The functional endometrium and hematometra in a rudimentary non-communicating horn is an exceptional malformative condition [
1] found in 7-48% of cases of unicornuate uterus [
2]. The exact prevalence of Müller duct anomalies (MDA) remains unknown because of underdiagnosing and underreporting. Several patients are asymptomatic and remain undetected despite routine gynecologic screening and even following obstetric management for childbirth and delivery. Common complications of MDA include haematosalpinx, endometriosis, chronic pelvic pain, and adhesions, all secondary to retrograde menstruation [
3]. From the obstetric perspective, most patients have significant obstetric complications, rendering term deliveries exceptional [
4]. In asymptomatic women with occult MDA, the diagnosis is a challenging task during a routine gynecological examination. Detection of MDA is also a surgical challenge, making the preoperative imaging workup essential – ultrasound, hysteroscopy, and MRI [
5].
We present a very rare case of occult unicornuate right uterus with rudimentary non-communicating functioning left horn and its natural evolution following an initially incomplete surgical treatment.
A 30-year-old Caucasian female patient, with a previous term vaginal delivery seven years prior to the current presentation, was referred to our hospital for severe secondary dysmenorrhea and a painful, non-inflammatory, Pfannenstiel scar tumor with progressively increasing size with passing menses. The patient had undergone classic adnexectomy five years before for an emergency presentation interpreted as hematatosalpinx and left ovarian endometrioma at a local county hospital. Medical records describing the initial surgery were not available.
Upon clinical examination, we identified a firm abdominal wall mass of approximately 8/5 cm at the level of the Pfannenstiel scar, with a violaceous appearance, adherent to deep tissues, painful at palpation, and suggestive of parietal endometrioma.
Figure 1.
Clinical appearance and ultrasound evaluation. A) Pelvic examination was unremarkable, with a normally looking cervix. In the middle portion of the Pfannenstiel scar, a complex tumor, adherent to the deep planes, painful to palpation. B) Abdominal and three-dimensional transvaginal ultrasound revealed a right unicornuate uterus with proliferative endometrium and a thick-walled left pelvic mass measuring 5.5x7 cm, suggestive for hematometra in a non-communicating left horn (white arrow). C) Silhouette ultrasound reconstruction of the uterus describes a fistulous communication between the left uterine horn and the anterior abdominal wall mass, with characteristics pointing to an endometrioma. The right ovary had a common ultrasound appearance.
Figure 1.
Clinical appearance and ultrasound evaluation. A) Pelvic examination was unremarkable, with a normally looking cervix. In the middle portion of the Pfannenstiel scar, a complex tumor, adherent to the deep planes, painful to palpation. B) Abdominal and three-dimensional transvaginal ultrasound revealed a right unicornuate uterus with proliferative endometrium and a thick-walled left pelvic mass measuring 5.5x7 cm, suggestive for hematometra in a non-communicating left horn (white arrow). C) Silhouette ultrasound reconstruction of the uterus describes a fistulous communication between the left uterine horn and the anterior abdominal wall mass, with characteristics pointing to an endometrioma. The right ovary had a common ultrasound appearance.
A minimal fluid collection was noted in the Douglas pouch. Renal ultrasound confirmed a solitary right kidney.
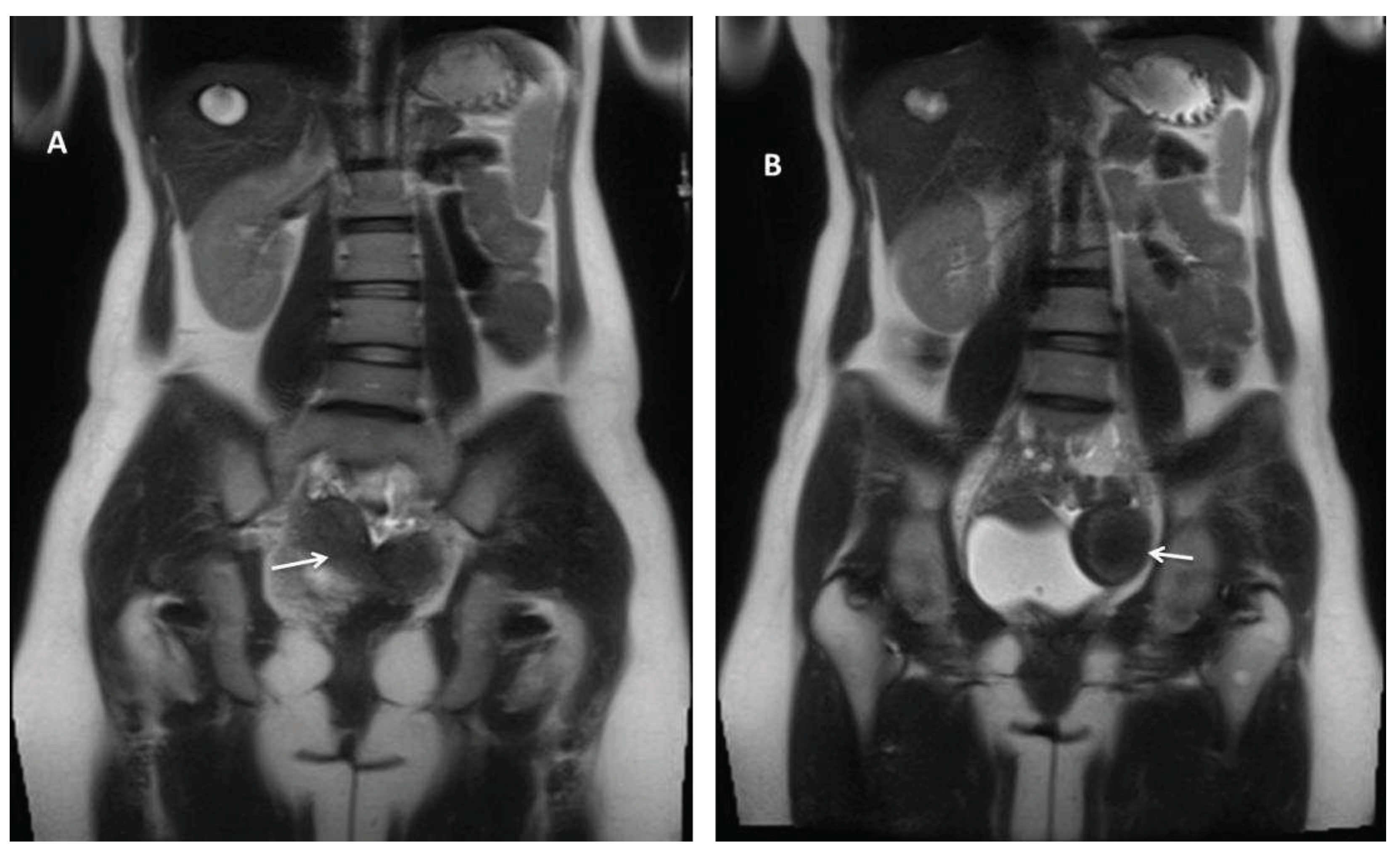
Figure 2.
Abdominal and pelvic MRI, coronal T2-weighted images. Pelvic magnetic resonance imaging (MRI) revealed: A) a normally looking right uterus (white arrow) and right ovary and B) a pelvic mass located mainly to the left (white arrow), measuring 47/63 mm, with similar enhancement to the uterus, advocating a Müllerian duct anomaly (MDA) type U4aC0V0 with large hematometra and solitary right kidney and absent left kidney.
Figure 2.
Abdominal and pelvic MRI, coronal T2-weighted images. Pelvic magnetic resonance imaging (MRI) revealed: A) a normally looking right uterus (white arrow) and right ovary and B) a pelvic mass located mainly to the left (white arrow), measuring 47/63 mm, with similar enhancement to the uterus, advocating a Müllerian duct anomaly (MDA) type U4aC0V0 with large hematometra and solitary right kidney and absent left kidney.
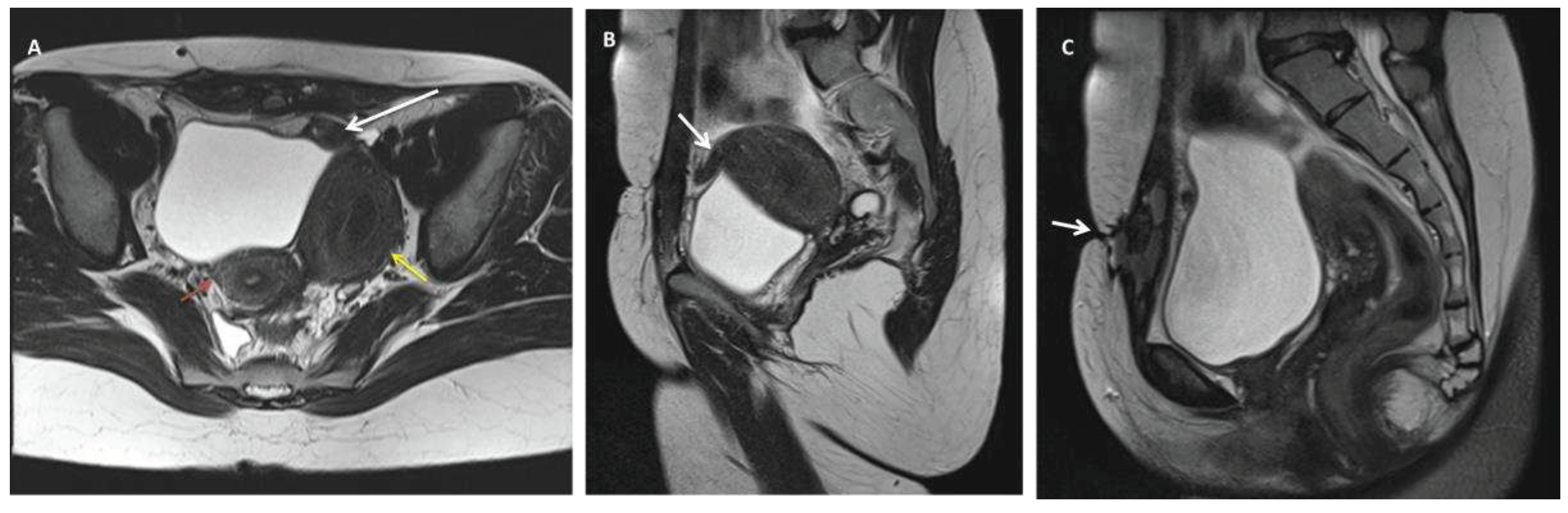
Figure 3.
Pelvic MRI T2 weighted images depicting: A fistulous tract between the left hemi-uterine fundus towards the urinary bladder (without its involvement), passing anteriorly through the rectus abdominis muscles, reaching the subcutaneous tissue and the tegument in the scar area. No other endometriosis lesions were noted, and the patient was classified as #Enzian (m) P0, O0/0, B0/0, C0, FU(0), FI (abdominal wall). A) Axial view of a unicornuate right uterus (red arrow) communicating with the cervix and large non-communicating cavitary left horn (U4a) with hematometria (yellow arrow). The white arrow is pointing to a fistulous trajectory towards anteriorly and medial, confirmed in B) sagittal view (white arrow), C) that drains in the rectus abdominis muscles and subcutaneous tissue, reaching the scar tegument (arrow).
Figure 3.
Pelvic MRI T2 weighted images depicting: A fistulous tract between the left hemi-uterine fundus towards the urinary bladder (without its involvement), passing anteriorly through the rectus abdominis muscles, reaching the subcutaneous tissue and the tegument in the scar area. No other endometriosis lesions were noted, and the patient was classified as #Enzian (m) P0, O0/0, B0/0, C0, FU(0), FI (abdominal wall). A) Axial view of a unicornuate right uterus (red arrow) communicating with the cervix and large non-communicating cavitary left horn (U4a) with hematometria (yellow arrow). The white arrow is pointing to a fistulous trajectory towards anteriorly and medial, confirmed in B) sagittal view (white arrow), C) that drains in the rectus abdominis muscles and subcutaneous tissue, reaching the scar tegument (arrow).
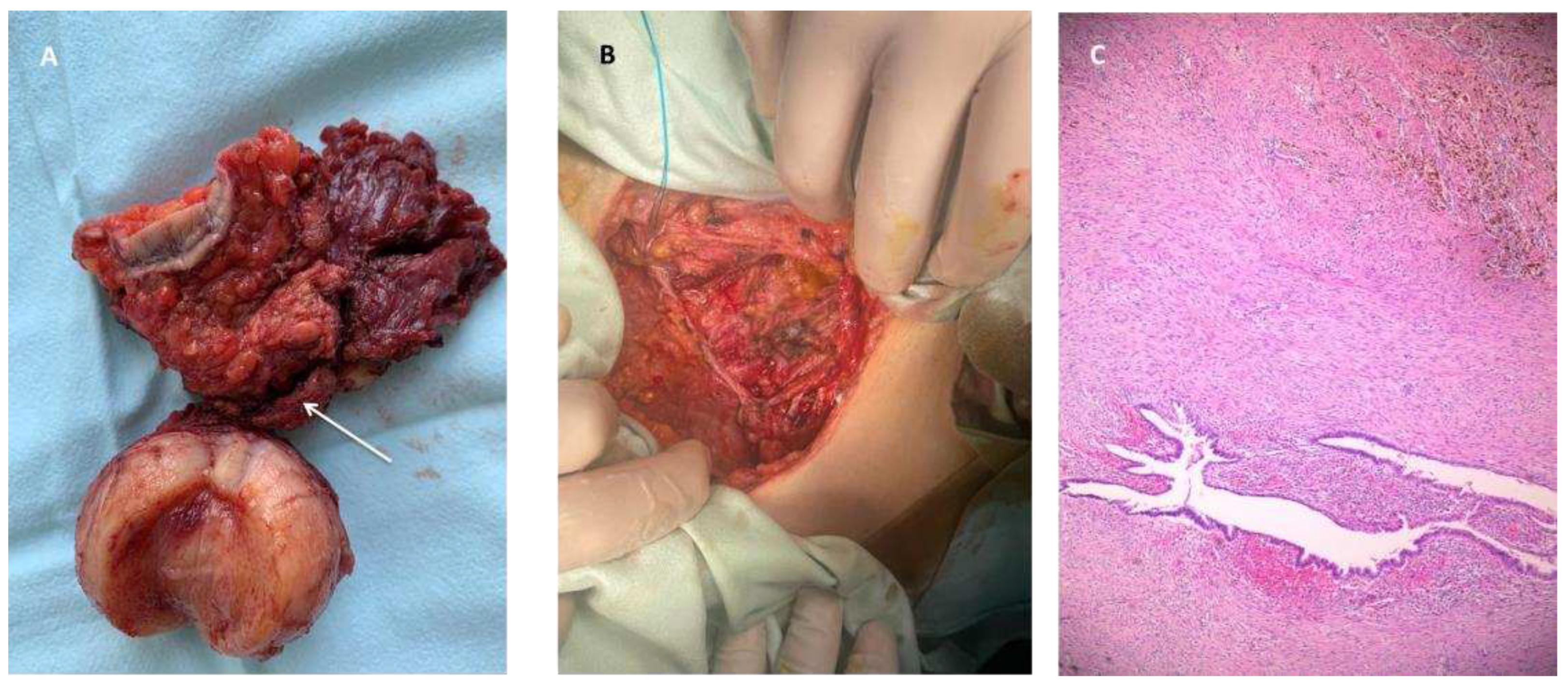
Figure 4.
Intraoperative and microscopic confirmation. Following patient counseling and approval, a laparotomy was performed. Intraoperatively, extensive adhesiolysis was required without evidence of other endometriotic lesions. The left non-communicating horn was resected together with the abdominal wall endometriosis lesions. The fascial defect was closed with a 10/10 cm low-weight polypropylene mesh. A) Surgical excision specimen. The arrow points to the fistulous trajectory from the rudimentary uterus (cut medially to demonstrate the endometrial cavity). B) Post-surgical excision fascial defect. C) HE 5X, depicting endometriosis lesions in the muscular tissue. Histopathological examination of the specimen confirmed adenomyosis in the rudimentary horn and abdominal wall endometriosis. The intraoperative and postoperative periods were uneventful. The patient was discharged on the 10th day.
Figure 4.
Intraoperative and microscopic confirmation. Following patient counseling and approval, a laparotomy was performed. Intraoperatively, extensive adhesiolysis was required without evidence of other endometriotic lesions. The left non-communicating horn was resected together with the abdominal wall endometriosis lesions. The fascial defect was closed with a 10/10 cm low-weight polypropylene mesh. A) Surgical excision specimen. The arrow points to the fistulous trajectory from the rudimentary uterus (cut medially to demonstrate the endometrial cavity). B) Post-surgical excision fascial defect. C) HE 5X, depicting endometriosis lesions in the muscular tissue. Histopathological examination of the specimen confirmed adenomyosis in the rudimentary horn and abdominal wall endometriosis. The intraoperative and postoperative periods were uneventful. The patient was discharged on the 10th day.
During the six-month follow-up period, there were no complications, and the patient had no complaints of dysmenorrhea or pelvic pain.
Conclusions
In the case of our patient, the unrecognized anomaly remained unresolved, favoring hematometra and later fistula formation in the weak spot of the uterine horn (potentially the tubal ostium). Abdominal wall endometriosis is otherwise the consequence of an ectopic endometrial implant at the site of prior cesarean delivery. The gold standard of care treatment is the resection of the rudimentary uterine horn to avoid unwanted medical consequences with a negative impact on the patient's quality of life.
Time should be taken to perform imaging investigations regardless the potential initial case presentation as an emergency, to refine diagnosis and ensure correct management. This would avoid improper and unwanted medical consequences and ensure a good quality of life for such patients.
Author Contributions
Conceptualization, G.C.; methodology, A.S.; investigation, A.F.; data curation, D.S.; writing—original draft preparation, G.N.; D.A.; writing—review and editing, D.M supervising and D.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
The patient signed a written consent before preparation of this manuscript.
Data Availability Statement
No new data was created.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Fedele L, Marchini M, Baglioni A, Carinelli S, Zamberletti D, Candiani GB. Endometrium of cavitary rudimentary horns in unicornuate uteri. Obstet Gynecol. 1990 Mar;75(3 Pt 1):437–40.
- Buttram VC, Gibbons WE. Müllerian anomalies: a proposed classification. (An analysis of 144 cases). Fertil Steril. 1979 Jul;32(1):40–6. [CrossRef]
- Acién P. Incidence of Müllerian defects in fertile and infertile women. Hum Reprod Oxf Engl. 1997 Jul;12(7):1372–6. [CrossRef]
- Donderwinkel PF, Dörr JP, Willemsen WN. The unicornuate uterus: clinical implications. Eur J Obstet Gynecol Reprod Biol. 1992 Nov 19;47(2):135–9. [CrossRef]
- Gitas G, Eckhoff K, Rody A, Ertan AK, Baum S, Hoffmans E, et al. An unprecedented occult non-communicating rudimentary uterine horn treated with laparoscopic excision and preservation of both fallopian tubes: a case report and review of the literature. J Med Case Reports. 2021 Feb 4;15(1):51. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).