1. Introduction
Halitosis is characterized by an offensive and unpleasant odor originating from the oral cavity and nasopharynx[
1]. This malodor mainly results from the presence of unpleasant smell substances–named volatile sulfur compounds (VSCs)–gases present in the breath air that are produced by oral bacteria on substrates containing sulfur. The main compounds associated with halitosis are: sulfide (H2S) (related to tongue coating), dimethylsulfide ((CH3)2S) (related to periodontal pockets) and methylmercaptan (CH3SH) (related to systemic alterations). These compounds are produced by Gram negative anaerobic bacteria [
2]. Epidemiological studies report the prevalence of halitosis can vary between 2.4–78%, depending mostly on the assessment method (reports or objective measurement of gases) [
3]. This condition has great social implications because it brings embarrassment to its bearer [
4]
The oral microbiome is made up of a huge variety of microorganisms. The terms “microbiota” and “microbiome” are often used interchangeably, however there are differences in their definitions. The microbiota refers to the living microorganisms themselves present in a given environment, such as the oral and intestinal microbiota. The term microbiome refers to the grouping of genomes from the entire environment, that is, in addition to living microorganisms, it includes structural elements as well as environmental conditions and metabolites. [
5]. When there is balance and harmony between the microbiome and the host, there is health, that is, the microorganisms contribute positively to the well-being of the host. Habits in general (food, stress, use of tobacco and other drugs, alcoholic beverages) directly interfere with the relationship between the host and the oral microbiome. This means that these habits can alter the composition of the microbiome in such a way that an imbalance in this ecosystem begins [
6]. When there is disharmony, there are diseases such as halitosis, caries, periodontal disease, among others [
7]. The balance in the microbiome is essential for oral health, which in turn is essential for the general health of the host.
Ye et al. reported that people with halitosis have a more diverse microbiome than those without halitosis. According to the authors, main bacteria related to halitosis are Prevotella, Alloprevotella, Leptotrichia, Peptostreptococcus and Stomatobaculum [
8]. Patients with halitosis apparently have a greater bacterial diversity than control patients. There are 13 phyla, 23 classes, 37 orders, 134 genera, 266 species and 349 operational taxonomic units that make up the microbial communities present in this diversity. [
8,
9]. With the advent of sequencing, these new genera of bacteria related to this condition are being studied.
There are three main methods for the diagnosis of halitosis. The most common of them consists of a subjective method called organoleptic test. In this test the patient exhales air close to the evaluator who quantifies the bad breath through a score. Some factors must be taken into account to contraindicate the use of the organoleptic test, such as the risk of contamination by SARS-CoV-2, for example. [
10]. Another method that can be used is the use of portable breath meters. The use of this equipment was evaluated and compared to the organoleptic test and showed high sensitivity and specificity, being a useful and practical instrument for the detection of halitosis. And finally, gas chromatography, which is the most suitable test for diagnosing the presence and type of halitosis by qualitatively and quantitatively analyzing volatile sulfur compounds [11,12,13].
Halitosis treatments are based on controlling and disorganizing biofilms rich in bacteria related to the production of VSC. Among them are the use of antimicrobial substances, such as chlorhexidine (CHX), cetylpyridinium chloride (CPC), and triclosan, contained in products for oral hygiene such as toothpaste and [
3], antimicrobial photodynamic therapy [
11,
14,
15,
16,
17,
18,
19,
20] and probiotic therapies [
21]. Antimicrobial photodynamic therapy (aPDT) has been commonly used in oral health treatments, including for the treatment of halitosis. This approach involves the use of a visible light source (laser or LED) and a compatible photosensitizer. Reactive oxygen species are formed by the interaction of light with the photosensitizer in the presence of oxygen, causing the cell death of microorganisms [
20].
Because it is a non-invasive technique that does not cause aftereffect, aPDT has been used as an alternative or adjuvant to conventional antimicrobial treatments. Treatments with probiotics consist of the administration of non-pathogenic live microorganisms that aim to enhance the equilibrium of the microbiome [
22]. Therefore, the objective of this study was to compare photodynam1ic therapy and the use of probiotics in reducing halitosis assessed through gas chromatography and microbiome analysis.
2. Materials and Methods
Six participantes were selected, according to inclusion criteria: participantes of both genders, aged from 18 to 25 years, showing on gas chromatography sulfide (SH2) ≥ 112 ppb. Exclusion criteria were: individuals with dentofacial anomalies (such as cleft lip, palatine and nasopalatine fissures), in orthodontic or orthopedic treatment, in oncological treatment, with any health problems (gastrointestinal, renal, hepatic), being treated with antibiotics up to 1 month before the survey and pregnant women. The study has been approved by the Ethics Committee of Universidade Nove de Julho (UNINOVE), under process number 3.669.442 and all participants signed an informed consent form.
Participants were instructed, through a lecture and digital files, to brush with amine fluoride toothpaste (Elmex®) and to floss 3 times a day after meals for 30 days. They were taught how to perfom the Bass technique, in which the bristles of the brush are positioned at an angle of approximately 45o towards the inside of the gingival sulcus, both on the free and proximal surfaces, in addition to short and slightly circular vibrating movements. After the oral hygiene instruction, the initial assessment of the tongue coating proposed by Shimizu et al was carried out using the Coated Tongue Index (CTI) [
23]. For this evaluation, the tongue is divided into 9 sectors, each sector receives a score, being 0-no coating, 1-coating allowing the visualization of the papillae, 2-thick coating not allowing the visualization of the papillae. These grades were added, divided by 18 and multiplied by 100, to obtain a final index of 0100%. It should be clarified that the participants were only instructed and did not brush and floss in the same treatment session. Afterwards, the evaluation was made by gas chromatography with the OralChromaTM device and the microbiological collection was performed for later evaluation of the microbiome.
The collection of oral air followed the manufacturer's instructions (Oral ChromaTM Manual Instruction), in which the subject was required to wash out his mouth with cysteine (10 mM) for 1 minute, then stay with the mouth closed for another 1 minute. A syringe from the same manufacturer designed to collect oral air was introduced into the subject’s mouth. The subjects stay for 1 minute with their mouth closed, respiring through the nose, without touching the syringe with the tongue. the plunger has been pulled out, pushed in, and pulled out again to fill the syringe with the breath sample. The gas injection needle was placed on the syringe, and the plunger was adjusted to 0.5 ml. The collected gases were injected into the inlet port of the device with a single movement. To avoid changes in 5 halimetry, subjects were instructed to follow the guidelines: 48 hours prior to the assessment, do not eat spicy foods (garlic, onion), do not drink alcohol and do not use breath freshener. On the day, eat up to 2 hours before the assessment. Do not consume coffee, candies, chewing gum and do not use oral and personal hygiene products (deodorant, perfumes, creams) and brushing should be performed with water only. The halimetry process with OralChromaTM was performed before, immediately after the treatments, 7 days, 14 days and 30 days after the initial collection, depending on the different treatments.
The collections for later microbiological analysis were made along with the halimetry.
Sterile swab was used to collected the tongue coating by passing on the dorsum of the tongue, performing one backward and forward movement. The samples were deposited in sterile tubes containing Tris – EDTA buffer (10mM Tris – HCL, o.1mM EDTA, pH7.5), identified and stored at -80 C until analyzed. Samples were frozen due to the impossibility of performing all analyzes in a single day.
In the microbiome procedure, all sequencing, raw data collection and analysis were executed by the ByMyCell laboratory. DNA extraction was performed using the DNeasy
PowerSoil Pro Kit (Qiagen®). The resulting fragments were submitted to sequencing of the V3-V4 region of the 16SrRNA gene on the Nanopore platform. After processing reads and removing chimeras, an average of 10,500 reads per sample remained. After filtering, the reads were classified taxonomically, using the SILVA 123 database, obtaining the classification of 414 genera and 901 species.
Participants received different proposed treatments for halitosis from tongue coating, according to the descriptions below.
In one individual (1), tongue scraping was performed with a plastic scraper. The lingual coating was removed using the scraper on the back of the tongue with ten posteroanterior movements, until the scraper came out clean of the surface.
In another individual (28), one session of aPDT was carried out with a LED photopolymerizing device – Valo Cordless Ultradent®, an device, with coupled radiometer, spectrum of 440-480nm and irradiance of 450mW/cm and with 5 sprays of photosensitizer (PS) annatto (manipulated at a concentration of 20% (Formula e Ação®)), covering the middle third and dorsum of the tongue in spray, the pre irradiation time was 2 minutes. The surplus was removed using a sucker to keep the surface moist with the PS itself, without using water. Six points were irradiated with a distance of 1 cm between points, considering the halo of light scattering and effectiveness of aPDT. The apparatus was previously calibrated with a wavelength of 395-480 nm, for 20 seconds per point, energy of 9.6J, and the light was irradiated so that a halo of 2 cm in diameter per point was formed [
18,
19].
Two participants (35 and 39) were instructed to ingest probiotic capsules. Pharmacy
compounded capsules containing strains of Lactobacillus salivarius WB21 (6.7 x 108 CFU) and xylitol (280mg) were used. Forty-two capsules were given to each patient, who 1 had to take 1 capsule, 3 times a day after meals, for 14 days.
Two participants (6 and 18) received both the aPDT and probiotic treatments, as described above.
3. Results
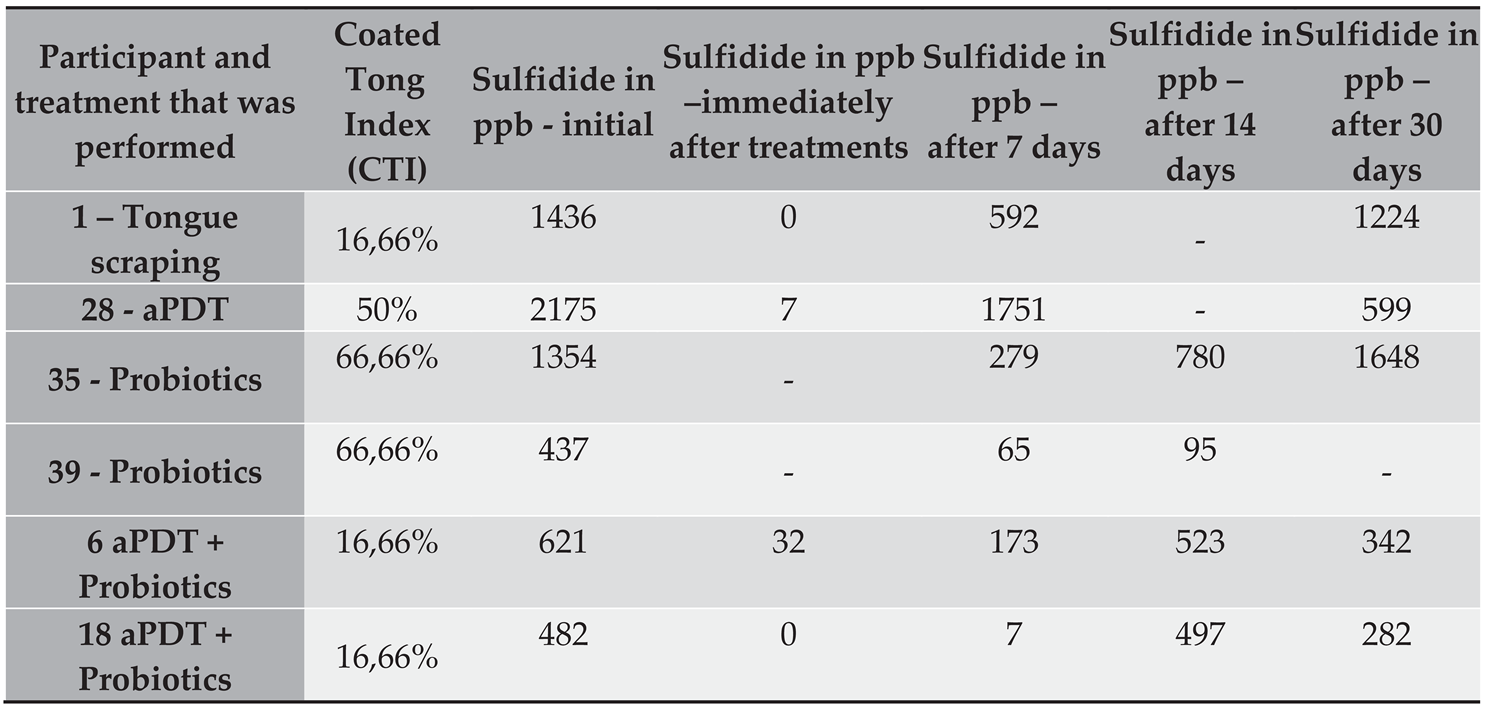
In the
Table 1, we have the results of the initial tongue coating index and the amount of sulfide in ppb in each halimetry. In those treated with scraper and aPDT, the measurements were taken at the initial times, immediately after, 7 days and 30 days, for control. In those treated with probiotics, the initial times, 7 days, 14 days and 30 days were performed. In these participants, it was not possible to carry out the “immediately after” time, since the participant had to start ingesting the probiotics. Consequently, the 14-day control period was added, as the participant ingested the capsules for 14 days. In participants treated with both aPDT and probiotics, all times were performed (initial, immediately after, 7 days, 14 days and 30 days after).
Microbiome
For the statistical analysis, the groups in
Table 2 were considered. To study abundance, the Kruskal-Wallis Test with Dunn's post test was used (Software Rstudio 2022.07.0 Build 548© 2009-2022 RStudio, PBC. The packages used were dbplyr, rstatix , ggplot2).
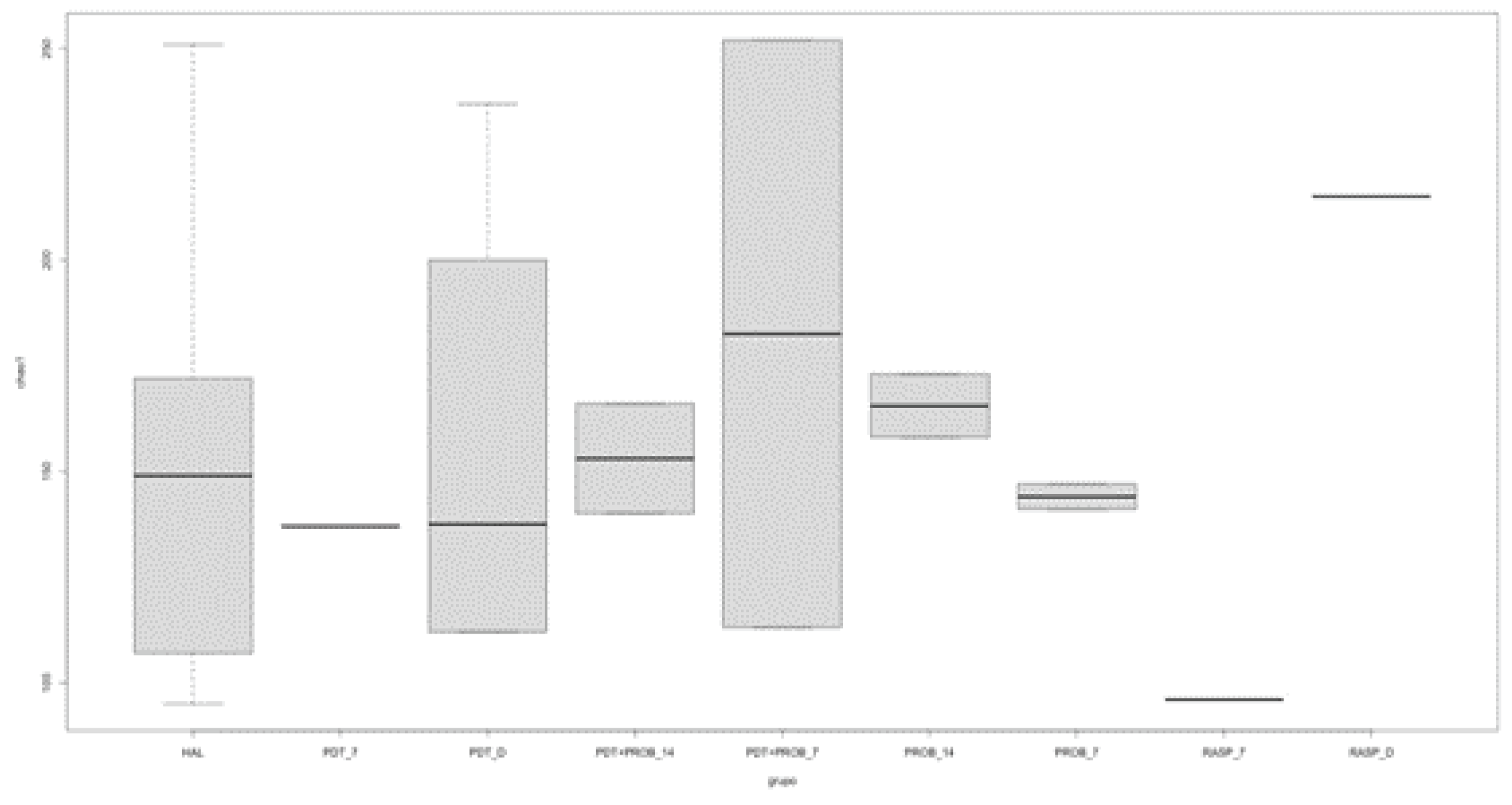
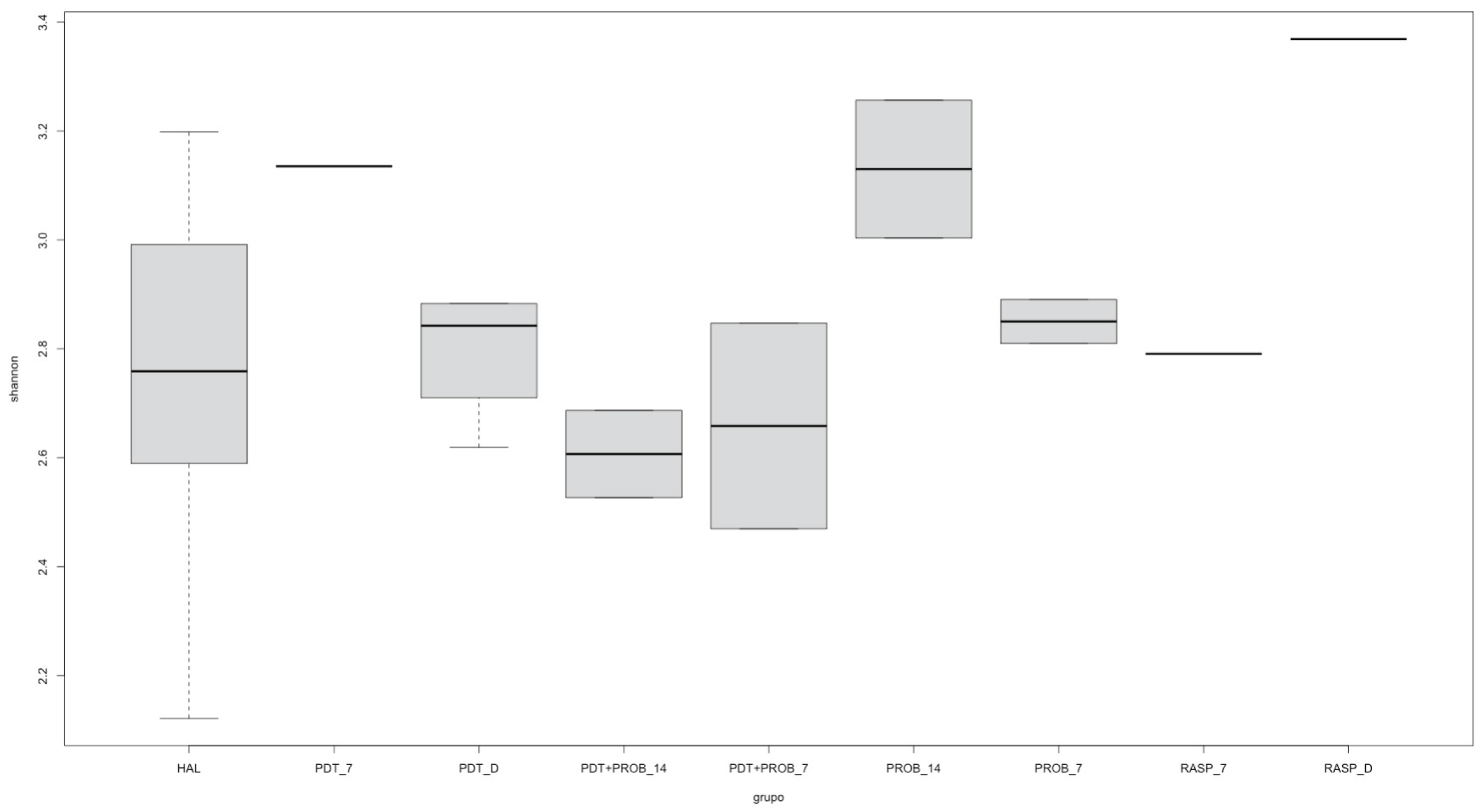
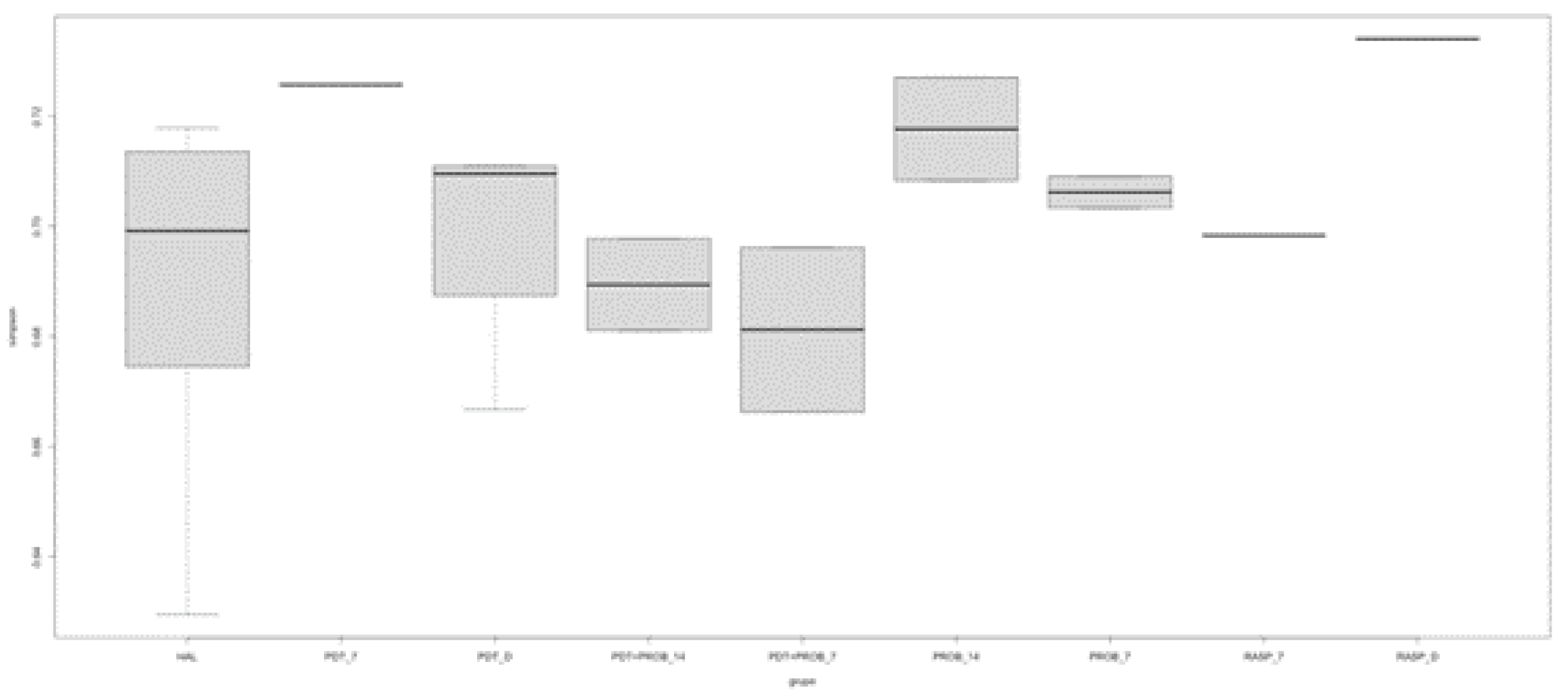
For the analysis of the microbiome of the tongue coating, the analysis of alpha diversity was performed. It can be observed that there was no difference between the groups by the analysis of Chao1, Shannon and Simpson.
From
Figure 1,
Figure 2 and
Figure 3, the comparison between times of the analyzed groups to verify the alpha diversity is shown.
RASP - Scraper Group, PDT - aPDT Group, PROB - Probiotics Group, PDT+PROB - aPDT + Probiotics Group. Times analyzed: Dimmediately after treatment, 7 -7 days, 14 -14 days.
RASP - Scraper Group, PDT - aPDT Group, PROB - Probiotics Group, PDT+PROB - aPDT + Probiotics Group. Times analyzed: Dimmediately after treatment, 7 -7 days, 14 -14 days.
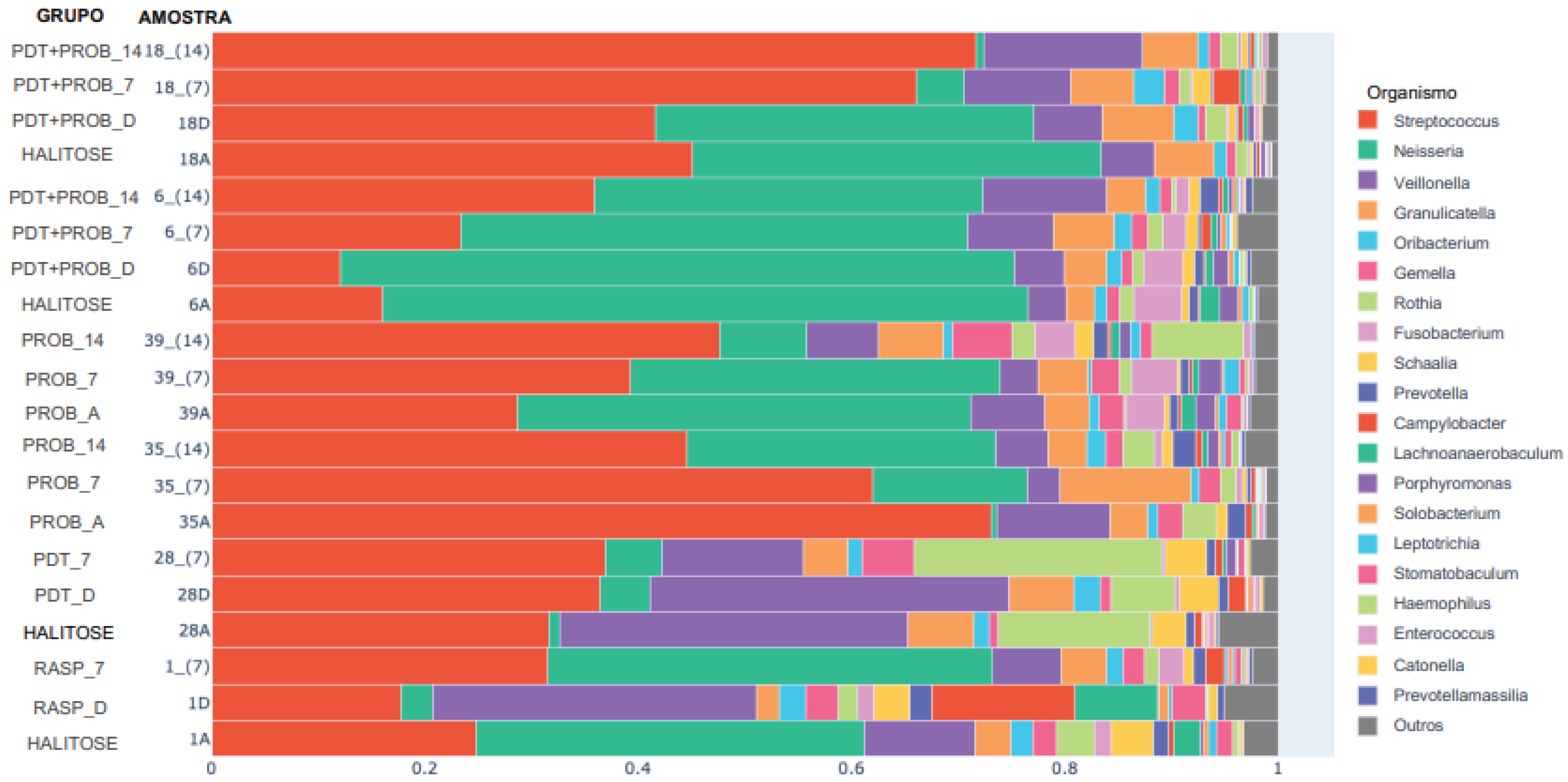
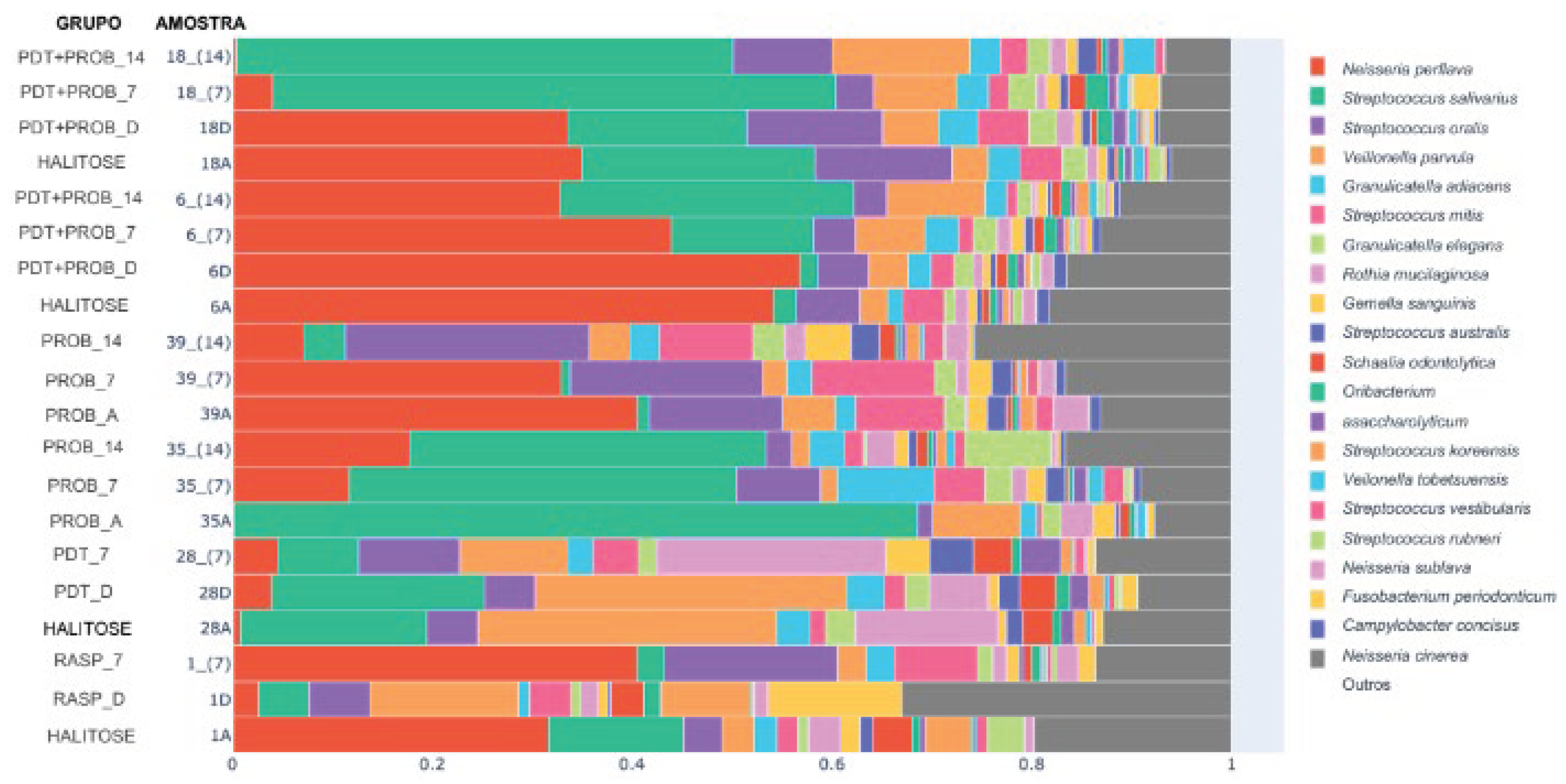
As for the relative abundance analysis regarding the genera found, a difference was observed only for the genus Pseudarthrobacter (p<0.05) between Group 2 and Group 3 at 14 days. In
Figure 4, we can see the 20 most abundant genera present in the analyzed samples.
RASP - Scraper Group, PDT - aPDT Group, PROB - Probiotics Group, PDT+PROB - aPDT + Probiotics Group. Times analyzed: A - before starting treatment, D- immediately after treatment, 7 -7 days, 14 -14 days.
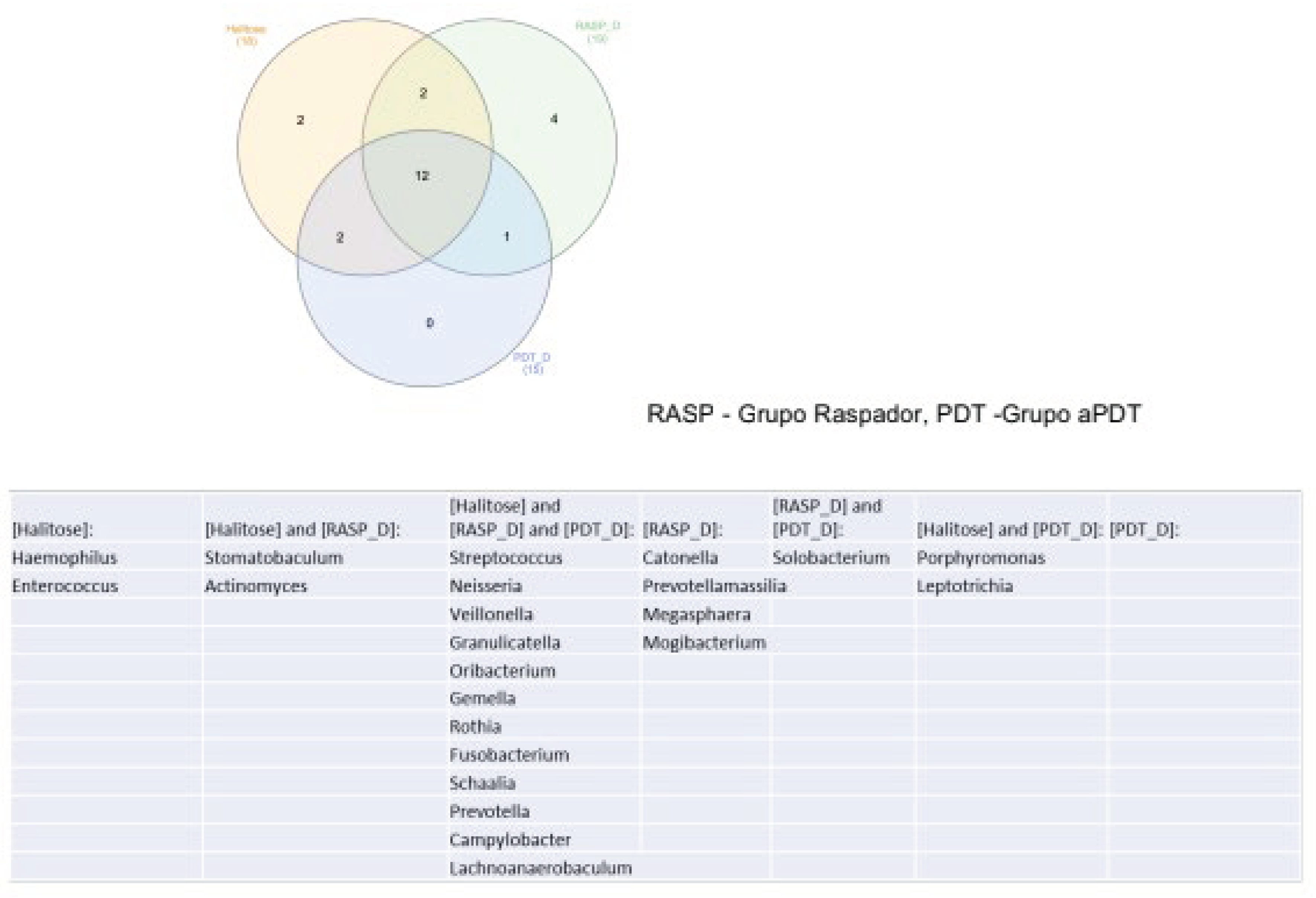
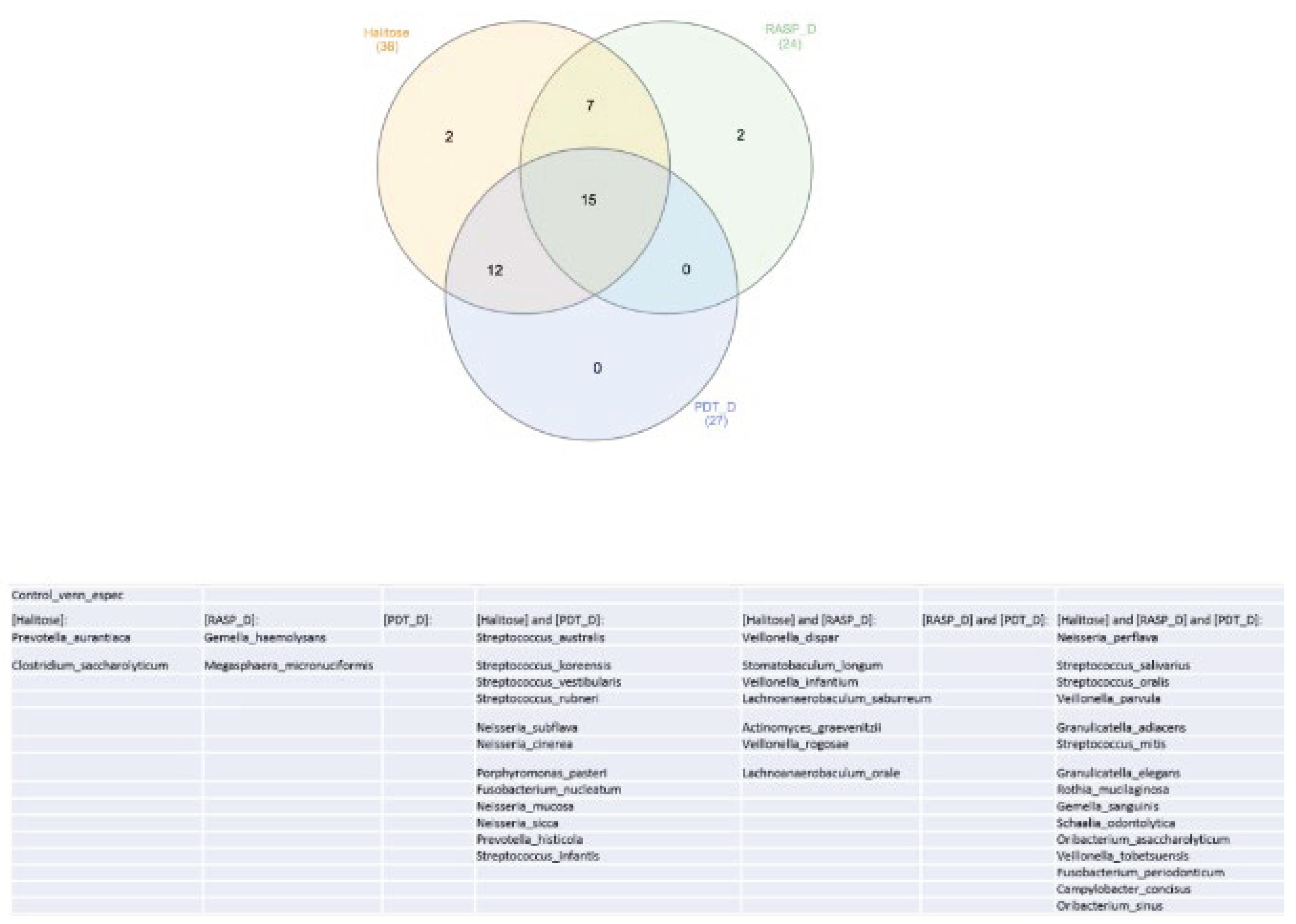
In the Venn diagram represented in
Figure 5, we can observe that 12 genera were common among the Halitosis, Scraping and aPDT groups.
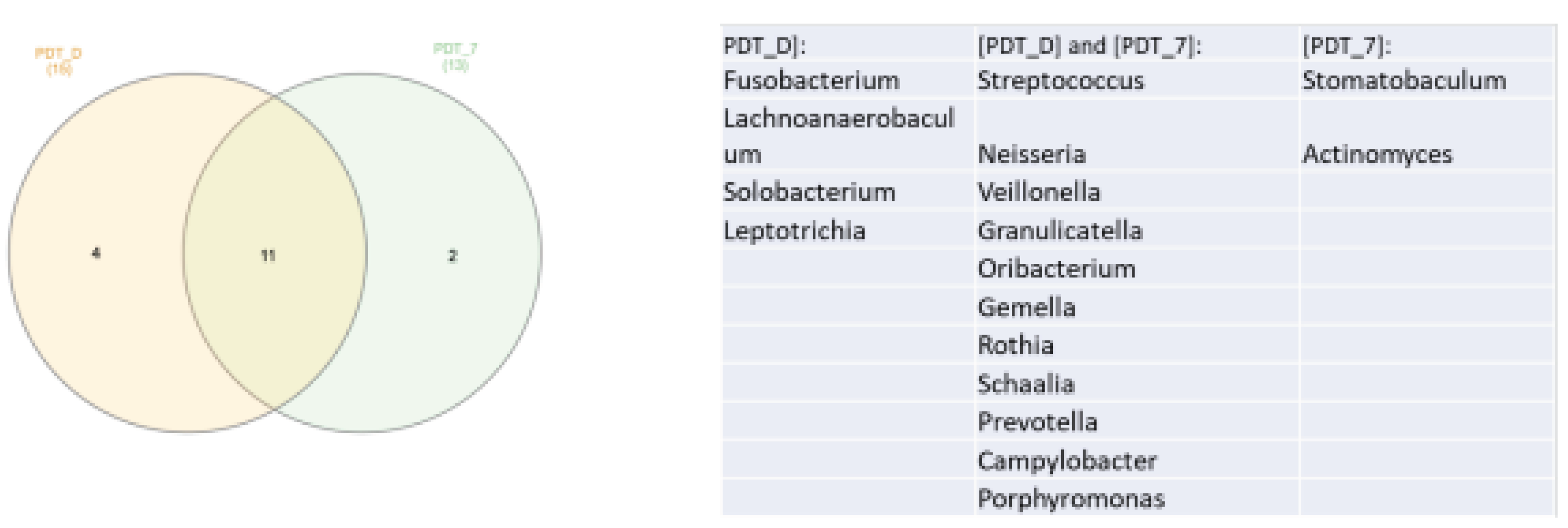
In the Venn diagram represented in
Figure 6, we can see that there was a decrease in the number of genera found when comparing the times immediately after treatment and 7 days.
PDT - aPDT group, PDT+PROB - aPDT group + probiotics. Times analyzed: A - before starting treatment, D- immediately after treatment, 7 -7 days, 14 -14 days.
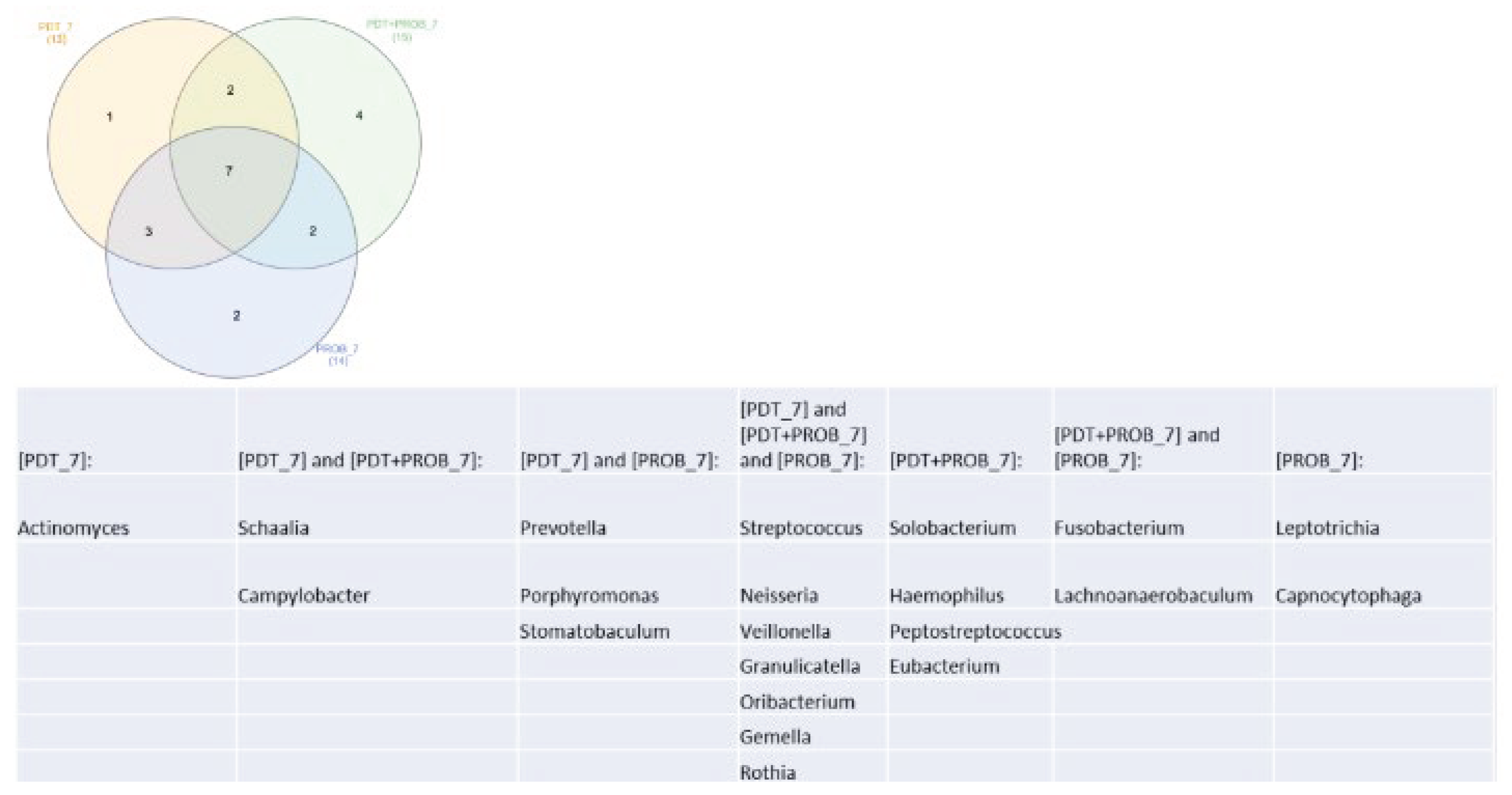
In the Venn diagram represented in
Figure 7, we can see that there was similarity of 7 genera found at 7 days.
In the Venn diagram represented in
Figure 8, we can see that there was similarity of 14 genera found at 14 days.
Relative abundance (species)
Regarding the relative abundance between the species present in the samples, in 25 general, we can say that there was no difference between the groups (p>0.05, KruskalWallis test).
Figure 9 shows the relative abundance of the 20 most abundant species 46 present in the analyzed samples.
Group. Times analyzed: A - before starting treatment, D- immediately after treatment, 7 -7 days, 14 -14 days.
In the Venn diagram represented in
Figure 10, we can see species that were more abundant than 1% in control groups.
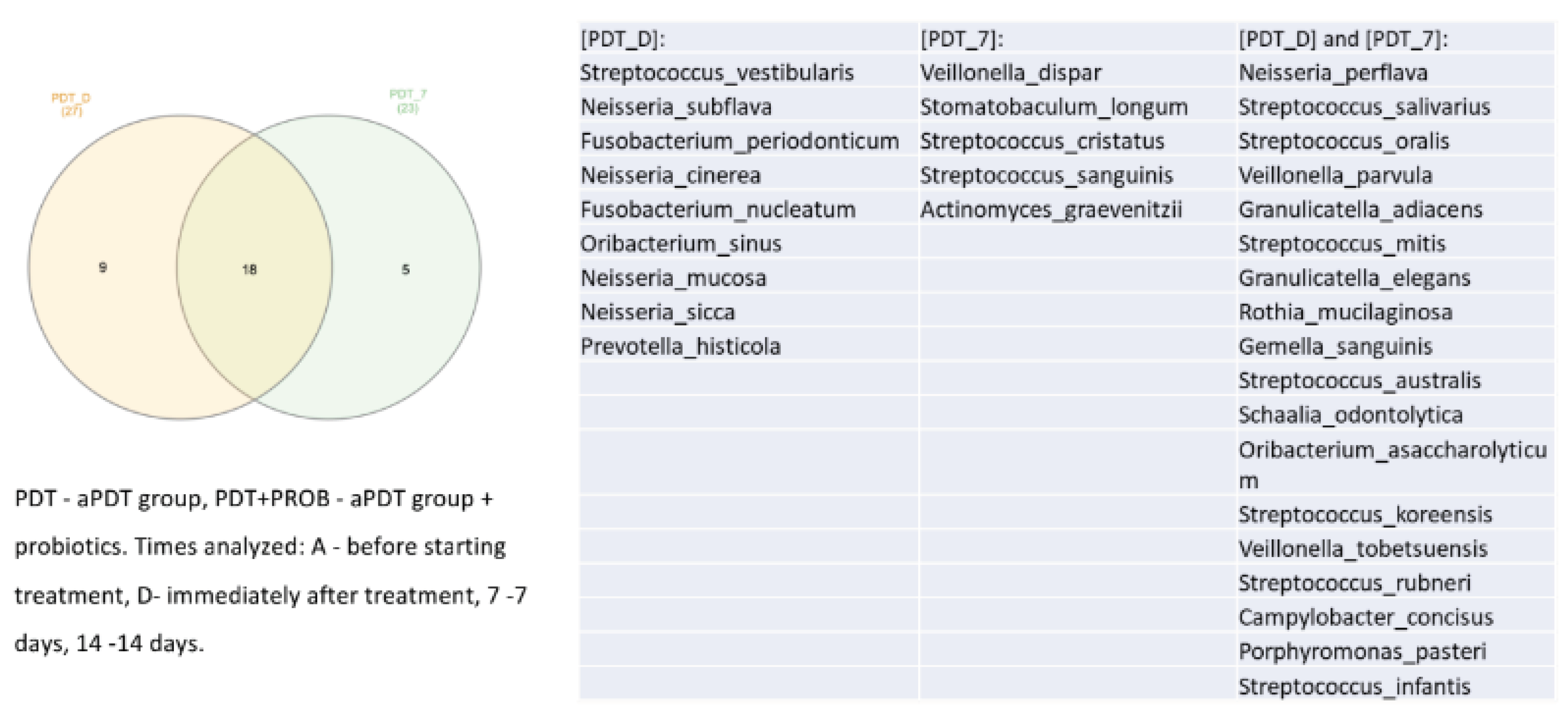
In the Venn diagram represented in
Figure 11, we can see that there was a decrease in the amount of species found when comparing the times immediately after treatment with aPDT and 7 days.
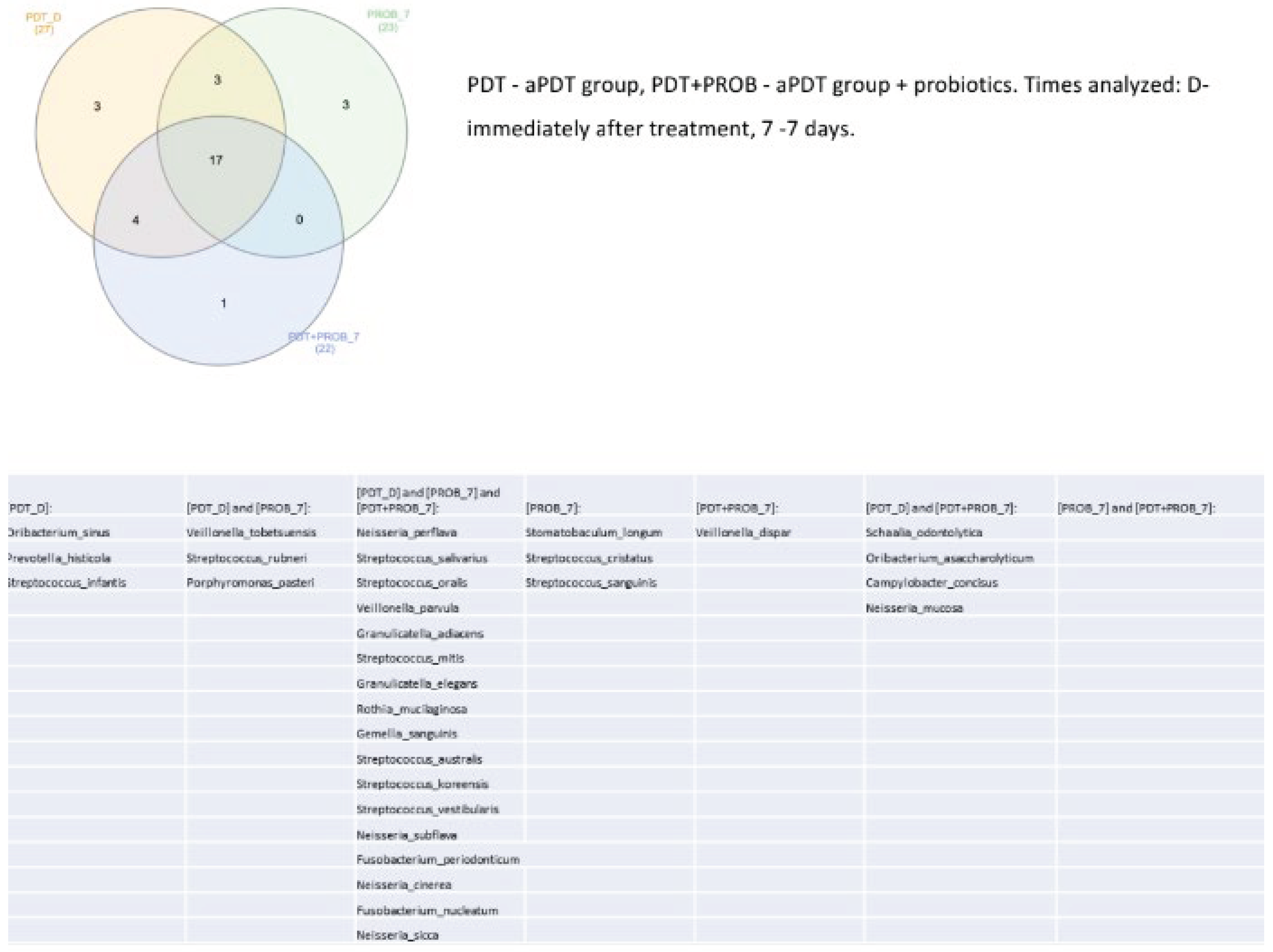
In the Venn diagram represented in
Figure 12, we can see that there was similarity of 17 species found at 7 days.
PDT - aPDT group, PDT+PROB - aPDT group + probiotics. Times analyzed: Dimmediately after treatment, 7 -7 days
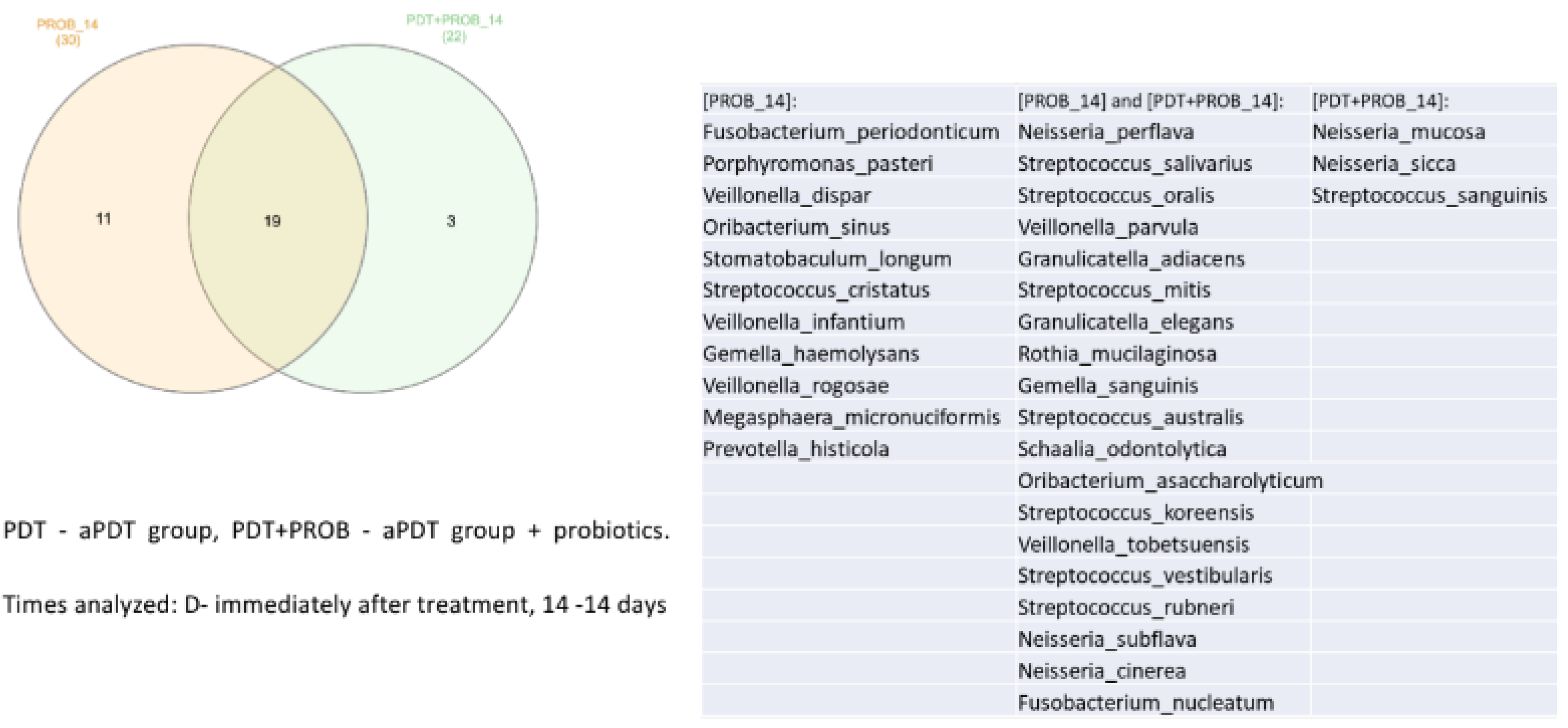
In the Venn diagram represented in
Figure 13, we can see that there was similarity of 19 species found at 14 days.
PDT - aPDT group, PDT+PROB – aPDT group + probiotics. Times analyzed: D- immediately after treatment, 14 -14 days.
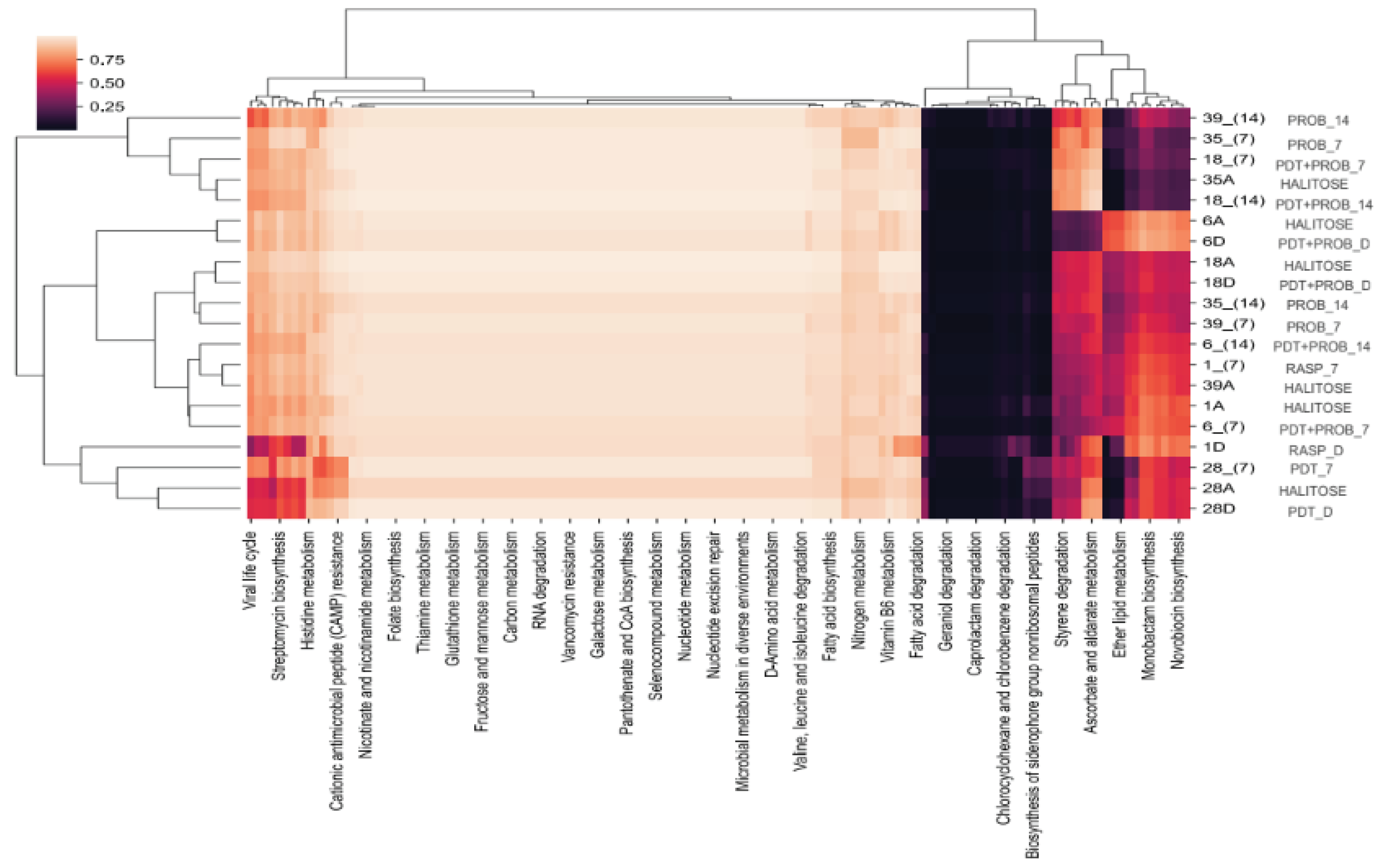
As for the prediction of metabolism, we can observe that there was no difference between the analyzed groups (p<0.05) (
Figure 14).
4. Discussion
The oral microbiota consists of 50 to 100 billion bacteria [
24,
25]. In 1963, Socransky et al. suggested that only 50% of the oral cavity microbiota had been cultured [
26,
27].
Recent work emphasizes that the oral microbiota can reach the intestine and throughout the body through blood circulation, potentially leading to numerous systemic diseases. This infiltration occurs through the junctional epithelium below the gingival sulcus, which is connected to the cementum by the hemidesmosome, which is weaker than the desmosome, becoming more permeable [
28].
Dysbiosis of the oral microbiota is the primary etiological factor of halitosis. Research began to study the relationship between the composition of the oral microbiome and systemic diseases instead of studying the pathogenicity of individual bacteria. Studies show that it is necessary to understand the specific mechanisms that regulate the balance of the oral microbiota for the development of prevention and treatment strategies for oral diseases and even systemic diseases [
29].
It is known that molecular techniques are more suitable for testing and evaluating the microbiome of the oral cavity [
24,
25] with qPCR and 16S rRNA amplicon sequencing being the most used [
30,
31,
32,
33].
In order to obtain an overview of the tongue microbiota at an ecological level, more recent work has carried out the sequencing of the 16S rRNA amplicon. These studies have shown that there is a prevalence of many other species in the development of halitosis [
2,
30,
31,
34]. It seems clear that a bacterial community is responsible for maintaining halitosis, and its treatment remains a challenge. In a published review [
31] the authors showed that the most prevalent genera in intraoral halitosis were Aggregatibacter, Capnocytophaga, Campylobacter, Clostridiales, Dialister, Leptotrichia, Prevotella, Peptostreptococcus, Peptococcus, Parvimonas, Selenomonas, Treponema and Tannerella. Other authors found Streptococcus, Veillonella, Gemella, Granulicatella, Neisseria, Haemophilus, Selenomonas, Fusobacterium, Leptotrichia, Prevotella, Porphyromonas and Lachnoanaerobaculum [
2]. Another study [
8] demonstrated that the genera Prevotella, Alloprevotella, Leptotrichia, Peptostreptococcus and Stomatobaculum exhibited higher relative percentages in halitosis samples, when 24 compared to healthy samples. In our work, the most abundant genera were Streptococcus, Neisseria, Veillonella, Granulicatella, Oribacterium, Gemella, Rothia, Fusobacterium, Schaalia, Prevotella, Campylobacter, Lanchnoanaerobaculum, Porphyromonas, Solobacterium, Leptotrichia, Stomatobaculum, Haemophilus, Enterococcus and Prevotellamassilia. Therefore, these results corroborate with other authors regarding genera: Campylobacter [
31], Leptotrichia [
8,
31], Prevotella [
2,
8,
31] Streptococcus, Neisseria, Veillonella, Granulicatella Fusobacterium, Lanchnoanaerobaculum, Porphyromonas Haemophilus, and Gemella [
2,
31].
As for the species, the most prevalent were Neisseria perflava, Streptococcus salivarius, Streptococcus oralis, Veillonella parvula, Granulicatella adiacens, Streptococcus mitis, Granulicatella elegans, Rothia micilaginosa, Gemella sanguis, Streptococcus australis, Schaalia odontolytica, Oribacterium, asaccharolyticum, Streptococcus koreensis tobeensis, Veilon, vestibular Streptococcus, Streptococcus sublava, Fusobacterium periodonticum, campylobacter concisus and Neisseria cirerea. They corroborate with other studies regarding the species Streptococcus mitis, [
35,
36] Fusobacterium periodonticum [
37], Streptococcus oralis, [
34] Streptococcus salivarius, [
34] Granulicatella elegans [
38].
In 2021, Zhang et al. [
1] conducted a study on the dynamism of the microbiota related to halitosis in children. 16S rRNA gene sequencing was also used to reveal the shift of the tongue coating microbiome in these children during a 12-month period. Halitosis enriched species Prevotella melaninogenica, Actinomyces sp._HMT_180 and Saccharibacteria TM7_G-1_bacterium_HMT_352 were finally selected as biomarkers in the halitosis-onset prediction model after screening, showing different types of species than the ones that were previoulsy more researched. In this study, the microbiome composition and relative abundance of the tongue coatings in the halitosis and control groups differed remarkably, even prior to the onset of the clinical manifestations of halitosis during the 12 months of the trial. These results suggest that as a preventive measure, the tongue coating plate control instructions can be done prior to the onset of halitosis. It is an interesting result, to which the authors could get once they used a group without halitosis, what was not done in our study, since we were testing treatment options.
Regarding the treatment options offered in our study, alternative options to conventional treatments were aPDT and probiotics. Several previous studies [
11,
14,
15,
16,
17,
18,
19,
20] demonstrated that, in gas chromatography analysis, aPDT was able to reduce CSV levels immediately, although this clinical success was not demonstrated in the analysis of the microbiome performed in the present study. The aPDT technique that was used was based on previous protocols and clinical trial studies [
18,
19]. In clinical studies with results, these were similar to our results regarding halimetry having only an immediate result. However, in these studies, unlike the present study, microbiological analyzes were not performed. In 2019 [
39], a systematic review was performed to summarize the evidence on the effect of probiotics on halitosis. Meta-analysis revealed that organoleptic assessment scores were significantly lower in subjects receiving probiotics than in placebo groups, but no significant difference was observed in VSC concentration, results similar to our sulfhydride and microbiome analysis. Another systematic review [
22], carried out in 2022, pointed out that the Lactobacillus species, also used in this study, is the most proposed for the treatment of halitosis. Both reviews agree on the fact that the available evidence is insufficient for recommending probiotics for oral malodor, requiring further clinical studies, such as the present study, in this area.
5. Conclusions
Increased knowledge of the microbiota of the oral cavity and especially of the lingual coating is essential to develop new strategies in the treatment of halitosis. Therefore, taking into account the limitations of this study, it can be concluded that treatment with aPDT or probiotics under these experimental conditions was not able to change the lingual coating microbiota of patients with halitosis. More research is needed to better understand the behavior of the oral microbiome in the presence of halitosis and the effectiveness of new treatments to be proposed.
Author Contributions
Conceptualization, PBM and MLLG; methodology, SKB and ACRTH; validation, RAMF; formal analysis, LJM and APTS; investigation, APTS; resources, SKB and PBM; data curation, LJM; writing—original draft preparation, PBM and MLLG; writing—review and editing, PBM and MLLG; visualization, SKB and DCA; supervision, KPSF, RAMF and SKB; project administration, SKB, EMS and CD; funding acquisition, SKB and PBM. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) grant number 2019/14229-6 and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) 306577/2020-8. It was also financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance code 001.
Institutional Review Board Statement
The project was approved by the Ethics Committee of Universidade Nove de Julho, under process number 20123519.4.0000.5511 (CAAE) and feedback number 3669442. Informed consent was obtained in written form from participants through an informed consent form.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is available upon request to interested researchers.
Acknowledgments
The authors would like to thank Universidade Nove de Julho for the support.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Zhang, Y.; Zhu, C.; Cao, G.; Zhan, J.; Feng, X.; Chen, X. Dynamic Alterations of Oral Microbiota Related to Halitosis in Preschool Children. Front. Cell. Infect. Microbiol. 2021, 11, 599467. [Google Scholar] [CrossRef] [PubMed]
- Hampelska, K.; Jaworska, M.M.; Babalska, Z.Ł.; Karpiński, T.M. The Role of Oral Microbiota in Intra-Oral Halitosis. J. Clin. Med. 2020, 9, 2484. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Izidoro, C.; Botelho, J.; Machado, V.; Reis, A.M.; Proença, L.; Alves, R.C.; Mendes, J.J. Revisiting Standard and Novel Therapeutic Approaches in Halitosis: A Review. Int. J. Environ. Res. Public Health 2022, 19, 11303. [Google Scholar] [CrossRef] [PubMed]
- BOLL, ENCurd ML; BEIKLER, Thomas. Halitosis: the multidisciplinary approach. International journal of oral science 2012, 4, 55–63. [CrossRef] [PubMed]
- Hou, K.; Wu, Z.X.; Chen, X.Y.; Wang, J.Q.; Zhang, D.; Xiao, C.; Zhu, D.; Koya, J.B.; Wei, L.; Li, J.; Chen, Z.S. Microbiota in health and diseases. Signal Transduct Target Ther. 2022, 7, 135. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Chung, S.W.; Auh, Q.S.; Hong, S.J.; Lee, Y.A.; Jung, J.; Lee, G.J.; Park, H.J.; Shin, S.I.; Hong, J.Y. Progress in Oral Microbiome Related to Oral and Systemic Diseases: An Update. Diagnostics 2021, 11, 1283. [Google Scholar] [CrossRef] [PubMed]
- Marsh, P.D.; Zaura, E. Dental biofilm: ecological interactions in health and disease. J. Clin. Periodontol. 2017, 44, S12–S22. [Google Scholar] [CrossRef] [PubMed]
- Ye, W.; Zhang, Y.; He, M.; Zhu, C.; Feng, X.-P. Relationship of tongue coating microbiome on volatile sulfur compounds in healthy and halitosis adults. J. Breath Res. 2019, 14, 016005. [Google Scholar] [CrossRef]
- Zanetti, F.; Semren, T.Z.; Battey, J.N.D.; Guy, P.A.; Ivanov, N.V.; van der Plas, A.; Hoeng, J. A Literature Review and Framework Proposal for Halitosis Assessment in Cigarette Smokers and Alternative Nicotine-Delivery Products Users. Front. Oral Health 2021, 2, 777442. [Google Scholar] [CrossRef]
- Conceicao, M. Diagnostic Technique for Assessing Halitosis Origin Using Oral and Nasal Organoleptic Tests, Including Safety Measures Post Covid-19. J. Dent. Oral Sci. 2020, 2, 1–19. [Google Scholar] [CrossRef]
- Motta, P.d.B.; Motta, L.J.; Campos, T.M.; Gonçalves, M.L.L.; Santos, E.M.; Martimbianco, A.L.C.; de Andrade, D.J.C.; Mesquita-Ferrari, R.A.; Fernandes, K.P.S.; Horliana, A.C.R.T.; et al. Effect of Photodynamic Therapy on Halitosis: A Systematic Review of Randomized Controlled Trials. Sensors 2022, 22, 469. [Google Scholar] [CrossRef]
- Porter, S.R.; Scully, C. Oral malodour (halitosis). BMJ 2006, 333, 632–635. [Google Scholar] [CrossRef]
- Kara, C.; Tezel, A.; Orbak, R. Effect of oral hygiene instruction and scaling on oral malodour in a population of Turkish children with gingival inflammation. Int. J. Paediatr. Dent. 2006, 16, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.G.; de Santi, M.E.S.O.; Franco, B.E.; Deana, A.M.; Prates, R.A.; França, C.M.; Fernandes, K.P.S.; Ferrari, R.A.M.; Bussadori, S.K. Photodynamic therapy as novel treatment for halitosis in adolescents: a case series study. J. Lasers Med. Sci. 2014, 5, 146. [Google Scholar]
- Lopes, R.G.; da Mota, A.C.C.; Soares, C.; Tarzia, O.; Deana, A.M.; Prates, R.A.; França, C.M.; Fernandes, K.P.S.; Ferrari, R.A.M.; Bussadori, S.K. Immediate results of photodynamic therapy for the treatment of halitosis in adolescents: a randomized, controlled, clinical trial. Lasers Med Sci. 2015, 31, 41–47. [Google Scholar] [CrossRef]
- Costa da Mota, A.C.; França, C.M.; Prates, R.; Deana, A.M.; Santos, L.C.; Garcia, R.L.; Gonçalves, M.L.L.; Ferrari, R.A.M.F.; Fernandes, K.P.S.; Bussadori, S.K. Effect of photodynamic therapy for the treatment of halitosis in adolescents–a controlled, microbiological. Clin. Trial. J. Biophotonics 2016, 9, 1337–1343. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, M.L.L.; Bussadori, S.K.; Fragoso, Y.D.; da Silva, V.V.B.; Deana, A.M.; da Mota, A.C.C.; Pinto, E.H.; Horliana, A.C.R.; França, C.M. Effect of photodynamic therapy in the reduction of halitosis in patients with multiple sclerosis: clinical trial. J. Breath Res. 2017, 11, 046006. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, M.L.L.; da Mota, A.C.C.; Deana, A.M.; Guedes, G.H.; Cavalcante, L.A.d.S.; Prates, R.A.; Horliana, A.C.R.T.; Pavani, C.; Motta, L.J.; Bitencourt, G.d.B.; et al. Photodynamic therapy with Bixa orellana extract and LED for the reduction of halitosis: study protocol for a randomized, microbiological and clinical trial. Trials 2018, 19, 590. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, M.L.L.; Costa da Mota, A.C.; Deana, A.M.; Cavalcante, L.A.S.; Horliana, A.C.R.T.; Pavani, C.; Motta, L.J.; Fernandes, K.P.S.; Mesquita-Ferrari, R.A.; da Silva, D.F.T.; Motta, P.B.; Prates, R.A.; Bussadori, S.K. Antimicrobial photodynamic therapy with Bixa orellana extract and blue LED in the reduction of halitosis – A randomized, controlled clinical trial. Photodiagnosis Photodyn. Ther. 2020, 30, 101751. [Google Scholar] [CrossRef]
- Costa da Mota, A.C.; Gonçalves, M.L.L.; Horliana, A.C.R.T.; Deana, A.M.; Cavalcante, L.A.S.; Gomes, A.O.; Mayer, M.P.A.; Suguimoto, E.S.A.; Fernandes, K.P.S.; Mesquita-Ferrari, R.A.; Prates, R.A.; Motta, L.J.; Bussadori, S.K. Effect of antimicrobial photodynamic therapy with red led and methylene blue on the reduction of halitosis: controlled microbiological clinical trial. Lasers Med Sci 2021, 21. [Google Scholar] [CrossRef]
- Iwamoto, T.; Suzuki, N.; Tanabe, K.; Takeshita, T.; Hirofuji, T. Effects of probiotic Lactobacillus salivarius WB21 on halitosis and oral health: an open-label pilot trial. Oral Surgery, Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 110, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Park, D.-Y.; Park, J.Y.; Lee, D.; Hwang, I.; Kim, H.-S. Leaky Gum: The Revisited Origin of Systemic Diseases. Cells 2022, 11, 1079. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.; Cheng, L.; You, Y.; Tang, C.; Ren, B.; Li, Y.; Xu, X.; Zhou, X. Oral microbiota in human systematic diseases. Int. J. Oral Sci. 2022, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- López-Valverde, N.; López-Valverde, A.; de Sousa, B.M.; Rodríguez, C.; Suárez, A.; Aragoneses, J.M. Role of Probiotics in Halitosis of Oral Origin: A Systematic Review and Meta-Analysis of Randomized Clinical Studies. Front. Nutr. 2022, 8, 787908. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Ueda, T.; Sakurai, K. New method for evaluation of tongue-coating status. J. Oral Rehabil. 2007, 34, 442–447. [Google Scholar] [CrossRef] [PubMed]
- HOMD: Human Oral Microbiome Database. Available online: http://www.homd.org/ (accessed on 19 June 2020).
- Krishnan, K.; Chen, T.; Paster, B. A practical guide to the oral microbiome and its relation to health and disease. Oral Dis. 2016, 23, 276–286. [Google Scholar] [CrossRef]
- Socransky, S.; Gibbons, R.; Dale, A.; Bortnick, L.; Rosenthal, E.; Macdonald, J. The microbiota of the gingival crevice area of man—I: Total microscopic and viable counts and counts of specific organisms. Arch. Oral Biol. 1963, 8, 275–280. [Google Scholar] [CrossRef]
- Olsen, I.; Preza, D.; Aas, J.A.; Paster, B.J. Cultivated and not-yet-cultivated bacteria in oral biofilms. Microb. Ecol. Health Dis. 2009, 21, 65–71. [Google Scholar] [CrossRef]
- Takeshita, T.; Suzuki, N.; Nakano, Y.; Yasui, M.; Yoneda, M.; Shimazaki, Y.; Hirofuji, T.; Yamashita, Y. Discrimination of the oral microbiota associated with high hydrogen sulfide and methyl mercaptan production. Sci. Rep. 2012, 2, 215. [Google Scholar] [CrossRef]
- Seerangaiyan, K.; van Winkelhoff, A.J.; Harmsen, H.J.M.; A Rossen, J.W.; Winkel, E.G. The tongue microbiome in healthy subjects and patients with intra-oral halitosis. J. Breath Res. 2017, 11, 036010. [Google Scholar] [CrossRef]
- Bernardi, S.; Karygianni, L.; Filippi, A.; Anderson, A.C.; Zürcher, A.; Hellwig, E.; Vach, K.; Macchiarelli, G.; Al-Ahmad, A. Combining culture and culture-independent methods reveals new microbial composition of halitosis patients' tongue biofilm. Microbiologyopen 2019, 9, e958. [Google Scholar] [CrossRef] [PubMed]
- Yitzhaki, S.; Reshef, L.; Gophna, U.; Rosenberg, M.; Sterer, N. Microbiome associated with denture malodour. J. Breath Res. 2018, 12, 027103. [Google Scholar] [CrossRef] [PubMed]
- Ren, W.; Zhang, Q.; Liu, X.; Zheng, S.; Ma, L.; Chen, F.; Xu, T.; Xu, B. Supragingival Plaque Microbial Community Analysis of Children with Halitosis. J. Microbiol. Biotechnol. 2016, 26, 2141–2147. [Google Scholar] [CrossRef] [PubMed]
- Ademovski, S.E.; Persson, G.R.; Winkel, E.; Tangerman, A.; Lingström, P.; Renvert, S. The short-term treatment effects on the microbiota at the dorsum of the tongue in intra-oral halitosis patients—a randomized clinical trial. Clin. Oral Investig. 2012, 17, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Riggio, M.P.; Lennon, A.; Rolph, H.J.; Hodge, P.J.; Donaldson, A.; Maxwell, A.J.; Bagg, J. Molecular identification of bacteria on the tongue dorsum of subjects with and without halitosis. Oral Dis. 2008, 14, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Persson, S.; Edlund, M.; Claesson, R.; Carlsson, J. The formation of hydrogen sulfide and methyl mercaptan by oral bacteria. Oral Microbiol. Immunol. 1990, 5, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Haraszthy, V.I.; Zambon, J.J.; Sreenivasan, P.K.; Zambon, M.M.; Gerber, D.; Rego, R.; Parker, C. Identification of oral bacterial species associated with halitosis. J. Am. Dent. Assoc. 2007, 138, 1113–1120. [Google Scholar] [CrossRef]
- Yoo, J.-I.; Shin, I.-S.; Jeon, J.-G.; Yang, Y.-M.; Kim, J.-G.; Lee, D.-W. The Effect of Probiotics on Halitosis: a Systematic Review and Meta-analysis. Probiotics Antimicrob. Proteins 2017, 11, 150–157. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).