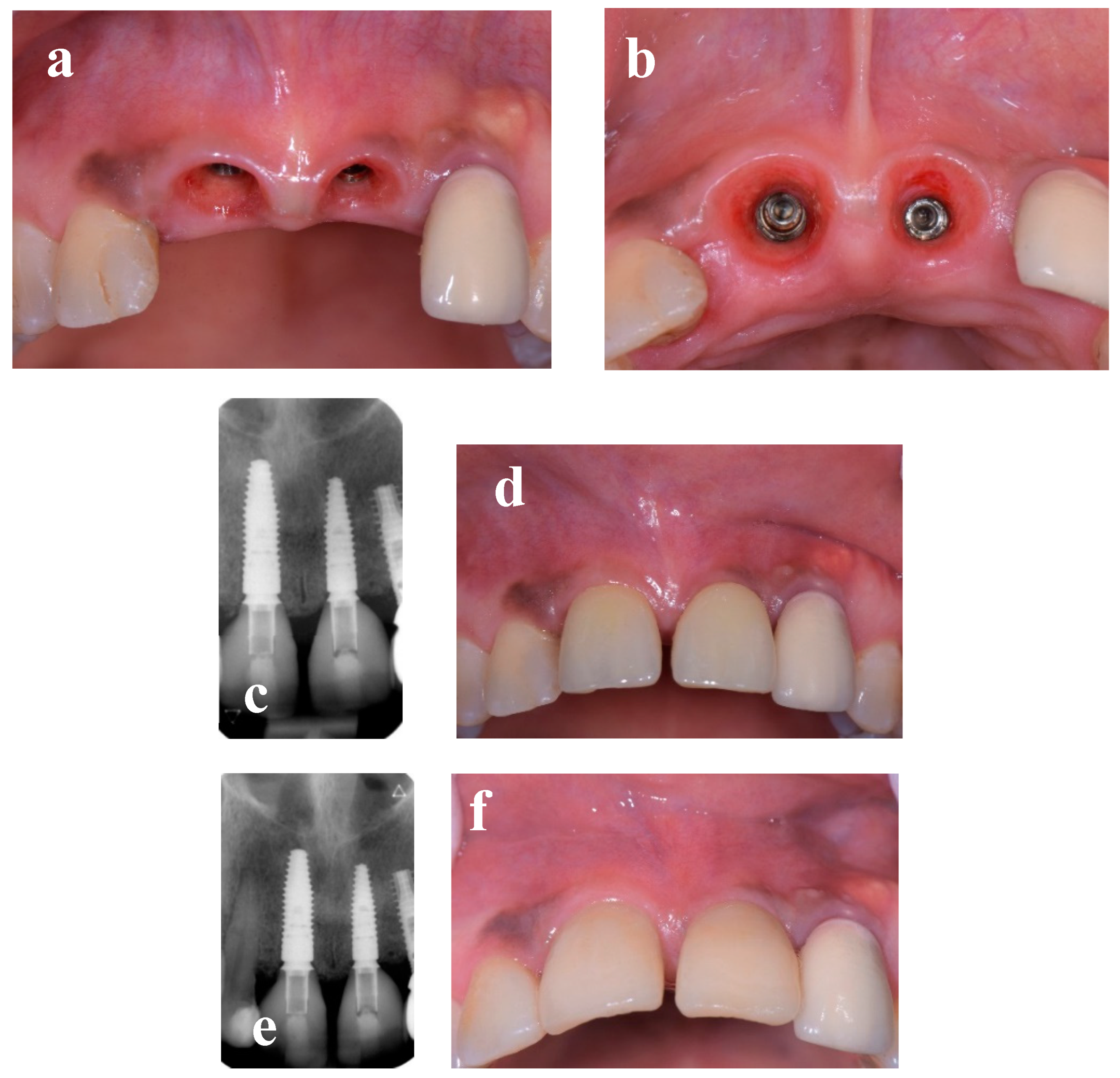
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef] [PubMed]
- Soegiantho, P.; Suryawinata, P.G.; Tran, W.; Kujan, O.; Koyi, B.; Khzam, N.; Miranda, L.A. Survival of Single Immediate Implants and Reasons for Loss: A Systematic Review. Prosthesis 2023, 5, 378–424. [Google Scholar] [CrossRef]
- Perez, A.; Hamzah, S.; Lombardi, T. Immediate versus Delayed Implant Placement in Patients with Tooth Agenesis: An In-Line Retrospective Pilot Study Comparing Clinical and Patient-Related Outcomes. Appl. Sci. 2023, 13, 9368. [Google Scholar] [CrossRef]
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol. 2000 2017, 73, 84–102. [Google Scholar] [CrossRef]
- Chen, S.T.; Buser, D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants 2009, 24, 186–217. [Google Scholar]
- Perez, A.; Caiazzo, A.; Valente, N.A.; Toti, P.; Alfonsi, F.; Barone, A. Standard vs customized healing abutments with simultaneous bone grafting for tissue changes around immediate implants. 1-year outcomes from a randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2020, 22, 42–53. [Google Scholar] [CrossRef]
- Lindeboom, J.A.H.; Tjiook, Y.; Kroon, F.H.M. Immediate placement of implants in periapical infected sites: A prospective randomized study in 50 patients. Oral Surgery, Oral Med. Oral Pathol. Oral Radiol. Endodontology 2006, 101, 705–710. [Google Scholar] [CrossRef]
- Manor, Y.; Alkasem, A.; Mardinger, O.; Chaushu, G.; Greenstein, R.B.N. Levels of bacterial contamination in fresh extraction sites after a saline rinse. Int. J. Oral Maxillofac. Implant. 2015, 30, 1362–1368. [Google Scholar] [CrossRef]
- Fugazzotto, P.A. A retrospective analysis of implants immediately placed in sites with and without periapical pathology in sixty-four patients. J. Periodontol. 2012, 83, 182–186. [Google Scholar] [CrossRef]
- Jung, R.E.; Zaugg, B.; Philipp, A.O.H.; Truninger, T.C.; Siegenthaler, D.W.; Hämmerle, C.H.F. A prospective, controlled clinical trial evaluating the clinical radiological and aesthetic outcome after 5 years of immediately placed implants in sockets exhibiting periapical pathology. Clin. Oral Implant. Res. 2012, 24, 839–846. [Google Scholar] [CrossRef]
- Kakar, A.; Kakar, K.; Leventis, M.D.; Jain, G. Immediate Implant Placement in Infected Sockets: a consecutive cohort study. J Lasers Med Sci 2020, 11, 167–173. [Google Scholar] [CrossRef]
- Johnson, N.R.; Gannon, O.M.; Savage, N.W.; Batstone, M.D. Frequency of odontogenic cysts and tumours: a systematic review. J Investig Clin Dent 2014, 5, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Shivhare, P.; Singh, A.; Haidry, N.; Yadav, M.; Shankarnarayan, L. Multilocular radicular cyst – a common pathology with uncommon radiological appearance. J Clin Diagn Res 2016, 10, 13–15. [Google Scholar] [CrossRef]
- Noda, A.; Abe, M.; Shinozaki-Ushiku, A.; Ohata, Y.; Zong, L.; Abe, T.; Hoshi, K. A bilocular radicular cyst in the mandible with tooth structure components inside. Case Rep. Dent. 2019, 2019, 6245808. [Google Scholar] [CrossRef]
- Quadri, A.; Keerthi, R.; Khan, T.A. Unusual aggressive large radicular cyst invading maxillary sinus: a case report. Int J Sci Stud 2016, 4, 180–183. [Google Scholar]
- Avril, L.; Lombardi, T.; Ailianou, A.; Burkhardt, K.; Varoquaux, A.; Scolozzi, P.; Becker, M. Radiolucent lesions of the mandible: a pattern-based approach to diagnosis. Insights Imaging 2014, 5, 85–101. [Google Scholar] [CrossRef]
- Kolari, V.; Rao, H.T.A.; Thomas, T. Maxillary and mandibular unusually large radicular cyst: A rare case report. Natl. J. Maxillofac. Surg. 2019, 10, 270–273. [Google Scholar] [CrossRef]
- El-Naggar, A.K.; Chan, J.K.C.; Grandis, J.R.; Takata, T.; Slootweg, P.J. WHO classification of head and neck tumours (4th edition). IARC 2017, 9, 204–207. [Google Scholar]
- Javed, F.; Romanos, G.E. The role of primary stability for successful immediate loading of dental implants. A literature review. J. Dent. 2010, 38, 612–620. [Google Scholar] [CrossRef]
- Trisi, P.; Perfetti, G.; Baldoni, E.; Berardi, D.; Colagiovanni, M.; Scogna, G. Implant micromotion is related to peak insertion torque and bone density. Clin. Oral Implant. Res. 2009, 20, 467–471. [Google Scholar] [CrossRef]
- Ebenezer, V.; Balakrishnan, K.; Asir, R.V.D.; Sragunar, B. Immediate placement of endosseous implants into the extraction sockets. J. Pharm. Bioallied Sci. 2015, 7, 234–237. [Google Scholar] [CrossRef]
- Roe, P.; Kan, J.Y.K.; Rungcharassaeng, K.; Caruso, J.M.; Zimmerman, G.; Mesquida, J. Horizontal and vertical dimensional changes of peri-implant facial bone following immediate placement and provisionalization of maxillary anterior single implants: a 1-year cone beam computed tomography study. Int J Oral Maxillofac Implants 2012, 27, 393–400. [Google Scholar]
- Cosyn, J.; Sabzevar, M.M.; De Bruyn, H. Predictors of inter-proximal and midfacial recession following single implant treatment in the anterior maxilla: a multivariate analysis. J. Clin. Periodontol. 2012, 39, 895–903. [Google Scholar] [CrossRef]
- Buser, D.; Halbritter, S.; Hart, C.; Bornstein, M.M.; Grütter, L.; Chappuis, V.; Belser, U.C. Early Implant Placement With Simultaneous Guided Bone Regeneration Following Single-Tooth Extraction in the Esthetic Zone: 12-Month Results of a Prospective Study With 20 Consecutive Patients. J. Periodontol. 2009, 80, 152–162. [Google Scholar] [CrossRef]
- Hämmerle, C.H.F.; Chen, S.T.; Wilson, T.G. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int. J. Oral Maxillofac. Implant. 2004, 19, 26–28. [Google Scholar]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Bolz, W.; Huerzeler, M. Tissue alterations after tooth extraction with and without surgical trauma: a volumetric study in the beagle dog. J. Clin. Periodontol. 2008, 35, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Rocci, A.; Martignoni, M.; Gottlow, J. Immediate Loading in the Maxilla Using Flapless Surgery, Implants Placed in Predetermined Positions, and Prefabricated Provisional Restorations: A Retrospective 3-Year Clinical Study. Clin Implant Dent Relat Res. 2003, 5, 29–36. [Google Scholar] [CrossRef]
- Merli, M.; Bernardelli, F.; Esposito, M. Immediate versus early nonocclusal loading of dental implants placed with a flapless procedure in partially edentulous patients: preliminary results from a randomized controlled clinical trial. Int J Periodontics Restorative Dent 2008, 28, 453–459. [Google Scholar] [PubMed]
- Degidi, M.; Piattelli, A. A 7-year Follow-up of 93 Immediately Loaded Titanium Dental Implants. J Oral Implantol 2005, 31, 25–31. [Google Scholar] [CrossRef]
- Ottoni, J.M.P.; Oliveira, Z.F.L.; Mansini, R.; Cabral, A.M. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants 2005, 20, 769–776. [Google Scholar]
- Greenstein, G.; Cavallaro, J. Implant Insertion Torque: Its Role in Achieving Primary Stability of Restorable Dental Implants. Compend. Contin. Educ. Dent. 2017, 38, 88–95. [Google Scholar] [PubMed]
- Balaji, P.; Balaji, S.M.; Ugandhar, P. Immediate implant in single rooted teeth - Study on primary stability and bone formation. Indian J. Dent. Res. 2015, 26, 421–426. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




