1. Introduction
The World Health Organization (WHO) has reported that more than 120 million people are affected by filariasis, a mosquito-borne disease [
1].
Dirofilaria immitis and
Dirofilaria repens are the main causative agents of dirofilariosis disease and subcutaneous dirofilariasis [
2]. Transmission of
Dirofilaria repens, also known as
D. repens, occurs mainly through mosquito bites, particularly transmitted by the
Aedes caspius mosquito [
3].
D. repens is a type of subcutaneous nematode that is characteristic of dogs and cats, but can also be transmitted to humans, causing an infectious condition called dirofilariasis. This infection is generally located in the upper areas of the body, but can also affect the male and female genitals, lungs or other internal organs [
4].
Dirofilariasis caused by
D. repens is more common in the ocular area, but the parasite has the ability to migrate to other regions of the body. It is estimated that its migration speed is about 30 centimetres in just two days, and previous research has reported significant migration between different parts of the body [
5].
It is crucial to raise awareness among healthcare professionals about infections caused by
Dirofilaria species [
6]. Surgeons might initially mistake dirofilariasis as a malignancy if they are unfamiliar with this infection, which could cause significant distress to patients. To accurately diagnose dirofilariasis, it is important to possess knowledge regarding the typical location and migration patterns of the nematode, take into account the patient’s travel history, and recognize the clinical symptoms associated with the infection [
7].
Differentiation of
Dirofilaria species from other nematodes is primarily based on morphological analysis, which includes the use of light microscopy, scanning electron microscopy and/or DNA-based analysis [
8]. Diagnosis of this condition is usually established by microscopic and macroscopic examination of the worm or by histopathological analysis, which reveals the presence of a thick, multilayered cuticle [
9]. In addition, high-resolution ultrasound imaging proves useful in detecting parasite movement within subcutaneous nodules. Treatment of subcutaneous dirofilariasis usually requires excision of the nematode or surgical removal of the nodule [
10].
In literature few cases of parasitic cysts caused by
D. repens located in the zygomatic region are reported [
1]. Our report presents an unusual clinical case of a patient diagnosed with a cystic outgrowth with parasitic origin in the right genian region in the context of dirofilariosis disease caused by
D. repens, treated in the Oral and Maxillo-facial Surgery Clinic of the “St. Spiridon” Emergency Clinical Hospital of Iasi, Romania.
2. Case Report
A 29-year-old male patient with no medical history, farm worker, was hospitalized in the Clinic of Oral and Maxillo-facial Surgery of “St. Spiridon” Emergency Clinical Hospital of Iasi, Romania, for the diagnosis and treatment of a facial asymmetry localized in the right genian region (
Figure 1). The patient declared that the swelling had a slow growth without producing sensitivity alterations of the infraorbital nerve or functional disorders. The patient could not specify any past facial trauma.
To evaluate the swelling located in the right genian region clinical examination associated with ultrasound investigation was realized. The outgrowth was covered by a normal and unmodified skin. Through clinical examination, an oval, mobilizable and painless formation with a diameter of 18/15/10 mM with a firm-elastic consistency was identified (
Figure 2).
No cervical or general limphadenopathy was detected. Through ultrasound scanning of the genian region was detected a well-defined round hypoechogenic lesion that included a moving tubular structure with a length of 10mM and a width of 1mM (
Figure 3 and Figure 4).
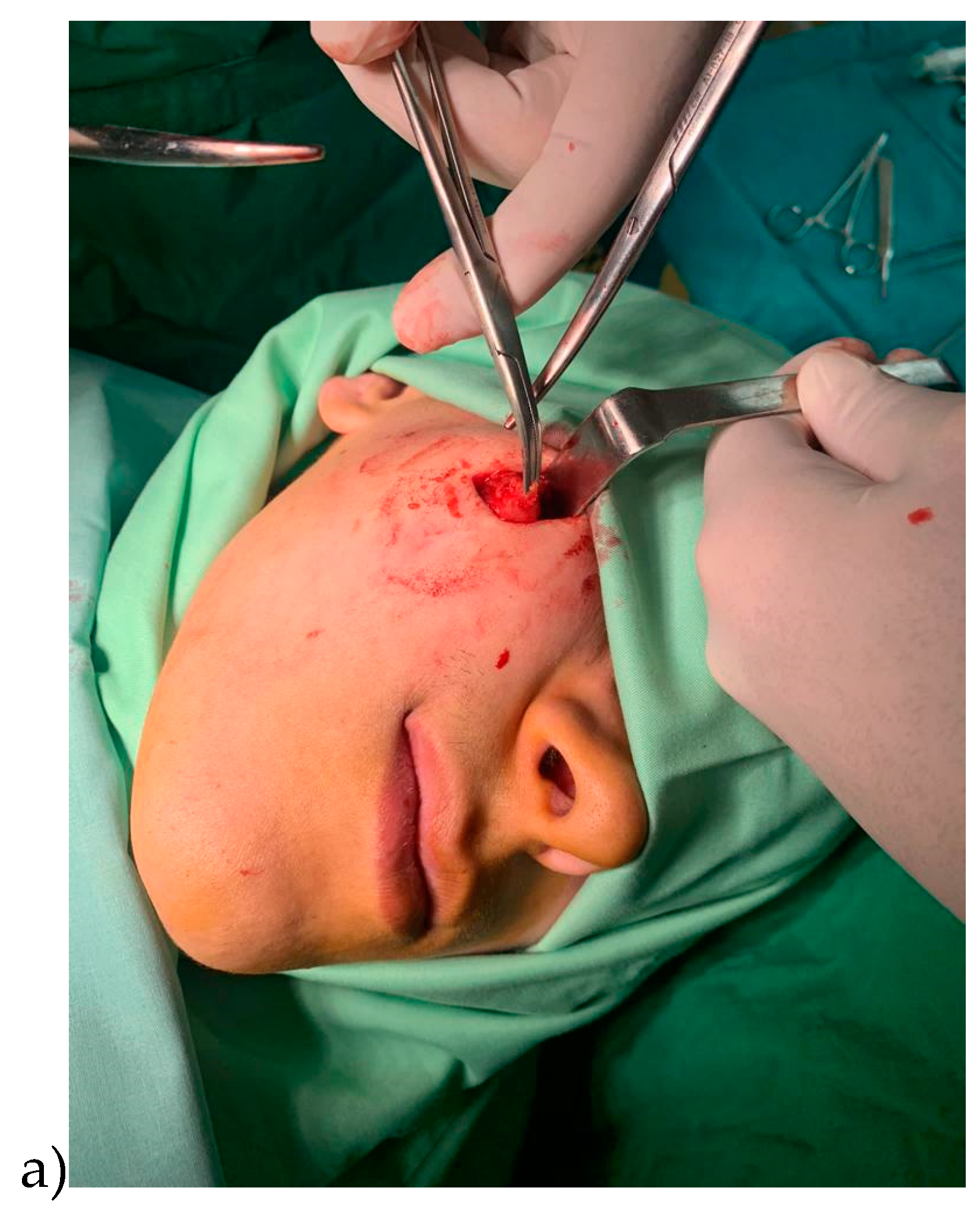
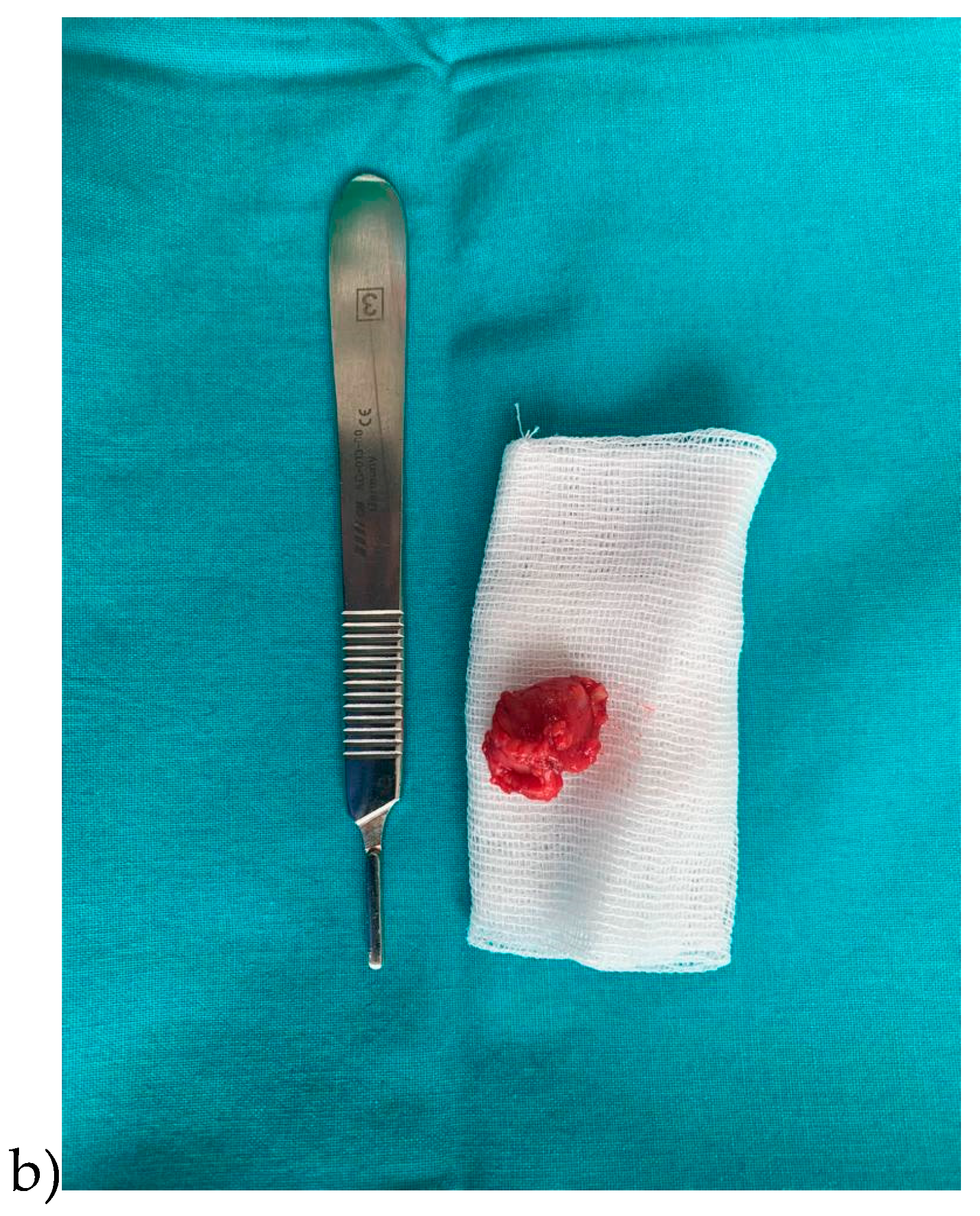
Following the clinical and ultrasound examination, the surgical team decided to remove the outgrowth through classical surgical treatment, thus the incision was made, followed by the excision of the entirely cystic formation without being damaged (
Figure 5a,b).
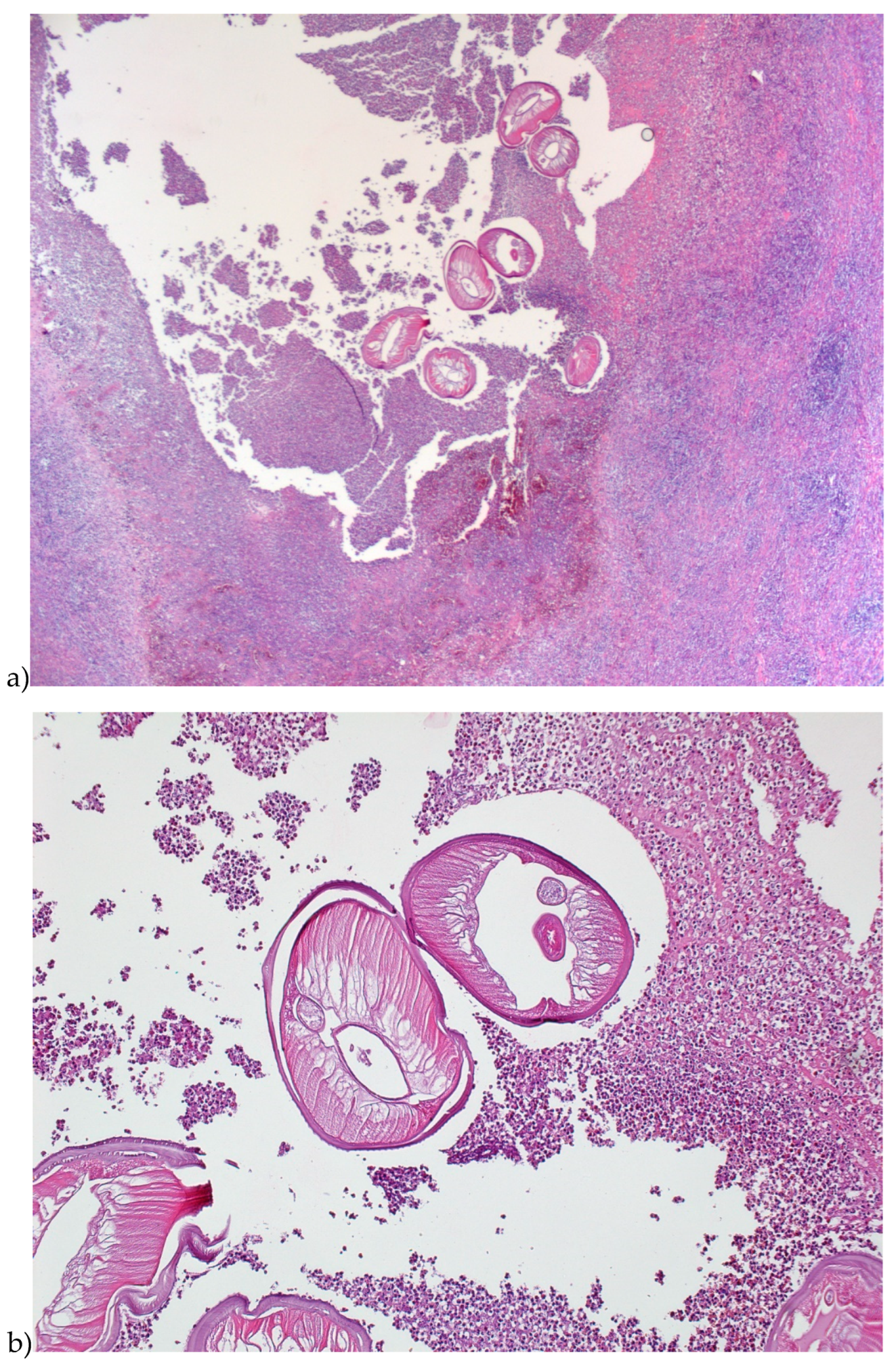
Histological examination of the excison piece revealed at macroscopic level a cystic cavity with liquid content and a filamentous structure of approximately 10 mM length and 1 mM thickness (
Figure 6).
At microscopic point, was identified, an abscess with a wall consisting of maturing granulation tissue with peripheral fibrosis and polymorphous inflammation associating lymphocytes, plasmocytes, eosinophils, polymorphonuclears and histocytes, some multinucleated, could be observed. The macroscopically observed filamentous structure was represented by a nematode mark off in the periphery by a cuticle with a discrete scalloped relief. (
Figure 7;)
From a morphopathologically point of view, the morphological aspects correspond to a parasitic cyst in the context of dirofilariosis disease, the external structure of the parasite suggesting D. repens.
Following the surgical excision, only prophylactic antibiotherapy was given, considering that the cystic outgrowth completely removed. No specific antiparasitic medication was necessary.
3. Discussion
Human nematode infections, although not very common, show an increasing trend, WHO statistics show that they affect approximately 90 million people worldwide [
1].
D. repens is a nematode that is localized subcutaneously, found especially in dogs and cats in Europe, Africa and Asia that can be transmitted to humans through mosquito bites [
11]. The infection has a predominant localization in the upper areas of the body in a percentage of 75.8%, but also in the male and female genital organs in a percentage of 6.5% or in the female breast in 5.4% of cases [
1,
11]. Among the infections appearing in the upper part of the body, 30.5% were reported as being localized in the eye region, but due to the movable character of the parasite, their location can change [
1,
12].
Dirofilariosis parasites are transmitted by insects such as
Aedes caspius mosquitoes which have the ability to travel long distances and bite during the entire day [
1,
13]. One study showed that 1.5% of this mosquito species contains
D. repens DNA [
14]. A previous paper reported the interesting cases of some patients that accused the existence of a worm under the skin, and the initial diagnosis was of illusory parasitosis, later was proved the presence of a movable nematode [
13]. The infection with the parasite
D. repens can be manifested by the appearance of a subcutaneous swelling with slow evolution, located predominantly in the eye area [
11]. Due to the localization and the slowly evolving and painless character, it can be confused with a benign tumor such as adenoma, mucocele or lipoma [
15].
This paper reports the case of a 29-year-old patient with no general medical conditions presenting a painless swelling in the right zygomatic region secondary to infection with the parasite
D. repens. Following the analysis of the literature, it can be affirmed that this is the first case of a parasitic cyst caused by
D. repens infection localized in the genian region reported in Romania [
16,
17,
18,
19].
Treatment against dirofilariosis is exclusively surgical consisting in the removal of the cystic outgrowth alongwith the parasite. Previous articles report a failure rate of surgical treatment of 5% [
15,
20]. Prevention of infection is performed by protection against mosquito bites and desinfestation of pets [
1]. In the case of migratory parasitic cysts, the administration of anthelmintic drugs is recommended to reduce the motility of the nematode and the creation of a fixed structure that can be removed [
7].
Although in other case reports patients infected with
D repens stated that prior to contact with the parasite they had traveled to areas such as Croatia, France, Italy, Russia or Sri Lanka. In our case report the patient had not traveled in recent years and had not reported any trauma in the antecedents [
6,
8,
21,
22,
23].
4. Conclusions
The presented case report demonstrates that dirofialriosis can be located in other areas outside the eye region. Dirofilariosis caused by Dirofilaria repens should also be suspected in geographic regions that are not considered endemic as long as a patient presents the specific symptoms. Surgical excision of the parasitic cyst and Dirofilaria repens are sufficiently to ensure healing.
Author Contributions
Conceptualization: A.N. and V.V.C. methodology, F.S.; software, F.P.S; validation, D.F., D.D. and M.L.C; formal analysis, A.N.; investigation, F.P.S; resources, A.N.; data curation, F.P.S; writing—original draft preparation, A.N, F.P.S.; writing—review and editing, A.N, F.S visualization, M.L.C.; supervision, V.V.C.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
Not applicable
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chan, C.; Kermanshahi, M.; Mathew, B.; England, R. A rare case of Dirofilaria repens infection. J. Laryngol. Otol. 2013, 127, 607–609. [Google Scholar] [CrossRef]
- Latifoglu, O.; Zmen, S.; Sezer, C. Dirofilaria repenspresenting as a premasseteric nodule. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 217–220. [Google Scholar] [CrossRef]
- Ganushkina, L.A.; Rakova, V.M.; Ivanova, I.B.; Supriaga, V.G.; Sergiev, V.P. Entomological monitoring of an area to assess Dirofilaria transmission risk. Med. Parazitol. (Mosk). 2014, 3, 9–12. [Google Scholar]
- Kondrashin, A.V.; Morozova, L.F.; Stepanova, E.V.; Turbabina, N.A.; Maksimova, M.S.; Morozov, E.N. Anthology of Dirofilariasis in Russia (1915-2017). Pathogens 2020, 9, 275. [Google Scholar] [CrossRef]
- Antolová, D.; Miterpakova, M.; Paralicova, Z. Case of human Dirofilaria repens infection manifested by cutaneous larva migrans syndrome. Parasitol. Res. 2015, 114, 2969–2973. [Google Scholar] [CrossRef]
- Mendoza-Roldan, J.A.; Gabrielli, S.; Cascio, A.; Manoj, R.R.; Bezerra-Santos, M.A.; Benelli, G.; Brianti, E.; Latrofa, M.S.; Otranto, D. Zoonotic Dirofilaria immitis and Dirofilaria repens infection in humans and an integrative approach to the diagnosis. Acta Trop. 2021, 223, 106083. [Google Scholar] [CrossRef]
- Mistry, M.A.; Hoejvig, J.; Helleberg, M.; Stensvold, C.R.; Jokelainen, P.; Noehr, A.; Bonde, C. Human subcutaneous dirofilariasis: the ‘migrating’ skin tumor. Case Reports Plast Surg Hand Surg. 2021, 8, 181–185. [Google Scholar] [CrossRef]
- Rose, R.; Kleitsch, K.U.; Born, D.; Heye, P. Dirofilaria repens in a Pediatric Patient—First Case Report from Switzerland. Eur. J. Pediatr. Surg. 2023, 11, 29–31. [Google Scholar] [CrossRef] [PubMed]
- Melasom, H.A.; Kurtzhals, J.A.L.; Qvortrup, K.; Bargum, R.; Barfod, T.S.; la Cour, M.; Heegaard, S. Subconjunctival Dirofilaria repens Infestation: A Light and Scanning Electron Microscopy Study. Open Ophtalmol. J. 2011, 5, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Lindner, A.K.; Tappe, D.; Gertler, M.; Equihua Martinez, G.; Richter, J. A live worm emerging from the eyelid. J. Travel Med. 2018, 25, 66. [Google Scholar] [CrossRef] [PubMed]
- Pampiglione, S.; Rivasi, F. Human dirofilariasis due to Dirofilaria (Nochtiella) repens: an update of world literature from 1995 to 2000. Parassitologia 2000, 42, 231–54. [Google Scholar]
- Permi, H.S.; Veena, S.; Prasad, H.K.; Kumar, Y.S.; Mohan, R.; Shetty, K.J. Subcutaneous human dirofilariasis due to Dirofilaria repens:report of two cases. J. Glob. Infect. Dis. 2011, 3, 199–201. [Google Scholar]
- Jelinek, T.; Schulte-Hillen, J.; Loscher, T. Human dirofilariasis. Int. J. Dermatol. 1996, 35, 872–5. [Google Scholar] [CrossRef]
- Tahir, D.; Bittar, F.; Barré-Cardi, H.; Sow, D.; Dahmani, M.; Mediannikov, O.; Raoult, D.; Davoust, B.; Parola, P. Molecular survey of Dirofilaria immitis and Dirofilaria repens by new realtime TaqMan PCR assay in dogs and mosquitoes (Diptera: Culicidae) in Corsica (France). Vet. Parasitol. 2017, 235, 1–7. [Google Scholar] [CrossRef]
- Skrinjar, I.; Brailo, V.; Loncar Brzak, B.; Lozic Erent, J.; Bukovski, S.; Juras, D.V. Live Intraoral Dirofilaria repens of Lower Lip Mimicking Mucocele—First Reported Case from Croatia. Int. J. Environ. Res. Public Health. 2022, 19, 4330. [Google Scholar] [CrossRef]
- Arbune, M.; Dobre, M. Dirofilariasis - an emergent human parasitosis in Romania. Acta Parasitol. 2015, 60, 485–7. [Google Scholar] [CrossRef]
- Ciuca, L.; Simòn, F.; Rinaldi, L.; Kramer, L.; Genchi, M.; Cringoli, G.; Acatrinei, D.; Miron, L.; Morchon, R. Seroepidemiological survey of human exposure to Dirofilaria spp. in Romania and Moldova. Acta Trop. 2018, 187, 169–74. [Google Scholar] [CrossRef] [PubMed]
- Mănescu, R.; Bărăscu, D.; Mocanu, C.; Pîrvănescu, H.; Mîndriă, I.; Bălăşoiu, M.; Turculeanu, A. Subconjunctival nodule with Dirofilaria repens. Chirurgia (Bucur). 2009, 104, 95–97. [Google Scholar] [PubMed]
- Popescu, I.; Tudose, I.; Racz, P.; Muntau, B.; Giurcaneanu, C.; Poppert, S. Human Dirofilaria repens Infection in Romania: A Case Report. Case. Rep. Infect. Dis. 2012, 472976. [Google Scholar]
- Nissen, T.; Wynn, R. The clinical case report: A review of its merits and limitations. BMC Res. Notes 2014, 7, 264. [Google Scholar] [CrossRef]
- Simon, F.; Siles-Lucas, M.; Morchon, R. Human and animal dirofilariasis: the emergence of a zoonotic mosaic. Clin. Microbiol. Rev. 2012, 25, 507–44. [Google Scholar] [CrossRef]
- Salamatin, R.V.; Pavlikovska, T.M.; Sagach, O.S.; et al. Human dirofilariasis due to dirofilaria repens in Ukraine, an emergent zoonosis: epidemiological report of 1465 cases. Acta Parasitol. 2013, 58, 592–8. [Google Scholar] [CrossRef]
- Hennocq, Q.; Helary, A.; Debelmas, A.; Monsel, G.; Labat, A.; Bertolus, C.; Martin, C.; Caumes, E. Oral migration of Dirofilaria repens after creeping dermatitis. Parasite. 2020, 27. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).