1 G. Ya. Remishevskaya Republican Clinical Hospital, Abakan, Russia, ruslanmellin@mail.ru (R.M.).
2 I.M. Sechenov First Moscow State Medical University, Moscow 119435, Russia; linavel83@gmail.com (E.V.); dydykin_ss@mail.ru (S.D.); maltseva_l_d@staff.sechenov.ru (M.D.); vasilev_yu_l@staff.sechenov.ru (Y.V.)
1. Introduction
Anthropogenic impact on the habitat of especially large carnivores leads to deterioration of conditions for stability of their prey base. This has a negative impact on people in the vicinity of habitats of large predatory mammals. Attacks of large wild animals on humans occur not only during a chance encounter in the wilderness. According to the observations of various authors, the most dangerous for human’s representatives of wildlife belong to the families Canidae, Felidae and Ursidae [
1]. According to
https://worldanimalfoundation.org/ globally, the average number of annual bear attacks on humans is 39.6, of which North America has 11.4 attacks and Europe has 18.2 at-tacks annually [
2]. In the 2000s, 46 bear attacks resulting in 48 fatalities were reported in North America. Of these, there were 25 fatal attacks by black bears and 21 by brown bears. Of these incidents, 19 were occurred in Canada and 27 in the United States. In Alaska, there were 8 fatal bear attacks in-volving 10 people between 2000 and 2017. During the same period, the proportion of Alaska accidents to all fatal attacks in the U.S. was 29.6%, which was 17.4% of all fatal attacks in North America. The number of fatalities in the state of Alaska out of all bear fatalities in the U.S. is 34.5% and out of all bear fatalities in North America is 20.8% [
3]. In Russia, according to statistical data from the Komi Republic, 98 cases of human encounters with brown bears were registered in 2019 alone. During the period 1999-2020 in this re-public bear attacks on humans (wounded/killed) amounted to 4.8% of the forms of bear activity in populated areas. At the same time, no unified statistics on accidents caused by human-bear encounters were found in the literature [
4,
5]. In China, 1.28% of cases in which bears inflicted harm resulted in human injuries [
6]. In Russia, Canada, and the United States, the bear-human conflict remains highly tense [
1,
2,
3,
4,
5], which is manifested not only by human deaths, but also by severe combined injuries, com-plicated by the development of shock, septic inflammation, and risks of rabies and tetanus infection [
7,
8,
9,
10]. This article presents a case report of a bear attack on a human, because of which the victim survived.
2. Materials and Methods
Patient S., 42 years old, was taken by air ambulance to the maxillofacial and plastic surgery department.
Case history
According to the reports of the air ambulance doctor and the victim, the latter was injured in the forest. On 18.09.2023 at 11:00 a.m., a wild bear attacked the person while he was harvesting pine nuts. According to the patient, first the bear had gnawed through his left hand, which the man used to cover his face, then pressed his body to the ground with a paw and started gnawing his face. Then the animal tried to open the cerebral part of the cranium, which was evidenced by 4 furrows from the canines, 2 each on the frontal and 2 on the occipital bones of the skull. The man remained conscious during the fight. After the victim had stopped resisting, the bear left him. After waiting for about 10 minutes, he got up on his own, made sure that there was no predator nearby and went to the side of the camp. A helicopter with rescue service was called there. After 9 hours and 30 minutes the patient was taken to the reception department of the Republican Clinical Hospital of Abakan. Spiral computed tomography of the whole body was performed. The patient was examined by the on-duty intensive care physician (traumatic, hemorrhagic shock was diagnosed), traumatologist (open fractures of the left upper limb were diagnosed), neurosurgeon (craniocerebral trauma was excluded), general surgeon (trauma of internal organs was excluded, multiple bite wounds of the trunk and extremities were diagnosed), and maxillofacial surgeon. Due to significant damage to the bones and soft tissues of the maxillofacial region, a decision was made to hospitalize the patient in the department of maxillofacial and plastic surgery. The patient was prophylactically injected with the following vaccines: antirabic culture vaccine concentrated purified inactivated COCAV (Microgen, Russia), tetanus anatoxin purified adsorbed liquid, AC-anatoxin (Microgen, Russia)
Objective examination findings
External examination revealed facial configuration disorder due to multiple wounds: bite wounds of the frontal, periorbital regions on both sides, suborbital, zygomatic, nasal wing on the right side, parotid region on the left side, upper and lower lips. Scalped wound of the occipital region. The wounds had contamination in the form of sand, hay, pine needles, grass, leaves, dead insects (
Figure 1). In the buccal-zygomatic region on the right side, the wound had a flap character with penetration into the oral cavity. At the bottom of the wound, the following were visualized: partially disconnected facial nerve; parotid salivary gland (the salivary duct of the gland was not visualized); mimic muscles with integrity disorders; fragments of the maxilla with teeth; fragments of the zygomatic bone. The right zygomatic bone was broken, its fracture was splintering with significant displacement of fragments. The nasal region was also visualized through the wound, the integrity of the bones of which was also broken. The wound in the left parotid region had a semi-lunar shape, the bottom of the wound was represented by the parotid salivary gland. In the oral cavity, the mucous membrane of the palate was torn into several parts. Due to the contamination of the wounds, it was not possible to determine their direction. Both maxillary sinuses had a connection with the oral cavity due to the detachment of the alveolar process. The alveolar and partially palatine processes of the maxilla were lying loose on the tongue and had no connection with the mucous membrane of the maxilla. The frontal part of the alveolar process together with teeth 1.1, 2.1 was rotated and displaced to the soft tissues of the left cheek. The mucous membrane of the cheeks and the oral vestibule had multiple flap wounds interacting with the external environment (
Figure 1A)
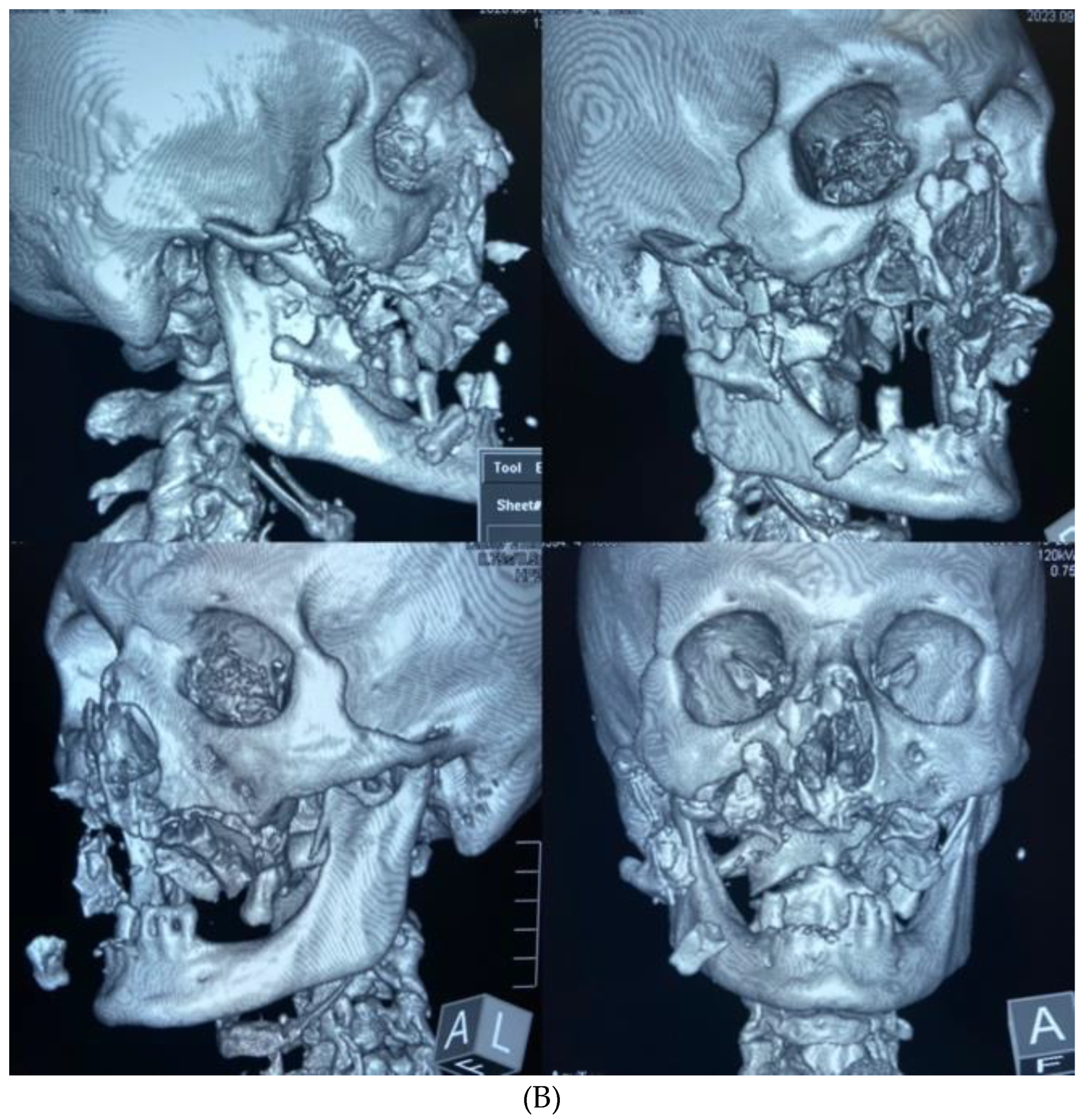
According to the spiral CT scan of 18.09.2023 #12905: No foci of pathological density were detected in the brain substance. Lateral ventricles were not dilated, symmetrical. The sub-arachnoid space was moderately dilated. No displacement of medial brain structures was revealed. The area of the Turkish saddle was unchanged. Fracture of the right zygomatic arch with angular displacement was detected. There was multifocal fracture of the alveolar process of the maxilla on the left side with displacement of bone fragments to the inside and downward and multifocal fracture of the anterior, inferior, and lateral walls of the right maxillary sinus with displacement of bone fragments into the sinus cavity up to 18 mm and laterally. Fracture of the lower wall of the left maxillary sinus (hemorrhagic substrate up to 5 mm thick in the cavity) was also found. Splinter fracture of the nasal bones with displacement was detected. Fracture of the coronary process of the mandible on the left side with moderate displacement was revealed. A large amount of free gas was detected subcutaneously in the soft tis-sues of the face on both sides, more significantly on the right side, right occipital and both parietal regions (
Figure 1B). Cervical spine, thoracic spine: No bone traumatic pathology was detected. Degenerative-dystrophic changes in the cervical and thoracic spine were found. Chest X-ray: Lungs were spread, there were no focal and infiltrative shadows. Pleural cavities were clear. There was no traumatic bone pathology at the level of scanning. Abdominal radiography: No free gas and fluid in the abdominal cavity and pelvic cavity. There was no traumatic pathology on the side of parenchymatous organs. Conclusion: Multiple fragmentary fractures of the facial skeleton with displacement of bone fragments. Subcutaneous emphysema of soft tissues of the face, parietal and right occipital regions. Paranasal sinus hemorrhage on the left side
A diagnosis has been made:
Multiple bite injuries to the face. Fracture of the zygomatic bone on the right side with displacement. Traumatic amputation of the maxilla on the right according to Le Fort fractures type II, on the left according to Le Fort fractures type I. Splinter fracture of the nasal bones with dis-placement. Multiple bite wounds of the face without soft tissue defects. Detachment of the left superior rectus muscle. Rupture of the Stenon's duct on the right. Paresis of the facial nerve on the right. Scalp wound of the occipital region. Multiple bite wounds of the trunk and extremities. Open multifocal fracture of the lower third of the left humerus. Open fracture of the base of 1-2 metacarpal bones on the left side.
NA02.8 Multiple fractures of the skull or facial bones
3. Results
The operation was divided into 5 steps:
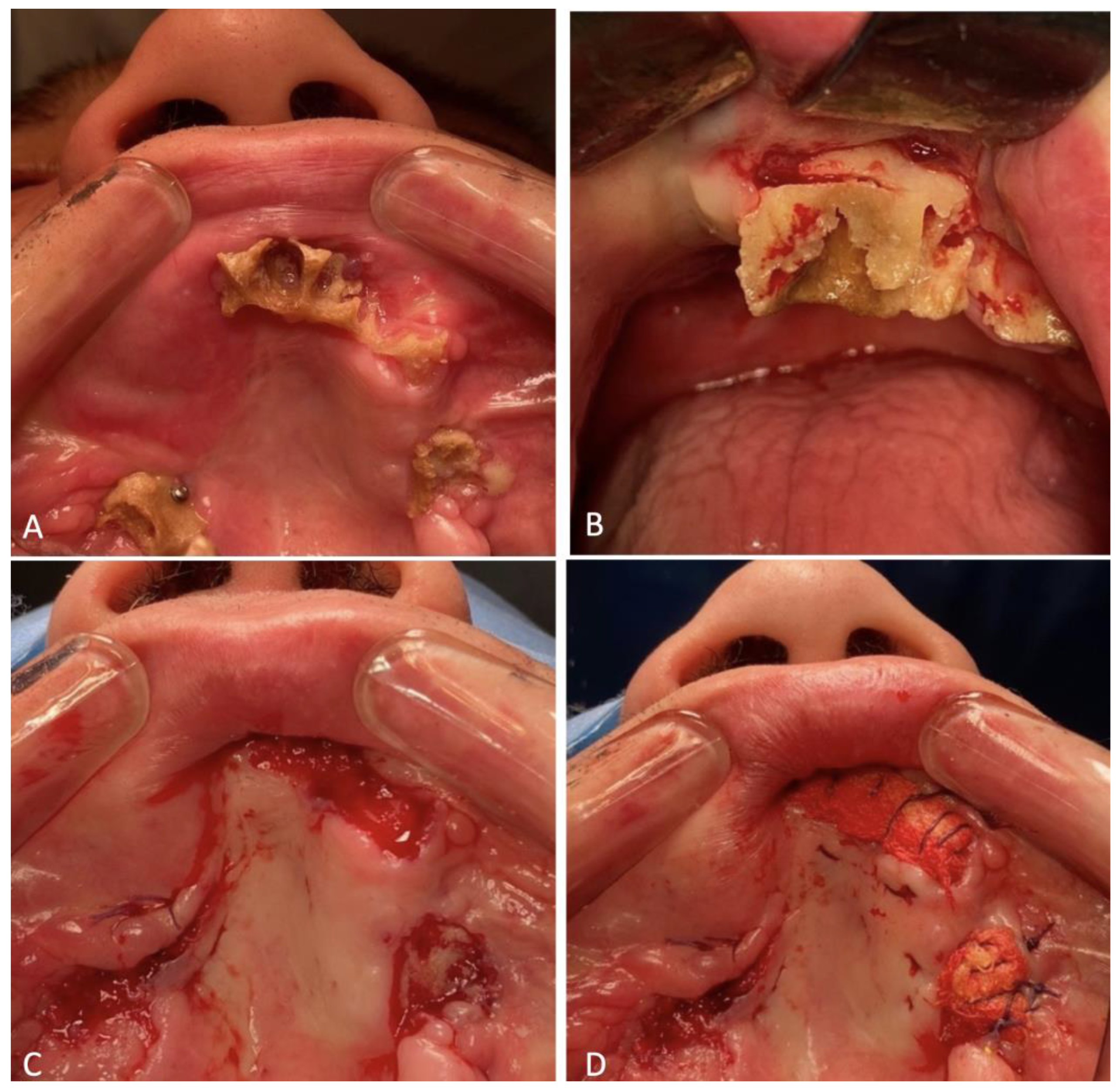
The first step was an initial surgical debridement. Foreign bodies were removed: leaves, pine needles, grass, teeth of the upper and lower jaws with small fragments of bones of the maxilla (
Figure 2).
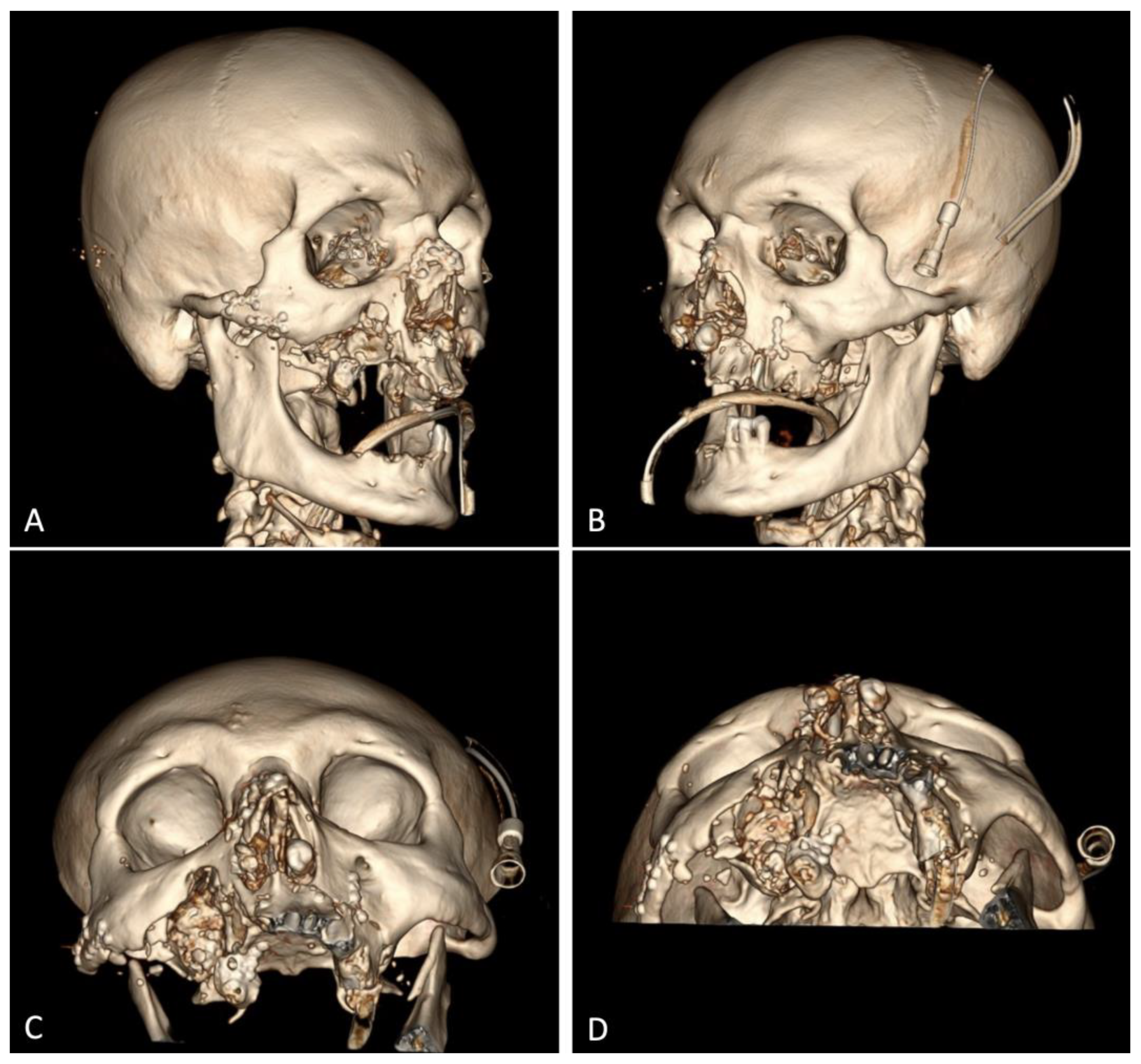
The second step: reconstruction of the facial skeleton.
Due to good visualization of the right zygomatic bone through the existing wound, repositioning and osteosynthesis with micro-plates and micro-screws manufactured by "Konmet" (Moscow, Russia) were performed. The displaced and rotated bones of the nasal dorsum were also placed in the anatomical position, and fixation with microplates and micro-screws was performed (
Figure 3).
The third step was oral reconstruction.
Loose-lying fragments of the maxillary alveolar process were removed from the soft tis-sues of the face. Three of them were of value due to their large size and anatomically important landmarks for subsequent reconstructive surgeries: 2 maxillary tubers and the frontal part of the alveolar process with teeth 1.1, 2.1 remained in it. The maxillary tubers were fixed on microplates and micro screws, the anterior segment on 2 mini-screws (
Figure 4). Excision of the crushed, in some places necrotized oral mucosa was performed. The paranasal sinuses were tamponaded through the fenestration of the maxillary sinuses with the oral cavity with the help of a nasal pack moistened with iodoform. The ends of the nasal packs were led out through the artificially formed junctions in the lower nasal passages from both sides. Plastic of the buccal mucosa was performed so that the flaps completely covered the fixed fragments of the maxilla. In the frontal section, the fixed bone fragment remained open when the surviving mucosa was brought together. The diastasis between the edges of the mucous membrane was about 1.0*1.7 cm. A decision was made to suture a nasal pack moistened with iodoform on the open bone area. The wounds of the lips were sutured, which made it possible to separate the oral cavity from the external part of the wound.
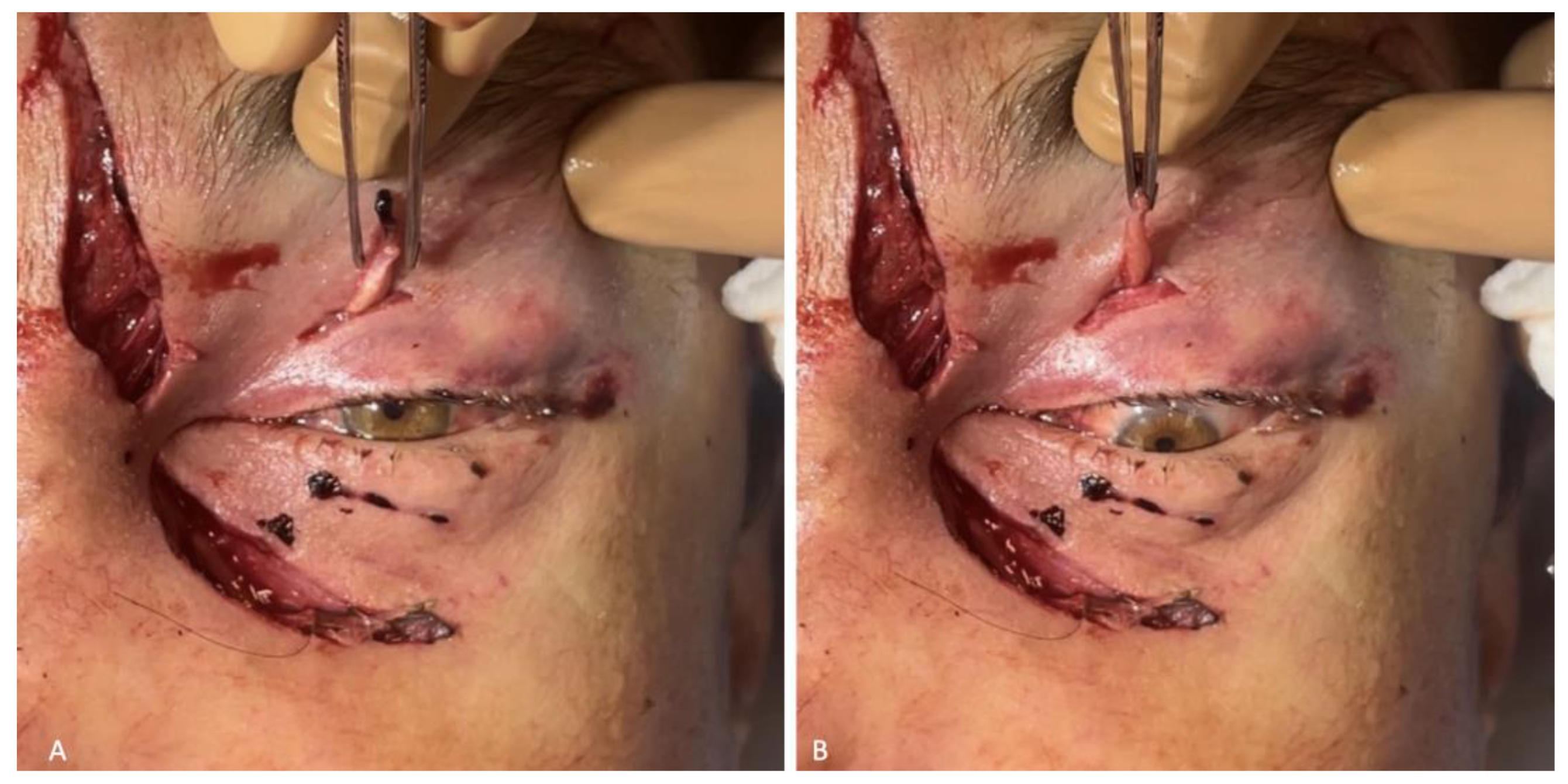
The fourth step was oculomotor function repair.
In the initial surgical debridement of facial wounds, a 0.7 cm long wound was found around the left upper eyelid. From the wound there was a formation dangling outward that looks like a tendon with a muscle. Having examined the muscle: when pulling it by its outer end, the pupil of the eye turned downward (
Figure 5). The stump of the left eye superior rectus muscle was fixed to the tarsal plate of the left upper eyelid. The skin was sutured with Surgic Pro 4/0 interrupted stitches.
When examining the patient on the first day after surgery, the eyes moved in all directions, symmetrically.
Step 5: the integrity of soft tissues of the face and scalp was restored.
This stage took 2/3 of the total operation time. The capsules of parotid glands, muscles and subcutaneous fatty tissue were sutured layer by layer with Vicryl 4/0. Surgic Pro 4/0 interrupted stitches were applied to the skin (
Figure 6). The wounds were drained with glove tapes. During the operation the patient underwent transfusion 686 ml of erythrocyte mass and 580 ml fresh frozen plasma.
To monitor vital functions, correct posthemorrhagic anemia (1350 ml erythrocyte mass was transfused during the period of stay in the Department of Anesthesiology and Reanimation (DAR)) and control the urinary function of the kidneys after surgery, the patient was transferred to the DAR on an artificial pulmonary ventilation machine. On the morning of the next day, he was taken off the ventilator for independent breathing through a naso-tracheal tube, later that day extubation was performed according to the indications. A naso-gastric tube was installed in the patient for nutrition. To prevent the development of salivary fistulas, atropine sulfate solution (0.1%, 5 drops 30 minutes before oral intake 3 times a day) was administered to inhibit the functions of salivary glands.
On the 8th day after stabilization of the state and normalization of renal excretory function, the patient was transferred from DAR to the specialized department. To prevent infection of the oral cavity wounds, the patient was left to eat through a naso-gastric tube. At the stage of postoperative treatment, the patient developed salivary fistulas in parotid salivary gland wounds, which closed independently on the 15th day from the moment of injury. Atropine sulfate administration was canceled. Due to the divergence of sutures in the projection of the alveolar process of the maxilla on both sides and to prevent the formation of oro-antral fistulas on the 16th day a repeated operation of plastic of the oral mucosa under endotracheal anesthesia was performed, the surgical sutures were additionally closed with nasal packs moistened with iodoform. The nasal packs were sutured to the oral mucosa. The previously installed nasal packs were removed from maxillary sinuses. On the 23rd day the patient was discharged in satisfactory condition for outpatient treatment.
Figure 7.
Patient's face after 1 month: A - full-face view; B - profile view.
Figure 7.
Patient's face after 1 month: A - full-face view; B - profile view.
On 27.11.2023 for the formation of normotrophic scars a course of scar treatment with neodymium laser of DEKA company with two nozzles (7mm 20-50 J/cm2 and 10mm 40 J/cm2) was performed by a cosmetologist (
Figure 8).
A pharmacy preparation based on a heterogeneous composition consisting of microparticles of "cross-linked" collagen of animal origin placed in a gel identical to the natural extracellular matrix was injected into the scar area (
Figure 9).
On 12.12.2023, the patient was rehospitalized to the maxillofacial and plastic surgery department in a planned procedure with the diagnosis: chronic posttraumatic osteomyelitis of the maxilla.
Osteonecrectomy was performed on 13.12.2023. Previously installed micro-screws and micro-plates fixing the maxillary tuber on the right side were removed. Ultrasonic surgical apparatus used to remove nonviable parts of the maxilla. Ribbon gauzes impregnated with iodoform were placed on the formed bone wounds. The latter were sutured to the oral mucosa (
Figure 10).
To date, the patient has completely lost chewing function and has a marked facial expression disorder on the right side of the face. The next stages of treatment will be the masticatory function repair and rehabilitation of the affected facial nerve. A peroneal graft will be transplanted to the midface to replace the missing alveolar process of the maxilla for further prosthetics with dental implants. (Fig11)
Figure 11.
Patient's face after 2.5 months: A - full-face; B - 2/3 view.
Figure 11.
Patient's face after 2.5 months: A - full-face; B - 2/3 view.
4. Discussion
According to the National Park Service, the risk of bear attack is 1 in 2.7 million visits to protected areas [
2,
10]. In the presented case, an unexpected encounter between a human and a bear occurred during daytime in September during harvesting pine nuts. This resulted in an attack of the predatory animal on the victim. According to Bombieri, G., Naves, J., Penteriani, V. et al. (2019) 50% of bear attacks on humans are just carried out during leisure activities in the forest such as picking berries, mushrooms, etc. Interestingly, bears attack adults in 99% of cases, of which 88% are males. In 63% of cases, the victims are unaccompanied in the forest [
5]. In our case, the male victim was also alone in the forest.
According to different authors, the frequency of bear encounters and attacks on humans is seasonal [
2,
4,
6,
11,
12]. The highest number of cases is recorded from May to October. According to a research paper presented by Cimpoca, A. and Voiculescu, M. (2022), the maximum number of bear sightings near humans is observed in summer (39.6% of all cases), less in autumn (28.3% of all cases), then in spring and winter (16.9% and 15.1% of all cases, respectively) [
11]. According to Korolev A.N. (2022), 55.5% of human encounters with bears are occurred in August-October, while May-June accounted for 30.2% of cases [
4]. According to Dai Y., Hacker C.E., Zhang Y., et al. (2019) 48.85% of bear intrusions into human dwellings are happened in summer, 42.38% in autumn, and only 5.72% in spring [
6]. This correlates with Bombieri, G., Naves, J., Penteriani, V. et al. (2019) data on the frequency of bear attacks on humans worldwide: 48% of the incidents are occurred during summer [
5]. The maximum number of bear attacks on humans according to the community data
https://blog.batchgeo.com/bear-attack-statistics/ had been happened in August (32 attacks), then equal in July, September, and October (28 attacks in each month), then June (22 attacks) and May (17 attacks) [
12]. The majority of attacks (73-97%) are occurred during the daytime [
5,
13].
Because of a bear attack, a person receives multiple injuries, the localization of which necessarily includes the head [
9,
10,
13,
14,
15,
16]. In the presented clinical case, the victim was found to have multiple bite injuries to the face, fractures of the nasal bones, zygomatic bone, maxilla, as well as detachment of the upper rectus muscle of the left eye, rupture of the Stenon's duct, paresis of the facial nerve, and a scalp wound of the occipital region. According to the data presented by Rasool A., Wani A.H., Darzi M.A., et al (2010), among the body injuries of bear attack victims 80.57% are facial injuries, 54.67% are head injuries and all victims have bite and laceration wounds of various localizations [
13]. According to Kar I.B., Chopda P.D., Mishra N., et al. (2016) facial injuries are occured in 80, 57% of victims. Fractures of facial bones in 45% include injuries to the mandible, 35% to the zygomatic bone, 20% to the maxilla and 10% to the nasal bones. 15% of victims have damage to the eyeball, which subsequently leads to visual impairment or loss [
15]. Mean-while, according to Ghezta N.K., Bhardwaj Y., Ram R., et al (2019) fractures of midface bones account for 71% and mandible bones 24% of all facial skull fractures [
16]. It is possible that bears injure the face of their victims because of the odor emanating from exposed body parts and the greater temperature of oral tissues than in other, less vascularized external body parts. This feature may reflect the behavior of a hungry predator. This is consistent with the findings of Maurer et al (2023) who noted the prevalence of trauma to parts of the face such as the perioral and periorbital regions, ear, and nose.
5. Conclusions
Multiple injuries of the facial part of the skull lead to the formation of large wound gates for infection, and complicate visual assessment of the volume of damage and access for interventions under anesthesia.
A comprehensive approach to treatment tactics in case of extensive injuries of bone and soft tissue structures of the maxillofacial region significantly reduce the patient's rehabilitation time and further increase the chances of complete elimination of both aesthetic and functional disorders.
Author Contributions
Conceptualization, R.M.; methodology, E.V., R.M.; software, R.M., L.M.; validation, L.M., S.D.; formal analysis, Y.V.; investigation, R.M., S.D.; resources, R.M.; data curation,Y.V.; writing—original draft preparation, E.V., L.M.; writing—review and editing, E.V., Y.V.; visualization, R.M., Y.V.; supervision, Y.V.; project administration, S.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by Sechenov university, Moscow, Russia (Approval Code:16-23; Approval Date: 15/09/2023).
Informed Consent Statement
Informed consent was obtained from subject involved in the clinical case study. Written informed consent has been obtained from the patient(s) to publish this paper” if applicable.
Acknowledgments
maxillofacial surgeon Podgornaya Natalia, traumatologist-orthopedist Martsevich Dmitry, anesthesiologist-resuscitator Ananyevskaya Valeria, radiologist Kondrashova Ksenia, operating nurse Erbes Tatyana.
Conflicts of Interest
authors declare no conflicts of interest.
References
- Puchkovskiy, S.V. Human - large predatory mammals conflict dynamics. Bulletin of Udmurt University. Series "Biology. Geosciences. 2018, 1, 32–41. [Google Scholar]
- https://worldanimalfoundation.org/advocate/bear-attacks-statistics/.
- https://www.alaskasnewssource.com/content/news/MAP-Fatal-Bear-Attacks-in-North-America-432734333.
- Korolev A., N. The human-bear conflict in the Komi Republic: manifestation dynamics and regional features. Trudy Karel’skogo nauchnogo tsentra RAN = Transactionsof the Karelian Research Centre RAS. 2022, 8, 5–19. [Google Scholar] [CrossRef]
- Bombieri, G. , Naves, J., Penteriani, V. et al. Brown bear attacks on humans: a worldwide perspective. Sci Rep 2019, 9, 8573. [Google Scholar] [CrossRef] [PubMed]
- Dai Y, Hacker CE, Zhang Y, Li W, Li J, Zhang Y, Bona G, Liu H, Li Y, Xue Y, Li D. Identifying the risk regions of house break-ins caused by Tibetan brown bears (Ursus arctos pruinosus) in the Sanjiangyuan region, China. Ecol Evol. 2019, 9, 13979–13990. [Google Scholar] [CrossRef] [PubMed]
- Singh PK, Ali SM, Radhakrishnan RV, Mohanty CR, Sahu MR, Patro BP, Ms I, Panda SK. Pattern of injuries due to wild animal attack among patients presenting to the emergency department: A retrospective observational study. Chin J Traumatol. 2021, 24, 383–388. [Google Scholar] [CrossRef]
- Feng Y, Ma J, Sun S, Chi L, Kou Z, Tu C. Epidemiology of Animal Rabies - China, 2010-2020. China CDC Wkly. 2021, 3, 815–818. [CrossRef] [PubMed]
- Cassone M, Vollmer T, Factor M, Sallade TD. Polytrauma from a north american black bear attack. Wilderness Environ Med. 2020, 31, 457–461. [Google Scholar] [CrossRef]
- Ingram BM, Colosimo CM, Weaver JS, Mentzer CJ, Yon JR. Reconstruction after grizzly bear attack in wyoming. Am Surg. 2023, 89, 2780–2781. [Google Scholar] [CrossRef] [PubMed]
- Cimpoca, A. Voiculescu M. Patterns of Human–Brown Bear Conflict in the Urban Area of Brașov, Romania. Sustainability 2022, 14, 7833. [Google Scholar] [CrossRef]
- https://blog.batchgeo.
- Rasool A, Wani AH, Darzi MA, Zaroo MI, Iqbal S, Bashir SA, Rashid S, Lone RA. Incidence and pattern of bear maul injuries in Kashmir. Injury. 2010, 41, 116–9. [Google Scholar] [CrossRef]
- Petrushin, A.L. , Matveev R.P., Minkin A.U., Fedotov S.N., Tishchenko A.I., Kudrin N.F., Freze Yu.A. Features of damage affected on human beings by brown bears in natural environment. Human ecology. 2008, 7, 14–17. [Google Scholar]
- Kar IB, Chopda PD, Mishra N, Sethi AK, Mahavoi BR. Management of maxillofacial injuries in bear mauling cases: a review of 20 cases. J Korean Assoc Oral Maxillofac Surg. 2016, 42, 13–9. [Google Scholar] [CrossRef] [PubMed]
- Ghezta NK, Bhardwaj Y, Ram R, Ahsan R, Arya S. Incidence pattern of bear-inflicted injuries to the maxillofacial region-soft and hard tissue injuries, their management, and sequelae. J Oral Maxillofac Surg. 2019, 77, 1043.e1–1043.e15. [Google Scholar] [CrossRef]
- Maurer M, Schlipköter C, Gottsauner M, Waiss W, Meier JK, Fiedler M, Schuderer JG, Taxis J, Reichert TE, Ettl T. Animal bite injuries to the face: a retrospective evaluation of 111 cases. J Clin Med. 2023, 12, 6942. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).