Submitted:
07 February 2024
Posted:
08 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
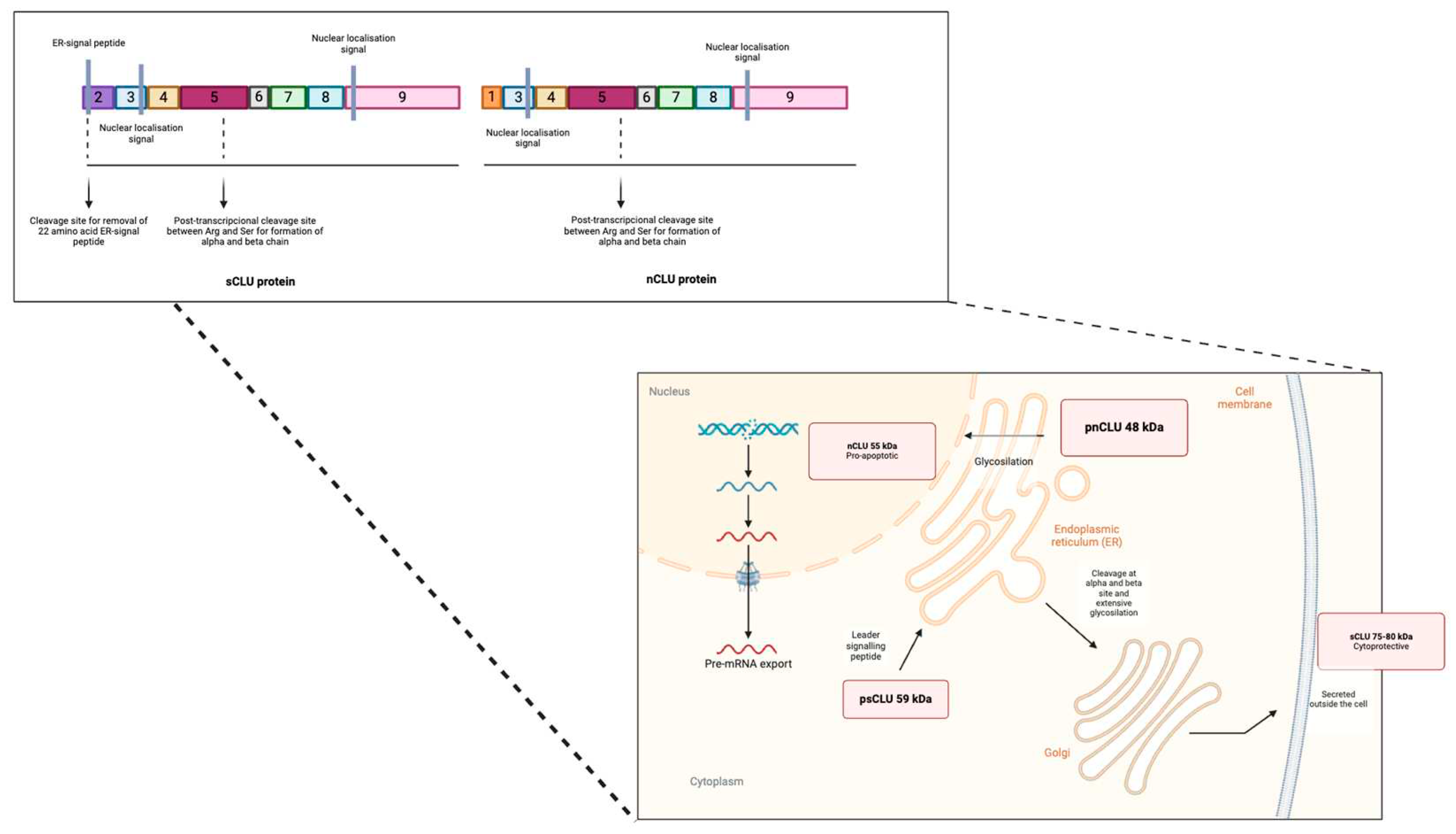
2. Isoforms and Regulation of CLU Expression Gene
3. Clusterin and Its Involvement in Cancer
3.1. Tumorigenesis
3.2. Cell Proliferation
3.3. Epithelial-Mesenchymal Transition and Metastasis
3.4. Chemoresistance and Chemosensitivity with Clusterin
4. Clusterin as a Biomarker and Therapeutic Target in Cancer
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hogg, S.D., Embery, G. The isolation and partial characterization of a sulphated glycoprotein from human whole saliva which aggregates strains of Streptococcus sanguis but not Streptococcus mutans. Arch. Oral Biol. 1979, 24, 791–797. [CrossRef]
- Jones, S.E., & C. Jomary. Clusterin. Int J Biochem Cell Biol. 2002, 34(5), 427-31.
- Trougakos, I.P., & E.S. Gonos. Regulation of clusterin/apolipoprotein J, a functional homologue to the small heat shock proteins, by oxidative stress in ageing and age-related diseases. Free Radic Res. 2006, 40(12), 1324-34. [CrossRef]
- Itahana, Y., Piens, M., Sumida, T., Fong, S., Muschler, J., & Desprez, P. Y. Regulation of clusterin expression in mammary epithelial cells. Exp Cell Res. 2007, 313(5), 943-51. [CrossRef]
- Trougakos, I.P. & E.S. Gonos. Clusterin/apolipoprotein J in human aging and cancer. Int J Biochem Cell Biol. 2002, 34(11), 1430-48. [CrossRef]
- Bettuzzi, S. Chapter 1: Introduction. Adv Cancer Res. 2009, 104, 1-8.
- Prochnow, H., Gollan, R., Rohne, P., Hassemer, M., Koch-Brandt, C., & Baiersdörfer, M. Non-secreted clusterin isoforms are translated in rare amounts from distinct human mRNA variants and do not affect Bax-mediated apoptosis or the NF-kappaB signaling pathway. PLoS One. 2013, 8(9), e75303.
- Athanas, K.M., S.L. Mauney, & T.U. Woo, Increased extracellular clusterin in the prefrontal cortex in schizophrenia. Schizophr Res. 2015, 169(1-3), 381-5. [CrossRef]
- Yu, B., Yang, Y., Liu, H., Gong, M., Millard, R. W., Wang, Y. G., Ashraf, M., & Xu, M. Clusterin/Akt Up-Regulation Is Critical for GATA-4 Mediated Cytoprotection of Mesenchymal Stem Cells against Ischemia Injury. PLoS One. 2016, 11(3), e0151542. [CrossRef]
- Fandridis, E., Apergis, G., Korres, D. S., Nikolopoulos, K., Zoubos, A. B., Papassideri, I., & Trougakos, I. P. Increased expression levels of apolipoprotein J/clusterin during primary osteoarthritis. In Vivo. 2011, 25(5), 745-9.
- Suuronen, T., Nuutinen, T., Ryhänen, T., Kaarniranta, K., & Salminen, A. Epigenetic regulation of clusterin/apolipoprotein J expression in retinal pigment epithelial cells. Biochem Biophys Res Commun. 2007, 357(2), 397-401. [CrossRef]
- Prikrylova Vranova, H., Mareš, J., Nevrlý, M., Stejskal, D., Zapletalová, J., Hluštík, P., & Kaňovský, P. CSF markers of neurodegeneration in Parkinson's disease. J Neural Transm (Vienna). 2010, 117(10), 1177-81. [CrossRef]
- Weinstein, G., Beiser, A. S., Preis, S. R., Courchesne, P., Chouraki, V., Levy, D., & Seshadri, S. Plasma clusterin levels and risk of dementia, Alzheimer's disease, and stroke. Alzheimers Dement (Amst). 2016, 3, 103-9. [CrossRef]
- Schrijvers, E.M., Koudstaal, P. J., Hofman, A., & Breteler, M. M. Plasma clusterin and the risk of Alzheimer disease. JAMA. 2011, 305(13), 1322-6. [CrossRef]
- Chen, D., et al. Antisense oligonucleotide against clusterin regulates human hepatocellular carcinoma invasion through transcriptional regulation of matrix metalloproteinase-2 and E-cadherin. Int J Mol Sci. 2012, 13(8), 10594-607. [CrossRef]
- Cheng, C.Y., Wang, Y., Zhang, K., Jiao, X., Yan, B., & Liang, J. Regulation of chemosensitivity and migration by clusterin in non-small cell lung cancer cells. Cancer Chemother Pharmacol. 2012, 69(1), 145-54.
- Lourda, M., I.P., Trougakos, & E.S. Gonos. Development of resistance to chemotherapeutic drugs in human osteosarcoma cell lines largely depends on up-regulation of Clusterin/Apolipoprotein J. Int J Cancer. 2007, 120(3), 611-22. [CrossRef]
- Yang, G., Zhang, H., Liu, Y., Zhou, J., He, W., Quick, C. M., Xie, D., Smoller, B. R., & Fan, C. Y. Epigenetic and immunohistochemical characterization of the Clusterin gene in ovarian tumors. Arch Gynecol Obstet. 2013, 287(5), 989-95. [CrossRef]
- Tellez, T., García-Aranda, M., & Redondo, M. The role of clusterin in carcinogenesis and its potential utility as a therapeutic target. Curr Med Chem. 2016, 23, 1-12 (In Press). [CrossRef]
- Trougakos, I.P., Pawelec, G., Tzavelas, C., Ntouroupi, T., & Gonos, E. S. Clusterin/Apolipoprotein J up-regulation after zinc exposure, replicative senescence, or differentiation of human hematopoietic cells. Biogerontolog. 2006, 7(5-6), 375-82. [CrossRef]
- http://www.ensembl.org. Available at: http://www.ensembl.org/Homo_sapiens/Gene/Summary?g=ENSG00000120885,r=8:27596917-27615031.
- http://vega.sanger.ac.uk. Available at: http://vega.sanger.ac.uk/Homo_sapiens/Gene/Summary?g=OTTHUMG00000102114,r=8:27596917-27615031.
- Bonacini, M., Coletta, M., Ramazzina, I., Naponelli, V., Modernelli, A., Davalli, P., Bettuzzi, S., & Rizzi, F. Distinct promoters, subjected to epigenetic regulation, drive the expression of two clusterin mRNAs in prostate cancer cells. Biochim Biophys Acta. 2015, 1849(1), 44-54. [CrossRef]
- Rizzi, F., M. Coletta, & S. Bettuzzi. Chapter 2: Clusterin (CLU): From one gene and two transcripts to many proteins. Adv Cancer Res. 2009, 104, 9-23.
- Yu, J.T. & L. Tan. The role of clusterin in Alzheimer's disease: pathways, pathogenesis, and therapy. Mol Neurobiol. 2012, 45(2), 314-26.
- Foster, E.M., Dangla-Valls, A., Lovestone, S., Ribe, E.M., Buckley, N.J. Clusterin in Alzheimer's Disease: Mechanisms, Genetics, and Lessons from Other Pathologies. Front. Neurosci. 2019, 13, 164.
- Rohne, P., H. Prochnow, & C. Koch-Brandt. The CLU-files: disentanglement of a mystery. Biomol Concepts. 2016, 7(1), 1-15. [CrossRef]
- Zhang, Q., Zhou, W., Kundu, S., Jang, T. L., Yang, X., Pins, M., Smith, N., Jovanovic, B., Xin, D., Liang, L., Guo, Y., & Lee, C. The leader sequence triggers and enhances several functions of clusterin and is instrumental in the progression of human prostate cancer in vivo and in vitro. BJU Int. 2006, 98(2), 452-60. [CrossRef]
- Poon, S., Treweek, T. M., Wilson, M. R., Easterbrook-Smith, S. B., & Carver, J. A. Clusterin is an extracellular chaperone that specifically interacts with slowly aggregating proteins on their off-folding pathway. FEBS Lett. 2002, 513(2-3), 259-66. [CrossRef]
- Trougakos, I.P., Gonos, E.S. Regulation of clusterin/apolipoprotein J, a functional homologue to the small heat shock proteins, by oxidative stress in aging and age-related diseases. Free. Radic. Res. 2006, 40, 1324–1334. [CrossRef]
- Bettuzzi, S., Scorcioni, F., Astancolle, S., Davalli, P., Scaltriti, M., Corti, A. Clusterin (SGP-2) transient overexpression decreases proliferation rate of SV40-immortalized human prostate epithelial cells by slowing down cell cycle progression. Oncogene 2002, 21, 4328–4334. [CrossRef]
- Pucci, S., Bonanno, E., Pichiorri, F., Angeloni, C., Spagnoli, L. G. Modulation of different clusterin isoforms in human colon tumorigenesis. Oncogene 2004, 23, 2298–2304. [CrossRef]
- Caccamo, A. E., Scaltriti, M., Caporali, A., D'Arca, D., Corti, A., Corvetta, D., Sala, A., Bettuzzi, S. Ca2+ depletion induces nuclear clusterin, a novel effector of apoptosis in immortalized human prostate cells. Cell Death Differ. 2005, 12, 101–104. [CrossRef]
- Caccamo, A.E., Scaltriti, M., Caporali, A., D'Arca, D., Scorcioni, F., Astancolle, S., Mangiola, M., Bettuzzi, S. Cell detachment and apoptosis induction of immortalized human prostate epithelial cells are associated with early accumulation of a 45 kDa nuclear isoform of clusterin. Biochem. J. 2004, 382, 157–168. [CrossRef]
- Leskov, K.S., Klokov, D.Y., Li, J., Kinsella, T.J., Boothman, D.A. Synthesis and functional analyses of nuclear clusterin, a cell death protein. J. Biol. Chem. 2003, 278, 11590–11600. [CrossRef]
- Li, N., Zoubeidi, A., Beraldi, E., Gleave, M. E. GRP78 regulates clusterin stability, retrotranslocation and mitochondrial localization under ER stress in prostate cancer. Oncogene 2013, 32, 1933–1942. [CrossRef]
- Trougakos, I.P., Gonos, E.S. Regulation of clusterin/apolipoprotein J, a functional homologue to the small heat shock proteins, by oxidative stress in aging and age-related diseases. Free. Radic. Res. 2006, 40, 1324–1334. [CrossRef]
- Nizard, P., Tetley, S., Le Dréan, Y., Watrin, T., Le Goff, P., Wilson, M.R., and Michel, D. Stress-Induced Retrotranslocation of Clusterin/ApoJ into the Cytosol. Traffic 2007, 8, 554–565. [CrossRef]
- Scaltriti, M., Bettuzzi, S., Sharrard, R.M., Caporali, A., Caccamo, A.E., Maitland, N.J. Clusterin overexpression in both malignant and nonmalignant prostate epithelial cells induces cell cycle arrest and apoptosis. Br. J. Cancer 2004, 91, 1842–1850. [CrossRef]
- Scaltriti, M., Santamaria, A., Paciucci, R., Bettuzzi, S. Intracellular clusterin induces G2-M phase arrest and cell death in PC-3 prostate cancer cells1. Cancer Res. 2004, 64, 6174–6182. [CrossRef]
- Park, S., Mathis, K.W., Lee, I.K. The physiological roles of apolipoprotein J/clusterin in metabolic and cardiovascular diseases. Rev. Endocr. Metab. Disord. 2014, 15, 45–53. [CrossRef]
- Zoubeidi, A., Chi, K., Gleave, M. Targeting the cytoprotective chaperone, clusterin, for treatment of advanced cancer. Clin. Cancer Res. 2010, 16, 1088–1093. [CrossRef]
- Goetz, E. M., Shankar, B., Zou, Y., Morales, J. C., Luo, X., Araki, S., Bachoo, R., Mayo, L. D., Boothman, D. A. ATM dependent IGF-1 induction regulates secretory clusterin expression after DNA damage and in genetic instability. Oncogene. Nat. Publ. Group 2011, 30, 3745–3754. [CrossRef]
- Prochnow, H., Gollan, R., Rohne, P., Hassemer, M., Koch-Brandt, C., Baiersdörfer, M. Non-Secreted Clusterin Isoforms Are Translated in Rare Amounts from Distinct Human mRNA Variants and Do Not Affect BaxMediated Apoptosis or the NF-κB Signaling Pathway. PLoS ONE 2013, 8, e75303.
- Michel, D., Chatelain, G., North, S., Brun, G. Stress-induced transcription of the clusterin/apoJ gene. Biochem. J. 1997, 50, 45–50. [CrossRef]
- Trougakos, I.P. The Molecular Chaperone Apolipoprotein J/Clusterin as a Sensor of Oxidative Stress: Implications in Therapeutic Approaches—A Mini-Review. Gerontology 2013, 59, 514–523. [CrossRef]
- July, L.V., Akbari, M., Zellweger, T., Jones, E.C., Goldenberg, S.L., Gleave, M.E. Clusterin expression is significantly enhanced in prostate cancer cells following androgen withdrawal therapy. Prostate 2002, 50, 179–188. [CrossRef]
- FitzGerald, P. C., Shlyakhtenko, A., Mir, A. A., & Vinson, C. Clustering of DNA sequences in human promoters. Genome research. 2004, 14(8), 1562–1574. [CrossRef]
- Kim, N., & Choi, W. S. Proapoptotic role of nuclear clusterin in brain. Anatomy & cell biology. 2011, 44(3), 169–175. [CrossRef]
- Wong, P., Taillefer, D., Lakins, J., Pineault, J., Chader, G., & Tenniswood, M. Molecular characterization of human TRPM-2/clusterin, a gene associated with sperm maturation, apoptosis and neurodegeneration. Eur J Biochem. 1994, 221(3), 917-25.
- Deb, M., Sengupta, D., Rath, S.K., Kar, S., Parbin, S., Shilpi, A., et al. Clusterin gene is predominantly regulated by histone modifications in human colon cancer and ectopic expression of the nuclear isoform induces cell death. Biochim. Biophys. Acta. Elsevier B.V. 2015, 1852, 1630–1645. [CrossRef]
- Suuronen, T., Nuutinen, T., Ryhänen, T., Kaarniranta, K., & Salminen, A. Epigenetic regulation of clusterin/apolipoprotein J expression in retinal pigment epithelial cells. Biochem Biophys Res Commun. 2007, 357(2), 397-401. [CrossRef]
- Hellebrekers, D. M., Melotte, V., Viré, E., Langenkamp, E., Molema, G., Fuks, F., Herman, J. G., Van Criekinge, W., Griffioen, A. W., & van Engeland, M. Identification of epigenetically silenced genes in tumor endothelial cells. Cancer research. 2007, 67(9), 4138–4148. [CrossRef]
- Serrano, A., Redondo, M., Tellez, T., Castro-Vega, I., Roldan, M.J., Mendez, R., Rueda, A., Jiménez, E. Regulation of clusterin expression in human cancer via DNA methylation. Tumour. Biol. 2009, 30, 286–291. [CrossRef]
- Handy, D.E., R. Castro, & J. Loscalzo, Epigenetic modifications: basic mechanisms and role in cardiovascular disease. Circulation. 2011, 123(19), 2145-56.
- Liao, F. T., Lee, Y. J., Ko, J. L., Tsai, C. C., Tseng, C. J., & Sheu, G. T. Hepatitis delta virus epigenetically enhances clusterin expression via histone acetylation in human hepatocellular carcinoma cells. The Journal of general virology. 2009, 90(Pt 5), 1124–1134. [CrossRef]
- Rauhala, H. E., Porkka, K. P., Saramäki, O. R., Tammela, T. L., & Visakorpi, T. Clusterin is epigenetically regulated in prostate cancer. International journal of cancer. 2008, 123(7), 1601–1609. [CrossRef]
- Rosemblit, N., Chen, C.L. Regulators for the rat clusterin gene: DNA methylation and cis-acting regulatory elements. J. Mol. Endocrinol. 1994, 13, 69–76. [CrossRef]
- Ambros V. The functions of animal microRNAs. Nature. 2004, 431(7006), 350–355. [CrossRef]
- Mydlarz, W., Uemura, M., Ahn, S., Hennessey, P., Chang, S., Demokan, S., Sun, W., Shao, C., Bishop, J., Krosting, J., Mambo, E., Westra, W., Ha, P., Sidransky, D., & Califano, J. Clusterin is a gene-specific target of microRNA-21 in head and neck squamous cell carcinoma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2014, 20(4), 868–877.
- Chen, X., Jiang, Y., Huang, Z., Li, D., Chen, X., Cao, M., Meng, Q., Pang, H., Sun, L., Zhao, Y., & Cai, L. miRNA-378 reverses chemoresistance to cisplatin in lung adenocarcinoma cells by targeting secreted clusterin. Scientific reports. 2016, 6, 19455. [CrossRef]
- Buttyan, R., Olsson, C. A., Pintar, J., Chang, C., Bandyk, M., Ng, P. Y., & Sawczuk, I. S. Induction of the TRPM-2 gene in cells undergoing programmed death. Mol Cell Biol. 1989, 9(8), 3473-81. [CrossRef]
- Leger, J.G., M.L. Montpetit, & M.P. Tenniswood, Characterization and cloning of androgen-repressed mRNAs from rat ventral prostate. Biochem Biophys Res Commun, 1987, 147(1), 196-203. [CrossRef]
- Leger, J.G., R. Le Guellec, & M.P. Tenniswood, Treatment with antiandrogens induces an androgen-repressed gene in the rat ventral prostate. Prostate. 1988, 13(2), 131-42. [CrossRef]
- Sensibar, J.A., Sutkowski, D. M., Raffo, A., Buttyan, R., Griswold, M. D., Sylvester, S. R., Kozlowski, J. M., & Lee, C. Prevention of cell death induced by tumor necrosis factor alpha in LNCaP cells by overexpression of sulfated glycoprotein-2 (clusterin). Cancer Res. 1995, 55(11), 2431-7.
- Schwochau, G.B., K.A. Nath, & M.E. Rosenberg. Clusterin protects against oxidative stress in vitro through aggregative and nonaggregative properties. Kidney Int. 1998, 53(6), 1647-53. [CrossRef]
- Leskov, K.S., Klokov, D. Y., Li, J., Kinsella, T. J., & Boothman, D. A. Synthesis and functional analyses of nuclear clusterin, a cell death protein. J Biol Chem. 2003, 278(13), 11590-600. [CrossRef]
- Yang, C.R., L.K., Hosley-Eberlein, K., Criswell, T., Pink, J., Kinsella, T., Boothman, D. Nuclear Clusterin/XIP8, an x-ray-induced Ku70-binding protein that signals cell death. PNAS. 2000, 97 (11), 5907-12.
- Leskov, K.S., Araki, S., Lavik, J. P., Gomez, J. A., Gama, V., Gonos, E. S., Trougakos, I. P., Matsuyama, S., & Boothman, D. A. CRM1 protein-mediated regulation of nuclear clusterin (nCLU), an ionizing radiation-stimulated, Bax-dependent pro-death factor. J Biol Chem. 2011, 286(46), 40083-90. [CrossRef]
- Essabbani, A., Garcia, L., Zonetti, M. J., Fisco, T., Pucci, S., & Chiocchia, G. Exon-skipping strategy by ratio modulation between cytoprotective versus pro-apoptotic clusterin forms increased sensitivity of LNCaP to cell death. PLoS One. 2013, 8(2), e54920. [CrossRef]
- Kim, N. & W.S. Choi. Proapoptotic role of nuclear clusterin in brain. Anat Cell Biol. 2011, 44(3), 169-75. [CrossRef]
- García-Aranda, M., Serrano, A., & Redondo, M. Regulation of Clusterin Gene Expression. Current protein & peptide science. 2017, 19. [CrossRef]
- Kim, N., Yoo, J. C., Han, J. Y., Hwang, E. M., Kim, Y. S., Jeong, E. Y., Sun, C. H., Yi, G. S., Roh, G. S., Kim, H. J., Kang, S. S., Cho, G. J., Park, J. Y., & Choi, W. S. Human nuclear clusterin mediates apoptosis by interacting with Bcl-XL through C-terminal coiled coil domain. J Cell Physiol. 2012, 227(3), 1157-67. [CrossRef]
- Shannan B, S.M., Leskov K, Willis J, Boothman D, Tilgen W, Reichrath J. Challenge and promise: roles for clusterin in pathogenesis, progression and therapy of cancer. Cell Death Differ. 2006, 13, 12-19.
- Prochnow, H., Gollan, R., Rohne, P., Hassemer, M., Koch-Brandt, C., & Baiersdörfer, M. Non-secreted clusterin isoforms are translated in rare amounts from distinct human mRNA variants and do not affect Bax-mediated apoptosis or the NF-kappaB signaling pathway. PLoS One. 2013, 8(9), e75303.
- Viard, I., Wehrli, P., Jornot, L., Bullani, R., Vechietti, J.-L., French, L.E., Schifferli, J.A., Tschopp, J. Clusterin gene expression mediates resistance to apoptotic cell death induced by heat shock and oxidative stress. J. Invest. Dermatol. 1999, 112, 290–296. [CrossRef]
- Nicholson, G., Lawrence, A., Ala, F.A., Bird, G.W. Semi-quantitative assay of antigen site density by flow cytometry analysis. Transfusion. Medicine. 1991, 1, 87–90.
- Trougakos, I.P., Lourda, M., Antonelou, M.H., Kletsas, D., Gorgoulis, V.G., Papassideri, I.S., Zou, Y., Margaritis, L.H., Boothman, D.A., Gonos, E.S. Intracellular clusterin inhibits mitochondrial apoptosis by suppressing stress signals activating p53 and stabilizing the cytosolic Ku70-Bax protein complex. Clin. Cancer Res. 2009, 15, 48–59. [CrossRef]
- Blume, A.J., Foster, C.J. Adenylate cyclase of mouse neuroblastoma cells: regulation by 2-chloroadenosine, prostaglandin E1, and the cations Mg2+, Ca2+, and Mn2+. J. Neurochem. 1976, 26, 305–311.
- Scaltriti, M., Bettuzzi, S., Sharrard, R.M., Caporali, A., Caccamo, A.E., Maitland, N.J. Overexpression of clusterin in both malignant and nonmalignant prostate epithelial cells induces cell cycle arrest and apoptosis. Br. J. Cancer. 2004, 91, 1842–1850. [CrossRef]
- Cervellera, M., Raschella, G., Santilli, G., Tanno, B., Ventura, A., Mancini, C., Sevignani, C., Calabretta, B., Sala, A. Direct transactivation of the antiapoptotic gene apolipoprotein J (Clusterin) by B-MYB. J. Biol. Chem. 2000, 275, 21055–21060. [CrossRef]
- Ma, X., Bai, Y. IGF-1 activates the P13K/AKT signaling pathway by positively regulating secretory clusterin. Mol. Med. Rep. 2012, 6, 1433-1437.
- Flanagan, L., Whyte, L., Chatterjee, N., Tenniswood, M. Effects of clusterin overexpression on metastatic progression and therapy in breast cancer. BMC Cancer. 2010, 10, 107. [CrossRef]
- Meunier, A., Cornet, F., Campos, M. Bacterial cell proliferation: from molecules to cells. FEMS Microbiol Rev. 2020. [CrossRef]
- Wang, Z. Regulation of cell cycle progression by growth factor-induced cell signaling. Cells. 2021, 10, 3327. [CrossRef]
- Zhang, Y., Lv, X., Chen, L., & Liu, Y. The role and function of CLU in cancer biology and therapy. Clinical and experimental medicine. 2023, 23(5), 1375–1391. [CrossRef]
- Dews, M., Fox, J. L., Hultine, S., Sundaram, P., Wang, W., Liu, Y. Y., Furth, E., Enders, G. H., El-Deiry, W., Schelter, J. M., Cleary, M. A., & Thomas-Tikhonenko, A. The myc-miR-17~92 axis blunts TGF{beta} signaling and production of multiple TGF{beta}-dependent antiangiogenic factors. Cancer research. 2010, 70(20), 8233–8246.
- Suzuki, S., Shiraga, K., Sato, S., Punfa, W., Naiki-Ito, A., Yamashita, Y., Shirai, T., & Takahashi, S. Apocynin, an NADPH oxidase inhibitor, suppresses rat prostate carcinogenesis. Cancer science. 2013, 104(12), 1711–1717. [CrossRef]
- Huang, H., Wang, L., Li, M., Wang, X., & Zhang, L. Secreted clusterin (sCLU) regulates cell proliferation and chemosensitivity to cisplatin by modulating ERK1/2 signals in human osteosarcoma cells. World journal of surgical oncology. 2014, 12, 255.
- Wang, X., Xie, J., Lu, X., Li, H., Wen, C., Huo, Z., Xie, J., Shi, M., Tang, X., Chen, H., Peng, C., Fang, Y., Deng, X., & Shen, B. Melittin inhibits tumor growth and decreases resistance to gemcitabine by downregulating cholesterol pathway gene CLU in pancreatic ductal adenocarcinoma. Cancer Lett. 2017, 399, 1–9. [CrossRef]
- Chen, Z., Fan, Z., Dou, X., Zhou, Q., Zeng, G., Liu, L., Chen, W., Lan, R., Liu, W., Ru, G., Yu, L., He, Q. Y., & Chen, L. Inactivation of tumor suppressor gene Clusterin leads to hyperactivation of TAK1-NF-kappaB signaling axis in lung cancer cells and denotes a therapeutic opportunity. Theranostics. 2020, 10(25), 11520–34.
- Chun, Y.J. Knockdown of clusterin expression increases the in vitro sensitivity of human prostate cancer cells to paclitaxel. J Toxicol Environ Health A. 2014, 77(22–24), 1443–50. [CrossRef]
- Zheng, W., Yao, M., Qian, Q., Sai, W., Qiu, L., Yang, J., Wu, W., Dong, Z., & Yao, D. Oncogenic secretory clusterin in hepatocellular carcinoma: Expression at early staging and emerging molecular target. Oncotarget. 2016, 8(32), 52321–32. [CrossRef]
- Bailes, J., Soloviev, M. Insulin-Like Growth Factor-1 (IGF-1) and Its Monitoring in Medical Diagnostic and in Sports. Biomolecules. 2021, 11(2), 217. [CrossRef]
- Ma, X., Bai, Y. IGF-1 activates the P13K/AKT signaling pathway via upregulation of secretory clusterin. Mol Med Rep. 2012, 6(6), 1433–7. [CrossRef]
- Takeuchi, A., Shiota, M., Beraldi, E., Thaper, D., Takahara, K., Ibuki, N., Pollak, M., Cox, M. E., Naito, S., Gleave, M. E., & Zoubeidi, A. Insulin-like growth factor-I induces CLU expression through Twist1 to promote prostate cancer growth. Mol Cell Endocrinol. 2014, 384(1–2), 117–25. [CrossRef]
- Chesnokova, V., Zonis, S., Wawrowsky, K., Tani, Y., Ben-Shlomo, A., Ljubimov, V., Mamelak, A., Bannykh, S., & Melmed, S. Clusterin and FOXL2 act concordantly to regulate pituitary gonadotroph adenoma growth. Mol Endocrinol. 2012, 26(12), 2092–103. [CrossRef]
- Deng, J., Peng, M., Zhou, S., Xiao, D., Hu, X., Xu, S., Wu, J., & Yang, X. Metformin targets Clusterin to control lipogenesis and inhibit the growth of bladder cancer cells through SREBP-1c/FASN axis. Signal Transduct Target Ther. 2021, 6(1), 98. [CrossRef]
- Liu, Y., Men, C., Xu, Y., Zhao, K., Luo, L., Dong, D., & Yu, Q. Clusterin promotes growth and invasion of clear cell renal carcinoma cell by upregulation of S100A4 expression. Cancer Biomark. 2018, 21(4), 915–23. [CrossRef]
- Pajak, B., Kania, E., Gajkowska, B., & Orzechowski, A. Lipid rafts mediate epigallocatechin-3-gallate- and green tea extract-dependent viability of human colon adenocarcinoma COLO 205 cells; clusterin affects lipid rafts-associated signaling pathways. J Physiol Pharmacol Official J Polish Physiol Soc. 2011, 62(4), 449–59.
- Tang, Z., Wang, W., Liu, Z., Sun, X., Liao, Z., Chen, F., Jiang, G., Huo, G. Blocking ERK signaling pathway reduces MMP-9 expression to alleviate cerebral edema after traumatic brain injury in rats. Nan Fang Yi Ke Da Xue Xue Bao. 2020, 40, 1018-1022.
- Shim, Y.-J., Kang, B.-H., Jeon, H.-S., Park, I.-S., Lee, K.-U., Lee, I.-K., Park, G.-H., Lee K.-M., Schedin P., Min B.-H. Clusterin induces matrix metalloproteinase-9 expression via ERK1/2 and PI3K/Akt/NF-κB pathways in monocytes/macrophages. J. Leukoc. Biol. 2011, 90, 761–769.
- Li, Y., Lu, J., Zhou, S., Wang, W., Tan, G., Zhang, Z., Dong, Z., Kang, T., Tang, F. N, N′-dinitrosopiperazine-induced clusterin participates in nasopharyngeal carcinoma metastasis. Oncotarget. 2016, 7, 5548–5563.
- Tian, Y., Wang, C., Chen, S., Liu, J., Fu, Y., Luo, Y. Extracellular Hsp90alpha and clusterin synergistically promote breast cancer epithelial-to-mesenchymal transition and metastasis through LRP1. J. Cell Sci. 2019, 132, jcs228213.
- Yang, P., Yang, Z., Dong, Y., Yang, L., Peng, S., Yuan, L., Hu, X., Chen, S., Tang, H., Yang, X., et al. Clusterin is a prognostic biomarker of breast cancer and correlates with the immune microenvironment. Transl Cancer Res. 2023, 12, 31–45.
- Yang, S., Tang, W., Azizian, A., Gaedcke, J., Strobel, P., Wang, L., Cawley, H., Ohara, Y., Valenzuela, P., Zhang L., et al. Dysregulation of the HNF1B/Clusterin axis enhances disease progression in a highly aggressive subset of pancreatic cancer patients. Carcinogenesis. 2022, 43, 1198-1210. [CrossRef]
- Mansoori, B., Mohammadi, A., Davudian, S., Shirjang, S., Baradaran, B. Different mechanisms of resistance to cancer drugs: a brief review. Adv. Pharm. Bull. 2017, 7, 339–348.
- Whitesell, L., Lindquist, S.L. HSP90 and the chaperoning of cancer. Nat. Rev. Cancer. 2005, 5, 761–772. [CrossRef]
- Zhang, H., Kim, J.K., Edwards, C.A., Xu, Z., Taichman, R., Wang, C.-Y. Clusterin inhibits apoptosis by interacting with activated Bax. Nat. Cell Biol. 2005, 7, 909–915. [CrossRef]
- Tang, M., Li, J., Liu, B., Song, N., Wang, Z., Yin, C. Clusterin expression in human testicular seminoma. Med. Hypotheses. 2013, 81, 635–637. [CrossRef]
- Wang, X., Zou, F., Zhong, J., Yue, L., Wang, F., Wei, H., Yang, G., Jin, T., Dong, X., Li J., et al. Secretory clusterin mediates resistance to oxaliplatin through the Gadd45a/PI3K/Akt signaling pathway in hepatocellular carcinoma. J. Cancer. 2018, 9, 1403-1413.
- Panico, F., Rizzi, F., Fabbri, L. M., Bettuzzi, S., & Luppi, F. Clusterin (CLU) and lung cancer. Advances in cancer research. 2009, 105, 63–76.
- July, L. V., Beraldi, E., So, A., Fazli, L., Evans, K., English, J. C., Gleave, M. E. Nucleotide-based therapies targeting clusterin chemosensitize human lung adenocarcinoma cells both in vitro and in vivo. Mol. Cancer Ther. 2004, 3, 223–232.
- Bi, J., Guo, A. L., Lai, Y. R., Li, B., Zhong, J. M., Wu, H. Q., Xie, Z., He, Y. L., Lv, Z. L., Lau, S. H., et al. Overexpression of clusterin correlates with tumor progression, metastasis in gastric cancer: A study on tissue microarrays. Neoplasm. 2010, 57, 191. [CrossRef]
- Xie, D., Lau, S.H., Sham, J.S., Wu, Q.L., Fang, Y., Liang, L.Z., Che, L.H., Zeng, Y.X., Guan, X.Y. Up-regulated expression of cytoplasmic clusterin in human ovarian carcinoma. Cancer. 2005, 103, 277–283. [CrossRef]
- Yang, G. F., Li, X. M., & Xie, D. Overexpression of clusterin in ovarian cancer is correlated with impaired survival. International journal of gynecological cancer: official journal of the International Gynecological Cancer Society. 2009, 19(8), 1342–1346.
- Al-Maghrabi, J. A., Butt, N. S., Anfinan, N., Sait, K., Sait, H., Bajouh, O., & Khabaz, M. N. Clusterin immunoexpression is associated with early stage endometrial carcinomas. Acta histochemical. 2016, 118(4), 430–434. [CrossRef]
- Fuzio, P., Valletti, A., Napoli, A., Napoli, G., Cormio, G., Selvaggi, L., Liuni, S., Pesole, G., Maiorano, E., & Perlino, E. Regulation of the expression of CLU isoforms in endometrial proliferative diseases. International journal of oncology. 2013, 42(6), 1929–1944. [CrossRef]
- Won, Y. S., Lee, S. J., Yeo, S. G., & Park, D. C. Effects of female sex hormones on clusterin expression and paclitaxel resistance in endometrial cancer cell lines. International journal of medical sciences. 2012, 9(1), 86–92. [CrossRef]
- Park, D. C., Yeo, S. G., Shin, E. Y., Mok, S. C., & Kim, D. H. Clusterin confers paclitaxel resistance in cervical cancer. Gynecologic oncology. 2006, 103(3), 996–1000. [CrossRef]
- Niu, Z., Li, X., Hu, B., Li, R., Wang, L., Wu, L., & Wang, X. Small interfering RNA targeted to secretory clusterin blocks tumor growth, motility, and invasion in breast cancer. Acta biochimica et biophysica Sinica. 2012, 44(12), 991–998. [CrossRef]
- Li, J., Jia, L., Zhao, P., Jiang, Y., Zhong, S., & Chen, D. Stable knockdown of clusterin by vectorbased RNA interference in a human breast cancer cell line inhibits tumour cell invasion and metastasis. The Journal of international medical research. 2012, 40(2), 545–555. [CrossRef]
- Redondo, M., Villar, E., Torres-Muñoz, J., Tellez, T., Morell, M., Petito, C. K. Overexpression of clusterin in human breast carcinoma. Am. J. Pathol. 2000, 157, 393–39. [CrossRef]
- Zhang, D., Sun, B., Zhao, X., Cui, Y., Xu, S., Dong, X., Zhao, J., Meng, J., Jia, X., & Chi, J. Secreted CLU is associated with the initiation of triple-negative breast cancer. Cancer biology & therapy. 2012, 13(5), 321–329. [CrossRef]
- Niu, Z. H., Wang, Y., Chun, B., Li, C. X., & Wu, L. Secretory clusterin (sCLU) overexpression is associated with resistance to preoperative neoadjuvant chemotherapy in primary breast cancer. European review for medical and pharmacological sciences. 2013, 17(10), 1337–1344.
- Redondo, M., Tellez, T., and Roldan, M.J. The role of clusterin (CLU) in malignant transformation and drug resistance in breast carcinomas. Adv. Cancer Res. 2009, 105, 21–43.
- Mazzarelli, P., Pucci, S., Spagnoli, L.G. CLU and colon cancer. The dual face of CLU: From the normal to the malignant phenotype. Adv. Cancer Res. 2009, 105, 45–61.
- Pucci, S., Bonanno, E., Pichiorri, F., Angeloni, C., & Spagnoli, L. G. Modulation of different clusterin isoforms in human colon tumorigenesis. Oncogene. 2004, 23(13), 2298–2304. [CrossRef]
- Redondo, M.; Rodrigo, I.; Alcaide, J.; Tellez, T.; Roldan, M.J.; Funez, R.; Diaz-Martin, A.; Rueda, A.; Jiménez, E. Clusterin expression is associated with decreased disease-free survival of patients with colorectal carcinomas. Histopathology. 2010, 56, 932–936. [CrossRef]
- Sun, B., Moibi, J. A., Mak, A., Xiao, Z., Roa, W., & Moore, R. B. Response of bladder carcinoma cells to TRAIL and antisense oligonucleotide, Bcl-2 or clusterin treatments. The Journal of urology. 2009, 181(3), 1361–1371. [CrossRef]
- Miyake, H., Gleave, M., Kamidono, S., Hara, I. Overexpression of clusterin in transitional cell carcinoma of the bladder is related to disease progression and recurrence. Urology. 2002, 59, 150–154. [CrossRef]
- Hazzaa, S. M., Elashry, O. M., & Afifi, I. K. Clusterin as a diagnostic and prognostic marker for transitional cell carcinoma of the bladder. Pathology oncology research:POR. 2010, 16(1), 101–109. [CrossRef]
- Lau, S. H., Sham, J. S., Xie, D., Tzang, C. H., Tang, D., Ma, N., Hu, L., Wang, Y., Wen, J. M., Xiao, G., Zhang, W. M., Lau, G. K., Yang, M., & Guan, X. Y. Clusterin plays an important role in hepatocellular carcinoma metastasis. Oncogene. 2006, 25(8), 1242–1250. [CrossRef]
- Chen, D., Wang, Y., Zhang, K., Jiao, X., Yan, B., & Liang, J. Antisense oligonucleotide against clusterin regulates human hepatocellular carcinoma invasion through transcriptional regulation of matrix metalloproteinase-2 and E-cadherin. International journal of molecular sciences. 2012, 13(8), 10594–10607. [CrossRef]
- Xiu, P., Dong, X., Dong, X., Xu, Z., Zhu, H., Liu, F., Wei, Z., Zhai, B., Kanwar, J. R., Jiang, H., Li, J., & Sun, X. Secretory clusterin contributes to oxaliplatin resistance by activating Akt pathway in hepatocellular carcinoma. Cancer science. 2013, 104(3), 375–382. [CrossRef]
- Patarat, R.; Riku, S.; Kunadirek, P.; Chuaypen, N.; Tangkijvanich, P.; Mutirangura, A.; Puttipanyalears, C. The expression of FLNA and CLU in PBMCs as a novel screening marker for hepatocellular carcinoma. Sci. Rep. 2021, 11, 14838. [CrossRef]
- Gao, G., Luan, X. Diagnostic performance of clusterin in hepatocellular carcinoma: A meta-analysis. Int. J. Biol. Markers. 2022, 37, 404–411. [CrossRef]
- Rasmy, H. S., Mohammed, H. A., Mohammed, E. S., Ahmed, A. S. M., & Isaac, A. Serum clusterin as a promising diagnostic and prognostic marker for hepatocellular carcinoma after locoregional treatment. The Egyptian journal of immunology. 2022, 29(2), 26–40. [CrossRef]
- Li, Y., Wang, X., Chen, Y. H., Tan, Q. Q., Liu, X. B., & Tan, C. Clusterin is upregulated by erastin, a ferroptosis inducer and exerts cytoprotective effects in pancreatic adenocarcinoma cells. Anti-cancer drugs. 2023, 10.1097/CAD.0000000000001561. Advance online publication.1. [CrossRef]
- Xie, M.J., Motoo, Y., Su, S.B., Mouri, H., Ohtsubo, K., Matsubara, F., Sawabu, N. Expression of clusterin in human pancreatic cancer. Pancreas. 2002, 25, 234–238. [CrossRef]
- Hoeller, C., Pratscher, B., Thallinger, C., Winter, D., Fink, D., Kovacic, B., Sexl, V., Wacheck, V., Gleave, M.E., Pehamberger, H., et al. Clusterin regulates drug-resistance in melanoma cells. J. Investig. Dermatol. 2005, 124, 1300–1307. [CrossRef]
- He, L.R., Liu, M.Z., Li, B.K., Rao, H.L., Liao, Y.J., Zhang, L.J., Guan, X.Y., Zeng, Y.X., Xie, D. Clusterin as a predictor for chemoradiotherapy sensitivity and patient survival in esophageal squamous cell carcinoma. Cancer Sci. 2009, 100, 2354–2360. [CrossRef]
- Bijian, K., Mlynarek, A. M., Balys, R. L., Jie, S., Xu, Y., Hier, M. P., Black, M. J., Di Falco, M. R., LaBoissiere, S., & Alaoui-Jamali, M. A. Serum proteomic approach for the identification of serum biomarkers contributed by oral squamous cell carcinoma and host tissue microenvironment. Journal of proteome research. 2009, 8(5), 2173–2185. [CrossRef]
- Redondo, M., Fùnez, R., Esteban, F. Apoptosis in the Development and Treatment of Laryngeal Cancer: Role of p53, Bcl-2 and Clusterin. 2009. In: Chen, G.G., Lai, P.B. (eds) Apoptosis in Carcinogenesis and Chemotherapy. Springer, Dordrecht.
- Wellmann, A., Thieblemont, C., Pittaluga, S., Sakai, A., Jaffe, E. S., Siebert, P., Raffeld, M. Detection of differentially expressed genes in lymphomas using cDNA arrays: Identification of clusterin as a new diagnostic marker for anaplastic large-cell lymphomas. Blood. 2000, 96, 398–404.
- Ma, J., Gao, W., Gao, J. sCLU as prognostic biomarker and therapeutic target in osteosarcoma. Bioengineered. 2019, 10, 229–239. [CrossRef]
- Rizzi, F., Bettuzzi, S. Clusterin (CLU) and prostate cancer. Adv. Cancer Res. 2009, 105, 1–19.
- Miyake, H., Gleave, M. E., Arakawa, S., Kamidono, S., & Hara, I. Introducing the clusterin gene into human renal cell carcinoma cells enhances their metastatic potential. The Journal of urology. 2002, 167(5), 2203–2208.
- Shi, H., Deng, J. H., Wang, Z., Cao, K. Y., Zhou, L., & Wan, H. Knockdown of clusterin inhibits the growth and migration of renal carcinoma cells and leads to differential gene expression. Molecular medicine reports. 2013, 8(1), 35–40. [CrossRef]
- Beheshti Namdar, A., Kabiri, M., Mosanan Mozaffari, H., Aminifar, E., Mehrad-Majd, H. Circulating clusterin levels and cancer risk: A systematic review and meta-analysis. Cancer Control. 2022, 29, 10732748211038437. [CrossRef]
- Chen, D., Wang, Y., Zhang, K., Jiao, X., Yan, B., & Liang, J. Antisense oligonucleotide against clusterin regulates human hepatocellular carcinoma invasion through transcriptional regulation of matrix metalloproteinase-2 and E-cadherin. Int J Mol Sci. 2012, 13(8), 10594–607. [CrossRef]
- Nishikawa, M., Miyake, H., Gleave, M., & Fujisawa, M. Effect of targeting clusterin using OGX-011 on antitumor activity of temsirolimus in a human renal cell carcinoma model. Target Oncol. 2016, 12(1), 1–11. [CrossRef]
- Yamanaka, K., Gleave, M., Muramaki, M., Hara, I., & Miyake, H. Enhanced radiosensitivity by inhibition of the anti-apoptotic gene clusterin using antisense oligodeoxynucleotide in a human bladder cancer model. Oncol Rep. 2005, 13(5), 885. [CrossRef]
- Chen, Q., Wang, Z., Zhang, K., Liu, X., Cao, W., Zhang, L., Zhang, S., Yan, B., Wang, Y., & Xia, C. Clusterin confers gemcitabine resistance in pancreatic cancer. World J Surgical Oncol. 2011, 9, 1–8. [CrossRef]
- Cao, C., Shinohara, E. T., Li, H., Niermann, K. J., Kim, K. W., Sekhar, K. R., Gleave, M., Freeman, M., & Lu, B. Clusterin as a therapeutic target for radiation sensitization in a lung cancer model. Int J Radiat Oncol Biol Phys. 2005, 63(4), 1228–36. [CrossRef]
- Zellweger, T., et al. Enhanced radiation sensitivity in prostate cancer by inhibition of the cell survival protein clusterin. Clin Cancer Res. 2002, 8(10), 3276–84.
- So, A., Chi, K., Miyake, H., Adomat, H., Kiyama, S., Skov, K., & Gleave, M. E. Knockdown of the cytoprotective chaperone, clusterin, chemosensitizes human breast cancer cells both in vitro and in vivo. Mol Cancer Ther. 2005, 4(12), 1837–49.
- July, L. V., Beraldi, E., So, A., Fazli, L., Evans, K., English, J. C., Gleave, M. E. Nucleotide-based therapies targeting clusterin chemosensitize human lung adenocarcinoma cells both in vitro and in vivo. Mol. Cancer Ther. 2004, 3, 223–232.
- Hoeller, C., Pratscher, B., Thallinger, C., Winter, D., Fink, D., Kovacic, B., Sexl, V., Wacheck, V., Gleave, M.E., Pehamberger, H., et al. Clusterin regulates drug-resistance in melanoma cells. J. Investig. Dermatol. 2005, 124, 1300–1307. [CrossRef]
- Ma, J., Gao, W., Gao, J. sCLU as prognostic biomarker and therapeutic target in osteosarcoma. Bioengineered. 2019, 10, 229–239. [CrossRef]
- Zwain, I., & Amato, P. Clusterin protects granulosa cells from apoptotic cell death during follicular atresia. Experimental cell research. 2000, 257(1), 101–110. [CrossRef]
- Kususda, Y., Miyake, H., Gleave, M. E., & Fujisawa, M. Clusterin inhibition using OGX-011 synergistically enhances antitumour activity of sorafenib in a human renal cell carcinoma model. British journal of cancer. 2012, 106(12), 1945–1952. [CrossRef]
- Hassan, M. K., Watari, H., Han, Y., Mitamura, T., Hosaka, M., Wang, L., Tanaka, S., & Sakuragi, N. Clusterin is a potential molecular predictor for ovarian cancer patient's survival: targeting clusterin improves response to paclitaxel. Journal of experimental & clinical cancer research: CR. 2011, 30(1), 113.
- Blumenstein, B., Saad, F., Hotte, S., Chi, K. N., Eigl, B., Gleave, M., & Jacobs, C. Reduction in serum clusterin is a potential therapeutic biomarker in patients with castration-resistant prostate cancer treated with custirsen. Cancer Med. 2013, 2(4), 468–77. [CrossRef]
- Higano, C. S. Potential use of custirsen to treat prostate cancer. OncoTargets and therapy. 2013, 6, 785–797. [CrossRef]
- Chi, K.N., Hotte, S.J., Yu, E.Y., Tu, D., Eigl, B.J., Tannock, I., Saad, F., North, S., Powers, J., Gleave, M.E., et al. Randomized phase II study of docetaxel and prednisone with or without OGX-011 in patients with metastatic castration-resistant prostate cancer. J. Clin. Oncol. 2010, 28, 4247–4254. [CrossRef]
- Chia, S., Dent, S., Ellard, S., Ellis, P. M., Vandenberg, T., Gelmon, K., Powers, J., Walsh, W., Seymour, L., & Eisenhauer, E. A. Phase II trial of OGX-011 in combination with docetaxel in metastatic breast cancer. Clin Cancer Res. 2009, 15(2), 708–13. [CrossRef]
- Laskin, J.J., Nicholas, G., Lee, C., Gitlitz, B., Vincent, M., Cormier, Y., Stephenson, J., Ung, Y., Sanborn, R., Pressnail B., et al. Phase I/II trial of custirsen (OGX-011), an inhibitor of clusterin, in combination with a gemcitabine and platinum regimen in patients with previously untreated advanced non-small cell lung cancer. J. Thorac. Oncol. 2012, 7, 579–586. [CrossRef]
- Ma, X., Zou, L., Li, X., Chen, Z., Lin, Q., & Wu, X. MicroRNA-195 regulates docetaxel resistance by targeting clusterin in prostate cancer. Biomed Pharmacother. 2018, 99, 445–50; Zhao, W., Wang, X., Jiang, Y., Jia, X., & Guo, Y. miR-217-5p inhibits invasion and metastasis of prostate cancer by targeting clusterin. Mamm Genome. 2021, 32(5), 371–80.
- Davalli, P., Rizzi, F., Caldara, G. F., Davoli, S., Corti, A., Silva, A., Astancolle, S., Vitale, M., Bettuzzi, S., Arcari, M., & Azzali, G. Chronic administration of green tea extract to TRAMP mice induces the collapse of Golgi apparatus in prostate secretory cells and results in alterations of protein post-translational processing. Int J Oncol. 2011, 39(6), 1521–7. [CrossRef]
- Zhu, Y., Chen, P., Gao, Y., Ta, N., Zhang, Y., Cai, J., Zhao, Y., Liu, S., & Zheng, J. MEG3 activated by Vitamin D inhibits colorectal cancer cells proliferation and migration via regulating clusterin. EBioMedicine. 2018, 30, 148–57. [CrossRef]
- Suzuki, S., Shiraga, K., Sato, S., Punfa, W., Naiki-Ito, A., Yamashita, Y., Shirai, T., & Takahashi, S. Apocynin, an NADPH oxidase inhibitor, suppresses rat prostate carcinogenesis. Cancer Sci. 2013, 104(12), 1711–7. [CrossRef]
- Wang, X., Xie, J., Lu, X., Li, H., Wen, C., Huo, Z., Xie, J., Shi, M., Tang, X., Chen, H., Peng, C., Fang, Y., Deng, X., & Shen, B. Melit-tin inhibits tumor growth and decreases resistance to gemcitabine by downregulating cholesterol pathway gene CLU in pancreatic ductal adenocarcinoma. Cancer Lett. 2017, 399, 1–9.
- Deng, J., Peng, M., Zhou, S., Xiao, D., Hu, X., Xu, S., Wu, J., & Yang, X. Metformin targets Clusterin to control lipogenesis and inhibit the growth of bladder cancer cells through SREBP-1c/FASN axis. Signal Transduct Target Ther. 2021, 6(1), 98. [CrossRef]
- Xiong, J., Wang, S., Chen, T., Shu, X., Mo, X., Chang, G., Chen, J. J., Li, C., Luo, H., & Lee, J. D. Verteporfin blocks Clusterin which is required for survival of gastric cancer stem cell by modulating HSP90 function. Int J Biol Sci. 2019, 15(2), 312–24. [CrossRef]
- https://clinicaltrials.gov/study/NCT02412462?intr=clusterin&page=2&rank=11, accessed on January 10, 2024.
| Types of cancer | Expression of CLU in vitro | Expression of CLU in vivo |
|---|---|---|
| Non-small cell lung | Non-small cell lung cancer cell lines show overexpression upon treatment with chemotherapy or radiotherapy. ASO therapy sensitizes cells to these treatments and decreases their metastatic potential [112] | In patients with positive CLU expression there is a better overall disease-free survival than in negative patients [113]. |
| More than 80% of the tumors are inmunoreactive for clusterin [113]. | ||
| Gastric | Overexpression of sCLU correlates significantly with metastasis, tumor invasion and TNM stage. In addition, of with unfavorable survival for advanced-stage gastric cancers [114]. | |
| Ovarian | Overexpression of sCLU is inversely correlated with tumor apoptotic index and is more frequently detected in metastatic lesions than in primary tumors [115]. | |
| Increased sCLU expression is associated with increased biological aggressiveness and decreased survival [116]. | ||
| Endometrial | When clusterin is expressed in endometrial tumors, it is associated with a lower stage, supporting its role in the diagnosis of endometrial carcinoma [117]. | |
| There has been detected higher mRNA expression in both neoplastic and hyperplastic tissues compared to normal endometrium. In this regard, an increase in mRNA expression of the specific sCLU isoform has been observed in neoplastic and hyperplastic endometrial diseases, but an increase in CLU protein was not detected. Furthermore, specific CLU immunoreactivity has been observed in all glandular cells of the endometrium compared to other cellular compartments where CLU immunoreactivity was lower or absent [118]. | ||
| Increased CLU expression enhances paclitaxel resistance in endometrial cancer [119,120]. | ||
| Breast | Studies with the MDA-MB-231 cell line show how sCLU silencing significantly inhibits cell proliferation and drastically reduces cell invasion, cell progression and metastatic potential [121,122]. | Atypical hyperplasias, intraductal carcinomas, and invasive carcinomas are characterized by clusterin overexpression, unlike benign lesions [123]. |
| Overexpression of sCLU is observed in a higher percentage of triple-negative breast cancer [124] and is associated with a negative estrogen and progesterone receptor status [123]. | ||
| Likewise, overexpression in the stroma tends to directly correlate with resistance to preoperative neoadjuvant chemotherapy in the primary tumor and inversely with the apoptosis rate, indicating that gene expression may not be necessary for apoptotic cell death [123,125,126]. | ||
| Colon | sCLU is overexpressed, while nCLU is downregulated [127]. Similarly, sCLU overexpression was mainly shown in the cytoplasm of highly infiltrative tumors and metastatic lymph nodes [128], suggesting that clusterin expression could help identify patients with more aggressive tumors who may benefit from targeted therapies [129]. | |
| Bladder | Treatment with the antisense oligonucleotide (ASO) targeting negative regulation of Bcl-2 and clusterin increases the sensitivity of partially resistant bladder carcinoma cells to the tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) [130]. | The recurrence-free survival time of patients with overexpression of clusterin was shorter than that of patients with normal clusterin expression [131,132]. |
| Hepatocellular | High levels of sCLU are associated with migration, invasion, and metastasis [133] due to increased MMP-2 expression and decreased E-cadherin expression [134]. | |
| Furthermore, sCLU overexpression contributes to oxaliplatin resistance [135]. | ||
| In peripheral blood mononuclear cells (PBMC) from hepatocellular carcinoma patients, it has been proposed as a prospective detection biomarker along with other genes for its sensitivity and specificity [136]. The combination of CLU and AFP further improves diagnostic performance [137]. | ||
| The initial levels of clusterin are initially higher for patients with progressive disease than for those with partial or complete response, respectively [138]. | ||
| Pancreatic | The inducer of ferroptosis, a type of cell death characterized by the accumulation of reactive oxygen species (ROS), interferes with apoptotic cell death by regulating clusterin. [139]. | Clusterin expression in stages I and II is not significantly associated with apoptosis. Moreover, patients with positive clusterin expression present better survival rates [140]. |
| Melanomas | Overexpression is associated with increased drug resistance and prolonged survival of tumor cells, while silencing reduces resistance and reduced survival of melanoma cells both in vitro and in vivo [141]. | |
| Esophageal squamous cells | High CLU expression correlates with poor locoregional, overall, and distant progression-free survival. Moreover, patients with CLU overexpression in both epithelium and stroma have shorter survival times [142]. | |
| Head and neck | Overexpression of CLU has been observed, but its implications have not yet been determined [143]. | Although is detected in a low proportion of laryngeal carcinomas, it seems to exert a significant role in local invasiveness [144]. |
| Anaplastic large cell lymphomas | The role of CLU is unknown, but its expression within this lymphoma type provides an additional marker for diagnosis [145]. | |
| Clusterin expression is not related to anaplastic lymphoma kinase-1 (ALK-1) expression, and in reactive lymphoid tissues, only fibroblastic reticular cells and follicular dendritic cells show positive expression [145]. | ||
| Osteosarcoma | sCLU overexpression is associated with metastasis and chemotherapy resistance [146]. | |
| Prostate | The expression of CLU increases in advanced stages of cancer, and its suppression sensitizes cells to chemotherapeutic drugs [147]. | It has been observed that clusterin expression decreases considerably compared to benign tissues [147]. |
| Renal | The introduction of the CLU gene enhances the metastatic potential of renal cell cancer [148], while the removal of the CLU gene inhibits growth and migration [149]. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




