1. Introduction
Velamentous cord insertion (VCI) is defined as abnormal insertion of the umbilical vessels into the fetal membranes without Wharton’s jelly before entering the placenta. The membranous vessels are at risk for rupture, kinking, and compression, which increases the risk for adverse pregnancy outcomes [
1,
2]. The reported incidence of VCI is approximately 0.1–1.8% in all pregnancies [
3], and as high as 40% in twin pregnancies [
3,
4,
5,
6]. In a study examining 1,498 twin placentas after delivery, the prevalence of VCI in dichorionic (DC) and monochorionic diamniotic (MCDA) twin pregnancies without and with twin-to-twin transfusion syndrome (TTTS) was 7.6, 34.7, and 36.1, respectively [
7]. A recent study reported a VCI prevalence in DC and MCDA twins of 5.8% and 7.8%, respectively [
8].
VCI contributes to adverse maternal and perinatal outcomes [
1,
2,
3,
4]. However, findings are controversial regarding its effect on perinatal outcomes in twin pregnancies. Costa-Castro et al. found that VCI increased the risk for adverse outcomes (such as severe birthweight discordance and/or small for gestational age) in MCDA twins, but not in DC twins [
7]. Furthermore, VCI was reported to be a risk factor for selective fetal growth restriction (sFGR), TTTS, and birthweight discordance in MCDA twins [
4,
9,
10]. In contrast, other studies concluded that the adverse complications in pregnancies with VCI were probably due to selection bias, noting that these specific adverse outcomes in MCDA twins were more likely the result of vascular complications due to the placental sharing rather than VCI [
8,
11]. Recently, we reported that VCI and marginal cord insertion in the second twin were significant risk factors for umbilical cord prolapse during vaginal delivery [
12].
This study aimed to examine VCI prevalence and related risk factors in twin pregnancies and to evaluate its effect on perinatal outcomes according to chorionicity. We hypothesized that VCI would be a significant risk factor for perinatal complications such as FGR and TTTS in MCDA twins, but not in DC twins.
2. Materials and Methods
2.1. Study design and population
This was a single-center retrospective study that included women with twin pregnancies who delivered at our institution between January 2012 and December 2021. The exclusion criteria were as follows: 1) monochorionic monoamniotic twin pregnancies; 2) twin pregnancies with unknown chorionicity; and 3) missing information regarding the umbilical cord insertion site.
This study conformed with the principles outlined in the Declaration of Helsinki of 1964. The study was approved by the Ethics Committee of the Japanese Red Cross Aichi Medical Center Nagoya Daiichi Hospital, Nagoya, Japan (approval number: 2023-162). Informed consent was not required for this study since we used existing anonymous clinical data.
2.2. Pregnancy management
After confirming twin pregnancy, chorionicity and amnionicity were determined by ultrasound in the first trimester. In brief, the presence of the “twin peak” or “lambda” sign at the inter-twin membrane indicated DC twins, while the presence of the “T” sign indicated MCDA twins. Pregnancy check-ups were performed every 2 weeks after gestational week 16 for MC twins and after gestational week 22 for DC twins. At each check-up, we assessed the fetal position, amniotic fluid volume, and fetal growth. Additionally, umbilical artery Doppler was performed for all MCDA twins and for DC twins with FGR and/or oligohydramnios. After delivery, the length, insertion site, number of vessels, and gross abnormalities (e.g., knots) of the umbilical cord were confirmed by gross examination.
2.3. Data collection and definitions
Data on maternal and fetal characteristics were extracted from the medical records. The method of conception was categorized as spontaneous, induction, or assisted reproductive technology (ART). Preeclampsia was defined as the presence of gestational hypertension (blood pressure >140/90 mmHg after 20 weeks of gestation), proteinuria (>300 mg per day), and/or findings of end-organ dysfunction during pregnancy [
13]. FGR was defined as a fetal body weight of less than -1.5 SD for the gestational age [
14]. TTTS was defined as discordant amniotic fluid volumes (maximal vertical pocket less than 2 cm and more than 8 cm in each amniotic sac at the same time) in MCDA twins [
15].
2.4. Statistical analyses
Extracted data were entered into a computerized spreadsheet (Excel, Microsoft Japan Co., Ltd., Tokyo, Japan). EZR software (version 1.38, Saitama, Japan) was used for all data analyses. For data analysis, patients were divided into two groups: DC and MCDA. After assessing data normality using the Shapiro-Wilk test, Mann-Whitney’s U test or Student’s t-test was used to compare continuous variables between the two groups, as appropriate. Continuous variables included maternal age, gestational age at delivery, body mass index (BMI), and birthweight. The chi-square test was performed to compare the following categorical variables: chorionicity, nulliparity, ART, male infant, preterm birth, diabetes mellitus, preeclampsia, FGR, and VCI. Logistic regression models were employed to identify risk factors for VCI (maternal age, BMI, nulliparity, ART, and monochorionic twin) and the prognostic value of VCI for perinatal outcomes (maternal age, BMI, nulliparity, ART, diabetes mellitus, preeclampsia, and FGR). For each variable, the adjusted odds ratio (aOR) and 95% confidence interval (CI) were estimated. P values less than 0.05 were considered to indicate statistical significance.
2.5. Patient and public involvement
Neither patients nor the public were involved in the design, conduct, reporting, or dissemination of this research.
3. Results
3.1. Participant selection process
Among the 716 women with twin pregnancies identified, 22 were excluded from the study (one with monochorionic monoamniotic twin pregnancy, four with unknown chorionicity, and 17 with missing information on the umbilical cord insertion site). Finally, 694 women with twin pregnancies (including 451 DC and 243 MCDA pregnancies) were included (
Figure S1).
3.2. Maternal characteristics and delivery outcomes
The maternal and fetal characteristics are shown in
Table 1. Pre-pregnancy maternal BMI and ART rate were significantly higher in DC than in MCDA twin pregnancies. Gestational age at delivery and neonatal body weight were significantly higher in DC than in MCDA twins. However, the rates of preterm birth at < 36 weeks and FGR were higher in MCDA than in DC twins. Additionally, the VCI rate was significantly higher in MCDA than in DC twins (9.7% vs. 4.4%,
P<0.001).
3.3. Maternal characteristics in VCI cases
In DC twins, the rate of ART pregnancies was significantly lower among VCI than among non-VCI cases and VCI was a significant risk factor for preterm birth at <36 weeks (
Table S1). In MCDA twins, VCI was a significant risk factor for preterm birth at <36 weeks and TTTS (
Table S2). No differences were observed in the incidence of VCI by mode of conception. As for FGR, VCI was a significant risk factor for FGR in MCDA twins, but not in DC twins.
3.4. Risk factors for VCI
In the multivariate analyses for risk factors for VCI, maternal BMI and MCDA pregnancy were significant risk factors for VCI (aOR, 1.09; 95% CI: 1.02–1.16;
P=0.009 and aOR, 2.34; 95% CI: 1.42–3.84;
P <0.001, respectively), while ART pregnancy was a significant protective factor against VCI (aOR, 0.452; 95% CI: 0.214–0.954;
P=0.037) (
Table 2).
3.5. VCI and perinatal outcomes
The multivariate analysis results for the prognostic role of VCI for perinatal outcomes are shown in
Table 3. In DC twins, no significant association was observed between VCI and perinatal outcomes (FGR and preterm birth at <36 weeks). In contrast, in MCDA twins, VCI was a significant risk factor for the following adverse perinatal outcomes: FGR (aOR, 3.01; 95% CI: 1.36–6.67;
P=0.007), TTTS (aOR, 5.22; 95% CI: 2.04–13.4;
P <0.001), and preterm birth at <36 weeks (aOR, 3.25; 95% CI: 1.54–6.85;
P=0.002).
4. Discussion
4.1. Main findings
In the present study, the VCI rate was 9.7% in MCDA twins and 4.4% in DC twins, being significantly higher in MCDA twins. Maternal BMI and MCDA pregnancy were identified as significant risk factors for VCI, while ART pregnancy was a significant protective factor. VCI was not associated with perinatal outcomes in DC twins, whereas in MCDA twins, it was associated with FGR, TTTS, and preterm birth at <36 weeks.
4.2. Interpretation
The reported prevalence of VCI in twin pregnancies ranges from 1.6% to 40% [
3,
4,
5,
6]. The VCI rates in the current study were similar to those of 5.8% in DC twins and 7.8% in MCDA twins reported by Lee et al [
8]. Furthermore, the VCI rate was significantly higher in MCDA than in DC twins, which aligns with the findings of Costa-Castro et al [
7]. Contrarily, other studies have reported similar VCI rates in DC and MCDA twins [
8,
16]. Nonetheless, the VCI rate is considered to be higher in twin pregnancies than in singleton pregnancies.
Regarding the impact of VCI on perinatal outcomes in twin pregnancies, reported findings are contradicting. Some studies have found that VCI is a risk factor for adverse perinatal outcomes in MCDA twins [
4,
7,
9,
10,
17], and that perinatal mortality is notably higher in VCI than in non-VCI MCDA twins (30% vs. 10.5%) [
18]. In contrast, in other studies, VCI in twin pregnancies was not associated with adverse perinatal outcomes neither in MCDA nor in DC twins [
8]. In the current study, we observed no significant association between VCI and perinatal outcomes in DC twins; however, VCI was associated with FGR, TTTS, and preterm birth at <36 weeks in MCDA twins. These findings suggest that we need to be vigilant about VCI in MCDA twins, which necessitates specialized management, including frequent check-ups of cervical length, fetal growth, amniotic fluid volume, and fetal blood flow measurements in such cases.
In our study, the rate of ART pregnancies was significantly lower among VCI than among non-VCI cases in DC twins. In addition, MCDA pregnancy was a significant risk factor for VCI (aOR, 1.09), whereas ART pregnancy was a significant protective factor against VCI (aOR, 0.452). In previous studies, VCI was reported to have a varying degree of association with in vitro fertilization (IVF) compared with natural pregnancy [
3,
4,
16,
19]. Furthermore, in a systematic review, ART pregnancy was associated with a higher rate of VCI compared with natural pregnancy, and the VCI rate was similar among the different ART methods (blastocyst vs. cleavage-stage transfer and frozen vs. fresh embryo transfer) [
20]. However, these studies included singleton pregnancies only [
3,
19], or both singleton and multiple pregnancies [
4,
20], and none included only multiple pregnancies. Delbaere et al. reported an increasing incidence of VCI according to the invasiveness of the reproductive technique in dizygotic twins: 3.6% in natural conception, 5% in artificial induction of ovulation, 7.4% in IVF, and 10.4% in intracytoplasmic sperm injection [
21]. Although our results differ from those of previous studies, few studies of ART pregnancies and VCI risk have been conducted among twin pregnancies only.
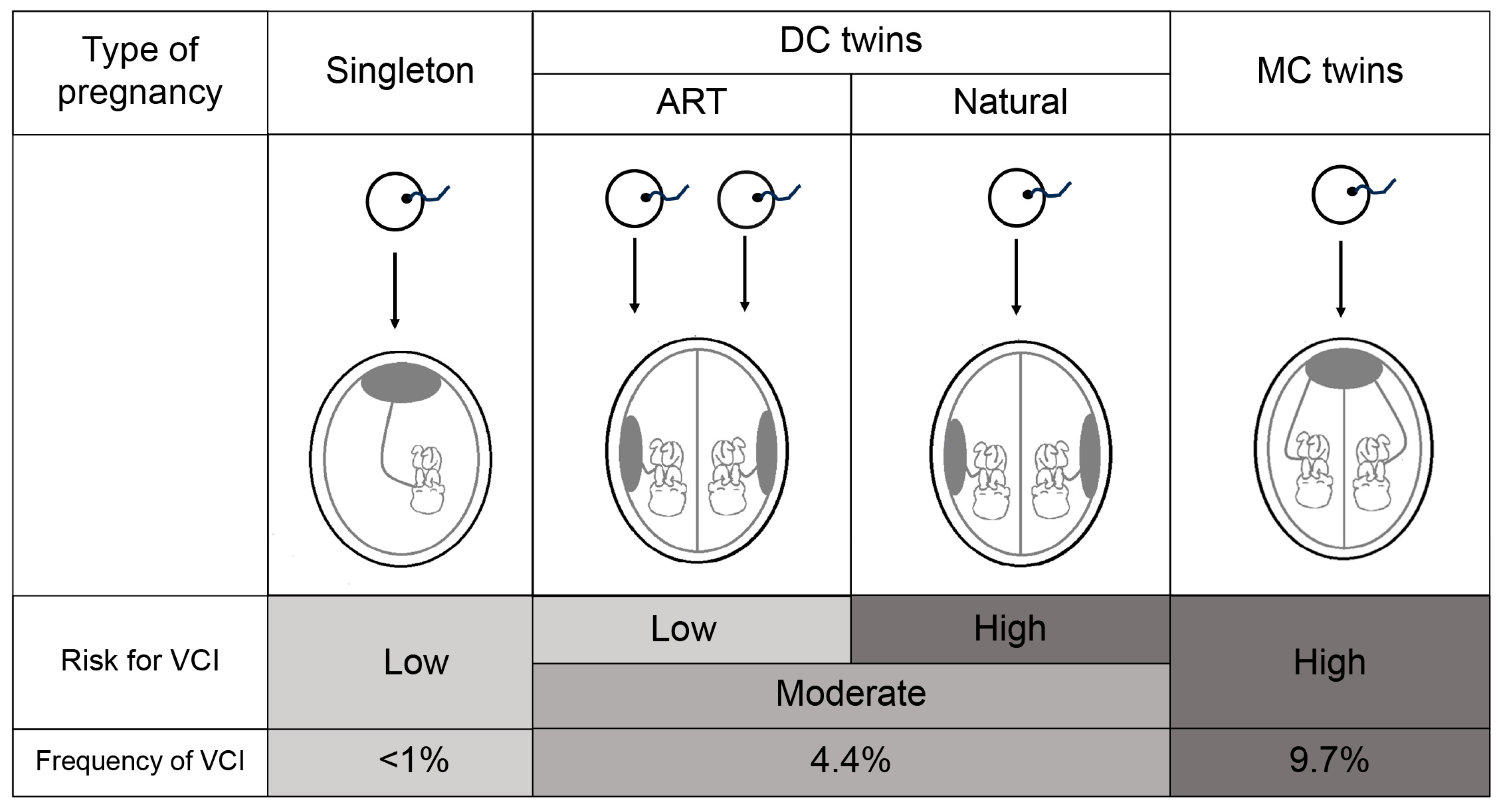
With regard to our finding that ART pregnancies reduced the risk for VCI, we speculate the reason to be as follows. The fact that singleton pregnancies have the lowest and MCDA pregnancies have the highest risk for VCI suggests that the reason may be the splitting of monozygotic twins after fertilization. In DC twins, most ART pregnancies involve dizygotic and no splitting process, and therefore follow a similar process to that in singleton pregnancies. Contrarily, naturally conceived DC twins have a higher risk for VCI than those conceived by ART because most of them undergo the same process of splitting after fertilization, similar to MCDA twins (
Figure 1). If ART pregnancy reduces the risk for VCI, particularly considering that ART pregnancies are more common in DC twins [
22], it would be positive information for the patient. However, further study is needed to confirm this.
In the present study, data on the umbilical cord insertion site was obtained by gross examination after delivery. As the study was retrospective, data on prenatal umbilical cord insertion site obtained by ultrasound examination were not complete. The overall accuracy of screening for VCI using transabdominal sonography (TAS) is considerably high [
16]. The second-trimester TAS has been reported to have consistently high specificity (>99.8%) [
23,
24,
25]. In the largest and highest-quality study, sensitivity was reported to be 62.5%, specificity 100%, positive predictive value 83%, negative predictive value 100%, and accuracy 99.8% [
25]. Although these data are from singleton pregnancies, we believe that the same high accuracy can be achieved in twin pregnancies. A well-designed prospective study with a larger cohort of women could examine this issue further. Accurate diagnosis of the umbilical cord insertion site by second-trimester TAS in twin pregnancies will require more careful observation for preterm birth, FGR, and TTTS, particularly in MCDA twins, leading to better pregnancy management.
4.3. Strengths and limitations
The main strength of this study is that it was conducted at a single center and included a relatively large sample size (694 twin cases). Due to the single-center design, pregnancy management and treatment policies were homogeneous and a certain quality of practice was maintained. Moreover, the institution complies with the Guideline for Obstetrical Practice in Japan and provides a standard of care. Another strength is the accuracy of the diagnosis of VCI, as it was made by macroscopic examination of the placenta after delivery.
The main limitation of this study is its retrospective nature, which limits the reliability of the results due to selection biases. Furthermore, VCI is associated with an increased risk for hemorrhage in the third stage of labor and need for manual removal of the placenta [
26]. In addition, VCI can sometimes coincide with vasa previa [
16,
27]. However, we did not have data regarding these adverse outcomes. Finally, the mechanism underlying the low rate of VCI in ART pregnancies remains unclear and should be examined by future studies.
In the future, it is important to confirm that antenatal TAS can diagnose VCI with a high degree of accuracy, and if so, from a clinical perspective, cases with antenatal diagnosis of VCI should be managed carefully to ensure better pregnancy outcomes for the mother and child.
5. Conclusions
The VCI rate in our study was significantly higher in MCDA than in DC twins. MCDA pregnancy was a significant risk factor for VCI, while ART pregnancy was a significant protective factor. VCI was a significant risk factor for adverse perinatal outcomes in MCDA twins, but not in DC twins. A notable finding is that ART pregnancies reduced the risk for VCI, which has rarely been reported. Further research is warranted to clarify the underlying mechanisms. We believe that the findings of this study will provide valuable and novel information for the future management of twin pregnancies.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org. Table S1: Maternal characteristics in dichorionic twins by cord insertion type. Table S2: Maternal characteristics in monochorionic twins by cord insertion type. Figure S1: Study flowchart
Author Contributions
Conceptualization, A.S. and H.T.; Design, A.S. and H.T.; Data collection and management, A.S., H.T., E.T., Y.N., M.K., H.A., Y.M., M.S., N.F., Y.I., A.T., T.A., and K.M.; Data analysis, A.S. and H.T.; Drafted the manuscript, H.T. All authors have read and approved the final version of the manuscript.
Funding
This research was funded by the [Japanese Red Cross, Nagoya Daiichi Hospital Research Grant] grant number [NFRCH23-0022].
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Japanese Red Cross Nagoya Daiichi Hospital, Nagoya, Japan (approval number: 2023-162 and approval date: November 14, 2023).
Informed Consent Statement
Patient informed consent was waived because this study used existing anonymous clinical data.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request (email:
hirotty7099@yahoo.co.jp).
Acknowledgments
We thank Editage (
https://www.editage.com/) for English language editing. We would also like to thank Atsushi Kubo for his help with data collection from the medical records.
Conflicts of Interest
The authors declare no conflicts of interest. The funder had no role in in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Ismail, K.I.; Hannigan, A.; O’Donoghue, K.; Cotter, A. Abnormal placental cord insertion and adverse pregnancy outcomes: a systematic review and meta-analysis. Syst Rev 2017, 6, 242. [CrossRef]
- Siargkas, A.; Tsakiridis, I.; Pachi, C.; Mamopoulos, A.; Athanasiadis, A.; Dagklis, T. Impact of velamentous cord insertion on perinatal outcomes: a systematic review and meta-analysis. Am J Obstet Gynecol MFM 2023, 5, 100812. [CrossRef]
- Räisänen, S.; Georgiadis, L.; Harju, M.; Keski-Nisula, L.; Heinonen, S. Risk factors and adverse pregnancy outcomes among births affected by velamentous umbilical cord insertion: a retrospective population-based register study. Eur J Obstet Gynecol Reprod Biol 2012, 165, 231–234. [CrossRef]
- Ebbing, C.; Kiserud, T.; Johnsen, S.L.; Albrechtsen, S.; Rasmussen, S. Prevalence, risk factors and outcomes of velamentous and marginal cord insertions: a population-based study of 634,741 pregnancies. PLOS ONE 2013, 8, e70380. [CrossRef]
- Suzuki, S.; Kato, M. Clinical significance of pregnancies complicated by velamentous umbilical cord insertion associated with other umbilical cord/placental abnormalities. J Clin Med Res 2015, 7, 853–856. [CrossRef]
- Yerlikaya, G.; Pils, S.; Springer, S.; Chalubinski, K.; Ott, J. Velamentous cord insertion as a risk factor for obstetric outcome: a retrospective case-control study. Arch Gynecol Obstet 2016, 293, 975–981. [CrossRef]
- Costa-Castro, T.; Zhao, D.P.; Lipa, M.; Haak, M.C.; Oepkes, D.; Severo, M.; Montenegro, N.; Matias, A.; Lopriore, E. Velamentous cord insertion in dichorionic and monochorionic twin pregnancies - Does it make a difference? Placenta 2016, 42, 87–92. [CrossRef]
- Lee, H.M.; Lee, S.; Park, M.K.; Han, Y.J.; Kim, M.Y.; Boo, H.Y.; Chung, J.H. Clinical significance of velamentous cord insertion prenatally diagnosed in twin pregnancy. J Clin Med 2021, 10, 572. [CrossRef]
- Kent, E.M.; Breathnach, F.M.; Gillan, J.E.; McAuliffe, F.M.; Geary, M.P.; Daly, S.; Higgins, J.R.; Dornan, J.; Morrison, J.J.; Burke, G.; et al. Placental cord insertion and birthweight discordance in twin pregnancies: results of the national prospective ESPRiT study. Am J Obstet Gynecol 2011, 205, 376.e1–7. [CrossRef]
- Yonetani, N.; Ishii, K.; Kawamura, H.; Mabuchi, A.; Hayashi, S.; Mitsuda, N. Significance of velamentous cord insertion for twin-twin transfusion syndrome. Fetal Diagn Ther 2015, 38, 276–281. [CrossRef]
- Ebbing, C.; Johnsen, S.L.; Albrechtsen, S.; Sunde, I.D.; Vekseth, C.; Rasmussen, S. Velamentous or marginal cord insertion and the risk of spontaneous preterm birth, prelabor rupture of the membranes, and anomalous cord length, a population-based study. Acta Obstet Gynecol Scand 2017, 96, 78–85. [CrossRef]
- Asahina, R.; Tsuda, H.; Nishiko, Y.; Fuma, K.; Kuribayashi, M.; Tezuka, A.; Ando, T.; Mizuno, K. Evaluation of the risk of umbilical cord prolapse in the second twin during vaginal delivery: a retrospective cohort study. BMJ Open 2021, 11, e046616. [CrossRef]
- Watanabe, K.; Matsubara, K.; Nakamoto, O.; Ushijima, J.; Ohkuchi, A.; Koide, K.; Makino, S.; Mimura, K.; Morikawa, M.; Naruse, K.; et al. Outline of the new definition and classification of “Hypertensive Disorders of Pregnancy (HDP)”; a revised JSSHP statement of 2005. Hypertens Res Pregnancy 2018, 6, 33–37. [CrossRef]
- Yoshida, S.; Unno, N.; Kagawa, H.; Shinozuka, N.; Kozuma, S.; Taketani, Y. Prenatal detection of a high-risk group for intrauterine growth restriction based on sonographic fetal biometry. Intl J Gynecology & Obste 2000, 68, 225–232. [CrossRef]
- Quintero, R.A.; Morales, W.J.; Allen, M.H.; Bornick, P.W.; Johnson, P.K.; Kruger, M. Staging of twin-twin transfusion syndrome. J Perinatol 1999, 19, 550–555. [CrossRef]
- Buchanan-Hughes, A.; Bobrowska, A.; Visintin, C.; Attilakos, G.; Marshall, J. Velamentous cord insertion: results from a rapid review of incidence, risk factors, adverse outcomes and screening. Syst Rev 2020, 9, 147. [CrossRef]
- Lopriore, E.; Sueters, M.; Middeldorp, J.M.; Oepkes, D.; Walther, F.J.; Vandenbussche, F.P. Velamentous cord insertion and unequal placental territories in monochorionic twins with and without twin-to-twin-transfusion syndrome. Am J Obstet Gynecol 2007, 196, 159.e1–5. [CrossRef]
- Hack, K.E.A.; Nikkels, P.G.J.; Koopman-Esseboom, C.; Derks, J.B.; Elias, S.G.; van Gemert, M.J.; Visser, G.H. Placental characteristics of monochorionic diamniotic twin pregnancies in relation to perinatal outcome. Placenta 2008, 29, 976–981. [CrossRef]
- Yanaihara, A.; Hatakeyama, S.; Ohgi, S.; Motomura, K.; Taniguchi, R.; Hirano, A.; Takenaka, S.; Yanaihara, T. Difference in the size of the placenta and umbilical cord between women with natural pregnancy and those with IVF pregnancy. J Assist Reprod Genet 2018, 35, 431–434. [CrossRef]
- Matsuzaki, S.; Ueda, Y.; Matsuzaki, S.; Nagase, Y.; Kakuda, M.; Lee, M.; Maeda, M.; Kurahashi, H.; Hayashida, H.; Hisa, T.; Mabuchi, S.; Kamiura, S. Assisted reproductive technique and abnormal cord insertion: a systematic review and meta-analysis Biomedicines 2022, 10, 1722. [CrossRef]
- Delbaere, I.; Goetgeluk, S.; Derom, C.; De Bacquer, D.; De Sutter, P.; Temmerman, M. Umbilical cord anomalies are more frequent in twins after assisted reproduction. Hum Reprod 2007, 22, 2763–2767. [CrossRef]
- Tsuda, H.; Kotani, T.; Nakano, T.; Imai, K.; Ushida, T.; Hirakawa, A.; Kinoshita, F.; Takahashi, Y.; Iwagaki, S.; Kikkawa, F. The impact of fertility treatment on the neonatal respiratory outcomes and amniotic lamellar body counts in twin pregnancies. Clin Chim Acta 2018, 484, 192–196. [CrossRef]
- Sepulveda, W. Velamentous insertion of the umbilical cord: a first-trimester sonographic screening study. J Ultrasound Med 2006, 25, 963–8; quiz 970. [CrossRef]
- Sepulveda, W.; Rojas, I.; Robert, J.A.; Schnapp, C.; Alcalde, J.L. Prenatal detection of velamentous insertion of the umbilical cord: a prospective color Doppler ultrasound study. Ultrasound Obstet Gynecol 2003, 21, 564–569. [CrossRef]
- Hasegawa, J.; Matsuoka, R.; Ichizuka, K.; Sekizawa, A.; Farina, A.; Okai, T. Velamentous cord insertion into the lower third of the uterus is associated with intrapartum fetal heart rate abnormalities. Ultrasound Obstet Gynecol 2006, 27, 425–429. [CrossRef]
- Ebbing, C.; Kiserud, T.; Johnsen, S.L.; Albrechtsen, S.; Rasmussen, S. Third stage of labor risks in velamentous and marginal cord insertion: a population-based study. Acta Obstet Gynecol Scand 2015, 94, 878–883. [CrossRef]
- Zhang, W.; Geris, S.; Beta, J.; Ramadan, G.; Nicolaides, K.H.; Akolekar, R. Prevention of stillbirth: impact of two-stage screening for vasa previa. Ultrasound Obstet Gynecol 2020, 55, 605–612. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).