Submitted:
01 February 2024
Posted:
02 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results and Discussion
2.1. The synthesis and Characterization of Amphiphilic Polymers and Dox-Containing Micelles
2.1.1. Heparin and Chitosan Micelles
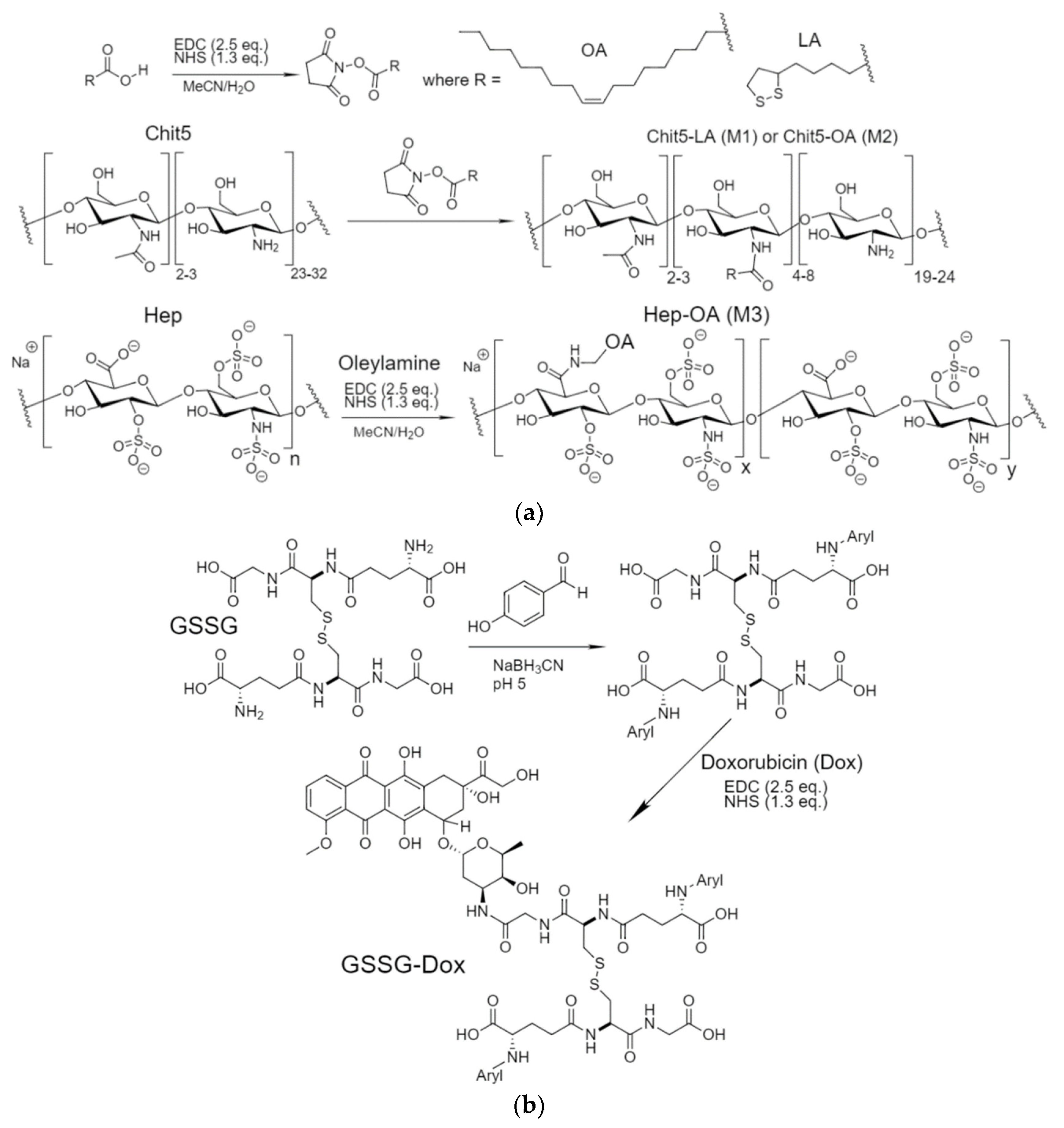
2.1.2. The Synthesis of Amphiphilic Polymers and Dox Prodrugs
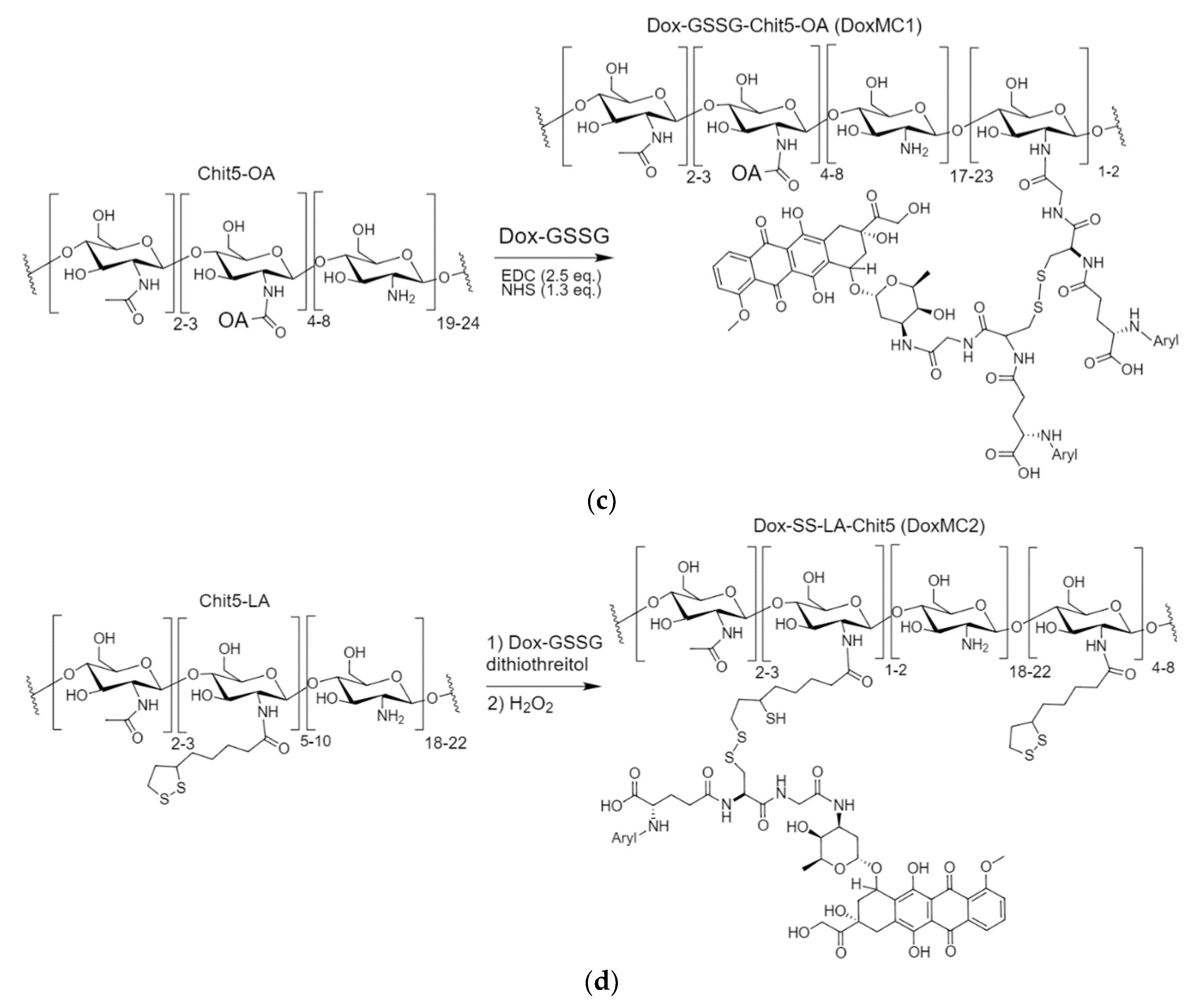
2.1.3. FTIR Spectroscopy for Characterization of Self-Assembled Chitosan and Heparin Conjugates
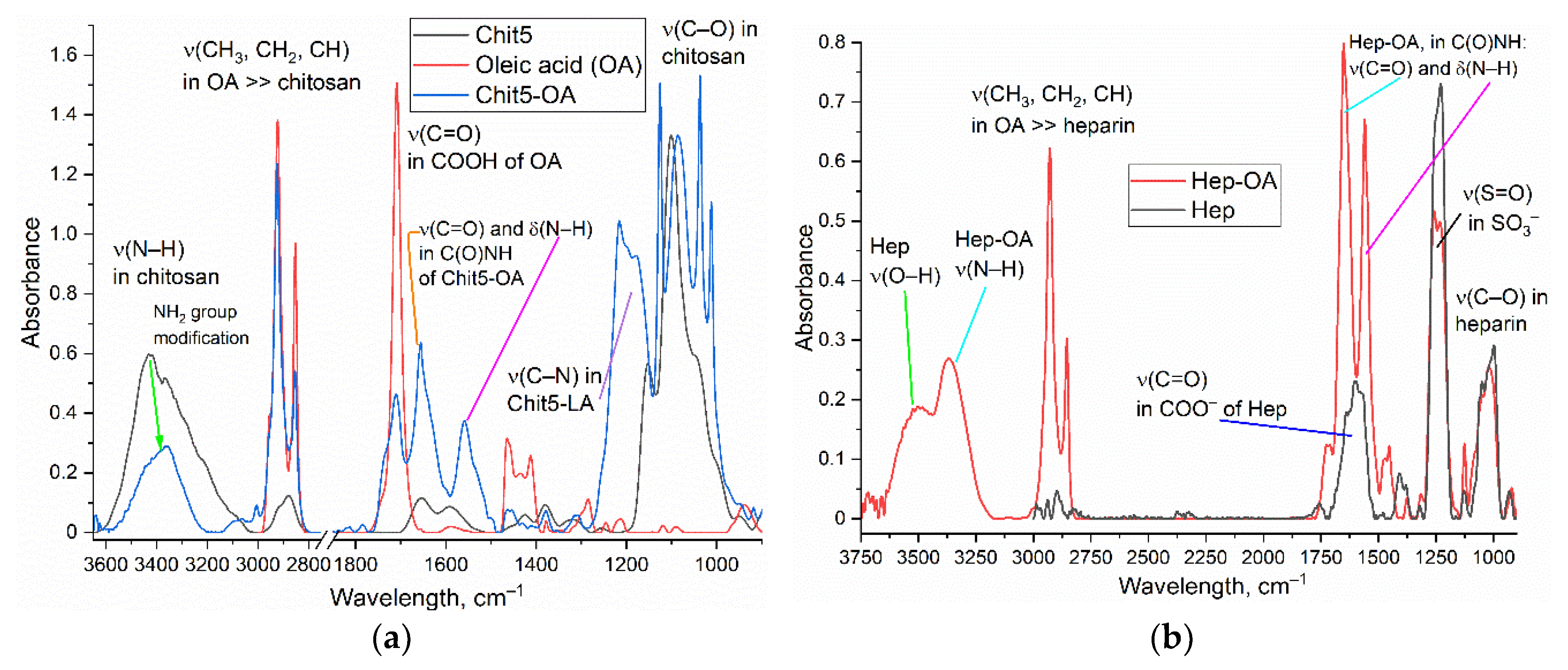
2.1.4. FTIR Spectroscopy for Characterization of Dox-Containing Micellar Formulations
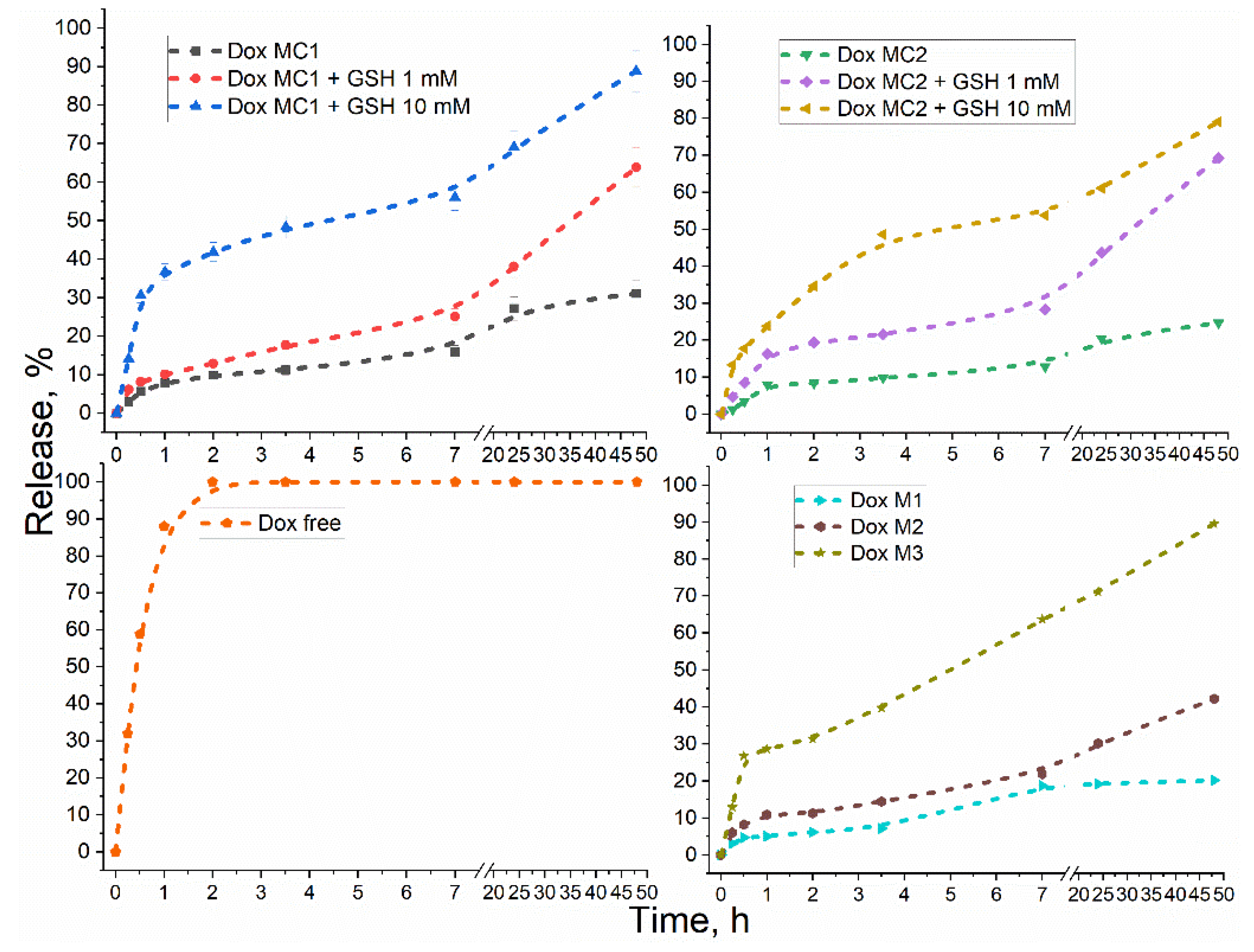
2.2. Glutathione-Sensitivity of Conjugates
2.3. Cytotoxicity Studies of Drugs
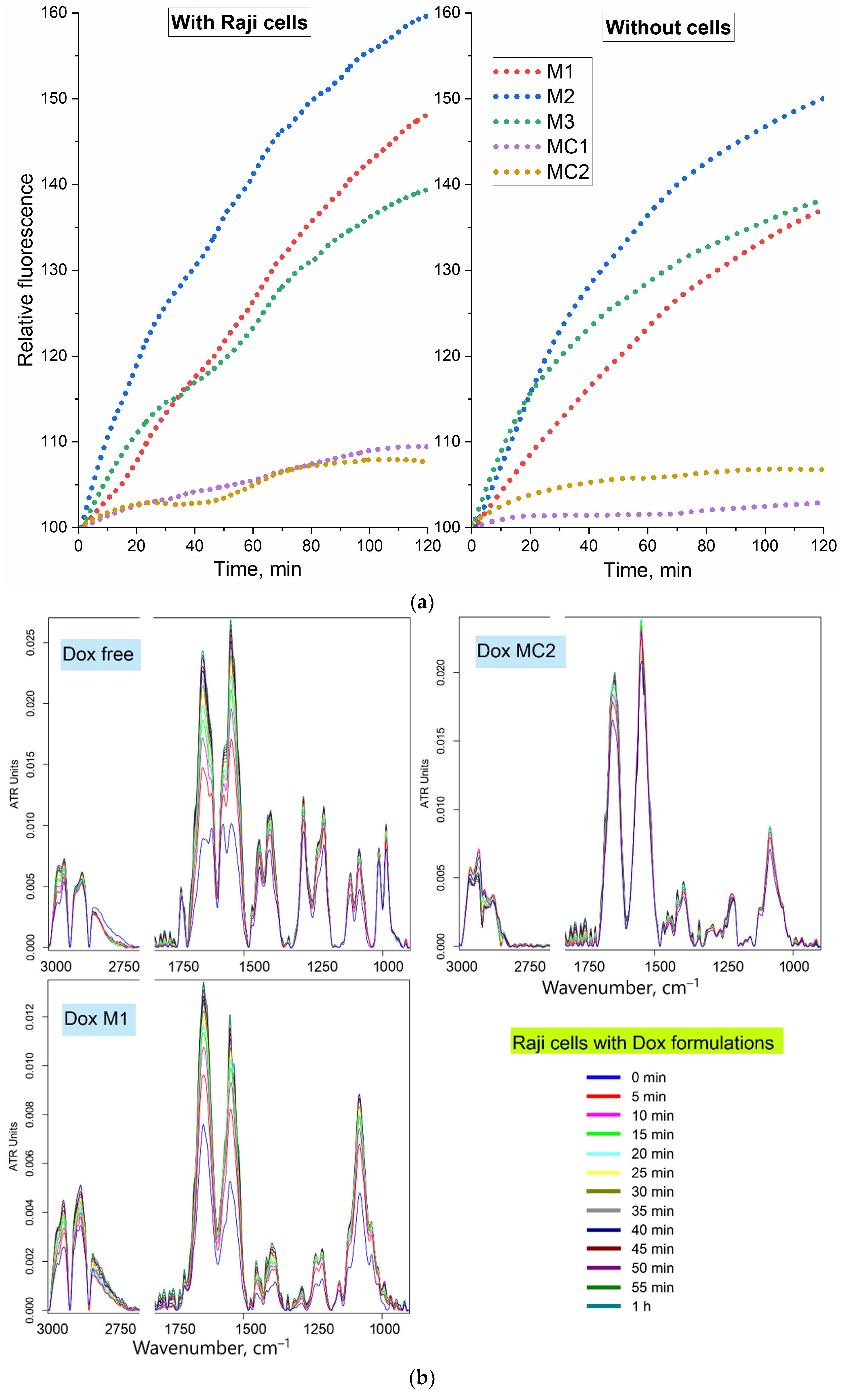
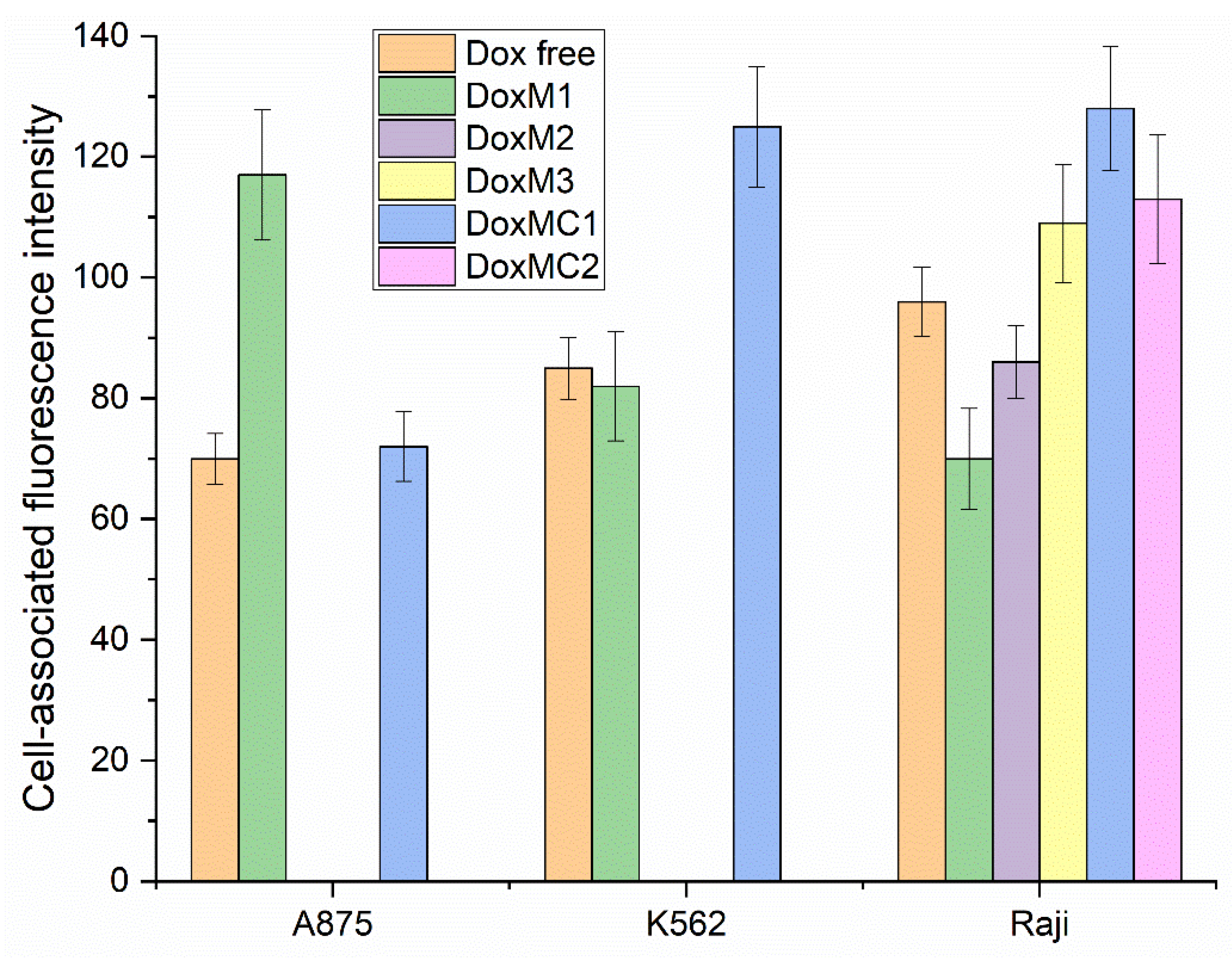
2.4. Permeability of Raji Cancer Cells to Dox-Containing Formulations
2.5. Dox-Containing Formulation Interactions with Eukaryotic Cells: The Molecular Details
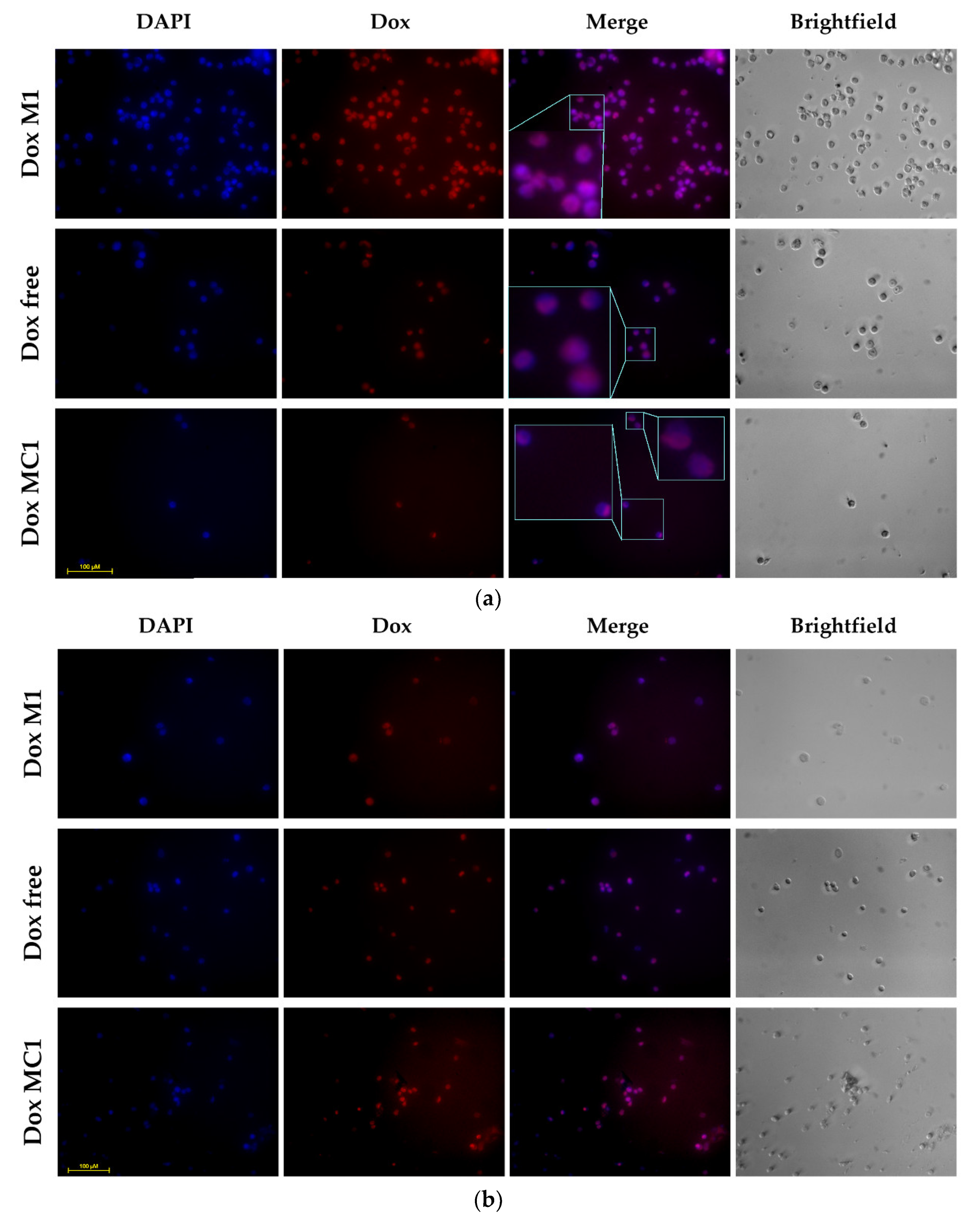
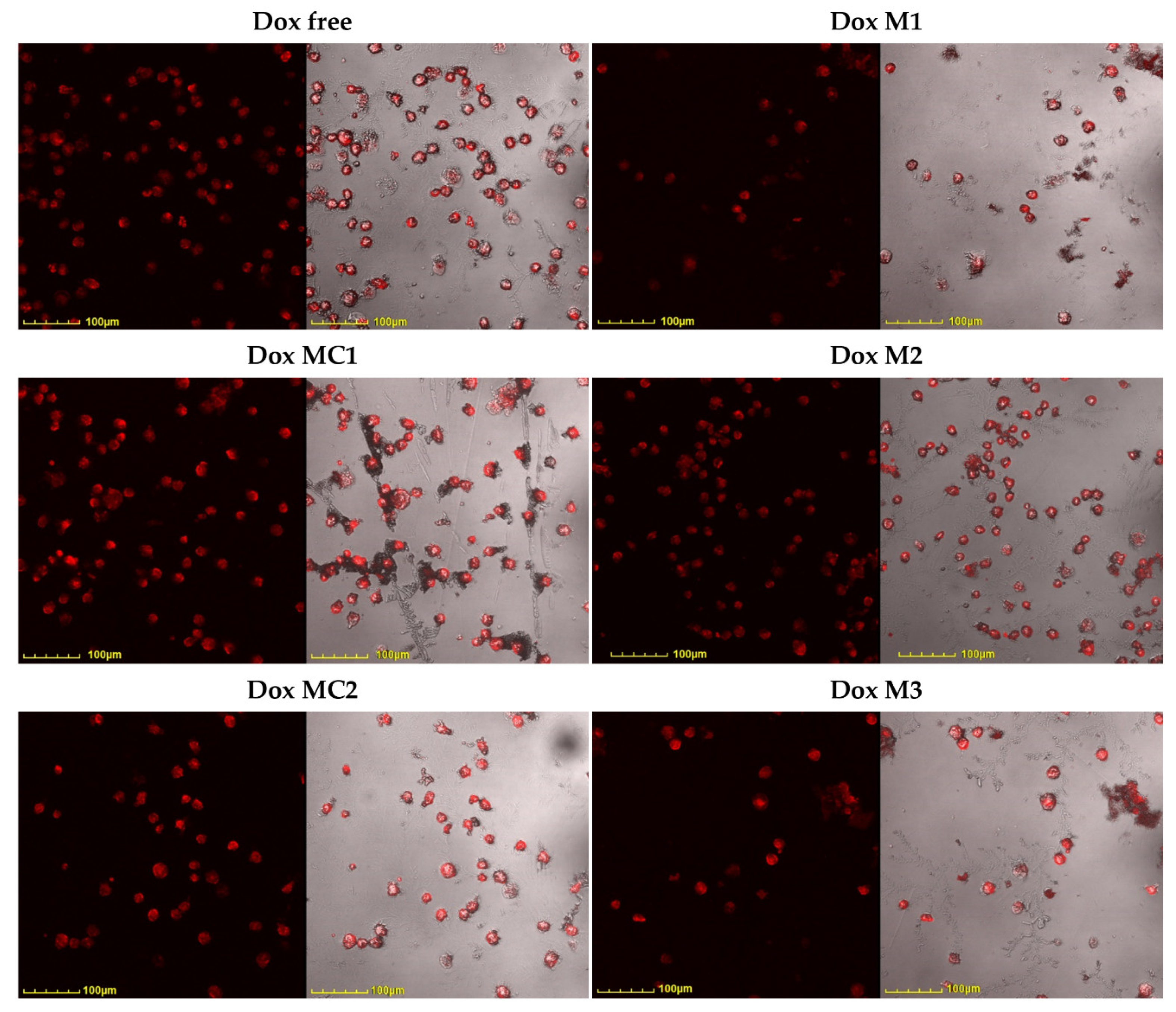
2.6. Confocal Visualization of Micellar Formulations Based on Doxorubicin Action on Cancer Cells
3. Conclusions
4. Materials and Methods
4.1. Reagents
4.2. The Synthesis and Characterization of Amphiphilic Polymers and Dox-Containing Micelles
4.2.1. Heparin and Chitosan Grafted Conjugates Synthesis
4.2.2. Non-Covalent Dox Micellar Formulation Synthesis
4.2.3. Covalent Dox Micellar Formulation Synthesis
4.3. Characterization of Polymers and Micelles
4.4. Determination of Dox Loading Degree into Micelles and Release Kinetics
4.5. Cell Cultivation and Toxicity Assay
4.6. FTIR Spectroscopy as A Tool for Studying of Dox Interaction with Cells
4.7. Confocal Laser Scanning Microscopy for Visualization of Dox Interaction with Cells
4.8. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Mavromoustakos, T.; Tzakos, A.G. Supramolecules in Drug Discovery and Drug Delivery; ISBN 9781071609194.
- Buranachai, T.; Praphairaksit, N.; Muangsin, N. Chitosan/polyethylene glycol beads crosslinked with tripolyphosphate and glutaraldehyde for gastrointestinal drug delivery. AAPS PharmSciTech 2010, 11, 1128–1137. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Jiao, Y.; Wang, Y.; Zhou, C.; Zhang, Z. Polysaccharides-based nanoparticles as drug delivery systems. Adv. Drug Deliv. Rev. 2008, 60, 1650–1662. [Google Scholar] [CrossRef] [PubMed]
- Haimhoffer, Á.; Rusznyák, Á.; Réti-Nagy, K.; Vasvári, G.; Váradi, J.; Vecsernyés, M.; Bácskay, I.; Fehér, P.; Ujhelyi, Z.; Fenyvesi, F. Cyclodextrins in drug delivery systems and their effects on biological barriers. Sci. Pharm. 2019, 87. [Google Scholar] [CrossRef]
- Stebbins, N.D.; Ouimet, M.A.; Uhrich, K.E. Antibiotic-containing polymers for localized, sustained drug delivery. Adv. Drug Deliv. Rev. 2014, 78, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.; Wang, X.; Nie, S.; Chen, Z.; Shin, D.M. Therapeutic nanoparticles for drug delivery in cancer. Clin. Cancer Res. 2008, 14, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Loftsson, T.; Jarho, P.; Másson, M.; Järvinen, T. Cyclodextrins in drug delivery system. Expert Opin. Drug Deliv. 2005, 2, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Zlotnikov, I.D.; Kudryashova, E. V. Computer simulation of the Receptor–Ligand Interactions of Mannose Receptor CD206 in Comparison with the Lectin Concanavalin A Model. Biochem. 2022, 87, 54–69. [Google Scholar] [CrossRef] [PubMed]
- Cavalcante, C.H.; Fernandes, R.S.; de Oliveira Silva, J.; Ramos Oda, C.M.; Leite, E.A.; Cassali, G.D.; Charlie-Silva, I.; Ventura Fernandes, B.H.; Miranda Ferreira, L.A.; de Barros, A.L.B. Doxorubicin-loaded pH-sensitive micelles: A promising alternative to enhance antitumor activity and reduce toxicity. Biomed. Pharmacother. 2021, 134. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Fajardo, L.; Mahajan, L.H.; Ndaya, D.; Hargrove, D.; Manautou, J.E.; Liang, B.T.; Chen, M.H.; Kasi, R.M.; Lu, X. Reduced in vivo toxicity of doxorubicin by encapsulation in cholesterol-containing self-assembled nanoparticles. Pharmacol. Res. 2016, 107, 93–101. [Google Scholar] [CrossRef]
- Tammam, S.N.; Azzazy, H.M.E.; Breitinger, H.G.; Lamprecht, A. Chitosan Nanoparticles for Nuclear Targeting: The Effect of Nanoparticle Size and Nuclear Localization Sequence Density. Mol. Pharm. 2015, 12, 4277–4289. [Google Scholar] [CrossRef]
- Zhong, P.; Zhang, J.; Deng, C.; Cheng, R.; Meng, F.; Zhong, Z. Glutathione-Sensitive Hyaluronic Acid-SS-Mertansine Prodrug with a High Drug Content: Facile Synthesis and Targeted Breast Tumor Therapy. Biomacromolecules 2016, 17, 3602–3608. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, M.; Validi, M.; Gholipour, A.; Makvandi, P.; Sharifi, E. Chitosan nanofiber biocomposites for potential wound healing applications: Antioxidant activity with synergic antibacterial effect. Bioeng. Transl. Med. 2022, 7, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Serra, P.; Santamaria, P. Nanoparticle-based autoimmune disease therapy. Clin. Immunol. 2015, 160, 3–13. [Google Scholar] [CrossRef]
- Yang, C.; Gao, S.; Dagnæs-Hansen, F.; Jakobsen, M.; Kjems, J. Impact of PEG Chain Length on the Physical Properties and Bioactivity of PEGylated Chitosan/siRNA Nanoparticles in Vitro and in Vivo. ACS Appl. Mater. Interfaces 2017, 9, 12203–12216. [Google Scholar] [CrossRef] [PubMed]
- Mahor, S.; Dash, B.C.; O’Connor, S.; Pandit, A. Mannosylated polyethyleneimine-hyaluronan nanohybrids for targeted gene delivery to macrophage-like cell lines. Bioconjug. Chem. 2012, 23, 1138–1148. [Google Scholar] [CrossRef]
- Huang, H.J.; Tsai, Y.L.; Lin, S.H.; Hsu, S.H. Smart polymers for cell therapy and precision medicine. J. Biomed. Sci. 2019, 26, 1–11. [Google Scholar] [CrossRef]
- Psimadas, D.; Georgoulias, P.; Valotassiou, V.; Loudos, G. Molecular Nanomedicine Towards Cancer : J. Pharm. Sci. 2012, 101, 2271–2280. [Google Scholar] [CrossRef]
- Negut, I.; Bita, B. Polymeric Micellar Systems—A Special Emphasis on “Smart” Drug Delivery. Pharmaceutics 2023, 15. [Google Scholar] [CrossRef]
- Raval, N.; Maheshwari, R.; Shukla, H.; Kalia, K.; Torchilin, V.P.; Tekade, R.K. Multifunctional polymeric micellar nanomedicine in the diagnosis and treatment of cancer. Mater. Sci. Eng. C 2021, 126, 112186. [Google Scholar] [CrossRef]
- Vaupel, P.; Kallinowski, F.; Okunieff, P. Blood Flow, Oxygen and Nutrient Supply, and Metabolic Microenvironment of Human Tumors: A Review. Cancer Res. 1989, 49, 6449–6465. [Google Scholar] [PubMed]
- Ray, P.; Confeld, M.; Borowicz, P.; Wang, T.; Mallik, S.; Quadir, M. PEG-b-poly (carbonate)-derived nanocarrier platform with pH-responsive properties for pancreatic cancer combination therapy; Elsevier B.V., 2019; Т. 174; ISBN 7012318333.
- Ngan, V.T.T.; Chiou, P.Y.; Ilhami, F.B.; Bayle, E.A.; Shieh, Y.T.; Chuang, W.T.; Chen, J.K.; Lai, J.Y.; Cheng, C.C. A CO2-Responsive Imidazole-Functionalized Fluorescent Material Mediates Cancer Chemotherapy. Pharmaceutics 2023, 15. [Google Scholar] [CrossRef]
- Wang, Z.; Deng, X.; Ding, J.; Zhou, W.; Zheng, X.; Tang, G. Mechanisms of drug release in pH-sensitive micelles for tumour targeted drug delivery system: A review. Int. J. Pharm. 2018, 535, 253–260. [Google Scholar] [CrossRef]
- Junnuthula, V.; Kolimi, P.; Nyavanandi, D.; Sampathi, S.; Vora, L.K.; Dyawanapelly, S. Polymeric Micelles for Breast Cancer Therapy: Recent Updates, Clinical Translation and Regulatory Considerations. Pharmaceutics 2022, 14. [Google Scholar] [CrossRef]
- He, L.; Qin, X.; Fan, D.; Feng, C.; Wang, Q.; Fang, J. Dual-Stimuli Responsive Polymeric Micelles for the Effective Treatment of Rheumatoid Arthritis. ACS Appl. Mater. Interfaces 2021, 13, 21076–21086. [Google Scholar] [CrossRef] [PubMed]
- Mutlu-Agardan, N.B.; Sarisozen, C.; Torchilin, V.P. Cytotoxicity of Novel Redox Sensitive PEG2000-S-S-PTX Micelles against Drug-Resistant Ovarian and Breast Cancer Cells. Pharm. Res. 2020, 37. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Li, C. PH responsive fluorescence nanoprobe imaging of tumors by sensing the acidic microenvironment. J. Mater. Chem. 2011, 21, 15862–15871. [Google Scholar] [CrossRef]
- Ribeiro, I.S.; Leornado, A.L.S.; Carneiro, M.J.M.; Filho, R.N.C.; Freire, R.S. pH-responsive prodrug nanoparticles based cashew gum as a doxorubicin delivery sys- tem. 2022, 1–18.
- Zlotnikov, I.D.; Dobryakova, N. V.; Ezhov, A.A.; Kudryashova, E. V. Achievement of the Selectivity of Cytotoxic Agents against Cancer Cells by Creation of Combined Formulation with Terpenoid Adjuvants as Prospects to Overcome Multidrug Resistance. Int. J. Mol. Sci. 2023, 24, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Zlotnikov, I.D.; Streltsov, D.A.; Ezhov, A.A.; Kudryashova, E. V. Smart pH- and Temperature-Sensitive Micelles Based on Chitosan Grafted with Fatty Acids to Increase the Efficiency and Selectivity of Doxorubicin and Its Adjuvant Regarding the Tumor Cells. Pharmaceutics 2023, 15. [Google Scholar] [CrossRef]
- Li, C.; Xia, J.; Wei, X.; Yan, H.; Si, Z.; Ju, S. PH-Activated near-infrared fluorescence nanoprobe imaging tumors by sensing the acidic microenvironment. Adv. Funct. Mater. 2010, 20, 2222–2230. [Google Scholar] [CrossRef]
- Huo, M.; Liu, Y.; Wang, L.; Yin, T.; Qin, C.; Xiao, Y.; Yin, L.; Liu, J.; Zhou, J. Redox-Sensitive Micelles Based on O,N-Hydroxyethyl Chitosan-Octylamine Conjugates for Triggered Intracellular Delivery of Paclitaxel; 2016; Т. 13; ISBN 8621311623.
- Luo, T.; Han, J.; Zhao, F.; Pan, X.; Tian, B.; Ding, X.; Zhang, J. Redox-sensitive micelles based on retinoic acid modified chitosan conjugate for intracellular drug delivery and smart drug release in cancer therapy. Carbohydr. Polym. 2019, 215, 8–19. [Google Scholar] [CrossRef]
- Shim, W.S.; Kim, J.H.; Kim, K.; Kim, Y.S.; Park, R.W.; Kim, I.S.; Kwon, I.C.; Lee, D.S. pH- and temperature-sensitive, injectable, biodegradable block copolymer hydrogels as carriers for paclitaxel. Int. J. Pharm. 2007, 331, 11–18. [Google Scholar] [CrossRef]
- Wu, J.; Su, Z.; Ma, G. A thermo- and pH-sensitive hydrogel composed of quaternized chitosan / glycerophosphate. 2006, 315, 1–11. [CrossRef]
- Liow, S.S.; Dou, Q.; Kai, D.; Karim, A.A.; Zhang, K.; Xu, F.; Loh, X.J. Thermogels: In Situ Gelling Biomaterial. ACS Biomater. Sci. Eng. 2016, 2, 295–316. [Google Scholar] [CrossRef]
- Takei, T.; Nakahara, H.; Ijima, H.; Kawakami, K. Synthesis of a chitosan derivative soluble at neutral pH and gellable by freeze-thawing, and its application in wound care. Acta Biomater. 2012, 8, 686–693. [Google Scholar] [CrossRef]
- Falanga, A.; Russo, L.; Verzeroli, C. Mechanisms of thrombosis in cancer. Thromb. Res. 2013, 131, S59–S62. [Google Scholar] [CrossRef]
- Falanga, A.; Russo, L.; Milesi, V.; Vignoli, A. Mechanisms and risk factors of thrombosis in cancer. Crit. Rev. Oncol. Hematol. 2017, 118, 79–83. [Google Scholar] [CrossRef]
- Young, A.; Chapman, O.; Connor, C.; Poole, C.; Rose, P.; Kakkar, A.K. Thrombosis and cancer. Nat. Rev. Clin. Oncol. 2012, 9, 437–449. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, R.S. The Role of Low-Molecular-Weight Heparins as Supportive Care Therapy in Cancer-Associated Thrombosis. Semin. Oncol. 2006, 33, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Devlin, A.; Mauri, L.; Guerrini, M.; Yates, E.A.; Skidmore, M.A. The use of ATR-FTIR spectroscopy to characterise crude heparin samples by composition and structural features. bioRxiv 2019, 744532. [Google Scholar]
- Martins, A.F.; Piai, J.F.; Schuquel, I.T.A.; Rubira, A.F.; Muniz, E.C. Polyelectrolyte complexes of chitosan/heparin and N,N,N-trimethyl chitosan/heparin obtained at different pH: I. Preparation, characterization, and controlled release of heparin. Colloid Polym. Sci. 2011, 289, 1133–1144. [Google Scholar] [CrossRef]
- Lundin, M.; Blomberg, E.; Tilton, R.D. Polymer dynamics in layer-by-layer assemblies of chitosan and heparin. Langmuir 2010, 26, 3242–3251. [Google Scholar] [CrossRef] [PubMed]
- Harada, N.S.; Oyama, H.T.; Bártoli, J.R.; Gouvêa, D.; Cestari, I.A.; Wang, S.H. Quantifying adsorption of heparin on a PVC substrate using ATR-FTIR. Polym. Int. 2005, 54, 209–214. [Google Scholar] [CrossRef]
- Fischer, E.G. Nuclear Morphology and the Biology of Cancer Cells. Acta Cytol. 2020, 64, 511–519. [Google Scholar] [CrossRef]
- Balendiran, G.K.; Dabur, R.; Fraser, D. The role of glutathione in cancer. Cell Biochem. Funct. 2004, 22, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, L.; Sandhu, J.K.; Harper, M.E.; Cuperlovic-culf, M. Role of glutathione in cancer: From mechanisms to therapies. Biomolecules 2020, 10, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Valtis, Y.K.; Flamand, Y.; Shimony, S.; Place, A.E.; Silverman, L.B.; Vrooman, L.M.; Brunner, A.M.; Sallan, S.E.; Wadleigh, M.; Stone, R.M.; et al. Treatment completion, asparaginase completion, and oncologic outcomes among children, adolescents and young adults with acute lymphoblastic leukemia treated with DFCI Consortium Protocols. Leukemia 2024. [Google Scholar] [CrossRef]
- Yao, H.; Zhang, C.; Tan, X.; Li, J.; Yin, X.; Deng, X.; Chen, T.; Rao, J.; Gao, L.; Kong, P.; и др. Efficacy and toxicity of CLAG combined with pegylated liposomal doxorubicin in the treatment of refractory or relapsed acute myeloid leukemia. Cancer Med. 2023, 12, 12377–12387. [Google Scholar] [CrossRef]
- Vrooman, L.M.; Blonquist, T.M.; Harris, M.H.; Stevenson, K.E.; Place, A.E.; Hunt, S.K.; O’Brien, J.E.; Asselin, B.L.; Athale, U.H.; Clavell, L.A.; и др. Refining risk classification in childhood b acute lymphoblastic leukemia: Results of DFCI ALL consortium protocol 05-001. Blood Adv. 2018, 2, 1449–1458. [Google Scholar] [CrossRef]
- Egler, R.A.; Ahuja, S.P.; Matloub, Y. L-asparaginase in the treatment of patients with acute lymphoblastic leukemia. J. Pharmacol. Pharmacother. 2016, 7, 62–71. [Google Scholar] [CrossRef]
- Shadman, M. Diagnosis and Treatment of Chronic Lymphocytic Leukemia: A Review. Jama 2023, 329, 918–932. [Google Scholar] [CrossRef]
- Wu, X.; Chen, S.; Huang, K.; Lin, G. Triptolide promotes ferroptosis by suppressing Nrf2 to overcome leukemia cell resistance to doxorubicin. Mol. Med. Rep. 2023, 27, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zlotnikov, I.D.; Ezhov, A.A.; Vigovskiy, M.A.; Grigorieva, O.A.; Dyachkova, U.D.; Belogurova, N.G.; Kudryashova, E. V. Application Prospects of FTIR Spectroscopy and CLSM to Monitor the Drugs Interaction with Bacteria Cells Localized in Macrophages for Diagnosis and Treatment Control of Respiratory Diseases. Diagnostics 2023, 13, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Zlotnikov, I.D.; Vigovskiy, M.A.; Davydova, M.P.; Danilov, M.R.; Dyachkova, U.D.; Grigorieva, O.A.; Kudryashova, E. V. Mannosylated Systems for Targeted Delivery of Antibacterial Drugs to Activated Macrophages. Int. J. Mol. Sci. 2022, 23, 1–29. [Google Scholar] [CrossRef] [PubMed]
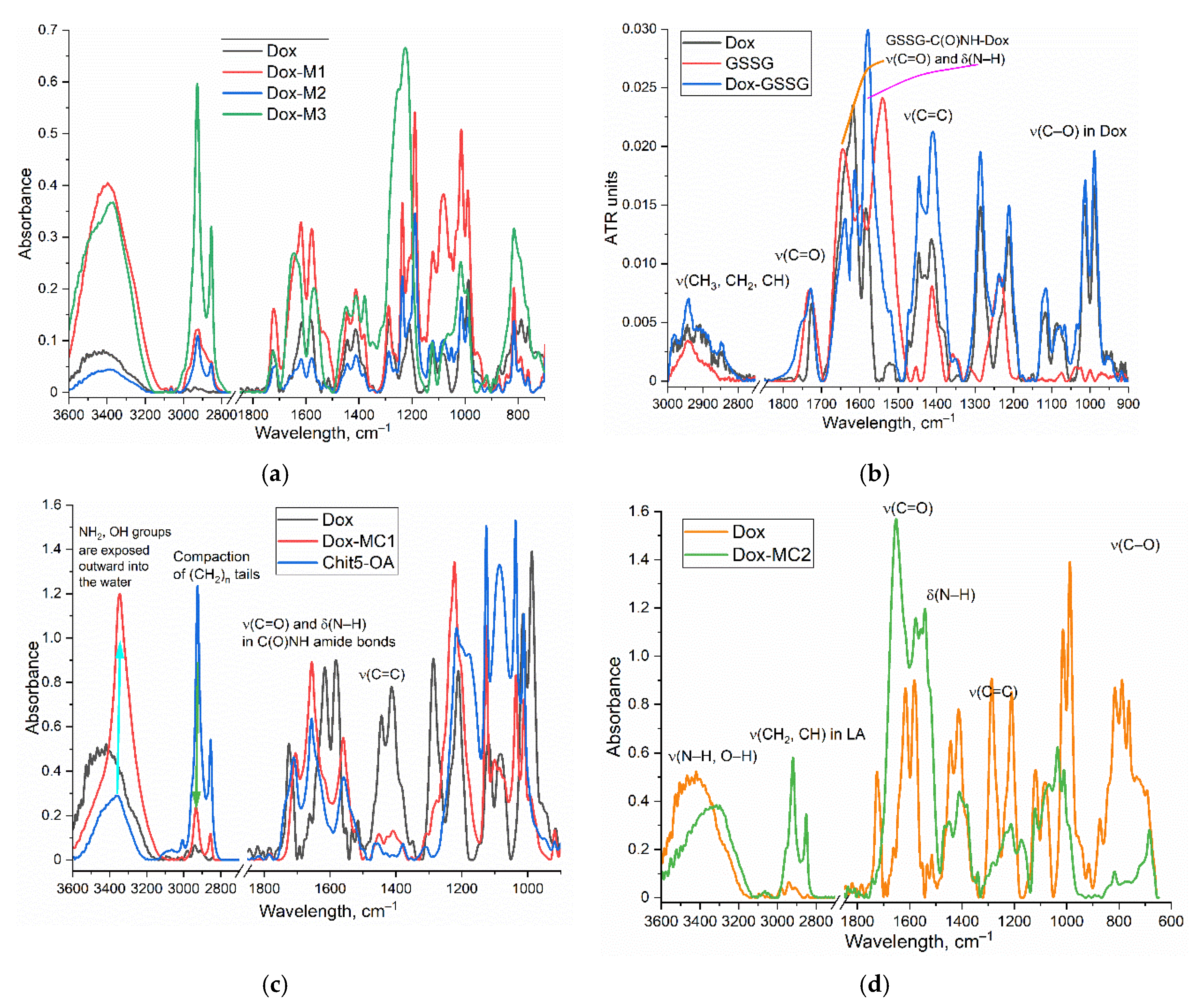
| Dox containing micellar formulation | Dox mass percentage, % | Average Mw of one polymeric structure unit, kDa | Ref | ||
|---|---|---|---|---|---|
| Brief designation* | Chemical composition** | Synthesis | FTIR spectra | ||
| DoxM1 | Dox in Chit5-LA | 13±1 | 6.2±0.4 | Figure 1a | Figure S1 and Figure 3a |
| DoxM2 | Dox in Chit5-OA | 10±1 | 6.6±0.5 | Figure 2a and Figure 3a | |
| DoxM3 | Dox in Hep-OA | 5.8±0.3 | 23±5 | Figure 2b and Figure 3a | |
| DoxMC1 | Dox-GSSG-Chit5-OA | 13±1 | 8.3±0.7 | Figure 1b,c | Figure 3b,c |
| DoxMC2 | Dox-SS-LA-Chit5 | 14±1 | 7.5±0.6 | Figure 1b,d | Figure 3b,d |
| Dox formulation | Initial rate, %/h | Accumulated concentration after 7 h, % |
|---|---|---|
| Dox free | 88±5 | 100 |
| DoxM1 | 5±1 | 19±2 |
| DoxM2 | 11±2 | 22±3 |
| DoxM3 | 29±4 | 64±5 |
| DoxMC1 | 8±1 (0 mM GSH) 10±1 (1 mM GSH) 37±4 (10 mM GSH) |
16±3 (0 mM GSH) 25±4 (1 mM GSH) 64±7 (10 mM GSH) |
| DoxMC2 | 8±1 (0 mM GSH) 16±2 (1 mM GSH) 25±2 (10 mM GSH) |
13±2 (0 mM GSH) 28±3 (1 mM GSH) 54±5 (10 mM GSH) |
| Dox formulation | CDox = 50 µM | CDox = 5 µM | ||
|---|---|---|---|---|
| 1 day | 3 day | 1 day | 3 day | |
| Dox free | 30±3 | 4.3±0.5 | 33±2 | 5±1 |
| Dox M1 | 31±2 | < 1 | 43±4 | 3.3±0.3 |
| Dox M2 | 26±3 | 40±5 | 4.1±0.7 | |
| Dox M3 | 14±1 | 23±1 | 2.9±0.2 | |
| Dox MC1 | 54±5 | 6.4±1.2 | 69±8 | 29±5 |
| Dox MC2 | 57±8 | 5.3±1.1 | 81±6 | 21±3 |
| Dox containing micellar formulation | Permeability to eukaryotic cells | Toxicity to eukaryotic cells | Tumor-sensitivity | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Brief designation | Chemical composition | Cancer K562 | Cancer Raji | Cancer A875 | Normal HEK293T | Cancer K562 | Normal HEK293T | pH 5.5–6.5 | glutathione |
| Dox | Dox free | + | + | ± | + | + | + | – | – |
| DoxM1 | Dox in Chit5-LA | ++ | ± | + | ± | ++ | ± | + | + |
| DoxM2 | Dox in Chit5-OA | + | + | + | ± | ++ | ± | + | – |
| DoxM3 | Dox in Hep-OA | ++ | ++ | + | ± | ++ | ± | ± | – |
| DoxMC1 | Dox-GSSG-Chit5-OA | + | ++ | ++ | – | + | –+ | + | ++ |
| DoxMC2 | Dox-SS-LA-Chit5 | + | ++ | + | – | + | –+ | + | ++ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





