1. Introduction
BC is a prevalent illness, standing as one of the foremost health challenges globally. It is estimated that this neoplasia constitutes approximately 22.9% of cancers in women, emerging as one of the leading causes of cancer-related death in this population group [
1]. Moreover, BC stands out as the most prevalent type of cancer, with the highest mortality rates, reaching approximately 2.3 million cases in 2020 [
2]. The molecular categorization of BC is based on the presence of four clinically standardized biomarkers: estrogen (ER) and progesterone (PR) hormone receptors, epidermal growth factor receptor 2 (HER2), and the cell proliferation marker Ki67. These biomarkers allow the classification of this neoplasm into at least four subgroups based on their presence or absence [
3,
4], including: luminal A and luminal B, HER2 enriched and basal like. Each subgroup carries a different prognosis [
5].
Luminal B tumors, accounting for 15%-20% of BC cases. They display a more aggressive phenotype, elevated histological grade, higher proliferative index, and an unfavorable prognosis [
6,
7]. This subtype exhibits an increased rate of recurrence and reduced survival rates following relapse in comparison to the luminal A subtype [
8]. According to the 2013 St. Gallen Consensus [
9], the luminal B BC subtype can be further classified into luminal B-like HER2 negative (HER2-) and luminal B-like HER2 positive (HER2+). Luminal B-like HER2- is characterized by its positivity for ER, negativity for HER2, and the presence of at least one of the following features: high Ki67 expression and negativity, or low expression of PR. Conversely, the luminal B-like HER2+ is characterized by its positivity for ER, overexpression or amplification of HER2, with any level of Ki67, and any PR expression. Therefore, understanding the pattern of recurrence and clinical outcomes of the luminal B BC subtype is crucial. Although technological advances have led to a greater understanding of luminal B BC as a heterogeneous disease, present immunohistochemical, clinicopathological, and molecular markers, continue to leave a significant portion of patients to the possibility of either, excessive or insufficient treatment. Thus, the identification and standardization of new easily accessible prognostic and predictive markers is imperative. These markers could provide additional information to improve the stratification of cancer risk, predict clinical outcomes, and guide future therapeutic strategies for luminal B BC patients. A promising prognostic and predictive marker is CIN, a prevalent characteristic in solid tumors. Given that BC is characterized by unstable karyotypes and the fact that disease outcome and therapy response may depend on such instability, defining the level of CIN and CH, could carry significant implications for stratification of risk and the development of future therapeutic strategies in BC.
CIN, is recognized as a distinctive characteristic of cancer [
10], where the loss or gain of complete chromosomes (aneuploidy) or chromosomal fragments is characteristic [
11]. Aneuploidy can be stable or unstable. Stable aneuploidy is characterized by the presence of the same type of numerical alterations in the majority of cells. Conversely, unstable aneuploidy is characterized by presenting cell-to-cell variability in the number of chromosomes, and is therefore a source of karyotypic heterogeneity [
12]. In fact, unstable aneuploidy promotes the simultaneous growth of diverse tumor subpopulations, promoting both inter- and intratumoral genomic heterogeneity [
11,
13]. CIN promotes intratumoral heterogeneity, allowing cancer cells to adapt to environmental stress. At the same time, it promotes the development of more aggressive cancer cells, thus contributing to treatment resistance [
14,
15]. The significance of CIN and CH in therapy response lies in their capacity to trigger gene regulatory interactions and alter protein concentrations. Both these factors, have the potential to influence cell responses to drug treatments [
16]. In this context, it has been proposed that chromosomal alterations in individual cancer cells, may give rise to diverse drug sensitivities, thereby fostering the survival of a subset of the tumor cell population [
17]. Another fact that remains unknown is whether CIN in luminal B BC tumors, above a specific threshold, could have a detrimental effect on the growth of human tumors, or whether low or intermediate CIN levels could be associated with a more favorable prognosis for luminal B BC patients compared to elevated levels. Considering the above, the objective of this study was to assess CIN and CH in tumor tissue samples from ten patients with luminal B BC, and compare them with established clinicopathological parameters. Evaluating CIN and CH in luminal B BC could improve cancer risk stratification, the prediction of clinical outcomes, and future therapeutic approaches.
2. Results
2.1. Patients and Clinicopathological Data
Clinical and pathological characteristics of the patients are described in
Table 1. All cases were free of metastasis at the time of diagnosis. Four cases (40%) were ER+/PR+/HER2-, 3 (30%) were ER+/PR-/HER2-, and 3 (30%) were ER+/PR+/HER2+.
2.2. CIN and CH Levels
Based on the CIN level (% CIN), each patient was categorized as having low CIN (CIN = 0-25%), intermediate CIN (CIN = 26%-50%), high CIN (CIN = 51%-70%), or extreme CIN (CIN>70%) [
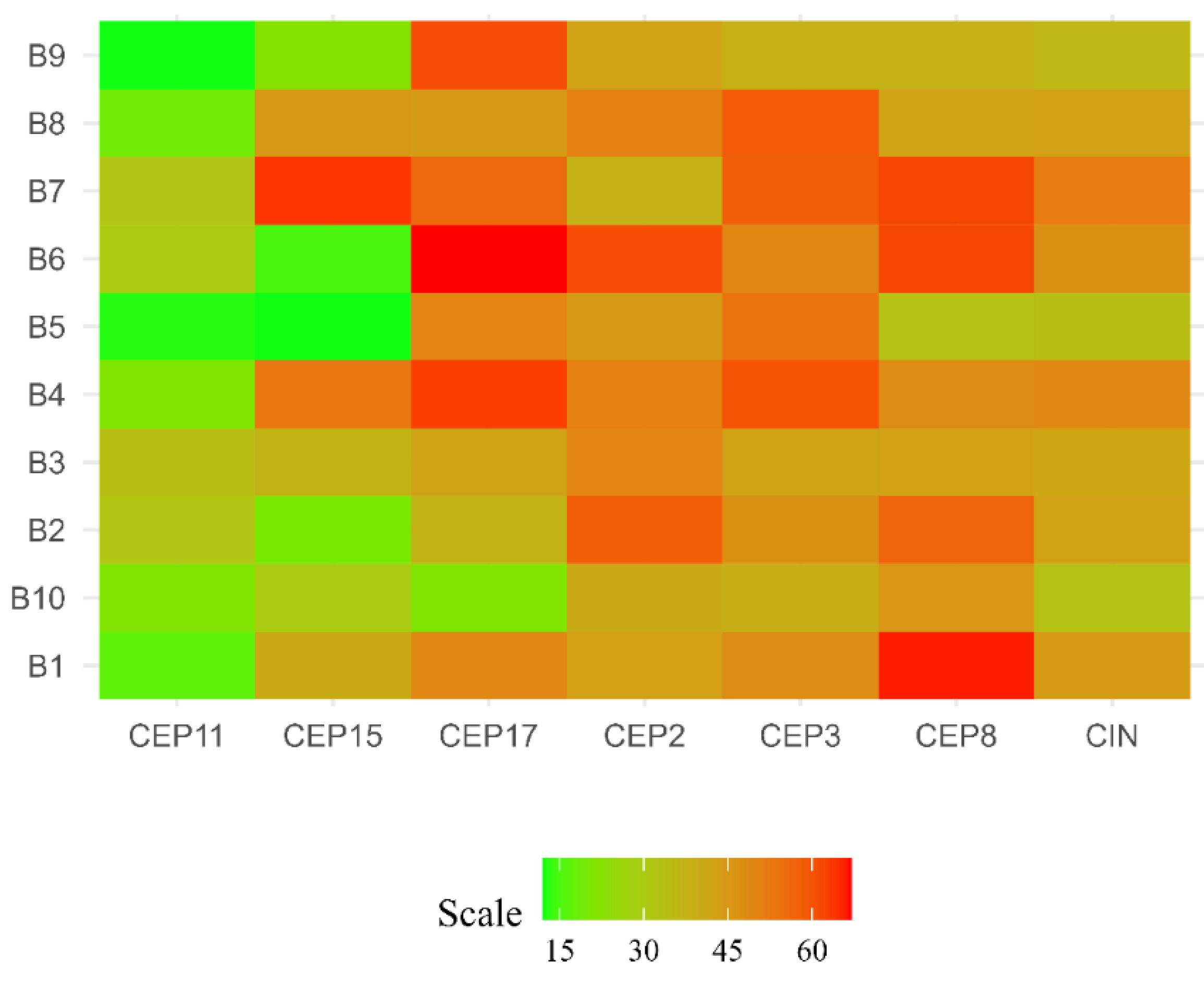
18]. The findings of this study reveal that most patients (90%), presented intermediate CIN, with values ranging between 33% and 49%. While only 1 (10%) patient (ER+/PR+/HER2+) presented high CIN (52%) (
Figure 1 and
Figure 2, and
Supplementary Table S1).
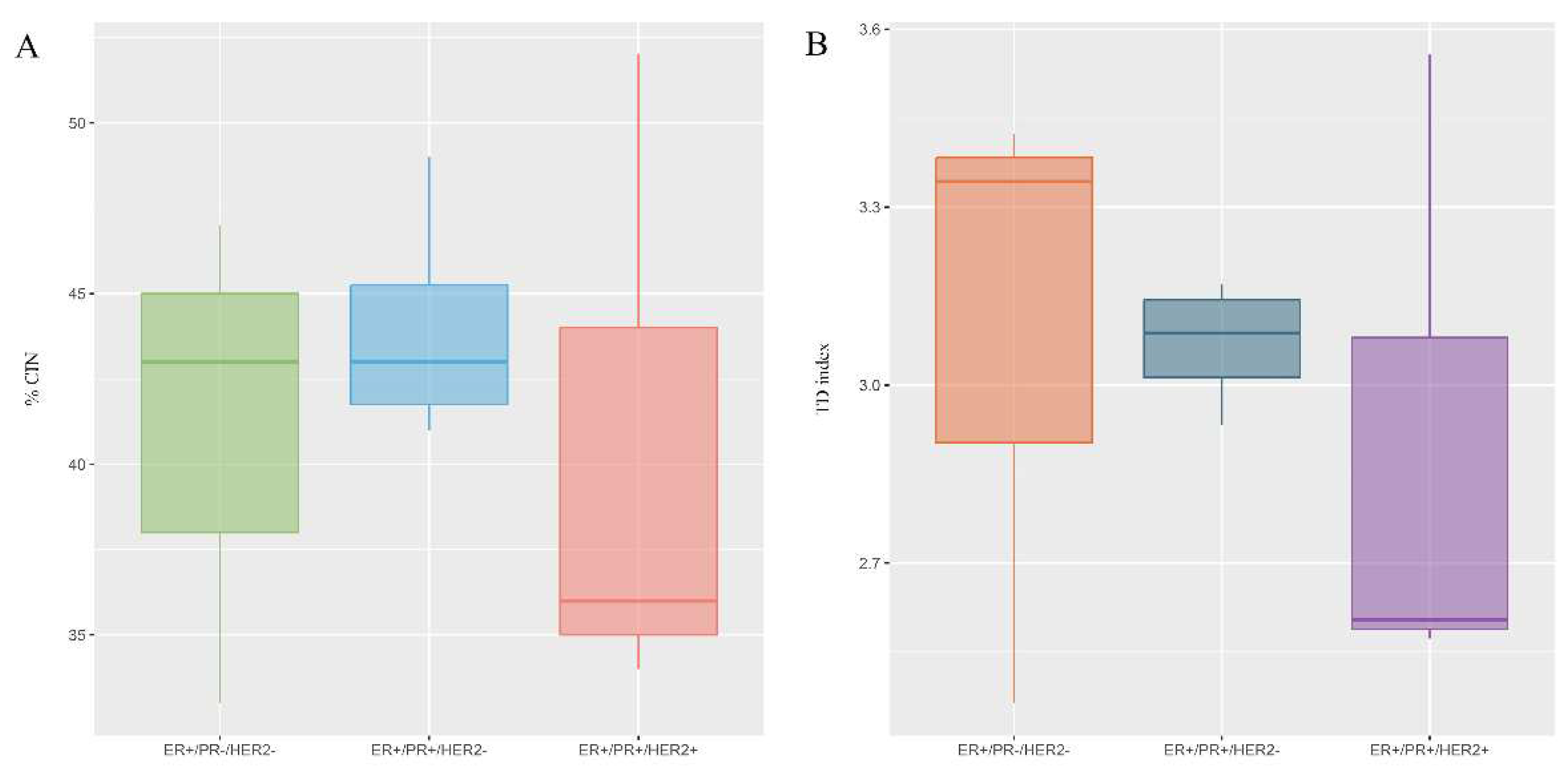
Once the possible existence of variations in the level of CIN according to PR and HER2 status was determined, no important variations were observed. However, the highest CIN ranges occurred in ER+/PR+/HER2- patients (
Figure 3A and Supplementary
Table 1). Notably, lymphovascular invasion appeared to be significant in patients with intermediate CIN.
All patients (100%) exhibited elevated CH, with values ranging between 2.5 and 3.4. There were no variations in the level of CH according to PR and HER2 status (
Figure 3B and Supplementary
Table 1).
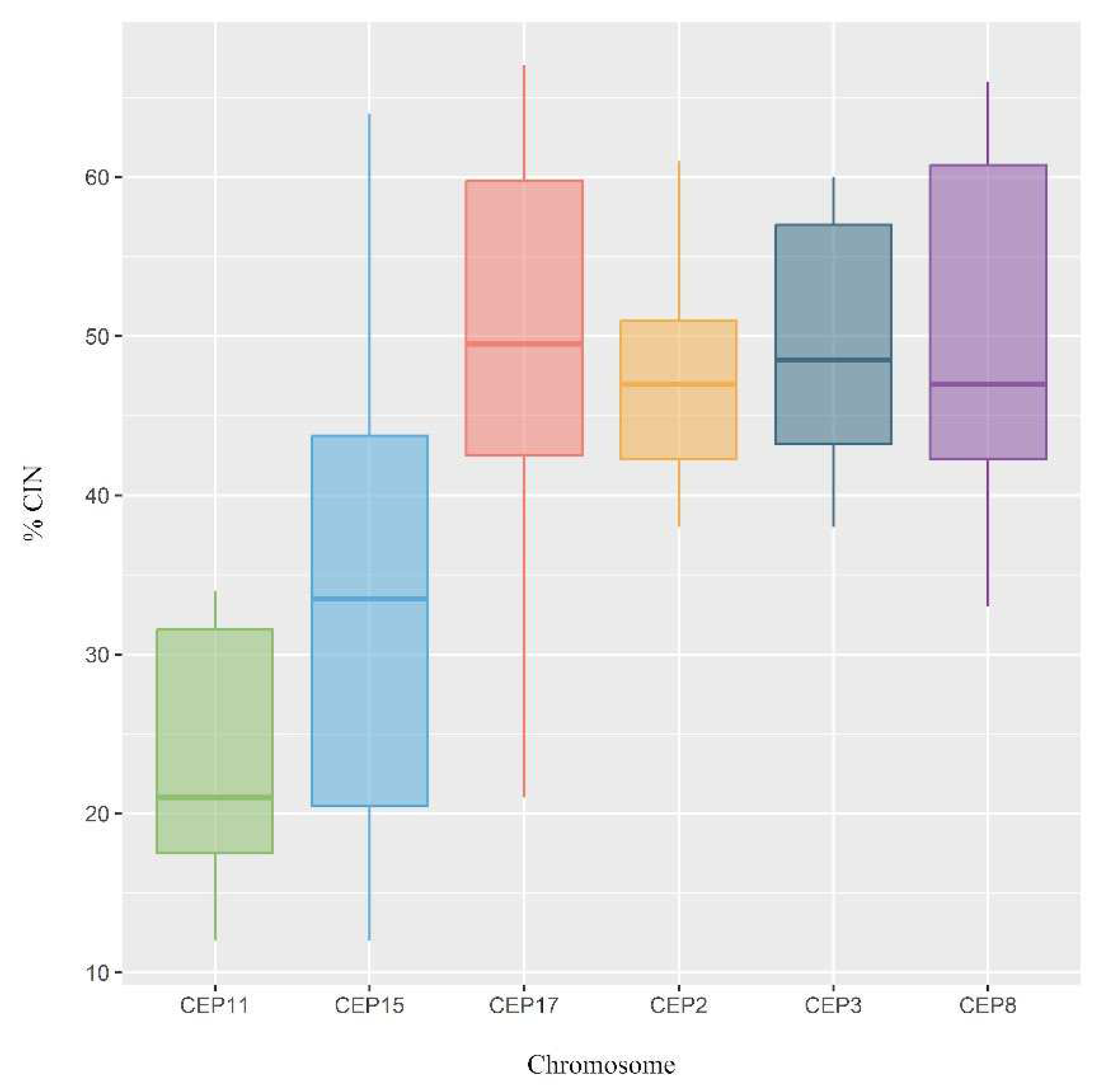
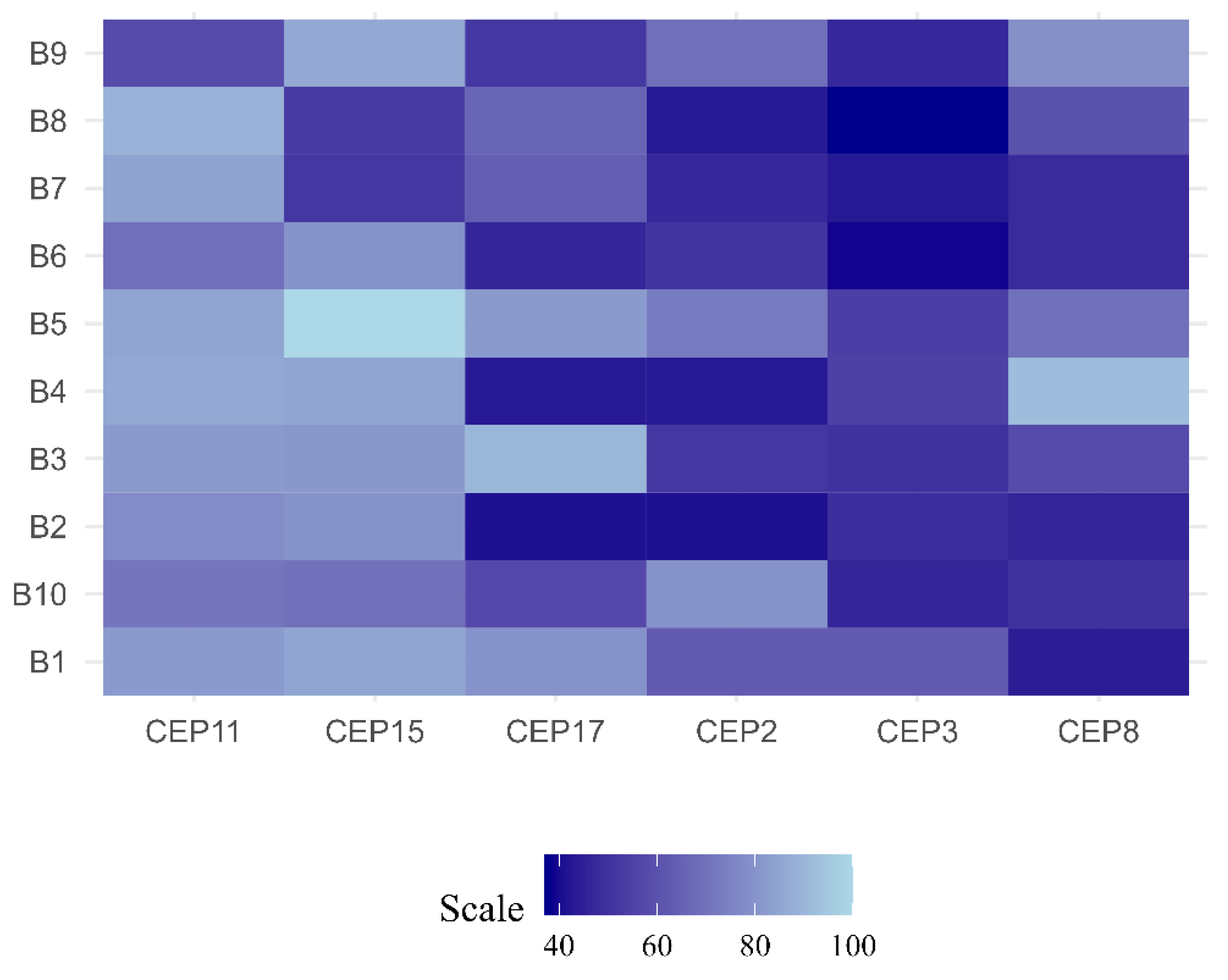
The CIN level for each chromosome was also determined. The results of this study highlight that the most stable chromosomes were chromosomes 11 (CEP11) and 15 (CEP15), while the least stable chromosomes were chromosomes 8 (CEP8) (CIN=50%), 3 (CEP3) (CIN=49%), and 17 (CEP17) (CIN=49%) (
Figure 4).
2.3. CEP Copy Number Variations (CNVs)
CNVs (gains and losses) for CEP2, CEP3, CEP8, CEP11, CEP15, and CEP17 were evaluated in all cases. Conforming to the criteria previously established in defining chromosomal gains and losses, a chromosome was deemed to exhibit gains when the mean count of centromeric signals was equal to or greater than 3 (CEP≥3), and losses, when the mean count of centromeric signals was less than 1.6 (CEP<1.6) [
19].
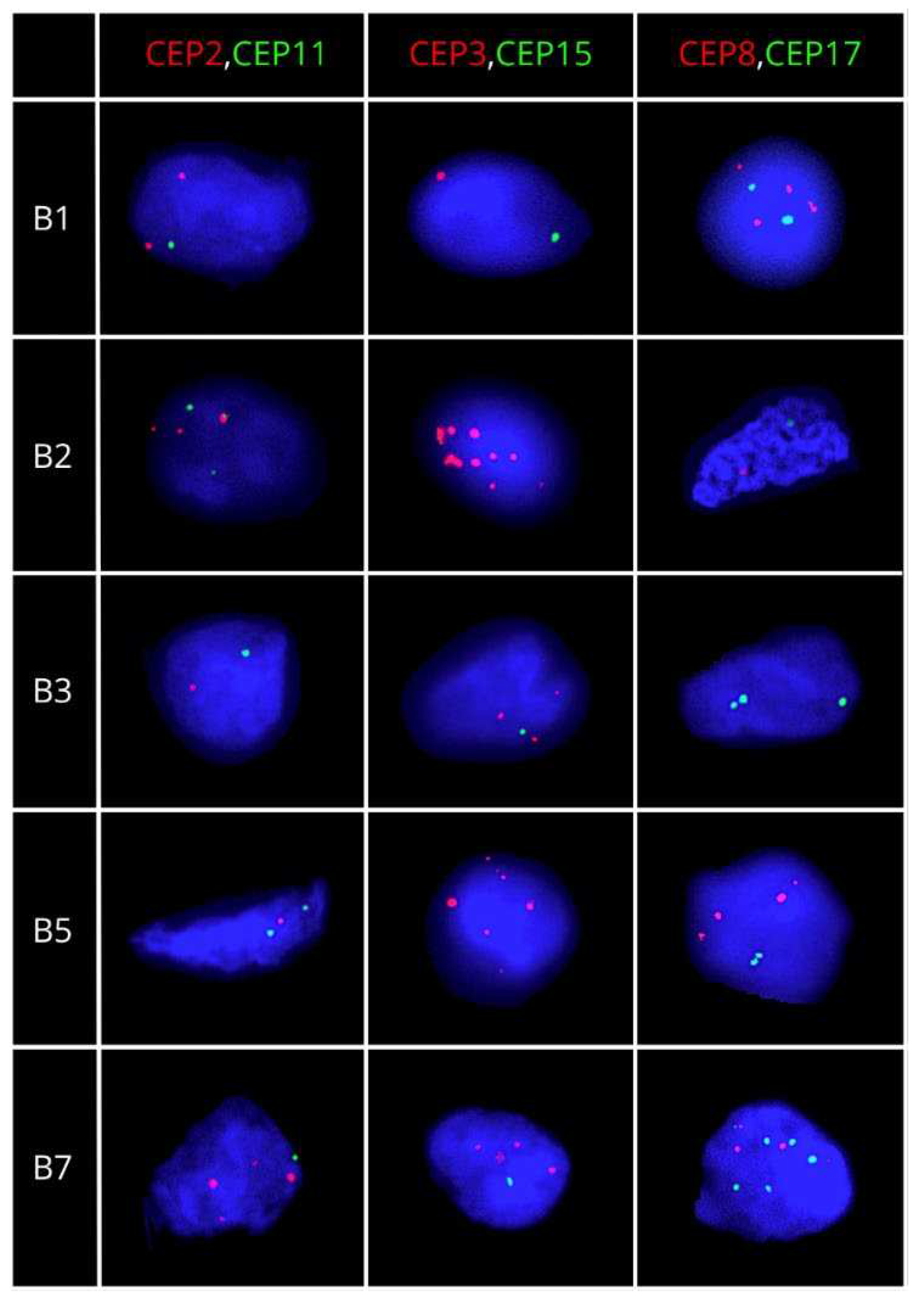
Copy number gain was observed only for CEP17 in 1 (10%) case (ER+/PR+/HER2-) (
Supplementary Table S2). While copy number losses for CEP2, CEP3, CEP8, CEP11, CEP15, and CEP17 were observed in 7 (70%), 6 (60%), 9 (90%), 10 (100%), 9 (90%), and 7 (70%) cases, respectively (
Figure 2). These results show that losses were more frequent than gains.
2.4. Determination of Stable and Unstable Aneuploidy
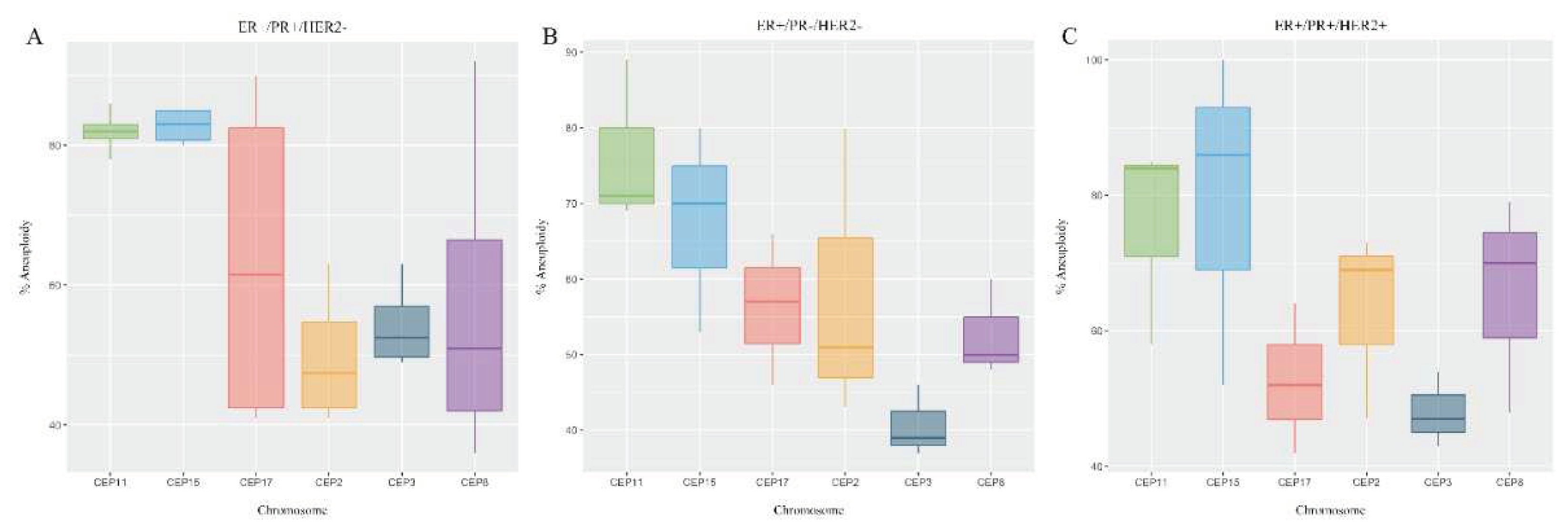
Stable or unstable aneuploidy was determined for each chromosome and for each BC patient according to PR and HER2 status. The chromosomes with the most stable aneuploidy were chromosomes 11 (CEP11) and 15 (CEP15), while the chromosomes with the least stable aneuploidy were chromosomes 2 (CEP2), 3 (CEP3), 8 (CEP8), and 17 (CEP17) (
Figure 5).
Regarding the assessment of aneuploidy stability in luminal B BC patients, it was observed that all patients, irrespective of PR and HER2 status (ER+/PR+/HER2-, ER+/PR-/HER2- and ER+/PR+/HER2+), exhibited stable aneuploidy. This stability was characterized by stability in the number of copies of chromosomes 11 and 15. Among the chromosomes exhibiting less stable aneuploidy were, chromosome 2 for ER+/PR+/HER2- patients, and chromosome 3 for ER+/PR-/HER2- and ER+/PR+/HER2+ patients (
Figure 6).
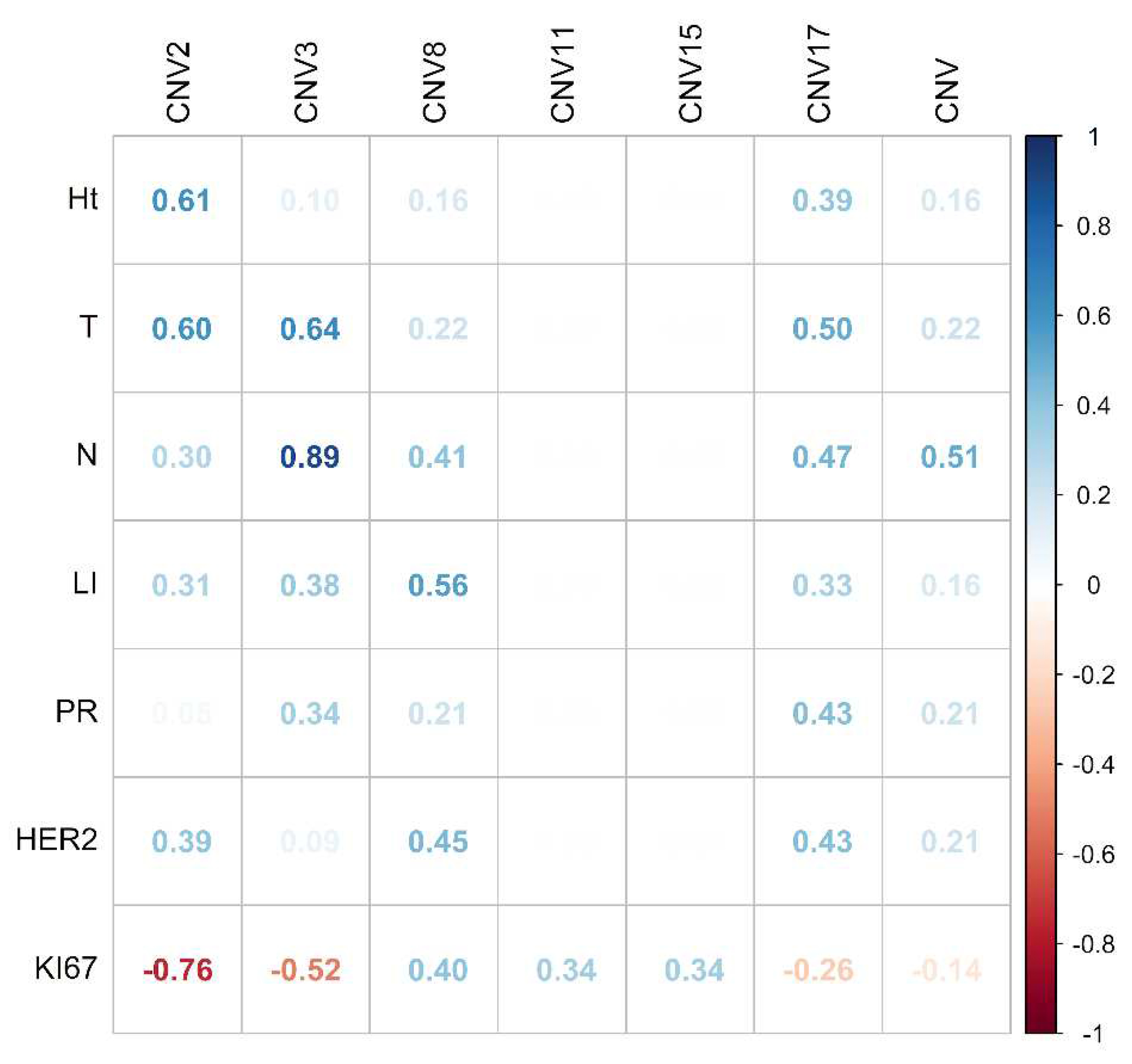
2.5. Association between CEP Copy Number Variations and CH, with Clinicopathological Parameters
To assess the associations between CNVs per chromosome and clinicopathological characteristics, a multivariate analysis with Pearson correlation coefficient was performed. A positive correlation was found between CNVs of chromosome 2 with T stage (0.60), between CNVs of chromosome 3 with N stage (0.89), and between CNVs of chromosome 8 with lymphovascular invasion (0.56) (
Figure 7). No correlations were found between CNVs of chromosomes 2, 3, 8, 11, 15, and 17, with PR, HER2, and Ki67, nor among CH with any of the clinicopathological characteristics studied (Ht, T, N, LI, PR, HER2, and Ki67) (
Supplementary Figure S1).
3. Discussion
The clinical outcome and therapeutic decision regarding luminal B BC patients are mainly based on clinicopathological parameters. Specifically, tumor size, histologic grade, histological type, immunohistochemical results of prognostic factors, and lymph node status play an important role in cancer risk stratification. However, despite the success of this approach, there is still a risk of over- or under-treating certain patients. The above underscores the need to conduct cancer risk stratification by integrating clinicopathological parameters with enhanced insights into molecular-level alterations. This integration could improve the prediction of clinical outcomes and inform future therapeutic strategies for luminal B BC patients. Given that CIN is a defining characteristic of BC and that risk stratification and prognosis definition may depend on this instability, defining the level of CIN and CH, could have significant implications for risk stratification and the development of future therapeutic strategies in BC. The above, in turn, could facilitate the optimization of BC diagnosis and prognosis.
The results of this study reveal that luminal B BC patients exhibit intermediate CIN and stable aneuploidy, with chromosomal losses being more frequent than gains. CIN, CH, and aneuploidy represent distinct and crucial characteristics of tumor cell populations, contributing to tumor evolution with significant implications for prognosis and therapy response. In fact, statistically significant correlations were observed between moderate CIN and lymphovascular invasion.
The findings of this study are in line with previous research, which suggests that ER+ tumors exhibit the lowest average CIN70 score [
18]. CIN70 is a method used to determine the level of CIN from the expression of 70 specific genes consistently associated with aneuploidy in populations of tumor samples [
20]. However, this method evaluates the level of CIN from a pool of cells, rather than assessing CIN cell by cell, as was done in this study using FISH with 6 centromeric probes.
Aneuploidy, potentially induced by CIN [
21], is among the most prevalent abnormalities in cancer. Therefore, identifying chromosomes associated with CIN may potentially improve risk stratification and optimize outcome prediction. In this regard, we found in luminal B BC patients, that chromosomes 11 and 15 exhibit the most stable aneuploidy, while the chromosomes 2, 3, and 8, were the least stable. These results are significant, as they suggest that determining the state of aneuploidy (stable or unstable) could enable the prediction of clinical outcomes in BC patients. Indeed, it has been indicated that individuals with genetically stable tumors exhibit a more favorable disease outcome compared to those with unstable tumors [
21]. In this sense, our results suggest that intermediate CIN could be associated with clinical characteristics of intermediate prognosis in luminal B BC patients. This is supported by the statistically significant correlation observed between stable aneuploidy (losses) of chromosomes 2, 3, and 8 with the T stage (T1 and T2), the N stage (N1 and N2), and with lymphovascular invasion, respectively.
CNVs were identified in all evaluated chromosomes, with losses being more frequent than gains. For instance, the gain of chromosome 17 (CEP17) was observed in only 1 patient (ER+/PR+/HER2-). This finding aligns with prior research suggesting that, among the associated copy number alterations, the gain of chromosome 17 is a characteristic feature of luminal B BC [
22]. Even though, copy number gain in CEP17 has been linked to adverse clinical outcomes [
19,
23,
24] and the response to chemotherapy with anthracyclines in BC patients [
25,
26], the relevance of a copy number gain in CEP17 remains unclear. The losses observed across all analyzed chromosomes are noteworthy, particularly due to the presence of tumor suppressor genes (TSGs) known for their pivotal roles in monitoring and repairing double-strand breaks (DSBs) and maintaining genome stability (
Table 2). In fact, CNVs in these genes have been associated with an increased risk of genomic instability and cancer development [
27,
28].
Notably, losses of chromosome 8 were observed in 90% of luminal B BC patients, which showed a statistically significant correlation with lymphovascular invasion. These results suggest that CEP8 copy number loss (indicative of CIN) could be a predictor for poor prognosis in luminal B BC patients. Indeed, some studies have shown that 8p loss is closely linked to a subset of breast cancers characterized by high aggressiveness and genetic instability, attributing to this chromosome a possible role in the regulation of genomic stability [
27]. The observed statistically significant correlation between losses in chromosome 8 and unfavorable tumor phenotype characteristics, suggests that this chromosome harbors one or more genes that are crucial to maintaining genome stability. Consequently, alterations in chromosome 8 could potentially contribute to the development of more aggressive cancer phenotypes and alterations in the response to therapy. Indeed, a recent study suggested that sub-clonal CNAs favor positive selection of oncogenes and negative selection of tumor suppressor genes (TSG) [
28]. Indeed, several candidate TSGs in BC located on chromosome 8p, have been identified (
Table 2).
The identification of CIN and losses on chromosome 8 (losses associated with lymphovascular invasion) could serve as a pivotal pathway for the development of novel therapeutic strategies. Validation of these findings in a larger cohort of samples could provide crucial insights into targeted therapeutic approaches for improved BC management. Further, understanding the specific genes residing in chromosome 8 and their roles in maintaining genome stability can unravel potential targets for precision therapies.
A limitation to this study involved restricted access to samples. However, these ten patients represent a subset of the tumoral subtype within the BC population, providing valuable insights into the role of CIN and CH in Luminal B BC. Furthermore, the results of this pilot study serve as a basis for future research with larger cohorts, enabling the validation of the findings, and the development of future therapeutic strategies in BC. Other factors contributing to the limited sample size include, firstly, negative responses from some patients who refused to participate in the study. Secondly, in Colombia, where the study was undertaken, gaining access to tumor samples is challenging, as laws allowing such access for research purposes are still in the early stages of consideration.
4. Materials and Methods
4.1. Patients and Clinicopathological Data
Archival Formalin-Fixed Paraffin-Embedded (FFPE) tumor tissue was obtained from ten (10) luminal B BC patients diagnosed at Hospital Universitario Mayor - Méderi, Bogotá, Colombia, between 2000 and 2018. Sections of these primary tumor tissues were selected from representative tumor areas by an expert pathologist. Clinicopathological data was obtained from medical records and sections stained with hematoxylin and eosin. Data on the primary tumor included: age, the breast affected by cancer (right or left), histologic subtype (Ht), T stage, N stage, lymphovascular invasion, HER2 status, progesterone, and estrogen receptor status, Ki67 index, and luminal B types. The main inclusion criteria encompassed individuals diagnosed with luminal B BC between 2000 and 2018, treated at the Hospital Universitario Mayor - Méderi for minimum of five (5) years, undergoing hormonal therapy and/or chemotherapy, with and without relapse. Exclusion criteria comprised individuals who have received neo-adjuvant or adjuvant therapy (chemotherapy, radiotherapy, hormonal therapy) prior to sample collection and those with a current diagnosis of other types of cancer. The research received approval from the Research Ethics Committee at Universidad del Rosario in Bogotá, Colombia. Informed consent was obtained from all individual participants included in the study.
4.2. Dual Color Fluorescence in Situ Hybridization (FISH) Assays
Dual color FISH assays were carried out on FFPE tissue sections of 4 μm, by using centromeric probes (CEP) for chromosomes 2, 3, 8, 11, 15, and 17 (Cytocell. Cytocell Ltd, Cambridge, UK). CEP for chromosomes 2, 3, and 8 (CEP2, CEP3, and CEP8) were labeled with spectrum orange, while CEP for chromosomes 11, 15, and 17 (CEP 11, CEP15, and CEP17) were labeled with spectrum green. Three different dual color FISH assays were performed using the following combination of probes: CEP2 and CEP11, CEP3 and CEP15, and CEP8 and CEP17. Ten randomly selected areas of the FFPE tissues slides were selected and captured using an Olympus microscope with Cytovision System 7.4 cytogenetic software (Leica Biosystems Richmond, Inc). Chromosomes 2 and 15 were chosen because alterations in their copy numbers are infrequent in BC [
40]. While chromosomes 3, 8, 11, and 17 were selected because they commonly undergo alterations in BC [
41].
4.3. Evaluation of CIN and CH
One hundred non-overlapping nuclei were examined for each chromosome and for each patient. CIN was established in accordance with the method specified by Lengauer et al (1997) [
42]. Briefly, the CIN level for each patient was determined as follows: first, for each individual chromosome, the percentage of nuclei with a number of centromeric signals (CEP) different from the most frequent number of signals in the tumor cell population (modal number) was calculated. After establishing the CIN level (% CIN) for each individual chromosome, the mean CIN level was computed for the six analyzed chromosomes [
42,
43]. According to the CIN level (% CIN), each patient was classified as having low CIN (CIN=0-25%), intermediate CIN (CIN=26%-50%), high CIN (CIN=51%-70%), or extreme CIN (CIN>70%) [
18].
CH was determined by calculating the true diversity index (TD) using order 1 (q=1), which integrates the Shannon index and is represented as follows: NEE =e^H, where NEE corresponds to the effective number of species, e is equal to Euler or Napier's constant and H is the Shannon index. Shannon index combines both, the quantity and prevalence of cell clones within each patient, adhering to established methods described in previous publications [
40,
44]. According to the CH level, each patient was classified as having low CH (CH<1.5), intermediate CH (CH>1.5 and <2) and high CH (CH>2).
4.4. Evaluation of CEP Copy Number Variations (CNVs)
For each of the six analyzed chromosomes (2, 3, 8, 11, 15, and 17), the centromeric signal (CEP probe) count was determined in 100 non-overlapping tumor nuclei. Subsequently, the mean CEP signal was calculated for each of the six chromosomes individually. Based on the mean of CEP signals, each chromosome was classified as having gains if the mean CEP signal count was ≥3 [
19], or losses if the mean CEP signal count was <1,6 [
45].
4.5. Determination of Stable and Unstable Aneuploidy
Given that CIN can classify stable aneuploid tumor cells (populations of tumor cells in which almost all cells have the same chromosome number), along with unstable aneuploid tumor cells (populations of tumor cells in which most cells have varying numbers of chromosomes) [
40], we decided to ascertain whether the type of aneuploidy present in each chromosome was stable or unstable. Stable or unstable aneuploidy was also determined for each BC patient according to PR and HER2 status (ER+/PR+/HER2-, ER+/PR-/HER2-, and ER+/PR+/HER2+). Stable or unstable aneuploidy, was calculated by assessing the proportion of cells with identical probe signal patterns. A chromosome and a BC patient were considered to exhibit stable aneuploidy if more than 20% (≥20%) of the cells showed identical probe signal patterns, while a BC patient or chromosome with less than 20% (<20%) of the cells showing identical probe signal patterns, was classified as having unstable aneuploidy [
46].
4.6. Data Analysis
Descriptive statistics were used to assess the distribution and frequency of clinicopathological variables, CIN, and CH, in patients with luminal B BC. The normality of the data was evaluated using the Shapiro Wilk test. Correlations between CIN and CH levels with clinicopathological variables were established by using the Pearson test for normally distributed data, and Spearman and Kruskal-Wallis tests for non-parametric data. To establish associations between CIN and CH with categorical clinicopathological variables, contingency tables, and measures of association such as Cramer's contingency coefficient were performed. Subsequently, to evaluate the existence of statistically significant differences between luminal B BC patients according to PR and HER2 status (ER+/PR+/HER2-, ER+/PR+/HER2+, ER+/PR-/HER2-), a test of difference between parametric and non-parametric means was performed using analysis of variance (ANOVA). Finally, in order to evaluate the association between CNVs per chromosome with clinicopathological variables, a multivariate analysis was performed using the Pearson correlation coefficient. All statistical analyses were performed using the R Studio version 4.0.2. P-values of less than 0.05 (p<0,05) were considered statistically significant.
5. Conclusions
The results of this pilot study reveal that luminal B BC patients exhibit intermediate CIN and stable aneuploidy, both of which correlated with lymphovascular invasion. The evaluation of CIN and CH levels holds potential value for validation with a larger cohort of patients and for their potential inclusion as prognostic or predictive biomarkers in luminal B BC. Despite the limited number of samples used, this study provides valuable contributions to the field of breast cancer research, as well as valuable preliminary data that lays the foundation for future research in this area.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Figure S1: Multivariate analysis with Pearson correlation coefficient between clonal heterogeneity (CH) and clinicopathologic characteristics; Table S1: Level of Chromosomal instability (CIN), Clonal Heterogeneity (True Diversity Index) and Aneuploidy observed in luminal B BC patients; Table S2: CEP copy number variation (gains and losses) observed in luminal B BC patients.
Author Contributions
Conceptualization, Nelson Rangel and Milena Rondón-Lagos; Data curation, Laura Camargo-Herrera, Giovanny Castellanos, Nelson Rangel and Milena Rondón-Lagos; Formal analysis, Laura Camargo-Herrera, Giovanny Castellanos, Nelson Rangel and Milena Rondón-Lagos; Funding acquisition, María Martínez-Agüero and Milena Rondón-Lagos; Investigation, Laura Camargo-Herrera, Giovanny Castellanos, Nelson Rangel, Guillermo Jiménez-Tobón and Milena Rondón-Lagos; Methodology, Laura Camargo-Herrera, Giovanny Castellanos, Guillermo Jiménez-Tobón, María Martínez-Agüero and Milena Rondón-Lagos; Project administration, María Martínez-Agüero; Resources, María Martínez-Agüero and Milena Rondón-Lagos; Software, Laura Camargo-Herrera, Giovanny Castellanos, Nelson Rangel and Milena Rondón-Lagos; Supervision, Nelson Rangel and Milena Rondón-Lagos; Validation, Laura Camargo-Herrera, Giovanny Castellanos, Nelson Rangel and Milena Rondón-Lagos; Visualization, Laura Camargo-Herrera, Giovanny Castellanos, Nelson Rangel and Milena Rondón-Lagos; Writing – original draft, Nelson Rangel and Milena Rondón-Lagos; Writing – review & editing, Laura Camargo-Herrera, Giovanny Castellanos, Nelson Rangel, Guillermo Jiménez-Tobón, María Martínez-Agüero and Milena Rondón-Lagos.
Funding
This research was funded by Hospital Universitario Mayor - Méderi, Bogotá, Colombia.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Research Ethics Committee of the Universidad del Rosario (protocol code DVO005 2019-CV1320. Date of approval August 5, 2022), for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Acknowledgments
We thank the patients who agreed to participate in this study as well as their families. Also, we thank the Méderi research team, who supported us during the development of the research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Mehrgou, A.; Akouchekian, M. The Importance of BRCA1 and BRCA2 Genes Mutations in Breast Cancer Development. Med J Islam Repub Iran 2016, 30, 369.
- Sung, H.; Ferlay, J.; Siegel, R. L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021, 71 (3), 209–249. [CrossRef]
- Haibe-Kains, B.; Desmedt, C.; Loi, S.; Culhane, A. C.; Bontempi, G.; Quackenbush, J.; Sotiriou, C. A Three-Gene Model to Robustly Identify Breast Cancer Molecular Subtypes. JNCI: Journal of the National Cancer Institute 2012, 104 (4), 311–325. [CrossRef]
- Harbeck, N.; Penault-Llorca, F.; Cortes, J.; Gnant, M.; Houssami, N.; Poortmans, P.; Ruddy, K.; Tsang, J.; Cardoso, F. Breast Cancer. Nat Rev Dis Primers 2019, 5 (1), 66. [CrossRef]
- Sørlie, T.; Tibshirani, R.; Parker, J.; Hastie, T.; Marron, J. S.; Nobel, A.; Deng, S.; Johnsen, H.; Pesich, R.; Geisler, S.; Demeter, J.; Perou, C. M.; Lønning, P. E.; Brown, P. O.; Børresen-Dale, A.-L.; Botstein, D. Repeated Observation of Breast Tumor Subtypes in Independent Gene Expression Data Sets. Proceedings of the National Academy of Sciences 2003, 100 (14), 8418–8423. [CrossRef]
- Tran, B.; Bedard, P. L. Luminal-B Breast Cancer and Novel Therapeutic Targets. Breast Cancer Research 2011, 13 (6), 221. [CrossRef]
- Creighton, C. The Molecular Profile of Luminal B Breast Cancer. Biologics 2012, 289. [CrossRef]
- Ellis, M. J.; Tao, Y.; Luo, J.; A’Hern, R.; Evans, D. B.; Bhatnagar, A. S.; Chaudri Ross, H. A.; von Kameke, A.; Miller, W. R.; Smith, I.; Eiermann, W.; Dowsett, M. Outcome Prediction for Estrogen Receptor-Positive Breast Cancer Based on Postneoadjuvant Endocrine Therapy Tumor Characteristics. JNCI Journal of the National Cancer Institute 2008, 100 (19), 1380–1388. [CrossRef]
- Goldhirsch, A.; Winer, E. P.; Coates, A. S.; Gelber, R. D.; Piccart-Gebhart, M.; Thürlimann, B.; Senn, H.-J.; Albain, K. S.; André, F.; Bergh, J.; Bonnefoi, H.; Bretel-Morales, D.; Burstein, H.; Cardoso, F.; Castiglione-Gertsch, M.; Coates, A. S.; Colleoni, M.; Costa, A.; Curigliano, G.; Davidson, N. E.; Di Leo, A.; Ejlertsen, B.; Forbes, J. F.; Gelber, R. D.; Gnant, M.; Goldhirsch, A.; Goodwin, P.; Goss, P. E.; Harris, J. R.; Hayes, D. F.; Hudis, C. A.; Ingle, J. N.; Jassem, J.; Jiang, Z.; Karlsson, P.; Loibl, S.; Morrow, M.; Namer, M.; Kent Osborne, C.; Partridge, A. H.; Penault-Llorca, F.; Perou, C. M.; Piccart-Gebhart, M. J.; Pritchard, K. I.; Rutgers, E. J. T.; Sedlmayer, F.; Semiglazov, V.; Shao, Z.-M.; Smith, I.; Thürlimann, B.; Toi, M.; Tutt, A.; Untch, M.; Viale, G.; Watanabe, T.; Wilcken, N.; Winer, E. P.; Wood, W. C. Personalizing the Treatment of Women with Early Breast Cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Annals of Oncology 2013, 24 (9), 2206–2223. [CrossRef]
- Pikor, L.; Thu, K.; Vucic, E.; Lam, W. The Detection and Implication of Genome Instability in Cancer. Cancer and Metastasis Reviews 2013, 32 (3–4), 341–352. [CrossRef]
- Tanaka, K.; Hirota, T. Chromosomal Instability: A Common Feature and a Therapeutic Target of Cancer. Biochimica et Biophysica Acta (BBA) - Reviews on Cancer 2016, 1866 (1), 64–75. [CrossRef]
- Geigl, J. B.; Obenauf, A. C.; Schwarzbraun, T.; Speicher, M. R. Defining ‘Chromosomal Instability.’ Trends in Genetics 2008, 24 (2), 64–69. [CrossRef]
- Gagos, S.; Irminger-Finger, I. Chromosome Instability in Neoplasia: Chaotic Roots to Continuous Growth. Int J Biochem Cell Biol 2005, 37 (5), 1014–1033. [CrossRef]
- Negrini, S.; Gorgoulis, V. G.; Halazonetis, T. D. Genomic Instability — an Evolving Hallmark of Cancer. Nat Rev Mol Cell Biol 2010, 11 (3), 220–228. [CrossRef]
- Kalimutho, M.; Nones, K.; Srihari, S.; Duijf, P. H. G.; Waddell, N.; Khanna, K. K. Patterns of Genomic Instability in Breast Cancer. Trends Pharmacol Sci 2019, 40 (3), 198–211. [CrossRef]
- Dayal, J. H. S.; Albergante, L.; Newman, T. J.; South, A. P. Quantitation of Multiclonality in Control and Drug-Treated Tumour Populations Using High-Throughput Analysis of Karyotypic Heterogeneity. Converg Sci Phys Oncol 2015, 1 (2), 025001. [CrossRef]
- 17. Fedorenko, I. V.; Wargo, J. A.; Flaherty, K. T.; Messina, J. L.; Smalley, K. S. M. BRAF Inhibition Generates a Host–Tumor Niche That Mediates Therapeutic Escape. Journal of Investigative Dermatology 2015, 135 (12), 3115–3124. [CrossRef]
- Birkbak, N. J.; Eklund, A. C.; Li, Q.; McClelland, S. E.; Endesfelder, D.; Tan, P.; Tan, I. B.; Richardson, A. L.; Szallasi, Z.; Swanton, C. Paradoxical Relationship between Chromosomal Instability and Survival Outcome in Cancer. Cancer Res 2011, 71 (10), 3447–3452. [CrossRef]
- Lee, K.; Jang, M. H.; Chung, Y. R.; Lee, Y.; Kang, E.; Kim, S.-W.; Kim, Y. J.; Kim, J. H.; Kim, I. A.; Park, S. Y. Prognostic Significance of Centromere 17 Copy Number Gain in Breast Cancer Depends on Breast Cancer Subtype. Hum Pathol 2017, 61, 111–120. [CrossRef]
- Andrade, J. R.; Gallagher, A. D.; Maharaj, J.; McClelland, S. E. Disentangling the Roles of Aneuploidy, Chromosomal Instability and Tumour Heterogeneity in Developing Resistance to Cancer Therapies. Chromosome Research 2023, 31 (4), 28. [CrossRef]
- Rajagopalan, H.; Lengauer, C. Aneuploidy and Cancer. Nature 2004, 432 (7015), 338–341. [CrossRef]
- Ades, F.; Zardavas, D.; Bozovic-Spasojevic, I.; Pugliano, L.; Fumagalli, D.; de Azambuja, E.; Viale, G.; Sotiriou, C.; Piccart, M. Luminal B Breast Cancer: Molecular Characterization, Clinical Management, and Future Perspectives. Journal of Clinical Oncology 2014, 32 (25), 2794–2803. [CrossRef]
- Kim, A.; Shin, H. C.; Bae, Y. K.; Kim, M. K.; Kang, S. H.; Lee, S. J.; Lee, E. H. Multiplication of Chromosome 17 Centromere Is Associated with Prognosis in Patients with Invasive Breast Cancers Exhibiting Normal HER2 and TOP2A Status. J Breast Cancer 2012, 15 (1), 24. [CrossRef]
- Nielsen, K. V.; Ejlertsen, B.; Møller, S.; Jensen, M.-B.; Balslev, E.; Müller, S.; Knoop, A.; Mouridsen, H. T. Lack of Independent Prognostic and Predictive Value of Centromere 17 Copy Number Changes in Breast Cancer Patients with Known HER2 and TOP2A Status. Mol Oncol 2012, 6 (1), 88–97. [CrossRef]
- Bartlett, J. M.; Munro, A. F.; Dunn, J. A.; McConkey, C.; Jordan, S.; Twelves, C. J.; Cameron, D. A.; Thomas, J.; Campbell, F. M.; Rea, D. W.; Provenzano, E.; Caldas, C.; Pharoah, P.; Hiller, L.; Earl, H.; Poole, C. J. Predictive Markers of Anthracycline Benefit: A Prospectively Planned Analysis of the UK National Epirubicin Adjuvant Trial (NEAT/BR9601). Lancet Oncol 2010, 11 (3), 266–274. [CrossRef]
- Tibau, A.; López-Vilaró, L.; Pérez-Olabarria, M.; Vázquez, T.; Pons, C.; Gich, I.; Alonso, C.; Ojeda, B.; Ramón y Cajal, T.; Lerma, E.; Barnadas, A.; Escuin, D. Chromosome 17 Centromere Duplication and Responsiveness to Anthracycline-Based Neoadjuvant Chemotherapy in Breast Cancer. Neoplasia 2014, 16 (10), 861–867. [CrossRef]
- Lebok, P.; Mittenzwei, A.; Kluth, M.; Özden, C.; Taskin, B.; Hussein, K.; Möller, K.; Hartmann, A.; Lebeau, A.; Witzel, I.; Mahner, S.; Wölber, L.; Jänicke, F.; Geist, S.; Paluchowski, P.; Wilke, C.; Heilenkötter, U.; Simon, R.; Sauter, G.; Terracciano, L.; Krech, R.; von der Assen, A.; Müller, V.; Burandt, E. 8p Deletion Is Strongly Linked to Poor Prognosis in Breast Cancer. Cancer Biol Ther 2015, 16 (7), 1080–1087. [CrossRef]
- Watkins, T. B. K.; Lim, E. L.; Petkovic, M.; Elizalde, S.; Birkbak, N. J.; Wilson, G. A.; Moore, D. A.; Grönroos, E.; Rowan, A.; Dewhurst, S. M.; Demeulemeester, J.; Dentro, S. C.; Horswell, S.; Au, L.; Haase, K.; Escudero, M.; Rosenthal, R.; Bakir, M. Al; Xu, H.; Litchfield, K.; Lu, W. T.; Mourikis, T. P.; Dietzen, M.; Spain, L.; Cresswell, G. D.; Biswas, D.; Lamy, P.; Nordentoft, I.; Harbst, K.; Castro-Giner, F.; Yates, L. R.; Caramia, F.; Jaulin, F.; Vicier, C.; Tomlinson, I. P. M.; Brastianos, P. K.; Cho, R. J.; Bastian, B. C.; Dyrskjøt, L.; Jönsson, G. B.; Savas, P.; Loi, S.; Campbell, P. J.; Andre, F.; Luscombe, N. M.; Steeghs, N.; Tjan-Heijnen, V. C. G.; Szallasi, Z.; Turajlic, S.; Jamal-Hanjani, M.; Van Loo, P.; Bakhoum, S. F.; Schwarz, R. F.; McGranahan, N.; Swanton, C. Pervasive Chromosomal Instability and Karyotype Order in Tumour Evolution. Nature 2020, 587 (7832), 126–132. [CrossRef]
- Oliveira, A. M.; Ross, J. S.; Fletcher, J. A. Tumor Suppressor Genes in Breast Cancer. Pathology Patterns Reviews 2005, 124 (suppl_1), S16–S28. [CrossRef]
- Liu, H.; Lu, Z.-G.; Miki, Y.; Yoshida, K. Protein Kinase C δ Induces Transcription of the TP53 Tumor Suppressor Gene by Controlling Death-Promoting Factor Btf in the Apoptotic Response to DNA Damage. Mol Cell Biol 2007, 27 (24), 8480–8491. [CrossRef]
- Shiovitz, S.; Korde, L. A. Genetics of Breast Cancer: A Topic in Evolution. Annals of Oncology 2015, 26 (7), 1291–1299. [CrossRef]
- Wang, L.; Lee, K.; Malonis, R.; Sanchez, I.; Dynlacht, B. D. Tethering of an E3 Ligase by PCM1 Regulates the Abundance of Centrosomal KIAA0586/Talpid3 and Promotes Ciliogenesis. Elife 2016, 5. [CrossRef]
- Yuan, B.-Z.; Zhou, X.; Durkin, M. E.; Zimonjic, D. B.; Gumundsdottir, K.; Eyfjord, J. E.; Thorgeirsson, S. S.; Popescu, N. C. DLC-1 Gene Inhibits Human Breast Cancer Cell Growth and in Vivo Tumorigenicity. Oncogene 2003, 22 (3), 445–450. [CrossRef]
- Guan, C.-N.; Zhang, P.-W.; Lou, H.-Q.; Liao, X.-H.; Chen, B.-Y. DLC-1 Expression Levels in Breast Cancer Assessed by QRT-PCR Are Negatively Associated with Malignancy. Asian Pacific Journal of Cancer Prevention 2012, 13 (4), 1231–1233. [CrossRef]
- Rodrigues-Ferreira, S.; Di Tommaso, A.; Dimitrov, A.; Cazaubon, S.; Gruel, N.; Colasson, H.; Nicolas, A.; Chaverot, N.; Molinié, V.; Reyal, F.; Sigal-Zafrani, B.; Terris, B.; Delattre, O.; Radvanyi, F.; Perez, F.; Vincent-Salomon, A.; Nahmias, C. 8p22 MTUS1 Gene Product ATIP3 Is a Novel Anti-Mitotic Protein Underexpressed in Invasive Breast Carcinoma of Poor Prognosis. PLoS One 2009, 4 (10), e7239. [CrossRef]
- Lovat, F.; Ishii, H.; Schiappacassi, M.; Fassan, M.; Barbareschi, M.; Galligioni, E.; Gasparini, P.; Baldassarre, G.; Croce, C. M.; Vecchione, A. LZTS1 Downregulation Confers Paclitaxel Resistance and Is Associated with Worse Prognosis in Breast Cancer. Oncotarget 2014, 5 (4), 970–977. [CrossRef]
- Pirzio, L. M.; Pichierri, P.; Bignami, M.; Franchitto, A. Werner Syndrome Helicase Activity Is Essential in Maintaining Fragile Site Stability. J Cell Biol 2008, 180 (2), 305–314. [CrossRef]
- Svoboda, M.; Sana, J.; Redova, M.; Navratil, J.; Palacova, M.; Fabian, P.; Slaby, O.; Vyzula, R. MiR-34b Is Associated with Clinical Outcome in Triple-Negative Breast Cancer Patients. Diagn Pathol 2012, 7 (1), 31. [CrossRef]
- Miki, Y.; Swensen, J.; Shattuck-Eidens, D.; Futreal, P. A.; Harshman, K.; Tavtigian, S.; Liu, Q.; Cochran, C.; Bennett, L. M.; Ding, W.; Bell, R.; Rosenthal, J.; Hussey, C.; Tran, T.; McClure, M.; Frye, C.; Hattier, T.; Phelps, R.; Haugen-Strano, A.; Katcher, H.; Yakumo, K.; Gholami, Z.; Shaffer, D.; Stone, S.; Bayer, S.; Wray, C.; Bogden, R.; Dayananth, P.; Ward, J.; Tonin, P.; Narod, S.; Bristow, P. K.; Norris, F. H.; Helvering, L.; Morrison, P.; Rosteck, P.; Lai, M.; Barrett, J. C.; Lewis, C.; Neuhausen, S.; Cannon-Albright, L.; Goldgar, D.; Wiseman, R.; Kamb, A.; Skolnick, M. H. A Strong Candidate for the Breast and Ovarian Cancer Susceptibility Gene BRCA1. Science (1979) 1994, 266 (5182), 66–71. [CrossRef]
- Roylance, R.; Endesfelder, D.; Gorman, P.; Burrell, R. A.; Sander, J.; Tomlinson, I.; Hanby, A. M.; Speirs, V.; Richardson, A. L.; Birkbak, N. J.; Eklund, A. C.; Downward, J.; Kschischo, M.; Szallasi, Z.; Swanton, C. Relationship of Extreme Chromosomal Instability with Long-Term Survival in a Retrospective Analysis of Primary Breast Cancer. Cancer Epidemiology, Biomarkers & Prevention 2011, 20 (10), 2183–2194. [CrossRef]
- Teixeira, M. R.; Pandis, N.; Heim, S. Tumors of the Breast. In Cancer Cytogenetics; Wiley, 2015; pp 426–446. [CrossRef]
- Lengauer, C.; Kinzler, K. W.; Vogelstein, B. Genetic Instability in Colorectal Cancers. Nature 1997, 386 (6625), 623–627. [CrossRef]
- Munro, A. F.; Twelves, C.; Thomas, J. S.; Cameron, D. A.; Bartlett, J. M. Chromosome Instability and Benefit from Adjuvant Anthracyclines in Breast Cancer. Br J Cancer 2012, 107 (1), 71–74. [CrossRef]
- Maley, C. C.; Galipeau, P. C.; Finley, J. C.; Wongsurawat, V. J.; Li, X.; Sanchez, C. A.; Paulson, T. G.; Blount, P. L.; Risques, R.-A.; Rabinovitch, P. S.; Reid, B. J. Genetic Clonal Diversity Predicts Progression to Esophageal Adenocarcinoma. Nat Genet 2006, 38 (4), 468–473. [CrossRef]
- Lee, K.; Kim, H. J.; Jang, M. H.; Lee, S.; Ahn, S.; Park, S. Y. Centromere 17 Copy Number Gain Reflects Chromosomal Instability in Breast Cancer. Sci Rep 2019, 9 (1), 17968. [CrossRef]
- Lingle, W. L.; Barrett, S. L.; Negron, V. C.; D’Assoro, A. B.; Boeneman, K.; Liu, W.; Whitehead, C. M.; Reynolds, C.; Salisbury, J. L. Centrosome Amplification Drives Chromosomal Instability in Breast Tumor Development. Proceedings of the National Academy of Sciences 2002, 99 (4), 1978–1983. [CrossRef]
Figure 1.
Chromosomal instability (CIN) observed in luminal B BC patients. Each row represents a patient, while that each column represents a chromosome. The level of CIN is color coded according to the legend at the bottom.
Figure 1.
Chromosomal instability (CIN) observed in luminal B BC patients. Each row represents a patient, while that each column represents a chromosome. The level of CIN is color coded according to the legend at the bottom.
Figure 2.
Representative FISH images for luminal B BC patients. Dual-color FISH was performed on nuclei spreads for chromosomes 2 and 11, chromosomes 3 and 15, and chromosomes 8 and 17, using centromeric probes (CEP) labeled with different spectrum colors: spectrum orange for CEP2, CEP3 and CEP8, and spectrum green for CEP 11, CEP15 and CEP17.
Figure 2.
Representative FISH images for luminal B BC patients. Dual-color FISH was performed on nuclei spreads for chromosomes 2 and 11, chromosomes 3 and 15, and chromosomes 8 and 17, using centromeric probes (CEP) labeled with different spectrum colors: spectrum orange for CEP2, CEP3 and CEP8, and spectrum green for CEP 11, CEP15 and CEP17.
Figure 3.
Chromosomal instability (CIN) and Clonal heterogeneity (CH) observed in luminal B BC patients according to PR and HER2 status. A) The level of CIN was classified as having low CIN (CIN=0-25%), intermediate CIN (CIN=26%-50%), high CIN (CIN=51%-70%), or extreme CIN (CIN>70%). B) CH was determinate by True Diversity (TD). Values below 1.5 were considered indicative of low CH, values between 1.6 and 2 were considered indicative of intermediate CH, and values higher than 2 were considered indicative of high CH.
Figure 3.
Chromosomal instability (CIN) and Clonal heterogeneity (CH) observed in luminal B BC patients according to PR and HER2 status. A) The level of CIN was classified as having low CIN (CIN=0-25%), intermediate CIN (CIN=26%-50%), high CIN (CIN=51%-70%), or extreme CIN (CIN>70%). B) CH was determinate by True Diversity (TD). Values below 1.5 were considered indicative of low CH, values between 1.6 and 2 were considered indicative of intermediate CH, and values higher than 2 were considered indicative of high CH.
Figure 4.
Chromosomal Instability (CIN) observed in all chromosomes analyzed in luminal B BC patients. Each chromosome was classified as having low CIN (CIN (CIN=0-25%), intermediate CIN (CIN=26%-50%), high CIN (CIN=51%-70%), or extreme CIN (CIN>70%).
Figure 4.
Chromosomal Instability (CIN) observed in all chromosomes analyzed in luminal B BC patients. Each chromosome was classified as having low CIN (CIN (CIN=0-25%), intermediate CIN (CIN=26%-50%), high CIN (CIN=51%-70%), or extreme CIN (CIN>70%).
Figure 5.
Stage of the aneuploidy observed in luminal B BC patients. Each row represents a patient, while that each column represents a chromosome. The stability of the aneuploidy is color coded according to the legend at the bottom. Values ≥20% were considered as stable aneuploidy, while values <20 were considered as unstable aneuploidy.
Figure 5.
Stage of the aneuploidy observed in luminal B BC patients. Each row represents a patient, while that each column represents a chromosome. The stability of the aneuploidy is color coded according to the legend at the bottom. Values ≥20% were considered as stable aneuploidy, while values <20 were considered as unstable aneuploidy.
Figure 6.
Stability of the aneuploidy in luminal B BC patients according to PR and HER2 status. A) ER+/PR+/HER2-, B) ER+/PR-/HER2- and C) ER+/PR+/HER2+. Values ≤20 were considered unstable, while values >20 were considered stable.
Figure 6.
Stability of the aneuploidy in luminal B BC patients according to PR and HER2 status. A) ER+/PR+/HER2-, B) ER+/PR-/HER2- and C) ER+/PR+/HER2+. Values ≤20 were considered unstable, while values >20 were considered stable.
Figure 7.
Multivariate analysis with Pearson correlation coefficient for copy number variations of chromosomes 2, 3, 8, 11, 15 and 17 and clinicopathologic characteristics. Values greater than 0.5 are indicative of a statistically significant correlation. Abbreviations: Ht, Histotype; T, tumor size; N, lymph nodes, LI; lymphovascular invasion; PR, progesterone receptor.
Figure 7.
Multivariate analysis with Pearson correlation coefficient for copy number variations of chromosomes 2, 3, 8, 11, 15 and 17 and clinicopathologic characteristics. Values greater than 0.5 are indicative of a statistically significant correlation. Abbreviations: Ht, Histotype; T, tumor size; N, lymph nodes, LI; lymphovascular invasion; PR, progesterone receptor.
Table 1.
Clinicopathological characteristics of luminal B BC patients.
Table 1.
Clinicopathological characteristics of luminal B BC patients.
| Clinicopathological Characteristics |
CIN |
P
value |
CH |
P
value |
| Intermediate |
High |
High |
| Total Number of patients |
|
9 (0,9) |
1 (0,1) |
- |
10 (1) |
- |
| Age |
≥ 50 years |
9 (0,9) |
1 (0,1) |
0,187 |
10 (1) |
0,467 |
| Breast |
Right |
6 (0,6) |
1 (0,1) |
0,788 |
7 (0,7) |
1 |
| Left |
3 (0,3) |
0 |
3 (0,3) |
| Histological type |
Invasive ductal carcinoma |
7 (0,7) |
1 (0,1) |
0,598 |
8 (0,8) |
1 |
| Mixed carcinoma |
2 (0,2) |
0 |
2 (0,2) |
| Histologic grade |
ll |
7 (0,7) |
1 (0,1) |
0,598 |
8 (0,8) |
1 |
| lll |
2 (0,2) |
0 |
2 (0,2) |
| T stage |
T1 |
2 (0,2) |
0 |
0,788 |
2 (0,2) |
1 |
| T2 |
6 (0,6) |
1 (0,1) |
7 (0,7) |
| T3 |
1 (0,1) |
0 |
1 (0,1) |
| N stage |
N0 |
0 |
1 (0,1) |
0,644 |
1 (0,1) |
1 |
| N1 |
3 (0,3) |
1 (0,1) |
4 (0,4) |
| N2 |
3 (0,3) |
0 |
3 (0,3) |
| N3 |
2 (0,2) |
0 |
2 (0,2) |
| Lymphovascular invasion |
Absent |
1 (0,1) |
1 (0,1) |
0,035* |
2 (0,2) |
1 |
| Present |
8 (0,8) |
0 |
8 (0,8) |
| Progesterone receptor |
Positive |
6 (0,6) |
1 (0,1) |
0,49 |
7 (0,7) |
1 |
| Negative |
3 (0,3) |
0 |
3 (0,3) |
| HER2 status |
Positive |
2 (0,2) |
1 (0,1) |
0,107 |
3 (0,3) |
1 |
| Negative |
7 (0,7) |
0 |
7 (0,7) |
| Ki67 index |
≥20% |
9 (0,9) |
1 (0,1) |
0,661 |
10 (1) |
0,467 |
| Receptor status |
ER+/PR+/HER2- |
4 (0,4) |
0 |
0,791 |
4 (0,4) |
0,92 |
| ER+/PR+/HER2+ |
2 (0,2) |
1 (0,1) |
3 (0,3) |
| ER+/PR-/HER2- |
3 (0,3) |
|
3 (0,3) |
Table 2.
Tumor suppressor genes located on the chromosomes analyzed in this study.
Table 2.
Tumor suppressor genes located on the chromosomes analyzed in this study.
| Gene |
Location |
Function |
References |
| MSH2 |
2p22 |
Mismatch repair |
[29] |
| RARβ2 |
3p24 |
Retinoic acid receptor |
[29] |
| PRKCD |
3p21.1 |
Involved in DNA damage response. |
[30] |
| BAP1 |
3p21.1 |
Regulate ubiquitination during the DNA damage response and the cell cycle |
[31] |
| MLH1 |
3p21 |
Mismatch repair |
[29] |
| FHIT |
3p14.2 |
Plays an important role in the regulation of apoptosis |
[31] |
| PMC1 |
8p22 |
Encoded for a protein essential for anchoring microtubules to the centrosome |
[32] |
| DLC1 |
8p22 |
Promoter of apoptosis |
[33,34] |
| MTUS1 |
8p22 |
Slows down mitotic progression by prolonging metaphase. |
[35] |
| LZTS1 |
8p21 |
Inhibits the Cdk1/cyclin B1 complex |
[36] |
| WRN |
8p12 |
Critical controller of fragile site stability, essential for preserving genome stability |
[37] |
| ATM |
11q22.3 |
DNA repair |
[31] |
| MIR34B |
11q23.1 |
Involved in DNA damage response |
[38] |
| TP53 |
17p13.1 |
DNA repair, cell cycle, apoptosis and angiogenesis regulator |
[31] |
| BRCA1 |
17q21.31 |
DNA repair. Maintains genomic stability |
[39] |
| BRIP1 |
17q23.2 |
Important in the normal double-strand break repair function of breast cancer |
[31] |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions, or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).