1. Introduction
The incidence of Chlamydia Trachomatis (CT) and Neisseria gonorrhoeae (NG) is increasing in many European countries 1,2 and elsewhere 3,4, with an raising concern regarding NG, which has developed resistance to all classes of antibiotics it has been exposed to, including the currently recommended therapies 5–7. Around half of the reported gonorrhea cases in European countries 1 (48%) and the US 3 (47%) are attributed to men who have sex with men (MSM).
Several modelling studies have described the transmission of CT and NG among MSM 8–45, which cluster in a few western countries, mainly from the US 9,11,17–19,21,28,29,41,42 and Australia 10,14–16,25,34–37. In Europe, notable modelling studies have been conducted in the UK 24,30,32,39 and Netherlands 22,23,26,33,38,45, with few papers from France 27, Belgium 8,44 and Switzerland 12,13. The majority of the published models from Europe are compartmental models, with only a hand-full of models using individual-based or network models 8,22,23,33,39,44. While the usefulness of compartmental models is undeniable, they lack both the complexity of the transmission mechanisms of STIs, and the fine-grain detail of individual characteristics that individual-based and network models exhibit.
Many models mention the lack of parameters in literature, to inform simulation models, leading to limitations in the validity and interpretation of the results 8,10,18,22,25,27,28,34,35,37,39,44,45. Besides transmission probabilities, that are difficult to calculate in a clinical setting, high quality clinical parameters such as the probability of symptoms and time intervals until recovery are not readily available in literature, especially reported by different anatomical sites 46,47. Another set of important parameters that are sparse in literature, are parameters critical to the structure of the sexual network, i.e. partnership duration and homophily rates. The role of homophily, or tendency of people to form sexual partnerships or other kinds of social bonds with persons similar to them in terms of various characteristics has been well established in the social network literature 48–52. These parameters are vital for the validity of the results. If the underlying network is mis-specified, one cannot guarantee that the model behavior is due to the mechanisms included and their parameters, or due to the structure of the network. A limited number of cohort and network cross-sectional studies are cited in individual-based and network models, in terms of partnership duration and homophily rates in the US 53,54 and Australia 55. In a European setting, estimates of partnership durations, came from a series of modeling papers from the Netherlands 22,23,33, where data from two Dutch studies were used to estimate the distributions of the duration of steady and casual partnerships. For the steady partnerships, a Weibull distribution was estimated with shape parameter 0.61 and scale 920, based on data from the Amsterdam Cohort Study (ACS) among MSM 56. Based on that we estimated an expected mean duration for steady partnerships of 1355 days. For casual partnerships, a Gamma distribution with shape 0.03 and rate 0.0002 was estimated based on the Network Study among MSM in Amsterdam data 57, yielding a mean duration of 155 days for casual partnerships.
Model calibration is widely used to estimate parameters that are difficult to find in literature, i.e. transmission probabilities. In this paper, we aim to use model calibration to estimate the average partnership duration and homophily rates among MSM in Belgium, in order to match the cumulative number of sex partners.
2. Methods
2.1. Data
Data from the Belgian-based participants of the European MSM Internet Survey (EMIS) 2017 were the primary data source for network structure and behavioral parameters used in the model. EMIS was an anonymous, self-administered online survey conducted in 50 countries and 33 languages. Participants were recruited through dating apps and other social networking websites targeting MSM. The methods of EMIS-2017 study have been described in detail elsewhere 58. In total, questionnaire data from 2763 persons based in Belgium were used to estimate parameters, such as information on partnership status, behavioral and epidemiological characteristics.
2.2. Overview
We developed a network model to describe sex acts among MSM in Belgium. Separable Temporal Exponential-family Random Graph Models (STERGMs)
59–61 were used to fit and simulate the structure of the sexual partnership network. The model was developed as an extension of the EpiModel platform (
www.epimodel.org).
Three different definitions for high sexual activity that were previously used in other modelling studies were included as scenarios in the model: 1) Eligibility to PrEP
44, 2) individuals reporting more than 15 partners
62, and 3) individuals reporting more than 15 casual partners
63. Individuals in the population were categorized into high- and low-activity (HA-MSM and LA-MSM, respectively). Eligibility criteria for PrEP in Belgium are reporting unprotected anal sex with one or more partners in the last 6 months, acquisition of multiple STIs in the last year, receiving post-exposure prophylaxis for HIV in the last year and use of psychotropic substances during sexual activities (
Online Supplement). Based on the EMIS-2017 data, we estimated that 34.6% (32.87–36.45 95% CI) of the Belgian MSM population would be eligible to receive Pre-Exposure Prophylaxis (PrEP). This estimate is similar to estimates from previously published studies from Belgium and Europe
62,64,65. According to the other two definitions of high-activity MSM, 30.41% (28.69–32.19 95% CI) and 27.90% (26.23–29.64 95% CI) of the EMIS-2017 participants reported more than 15 total and casual partners over a 12 months period respectively. Thus, 34.6%, 30.41% and 27.90% of the model population was classified as HA-MSM in the three scenarios respectively and the remaining was classified as LA-MSM.
The model consisted of three parallel, interacting networks representing steady, persistent casual and one-off (one-night stand) partnerships. The term “steady partners” was used to describe husbands, boyfriends or the partners with whom EMIS participants would not describe themselves as single. Persistent casual partners would be the partners that would not qualify as steady, but the EMIS participants would have sex with, more than one time. One-off partners would be casual partners that EMIS participants would only have sex with once. All definitions, processes and parameters in the model are described in detail in the Online Supplement.
2.3. Partnership Formation and Homophily
The formation of partnerships in all three networks (steady, casual, and one-off) was governed by similar formation equations, in order to be able to preserve the distinct behavioral characteristics linked to each partnership type. The formation of steady (and casual) partnerships was associated with the total number of steady (casual) partnerships currently in the network, the proportion of concordant partnerships (HA-MSM with HA-MSM, or LA-MSM with LA-MSM) different for each group, the proportion of individuals with concurrent partners (2 or more active partnerships simultaneously) and their status regarding casual (steady) partners (proportion of individuals with 0, 1, or more than 1 casual (steady) partners). The formation of one-off partnerships depended on the total number of one-off partnerships, the proportion of concordant partnerships (different for each group), the proportion of individuals with 0, 1 or more than 1 steady partners, and the proportion of individuals with 0, 1, or more than 1 casual partners. All those characteristics were targeted to match observed statistics from the EMIS 2017 dataset for each group and partnership type and the underlying network was fitted so that they would be held constant over time.
The number of ongoing partnerships (steady and persistent casual) and their combination was estimated using the EMIS-2017 dataset. We allowed each individual in the model to have zero, one or more than one steady partner and zero, one or more than one casual partners at any given time step.
For both steady and persistent casual partnerships, there was a constant hazard of relationship dissolution, modeled as a memoryless process. For steady partnerships, we used a constant hazard depending on the total number of partnerships present in the network. For casual partners, the dissolution of partnerships depended on the activity group of the two partners in a dyad (different for the HA- and LA-MSM). The duration of one-off partnerships was set to 1 day.
2.4. Homophily
Regarding homophily, we adopted the premise from the paper of Hansson et al. 62 that the number of HA-individuals having LA-partners should be the same as the number of LA-individuals having a HA-partner within the same MSM population, to calculate the ratio of the homophily rates between the two groups, for each type of partnership type. The process of deducting the final equations is shown in detail in the Online Supplement.
2.5. Sex Acts
At each time step, the number of sexual acts that occurred between two partners was calculated by random draws from a Bernoulli distribution with a success probability depending on the type of partnership and the activity-group of the two partners. Each sex act could be a combination of six sex types: oral, oro-anal and anal sex, each of which could be insertive or receptive. For each sex act, a combination of sex types was randomly assigned based on the frequency reported among EMIS 2017 participants (
Online Supplement Table S7).
2.6. Model Calibration
The model simulated a population of 10 000 MSM in Belgium. Parameters for partnership duration and homophily rates were not available in the EMIS data. We opted to use the cumulative number of partners per partnership type and group over a period of 12 months as a measure of goodness-of-fit for our model. Approximate Bayesian computation with sequential Monte Carlo (ABC-SMC) sampling 66–69 was used to estimate the unknown parameters. The ABC-SMC method returns posterior distributions of the parameters of interest after defining prior distributions. The Lenormand method of the EasyABC package 70 (Version 1.5) was used for the parameter estimation.
3. Results
Distribution of Cumulative Sex Partners
The total numbers of steady and casual partners over a period of 12 months are reported in the EMIS 2017 dataset as a categorical variables: 0, 1, 2, …, 9, or 10 or more for steady and 0, 1, 2, …, 10, 11–20, 21–30, 31–40, 41–50, or more than 50 for casual partners. Assuming at most 12 steady partners over 12 months, we used the methodology and statistics described by Mendez-Lopez et al 71, to build an algorithm to assign integer values to the total number of partners that match the mean (standard deviation) and median (interquartile range) for each category level and overall (Error! Reference source not found.). At each iteration of the algorithm, we randomly assigned persons reporting more than 10 steady partners into the categories 10, 11 or 12. For participants who had reported 10 or fewer casual partners, the sum of steady and casual partners was calculated. For those who reported more than 10 casual partners, the possible range of the sum of steady and casual partners was determined, and if the result spanned two EMIS categories (e.g. 11-20, 21-30, etc.), one of them was randomly selected with a probability based on the overlap of the two categories. Subsequently, random integers with the reported target mean and standard deviation were generated, and the resulting means and medians both by category and overall were compared to the target statistics. The algorithm iterated until an absolute sum of errors below 1.5 was produced. The produced statistics are presented in Error! Reference source not found.
Table 1.
Target and produced statistics for number of partners in the past 12 months, overall and by category.
Table 1.
Target and produced statistics for number of partners in the past 12 months, overall and by category.
| |
Target statistics (Mendez-Lopez et al, 2022) |
Estimated statistics |
| Number of partners in the past 12 months |
Mean (SD) |
Median (IQR) |
Mean (SD) |
Median (IQR) |
| Overall |
15.8 (36.60) |
5 (2–15) |
16.8 (6.00) |
6 (2–19) |
| 11–20 |
16.4 (3.30) |
15 (14–20) |
16.4 (2.59) |
16 (15–19) |
| 21–30 |
27.8 (2.80) |
30 (25–30) |
27.8 (2.29) |
29 (26–30) |
| 31–40 |
38.6 (2.40) |
40 (37–40) |
38.3 (1.63) |
39 (37–40) |
| 41–50 |
49.6 (1.50) |
50 (50–50) |
49.1 (1.01) |
49 (49–50) |
| More than 50 |
128.2 (98.10) |
100 (75–150) |
129.0 (87.50) |
99.5 (55.25–172.50) |
With the newly estimated number of total partners, we could calculate the cumulative number of steady and casual partners per risk-group over 12 months. The number of one-off partners was calculated by multiplying the total number of casual partners with the proportion of EMIS participants reporting a one-off partnership in their last sexual encounter (
Online Supplement Table S4). The remaining casual partners were classified as persistent casual partners. The distributions of the cumulative number of partners per relationship type and group were summarized as medians and interquartile ranges, and were used as target statistics in the calibration process of the model.
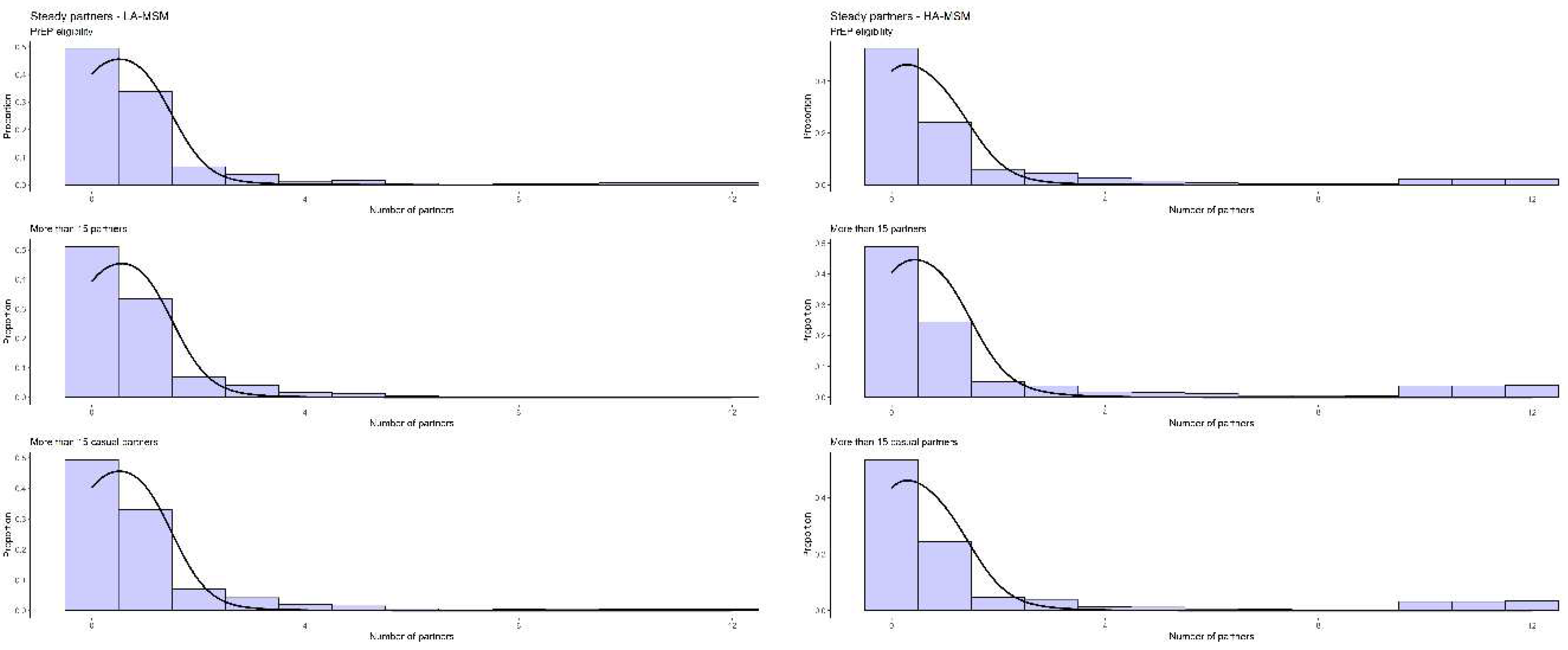
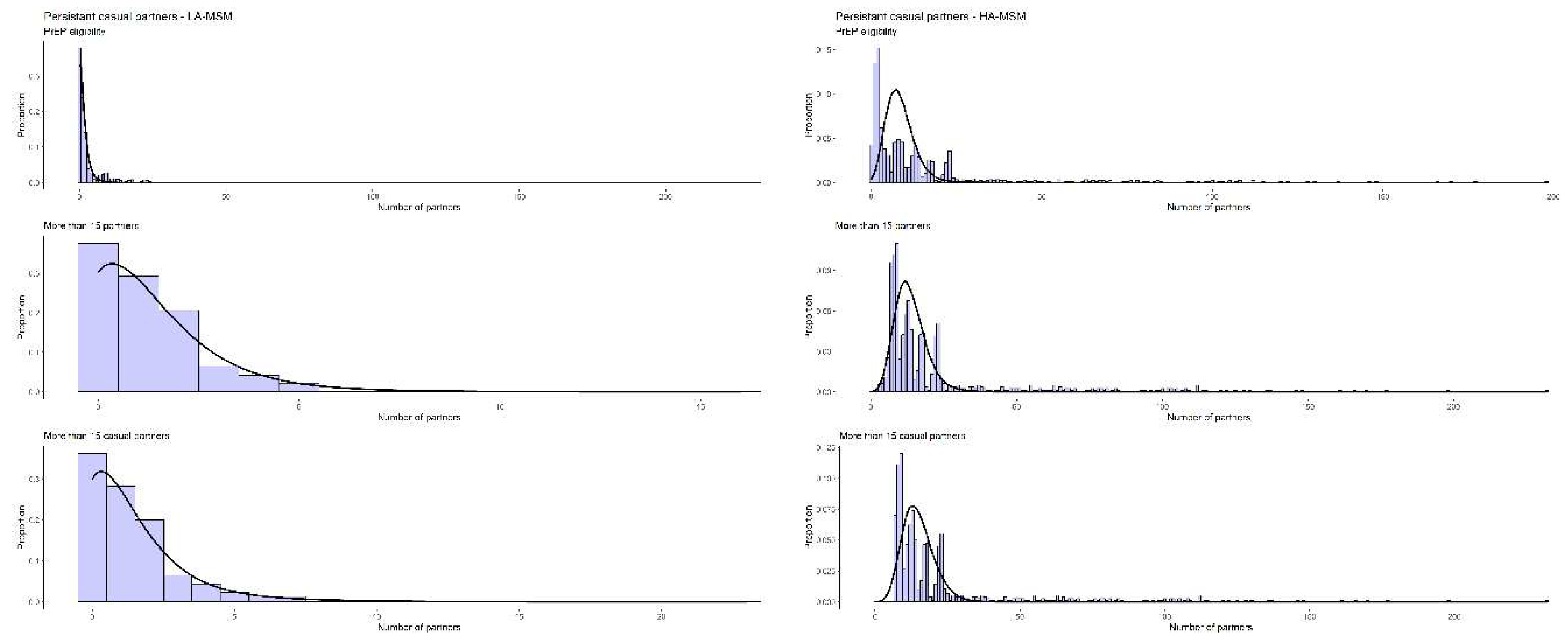
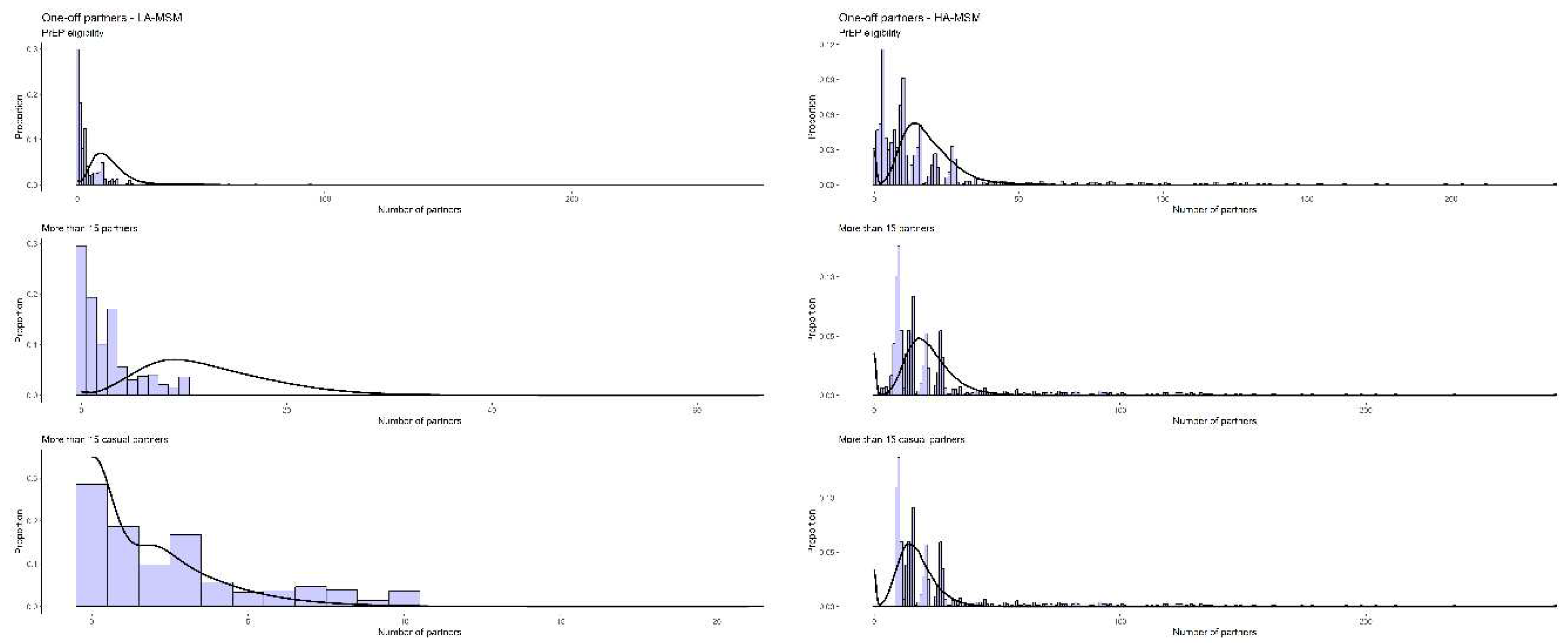
The final estimates for partnership durations were between 1065 and 1409 days for steady, and 4-6, 251-299 and 8-13 days for assortative HA-, LA- and mixed persistent casual partnerships, respectively, varying across the three definitions for activity group (Error! Reference source not found.). The estimated homophily rates for all three relationship types were high for steady and one-off partnership, for both activity groups, but lower for persistent casual partnerships (Error! Reference source not found.). The distributions of the observed and simulated cumulative number of partners in a period of 12 months is shown below, as a histogram for the EMIS reported partners and as a density plot for the simulated ones (
Figure 1,
Figure 2 and
Figure 3).
Table 2.
Final estimates for partnership duration and homophily rates based on model calibration.
Table 2.
Final estimates for partnership duration and homophily rates based on model calibration.
| |
|
Prior |
Weighted mean (95% CI) |
| PrEP eligibility |
Average duration of steady partnerships (in days) |
Uniform(800, 2000) |
1409 (1357 – 1462) |
| Average duration of casual partnerships between (in days) |
|
|
- -
Two HA-MSM |
Uniform(4, 15) |
6 (6 – 6) |
- -
Two LA-MSM |
Uniform(15, 500) |
251 (223 – 279) |
- -
A LA- and a HA-MSM |
Uniform(10, 30) |
13 (12– 13) |
| Homophily rates |
|
|
- -
Steady HA-MSM |
Uniform(0.55, 1) |
0.79 (0.76 – 0.81) |
- -
Steady LA-MSM |
Calculated from network |
0.90 |
- -
Casual HA-MSM |
Uniform(0.45, 1) |
0.65 (0.65 – 0.64) |
- -
Casual LA-MSM |
Calculated from network |
0.58 |
- -
One-off HA-MSM |
Uniform(0.45, 1) |
0.99 (0.98 – 0.99) |
- -
One-off LA-MSM |
Calculated from network |
0.99 |
| >15 partners |
Average duration of steady partnerships (in days) |
Uniform(800, 2000) |
1065 (1031 – 1099) |
| Average duration of casual partnerships between (in days) |
|
|
- -
Two HA-MSM |
Uniform(3, 100) |
4 (4 – 4) |
- -
Two LA-MSM |
Uniform(15, 500) |
299 (272 – 326) |
- -
A LA- and a HA-MSM |
Uniform(5, 100) |
11 (11 – 11) |
- -
Homophily rates |
|
|
- -
Steady HA-MSM |
Uniform(0.55, 1) |
0.75 (0.73 – 0.78) |
- -
Steady LA-MSM |
Calculated from network |
0.90 |
- -
Casual HA-MSM |
Uniform(0.60, 1) |
0.68 (0.67 – 0.69) |
- -
Casual LA-MSM |
Calculated from network |
0.35 |
- -
One-off HA-MSM |
Uniform(0.45, 1) |
0.98 (0.98 – 0.99) |
- -
One-off LA-MSM |
Calculated from network |
0.98 |
| >15 casual partners |
Average duration of steady partnerships (in days) |
Uniform(800, 2000) |
1314 (1260 – 1367) |
| Average duration of casual partnerships between (in days) |
|
|
- -
Two HA-MSM |
Uniform(3, 100) |
4 (4 – 4) |
- -
Two LA-MSM |
Uniform(15, 500) |
266 (244 – 289) |
- -
A LA- and a HA-MSM |
Uniform(5, 100) |
8 (8 – 9) |
| Homophily rates |
|
|
- -
Steady HA-MSM |
Uniform(0.55, 1) |
0.77 (0.74 – 0.79) |
- -
Steady LA-MSM |
Calculated from network |
0.92 |
- -
Casual HA-MSM |
Uniform(0.45, 1) |
0.69 (0.68 – 0.7) |
- -
Casual LA-MSM |
Calculated from network |
0.48 |
- -
One-off HA-MSM |
Uniform(0.45, 1) |
0.98 (0.98 – 0.99) |
- -
One-off LA-MSM |
Calculated from network |
0.98 |
4. Discussion
We estimated the average partnership durations among MSM in Belgium, distinguishing for the activity group, by employing three different definitions that have been used in previous modelling studies. Estimates for partnership durations and homophily rates are similar in all 3 scenarios, indicating quite robust results. The estimates for the duration of steady partnerships were comparable to the data reported by the ACS study 56 (1355 days), as well as well as studies from Hui et al 14–16 and Kasaie et al 18, all reporting an average duration of 4 years. The average duration for persistent causal partnerships, was affected by the activity group of the two partners, with much shorter duration if one of the two partners was HA-MSM. The durations varied between 4-6 and 8-13 for a HA-MSM assortative and disassortative partnership respectively, and were in the same order of magnitude to the 12–14 days reported by Hui et al 14, but different enough to be considered as a consistent result. Similarly, the duration of varied between 251–299 days (between two LA-MSM individuals) and could not be considered close to the 155 days reported by Heymans et al 57. Homophily rates in the literature rarely reflect on activity or risk-groups 33 and more often refer to racial, religious or socioeconomic mixing 9,28,29,41,72,73. However, the homophily rates reported from a Dutch modelling paper were similar to our findings (75% for steady and 60% for casual partnerships) 33.
Many studies have mentioned in their limitations the lack of available high-quality social network and behavioral parameters 8,10,18,22,25,27,28,34,35,37,39,44,45. In this paper, we present an alternative approach to estimate underlying networks, even with the lack of high-quality social network parameters. Although the focus of this paper is the structure of the underlying sexual network among Belgian participants of EMIS-2017, the same methodology could be applied to the other countries where EMIS-2017 or similar data exist. Such an experiment, would allow researchers to estimate partnership durations and homophily rates in their respective networks or highlight the areas that could prohibit such an effort.
Although the scenario defining individuals reporting more than 15 partners in a period of 12 months as the higher-activity group gave a better fit between simulated and observed number of partners, there is still a visible mismatch between simulated and observed numbers of cumulative partners, that one could argue against the validity of the results. Both the nature of the data and the structure of the model could be suspect in our case. The EMIS-2017 data were collected among individuals using dating apps or other social media, likely yielding biased results towards the more outgoing MSM. In our effort to match the observed statistics, the model gives the best possible output to that end, though the fit is imperfect. The second factor for the mismatch is the specification of the model, both in terms of information needed to specify the mixing mechanism among MSM in our network and in terms of the definition of the sub-groups. Unfortunately, more detailed information regarding the partnership formation were not available in the EMIS-2017 dataset. More comprehensive surveys would be required to highlight the mixing mechanisms among MSM, taking into account cultural and behavioural differences among countries. In our study, the MSM population was divided into two groups, representing different levels of sexual activity, using three different definitions that have been previously used in modelling studies. Both the number of activity-groups and the definition of each group, affect drastically the structure of the assumed underlying network. The mismatch between the observed and simulated data, especially in the casual and one-off partnerships, might indicate the presence of more than 2 sub-groups in the population, which should be investigated further in future studies. Such attempts, though, could be challenging since the number of groups is uncertain and could differ among countries.
The other main limitation of our model is paradoxically the same that we were trying to rectify. Although the EMIS 2017 data is the most detailed pan-European dataset reporting MSM behaviour to our knowledge, many of the parameters in the model regarding behavioral characteristics were deduced, by making assumptions or by combining information in the available dataset. The need for additional high-quality data of sexual behaviour that includes behaviour of the study participants and their partners remains high, especially in a public health setting where transmission and social network modeling is becoming more and more frequent.
Notwithstanding this limitation, our study has two important findings. First, we can estimate relatable partnership durations for all three partnership types in our network, to be able to re-create a well-defined behavioral statistic, such as total number of partners. Second, we calculated that the ratio of homophily rates between the two activity groups is constant and can be quantified using information from the assumed underlying network.
The majority of the studies that provide information on model parameters come from cross-sectional or cohort studies 53–57. A few studies collecting egocentric data have been published recently 74–76. Egocentric data are collected by members of the population who share information about themselves (ego) and about other members with whom they interact (alters). These studies have been designed to produce parameters to inform models, thus making them the most suitable type of studies. A long list of scientists have reported a lack of good quality data, that could inform transmission models 18,21,37,39. We would like to join this call for design and conduct of studies to inform parameters of transmission models and prove or disprove the estimated parameters from our study.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, Achilleas Tsoumanis, Niel Hens and Christophe Van Dijck; Data curation, Achilleas Tsoumanis; Methodology, Achilleas Tsoumanis and Christophe Van Dijck; Software, Achilleas Tsoumanis; Supervision, Niel Hens and Christophe Van Dijck; Writing – original draft, Achilleas Tsoumanis; Writing – review & editing, Win Vanden Berghe, Niel Hens and Christophe Van Dijck.
Funding
EMIS-2017 was carried out as part of ESTICOM, under the service contract 2015 71 01 with The Consumers, Health, Agriculture and Food Executive Agency (Chafea), acting under powers delegated by the Commission of the European Union. The contract arises from the Call for tender No Chafea/2015/Health/38. CVD is a fellow of the Research Foundation Flanders (FWO 12B1M24N).
Institutional Review Board Statement
EMIS-2017 received a favourable ethical opinion from the Observational Research Ethics Committee at the London School of Hygiene and Tropical Medicine (review reference 14421 /RR/8805) on 31 July 2017.
Acknowledgments
The authors would like to thank the Belgian EMIS participants who took part in EMIS-2017 as well as the EMIS partners for their efforts in the EMIS study (Europe: PlanetRomeo, European AIDS Treatment Group (EATG), Eurasian Coalition on Male Health (ECOM), European Centre for Disease Prevention and Control (ECDC), European Monitoring Centre for Drugs & Drug Addiction (EMCDDA), European Commission (DG SANTE), Belgium: SENSOA, exaequo, Observatoire du SIDA et des sexualités, Sciensano). EMIS-2017 was coordinated by Sigma Research at the London School of Hygiene and Tropical Medicine (LSHTM) in association with the Robert Koch Institute (RKI) in Berlin. EMIS core team @ Sigma Research (LSHTM): Dr Axel J. Schmidt, Dr Ford Hickson; David Reid, and Peter Weatherburn; in association with Dr Ulrich Marcus and Susanne B. Schink @ RKI. Last, we would like to thank Dr. Peter Weatherburn and Dr. Axel J. Schmidt, for reviewing and approving the manuscript on behalf of the EMIS consortium. The resources and services used in this work were provided by the VSC (Flemish Supercomputer Center), funded by the Research Foundation - Flanders (FWO) and the Flemish Government. Last, the authors would like to thank Dr. Chris Kenyon for his valuable feedback and suggestions.
Conflicts of interest: The authors declare no conflicts of interest.
References
- European Centre for Disease Prevention and Control (ECDC). European Centre for Disease Prevention and Control (ECDC). Gonorrhoea. Annual Epidemiological Report for 2018. Eur. Cent. Dis. Prev. Control. 2020, 1–4. 2018. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/gonorrhoea-annual-epidemiological-report-2018.pdf.
- European Centre for Disease Prevention and Control (ECDC). italic>Chlamydia Infection - Annual Epidemiological Report. for 2019; 2022.
- Centre for Disease Prevention and Control (CDC). Sexually Transmitted Disease Surveillance 2019. 2021.
- Centre for Disease Prevention and Control (CDC). Sexually Transmitted Disease Surveillance 2018. Sexually Transmitted Disease Surveillance 2018, 2019. [CrossRef]
- Low, N.; Unemo, M.; Skov Jensen, J.; Breuer, J.; Stephenson, J.M. Molecular Diagnostics for Gonorrhoea: Implications for Antimicrobial Resistance and the Threat of Untreatable Gonorrhoea. PLoS Med. 2014, 11. [Google Scholar] [CrossRef] [PubMed]
- Kirkcaldy, R.D.; Harvey, A.; Papp, J.R.; et al. Neisseria gonorrhoeae antimicrobial susceptibility surveillance - The Gonococcal Isolate Surveillance Project, 27 sites, United States, 2014. MMWR Surveill Summ. 2016, 65, 1–24. [Google Scholar] [CrossRef] [PubMed]
- STD Prevention Conference [Press Release]. New Warning Signs that Gonorrhea Treatment May be Losing Effectiveness. In: ; 2016.
- Buyze, J.; Vanden Berghe, W.; Hens, N.; Kenyon, C. Current levels of gonorrhoea screening in MSM in Belgium may have little effect on prevalence: A modelling study. Epidemiol. Infect. 2018, 146, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Earnest, R.; Rönn, M.M.; Bellerose, M.; et al. Population-level Benefits of Extragenital Gonorrhea Screening among Men Who Have Sex with Men: An Exploratory Modeling Analysis. Sex. Transm. Dis. 2020, 47, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Duan, Q.; Carmody, C.; Donovan, B.; et al. Modelling response strategies for controlling gonorrhoea outbreaks in men who have sex with men in Australia. PLoS Comput. Biol. 2021, 17, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Escobar, E.; Durgham, R.; Dammann, O.; Stopka, T. Agent-based computational model of the prevalence of gonococcal infections after the implementation of HIV pre-exposure prophylaxis guidelines. Online J. Public. Health Inform. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Fingerhuth, S.M.; Bonhoeffer, S.; Low, N.; Althaus, C.L. Antibiotic-Resistant Neisseria gonorrhoeae Spread Faster with More Treatment, Not More Sexual Partners. PLoS Pathog. 2016, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Fingerhuth, S.M.; Low, N.; Bonhoeffer, S.; Althaus, C.L. Detection of antibiotic resistance is essential for gonorrhoea point-of-care testing: A mathematical modelling study. BMC Med. 2017, 15, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hui, B.; Fairley, C.K.; Chen, M.; et al. Oral and anal sex are key to sustaining gonorrhoea at endemic levels in MSM populations: A mathematical model. Sex. Transm. Infect. 2015, 91, 365–369. [Google Scholar] [CrossRef]
- Hui, B.B.; Whiley, D.M.; Donovan, B.; Law, M.G.; Regan, D.G. Identifying factors that lead to the persistence of imported gonorrhoeae strains: A modelling study. Sex. Transm. Infect. 2017, 93, 221–225. [Google Scholar] [CrossRef]
- Hui, B.B.; Padeniya, T.N.; Rebuli, N.; et al. A Gonococcal Vaccine Has the Potential to Rapidly Reduce the Incidence of Neisseria gonorrhoeae Infection among Urban Men Who Have Sex with Men. J. Infect. Dis. 2022, 225, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.; Weiss, K.; Mermin, J.; et al. Proportion of Incident Human Immunodeficiency Virus Cases among Men Who Have Sex with Men Attributable to Gonorrhea and Chlamydia: A Modeling Analysis. Sex. Transm. Dis. 2019, 46, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Kasaie, P.; Schumacher, C.M.; Jennings, J.M.; et al. Gonorrhoea and chlamydia diagnosis as an entry point for HIV pre-exposure prophylaxis: A modelling study. BMJ Open. 2019, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Reichert, E.; Grad, Y.H. Resistance and Prevalence Implications of Doxycycline Post-Exposure Prophylaxis for Gonorrhea Prevention in Men Who Have Sex with Men: A Modeling Study; 2023. [CrossRef]
- Kretzschmar, M.; Van Duynhoven, Y.T.H.P.; Severijnen, A.J. Modeling prevention strategies for gonorrhea and chlamydia using stochastic network simulations. Am. J. Epidemiol. 1996, 144, 306–317. [Google Scholar] [CrossRef] [PubMed]
- Reichert, E.; Yaesoubi, R.; Rönn, M.M.; Gift, T.L.; Salomon, J.A.; Grad, Y.H. Resistance-minimising strategies for introducing a novel antibiotic for gonorrhoea treatment: a mathematical modelling study. Lancet Microbe 2023, 4, e781–e789. [Google Scholar] [CrossRef] [PubMed]
- Reitsema, M.; Hoek AJVan Van Der Loeff, M.S.; et al. Preexposure prophylaxis for men who have sex with men in the Netherlands: Impact on HIV and Neisseria gonorrhoeae transmission and cost-effectiveness. Aids 2020, 34, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Reitsema, M.; Heijne, J.; Visser, M.; et al. Impact of frequent testing on the transmission of HIV and N. gonorrhoeae among men who have sex with men: A mathematical modelling study. Sex. Transm. Infect. 2020, 96, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Riou, J.; Althaus, C.L.; Allen, H.; et al. Projecting the development of antimicrobial resistance in Neisseria gonorrhoeae from antimicrobial surveillance data: a mathematical modelling study. BMC Infect. Dis. 2023, 23, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Spicknall, I.H.; Mayer, K.H.; Aral, S.O.; Romero-Severson, E.O. Assessing Uncertainty in an Anatomical Site-Specific Gonorrhea Transmission Model of Men Who Have Sex with Men. Sex. Transm. Dis. 2019, 46, 321–328. [Google Scholar] [CrossRef]
- Van Wifferen, F.; Hoornenborg, E.; Schim Van Der Loeff, M.F.; Heijne, J.; Van Hoek, A.J. Cost-effectiveness of two screening strategies for Chlamydia trachomatis and Neisseria gonorrhoeae as part of the PrEP programme in the Netherlands: A modelling study. Sex. Transm. Infect. 2021, 97, 607–612. [Google Scholar] [CrossRef]
- Voirin, N.; Allam, C.; Charre, C.; et al. Optimizing Strategies for Chlamydia trachomatis and Neisseria gonorrhoeae Screening in Men Who Have Sex with Men: A Modeling Study. Clin. Infect. Dis. 2020, 70, 1966–1972. [Google Scholar] [CrossRef]
- Weiss, K.M.; Jones, J.S.; Anderson, E.J.; et al. Optimizing Coverage vs Frequency for Sexually Transmitted Infection Screening of Men Who Have Sex with Men. Open Forum Infect. Dis. 2019, 6. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.M.; Jones, J.S.; Katz, D.A.; et al. Epidemiological Impact of Expedited Partner Therapy for Men Who Have Sex With Men: A Modeling Study. Sex. Transm. Dis. 2019, 46, 697–705. [Google Scholar] [CrossRef]
- Whittles, L.K.; White, P.J.; Didelot, X. Estimating the fitness cost and benefit of cefixime resistance in Neisseria gonorrhoeae to inform prescription policy: A modelling study. PLoS Med. 2017, 14, 1–20. [Google Scholar] [CrossRef]
- Garnett, G.P.; Mertz, K.J.; Finelli, L.; Levine, W.C.; St Louis, M.E. The transmission dynamics of gonorrhoea: Modelling the reported behaviour of infected patients from Newark, New Jersey. Philos. Trans. R. Soc. B Biol. Sci. 1999, 354, 787–797. [Google Scholar] [CrossRef]
- Whittles, L.K.; White, P.J.; Didelot, X. Assessment of the Potential of Vaccination to Combat Antibiotic Resistance in Gonorrhea: A Modeling Analysis to Determine Preferred Product Characteristics. Clin. Infect. Dis. 2020, 71, 1912–1919. [Google Scholar] [CrossRef]
- Xiridou, M.; Heijne, J.; Adam, P.; et al. How the Disruption in Sexually Transmitted Infection Care Due to the COVID-19 Pandemic Could Lead to Increased Sexually Transmitted Infection Transmission Among Men Who Have Sex With Men in The Netherlands: A Mathematical Modeling Study. Sex. Transm. Dis. 2022, 49, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Chow, E.P.F.; Ong, J.J.; et al. Chlamydia trachomatis transmission between the oropharynx, urethra and anorectum in men who have sex with men: a mathematical model. BMC Med. 2020, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Chow, E.P.F.; Shen, M.; et al. Potential effect of antiseptic mouthwash on the incidence of Neisseria gonorrhoeae among men who have sex with men: A mathematical modelling study. BMJ Open 2021, 11. [Google Scholar] [CrossRef]
- Xu, X.; Chow, E.P.F.; Ong, J.J.; et al. Modelling the contribution that different sexual practices involving the oropharynx and saliva have on Neisseria gonorrhoeae infections at multiple anatomical sites in men who have sex with men. Sex. Transm. Infect. 2021, 97, 183–189. [Google Scholar] [CrossRef]
- Zhang, L.; Regan, D.G.; Chow, E.P.F.; et al. Neisseria gonorrhoeae Transmission among Men Who Have Sex with Men: An Anatomical Site-Specific Mathematical Model Evaluating the Potential Preventive Impact of Mouthwash. Sex. Transm. Dis. 2017, 44, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Zwart, J.M.; Mangen, M.J.J.; Bartelsman, M.; Van Rooijen, M.S.; De Vries, H.J.C.; Xiridou, M. Microscopic examination of Gram-stained smears for anogenital gonorrhoea in men who have sex with men is cost-effective: Evidence from a modelling study. Sex. Transm. Infect. 2019, 95, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Zienkiewicz, A.K.; Verschueren Van Rees, N.; Homer, M.; et al. Agent-based modelling study of antimicrobial-resistant Neisseria gonorrhoeae transmission in men who have sex with men: Towards individualised diagnosis and treatment. Sex. Health. 2019, 16, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Tuite, A.R.; Rönn, M.M.; Wolf, E.E.; et al. Estimated Impact of Screening on Gonorrhea Epidemiology in the United States: Insights from a Mathematical Model. Sex. Transm. Dis. 2018, 45, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Jenness, S.M.; Weiss, K.M.; Goodreau, S.M.; et al. Incidence of gonorrhea and chlamydia following human immunodeficiency virus preexposure prophylaxis among men who have sex with men: A modeling study. Clin. Infect. Dis. 2017, 65, 712–718. [Google Scholar] [CrossRef] [PubMed]
- Yaesoubi, R.; Cohen, T.; Hsu, K.; et al. Adaptive guidelines for the treatment of gonorrhea to increase the effective life span of antibiotics among men who have sex with men in the United States: A mathematical modeling study. PLoS Med. 2020, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Tuite, A.R.; Gift, T.L.; Chesson, H.W.; Hsu, K.; Salomon, J.A.; Grad, Y.H. Impact of rapid susceptibility testing and antibiotic selection strategy on the emergence and spread of antibiotic resistance in Gonorrhea. J. Infect. Dis. 2017, 216, 1141–1149. [Google Scholar] [CrossRef] [PubMed]
- Tsoumanis, A.; Van Dijck, C.; Hens, N.; Kenyon, C. Rethinking Screening Intensity in Terms of Reducing Prevalence or Increasing Selection Pressure for the Emergence of Resistant Gonorrhea: A Modeling Study of Men Who Have Sex With Men in Belgium. Open Forum Infect. Dis. 2023, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bartelsman, M.; Vaughan, K.; van Rooijen, M.S.; de Vries, H.J.C.; Xiridou, M. Impact of point-of-care management on the transmission of anogenital gonococcal infections among men who have sex with men in Amsterdam: a mathematical modelling and cost-effectiveness study. Sex. Transm. Infect. 2018, 94, 174–179. [Google Scholar] [CrossRef]
- Barbee, L.A.; Khosropour, C.M.; Soge, O.O.; et al. The Natural History of Rectal Gonococcal and Chlamydial Infections: The ExGen Study. Clin. Infect. Dis. 2022, 74, 1549–1556. [Google Scholar] [CrossRef]
- Barbee, L.A.; Soge, O.O.; Khosropour, C.M.; et al. The Duration of Pharyngeal Gonorrhea: A Natural History Study. Clin. Infect. Dis. 2021, 73, 575–582. [Google Scholar] [CrossRef]
- Krivitsky, P.N.; Handcock, M.S.; Morris, M. Adjusting for network size and composition effects in exponential-family random graph models. Stat. Methodol. 2011, 8, 319–339. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Lu, X. Network evolution of a large online MSM dating community: 2005–2018. Int. J. Environ. Res. Public. Health. 2019, 16. [Google Scholar] [CrossRef] [PubMed]
- Currarini, S.; Vega Redondo, F. A Simple Model of Homophily in Social Networks Department of Economics A Simple Model of Homophily in Social Networks. 2011;(16).
- Cai, M.; Huang, G.; Kretzschmar, M.E.; Chen, X.; Lu, X. Extremely Low Reciprocity and Strong Homophily in the World Largest MSM Social Network. IEEE Trans. Netw. Sci. Eng. 2021, 8, 2279–2287. [Google Scholar] [CrossRef]
- Murase, Y.; Jo, H.H.; Török, J.; Kertész, J.; Kaski, K. Structural transition in social networks: The role of homophily. Sci. Rep. 2019, 9, 1–8. [Google Scholar] [CrossRef]
- Sullivan, P.S.; Rosenberg, E.S.; Sanchez, T.H.; et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann. Epidemiol. 2015, 25, 445–454. [Google Scholar] [CrossRef]
- Hernández-Romieu, A.C.; Sullivan, P.S.; Rothenberg, R.; et al. Heterogeneity of HIV Prevalence Among the Sexual Networks of Black and White Men Who Have Sex With Men in Atlanta. Sex. Transm. Dis. 2015, 42, 505–512. [Google Scholar] [CrossRef]
- Prestage, G.P.; Hudson, J.; Bradley, J.; et al. TOMS—Three or More Study.; 2008.
- Heijman, T.; Geskus, R.B.; Davidovich, U.; Coutinho, R.A.; Prins, M.; Stolte, I.G. Less decrease in risk behaviour from pre-HIV to post-HIV seroconversion among MSM in the combination antiretroviral therapy era compared with the pre-combination antiretroviral therapy era. Aids 2012, 26, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Heymans, R.; Matser, A.A.; Bruisten, S.M.; et al. Distinct neisseria gonorrhoeae transmission networks among men who have sex with men in Amsterdam, the Netherlands. J. Infect. Dis. 2012, 206, 596–605. [Google Scholar] [CrossRef]
- Weatherburn, P.; Hickson, F.; Reid, D.S.; Marcus, U.; Schmidt, A.J. European Men-Who-Have-Sex-With-Men Internet Survey (EMIS-2017): Design and Methods. Sex. Res. Soc. Policy. 2020, 17, 543–557. [Google Scholar] [CrossRef]
- Krivitsky, P.N.; Handcock, M.S. A separable model for dynamic networks. J. R. Stat. Soc. Ser. B Stat. Methodol. 2014, 76, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.R.; Handcock, M.S.; Butts, C.T.; Goodreau, S.M.; Morris, M. ergm: A package to fit, simulate and diagnose exponential-family models for networks. J. Stat. Softw. [CrossRef]
- Goodreau, S.M.; Carnegie, N.B.; Vittinghoff, E.; et al. What Drives the US and Peruvian HIV Epidemics in Men Who Have Sex with Men (MSM)? PLoS One 2012, 7. [Google Scholar] [CrossRef] [PubMed]
- Hansson, D.; Strömdahl, S.; Leung, K.Y.; Britton, T. Introducing Pre-Exposure Prophylaxis to Prevent HIV Acquisition among Men Who Have Sex with Men in Sweden: Insights from a Mathematical Pair Formation Model. Vol 10.; 2020. [CrossRef]
- Cox, A.P.; Foss, A.M.; Shafer, L.A.; et al. Attaining realistic and substantial reductions in HIV incidence: Model projections of combining microbicide and male circumcision interventions in rural Uganda. Sex. Transm. Infect. 2011, 87, 635–639. [Google Scholar] [CrossRef] [PubMed]
- Buffel, V.; Reyniers, T.; Masquillier, C.; et al. Awareness of, Willingness to Take PrEP and Its Actual Use Among Belgian MSM at High Risk of HIV Infection: Secondary Analysis of the Belgian European MSM Internet Survey. AIDS Behav. 2022, 26, 1793–1807. [Google Scholar] [CrossRef] [PubMed]
- Sherriff, N.S.; Jones, A.M.; Mirandola, M.; et al. Factors related to condomless anal intercourse between men who have sex with men: Results from a European bio-behavioural survey. J Public Heal (United Kingdom). 2020, 42, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Toni, T.; Welch, D.; Strelkowa, N.; Ipsen, A.; Stumpf, M.P.H. Approximate Bayesian computation scheme for parameter inference and model selection in dynamical systems. J. R. Soc. Interface. 2009, 6, 187–202. [Google Scholar] [CrossRef]
- Held, L.; Hens, N.; O’Neil, P.; Wallinga, J. Handbook of Infectious Disease Data Analysis; Chapman and Hall/CRC, 2020. [Google Scholar] [CrossRef]
- Beaumont, M.A.; Cornuet, J.M.; Marin, J.M.; Robert, C.P. Adaptive approximate Bayesian computation. Biometrika 2009, 96, 983–990. [Google Scholar] [CrossRef]
- Sisson, S.A.; Fan, Y.; Tanaka, M.M. Sequential Monte Carlo without likelihoods (Proceedings of the National Academy of Sciences of the United States of America (2007) 104, 6, (1760-1765) DOI:10.1073/pnas.0607208104). Proc Natl Acad Sci USA, 2009; 106, 16889. [Google Scholar] [CrossRef]
- Jabot, F.; Faure, T.; Dumoulin, N. EasyABC: Efficient Approximate Bayesian Computation Sampling Schemes. Published online 2015.
- Mendez-Lopez, A.; Hickson, F.; Jansen, K.; et al. What is the empirical basis for converting banded ordinal data on numbers of sex partners among MSM into a continuous scale level variable? A secondary analysis of 13 surveys across 17 countries. BMC Med. Res. Methodol. 2022, 22, 1–7. [Google Scholar] [CrossRef]
- Kenyon, C.; Colebunders, R. Birds of a feather: Homophily and sexual network structure in sub-Saharan Africa. Int. J. STD AIDS. 2013, 24, 211–215. [Google Scholar] [CrossRef]
- Jones, J.; Le Guillou, A.; Gift, T.L.; et al. Effect of Screening and Treatment for Gonorrhea and Chlamydia on HIV Incidence Among Men Who Have Sex With Men in the United States: A Modeling Analysis. Sex. Transm. Dis. 2022, 49, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.M.; Goodreau, S.M.; Morris, M.; et al. Egocentric sexual networks of men who have sex with men in the United States: Results from the ARTnet study. Published online 2020. [CrossRef] [PubMed]
- Hansson, D.; Strömdahl, S. Estimating individual action dispositions using binary and frequency egocentric sexual network data. Stat. Neerl. 2020, 74, 242–260. [Google Scholar] [CrossRef]
- Cao, B.; Saffer, A.J.; Yang, C.; et al. MSM Behavior Disclosure Networks and HIV Testing: An Egocentric Network Analysis Among MSM in China. AIDS Behav. 2019, 23, 1368–1374. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).