1. Introduction
In 2022, the United States (U.S.) faced an acute infant formula shortage that was initiated by a recall by Abbott Nutrition, the largest U.S. infant formula manufacturer that provides 40% of the nation’s infant formula. [
1] Abbott voluntarily recalled several brands of its powdered formula products due to bacterial contamination from
Cronobacter sakazakii [
2]. Additionally, Abbott also voluntarily closed one of the country’s largest manufacturing plant in Michigan that was found to be connected to the contamination [
3]. These events were exacerbated by supply chain issues related to the COVID-19 pandemic and restrictive U.S. trade and tariff policies that led to a reduction of available infant formula [
4]. By the end of May 2022 the shortage reached its height, with a national out-of-stock rate for infant formula as high as 90% in several states [
5] which left millions of parents to face uncertainty in safely feeding their infants [
6,
7]. In response, the U.S government introduced “Operation Fly” to assist families in accessing safe imported infant formulas.
The 2022 infant formula shortage was especially distressful for vulnerable populations such as families from low-income communities that participate in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and heavily rely on infant formula (consume >50% of U.S. produced formula) [
8,
9] and infants requiring specialty formulas due to medical or other conditions [
10]. Infants that require specialty formulas due to metabolic or medical conditions such as inborn error of metabolism, low birth weight or other medical or dietary conditions represent approximately 6% of infants that use infant formula in the U.S.[
11].
Due to the inaccessibility of infant formula, health officials were concerned parents would rely on unsafe infant feeding practices that the American Academy of Pediatrics (AAP), Centers for Disease Control and Prevention (CDC) and Food and Drug Administration (FDA) recommend against. Such unsafe infant feeding practices include: 1) modifying formula by diluting it with water [
12]; 2) making homemade infant formula [
13]; 3) feeding cow’s milk before one year of age [
14]; and 4) informal human milk sharing [
15]. In a recent prospective cross-sectional study, predominately of families from low-income communities, the number of individuals that used at least one unsafe infant feeding practice increased from 8% before to 48.5% during the 2022 infant formula shortage. Specifically, the percentage of parents that reported infant feeding practices before and during the infant formula shortage significantly increased from 2% to 28% for banked donor milk use; 5% to 26% for use of human milk from informal sharing; and 2% to 29% for use of watered-down infant formula [
16]. These unsafe infant feeding practices increase the health and safety risks of infants who rely on infant formula exclusively or as a supplement to human milk.
To date, no studies have reported the impact of the 2022 infant formula shortage on parental consumer behaviors, infant health or quality of life outcomes or breastfeeding outcomes. The purpose of this study was to identify infant feeding practices, health, and quality of life outcomes during the 2022 infant formula shortage. We conducted a retrospective cross-sectional analysis and needs assessment in families from middle-high income communities and reported a high percentage of infants who required specialty formulas. The goal of this study was to identify areas within regulatory and healthcare policies and programs that could improve the resiliency of the infant food system and prevent a future infant feeding crisis.
2. Materials and Methods
2.1. Subjects and Design
Parents who were signed up with Bobbie Labs listserv who agreed to be contacted for future research purposes were emailed an invitation email to participate in an anonymous, cross-sectional, electronic survey. Individuals who met all study criteria completed the survey between December 18, 2022, and January 31, 2023. The first one hundred individuals who completed the survey received a $50 electronic gift card. Parents were eligible to participate if they fulfilled the following criteria: 1) were 18 years old or older; 2) lived with their infants in the U.S. in May 2022; 3) were the parent of an infant who was 6 months old or younger in May 2022; 4) their infant consumed some amount of infant formula before the May 2022 shortage; 5) they experienced challenges with feeding their infant because of the infant formula shortage in May 2022; and 6) they agreed that only one parent of one baby from the same household would complete the survey. Parents reported their demographics and answered questions about their infant feeding practices, experiences, and sentiments in response to the infant formula shortage. The study was approved by the UC Davis Institutional Review Board (IRB ID: 1920147).
The online survey was created in Qualtrics 2022 (Provo, Utah, USA) and included ninety-four unique questions. Participants answered yes/no, multiple choice, rating on a sliding scale (0 to 10), and open-ended questions. The survey contained questions about demographics including, infant and parental age, socioeconomic status, and ethnicity. Participants were asked what their infants typically ate over a 7-day period right before and a 7-day period during the infant formula shortage. Additionally, use of human milk from informal sharing, homemade infant formula, watered-down formula and expired infant formula were aggregated into one variable as “unsafe infant feeding practices” for a 7-day period right before and a 7-day period during the most challenging time of the shortage.
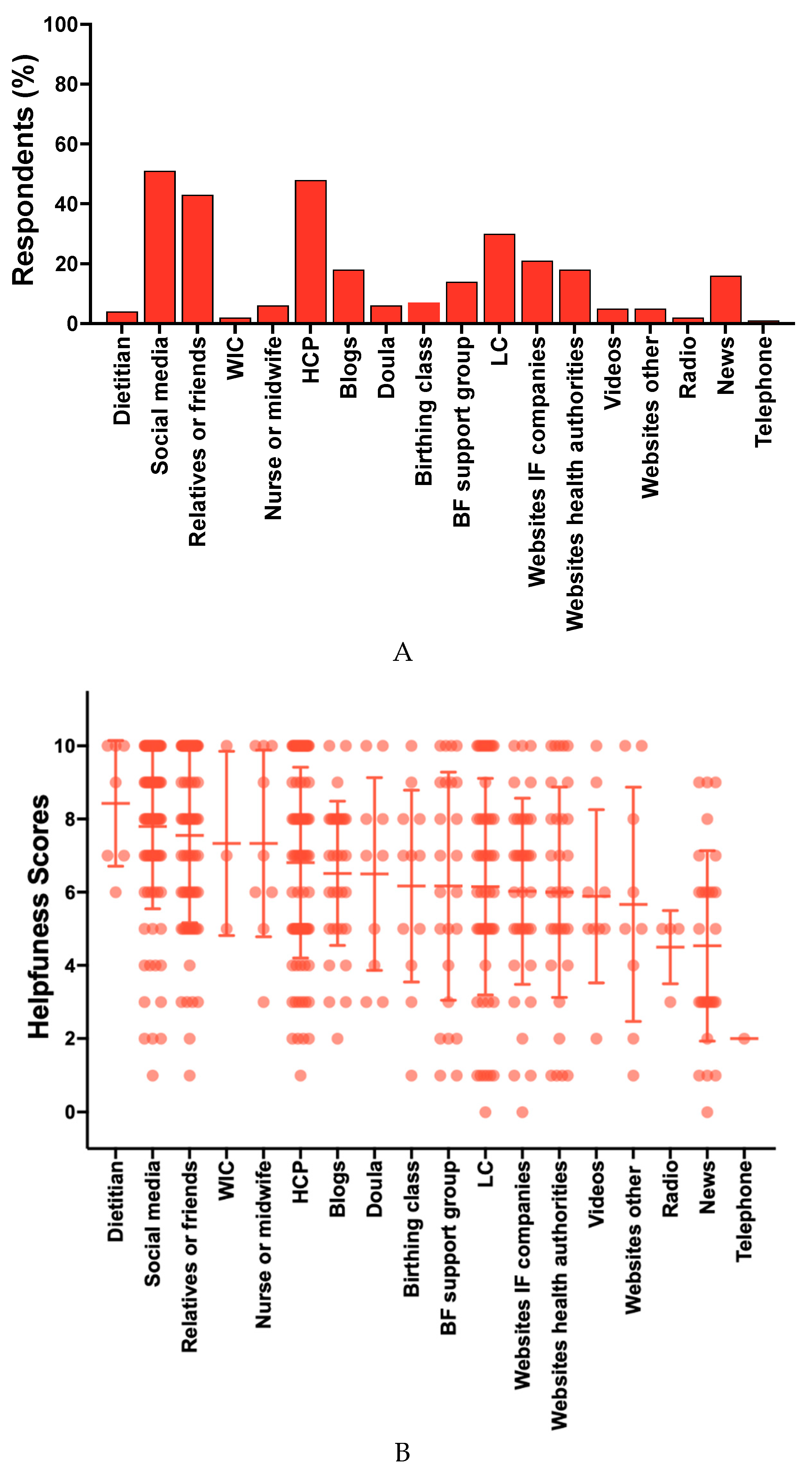
Participants were asked to select all the resources that provided guidance or support in feeding their infants during the shortage. Participants were also asked to rate on a sliding scale from 0 to 10 how helpful a list of resources
have been with providing guidance or support to feed their infants or to select “non-applicable” if they did not experience any help from the listed resource. Infant feeding sources and resources used in this survey were adapted from the Infant Feeding Practices Study II (IFPS II) [
17] which differentiated lactation consultants from other healthcare providers and included up-to-date online resources such as social media, and blogs.
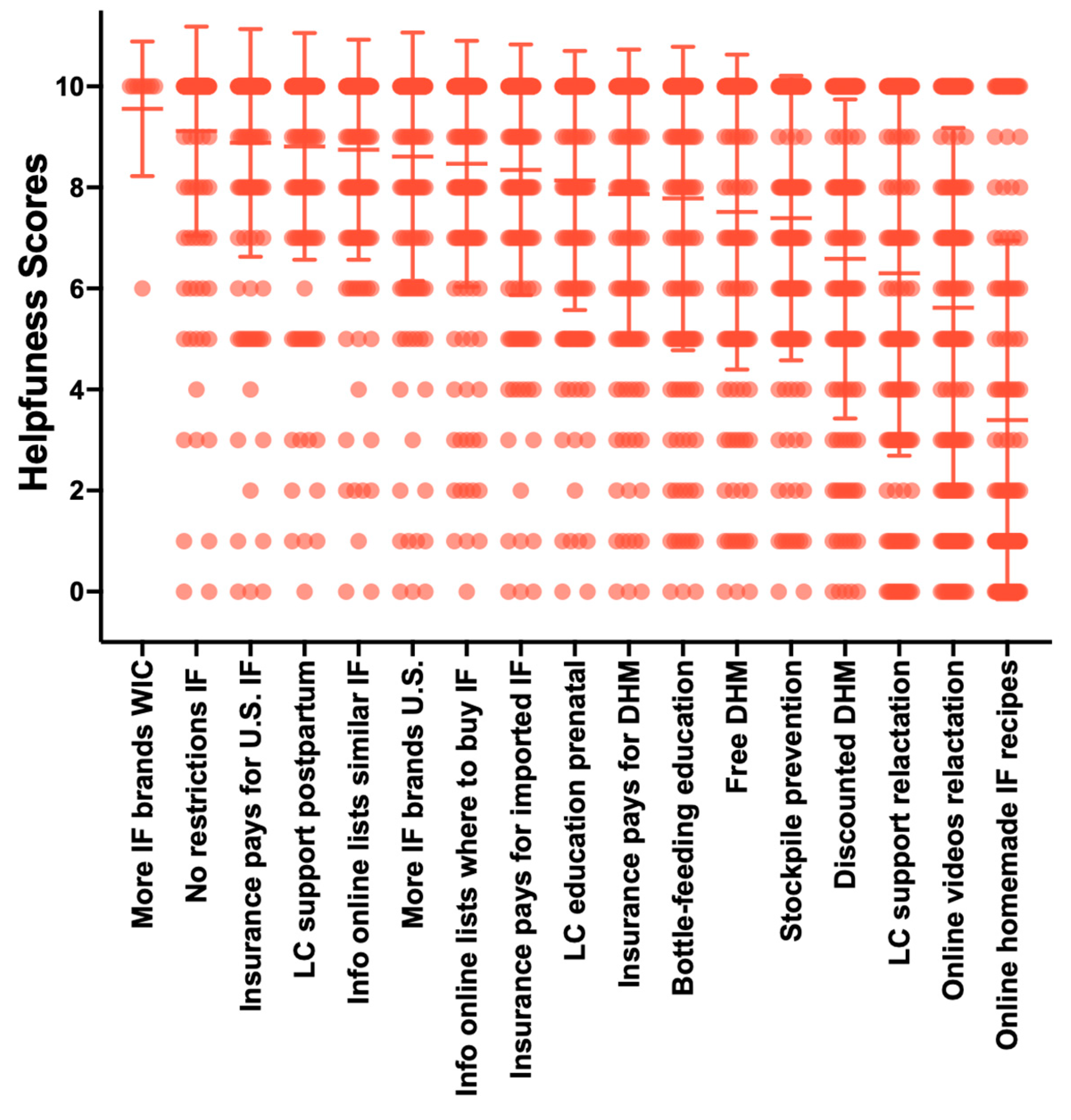
Participants were asked to rate on a sliding scale from 0 to 10 how helpful a list of activities would be in helping families feed their infants in the “near future” or to select “non-applicable” if they were unsure. These activities were compiled from comments posted on several multiple social media outlets (Reddit, Facebook, Twitter) by parents during the height of the 2022 infant formula shortage. The survey used in this study is available as Supplementary File S1.
2.2. Data Validation
To ensure the data collected from the study survey was reliable and not completed in duplicate by the same individuals, individuals completed two surveys. The first survey was used for screening and prompted individuals from the Bobbie Labs listserv to answer questions about their eligibility. Individuals who met all eligibility criteria were emailed the cross-sectional survey and were required to use the same email addresses entered in the screening survey. The cross-sectional survey excluded individuals with the same email addresses. Data for completed surveys were included in the statistical analyses.
2.3. Statistics
All statistical analyses were conducted using IBM SPSS Statistics version 29 and figures were generated in Graphpad PRISM v.10.1.2 Statistical significance was considered as p < 0.05. Bonferroni-adjusted p-values for multiple comparisons are reported herein. Descriptive statistics (means, standard deviations, ranges, frequencies, and percentages) are reported for demographics, breastfeeding experience, infant feeding practices, consumer behavior, infant outcomes, use and sentiments about resources, and sentiments about future activities that could help families feed their infants in the future.
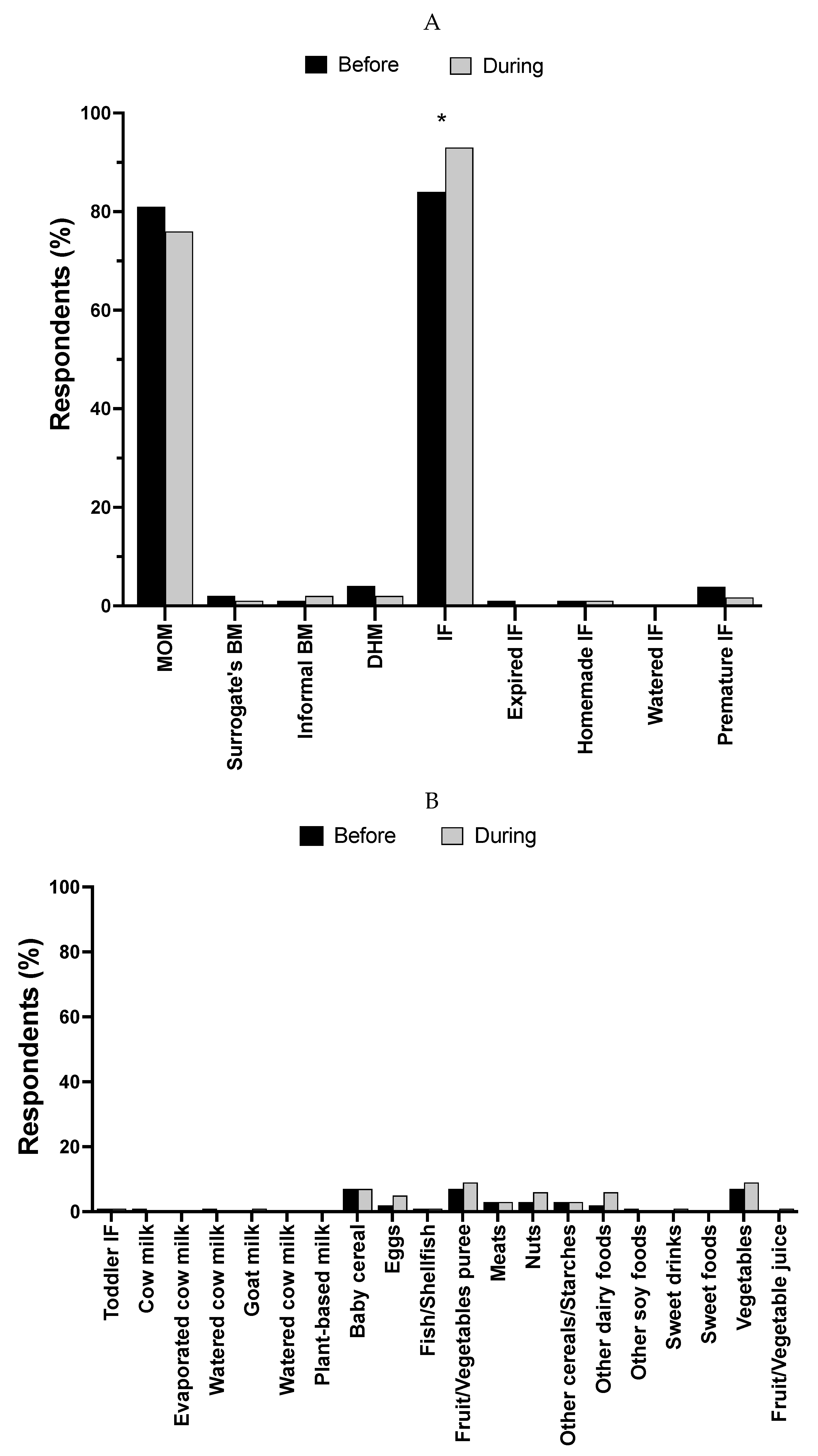
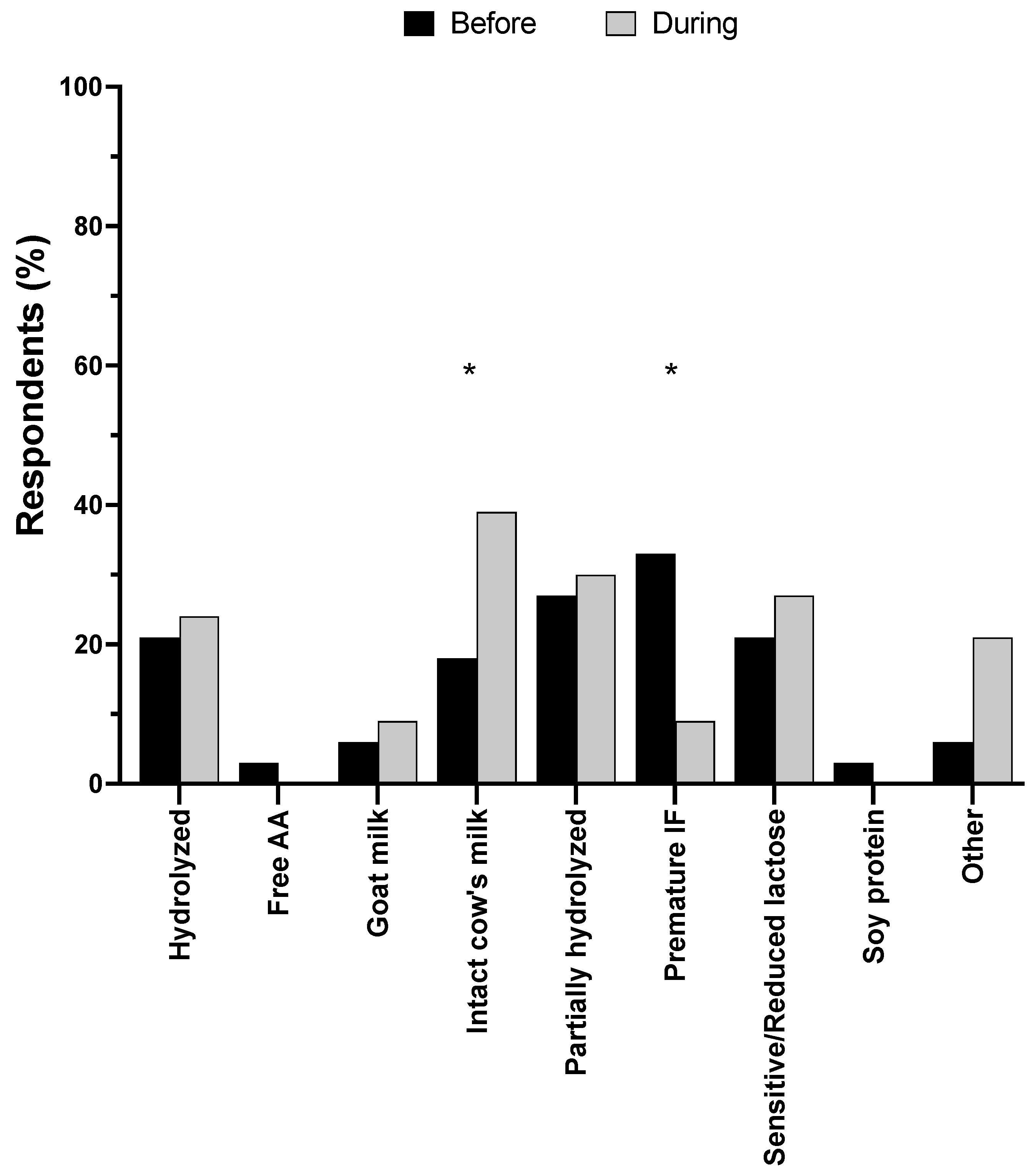
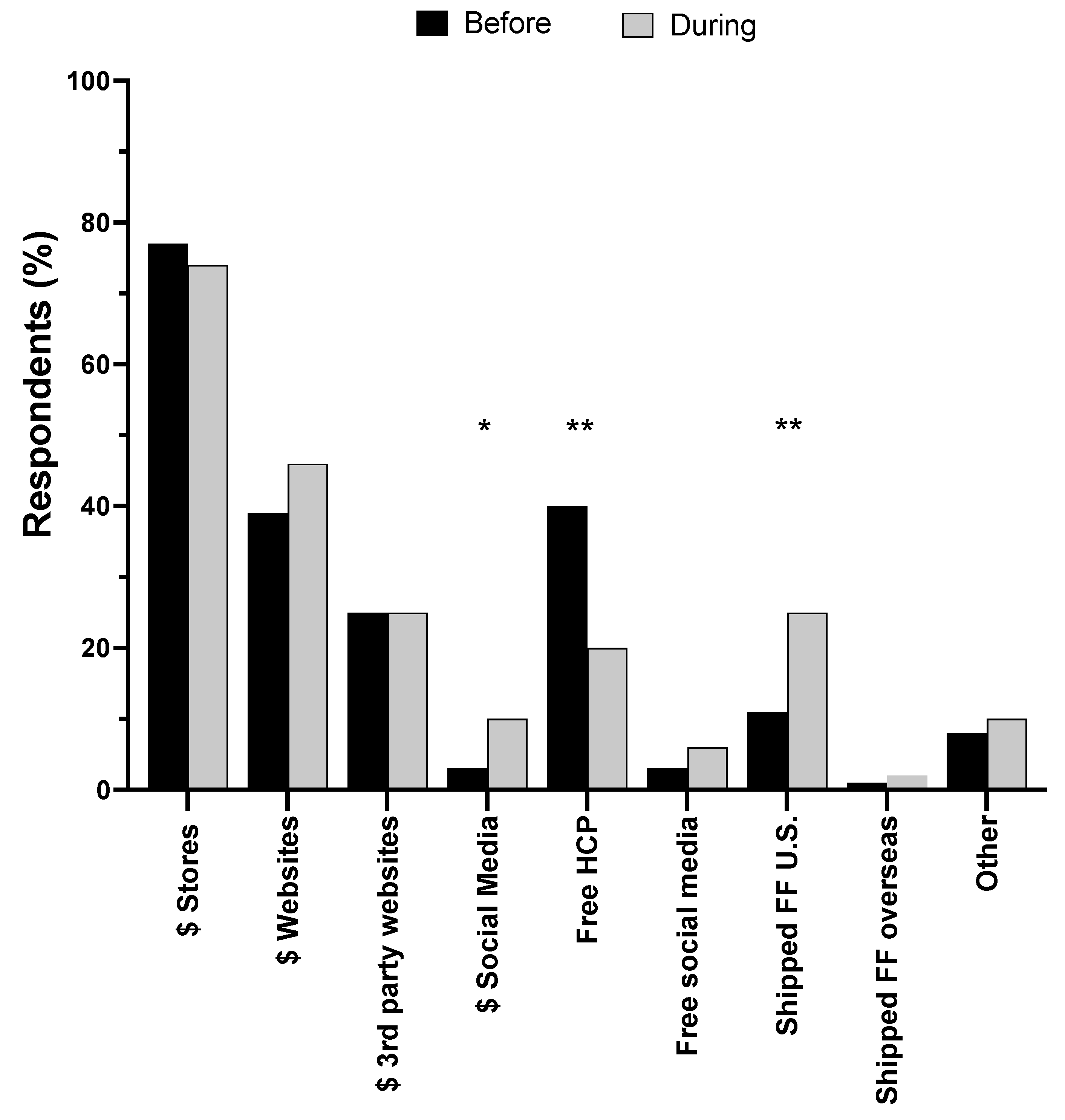
To understand how infant feeding changed in response to the infant formula crisis, parents were asked what their infants typically ate over a 7-day period right before and a 7-day period during the most challenging time of the infant formula shortage. Parents were also asked how they obtained formula before and during the shortage. Data were treated as binary (yes/no) responses and the McNemar test was used to determine if there were differences for each item before and during the infant formula shortage.
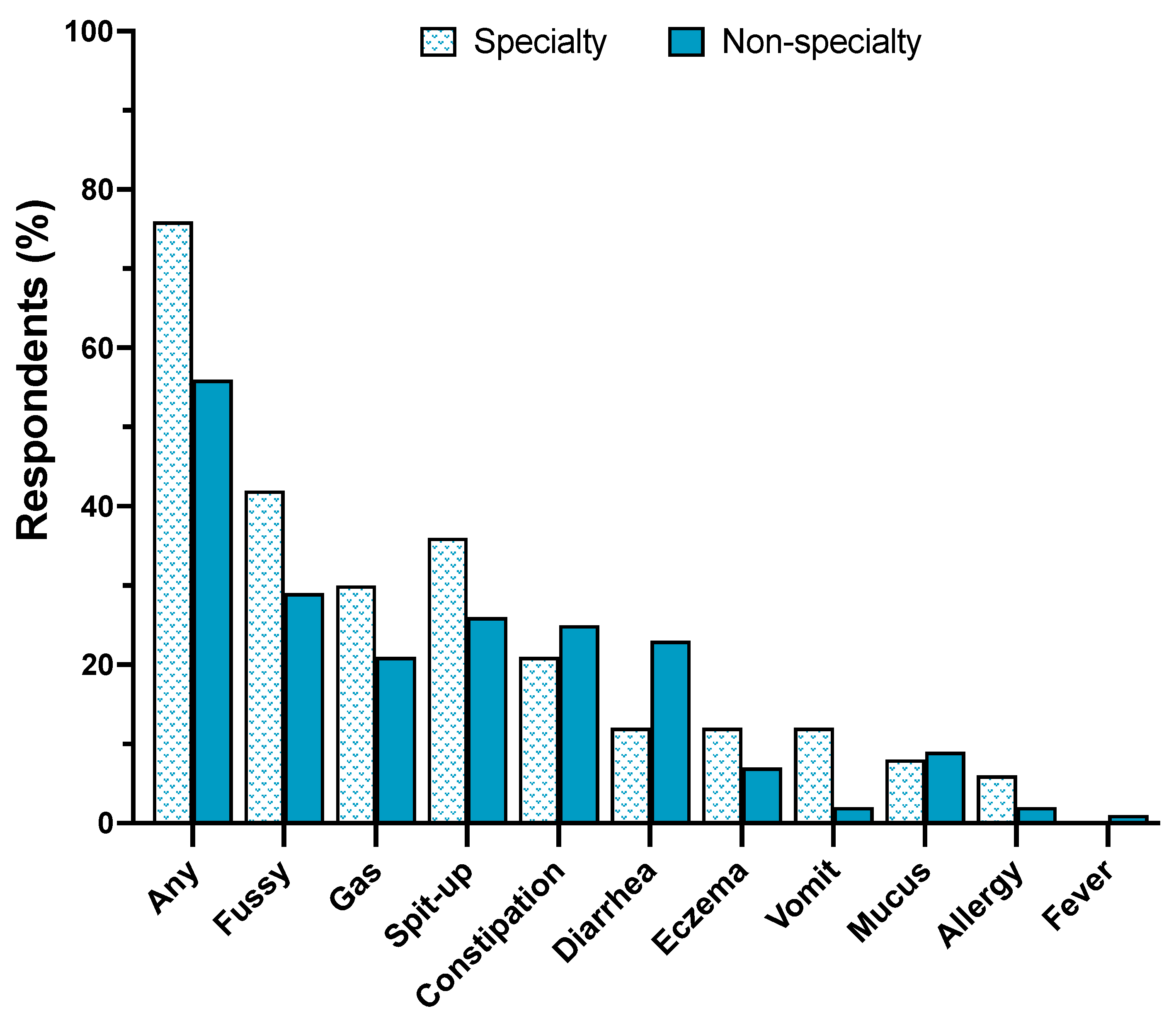
Parents were asked if their infants experienced any problems in response to changing infant formulas during the shortage. Parents selected problems from a list which were treated as binary (yes/no) responses and Pearson Chi-Square, 2-sided test and Phi correlation were used to determine differences and their effect sizes, respectively, in the number of individuals whose infants experienced problems based on their requirement for specialty formulas (vs. no requirement for specialty formulas).
The survey prompted parents to select all that apply from a list of nineteen resources that provided guidance or support in feeding their infants during the infant formula shortage. Parents who selected “yes” to using any of the nineteen resources, were asked to rate on a scale 0-10 how helpful those resources have been in providing guidance or support in feeding their infants during the infant formula shortage. Parents were also asked to rate on a scale 0-10 how helpful they think seventeen activities would be in helping families feed their babies in the “near future”.
This study also collected qualitative data and prompted parents to offer open responses about how they dealt with the infant formula shortage and the actions they feel should be taken by health authorities, food companies, and the government that could help them feed their infants during this crisis and prevent future crises. Open-ended responses were searched for repetition in 5% or more of respondents and reduced to thirty-eight words, themes, or key phrases shown in
Table S1. Canva® 2023 was used to manually generate a word cloud of terms for which font size and color are proportional to the frequency of repeated words, themes, or key phrases.
4. Discussion
The 2022 infant formula shortage was an unprecedented infant feeding crisis that led to nationwide food and nutrition insecurity in our most vulnerable population [
7]. This study used a semi-structural questionnaire to investigate infant feeding practices, parents’ consumer behaviors and infant outcomes in response to the shortage to identify areas within government, regulatory and healthcare systems and policies that could result in a resilient infant food system.
The use of human milk from informal sharing, homemade infant formula, diluted formula, or expired infant formula was low in this population and did not change in response to the infant formula shortage. These findings are in contrast to Cernioglo et al. that reported a significant increase in the use of any unsafe infant feeding practice from 8% before the infant formula shortage to nearly half during the infant formula shortage [
16]. The differences in use of unsafe infant feeding practices between Cernioglo et al., and our study may reflect the differences between the two populations’ socioeconomic statuses and supported by Marino et al., that reported higher use of unsafe infant feeding practices by families from lower compared with higher income communities[
18].
While the use of cow milk, goat milk, and alternative milk beverages were low (<1%) and did not change, other complementary foods such as baby cereal was used by 7% of parents before and during the shortage, and the use of other dairy such as yogurt increased from 2% before to 6% during the shortage. These data are consistent with a cross-sectional analysis by Marino and co-workers for which 10% of infant formula users added cereal to formula and 7% fed their infants with solid foods instead of feeding infant formula [
18].
The use of pasteurized donor human milk was low (2-4%) and did not significantly change in response to the shortage. Use of pasteurized donor human milk in our study was lower than a recent cross-sectional study of 2,315 individuals by DiMaggio and colleagues that reported 8% of survey respondents reported using donor milk [23]. Similar reports were made by the Human Milk Bank Association of North America (HMBANA) which experienced a high demand for donor milk during the 2022 infant formula shortage [
19]. However, our data are consistent with a generally low use of pasteurized donor human milk in mostly term and healthy infants which is largely reserved for premature and very low birthweight infants.
Approximately 80% of infants were combination feeders (mother’s own breast milk and formula) and unexpectedly, use of infant formula significantly increased during the shortage when out-of-stock rates climbed as high as 90% in some states. This study found 14% of parents acquired imported formulas through Operation Fly, however the survey did not prompt families to report how many units of formula they acquired so we are unable to estimate the impact of the federal program. Additionally, in response to the shortage, the number of parents who acquired free infant formula samples from healthcare providers decreased, yet more parents purchased infant formula via social media and acquired formula from shipments sent from family and friends in the United States. These data are consistent with a recent qualitative study that reported white female parents expressed positive feelings for having supportive family members and friends who helped them find formula which was not described by any Black, or SNAP or WIC eligible participants [
20]. This study also revealed that about 20% of parents stockpiled infant formula during the shortage with 4 weeks-worth or more of infant formula at home. The American Academy of Pediatrics’ recommends purchasing no more than a 10-day to 2-week supply of formula to prevent hoarding [
21].
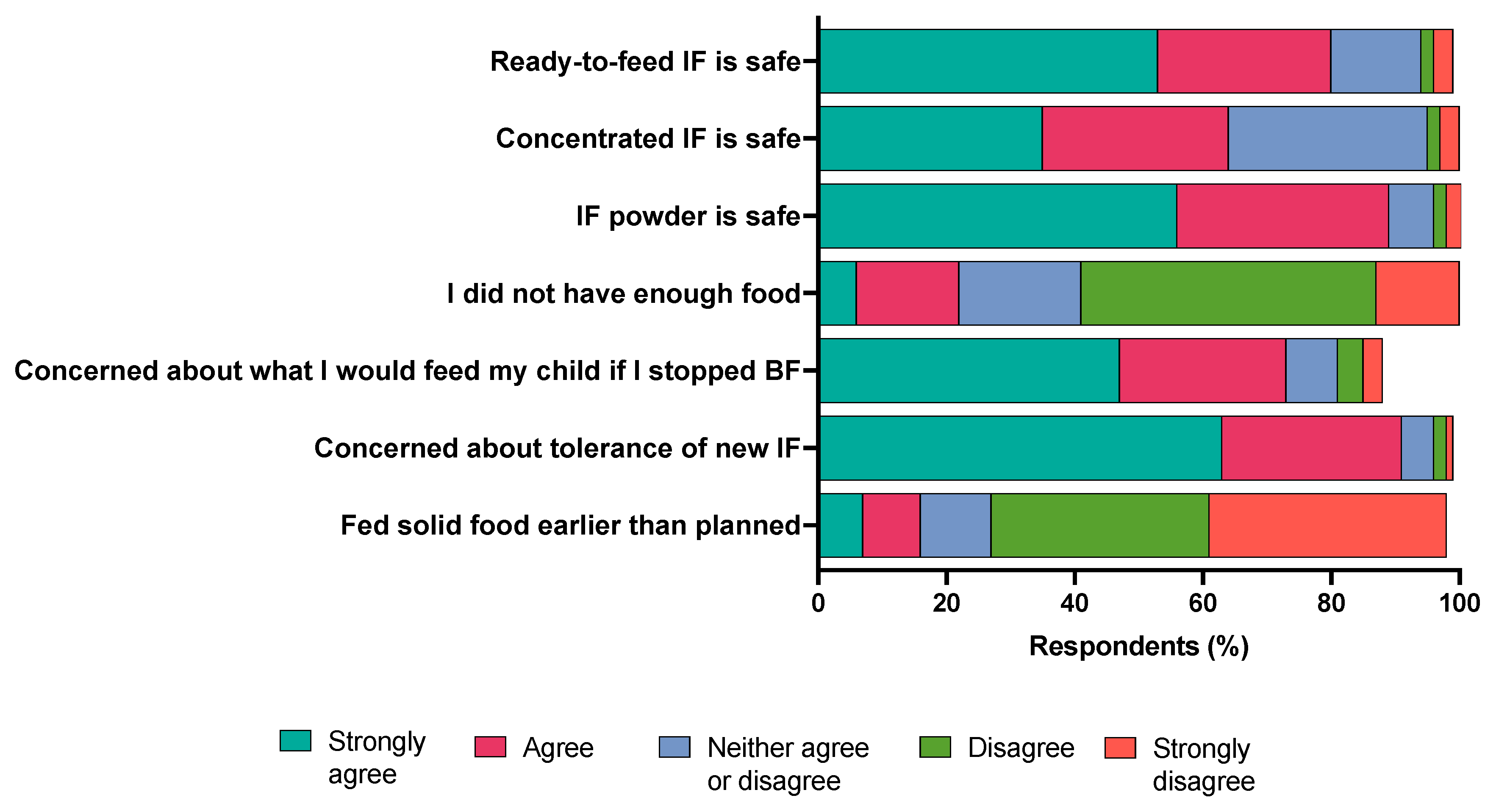
Consumer behavior questions were asked to investigate the burden parents experienced in navigating the May 2022 infant formula shortage. Approximately 90% of parents used U.S. brands of infant formula which is consistent with the dominance of the infant formula market by U.S. companies [33]. Approximately 80% of parents switched infant formula types or brands during the shortage, and of these individuals, 87% switched because they could not find the formula they
typically used. One third or more of parents switched infant formula brands or types 3 to 5 times, and over a 24-hour period visited four or more stores and traveled more than twenty miles to one store to purchase infant formula. These data are similar to a recent report from an online survey in 1,070 U.S consumers, of which one-third had to tried to purchase formula during the May 2022 infant formula shortage and of those consumers, 30% reported purchasing formula at multiple stores [
22]. A recent qualitative study by Sylvetsky and colleagues reported that parents spent hours searching for formula by driving from store to store and searching online during the May 2022 infant formula shortage [
20]. These data identify a high burden to parents and potentially those from low-income communities for which transportation and time are barriers in accessing food [
23].
Switching infant formula brands and types reduced infant quality of life and especially in infants that relied on specialty formulas. Approximately 60% parents who switched formulas reported that their infants had one or more problems in response to switching infant formulas. In a sub-group analysis, the number of infants that experienced problems in response to switching formulas was higher in infants requiring specialty formulas compared with infants that did not require specialty formulas. These data may be explained in part to the increased use of intact cow’s milk formula during the shortage. These observations are supported by Marino et al., that found two-thirds of parents whose infants relied on specialty formulas reported difficulties accessing these formulas during the COVID-19 pandemic [
18].
Parents relied on several resources to navigate the infant formula shortage with social media and healthcare providers (50%) as the most used resources followed by relatives or friends (43%) about one-third of parents used a lactation consultant or lactation counselor. These data are much lower compared with the CDC and FDA’s 2006
Infant Feeding Practices Study II (
IFPSII) in which about 80% of parents acquired information about infant feeding practices from healthcare professionals, followed by relatives or friends, and books or videos [
17]. Discrepancies in the data may result in the size and composition of each study. IFPSII enrolled a larger and more representative sample size of 2,000 women across the nation relative to this study’s smaller sample size of 178. The mean helpfulness scores of these resources were moderate with social media scoring the highest suggesting social media as a powerful tool for diet and health education and support and confirmed by other studies [
16,
20]. Parents’ mean helpfulness scores of future activities that would facilitate feeding infants in the “near future” include freedom to choose infant formula brands, health insurance coverage for infant formula, online resources describing formula types or brands that meet infants’ unique health needs and free universal prenatal lactation education and postpartum lactation support. These activities highlight facilitator that would address the barriers in infant feeding that are summarized in the word cloud.
Because exclusive human milk feeding is recommended for infants during the first six months of life, female parents were asked questions about their breastfeeding goals, experience, and support. Most (80.5%) female parents planned to exclusively breastfeed their infants, however 87% did not meet their exclusive breastfeeding goals. These data are fairly consistent with the CDC Breastfeeding Report Card for which most U.S. infants (84.1%) have ever consumed any breast milk but only 25% of infants meet the national recommendations of exclusive breastfeeding through 6 months of life [
24]. These data suggest that while most parents aim to meet national health recommendations to exclusively breastfeed their infants until 6 months of age, they are unable or choose not to. There are a several factors that explain why women are unable to meet their breastfeeding goals from lack of federal paid family and medical leave that prevent women from having the time and support to initiate and sustain breastfeeding; a lack of flexibility and privacy for mothers to breastfeed or pump while at work; and barriers in affording or accessing prenatal lactation education and postpartum lactation support which are not part of standard care [
25,
26,
27].
Female participants were asked about their experience with prenatal lactation education and postpartum lactation support. Approximately 50% of female parents participated in a prenatal breastfeeding support group or class and 35% of female parents participated in a postpartum breastfeeding support group or class. The helpfulness scores for these two activities were low (5.5 and 6.7, respectively), however, their mean helpfulness scores were higher (7.5 and 7.9, respectively) by female parents who did not participate in these activities. These data suggest there is a high unmet need for universal and free breastfeeding education and support that are critical for increasing breastfeeding intention, initiation, duration and exclusivity [
28,
29].
This is the first report of infant feeding outcomes and consumer behavior in response to the May 2022 infant formula shortage with different limitations and strengths. The limitations include the study design which was retrospective which is at risk for high recall errors. Specifically, parents completed the survey 7-8 months following the height of the May 2022 infant formula shortage. This may explain in part the fewer number of parents reporting use of unsafe infant feeding practices compared to a more recent prospective cross-sectional study in a similar population [
30]. Second, our target population included parents who subscribed to the Bobbie Labs listserv and limits the generalizability of the results. Nearly 80% of respondents were derived of largely white communities with annual household incomes equal to or greater than
$100,000, and not representative of U.S. families that were severely impacted by the infant formula shortage. Notably, our survey failed to capture many responses from individuals who represent families from low-income, black, and Hispanic communities that were hit the hardest by the shortage [
10]. There are also several strengths of this study. First, data from this cross-sectional study was collected from a large sample of parents who resided across the United States which improves the study’s generalizability. Second, nearly 90% of respondents reported being “extremely sure” about their answers choices regarding their infant’s feeding practices before and during the shortage demonstrating potential low recall biases. Additionally, 70% of parents answered the open-response question which suggests high engagement with the survey and a proxy for high-quality data. Finally, the survey collected a combination of categorical and continuous data on infant feeding, parental experiences and sentiments and infant outcomes that could identify areas in policy and educational strategies to assist families in averting future infant feeding crises. We propose a call to action to government, regulatory, health and workplace policies that prioritize infant feeding practices that deliver optimal nutrition, safety, and food security. First, the U.S. infant formula supply is controlled by U.S. trade and regulatory policies that result in a U.S. infant formula monopoly [
31]. High tariffs on formula thwart the import of infant formula to the U.S. and federal policies that govern the manufacture and labeling of infant formula exclude them from enter the U.S. legally [
4]. Systemic failures that reduce infant formula diversification and support a monopoly inequitably impacted low-income communities such as WIC recipients and nutritionally vulnerable infants [
4]. There is recent temporary solution with recent modifications to the Access to Baby Formula Act that becomes law in February 2024. This amendment to the Child Nutrition Act of 1966 will develop a waiver authority to address emergencies, disasters, and supply chain disruptions by ensuring WIC state offices can secure supplies from additional manufacturers outside of their contracts. Yet, this law is a stopgap and prevention of another feeding crisis will depend on systemic changes to healthcare policies that also protect the infant feeding system with access to banked donor milk and lactation education and support. The accessibility and growth of donor milk banking services are thwarted in part to a lack of federal public health policies that integrate donor milk banking or regulate its operations. Finally, the U.S. government and healthcare system should commit to implementing policies that prioritize lactation education and support. The suboptimal breastfeeding rates in the U.S. and within low-income communities are a result of a lack of federal paid family and medical leave; a lack of flexibility and privacy for mothers to breastfeed or pump while at work; and difficultly affording lactation services, which are not part of standard care. The future of individual, community and societal health rely on optimal early life nutrition that is resilient and equitable for all.
Author Contributions
Conceptualization, J.T.S.; methodology, J.T.S., K.C., D.M.D. and A.F.P.; investigation, J.T.S. and K.C.; formal analysis and visualization, J.T.S., K.C. and K.D-M.; interpretation of data, J.T.S., K.C., K.D-M., and M.W.; writing—original draft preparation, J.T.S., K.C., K.D-M., M.W.; writing—review and editing J.T.S., K.C., K.D-M., M.W., D.M.D. and A.F.P.; supervision and funding acquisition, J.T.S. All authors have read and agreed to the published version of the manuscript.