Preprint
Article
Development and Implementation of Virtual Reality Application: Age-Friendly Health System Scenario
Altmetrics
Downloads
145
Views
71
Comments
0
This version is not peer-reviewed
Submitted:
15 February 2024
Posted:
19 February 2024
You are already at the latest version
Alerts
Abstract
INTRODUCTION: With an increase in the aging population, the application of evidence-based practice in geriatric education can strengthen knowledge, skills, and clinical experience for healthcare students caring for older adults. Age Friendly Health Systems (AFHS) is one of the frameworks founded on providing evidence-based and low-risk care centered on what matters most to older adults, their families, and caregivers. Virtual Reality (VR) platforms are gaining popularity due to their ability to provide an immersive, hands-on learning experience resembling an actual medical practice or care setting. Immersive learning enhances students’ sensory perceptions, promoting an innovative and engaging way of acquiring concepts that are difficult to teach in real life. This study aimed to design, develop, implement, and evaluate a case-based training module highlighting AFHS and educating medical students on the 4Ms approach in geriatric care (What Matters, Medication, Mentation, and Mobility).
METHODOLOGY: The project was a feasibility study completed in two phases. Phase one included planning and development of a case-based scenario incorporating 4Ms of AFHS. Phase two included implementing and evaluating the VR training module into the geriatric curriculum for medical students.
RESULTS: The final VR case displays a hospital and post-acute setting where an elderly patient is admitted for a hip fracture. Students learn how to triage and treat patients from admission to discharge while demonstrating their knowledge of AFHS. Approximately 10% of students completed the evaluation survey, and preliminary results indicate significant knowledge change in pre-post scenario-based training on AFHS.
CONCLUSION: The VR education platform and embedded scenario promise an innovative adaptation of technology in learning the concepts of the 4Ms of AFHS. However, future studies should explore VR education with clinical assessment evaluation to ensure competence in providing Age-Friendly care.
Keywords:
Subject: Public Health and Healthcare - Primary Health Care
Background
Age-Friendly Health Systems and Geriatric Care
There is a growing need for improved competency and practice change for the healthcare workforce in providing care to older adults with complex needs. In the U.S., nearly half of older adults have four or more chronic conditions, and addressing all health needs of patients with multiple comorbidities during primary care visits within current practice guidelines may be challenging [1]. Age-Friendly Health Systems (AFHS) is one of the practice frameworks that is based on providing evidence-based, low-risk, coordinated care centered on what matters most to older adults, their families, and caregivers. This practice approach uses the 4M model (What Matters, Medication, Mentation, and Mobility) on patient-centered care [2]. AFHS helps promote overall care for older adults at every point of care, ranging from primary care, hospitalizations, and skilled rehabilitation facilities to assisted living facilities [3]. The main goal of AFHS is to maintain a healthy, safe, and improved quality of life in older adult patients by proactively providing essential care, timely deprescribing or avoiding unnecessary medications, supporting mental health, and managing end-of-life issues [4].
We have partially successfully implemented 4Ms in a geriatric medicine clinic in an academic setting and have Level 2 certification through the Institute of Health Care Improvement (IHI); however, AFHS transformation is a complex process and requires participation at multiple levels. These include the organization, provider, staff, and patient participation. Consistent education for physicians, residents, fellows, and students provides ongoing reinforcement within the organizations to improve many e-clinical measures successfully. Practicing physicians lack education regarding the benefits of providing 4Ms care across the care continuum. The challenge to implementing medication reconciliation, mentation screenings, assessing fall risk for every older adult over 65, and discussing health-related goals, as well as advance directives is still a struggle.
Innovations in Medical Education
The COVID-19 pandemic expedited the digital transformation of the education sector by expanding distance learning trends and advancing innovations in educational technologies [5]. The pandemic has forced educators to provide teaching outside the traditional curriculum and adopt new education delivery methods, including e-learning [6]. With didactic education still being the driving force to educate medical students, innovative teaching methods are included in the medical education curriculum to improve students’ attention and practice competency. Advances in recent technology have helped shape education and practice in rural and underserved areas to meet the educational needs of healthcare providers.
The complexity of the healthcare needs of an aging population further enforces the need to educate future clinicians through innovative clinical learning experiences and interprofessional approaches in medical education [7]. Virtual Reality (VR) in medical education has been evolving over the past several decades, and its usage is expected to grow by $143.3 billion during 2021-2025 [8,9]. VR simulations are being progressively introduced across medical and nursing schools as an effective method of delivering experiential learning [7]. The use of immersive technology as an educational tool has shown an improvement in learning outcomes for healthcare students [10]. Compared with traditional clinical education, VR simulations have proven more effective in both immediate and long-term education outcomes [11].
Medical education offers a number of hours for clinical training in geriatrics, and it is important that 4Ms training is included in the curriculum to advance practice change in geriatrics, and it is important that 4Ms training is included in the curriculum to advance practice change for future clinicians. We propose the project planning, curriculum development, curriculum implementation, and evaluation of a VR curriculum with hands-on training that captures an evidence-based approach based on AFHS to care for older adults. By working with our medical providers and students on enhancing education in both classroom and hands-on experiences, we will integrate learning opportunities throughout the 4-year medical education program. The objectives of the paper are 1) to plan and develop a virtual reality case; 2) to implement the VR case to medical students through geriatric curriculum, and 3) to compare changes in knowledge and attitudes toward AFHS before and after completing the case-based virtual reality.
Methods
Phase 1. Planning and development of AFHS curriculum: The study planning phase required purchasing and training Alienware software and an Oculus Rift headset. The Acadicus software was directly downloaded from their website with a secure User ID and Password. The development process included a detailed design document populating the case through Acadicus scenes with prop assets, interactive elements, character assets, integrated quiz boards, playable 3D recordings (holocrons), scene change buttons, and the student starting location. The different scenarios and healthcare settings were specifically developed to provide students with diverse clinical experience and address each of the 4Ms. The educational content of the AFHS training module was based on a unique case of a geriatric patient (Millie) and included clinical and interactive components developed by a team of experts, including geriatricians, faculty, and biomedical informatics technology specialists. The module includes audio narration by a senior geriatrician to help navigate students through the course and various settings.
Phase 2: Implementation and evaluation of the VR training module. Following the module development, we conceptualized the implementation process of the case-based AFHS training in medical students’ curriculum. Since the geriatrics elective was offered for third- and fourth-year students in medical school, we modified the geriatric curriculum to incorporate AFHS education in medical school’s third and fourth years.
AFHS training was delivered to approximately 400 medical students via different modalities: 1) Virtual Reality Simulation (students used the VR equipment in the campus lab settings), 2) non-VR mode (students connected to the Acadicus platform and were able to navigate through the scenes and use interactive tools to complete training session), and 3) Recorded YouTube training video (option available for interprofessional education and independent distant learning).
Upon completion of the training, all students were asked to answer a self-administered short knowledge survey, which consisted of multiple-choice questions related to knowledge improvement developed by the SFGWEP team. Data was entered into RedCap, a mature, secure web application for building and managing online surveys and databases. Descriptive data, including frequencies and percentages, were used to summarize and describe the data collected through feedback surveys. A Post design using the matched sample T-Test was used to analyze the data through SPSS version 26. IRB approval was waived for this study due to the nature of the study. The study was a quality improvement project and nonhuman subject research. IRB # 2023-282. The protocol does not require IRB review or approval because its procedures do not fall within IRB’s jurisdiction based on 45 CFR 46.102. Therefore, the protocol has been classified as “Research outside the purview of the IRB” for IRB purposes; the study may still be classified as “research” for academic purposes or for other regulations, such as regulations pertaining to educational records (FERPA) and/or protected health information (HIPAA).
Results
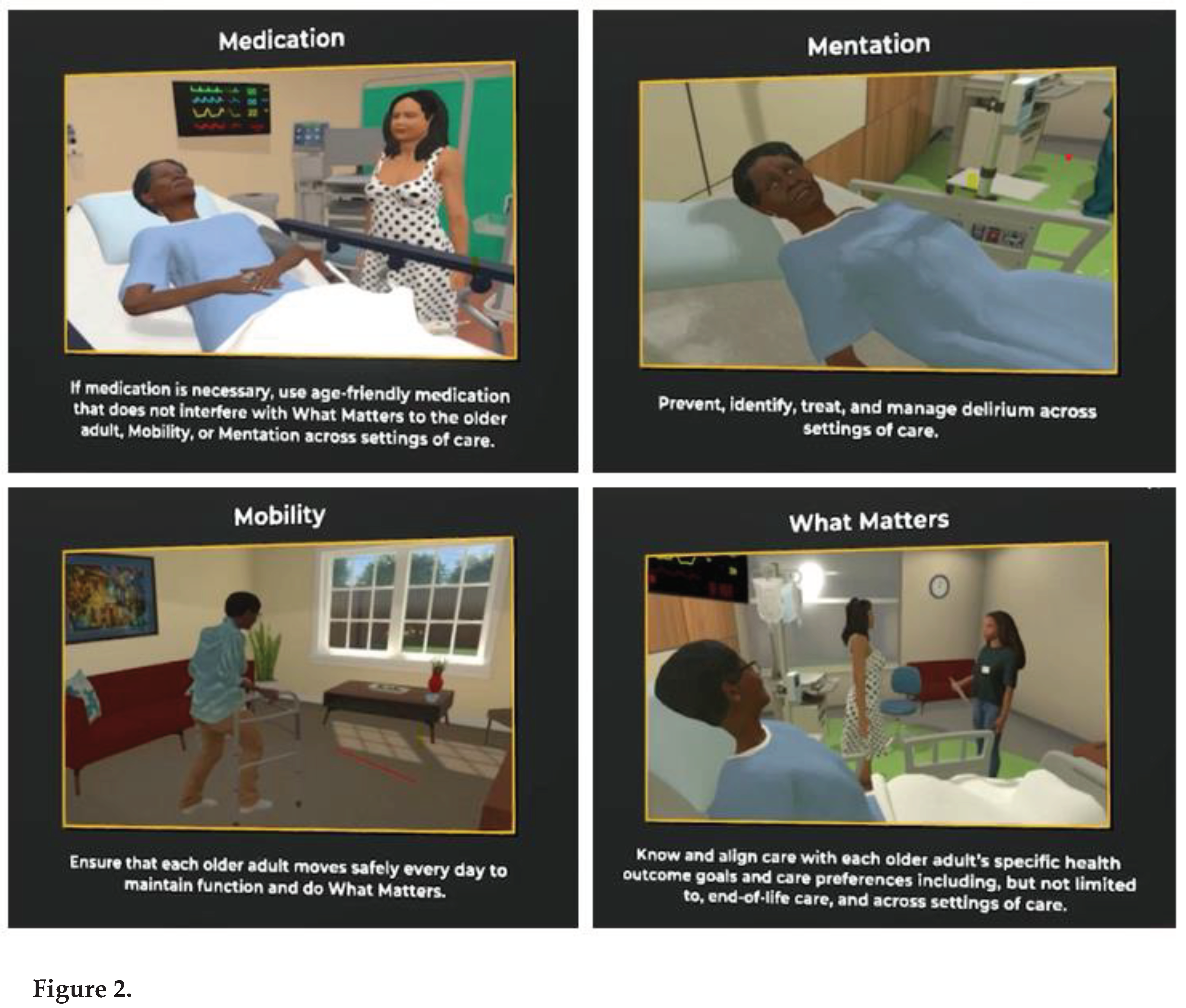
Phase 1. Planning and development of AFHS curriculum: Laptops and headsets were expensive to purchase, maintain, and store in a safe place. Training faculty and staff in using virtual reality was challenging and time-consuming. Development of the case scenario and the user design document required almost 20 hours of faculty time which involved several group meetings and editing the “script” for the developers. The case was written and edited from an AFHS perspective, detailing all the 4Ms necessary for medical students to learn and apply in their clinical practice. The published case introduces students to several situations in which an older adult named “Millie” who is an 87-year-old female is presented with a history of hypertension, diabetes mellitus, diabetic peripheral neuropathy, urinary incontinence, chronic kidney disease, osteoarthritis, and macular degeneration. She fell while going to the bathroom at night and pressed the emergency alert button. The scenario illustrates her healthcare journey and describes the importance of aligning care with an older adult’s preferences and health outcome goals to help students identify strategies for incorporating the 4Ms framework (What Matters, Medication, Mentation, and Mobility) into a healthcare setting for older adults. See Figure 1 and Figure 2.

Phase 2: Implementation and Evaluation of the VR Training Module
Students who chose geriatrics as an elective rotation were provided hands-on experience in implementing 4Ms through the interactive case scenario. In stage 1, students navigate through the hospital setting and review “Millie’s” medication history to complete full medication reconciliation since Millie probably fell due to poor lighting, neuropathy, and hypoglycemia. In stage 2, students review the demonstration of a mentation assessment for dementia and depression using screening tools (PHQ 2 and Mini-Cog) since Millie developed delirium after her surgery for a fractured hip. In stage 3, the patient “Millie” is ready to be discharged, and the students review “What Matters” and an introductory discussion of advance care directives with the patient’s caregiver while she is being discharged to a Skilled Nursing Facility. In the final stage, Millie is transferred to a skilled nursing facility for rehab, and the students learn to use falls risk assessment Timed Up and Go (TUG) while answering an interactive quiz to identify fall risk hazards, for example, handlebars, tables, bed height (too high), no shower chair, no night light, etc. Medical students were also taught interviewing skills to help them communicate with patients struggling with dementia and encourage advance care discussion for appropriate intervention and referral.
Descriptive Statistics
In total, 400 medical students received VR geriatric training, and 40 (10%) students completed the knowledge survey and provided demographic information. Thirty-two (80%) participants were non-Hispanic, 26 (65%) were female, and 13 (33%) were male. Twenty-six (65%) participants identified themselves as White. The majority of the participants, 36 (90%), were in the age range of 20-29 years old. (See Table 1). Survey participants were asked to rate their knowledge on the topic of the Age-Friendly Health System and the 4M’s; and scored on multiple choice questions specific to what matters, medication, mentation, and mobility.
General Knowledge Pre/Post Training. The questions on the survey evaluated students’ knowledge through a 3-point Likert scale question with responses ranging from low, moderate, and high. A paired sample T-test showed that the students’ knowledge significantly increased from pre-training (M= 2.6, SD= 0.778) to post-training (M=-3.2, SD= 0.608, -3.972), with p <.001, df = 39) (See Table 2). Twenty-three (58 %) participants responded that they would apply the training in their practice.
Content-based knowledge-Post Training. The survey also asked multiple choice questions about what matters, medication, mentation, and mobility after the training. Each question consisted of four correct and one incorrect answer. All responses were analyzed and compared. The comparative analysis of student responses on specific topics showed that higher number of students provided correct responses on questions related to AFHS, 34 (85%), what matters, 35 (88%), medication, 37 (93%), and mentation,36 (90%) as compared to a question on mobility, 18 (45%). Overall, 13 students (33%) received a perfect score of 100% on each question, and 30 students (75 %) scored above 90% on all questions, highlighting a clear understanding of the VR training content. (See Table 3).
Discussion
Our study aims to demonstrate the process of developing, implementing, and evaluating a virtual reality case to teach medical students. Planning and developing a virtual reality case is fun and engaging, however, learning in a virtual environment has its own set of challenges [12]. One study found that the development and implementation of VR applications are associated with high costs, reduced face-to-face interaction, and a cumbersome design and development process. Another review study found technological challenges and usability issues in VR implementation [13]. Our study also encountered several development and implementation challenges. Learning space for the VR experience of AFHS was limited to a few students for each session. This was due to a limited amount of available VR equipment, including VR laptops with Acadicus access and Oculus headsets. Additionally, faculty training was time-consuming, with a learning curve. Several faculty members preferred teaching in a didactic environment and, even though motivated, struggled through the technological issues in navigating the case.
Evaluation feedback from the students was positive and demonstrated an increase in students’ knowledge about the 4Ms of the Age-Friendly Health Systems. Demographics in this study suggest the participation of mostly White students, which demonstrates the continued need for diversity in medical education. There was a significant improvement in knowledge of the 4Ms of AFHS. However, these differences in knowledge post-training may be biased due to social desirability and self-report responses. It is also difficult to estimate if participants remembered the information after completing the case experience. Survey fatigue and participant skipping questions on the knowledge survey were among other limitations. In addition, the VR reality case was uploaded as a YouTube link and distributed during the class. Our survey did not ask questions related to the differences in the experience of YouTube video training vs real-time VR case scenarios. Future studies should control these limitations to evaluate the overall improvement and retention of medical students’ knowledge.
Conclusion
The quality improvement project demonstrates the value of VR applications in medical student’s education programs. Innovative teaching models such as VR have been helpful in student engagement due to their benefit of simulating a real-world environment. Medical education is continuously evolving and adapting to new opportunities for student learning. Our study planned, developed, implemented, and evaluated a case-based scenario to teach 4Ms of AFHS through VR application scenarios. The curriculum included an innovative way to teach geriatrics to medical students by integrating several components essential for effective and engaging education, including hands-on clinical experience, interprofessional education, and autonomous learning, in a safe, controlled environment. Medical education must keep pace with the relentlessly changing medical practices and the complex health needs of the growing population of older adults.
Funding
Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS)
References
- Buttorff C, Ruder T, & Bauman M. Multiple chronic conditions in the United States. RAND Corporation. TL-221-PFCD, 2017.
- Institute for Healthcare Improvement (2020). Age-Friendly Health Systems: Guide to Using the 4Ms in the Care of Older Adults. Accessed on September 10, 2023, from https://www.ihi.org/initiatives/age-friendly-health-systems.
- Mate, K.; Fulmer, T.; Pelton, L.; Berman, A.; Bonner, A.; Huang, W.; Zhang, J. Evidence for the 4Ms: Interactions and Outcomes across the Care Continuum. J Aging Health Feb 8:898264321991658. 2021. Epub ahead of print. PMID: 33555233. [Google Scholar] [CrossRef] [PubMed]
- Fulmer, T. , Mate, K. S., & Berman, A.. The Age-Friendly Health System Imperative. J Am Geriatr Soc 2018, 66, 22–24. [Google Scholar] [CrossRef] [PubMed]
- Kang, B. How the COVID-19 Pandemic Is Reshaping the Education Service. In The Future of Service Post-COVID-19 Pandemic; 2021; Volume 1, p. Feb 9:15–36. [Google Scholar] [CrossRef]
- Dwidienawati, D. , Abdinagoro S.B., Tjahjana D., Gandasari D. E-learning implementation during the COVID-19 outbreak: The perspective of students and lecturers. J. Soc. Sci. 2020, 48, 1189–1201. [Google Scholar]
- Pottle, J. Virtual reality and the transformation of medical education. Future Healthc J. 2019, 6, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Pantelidis, P. , Chorti, A., Papagiouvanni, I., Paparoidamis, G., Drosos, C., Panagiotakopoulos, T., … Sideris, M. Virtual and Augmented Reality in Medical Education. InTech. 2018. [Google Scholar] [CrossRef]
- TechNavio . Global medical education market 2021-2025. London, UK: TechNavio; 2021.
- Ryan GV, Callaghan S, Rafferty A, Higgins MF, Mangina E, McAuliffe F. Learning Outcomes of Immersive Technologies in Health Care Student Education: Systematic Review of the Literature. J Med Internet Res. 2022, 24, e30082. [Google Scholar] [CrossRef] [PubMed]
- McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003-2009. Med Educ 2010, 44, 50–63. [Google Scholar] [CrossRef]
- Baniasadi T, Ayyoubzadeh SM, Mohammadzadeh N. Challenges and Practical Considerations in Applying Virtual Reality in Medical Education and Treatment. Oman Med J. PMID: 32489677; PMCID: PMC7232669. 2020, 35, e125. [Google Scholar] [CrossRef] [PubMed]
- Lie SS, Helle N, Sletteland NV, Vikman MD, Bonsaksen TImplementation of Virtual Reality in Health Professions Education: Scoping Review. JMIR Med Educ 2023, 9, e41589. [CrossRef] [PubMed]
Table 1.
Demographics.
| Sample Characteristics | # of Students | % of Students |
|---|---|---|
| M3/M4 | 40 | |
| Age | ||
| 20-29 | 36 | 90% |
| 30-39 | 4 | 10% |
| Gender | ||
| Female | 26 | 65% |
| Male | 13 | 32% |
| Not Reported | 1 | 3% |
| Race | ||
| White | 26 | 65% |
| African American | 2 | 5% |
| Asian | 10 | 25% |
| Unspecified | 2 | 5% |
| Ethnicity | ||
| Hispanic | 7 | 18% |
| Non-Hispanic | 32 | 80% |
| Unspecified | 1 | 3% |
Table 2.
T-Test.
| Pre | Post | N | Mean | Std Deviation | Standard Error of the Mean | Sig (2 tailed) | |
|---|---|---|---|---|---|---|---|
| Knowledge Change | 2.6 | 3.2 | 40 | 0.6 | 0.955 | 0.151 | <.001 |
Table 3.
Participant’s Knowledge Post Training.
| Post Training Participants’ Knowledge Rating (Success Rate) N=40 | # of Participants with correct responses | % of Participants with correct responses |
|---|---|---|
| Good (80%+) - learned a lot of the presented material | 93% | |
| 37 | ||
| High (90%) - learned most of the presented material | 75% | |
| 30 | ||
| Excellent (100%) - learned all of the presented material | 33% | |
| 13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated






