1. Introduction
Olecranon fractures are common adult injuries and account for 10% of the upper limb fractures [
1,
2] They represent the most frequent elbow fractures. The overall incidence is estimated at 11.5 - 12 per 100,000 population [
1,
3]. Because of its subcutaneous location, olecranon fractures may occur as a result of direct trauma, indirect trauma, or a combination of both [
4]. These fractures commonly show a bimodal distribution: they occur after high-energy trauma in young patients and after simple falls in older patients due to poor bone quality [
5]. These fractures are all intraarticular injuries, and they benefit from anatomic reduction and restoration of the joint surface to allow early range of motion and restore functional elbow motion and strength. Olecranon fractures range from simple nondisplaced fractures to complex fracture-dislocations.
Approximately 85% of all olecranon fractures in the adult population can be described as simple isolated and displaced transverse fractures.
Multiple classification systems for olecranon fractures exist (Mayo, AO, Colton, Schatzker, Horne and Tanzer), but none of them is unequivocally accepted nor can be used in clinical setting to provide direct and reliable guidance on strategies to be followed [
6]. One of the most common is the Mayo classification where simple isolated and displaced fractures are described as Mayo IIA.
These fractures are traditionally managed operatively, and several methods of open reduction and internal fixation used. The chosen method of surgical procedure usually depends on the amount of bone loss, the amount of comminution, the ability to reduce the articular surface, and whether the fracture is defined as stable or unstable [
7,
8]. Two main methods of operative management of olecranon fractures are used: tension-band wiring (TBW) and plate fixation (PF). Others, such as intramedullary fixation and excision of the proximal fragment with triceps advancement, are rare.
Historically, TBW was recommended for the treatment of simple isolated and displaced fractures, whereas plate fixation (PF) is reserved for more complex patterns [
9,
10].
Tension-band wiring is a simple, approved, and low-cost technique. It is the most widely used method. However, its disadvantages include the high number of symptomatic prominences of Kirschner wires (K-wires) and the subsequent removal of metalwork [
11,
12,
13]. Plate fixation is indeed better and provides superior fracture reduction in all fracture patterns as well as resistance against screw pull-out in osteoporotic bone [
14,
15]. Thus, the use of plates has become more common in recent years but there is still controversy regarding the optimal surgical treatment for simple isolated, displaced fractures.
Several studies have compared outcomes and complications between TBW and PF, but no statistical differences were reported.
The purpose was to verify whether a treatment choice was superior in the management of this specific olecranon fracture pattern. Our zero hypothesis was that no difference would emerge between the two surgical options studied either in terms of outcomes and post-treatment complication and removal rates.
2. Materials and Methods
This was a retrospective medical record review on all patients surgically treated with open reduction internal fixation (ORIF) for an olecranon fracture at the Unit of Orthopedics and Traumatology of the University Hospital Policlinico “G. Rodolico - San Marco” in Catania in a period between January 2017 and June 2022. We identified all the patients who had suffered a simple isolated, displaced fracture of the olecranon and had been treated either with tension-band wire or plate fixation.
In the period under analysis, a total of 115 patients with a Mayo IIA – AO/OTA 2U1B1(d) olecranon fracture were treated surgically with tension-band wiring or plate fixation; 25 were excluded from the study because they met exclusion criteria or did not meet inclusion criteria; 18 were lost to follow-up because they were not available to participate or could not be reached using the contact details provided. Finally, 72 patients were eligible and successfully completed the survey.
The inclusion criteria were: 1) simple isolated and displaced fracture; 2) ORIF treatment with either single plate or tension-band wiring; 3) greater than 16 years of age at the time of surgery; and 4) minimum one-year period follow-up. The exclusion criteria were: 1) complex fracture pattern (comminuted fracture; associated elbow fractures with attention to radial head, coronoid process or distal humeral fracture; fracture-dislocation; open fracture); 2) additional ipsilateral upper extremity injury; 3) pathological fracture; 4) greater than 85 years of age at the time of surgery; 5) ORIF technique other than TBW and single plate fixation such as double plates or intramedullary screw or nail; 6) follow-up less than one year; and 7) incomplete documentation or radiographs.
All patients’ demographic and clinical data, such as limb involved, complications, reoperations, and hospitalization time were collected and reviewed from medical records, discharge sheets, and ambulatory reports. Using a picture archiving and communication system (PACs), pre-operative anteroposterior and lateral injury X-rays were carefully reviewed in order to classify fracture pattern and concomitant injuries as well as CT scans in bone windowing, when available. The two most common classification systems were applied: the Mayo classification and the latest version of the classification proposed by AO/OTA. Thus, all Mayo IIA and AO/OTA 2U1B1(d) fractures were identified for being included into the study.
Operative reports were also reviewed to determine the implants, the surgical technique utilized in each case and the duration of the surgery. All patients underwent TBW or plate fixation performed by orthopaedic surgeons working at our Unit, both orthopaedic consultants and orthopaedic residents working alongside them.
2.1. Surgical technique
All operations were performed with the patients under general or regional anesthesia (axillary block) with sedation and in supine decubitus position. A longitudinal posterior approach was adequate for this fracture pattern. The fracture was exposed through a posterior midline incision with the proximal end curving to the lateral aspect of the olecranon.
The tension-band wiring (TBW) technique was first introduced by Weber and Vasey in 1963 [
16,
17]. More recently, it was modified and formalized by the AO group becoming the gold standard procedure for the treatment of intra-articular simple transverse olecranon fractures [
18]. The working principle of TBW is to convert tensile forces applied across the fracture by the longitudinal pull of the extensor mechanism into a compressive dynamic force at the joint surface which hold the fracture site more closely leading to better fracture healing [
12,
19,
20,
21,
22].
After a preliminary reduction, two parallel 1.6-mm Kirschner wires were placed antegrade across the fracture site through the proximal end of the olecranon as perpendicular to the fracture line as possible. Some surgeons prefer to angle the K-wires volarly to penetrate and engage the distal anterior cortex, whereas others place them parallel to the long axis of the ulna in the intramedullary canal.
Once the proximal end of the K-wires is bent 180°, the fibers of the triceps tendon should be split sharply with a scalpel at the site of the wires to allow to cut and bent ends to be impacted against the cortex. These gaps between the fibres of the triceps will then be closed over the wires to cover them and reduce protruding and prevent backing out.
An 18-gauge stainless steel wire is passed through a pre-drilled hole perpendicular to the ulnar shaft made with a 2-mm drill in the distal fragment, approximately 3,5 - 4 cm away from the fracture site line and 5 mm away from the posterior cortex. The wire is then passed in a figure-of-eight configuration and crossed over the posterior aspect of the fracture to the insertion of the triceps brachii muscle at the olecranon. Both wire ends are then united with a twist and tightened with tongs. To produce symmetric tension at the fracture site and more rigid fixation, two twisted knots [
19] are placed one radial ad one ulnar (usually 3 or 4 twists are needed to achieve the appropriate tension). These are later bent down against the cortex in order not to irritate the soft-tissues. When the figure-eight wire loop is tensioned, the tension band mechanism starts working.
Plate fixation (PF) has been used mainly for the fixation of comminuted olecranon fractures in which tension band wire fixation is not feasible. Other possible indications are complex fracture patterns requiring a high stability fixation: coexisting coronoid fractures, oblique fractures distal to the midpoint of the trochlear notch, and Monteggia fracture-dislocations with associated olecranon fractures (6,32).
The PF adapts to the shape of the proximal ulna, lying as close as possible to the bony surface of the olecranon to ensure greater reliability and stability of the fixation (33).
There are different types of plates that can be used: One-third tubular, 3.5 mm contoured limited contact dynamic compression (LC–DCP), 3.5 mm reconstruction, hook plates, and pre-contoured locking plates are frequently used [
23]. The choice of a specific plate and fixation technique is determined by the fracture pattern, the quality of the bone and the surgeon's preference.
Plates are commonly applied posteriorly along the dorsal surface of the ulna and contoured around the tip of the olecranon. This represents the side of the olecranon where the tension is greatest and thus makes the structure biomechanically more capable of resisting the bending forces of the triceps tendon [
24,
25]. Fragments are reduced directly with the help of small pointed reduction forceps and can be temporarily held with k-wires to the proximal and distal ulnar between each other or the trochlea of the distal humerus.
The plate may be applied once the reduction is obtained. If an anatomic plate is not used, then the plate must be contoured to fit the proximal ulna bending around the tip of the olecranon and following its curvature. Proximally, the plate may sit off the triceps insertion [
26] or a longitudinal incision can be made to allow the device to sit flush with the posterior cortex. The fixation is then completed by applying locking screws to provide rigidity. AO suggests the plate should be anchored to the bone, whenever possible, with three screws proximal and three screws distal to the fracture applied bi-cortically and without protruding into the joint [
18].
After surgery, patients followed an identical protocol for TBW and plate which provided elbow immobilization for two weeks with the use of a splint. Careful passive and active mobilization were then removed followed by active movement against resistance under physiotherapy guidance at four weeks. After hospital discharge, patients were followed-up regularly: For the first month, they were monitored weekly for wound healing and removal of stitches and splint. Patients were then seen at 1 month, 3-6 months, and 1 year postoperatively for clinical and radiological follow-up. The radiographic outcome was assessed for fracture union, but also for possible complications such as hardware migration/failure, malunion/nonunion, and post-traumatic osteoarthritis.
2.2. Clinical and radiographic evaluation
After hospital discharge, patients were followed-up regularly following a protocol identical for TBW and plate. For the first month, patients were monitored weekly for wound healing and removal of stitches and plaster. Patients were then seen at 1 month, 3-6 months, and 1 year postoperatively for clinical and radiological follow-up. The radiographic outcome was assessed for fracture union, but also for possible complications such as hardware migration/failure, malunion/nonunion. And post-traumatic osteoarthritis.
Patients were divided into two groups according to the type of treatment they received (TBW or PF) and were evaluated in terms of age, sex, involved side, clinical-functional outcomes, hospital stay, surgical duration, complications, and reoperation. All data were maintained in a de-identified database.
To assess the functional outcome after surgical therapy of olecranon fractures, we measured the elbow joint ROMs and use three different validated scoring systems described in the current literature: the Disabilities of the Arm, Shoulder and Hand score (DASH), the Mayo Elbow Performance Score (MEPS), and the Patient American Shoulder and Elbow Surgeons Standardized Elbow Assessment score (pASES-e) [
27,
28]. The aim of the scoring systems is to simplify complex clinical situations and to ensure reproducibility of the results, make comparisons, and extrapolate findings.
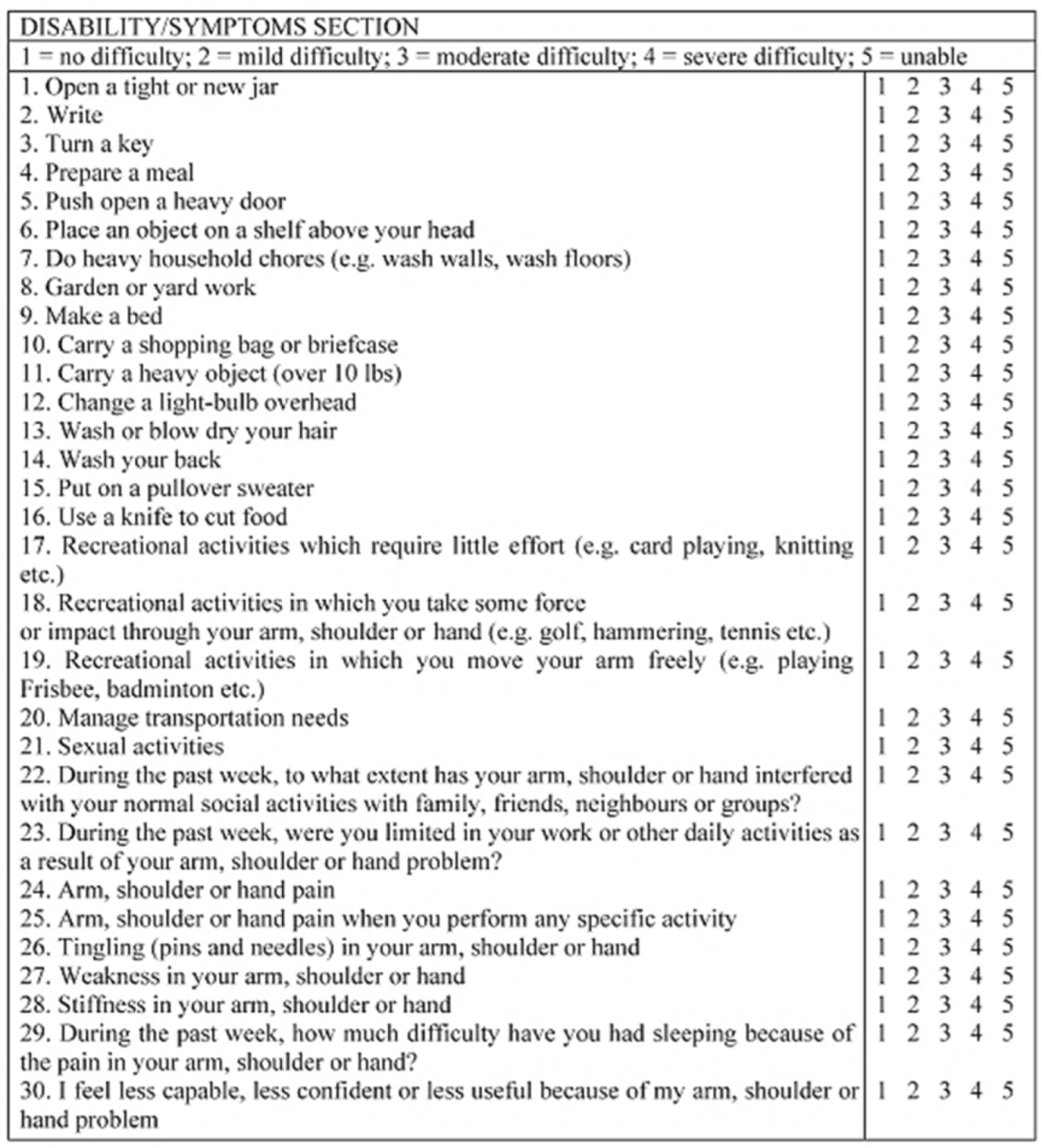
The DASH is one of the most common tools utilized to evaluate the daily function following injuries of the upper limb (Attachment A1) [
29,
30]. It is a 30-item questionnaire in which patients are asked about the degree of difficulty in performing activities of daily living and specific symptoms such as pain, weakness, or paraesthesia of the upper limb. Shoulder, arm, and hand are assessed as a functional unit whose degree of impairment is measured via score. All items of DASH are scored with a five-point scale: 1 = no difficulty; 2 = mild difficulty; 3 = moderate difficulty; 4 = severe difficulty; and 5 = unable. Scores range from 0 (no disability) to 100 (most severe disability).
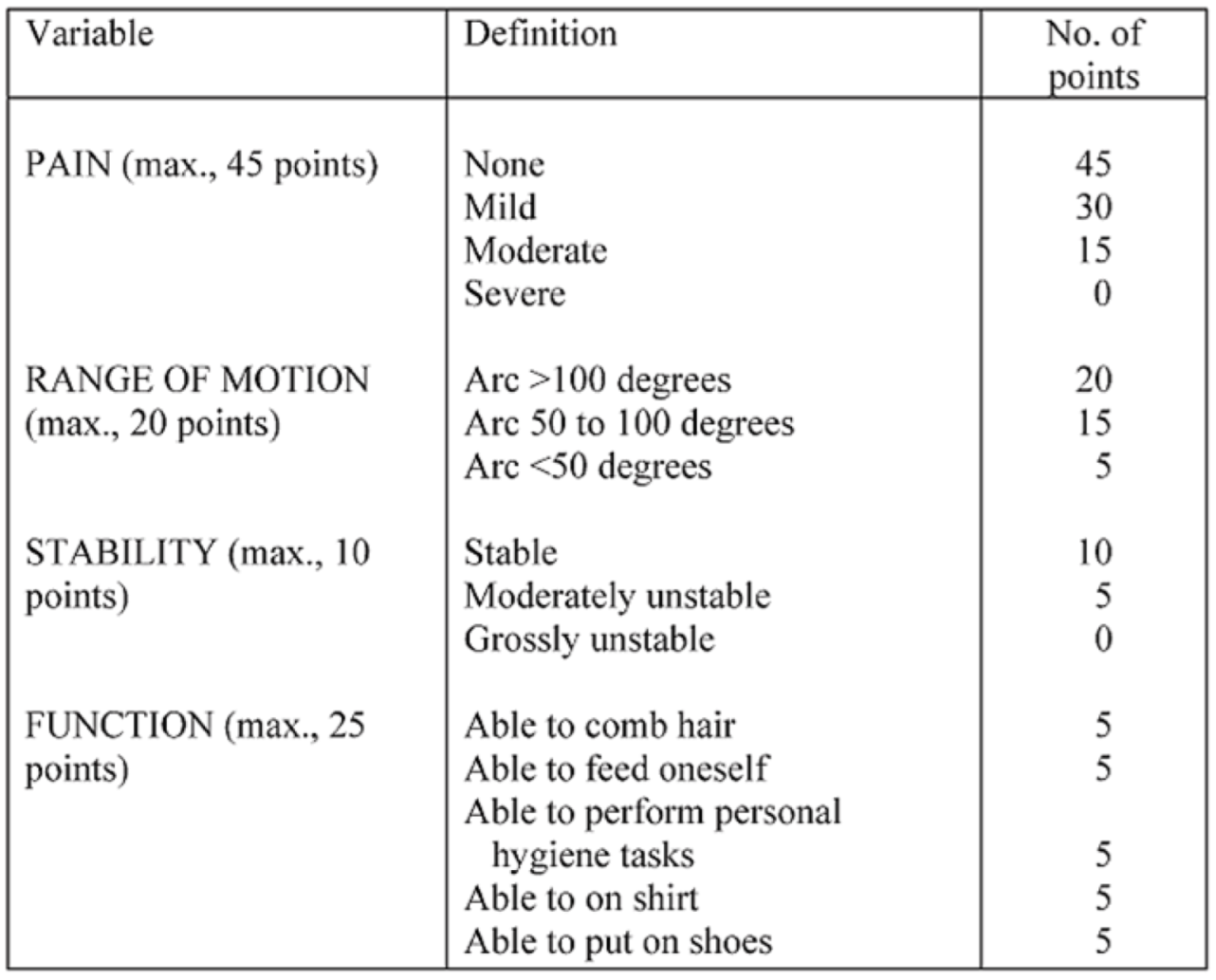
The Mayo Elbow Performance Score, or MEPS, was developed specifically for assessing elbow function following fractures (Attachment A2) [
31,
32,
33]. The MEPS measures elbow function across four subscales: pain (45 points), ulnohumeral stability (10 points), range of motion (20 points), and five daily functional tasks (25 points). The score ranges from 5 to 100 points and is summarized into four outcome categories. Scores are weighted markedly in favor of the subjective parameters such as pain and daily function. The outcome can be rated as poor (less than 60 points), fair (60–74 points), good (75–89 points), or excellent (90–100 points).
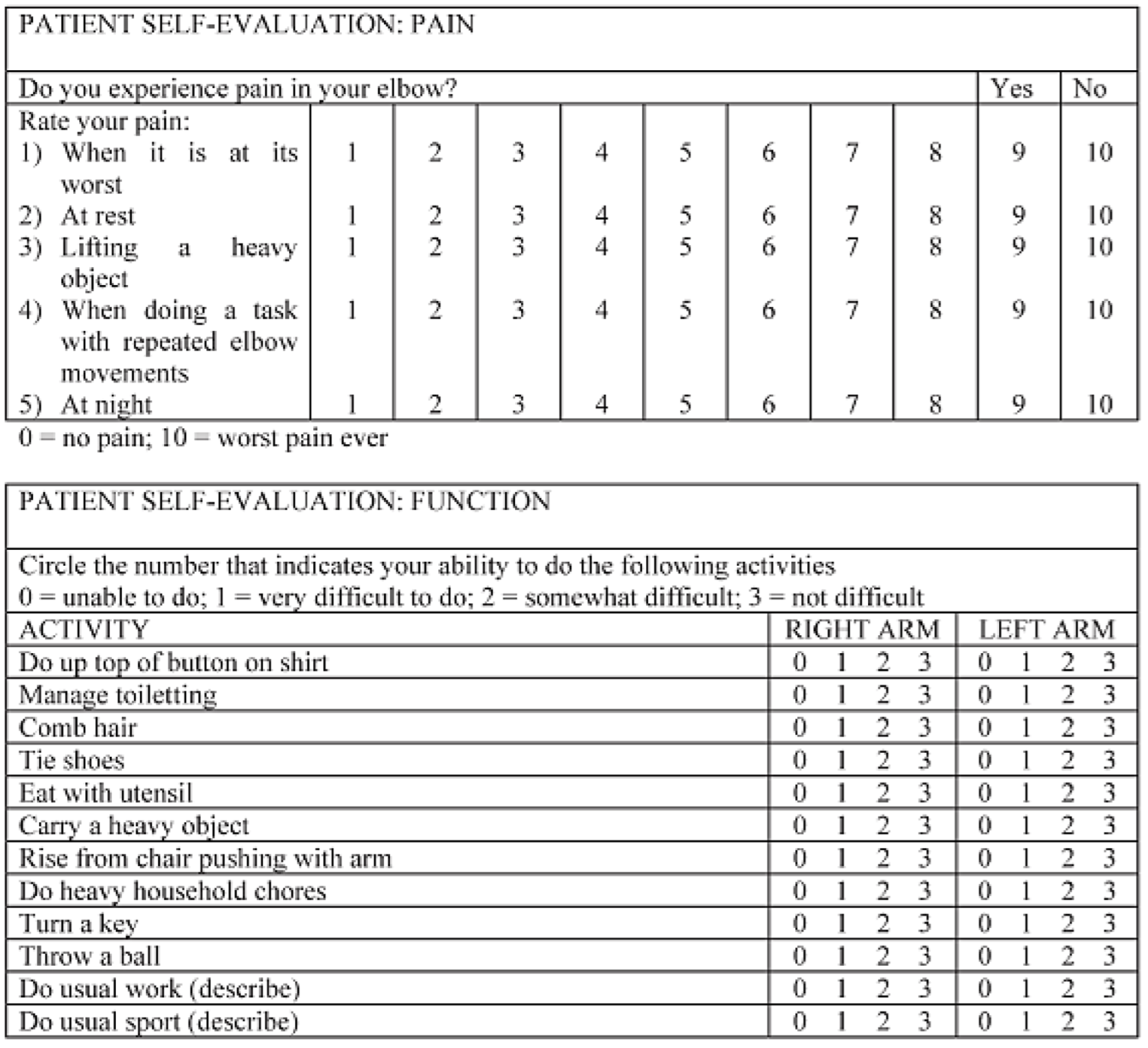
The American Shoulder and Elbow Surgeons-Elbow, or ASES-e, is a standardized elbow assessment tool proposed by the Research Committee of the American Shoulder and Elbow Surgeons (ASES) (Attachment A3). ASES-e is suitable for assessing elbow function regardless of the underlying pathological condition. It consists of two sections: a patient self-evaluation questionnaire (patient ASES-e: pASES-e) and a form intended for the physician to record the degree of clinically detectable elbow impairment (clinical ASES-e: cASES-e) [
34,
35]. The pASES-e form is further subdivided into three sections: pain, function, and satisfaction. In the first section, the pain evaluation is based on a visual analogical scale (from 0 = no pain, to 10 = worst pain ever). The second section contains 12 questions concerning the function of right and left arms, and answers are rated on a four-point scale (from 0 = unable to do, to 3 = no difficult). The maximum score for the function of each arm is 36 with lower scores indicating worse function. In the third section the patient is asked to rate his/her satisfaction with the surgery on a scale of 0 to 10. The pASES-e total score results from the sum of the pain and function subscales equally weighted and can thus range from 0 to 100. The pain score was derived by subtracting the resultant pain score from 50. The function score was derived with the following formula: 50/3 x (arithmetic mean of the 12 function items).
The experimental data collection phase of the study took place at two different points in time. At first, the information necessary to determine the scores was recorded by telephone consultation. Patients were then contacted via telephone, verbally consented for participation in the study, and were asked to provide the required answers. Subsequently, the patients were clinically evaluated in our department for ROMs measurements. The text was translated into Italian, and validated versions of the questionnaires were administered. Orthopedic goniometers were used to measure the joint's ranges of motion.
2.3. Statistical analysis
Data collected were analyzed and statistically elaborated using Microsoft Excel 365 for Windows (Microsoft, Redmond, WA, USA). Characteristics of the study patients were described as mean values (with standard deviation) or numbers (with percentages) as appropriate. Student’s t-test was used to detect any significant differences in continuous variables such as age, functional outcomes, surgery time, hospital stay, and time elapsed before reoperation between the two groups. In case of normal distribution independent samples, a t-test was used to define the two-sided probability of statistical significance and in the analyses that reported a F-test, a P-value less than 0.05 (variances of the two samples cannot be assumed to be equal) were applied; t-tests were corrected for unequal variances (Welch test).
A Chi-squared test was used in categorical variables to determine whether there was a statistically significant difference between the expected frequencies and the observed ones. It was used to analyze statistical differences for sex, complications, and reoperation rates between the two groups. Values of p<0.05 were accepted as statistically significant.
4. Discussion
In this study, we evaluated the clinical-functional outcomes of a retrospective series of simple isolated, displaced olecranon fractures treated with TBW and PF with minimum 1-year follow-up. Several studies in the literature have already tried to compare these two surgical techniques to identify which would give better results. Classically, TBW fixation has been considered the most appropriate treatment for simple displaced olecranon fracture, whereas PF has been reserved for more comminuted fractures [
9,
14,
19,
36,
37].
However, in current clinical practice, TBW has been questioned as the gold standard technique, and PF has become more common even for more simple fracture patterns. The study of Hutchison et al. [
38] failed to prove the theory that posterior tensile forces are converted to compressive force at the articular fracture site. Brink et al. [
39] showed that the tension band principle only works under certain circumstances, which are usually not met in daily life, thus suggesting the presence of a static component acting on the fracture in order to keep reduction and achieve bone healing. Schneider et al. [
40] debunked the popular belief that tension band wire fixation is a surgical technique easy to learn and to apply, drawing attention to potential risks, errors, and complications.
On the other hand, Wilson et al. [
41] compared compression at the fracture site during rest and simulated muscle activity in a cadaveric model. They showed that, in comparison with tension bands in the treatment of transverse olecranon fracture, plate fixation can secure greater compression both over the entire fracture and specifically on the articular surface involved.
Many previous articles have often reported similar clinical outcomes for TBW and PF, but the results remain mixed with data supporting both fixation methods. A Cochrane systematic review of 2014 [
42] of six randomized controlled trials and 244 surgically-managed olecranon fractures showed that there is no sufficient evidence for robust conclusions on the effects of different surgical treatment options. This meta-analysis concluded that more randomized blinded clinical studies are needed to determine the optimal surgical management of simple isolated fractures.
A more recent systematic review from 2021 [
43] analyzed 229 patients from five studies and found no differences both in clinical and patient-rated outcomes between displaced olecranon fractures treated with the two most common fixation techniques (TBW and PF). There was insufficient evidence to draw robust conclusions on the clinical superiority of one treatment over another.
In 1992, Hume and Wiss [
44] were among the first to evaluated in a randomized trial the results of PF versus TBW in different olecranon fractures patterns. They found better clinical outcome and lower complication rate in the PF cohort. No validated patient-reported outcome measures were used, but symptomatic metalwork was seen more frequently in the TBW group (42%) than in the PF group (5%).
Duckworth et al. [
45] more recently reported an ambitious prospective and randomized trial including adult patients with an isolated and displaced fracture of the olecranon. The aim of the study was to determine if any difference existed between TBW and PF with respect to the outcome. The data demonstrated that both techniques provided comparable outcomes for DASH score, MEPS and joint ROM. The overall complication rate was higher following TBW fixation (63.3% TBW vs 37.5% PF) because of an increased rate of symptomatic implant removal (50% TBW vs 21.9% PF).
Tarallo et al. [
46] compared TBW fixation and PF for both Mayo 2A and 2B fractures. No significant differences in functional and clinical outcome were observed between the two groups.Specifically, type 2A fractures had slightly better values for all the outcomes evaluated for the PF group, except for flexion and pronation, but without any significant differences.Likewise, there was no significative difference in complications and hardware removal although rates were higher in TBW than the plate as a whole. However, a statistically significant increase in hardware removal was seen in the TBW group only when grouping both 2A and 2B fracture patterns.
Delsole et al. [
47] compared TBW fixation constructs versus the hook plate, and they both used Mayo-type 1, 2, and 3 fractures (the largest subgroup contained Mayo 2A fractures). Good outcomes were achieved in both groups according to MEPS and ranges of motion. No significant differences were reported except for flexion, which was worse in the PF group than in the TBW one. There was also a non-significant increased rate of symptomatic hardware (30.4% vs 20%) and removal (9% vs 0%) in TBW group.
Claessen et al. [
48] worked on a large retrospective study involving olecranon fractures treated with plate or tension-band wire for the purpose of predicting reoperation and implant removal. Their analysis grouped both Mayo 2A and 2B fractures and a variety of different implants and showed a reoperation rate of 25%. When comparing reoperation and implant removal rates, no significative difference was shown between fracture types and TBW versus plating (22% vs 26% respectively).However, there was a statistically significance increase in both reoperation and request for reoperation in younger patients and those of female sex. Schliemann et al. [
49] compared the clinical and radiological outcomes in TBW fixation constructs versus locking compression plates looking at Mayo 2A fractures in isolation. The outcomes were good with no difference between the cohorts, but twice as many patients required TBW removal as plate removal.
Powell et al. [
50] compared patients treated surgically with either TBW or locking PF for Mayo 2A fractures of the olecranon. In this case, patient outcomes were calculated using the QuickDASH, but no statistically significant difference were found when comparing the two cohorts. In terms of post-surgical complications and reoperation, significantly higher rates were shown in TBW group: 39.6% and 33.3%, respectively.
Gathen et al. [
51] compared the outcomes of patients treated with PF or TBW after isolated olecranon fracture. Different fracture patterns were evaluated, but Mayo 2A were the most represented (52%). Both treatment groups showed good to excellent outcomes regardless of which scoring system was used including DASH. There were no significant differences in complication rates (32.5% in all cases) even if symptomatic metalwork was more common in the TBW group (40% TBW vs 25% PF). The mean duration of surgery and the mean time of hospital stay were compared as well with longer timing in the in the PF group.
Recent studies focused their attention on complication and re-operation rates between TBW and locking PF for olecranon fractures. Rantalaiho et al. [
52] published a ten-year retrospective analysis, although identifying higher rates of complications (50%) and re-interventions (40%) recorded no statistically significant difference in the rate of early complications (49% vs. 62%) or reoperations (38% vs. 53%) between patients treated with TBW and PF even when only looking at Mayo 2 fractures.
Oputa et al. [
53] published a multi-center study and found that the overall complication rate was 25%, and the overall re-operation rate was 17%. There were no significant differences between the two procedures, although complication rates were 28% and 22% and re-operation rates of 15% and 19% for PF vs TBW, respectively.
Previous studies include an interesting comparative economic analysis between the two surgical approaches [
45,
49,
50]. They argue that although plate implant has higher costs per se, the higher frequency of complications and implant removal makes the overall costs of TBW are comparable if not higher.
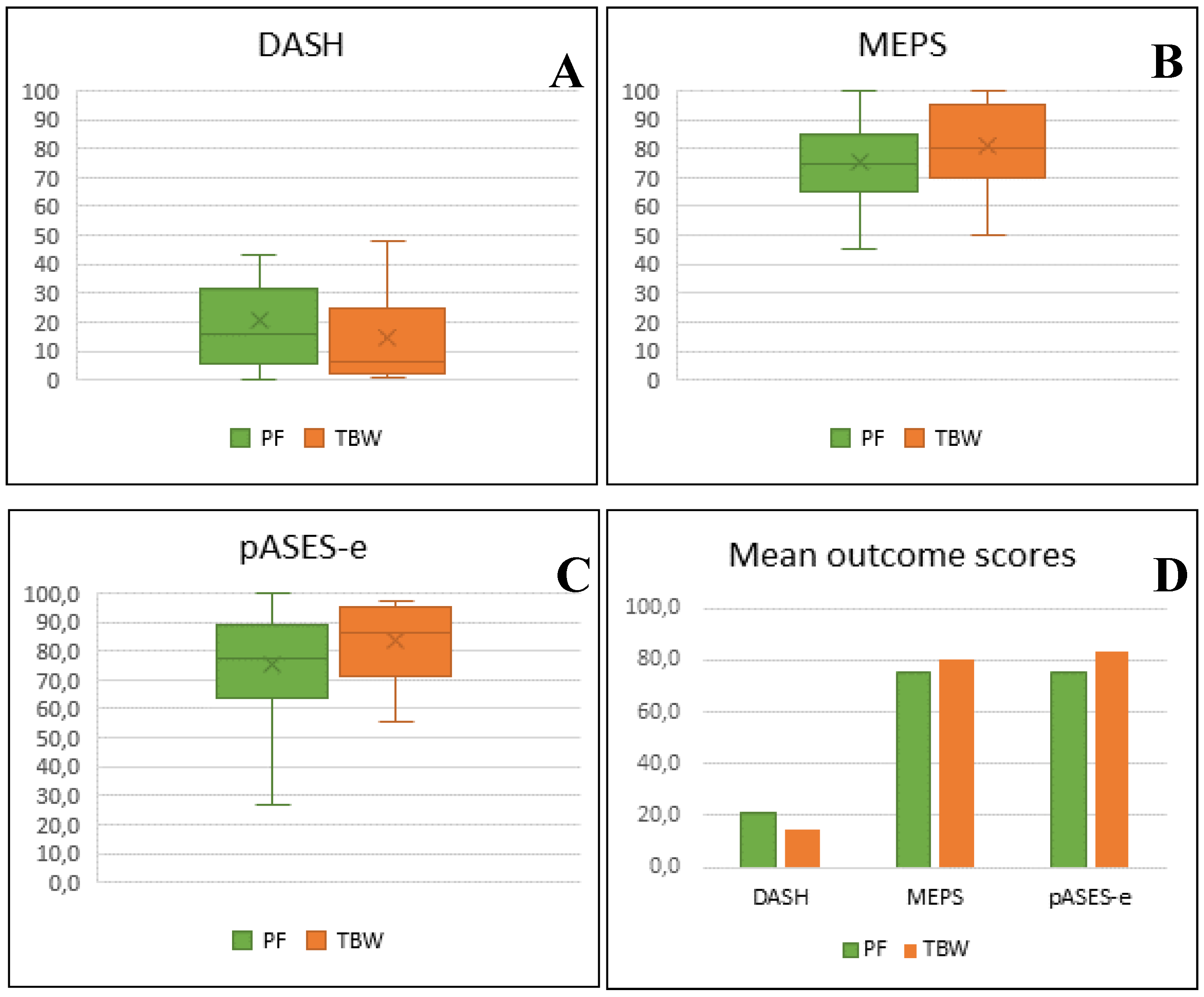
In our cohort, we found that both fixation strategies yielded similar results. We used not only three different patient-reported outcome scores (DASH, MEPS, pASES-e) but also the evaluation of elbow range of motion. The findings indicated that both with TBW and PF have excellent/good clinical outcomes can be obtained.
Although the absolute data deriving from the scoring systems used would seem to suggest slightly better results in TBW, clinical-functional outcomes resulted in statistically comparable values with a significative difference just for pASES-e. This seamlessly mirrors the existing literature.
Indeed, our results are similar to the literature with regard to the time of hospital stay and the duration of surgery, although for these elements have fewer studies with which to compare. Our findings showed a complication rate of 15.3% in all patients, although the rate was higher in the TBW group at 21.1% compared to 8.8% in the PF.
Painful hardware irritation requiring hardware removal was the most common complication after open reduction and internal fixation for olecranon fractures. The higher incidence of metalwork irritation, as well as the higher rate of hardware removal, were reported after TBW versus plating (15.8% vs 2.9% and 18.4% vs 8.8%, respectively). Our results are concordant with other findings in the literature and showed significantly lower rates. In our cohort, as in the literature, TBW was more problematic in terms of complication and subsequential removal, but our numbers are lower than expected.
This apparent discrepancy may be due to several reasons. It is not always easy to assess and quantify hardware-related pain after surgery leading to removal as multiple subjective and objective variables are involved.
Several studies argued that this could be due to the prominence of the tip of the K-wires as a result of their proximal migration out of the proximal end of the ulna. Pain or irritation could, therefore, be affected not only by the subjective threshold of tolerance, but also by the thickness of the overlying soft tissue or by the poor consistency of the patient's bone, which does not guarantee an adequate grip for the K-wires to resist against the traction of the triceps and maintain their position.
To confirm this, Edwards et al. [
54] reported that many patients had their implant removed for the most varied reasons, not always objectifiable. But at the same time, they reported that many others renounced the hardware removal for the fear of another surgery. Long-term follow-up studies showed rates of complications and subsequential hardware removal of >80% [
3,
36,
55]. In addition to the studies mentioned above, Macko and Szabo [
56] reported painful hardware following TBW in 75% of patients, with hardware removed in 65% of all patients. Villanueva et al. [
13] reported a 46% of hardware removal at a mean four-years of follow-up. In Terstappen at al. [
57], implant removal rates were 84% at a mean 7-years follow-up; in 79% of cases this was due to wire prominence.
Longer follow-up may allow us to record more numerous post-treatment severities and elective removals later. Therefore, our follow-up periods may not be extended enough to conclude for certain that there are or are not statistically significant differences between complications and reoperation rates.
Furthermore, as discussed, Edwards et al. [
54] reported that 78% of patients for removal of tension-band wire or plate referred to a different surgeon than the one who had originally performed the surgery, especially if a long time has passed. This showed that removal rates may be much higher than believed and recorded by surgeons and institutions. If this is the case, then even our study may significantly underestimate the hardware removal rates for both types of surgeries.
One of the main limitations of our study is its retrospective design. Different surgeons performed the procedures over the study period and, even if case record analysis revealed that similar surgical techniques were employed, a bias may be represented by each surgeon’s personal device preference or expertise.
It was not always easy to contact patients because of incomplete or incorrect contact details and poor patient compliance. Another limitation is represented by the follow-up length. As mentioned, a longer period of study may have allowed a different identification and quantifications of complications and reoperations. Finally, the COVID-19 pandemic led to restrictions and fear that could have delayed participation. Many patients were lost on follow-up, and others confessed having renounced seeing their surgeons despite having post-treatment discomforts.