1. Introduction
According to the latest data, cervical cancer ranks the fifth most common cancer in females in China [
1], which is still a huge threaten to Chinese women health. Human papillomavirus (HPV) infection is well known as the major reason of cervical cancer, while a few are non-HPV-related. Gastric-type endocervical adenocarcinoma (GAS) is a kind of non-HPV associated mucinous adenocarcinoma of the cervix, with low incidence rate whereas high malignancy and poor prognosis. Due to lack of sufficient diagnosis and treatment experience of GAS, some clinicians have not yet fully understood of this tumor. Here, we reported a case of GAS with "pelvic mass" as the initial symptom, which were endometriosis cysts confirmed by post-operative pathology. Through case report and literature review, the characteristics and current research progress of GAS were summarized, in order to provide references for diagnosis of GAS, and provide theoretical guidance for formulating reasonable treatment strategy and improving patient prognosis.
2. Case report
2.1. The clinical features of the patient during outpatient
The patient was a 44-year-old female who presented to the outpatient of our hospital in October 2023 with the chief complaint of "Discovering a pelvic mass by herself for one month." Vagino-recto-abdominal examination revealed cervical hypertrophy with a diameter of approximately 4.5 cm, and firm consistency. Bilateral adnexal areas palpated cystic masses, with the left mass measuring approximately 6 cm in diameter and the right mass measuring approximately 8 cm in diameter, with reduced mobility. ThinPrep cytologic test showed atypical glandular cells, suggestive of neoplastic transformation. HPV subtype 66 was positive. Since the abnormal cytology result and the infection of low risk HPV, cervical biopsy was performed. The biopsy pathology result revealed moderately differentiated adenocarcinoma with positive lymph vascular space invasion (LVSI). Immunohistochemistry (IHC) showed P16 (-), Ki-67 (approximately 15%). Based on the above results, the patient was hospitalized to accept further treatment.
2.2. The clinical features of the patient during hospitalization
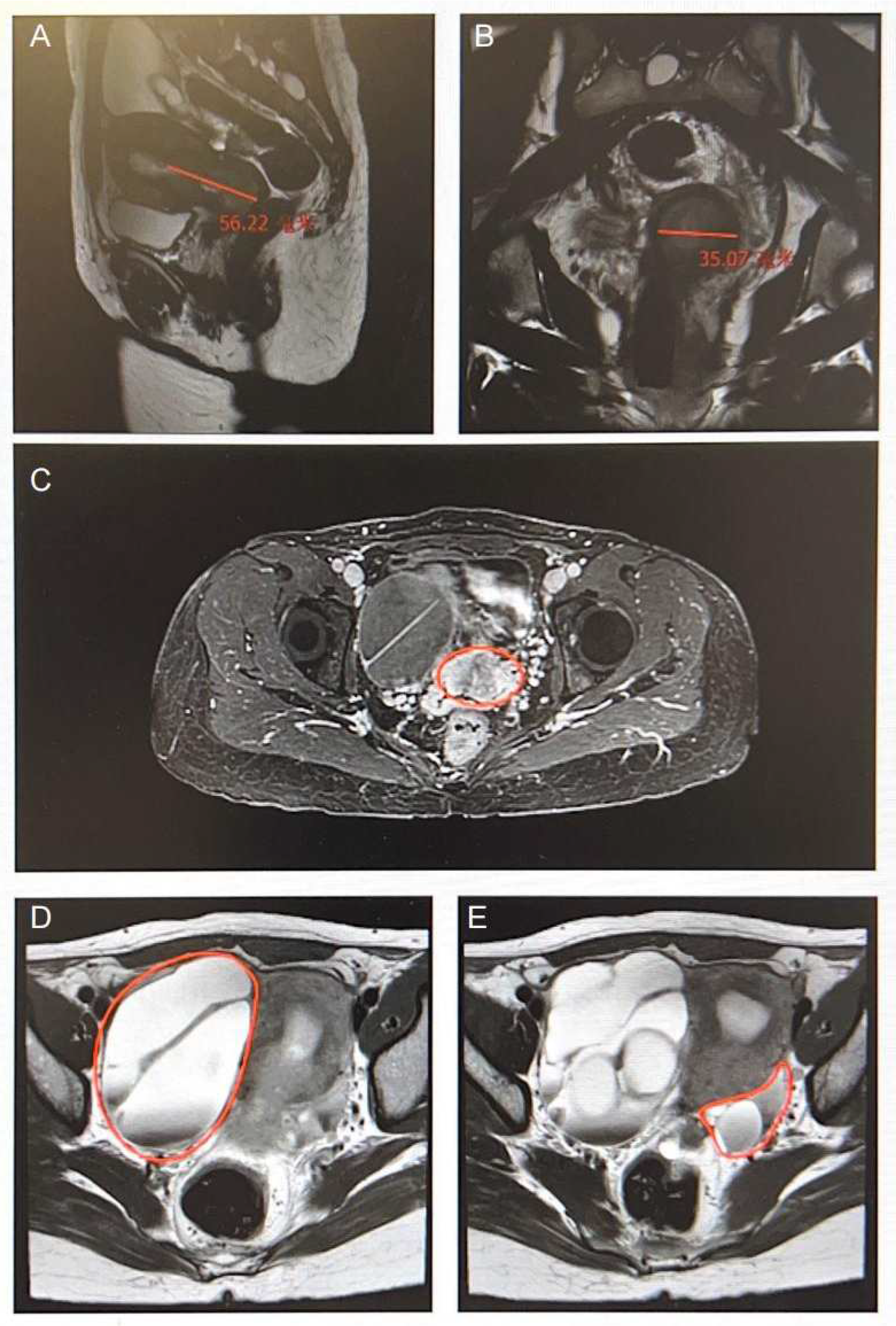
Tumor markers were elevated with CA19-9 at 360.00 U/ml and CA125 at 101.00 U/ml. Pelvic MRI showed irregular soft tissue mass from the lower segment of the uterine body to the cervix, 3.1×3.5×5.6 cm, with unclear boundaries and rough edges (
Figure 1 A, B), suggestive of a high possibility of cervical cancer, involving the cervical stroma, partially reaching the full layer (
Figure 1 C). Multiple separated cystic masses were observed in the bilateral adnexal areas, with the largest of 8.9×5.7 cm on the right side and several string-like cystic nodules on the left adnexal area, with the larger one of 2.4×1.8 cm, suggesting bilateral ovarian masses with accompanying hydrosalpinx, leaning towards metastatic tumors (
Figure 1 D, E). Multiple para-iliac vessels lymph nodes were found, with the largest of 0.5 cm in short diameter.
On October 17, 2023, the patient underwent radical abdominal hysterectomy with bilateral salpingo-oophorectomy, pelvic and para-aortic lymph node dissection. The intraoperative specimen revealed an irregular mass from the lower segment of the uterine body to the cervix, 4.5×1.8×0.5 cm, with a firm consistency, suspected involvement of the full layer of the cervical wall, and possible extension to the cul-de-sac. Two cystic cavities were visible in the left ovary, with chocolate-like liquids and soft consistency. The right ovary was cystic-solid and densely adhered to the fallopian tube. Postoperative pathology results were as follows: cervical adenocarcinoma, moderately to poorly differentiated, consistent with gastric-type adenocarcinoma (non-HPV-related) according to the IHC. The tumor infiltrated the full layer of the cervical canal wall, reaching the proximal parametrium, involving the lower segment of the uterine body, vaginal wall (from the cul-de-sac to more than 1/3 of the upper vagina), and the stroma of the right fallopian tube, with positive LVSI and neural invasion. No cancer was found at the distal parametrium and vaginal margins. Both sides of ovaries showed endometriotic cysts. Lymph node metastasis was observed (total 8/32), with partial extracapsular spread. Among which, the para-aortic lymph nodes were negative (0/9), left pelvic lymph nodes were positive (5/11), and right ones were positive (3/12). Major IHC results were as follow: ER (-), PR (-), Ki-67 (40%+), NapsinA (-), P16 (-), P53 (-, mutant expression), PAX8 (-), Vimentin (-), MUC5AC (2+), MUC6 (focal+), CDX-2 (3+), CD10 (2+), HNF1 (1+), PAX2 (-). The postoperative diagnosis was GAC, FIGO stage IIIC1, with bilateral ovary endometriosis cysts.
2.3. Follow up of the patient
One month after the surgery, the patient began adjuvant treatment. Now she is currently undergoing concurrent chemo-radiotherapy. The clinical features of the patient at both baseline and post-operative are summarized in
Table 1.
3. Discussion
3.1. The characteristics of this case and GAS
Due to the unrelated to HPV infection, the lesion is covert and difficult to sample, resulting in a low positivity rate for screening and biopsy at the initial visit, making a challenge to preoperative diagnosis [
2]. This reminds us that we should still be pay attention to patients with "double-negative" results of cytology and HPV tests and based on clinical history and clinical presentations to increase our awareness to this disease. In this case, abnormal findings were detected in cytology test, and the biopsy results suggested moderately differentiated adenocarcinoma. Although HPV 66 infection was present, it was still considered as non-HPV-related GAS based on the postoperative pathology. Despite the relatively clear preoperative diagnosis, it was still not possible to definitively determine whether it was primary endometrial adenocarcinoma involving the cervix or primary cervical adenocarcinoma.
The clinical presentation of GAS is atypical and diverse. Vaginal mucous or watery discharge is a common symptom [
3]. Upon further inquiry into the patient's medical history, she reported a transient vaginal discharge, which was not of concern due to its short duration. This indicates that for the complaint of "vaginal discharge," differential diagnosis should include common inflammatory diseases, tubal tumors, and GAS. Additionally, the occurrence of ovarian metastasis may present as the initial symptom of "pelvic mass" [
4]. However, in this case, although the chief complaint was also "pelvic mass," the postoperative pathology confirmed ovarian endometriosis cysts rather than metastasis.
In terms of auxiliary examinations, GAS may present with elevated tumor markers, with over 1/2 showing elevated CA19-9 and about 1/3 having elevated serum CA125, with the latter suggesting the presence of pelvic and abdominal cavity metastases [
5]. In this case, CA19-9 was significantly elevated, and although CA125 was abnormal, it does not exclude the possibility of concomitant ovarian endometriosis. In terms of imaging examinations, pelvic MRI has a certain diagnostic specificity. The lesion of GAS is usually located in the middle and upper segments of the cervical canal, showing a specific "cosmic sign" [
6]. The MRI results of our case were consistent with these image characteristics.
In terms of pathology, the cut surfaces of GAS gross specimens may present yellow or gray-white, with typical honeycomb-like changes, densely filled with mucous-containing cysts of varying sizes, with diameters of 0.5 – 1.0 cm. The morphologic criteria for distinguishing GAS were defined as a tumor showing clear and/or pale eosinophilic and voluminous cytoplasm, with distinct cell borders [
7] (
Figure 2). IHC markers HIK1083 and MUC6 may help to confirm the gastric-type differentiation [
8]. However, in most parts of the world, HIK1083 is not commercially available for use [
9]. P16, ER, and PR are mostly negative, with only a few cases showing positivity [
10]. Additionally, CDX2 and PAX8 are partially positive [
11], and in some cases, P53 shows mutant expression [
12]. The IHC results of our case were generally consistent with the aforementioned pathological features.
In terms of treatment, due to low incidence rate and lacking large-scale clinical research data, its treatment should be individualized based on the reference of squamous cell carcinoma and common type cervical adenocarcinoma. In this case, surgical treatment was chosen, including radical hysterectomy with bilateral adnexectomy, pelvic and para-aortic lymph node dissection, and comprehensive exploration of the pelvic and abdominal cavities. According to the postoperative pathology, there were some high-risk factors such as parametrial involvement and lymph nodes metastasis, the recommended follow-up treatment includes adjuvant radiotherapy and chemotherapy. According to “The Chinese Expert Consensus on the Clinical Diagnosis and Treatment of Gastric-type Endocervical Adenocarcinoma (2021 Edition)” [
13], the chemotherapy regimen refers to the chemotherapy regimen for ovarian cancer (paclitaxel combined with carboplatin). It has been reported that human epidermal growth factor receptor-2 (HER-2) amplification is more common in GAS, suggesting that HER-2 may be one of the potential therapeutic targets [
14]. Furthermore, it was reported that through next-generation sequencing technology 161 different cancer driver genes in GAS tissue were detected, with the most common mutated gene being TP53 [
15,
16]. In the future, the exploration of more molecular targets is expected, aiming for targeted therapy and encouraging participation in clinical trials, with the goal of standardizing treatment strategies based on individualized diagnosis and treatment and improving patient prognosis.
3.2. The Relationship between Endometriosis cysts and Cervical Cancer
Endometriosis refers to the presence of endometrial tissue outside the uterine cavity, mainly involving the ovaries, fallopian tubes, and pelvic peritoneum. Endometriosis causes clinical symptoms such as pain, infertility, and the formation of nodules or masses through infiltrative growth and recurrent bleeding [
14]. Endometriosis is a common benign gynecological disease, but with ongoing research, it has been found to have certain associations with various malignant tumors, especially epithelial ovarian cancer [
18]. However, current research has not found a definitive correlation between endometriosis and cervical cancer or cervical adenocarcinoma [
19]. Therefore, although the primary symptom of our case was "pelvic mass," and the preoperative imaging evaluation considered metastatic tumors, the postoperative pathology confirmed as ovarian endometriosis at last. Hence, as far as we know, it is considered that GAS and ovary endometriosis cysts were both the primary disease of our case.
4. Conclusions
GAS has a low incidence rate, HPV screening are commonly negative, clinical presentations are atypical, hence it is easy to be missed. However, with the assistance of tumor markers CA125, CA19-9, and MRI may help to diagnosis. IHC is an important means of differential diagnosis, and pathology remains the gold standard for diagnosis. Its malignant biological behavior, high invasiveness and metastasis, and poor prognosis should be highly valued by clinical physicians. Detailed inquiry, necessary auxiliary examinations, increased diagnostic rates, and the development of rational treatment plans are of great significance in improving patient prognosis.
Currently, it is urgent to explore diagnostic molecular targets with high specificity for GAS. In the future, more targeted treatments based on molecular pathological features need to be explored, aiming to achieve early diagnosis and precise treatment of GAS.
Author Contributions
Conceptualization, Xiaodan Sun; methodology, Xuying Liu.; writing—original draft preparation, Si Gao. ; funding acquisition, Xiaodan Sun. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Jilin Province Health Technology Capability Enhancement Project (grant No. 2022JC007) and Project of Lung cancer targeted therapy research of Beijing CSCO (grant No. Y-2021AST/qn-0013).
Institutional Review Board Statement
The retrospective review of patient data did not require ethical approval in accordance with local/national guidelines.
Informed Consent Statement
Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Han, B.; Zheng, R.; Zeng, H.; et al. Cancer incidence and mortality in China,2022. Journal of the National Cancer Center. 2024. [CrossRef]
- Seki, T.; Kojima, A.; Okame, S.; et al. Poor Treatment Outcomes of Locally Advanced Cervical Adenocarcinoma of Human Papilloma Virus Independent Type, Represented by Gastric Type Adenocarcinoma: A Multi-Center Retrospective Study (Sankai Gynecology Study Group). Cancers (Basel). 2023, 15, 1730. [Google Scholar] [CrossRef] [PubMed]
- Kerwin, C.M.; Markese, M.; Moroney, M.R.; et al. Adenocarcinoma of the uterine cervix, gastric-type (GAS): a review of the literature focused on pathology and multimodality imaging. Abdom Radiol (NY). 2023, 48, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Lee, E. Huge Ovarian Tumor: An Unusual Presentation of Gastric-Type Endocervical Adenocarcinoma. Case Rep Oncol. 2022, 15, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, A.; Yamaguchi, K.; Minamiguchi, S.; et al. Mucinous adenocarcinoma, gastric type of the uterine cervix:clinical features and HER2 amplification[J]. Med Mol Morphol 2019, 52, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Ohya, A.; Kobara, H.; Miyamoto, T.; et al. Usefulness of the 'cosmos pattern' for differentiating between cervical gastric-type mucin-positive lesions and other benign cervical cystic lesions in magnetic resonance images[J]. J Obstet Gynaecol Res, 2021, 47, 745–756. [Google Scholar] [CrossRef] [PubMed]
- Kojima, A.; Mikami, Y.; Sudo, T.; et al. Gastric morphology and immunophenotype predict poor outcome in mucinous adenocarcinoma of the uterine cervix. Am J Surg Pathol. 2007, 31, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Fulgione, C.; Raffone, A.; Travaglino, A.; et al. Diagnostic accuracy of HIK1083 and MUC6 as immunohistochemical markers of endocervical gastric-type adenocarcinoma: A systematic review and meta-analysis. Pathol Res Pract. 2023, 241, 154261. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, A.; Sekine, S.; Ogawa, R.; et al. Lobular endocervical glandular hyperplasia is a neoplastic entity with frequent activating GNAS mutations. Am J Surg Pathol. 2014, 38, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Talia, K.L.; Mccluggage, W.G. The developing spectrum of gastric-type cervical glandular lesions[J]. Pathology 2018, 50, 122–133. [Google Scholar] [CrossRef] [PubMed]
- Carleton, C.; Hoang, L.; Sah, S. , et al. A detailed immunohistochemical analysis of a large series of cervical and vaginal gastric-type adenocarcinomas[J]. The American Journal of Surgical Pathology, 2016, 40, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Turashvili, G.; Morency, E.G.; Kracun, M.; et al. Morphologic features of gastric-type cervical adenocarcinoma in small surgical and cytology specimens[J]. Int J Gynecol Pathol, 2019, 38, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Gynecological oncology professional committee (Study Group) of gynecologist and obstetrician branch of Chinese Medical Association. The Chinese expert consensus on the clinical diagnosis and treatment of cervical and gastric adenocarcinoma (2021 edition). Chin J Pract Gynecol Obstet. 2021, 37, 1133–8.
- Shi, H.; Shao, Y.; Lu, W.; et al. An analysis of HER2 amplification in cervical adenocarcinoma: correlation with clinical outcomes and the international endocervical adenocarcinoma criteria and classification. J Pathol Clin Res 2021, 7, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Nagaria, T.S.; Clarke, B.; et al. Molecular characterization of gastric-type endocervical adenocarcinoma using next-generation sequencing. Mod Pathol. 2019, 32, 1823–1833. [Google Scholar] [CrossRef] [PubMed]
- Park, E.; Kim, S.W.; Kim, S.; et al. Genetic characteristics of gastric-type mucinous carcinoma of the uterine cervix. Mod Pathol. 2021, 34, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Allaire, C.; Bedaiwy, M.A.; Yong, P.J. Diagnosis and management of endometriosis. CMAJ. 2023, 195, E363–E371. [Google Scholar] [CrossRef] [PubMed]
- Guidozzi, F. Endometriosis-associated cancer. Climacteric. 2021, 24, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Liu, R.; Tang, S.; et al. Impact of endometriosis on risk of ovarian, endometrial and cervical cancers: a meta-analysis. Arch Gynecol Obstet. 2019, 299, 35–46. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).