Submitted:
31 January 2024
Posted:
01 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
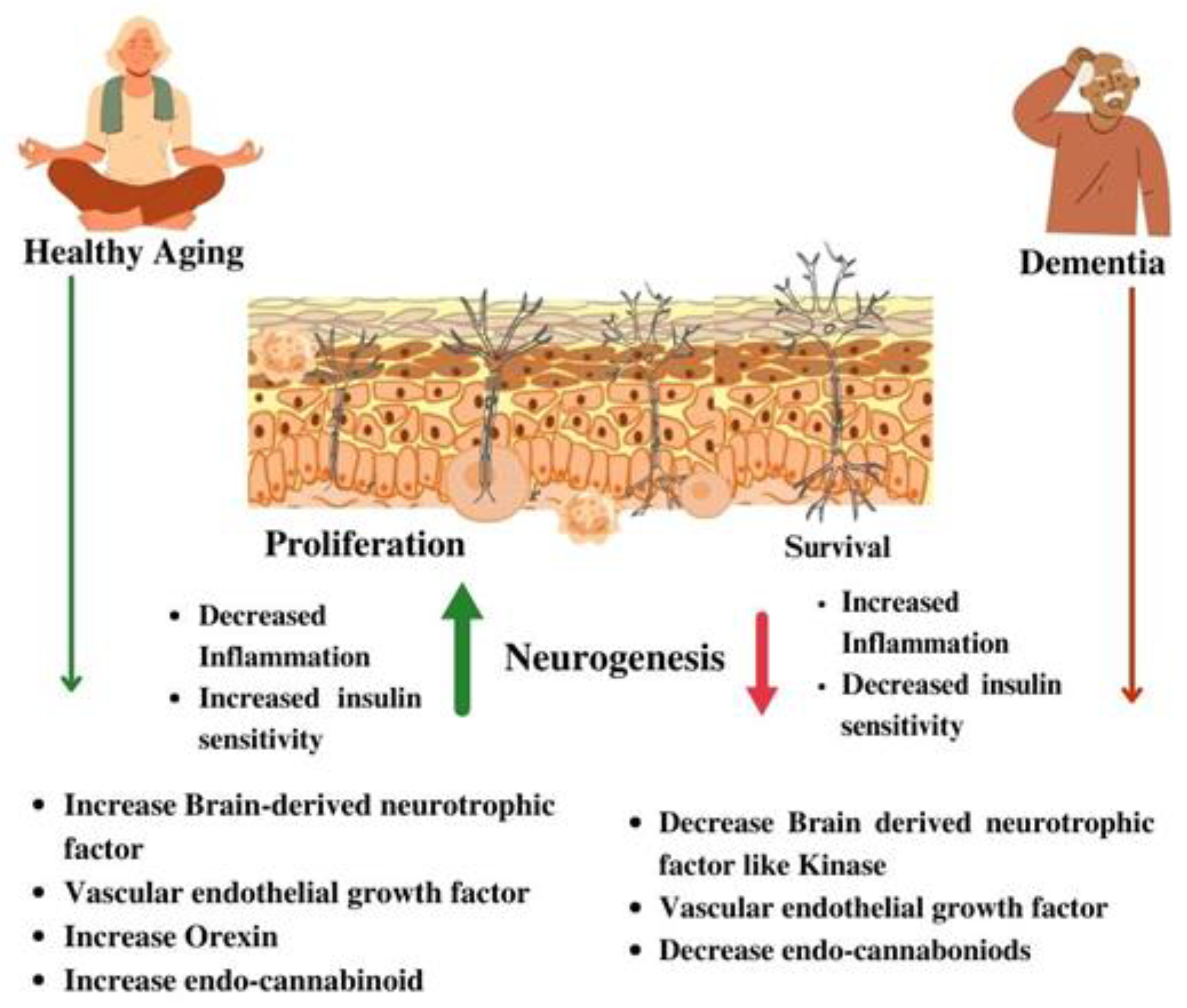
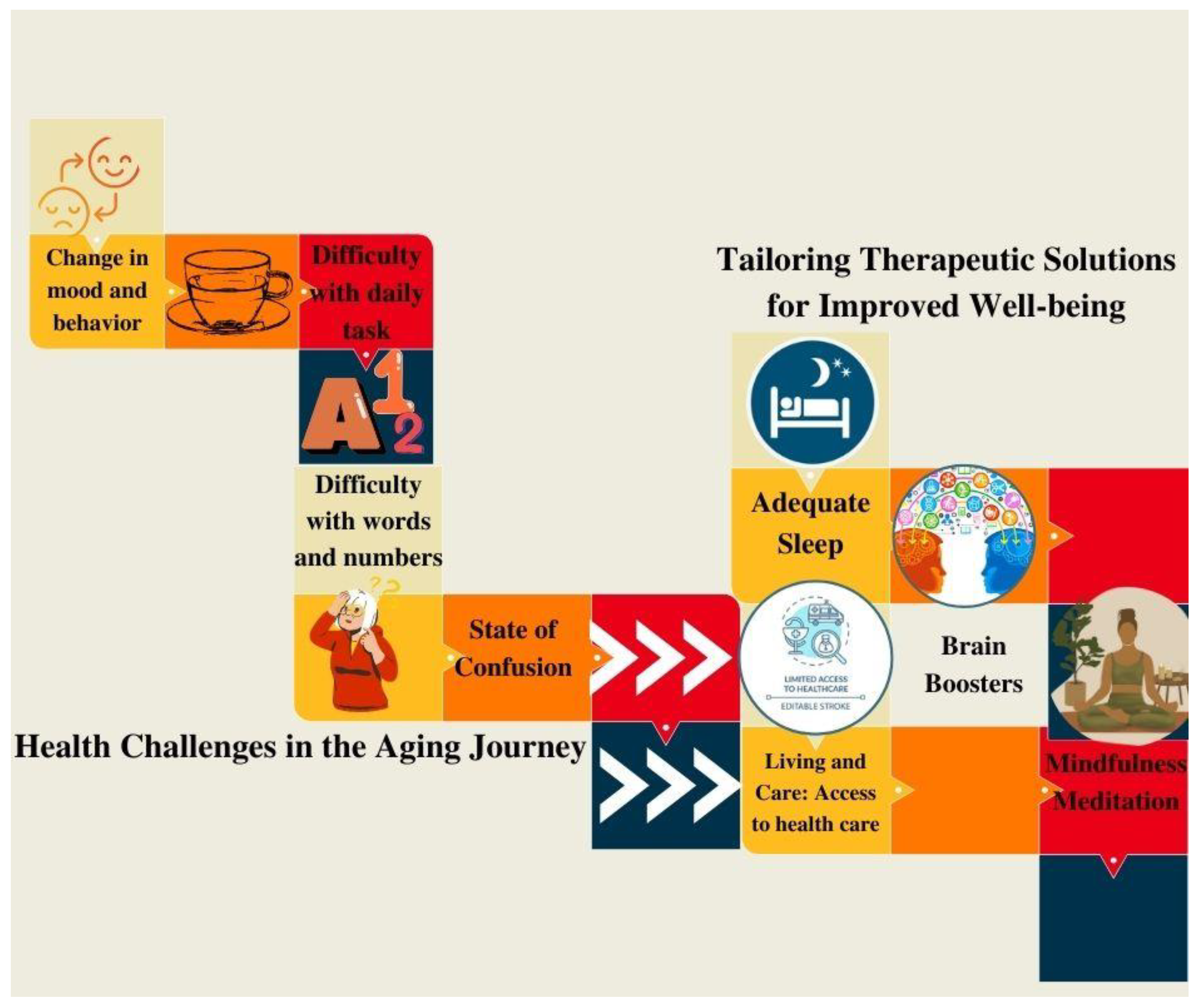
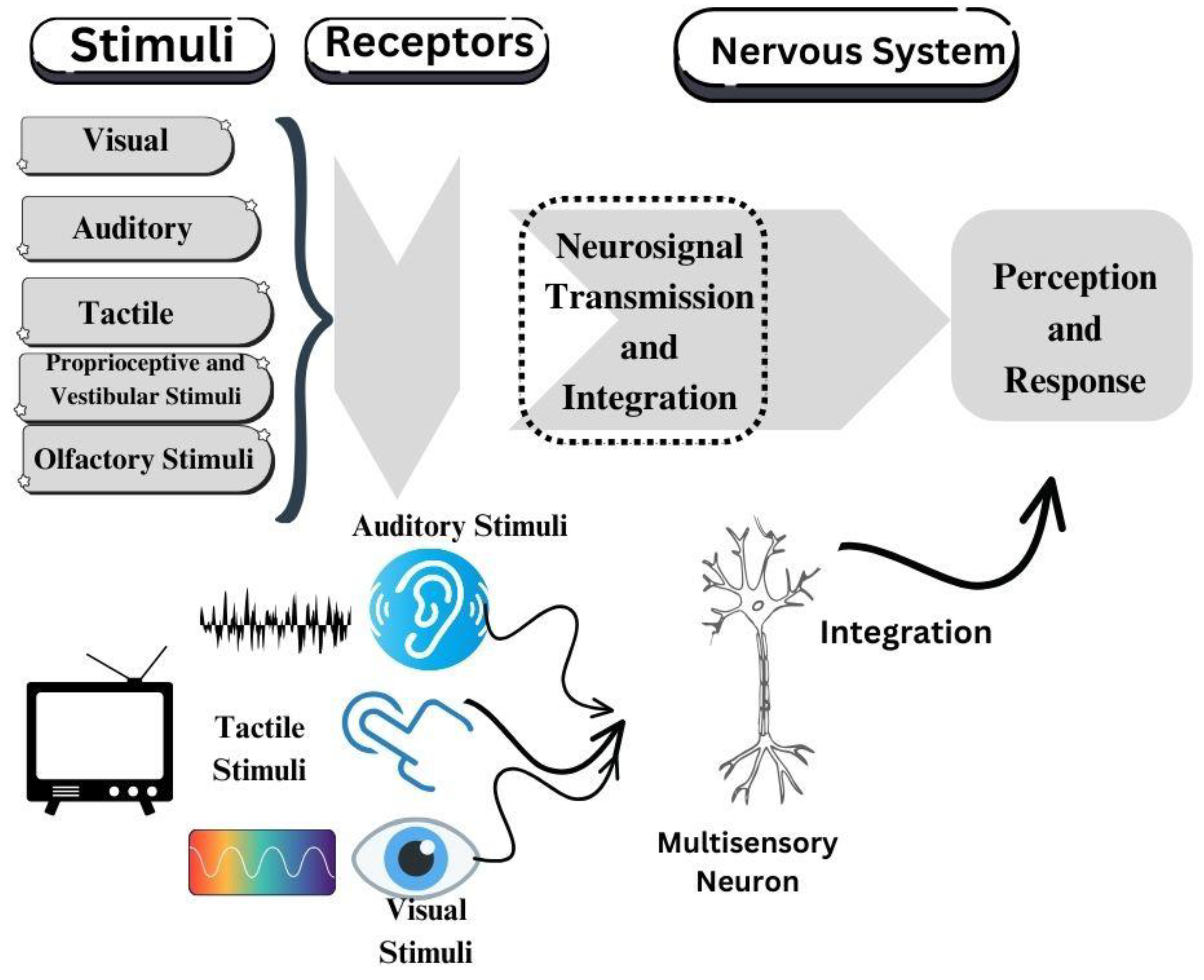
2. Understanding Sensory Needs in Aging
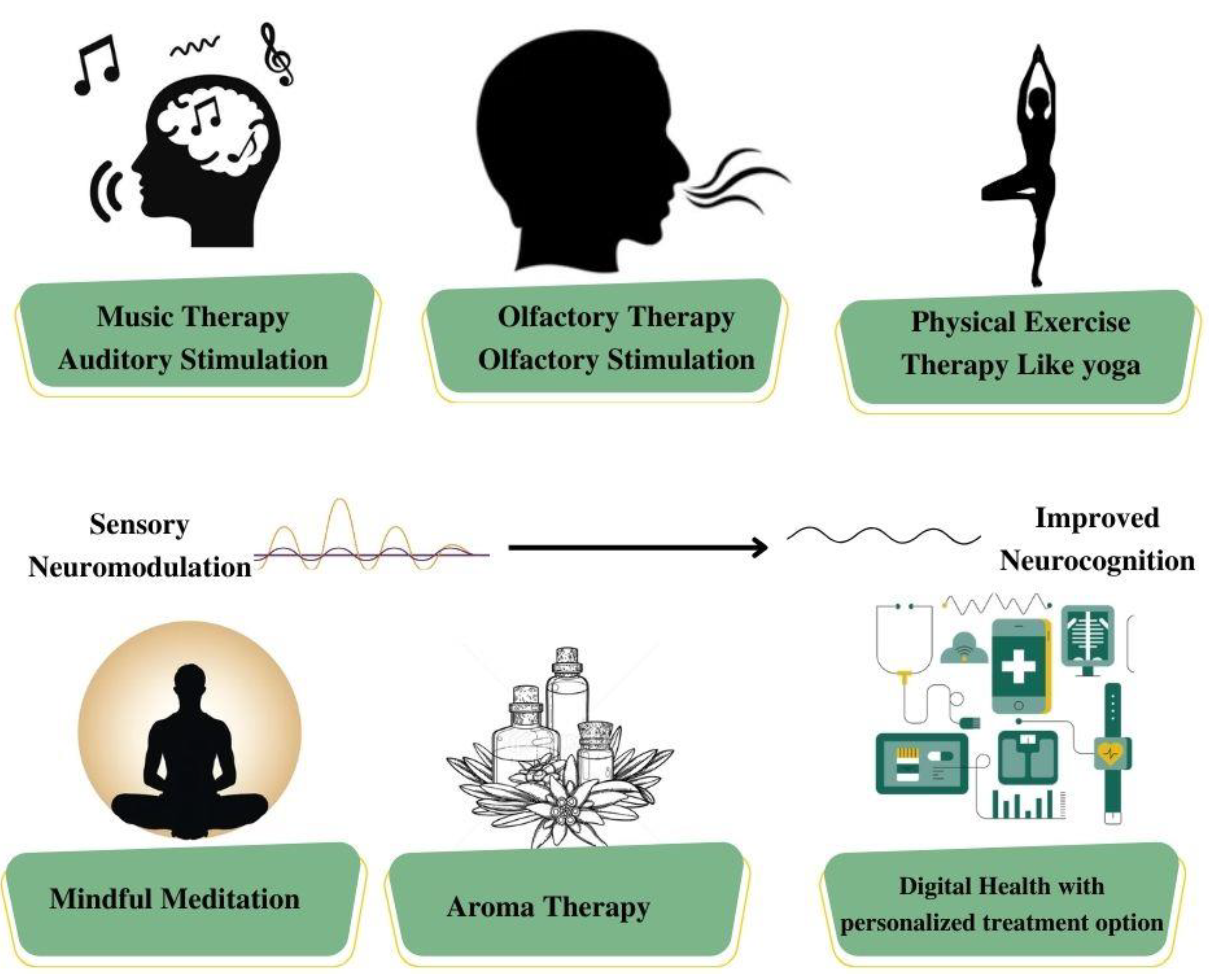
2.1. The Role of Sensory Diet in Dementia Management
3. Implementing a Customized Sensory Diet: Strategies for Effective Application
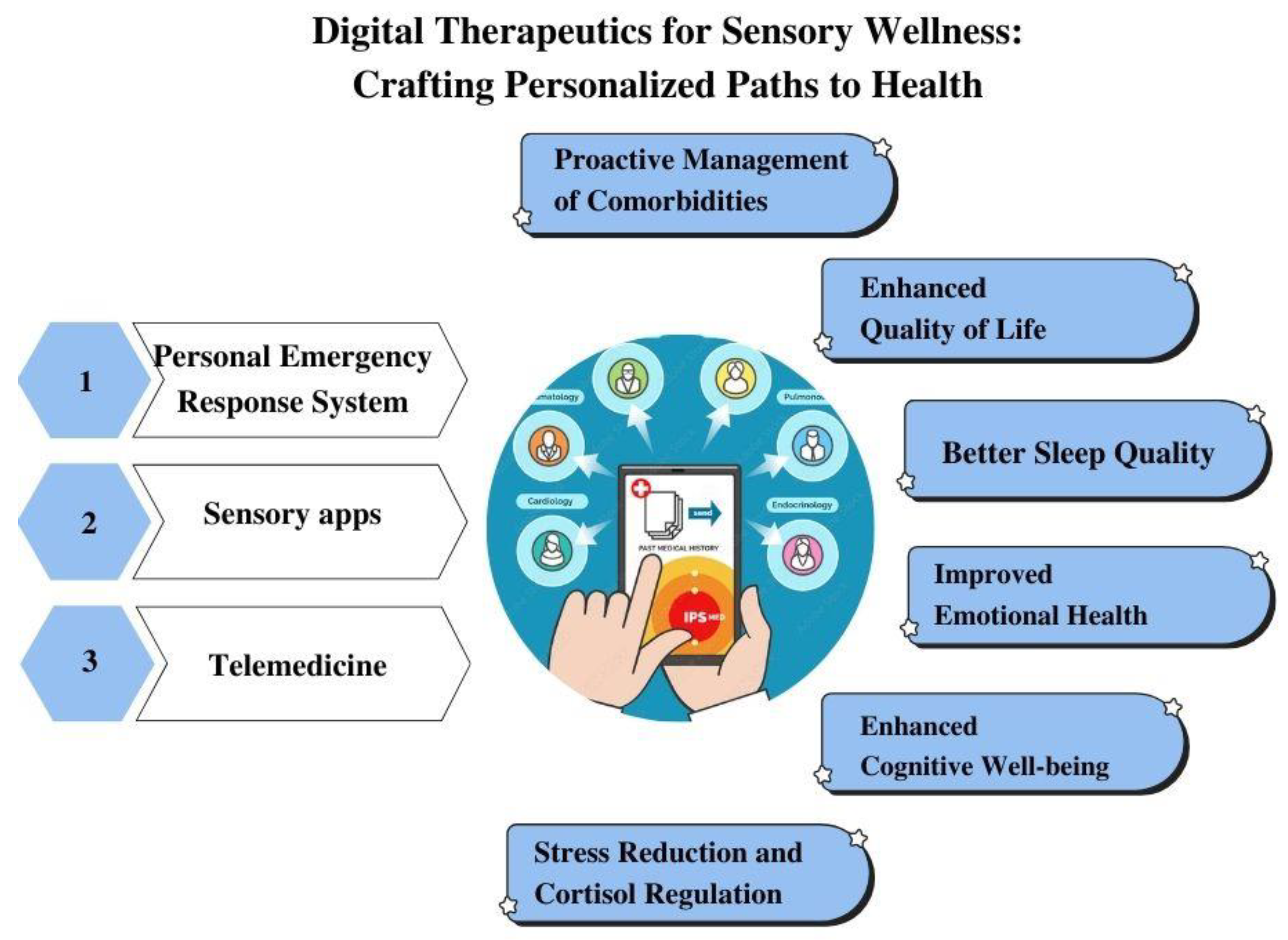
4. Innovative Convergence: Exploring the Intersection of Sensory Diets and Technology for Enhanced Support in Sensory Processing Difficulties
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mileski M, Baar Topinka J, Brooks M, Lonidier C, Linker K, Vander Veen K. Sensory and memory stimulation as a means to care for individuals with dementia in long-term care facilities. Clin Interv Aging. 2018 May 17;13:967–74. [CrossRef]
- Malek Rivan NF, Shahar S, Fakhruddin NNINM, You YX, Che Din N, Rajikan R. The effect of dietary patterns on mild cognitive impairment and dementia incidence among community-dwelling older adults. Frontiers in Nutrition [Internet]. 2022 [cited 2023 Oct 18];9. Available from: https://www.frontiersin.org/articles/10.3389/fnut.2022.901750. [CrossRef]
- Costa-López B, Ferrer-Cascales R, Ruiz-Robledillo N, Albaladejo-Blázquez N, Baryła-Matejczuk M. Relationship between Sensory Processing and Quality of Life: A Systematic Review. J Clin Med. 2021 Aug 31;10(17):3961. [CrossRef]
- Kilroy E, Aziz-Zadeh L, Cermak S. Ayres Theories of Autism and Sensory Integration Revisited: What Contemporary Neuroscience Has to Say. Brain Sci. 2019 Mar 21;9(3):68. [CrossRef]
- Camarata S, Miller LJ, Wallace MT. Evaluating Sensory Integration/Sensory Processing Treatment: Issues and Analysis. Front Integr Neurosci. 2020 Nov 26;14:556660. [CrossRef]
- Svob Strac D, Konjevod M, Sagud M, Nikolac Perkovic M, Nedic Erjavec G, Vuic B, et al. Personalizing the Care and Treatment of Alzheimer’s Disease: An Overview. Pharmacogenomics and Personalized Medicine. 2021 May 28;14:631–53. [CrossRef]
- Crofton EC, Botinestean C, Fenelon M, Gallagher E. Potential applications for virtual and augmented reality technologies in sensory science. Innovative Food Science & Emerging Technologies. 2019 Aug 1;56:102178. [CrossRef]
- Tian K, Sautter P, Fisher D, Fischbach S, Luna-Nevarez C, Boberg K, et al. Transforming Health Care: Empowering Therapeutic Communities through Technology-Enhanced Narratives. Journal of Consumer Research. 2014 Aug 1;41(2):237–60. [CrossRef]
- Shaikh TA, Dar TR, Sofi S. A data-centric artificial intelligent and extended reality technology in smart healthcare systems. Soc Netw Anal Min. 2022 Sep 1;12(1):122. [CrossRef]
- Vuillier L, May L, Greville-Harris M, Surman R, Moseley RL. The impact of the COVID-19 pandemic on individuals with eating disorders: the role of emotion regulation and exploration of online treatment experiences. J Eat Disord. 2021 Jan 12;9(1):10. [CrossRef]
- Valentino LA, Skinner MW, Pipe SW. The role of telemedicine in the delivery of health care in the COVID-19 pandemic. Haemophilia. 2020 Sep;26(5):e230–1. [CrossRef]
- Yi JS, Pittman CA, Price CL, Nieman CL, Oh ES. Telemedicine and Dementia Care: A Systematic Review of Barriers and Facilitators. Journal of the American Medical Directors Association. 2021 Jul 1;22(7):1396-1402.e18. [CrossRef]
- Vago D, David S. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Frontiers in Human Neuroscience [Internet]. 2012 [cited 2023 Oct 18];6. Available from: https://www.frontiersin.org/articles/10.3389/fnhum.2012.00296. [CrossRef]
- Huang H, Wu J, Chang Y, Wang H, Tian Y, Chen Z, et al. Molecular and Cellular Mechanisms of Neuropathic Pain in Aging. ACS Chem Neurosci. 2023 May 17;14(10):1701–16. [CrossRef]
- Deery HA, Di Paolo R, Moran C, Egan GF, Jamadar SD. The older adult brain is less modular, more integrated, and less efficient at rest: A systematic review of large-scale resting-state functional brain networks in aging. Psychophysiology. 2023;60(1):e14159. [CrossRef]
- Yamasaki T, Tobimatsu S. Driving Ability in Alzheimer Disease Spectrum: Neural Basis, Assessment, and Potential Use of Optic Flow Event-Related Potentials. Front Neurol. 2018;9:750. [CrossRef]
- Yamasaki T, Horie S, Ohyagi Y, Tanaka E, Nakamura N, Goto Y, et al. A Potential VEP Biomarker for Mild Cognitive Impairment: Evidence from Selective Visual Deficit of Higher-Level Dorsal Pathway. J Alzheimers Dis. 2016 May 23;53(2):661–76. [CrossRef]
- Yamasaki T, Goto Y, Ohyagi Y, Monji A, Munetsuna S, Minohara M, et al. Selective impairment of optic flow perception in amnestic mild cognitive impairment: evidence from event-related potentials. J Alzheimers Dis. 2012;28(3):695–708. [CrossRef]
- Ramalho A, Petrica J. The Quiet Epidemic: An Overview of Emerging Qualitative Research Trends on Sedentary Behavior in Aging Populations. Healthcare. 2023 Jan;11(15):2215. [CrossRef]
- Fortunato S, Forli F, Guglielmi V, De Corso E, Paludetti G, Berrettini S, et al. A review of new insights on the association between hearing loss and cognitive decline in ageing. Acta Otorhinolaryngol Ital. 2016 Jun;36(3):155–66. [CrossRef]
- Cai Y, Song W, Li J, Jing Y, Liang C, Zhang L, et al. The landscape of aging. Sci China Life Sci. 2022 Dec 1;65(12):2354–454. [CrossRef]
- López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. Hallmarks of aging: An expanding universe. Cell. 2023 Jan 19;186(2):243–78. [CrossRef]
- Duboc H, Latrache S, Nebunu N, Coffin B. The Role of Diet in Functional Dyspepsia Management. Frontiers in Psychiatry [Internet]. 2020 [cited 2023 Oct 18];11. Available from: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00023. [CrossRef]
- Blackwell SE. Mental Imagery in the Science and Practice of Cognitive Behaviour Therapy: Past, Present, and Future Perspectives. J Cogn Ther. 2021 Mar 1;14(1):160–81. [CrossRef]
- Rajiyah T. Sensory stimulation in the treatment of neuropsychiatric symptoms of dementia. 2023 Aug 1 [cited 2023 Oct 18]; Available from: https://repository.rcsi.com/articles/journal_contribution/Sensory_stimulation_in_the_treatment_of_neuropsychiatric_symptoms_of_dementia/23523951/1.
- Wójcik D, Szczechowiak K, Konopka P, Owczarek M, Kuzia A, Rydlewska-Liszkowska I, et al. Informal Dementia Caregivers: Current Technology Use and Acceptance of Technology in Care. International Journal of Environmental Research and Public Health. 2021 Jan;18(6):3167. [CrossRef]
- Hwang PH, Longstreth Jr W t., Brenowitz WD, Thielke SM, Lopez OL, Francis CE, et al. Dual sensory impairment in older adults and risk of dementia from the GEM Study. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring. 2020;12(1):e12054. [CrossRef]
- van Hoof J, Kort HSM, Duijnstee MSH, Rutten PGS, Hensen JLM. The indoor environment and the integrated design of homes for older people with dementia. Building and Environment. 2010 May 1;45(5):1244–61. [CrossRef]
- Dominguez LJ, Veronese N, Vernuccio L, Catanese G, Inzerillo F, Salemi G, et al. Nutrition, Physical Activity, and Other Lifestyle Factors in the Prevention of Cognitive Decline and Dementia. Nutrients. 2021 Nov;13(11):4080. [CrossRef]
- Phillips C. Lifestyle Modulators of Neuroplasticity: How Physical Activity, Mental Engagement, and Diet Promote Cognitive Health during Aging. Neural Plasticity. 2017 Jun 12;2017:e3589271. [CrossRef]
- Woodbridge R, Sullivan M, Harding E, Crutch S, Gilhooly K, Gilhooly M, et al. Use of the physical environment to support everyday activities for people with dementia: A systematic review. Dementia. 2018 Jul 1;17(5):533–72. [CrossRef]
- Brett L, Traynor V, Stapley P. Effects of Physical Exercise on Health and Well-Being of Individuals Living With a Dementia in Nursing Homes: A Systematic Review. Journal of the American Medical Directors Association. 2016 Feb 1;17(2):104–16. [CrossRef]
- Gómez-Pinilla F. Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci. 2008 Jul;9(7):568–78. [CrossRef]
- Zavitz E, Price NSC. Understanding Sensory Information Processing Through Simultaneous Multi-area Population Recordings. Frontiers in Neural Circuits [Internet]. 2019 [cited 2024 Jan 16];12. Available from: https://www.frontiersin.org/articles/10.3389/fncir.2018.00115. [CrossRef]
- McCarty R. Learning about stress: neural, endocrine and behavioral adaptations. Stress. 2016 Jun 13;19:1–30. [CrossRef]
- Hazen EP, Stornelli JL, O’Rourke JA, Koesterer K, McDougle CJ. Sensory Symptoms in Autism Spectrum Disorders. Harvard Review of Psychiatry. 2014 Apr;22(2):112. [CrossRef]
- Sánchez A, Millán-Calenti JC, Lorenzo-López L, Maseda A. Multisensory Stimulation for People With Dementia: A Review of the Literature. Am J Alzheimers Dis Other Demen. 2013 Feb 1;28(1):7–14. [CrossRef]
- Sánchez A, Marante-Moar MP, Sarabia C, de Labra C, Lorenzo T, Maseda A, et al. Multisensory Stimulation as an Intervention Strategy for Elderly Patients With Severe Dementia: A Pilot Randomized Controlled Trial. Am J Alzheimers Dis Other Demen. 2016 Jun 1;31(4):341–50. [CrossRef]
- Dixon E, Lazar A. The Role of Sensory Changes in Everyday Technology use by People with Mild to Moderate Dementia. In: Proceedings of the 22nd International ACM SIGACCESS Conference on Computers and Accessibility [Internet]. New York, NY, USA: Association for Computing Machinery; 2020 [cited 2023 Oct 18]. p. 1–12. (ASSETS ’20). Available from: https://doi.org/10.1145/3373625.3417000. [CrossRef]
- Zgonec S. Mobile apps supporting people with dementia and their carers: Literature Review and Research Agenda. IFAC-PapersOnLine. 2021 Jan 1;54(13):663–8. [CrossRef]
- Kuo HL, Chang CH, Ma WF. A Survey of Mobile Apps for the Care Management of Patients with Dementia. Healthcare (Basel). 2022 Jun 23;10(7):1173. [CrossRef]
- García-Requejo A, Pérez-Rubio MC, Villadangos JM, Hernández Á. Activity Monitoring and Location Sensory System for People With Mild Cognitive Impairments. IEEE Sensors Journal. 2023 Mar;23(5):5448–58. [CrossRef]
- Baragash RS, Aldowah H, Ghazal S. Virtual and augmented reality applications to improve older adults’ quality of life: A systematic mapping review and future directions. DIGITAL HEALTH. 2022 Jan 1;8:20552076221132100. [CrossRef]
- Tay JL, Xie H, Sim K. Effectiveness of Augmented and Virtual Reality-Based Interventions in Improving Knowledge, Attitudes, Empathy and Stigma Regarding People with Mental Illnesses—A Scoping Review. Journal of Personalized Medicine. 2023 Jan;13(1):112. [CrossRef]
- Laukkanen T, Xi N, Hallikainen H, Ruusunen N, Hamari J. Virtual technologies in supporting sustainable consumption: From a single-sensory stimulus to a multi-sensory experience. International Journal of Information Management. 2022 Apr 1;63:102455. [CrossRef]
- Fuentes S, Tongson E, Gonzalez Viejo C. Novel digital technologies implemented in sensory science and consumer perception. Current Opinion in Food Science. 2021 Oct 1;41:99–106. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




