1. Introduction
Childhood obesity is a critical public health concern that has become increasingly prevalent, posing significant risks for chronic physical and mental health conditions [
1]. This complex condition is influenced by an interplay of genetic, environmental, and behavioral factors, with emerging research highlighting the substantial impact of psychological health on a child's risk of developing obesity [
2]. The present study aims to dissect this intricate relationship by examining psychological predictors of childhood obesity, with a unique focus on how these factors interact across different developmental stages.
The psychological landscape of childhood obesity is nuanced, with various factors such as self-esteem, body image, and emotional regulation playing critical roles in children's eating behaviors and physical activity levels [
3]. However, despite the known associations between psychological distress and obesity, there is a lack of research systematically analyzing these factors through the developmental trajectory of childhood [
4]. This research gap underscores the need for a study that not only identifies psychological predictors of obesity but also understands how they manifest and evolve from early childhood to adolescence.
Accordingly, this study is designed to fill the existing gap by investigating the psychological determinants of obesity in a developmental context. The objectives are to delineate the psychological characteristics that correlate with obesity and to track these associations through the critical stages of child development. Such an approach is critical for developing age-appropriate interventions and could have far-reaching implications for pediatric health care [
5].
The literature points to a bidirectional relationship between obesity and psychological health, with obesity increasing the risk of psychological issues and vice versa [
6]. Our study draws from this existing knowledge base, aiming to expand on it by using longitudinal data to trace the progression of psychological factors and their influence on body weight throughout childhood. This longitudinal aspect is vital, as it allows for the observation of how early psychological patterns may predict later obesity, potentially offering new insights into critical periods for intervention [
7].
Psychological factors such as stress, anxiety, and depression have been shown to contribute to the development of obesity, often through mechanisms like emotional eating and reduced physical activity [
8]. Yet, the impact of these factors may vary by developmental stage due to the evolving cognitive, emotional, and social capacities of children as they grow [
9]. Recognizing these developmental differences is essential for tailoring interventions that are developmentally appropriate and thus more likely to be effective.
In addressing these issues, the study utilizes a bioinformatic approach to analyze complex datasets, applying advanced statistical methods to unravel the relationships between psychological health and obesity across different ages [
10]. By situating the research within the broader context of bioinformatics and public health, this study not only seeks to elucidate the psychological aspects of childhood obesity but also to offer a data-driven foundation for future interventions [
11]. The expected outcomes include the identification of psychological markers that could serve as targets for early prevention efforts, thus contributing to the overarching goal of reducing the prevalence and impact of childhood obesity [
12].
In sum, this introduction lays the groundwork for a comprehensive analysis of the psychological determinants of childhood obesity, viewed through the lens of developmental stages. The findings from this research are anticipated to provide valuable insights for healthcare professionals and policymakers, informing strategies to combat the childhood obesity epidemic with a heightened awareness of the psychological dimensions involved [
13].
The escalating issue of childhood obesity extends beyond individual choices, deeply influenced by environmental factors. This research suggests that psychological factors such as affect dysregulation and attachment styles play a pivotal role in determining the risk of obesity in children. It aims to explore these psychological aspects and to uncover their significant, yet often overlooked, impact on child health.
Affect dysregulation, referring to the ability to regulate emotional responses, can indirectly influence children's eating habits and stress management, which are closely linked to weight gain. Similarly, issues related to attachment anxiety and avoidance could lead to unhealthy eating behaviors and lifestyle choices in children. These psychological factors are believed to have varying effects throughout different stages of childhood and adolescence.
The study utilizes advanced bioinformatics tools to analyze complex data sets that include psychological evaluations and biometric measurements. This method will help identify patterns and correlations not easily detected through conventional statistical analysis. By applying bioinformatics, the research aims to offer a comprehensive perspective on how psychological health impacts and possibly forecasts obesity risk in children.
By bridging psychological constructs with physical health outcomes, the research is positioned to offer new perspectives on the prevention and management of childhood obesity. It stands to inform intervention strategies that can be implemented by healthcare professionals, targeting not just the children in clinical settings but also supporting parents in cultivating a home environment conducive to psychological and physical well-being.
2. Materials and Methods
This is an ongoing cross-sectional study of a pediatric clinical population conducted by the Child and Adolescent Psychiatric Department in collaboration with the Endocrinology Outpatient Clinic and the Pediatric Clinic of Penteli General Children’s Hospital. This study explored the links between psychological well-being and body weight among a diverse cohort of children aged 5-16 years. Our participants were divided into two groups based on their Body Mass Index (BMI): one consisting of overweight and obese children (experimental group) and the other comprising children with a BMI within the normal range (control group). Recruitment was conducted across hospital outpatient and inpatient settings to ensure representation across a broad demographic and health spectrum.
Prior to their participation, detailed information about the study's aims and procedures was provided to both the children and their guardians by our research team. This briefing highlighted the investigation's focus on the interconnections between psychological factors and body weight. Ethical adherence was a cornerstone of our methodology, with informed consent and child assent obtained in alignment with established ethical standards. Precise measurements of height, weight, and BMI complemented comprehensive documentation of each participant's medical history.
To delve deeper into the psychological landscape, participants were asked to complete a battery of self-report questionnaires. These tools were selected for their robustness in assessing critical psychological dimensions:
Strengths and Difficulties Questionnaire (SDQ) by Goodman R (1997), which provides insight into emotional and behavioral problems. (Emotional Problems Scale, Conduct Problems Scale, Hyperactivity Scale, Peer Problems Scale, Prosocial Scale, Total Difficulties score, Externalizing and Internalizing scores )[
14].
The Adolescent Anxiety and Avoidant Attachment Inventory (AAAAI) by Moretti (2015), examines the nuances of adolescent attachment (Attachment Anxiety, Attachment Avoidance) [
15].
The Affect Regulation Checklist (ARC) by Moretti (2003), focuses on affect dysregulation and its roles in behavior (Affect Dysregulation, Affect Suppression, Adaptive reflection)[
16].
These instruments allowed for a multifaceted assessment of attachment quality, emotional regulation, and emotional or behavioral issues. By integrating these psychological constructs with biometric data, our study was poised to perform an in-depth analysis of the potential contributions of these factors to increased body weight among pediatric populations.
The collected data set the stage for a rigorous analysis aimed at unraveling the intricate dynamics between psychological health and obesity in children and adolescents. Through this methodological framework, our goal was to identify psychosocial markers for early intervention, potentially mitigating the risk and prevalence of childhood obesity. This approach reflects a commitment to advancing understanding in the field and contributing to the development of targeted strategies for promoting healthier outcomes in pediatric health.
2.1. Psychological Measures and BMI in Early Childhood (8-11 years old)
The dataset contains several variables that are associated with both psychological measures and biometric data of children aged between 8 and 11 years. The variables included in the dataset are as follows:
2.1.1. Psychological Metrics
This score quantifies a child’s difficulty in managing emotional responses to various stimuli. High scores indicate greater challenges in emotional regulation, potentially leading to adverse reactions in stressful situations or difficulties in calming down after an emotional event. Affect dysregulation is associated with a variety of mental health issues and can impact physical health and behavior, including eating habits and activity levels [
17].
- 2.
Affect Suppression Score
Reflects the extent to which individuals consciously attempt to suppress their emotional expressions. Higher scores suggest a greater tendency toward hiding or inhibiting emotional displays, which can be a coping strategy to manage social interactions but may also lead to psychological distress and physical health problems if overused [
18].
- 3.
Adaptive Reflection Score
Measures the ability to reflect on and adaptively manage one’s emotions and thoughts. This involves a more mindful approach to dealing with emotional experiences, promoting better emotional intelligence, problem-solving, and coping strategies. High scores indicate a healthier emotional processing style that can mitigate stress-related impacts on health and behavior [
19].
2.1.2. Biometric and Demographic Data
BMI Category: Categorizes the child’s weight status based on BMI calculations, divided into "Healthy," "Overweight," and "Obese" categories according to standardized pediatric BMI percentiles [
20]. This source provides guidelines for interpreting BMI in children and adolescents, defining the thresholds for various weight status categories.
- 4.
BMI (Body Mass Index): A numerical value calculated from a child's weight and height, provides a reliable indicator of body fatness for most children and adolescents. BMI is used to screen for weight categories that may lead to health problems but is not diagnostic of the body fatness or health of an individual [
21].
- 5.
BMI Percentile: Represents the child's BMI relative to peers of the same age and sex, providing a percentile ranking that indicates the distribution of BMI in a reference population. This helps in understanding whether a child is within the expected range of body weight for their age group [
22]. This document details the methodology behind the growth charts used to determine BMI percentiles for children and adolescents.
- 6.
Gender: Indicates the biological sex of the child (male or female). This demographic variable is crucial for interpreting BMI percentiles, which vary by gender, and can also be relevant in the analysis of psychological measures due to differences in emotional expression and regulation across genders [
23].
These detailed attribute descriptions, grounded in psychological and biometric research, provide a comprehensive understanding of the dataset's variables. The population represented in this dataset comprises children in the pre-adolescent developmental stage, a critical period where psychological and physical health patterns begin to emerge and solidify. These data could be used to explore the relationships between psychological well-being and obesity risk in children.
This dataset allows for the analysis of how psychological factors relate to obesity during this developmental stage and could be instrumental in identifying early predictors of obesity. It may also help in understanding how emotional regulation skills are associated with weight status in children. For a more complete methodology, additional details about how the scores were obtained, the sample size, the geographical location, and the socio-economic background of the participants would also be necessary.
The dataset for children aged 8-11 years old encompasses a variety of psychological and biometric measures, collected through questionnaires. This data subset specifically aims to investigate the interplay between psychological well-being and physical health, as indicated by Body Mass Index (BMI) categories and percentiles, across 36 participants.
Numerically, the dataset details scores on Affect Dysregulation and Suppression, as well as Adaptive Reflection abilities. On average, children exhibit a moderate level of affect dysregulation (mean=2.65, SD=0.89) and suppression (mean=2.35, SD=0.82), with adaptive reflection also showing a moderate mean score of 3.20 (SD=0.87). The BMI values range from 13.5 to 26.1, with an average BMI of 18.36 (SD=3.10), reflecting a broad spectrum of body weights. The BMI percentiles, ranging from 6 to 98.3, with a mean of 62.65 (SD=29.17), further contextualize the children's BMI concerning age and gender norms.
Categorically, the dataset reveals 'Healthy' as the predominant BMI category, represented by 23 of the 36 children, indicating a majority within normal weight parameters for their age group. Gender distribution within this cohort leans towards females, comprising 26 out of 36 participants.
2.1.3. Methodological Approach
In the present study, we analyzed the data collected from questionnaires filled out by children aged 8-11. These questionnaires encompassed a range of psychological measures, including Affect Dysregulation Score, Affect Suppression Score, and Adaptive Reflection. Alongside these psychological metrics, data on the children's Body Mass Index (BMI) categories, specific BMI values, and BMI percentiles were collected. The BMI categories were encoded into numerical values for analytical purposes: Healthy (0), Overweight (1), and Obese (2). A Spearman correlation analysis was conducted to explore the relationship between children's psychological measures and their BMI categories, aiming to uncover any significant associations that could illuminate the interplay between psychological well-being and physical health in this age group.
2.2. Navigating the Transitional Years: Psychological and Biometric Profiles in Pre-Teens (11-12 Years Old)
The dataset encompasses a variety of variables that intricately combine psychological assessments with biometric information for children aged 11 to 12 years. This comprehensive collection of data includes the following key elements:
2.2.1. Psychological Metrics
Apart from the Affect Dysregulation,, Affect Suppression, and Adaptive Reflection scores that are described in
Section 2.1.1 we also evaluated the following metrics:
Attachment Anxiety: Quantifies the extent of a child’s apprehension about being abandoned or rejected by attachment figures. Children with high levels of attachment anxiety may exhibit clinginess, neediness, or excessive seeking of reassurance, potentially affecting their ability to form healthy, independent relationships [
24].
- 7.
Attachment Avoidance: Assesses the extent to which a child distances themselves from emotional closeness and interdependence in relationships. Avoidant attachment can manifest as a preference for solitude, difficulty in trusting others, and a reluctance to express needs or seek comfort [
25].
- 8.
Emotional Problems Scale: Identifies the prevalence and intensity of internalizing emotional issues, including symptoms of anxiety, depression, and mood dysregulation. Recognizing these problems early can lead to timely interventions that may prevent the development of more serious mental health conditions [
26].
- 9.
Conduct Problems Scale: Evaluates the presence of externalizing behavioral problems, such as aggression, defiance, and antisocial behavior. This scale helps identify children who may benefit from behavioral interventions to improve social functioning and prevent escalation into more severe conduct disorders [
27].
- 10.
Hyperactivity Scale: Measures signs of excessive activity, impulsivity, and difficulty maintaining attention. Hyperactivity and attentional challenges are characteristic of ADHD but can also occur in other contexts. Addressing these symptoms can improve academic performance and social interactions [
28].
- 11.
Peer Problems: Scores the extent of difficulties a child encounters in forming and maintaining peer relationships. Challenges in this area can impact self-esteem, social skills development, and overall well-being, highlighting the importance of supportive interventions [
29].
- 12.
Prosocial Scale: Assesses the frequency and quality of positive, altruistic behaviors directed toward others, such as sharing, helping, and showing concern. Prosocial behavior is linked to social acceptance, relationship building, and emotional well-being [
30].
- 13.
Total Difficulty Score: Provides an overall assessment of a child's emotional and behavioral challenges, integrating data across various domains. This comprehensive score can guide clinicians, educators, and parents in understanding the child's needs and planning appropriate support or interventions [
14].
- 14.
Externalizing Score: Highlights behaviors that are outwardly directed and potentially disruptive, including aggressive actions and defiance. Identifying these behaviors early allows for targeted interventions that can help manage these tendencies and support positive social interactions [
31].
- 15.
Internalizing Score: Focuses on inwardly directed behaviors and emotions, such as withdrawal, anxiety, and depressive symptoms, offering insights into the child's internal emotional state and potential need for psychological support [
32].
2.2.2. Biometric and Demographic Data
Please refer to
Section 2.1.2 for a detailed overview of the biometric and demographic data, including BMI Category, BMI, and BMI Percentile. The criteria and methodologies outlined in that section apply equally to this age group, providing a consistent basis for evaluating weight status and its potential health implications across different developmental stages.
The dataset for children aged 11-12 years provides a detailed examination of various psychological measures biometric data and BMI measurements. Numerically, the dataset encompasses 15 entries, with measures such as Affect Dysregulation Score and Affect Suppression Score averaging at 2.27 and 2.48 respectively, indicating a range of emotional regulation capabilities among the children. Adaptive reflection scores average at 3.5, suggesting a moderate level of reflective thinking. The Attachment anxiety and Attachment avoidance scores hover around 1.96 and 2.04, pointing to varied levels of attachment-related anxieties and avoidance behaviors.
The Emotional Problems Scale and Conduct Problems Scale average scores are 2.33 and 2.13, respectively. The Hyperactivity Scale averages at 3.07, with Peer Problems averaging at 0.87, indicating a relatively low level of peer-related issues. The Prosocial Scale, with an average of 8.4, suggests a high level of prosocial behavior, and the Total Difficulty Score averages at 8.4. The Externalizing Score and Internalizing Score averages at 5.2 and 3.2 respectively, highlight externalized behaviors and internalized emotions. The BMI data, with an average of 22.61 and a percentile average of 81.55, indicate a diverse range of physical well-being among the children.
Categorically, the dataset reveals that most children fall into the "Healthy" BMI category, with females slightly outnumbering males. This comprehensive dataset not only provides insight into the psychological well-being of children aged 11-12 but also correlates these findings with their physical health, represented by BMI and its percentile. This data underscores the intricate interplay between psychological health and physical well-being in children, serving as a valuable resource for further research into child development and health.
2.2.3. Methodological Approach
The study utilized data collected through questionnaires completed by children, focusing on a range of psychological measures including Affect Dysregulation Score, Affect Suppression Score, Adaptive Reflection, Attachment Anxiety, Attachment Avoidance, Emotional Problems Scale, Conduct Problems Scale, Hyperactivity Scale, Peer Problems, Prosocial Scale, Total Difficulty Score, Externalizing Score, and Internalizing Score. In addition, data on the children's BMI Category, BMI, and BMI Percentile were included to explore potential correlations. The BMI categories were encoded into numerical values (HEALTHY: 0, OVERWEIGHT: 1, OBESE: 2) to facilitate statistical analysis. Spearman's rank correlation coefficient was used to assess the relationship between the psychological measures and the BMI Category Code, providing insights into how these variables may be interconnected.
2.3. Beyond the Threshold: Delving into the Psychological and Biometric Terrain of Early Adolescents (12-16 Years Old)
This dataset integrates a broad array of variables, merging psychological evaluations and biometric indicators for children aged 12-16 years of age. It meticulously compiles the following critical components.
2.3.1. Psychological Metrics
The metrics that have been evaluated for this age group are the same as those described in Section 2.2.1.
2.3.2. Biometric and Demographic Data
For insights into the biometric and demographic data such as BMI Category, BMI, and BMI Percentile, please see the comprehensive explanations provided in
Section 2.1.2. The guidelines and approaches detailed there are uniformly applicable to this demographic segment as well, ensuring a uniform framework for assessing weight status and related health considerations throughout varying developmental phases.
2.3.3. Methodological Approach
For the dataset related to children above 12 years of age, encompassing various psychological measures and biometric data, we conducted a comprehensive analysis. This dataset, derived from questionnaires and biometric measures of the children, comprised 32 participants. The psychological assessments included Affect Dysregulation Score, Affect Suppression Score, Adaptive Reflection, Attachment Anxiety, Attachment Avoidance, Emotional Problems Scale, Conduct Problems Scale, Hyperactivity Scale, Peer Problems, Prosocial Scale, Total Difficulty Score, Externalizing Score, Internalizing Score. Additionally, it included Biometric data: BMI, and BMI Percentile, alongside the categorical variables of BMI Category and Gender.
The numerical analysis revealed a mean Affect Dysregulation Score of approximately 2.74, with a standard deviation suggesting moderate variability among participants. The Affect Suppression Score averaged around 2.82, indicating a slight variation in how individuals suppress negative emotions. The Adaptive Reflection scores, reflecting the capacity for mentalization or understanding the mental states that underlie behavior, averaged 2.91. Attachment-related measures varied, with Attachment Anxiety averaging around 1.85 and Attachment Avoidance at about 2.86, hinting at the diverse attachment styles present within the sample.
Emotional and behavioral problem scales showed a range of responses, with the Emotional Problems Scale averaging 3.53 and the Conduct Problems Scale at 3.19. Hyperactivity scores averaged 4, suggesting varying degrees of attentional focus among the children. Social functioning, as measured by the Peer Problems scale, had a mean score of 2.13, and the Prosocial Scale, indicating positive social behavior, averaged 7.72. The Total Difficulty Score, a composite measure of psychological difficulties, was 12.84 on average, with Externalizing and Internalizing Scores highlighting the external and internal psychological focus faced by the participants. The biometric data revealed an average BMI of 22.8, with a BMI Percentile mean of 73.06, suggesting a healthy weight status for the majority but also indicating the presence of overweight and obesity in the cohort.
Categorically, the dataset was almost evenly split between genders, with a slight majority of male participants. The BMI Category distribution showed that most children were classified as healthy, with fewer instances of being overweight and obese.
This detailed dataset offers a nuanced view of the psychological and biometric profiles of children above 12 years of age, highlighting the interplay between mental health, social functioning, and physical health status. These findings underscore the importance of considering a wide range of factors when assessing the well-being of adolescents, pointing towards the need for holistic approaches to their health and development.
This dataset captures critical psychological and physical health variables during a pivotal developmental stage. The included psychological assessments cover a range of emotional and behavioral domains, which can be instrumental in understanding the multifaceted nature of childhood obesity. The attachment styles may provide insights into the children's interpersonal relationships and how these might affect or be affected by their weight status.
3. Results
This section delves into the intricate relationships between psychological health and obesity across different developmental stages, employing bioinformatics techniques for data analysis.
3.1. Analysis in Early Childhood (Ages 8-11)
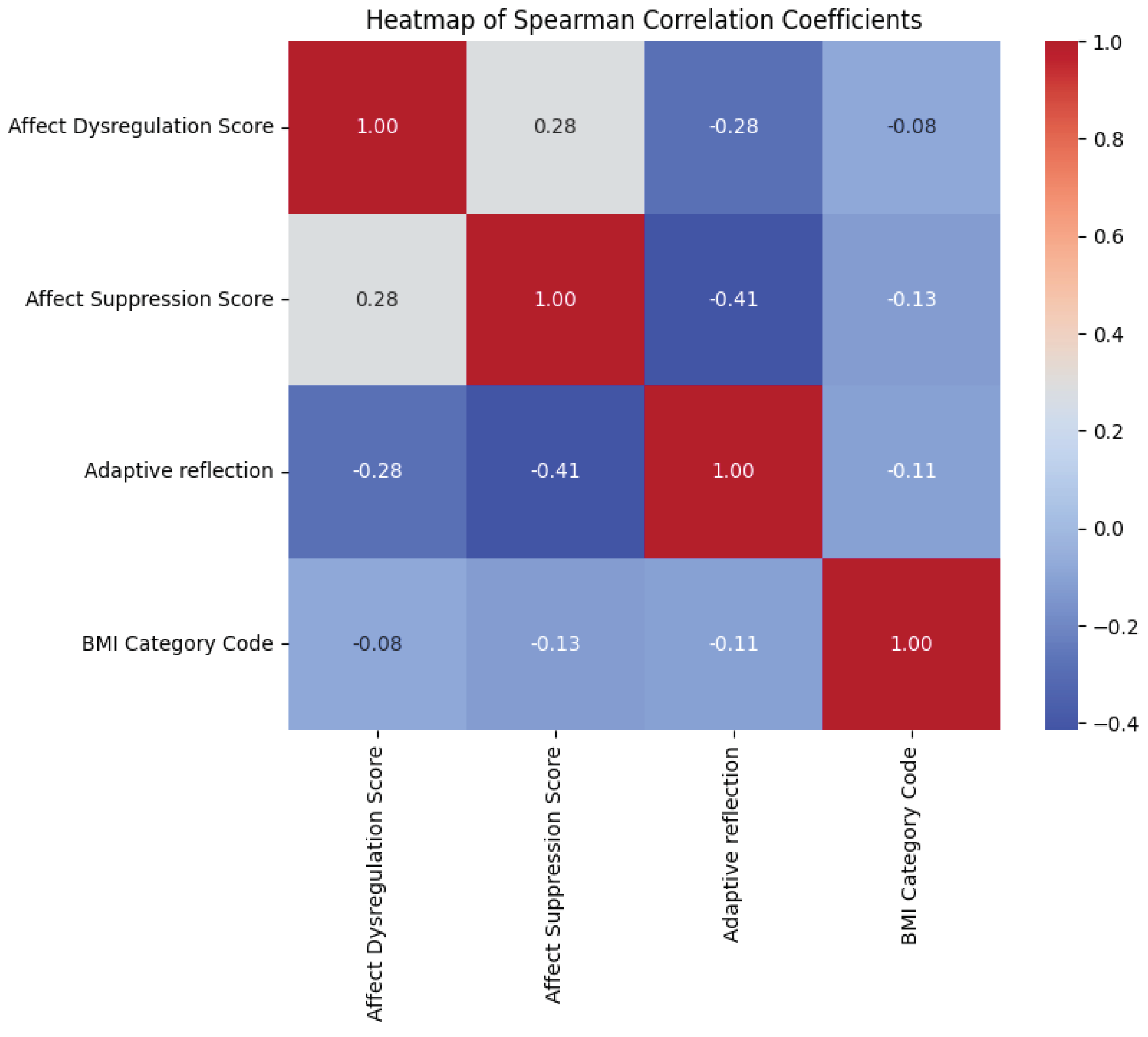
The Spearman correlation analysis revealed that all three psychological measures analyzed concerning the BMI categories of children aged 8-11 displayed negative correlations. Specifically, the Affect Dysregulation Score correlated with the BMI Category Code at -0.083002, indicating a slight inverse relationship where higher dysregulation scores were marginally associated with lower BMI categories. Similarly, the Affect Suppression Score showed a more pronounced negative correlation of -0.126732, suggesting that higher levels of affect suppression were related to lower BMI categories. The Adaptive Reflection score also demonstrated a negative correlation (-0.106170), albeit slightly stronger than that of the Affect Dysregulation Score, indicating that more adaptive reflection capabilities were inversely related to the BMI category. In the exploration of the relationship between psychological well-being and BMI categories among children aged 8-11, we constructed a heatmap to visually represent the Spearman correlation coefficients (
Figure 1). This heatmap elucidates the degree and direction of associations among the variables: Affect Dysregulation Score, Affect Suppression Score, Adaptive Reflection, and the encoded BMI Category Code. The intensity of the colors corresponds to the strength of the correlation, with red denoting positive and blue indicating negative associations.
Notably, the heatmap illustrates a mild negative correlation between Adaptive Reflection and BMI Category Code (r = -0.11), suggesting that children with higher capacities for adaptive reflection may tend to have a lower BMI category. Conversely, the Affect Suppression Score shows a very slight negative correlation with the BMI Category Code (r = -0.13), indicating that this psychological measure has a negligible association with BMI categories. The heatmap underscores the intricate, multifaceted nature of these relationships, inviting further analysis to uncover the underlying mechanisms at play in the interaction between psychological factors and obesity risk in early childhood.
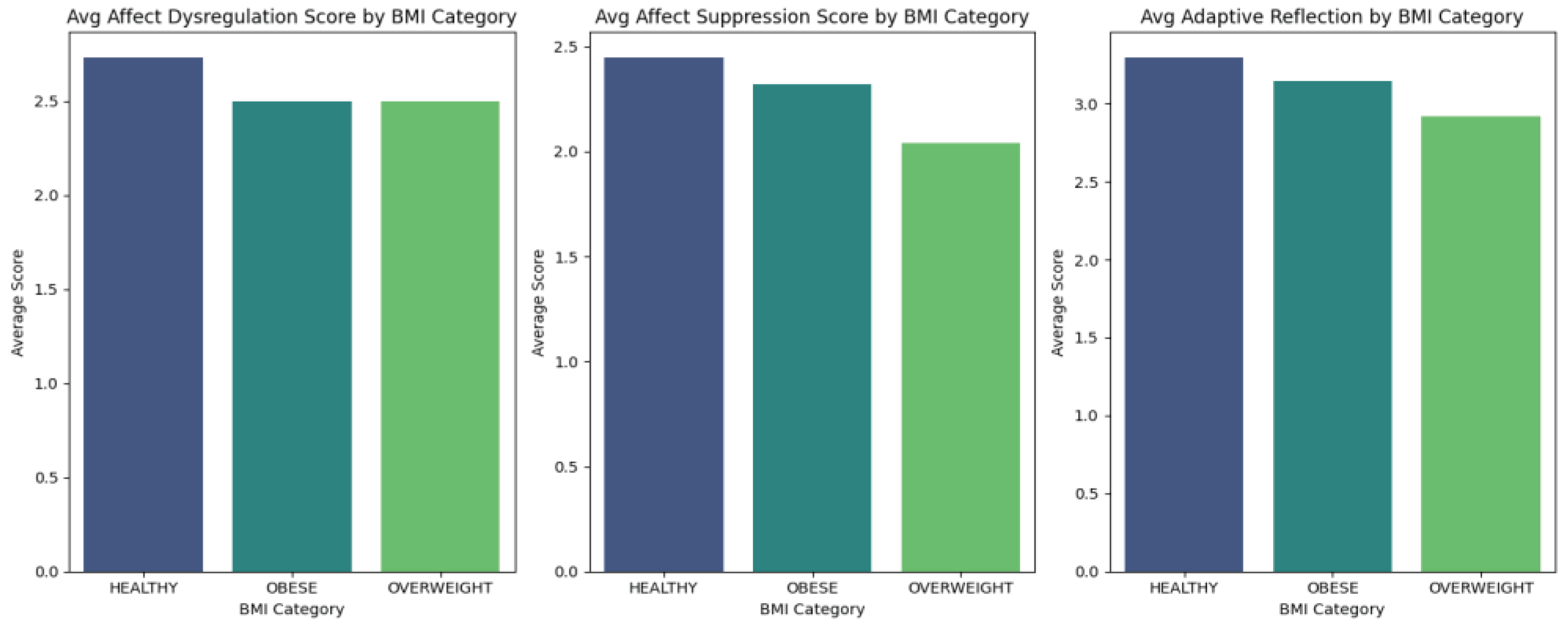
Figure 2 presents a comparative visualization of the average psychological scores across BMI categories for children aged 8-11. The bar graphs depict a trend where the Affect Dysregulation and Affect Suppression scores do not vary significantly across the BMI categories. However, the Adaptive Reflection scores show a slight decrease from the Healthy to Overweight and Obese categories. The graph indicates that while children's ability to regulate and suppress affect might not differ markedly with their BMI status, their adaptive reflection abilities may be inversely related to higher BMI categories. This pattern suggests that children who are overweight or obese might experience challenges in effectively reflecting on and adapting to situations, which is an aspect worth exploring further in the context of obesity interventions.
3.2. Insights into Pre-Adolescence (Ages 11-12)
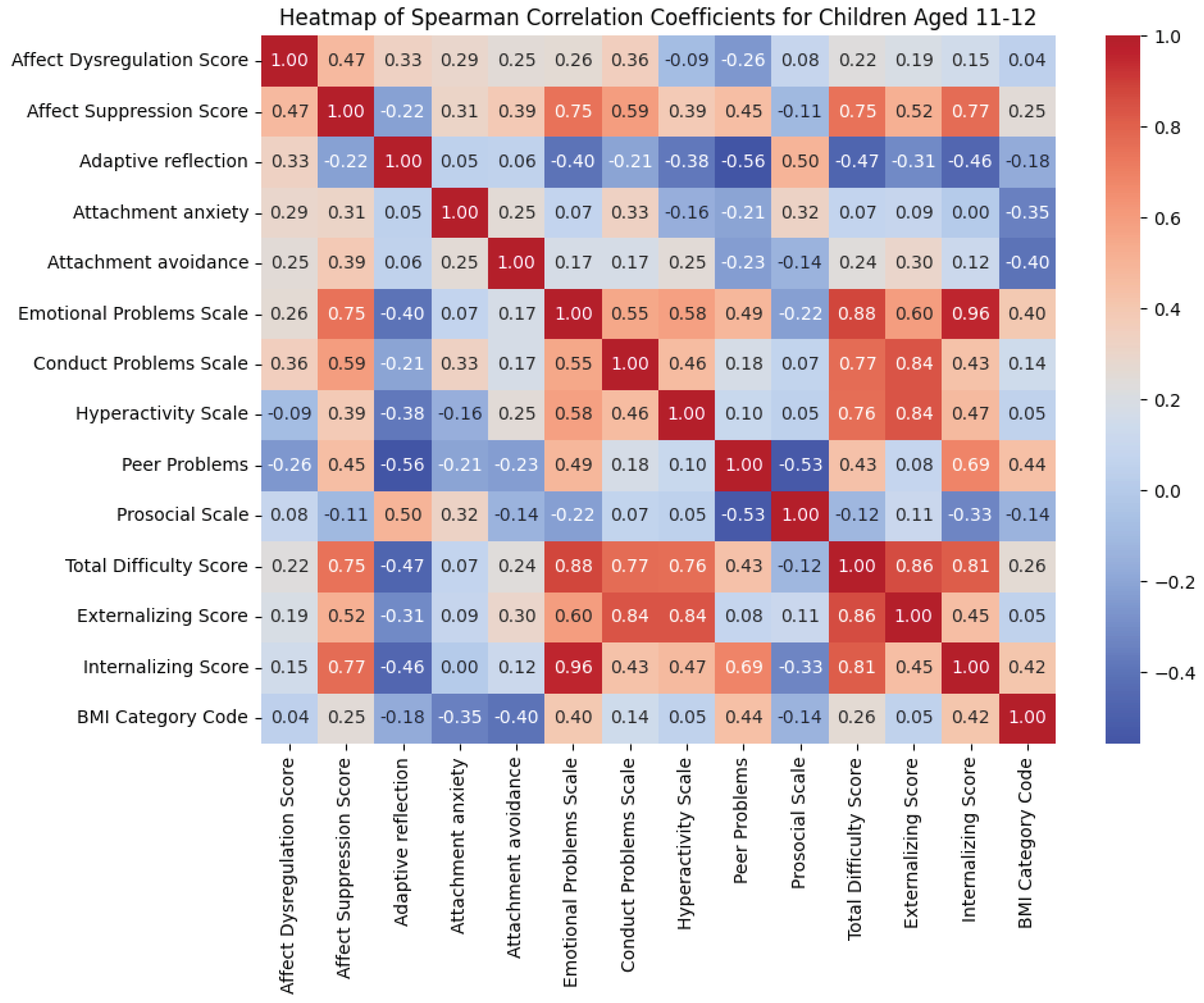
The analysis revealed varying degrees of correlation between psychological measures and BMI categories. Notably, Attachment Avoidance (-0.402629) and Peer Problems (0.437186) showed significant correlations with BMI categories, suggesting a potential link between these psychological factors and obesity risk in children. Emotional Problems Scale (0.397872) and Internalizing Score (0.416022) were also notably correlated with BMI categories, indicating that emotional and internalizing behaviors could be associated with BMI changes. Conversely, some measures such as Adaptive Reflection (-0.178892) and Prosocial Scale (-0.135218) exhibited negative correlations, suggesting that higher scores in these areas might relate to healthier BMI categories.
In our analysis, we explored the interrelationships between a comprehensive set of psychological variables and BMI categories for children aged 11-12, as depicted in
Figure 3. The heatmap provides a visual representation of the Spearman correlation coefficients, facilitating an immediate grasp of the complex web of associations. Notably, the scale reflects both positive and negative correlations, with more intense colors denoting stronger relationships.
A significant negative correlation is observed between Adaptive Reflection and Affect Suppression Score, suggesting that children who are better at reflecting on their experiences may be less likely to suppress their effects.
The BMI Category Code shows varied correlation strengths with psychological measures, indicating the nuanced and multifaceted nature of the relationship between psychological factors and obesity. This heatmap underscores the critical need to approach childhood obesity by considering a wide array of psychological influences, which may interact in complex ways to shape physical health outcomes.
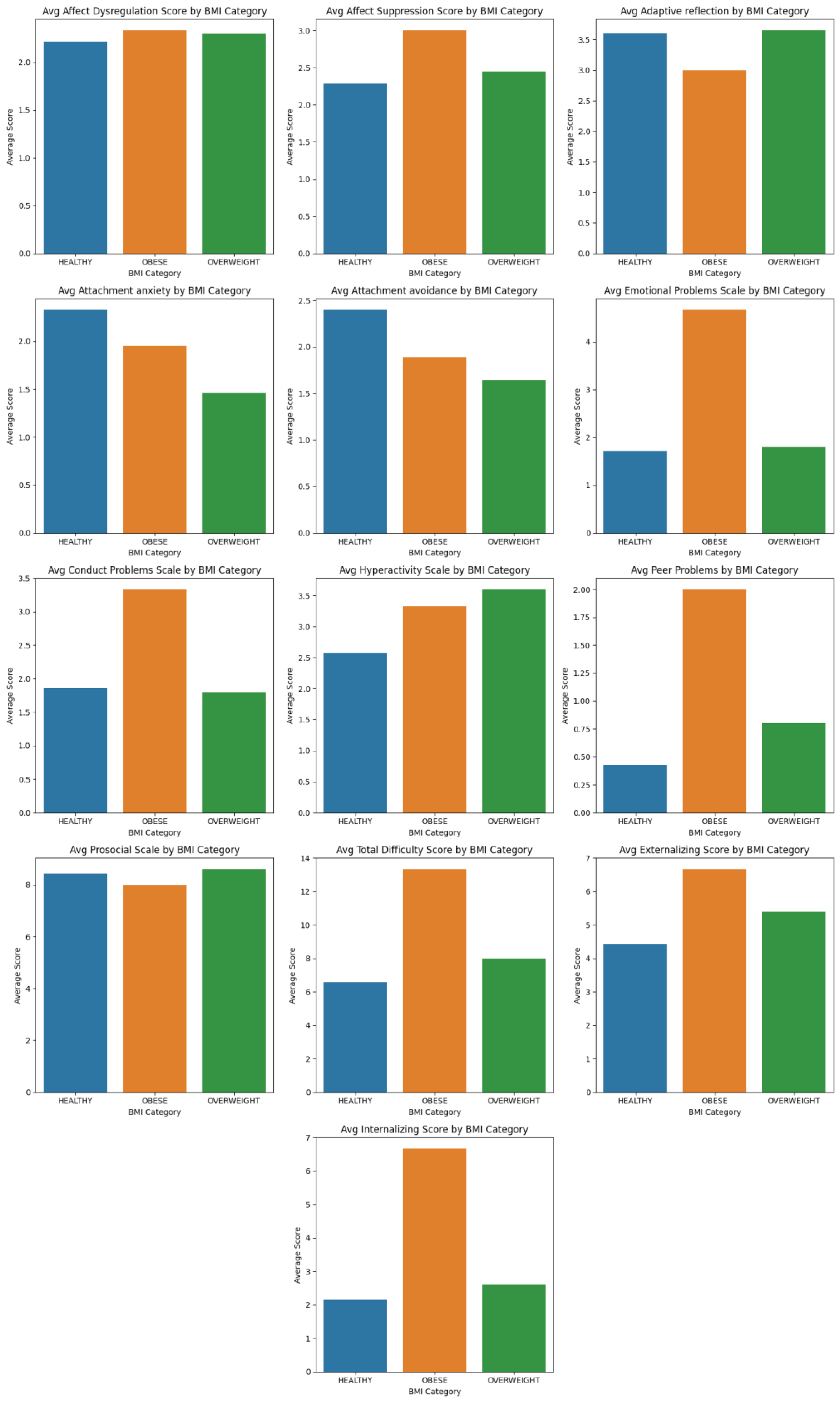
In
Figure 4, we present a series of bar graphs that detail the average scores of twelve psychological measures as stratified by BMI category for the children aged 11-12 in our study. Notably, the bar graphs illustrate that children with an 'Obese' BMI category tend to have higher average scores on Conduct Problems Scale, Hyperactivity Scale, Total Difficulty Score, and Externalizing Score, which may suggest a link between behavioral challenges and increased BMI. In contrast, the 'Healthy' BMI category is associated with higher scores on Adaptive Reflection and Prosocial Scale, potentially indicating better emotional regulation and social behaviors in children within normal weight ranges. These visual trends underscore the necessity of a multifaceted approach to childhood obesity that considers not only physical but also psychological dimensions. The differences in average scores across BMI categories emphasize the interrelated nature of mental health and obesity, hinting at the complex causative pathways that require further research and comprehensive intervention strategies.
This figure displays the mean scores of various psychological measures for children aged 11-12, broken down by BMI category. Each bar graph represents the average score for a specific psychological construct, illustrating how scores differ among children classified as 'Healthy,' 'Overweight,' and 'Obese.' These visual representations highlight potential associations between psychological well-being and BMI, suggesting areas for targeted interventions.
3.3. Adolescent Analysis (Above 12 Years)
Our analysis revealed varied correlations between psychological measures and BMI categories. Notably, the Affect Dysregulation Score (-0.281) and Affect Suppression Score (-0.191) were negatively correlated with BMI categories, suggesting a decrease in these psychological problems as the BMI category increases. Conversely, Peer Problems (0.210) and Internalizing Score (0.138) showed positive correlations, indicating an increase in these issues with higher BMI categories. Adaptive Reflection (0.085) and Total Difficulty Score (0.092) also displayed positive but weak correlations with BMI categories.
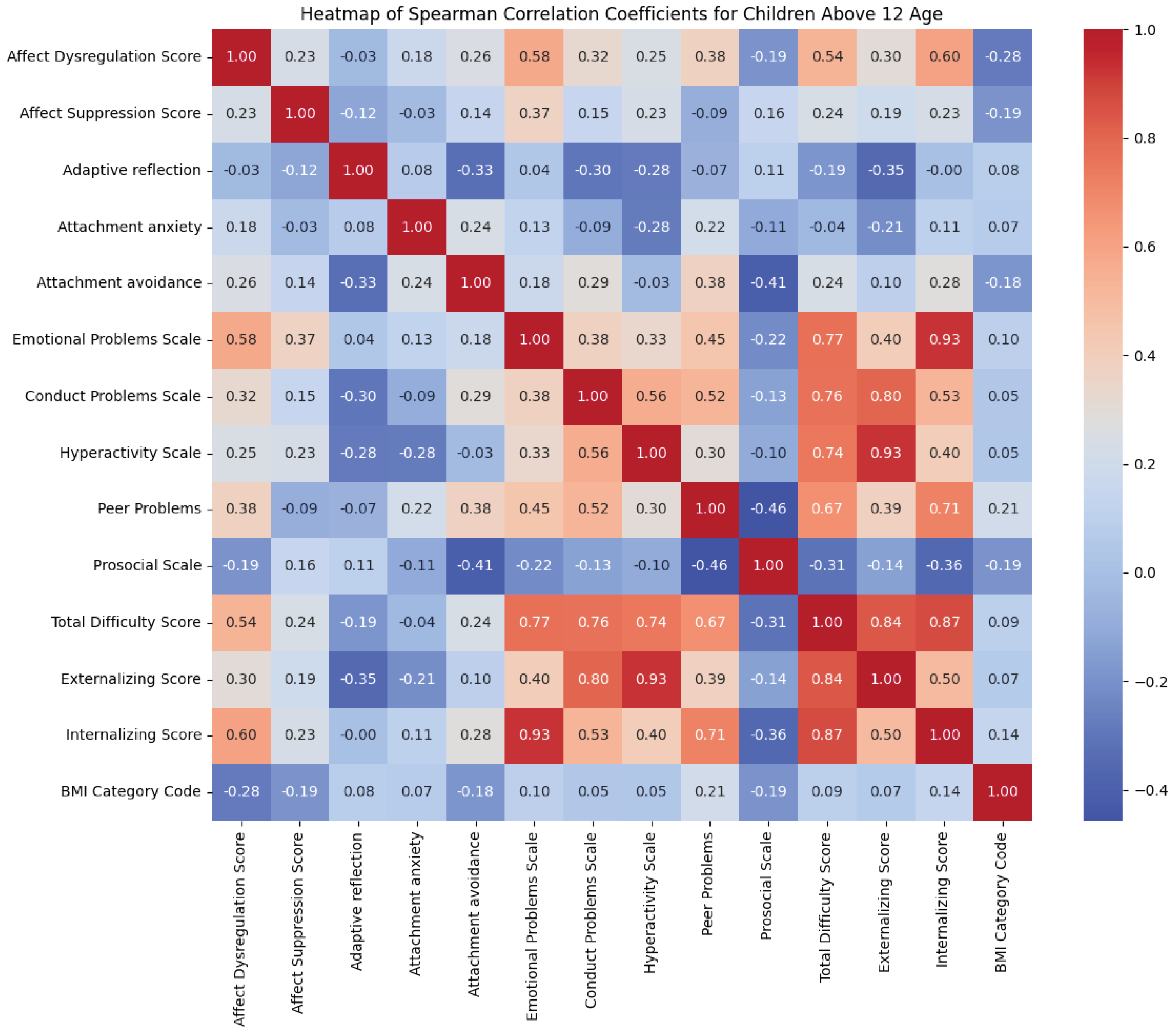
In
Figure 5, we present a heatmap of Spearman correlation coefficients that provides a visual summary of the relationships between a range of psychological variables and BMI Category Codes in children above the age of 12. The heatmap illustrates both the magnitude and the direction of correlations, with warmer colors (red) representing stronger positive correlations and cooler colors (blue) signifying stronger negative correlations. For instance, the scale of Emotional Problems shows a notable positive correlation with the BMI Category Code, suggesting that children with higher scores in emotional problems tend to have a higher BMI category. In contrast, variables such as Affect Dysregulation and Internalizing Scores exhibit negative correlations with the BMI Category Code, indicating an inverse relationship. This nuanced portrayal aids in identifying patterns and potential areas of focus for interventions aimed at addressing obesity and psychological distress in children.
This heatmap displays the Spearman correlation coefficients among various psychological measures and BMI Category Codes for children above 12 years of age. The color intensity represents the strength and direction of the correlation, with red indicating positive relationships and blue indicating negative relationships.
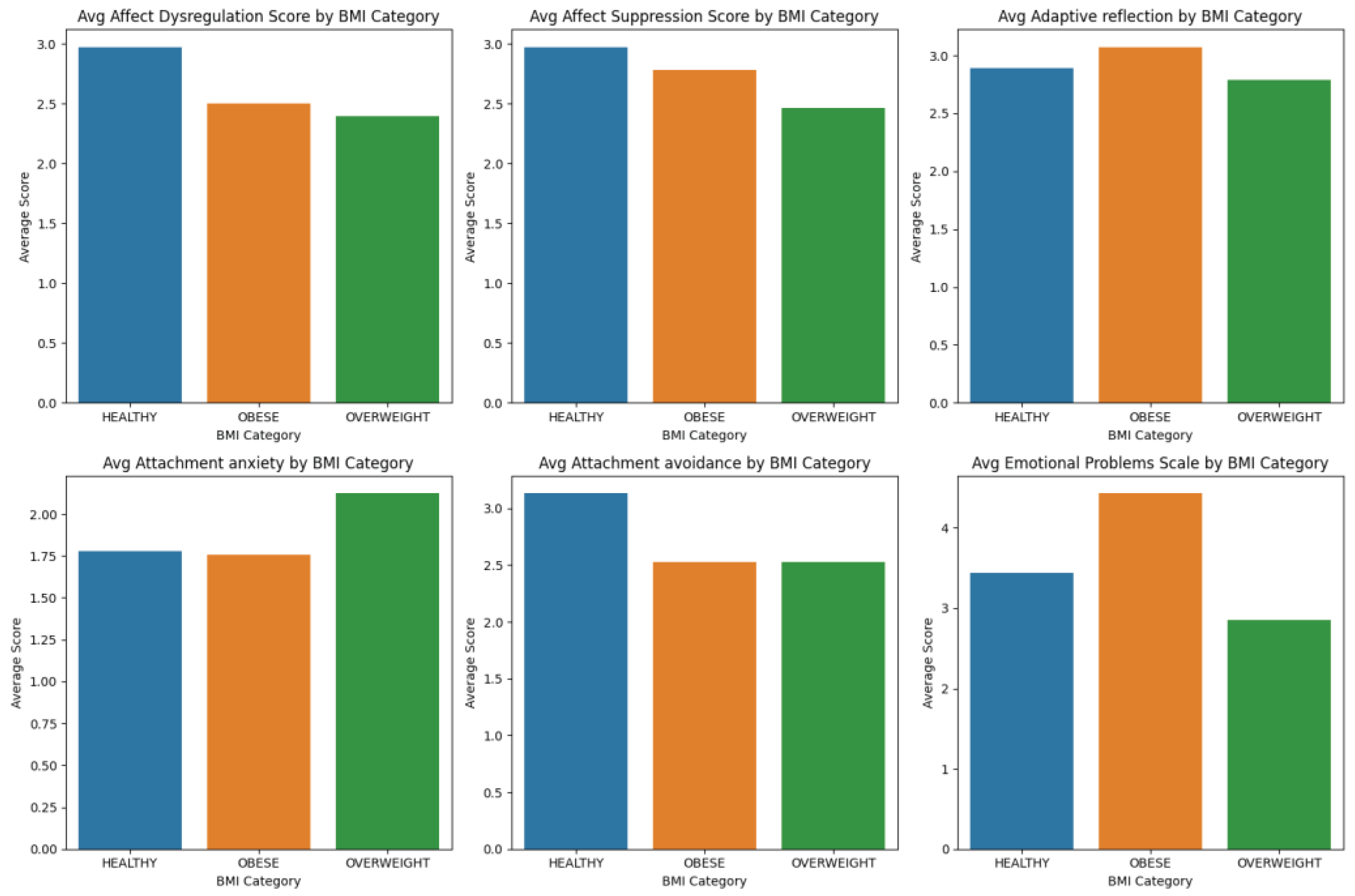
Figure 6 illustrates the average scores for various psychological measures across different Body Mass Index (BMI) categories among children above 12 years of age. The bar graphs represent the mean scores for Affect Dysregulation, Affect Suppression, Adaptive Reflection, Attachment Anxiety, Attachment Avoidance, and Emotional Problems Scale, delineated by the BMI categories of Healthy, Overweight, and Obese. This visual representation allows for an immediate comparison of psychological patterns across the spectrum of weight status, hinting at the interrelation between psychological well-being and obesity in children.
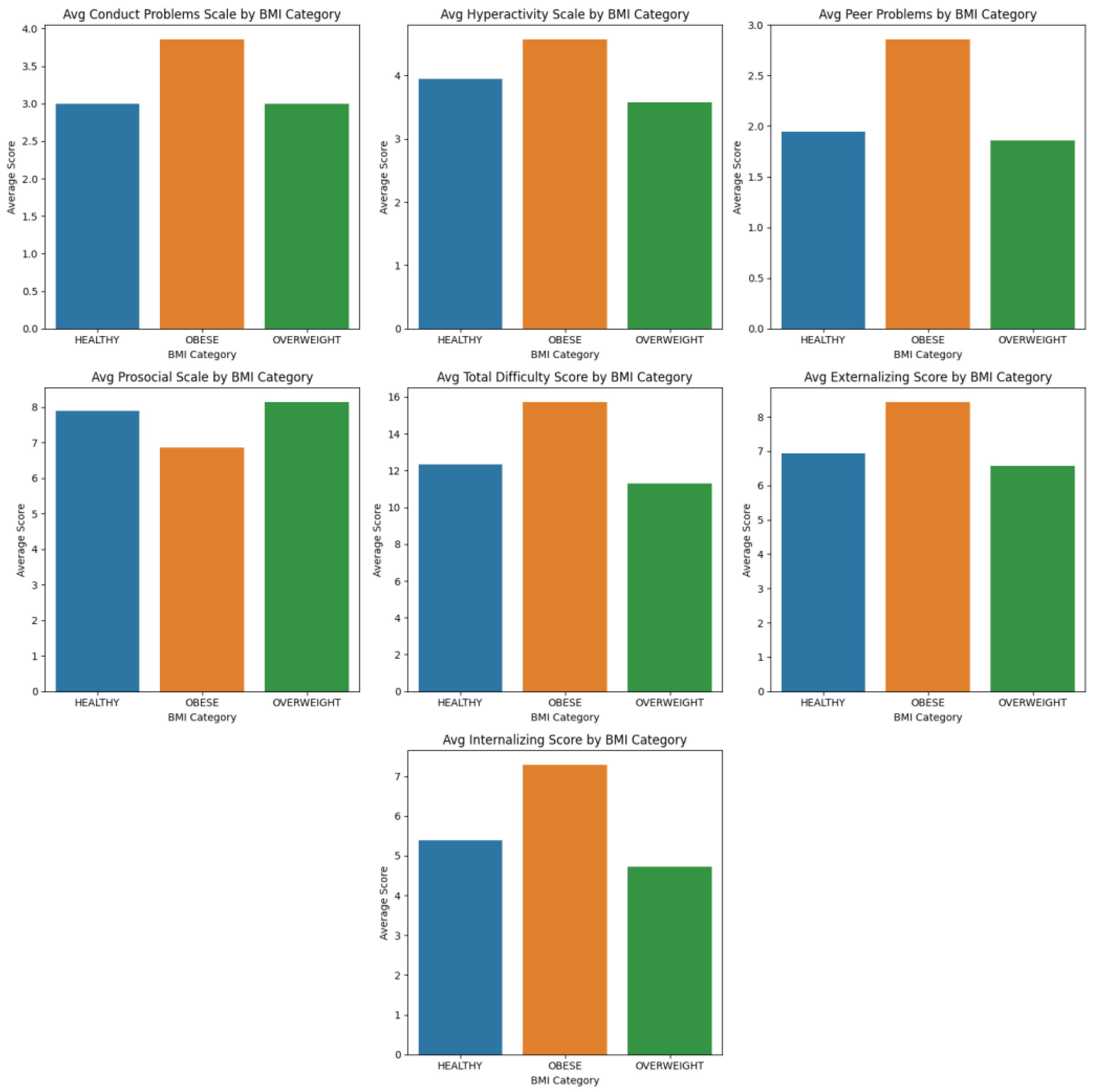
Figure 7 continues the exploration of psychological dimensions related to BMI categories, presenting the average scores for Conduct Problems, Hyperactivity, Peer Problems, Prosocial Behavior, Total Difficulty, Externalizing Behaviors, and Internalizing Behaviors. Each bar graph provides insights into how children within each BMI classification score on these psychological measures, suggesting trends that may indicate broader behavioral and emotional challenges associated with childhood obesity. These plots underscore the potential impact of various psychosocial factors on children's physical health outcomes.
The results of this research indicate some preliminary correlations between psychometric tests and biometric data across categories. These findings illuminate potential pathways through which psychological well-being and physical health intersect in the context of childhood obesity. However, further analysis is essential to delineate the pathological or normal nature of these characteristics, providing a foundation for more targeted interventions
4. Discussion
The intricate relationship between psychological well-being and physical health during childhood underscores the potential of bioinformatics in revolutionizing public health and pediatric practices. This study leverages advanced data analytics to elucidate the complex dynamics underpinning obesity in children and adolescents, marking a significant stride toward integrative healthcare solutions.
4.1. Early Childhood (Ages 8-11): Leveraging Bioinformatics for Personalized Obesity Prevention
The foundational years of early childhood represent a pivotal stage in the development of physical health, emotional well-being, and lifestyle habits. Our application of bioinformatics techniques to this critical period has uncovered nuanced yet distinctly significant negative correlations between psychological well-being and Body Mass Index (BMI) categories. Incorporating bioinformatics into early childhood obesity prevention strategies offers a groundbreaking way to address the multifaceted challenges of pediatric obesity. By providing insights into the complex interplay between psychological well-being and physical health, bioinformatics enables the design of comprehensive, evidence-based interventions. These interventions, grounded in a deep understanding of individual behavioral and emotional patterns, hold the promise of initiating sustainable lifestyle changes. Such changes are critical not only for preventing obesity but also for laying the foundation for a lifetime of health and well-being.
As we move forward, it is essential to continue refining these bioinformatic models and digital health platforms through ongoing research and development. Collaborations between pediatricians, psychologists, data scientists, and technology developers will be key in advancing these tools and ensuring they are accessible, user-friendly, and effective. Ultimately, the integration of bioinformatics into the field of pediatric healthcare represents a significant step towards a future where childhood obesity can be preemptively addressed, ensuring brighter, healthier futures for our youngest populations.
4.2. Pre-Adolescence (Ages 11-12): Integrating Bioinformatics in Understanding Social Dynamics and Cognitive Behaviors
The transition from childhood to adolescence is a critical developmental period marked by profound changes in social relationships, emotional processing, and self-identity. Our study, at the intersection of bioinformatics and pediatric health, casts a spotlight on the intricate ways in which social relationships and emotional bonds during pre-adolescence influence Body Mass Index (BMI) and, by extension, obesity risk. By harnessing the analytical power of bioinformatics to scrutinize social network data, we glean valuable insights into the complex interplay between peer interactions and lifestyle choices such as eating behaviors and physical activity levels. This innovative approach unveils the potential of social dynamics as a pivotal factor in obesity prevention, suggesting that interventions could be significantly enhanced by focusing on the social environment of pre-adolescents [
33].
The application of bioinformatics in this context allows for the nuanced analysis of large-scale data sets, capturing the subtleties of social relationships and their impact on health behaviors. This methodology can identify patterns of social connectivity, isolation, or peer influence that are otherwise challenging to discern. Such insights pave the way for developing targeted interventions that not only address dietary and physical activity factors but also seek to improve social interactions and support networks among pre-adolescents. These findings advocate for a paradigm shift towards interventions that are deeply rooted in understanding and leveraging social dynamics to foster healthier behaviors and prevent obesity.
Furthermore, the observed negative correlation between adaptive reflection and BMI underscores the importance of cognitive and emotional skills in managing health and nutrition. This correlation invites the exploration of interactive, web-based tailored to the unique psychological profiles of pre-adolescents. Such digital interventions can offer personalized strategies to enhance decision-making, problem-solving, and emotional regulation skills. By incorporating bioinformatics techniques to analyze behavioral and emotional data, these programs can be optimized for maximum relevance and impact, ensuring they resonate with the individual experiences and challenges of pre-adolescents [
34].
The potential of bioinformatics extends beyond data analysis to the development of digital platforms that deliver these interventions in an engaging, accessible, and effective manner. By integrating game design principles, social networking elements, and interactive learning modules, these digital programs can captivate the interest of pre-adolescents, encouraging active participation and sustained engagement. The adaptability of such programs allows for continuous refinement based on real-time data and feedback, enhancing their effectiveness in fostering healthy behaviors and attitudes toward nutrition and physical activity.
In essence, the pre-adolescent phase is a window of opportunity for impactful interventions that can alter the trajectory toward obesity. The integration of bioinformatics in understanding and addressing the complex web of social, emotional, and cognitive factors presents a forward-thinking approach to obesity prevention. By acknowledging and targeting the multifaceted influences on pre-adolescents' health behaviors, we can develop more comprehensive, effective, and personalized strategies that not only combat obesity but also support the overall well-being and development of children as they navigate the challenging transition to adolescence.
4.3. Adolescence (12-16 years old): Bioinformatics and the Complex Landscape of Obesity and Psychological Health
In the adolescent phase, the landscape of obesity is intertwined with the psychological and social dimensions of health. Our exploration into this critical period reveals a nuanced narrative that diverges from conventional perspectives on obesity and psychological well-being. Utilizing the advanced methodologies of bioinformatics to dissect the intricate web of behavioral and emotional data, our study uncovers a compelling association: a higher Body Mass Index (BMI) may not solely be a marker of health risk but also an indicator of adaptive emotional strategies. This revelation challenges the stigma often associated with obesity and opens new avenues for leveraging supportive technologies aimed at enhancing resilience and self-esteem among adolescents grappling with obesity-related issues [
10].
The intricate relationship between increased BMI and psychological adaptability underscores the complexity of adolescent obesity. Far from being a straightforward issue of caloric imbalance, obesity in adolescents emerges as a multifaceted phenomenon, where psychological resilience plays a critical role. Adolescents with higher BMI may develop sophisticated coping mechanisms to navigate the social challenges and emotional turmoil often associated with obesity. This adaptive capacity highlights the potential for interventions that not only address physical health but also bolster psychological resilience, facilitating a more holistic approach to obesity management.
Moreover, our findings illuminate the significant role of social dynamics in the context of adolescent obesity. The pronounced correlation between peer-related issues and higher BMI categories underscores the pressing need for interventions that transcend the individual, targeting the broader social network to foster inclusion, support, and understanding. In this regard, bioinformatics offers a powerful toolkit for identifying patterns and predictors of social isolation and peer challenges, guiding the development of community-based interventions that harness digital platforms for social connectivity. These platforms can host peer support groups, offer social networking features, and deliver targeted content designed to enhance social skills, reduce feelings of isolation, and promote a sense of belonging among adolescents facing obesity [
12].
The advent of digital health technologies, powered by bioinformatic analyses, presents an unprecedented opportunity to address adolescent obesity in a nuanced and personalized manner. Through the aggregation and analysis of vast datasets, encompassing genetic, behavioral, and environmental factors, bioinformatics enables the identification of unique risk profiles and the tailoring of interventions to meet the specific needs of adolescents. This approach not only enhances the efficacy of obesity interventions but also empowers adolescents to take an active role in their health journey, equipped with insights and tools tailored to their unique circumstances.
In conclusion, the adolescence phase, characterized by significant physical, emotional, and social development, demands a reevaluation of our approach to obesity. Bioinformatics emerges as a critical ally in this endeavor, offering insights that challenge traditional narratives and pave the way for innovative interventions. By embracing the complexity of adolescent obesity and leveraging the power of bioinformatics, we can develop more effective, empathetic, and holistic strategies that address the physical, psychological, and social dimensions of health, ultimately fostering a healthier, more resilient generation of adolescents.
4.4. Implications for Interventions and Policy
The convergence of bioinformatics and healthcare heralds a paradigm shift in addressing childhood obesity. Our study emphasizes the necessity of a multifaceted approach that incorporates genetic, environmental, and behavioral data into comprehensive prevention and treatment strategies.
Educational Strategies: Deploying bioinformatic tools to personalize educational content can enhance understanding and engagement with healthy lifestyles. Gamified apps and interactive platforms can make learning about nutrition and exercise appealing and effective for children [
4].
Emotional and Social Support Systems: Leveraging data analytics to understand and support the emotional and social development of children is crucial. Predictive models can identify children at risk of psychological distress, enabling timely intervention [
2].
Family and Community Engagement: Bioinformatics can facilitate the development of community health portals that offer resources, support networks, and personalized health recommendations, fostering an environment that supports healthy growth [
34].
Adaptable and Culturally Sensitive Interventions: Advanced data analysis techniques can help tailor interventions to diverse cultural backgrounds, ensuring that obesity prevention programs are inclusive and effective across different populations [
11].
Policy Initiatives: Integrating bioinformatic insights into public health policy can inform the creation of environments that promote physical and psychological well-being. Data-driven urban planning can ensure access to recreational spaces, healthy foods, and mental health resources [
13].
A Shift in Paradigm: Embracing a bioinformatics-informed approach to healthcare enables a holistic view of childhood obesity, considering the totality of a child's experience. This integrative model promises more effective and enduring solutions to one of the most pressing health challenges of our time [
10].
In essence, the fusion of bioinformatics and healthcare offers unprecedented opportunities to combat childhood obesity through personalized, data-driven interventions. By acknowledging the complex interplay of psychological, social, and biological factors, we can forge a path towards a healthier future for our children.
5. Conclusions: Advancing Childhood Obesity Management through Bioinformatics
Our investigation embarked on an intricate journey through the realms of psychological health and childhood obesity, dissecting their interplay across various developmental stages with a keen eye on bioinformatics. By leveraging sophisticated bioinformatic tools, our analysis explored connections between psychological factors such as affect dysregulation, attachment styles, and adaptive reflection, and the pervasive issue of obesity in children. The insights gleaned from this study underscore the significant, bidirectional nexus between psychological distress and obesity, enriched by the understanding that these relationships are deeply embedded within the fabric of familial and environmental contexts.
The application of bioinformatics has been instrumental in our exploration, enabling the parsing and interpretation of complex datasets to reveal patterns and correlations that traditional analytical methods might overlook. This approach has opened up new vistas for probing into the epigenetic mechanisms that potentially link psychological stressors with obesity, laying the groundwork for groundbreaking research and therapeutic innovations that transcend conventional boundaries.
In light of our findings, the imperative for early psychological interventions stands out as a cornerstone in the preventive strategy against childhood obesity. The identification of specific psychological markers, understood within the continuum from early childhood to adolescence, heralds a new era of targeted interventions. These interventions envisioned to harmonize the mental and physical aspects of health, draw strength from the sophisticated analyses made possible by bioinformatics. Such tools not only enhance our understanding of the stress-obesity relationship but also facilitate the development of personalized, age-appropriate strategies that are sensitive to the individual's psychological and genetic makeup.
Moreover, our study advocates for an interdisciplinary approach, integrating psychological assessments with biometric data—and, prospectively, epigenetic information—to forge holistic healthcare models. These models aspire to balance the scales between psychological well-being and physical health, emphasizing the integration of psychological support within obesity prevention and management frameworks. The path forward calls for an alignment of efforts across genetics, epigenetics, psychology, bioinformatics, pediatrics, and public health to craft innovative solutions to the multifaceted challenge of childhood obesity.
As we pivot towards the future, the exploration of genetic and epigenetic foundations underlying the observed associations becomes paramount. Utilizing bioinformatics to analyze broader, more diverse datasets will refine our comprehension of the complex interplay between stress and obesity. Longitudinal studies, critical for establishing causality and mapping the trajectory of these relationships, will further solidify the foundation for effective, evidence-based interventions. The synergy of disciplines, uniting under the banner of bioinformatics, heralds a transformative shift in how childhood obesity is understood, prevented, and treated.
In encapsulating our findings, this study not only contributes a significant chapter to the scholarly dialogue on childhood obesity but also issues a clarion call to healthcare professionals, educators, and policymakers. It underscores the critical role of psychological factors in both the genesis and resolution of obesity, advocating for a comprehensive, bioinformatics-enhanced approach to pediatric healthcare. This approach, which embraces the psychological dimensions of obesity alongside physical health measures, paves the way for more effective, holistic healthcare solutions.
While this study offers valuable insights into the interplay between psychological factors and BMI in children, it is important to acknowledge its limitations. The limited sample size and the imbalance in datasets may constrain the generalizability of the findings. These limitations highlight the need for further research with larger, more balanced cohorts to fully understand the implications of our preliminary correlations and to robustly characterize the pathological or normal nature of these observed characteristics.
As we venture forward, our collective endeavor should be to cultivate environments that nurture both the psychological and physical well-being of our children. The integration of bioinformatics into the fight against childhood obesity represents a promising leap towards realizing this vision, promising a healthier, more resilient future generation. This paper, while enriching academic discourse, serves as a beacon, guiding healthcare professionals, educators, and policymakers toward a more profound appreciation of the psychological underpinnings of obesity and the promise of bioinformatics in crafting holistic, effective healthcare strategies.
Author Contributions
Conceptualization, A.H., G.G., O.F. and G.F.; methodology, A.H., G.G., O.F., A.B., A.K. and G.F.; software, G.F, A.K. .; validation, A.H., G.G., O.F., A.B., A.K. and G.F.; formal analysis, A.H., G.G., O.F., A.B., A.K. and G.F.; investigation, A.H., G.G., O.F., A.B., A.K. and G.F.; resources, A.H., G.G., O.F., A.B., A.K. and G.F.; data curation, A.H., G.G., O.F., A.B., A.K. and G.F.; writing—original draft preparation, A.H., G.G., O.F., A.B., A.K., E.K., A.A., G.Z., I.D. and G.F.; writing—review and editing, A.H., G.G., O.F., A.B., A.K., E.K., A.A., G.Z., I.D. and G.F..; visualization, G.F..; supervision, A.H., G.G., O.F.; project administration, G.G., E.K. and I.D.; funding acquisition, G.Z. and E.K. All authors have read and agreed to the published version of the manuscript.”
Funding
This research was funded by the 'Multi-Pillar Framework for Children Anti-Obesity Behavior building on an EU biobank, Micro-Moments, and Mobile Recommendation Systems', under the grant HORIZON-HLTH-2022-STAYHLTH-01 (BIO-STREAMS)
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Penteli General Children’s Hospital (7133/27-6-2022, 4229/06.04.2023, 7719/26-6-2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets presented in this article are not readily available because the data are part of an ongoing study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Skinner, A.C.; Ravanbakht, S. N.; Skelton, J. A.; Perrin, E. M.; Armstrong, S. C. Prevalence of Obesity and Severe Obesity in US Children, 1999-2016, Pediatrics 2018, vol. 141, no. 3. [CrossRef]
- Lobstein, T.; Jackson-Leach, R.; Moodie, M. L.; Hall, K. D.; Gortmaker, S. L.; Swinburn, B. A.; Wang, Y.; McPherson, K. Child and adolescent obesity: part of a bigger picture. The Lancet 2015, vol. 385, no. 9986, pp. 2510–2520. [CrossRef]
- Sanders, R. H.; Han, A.; Baker, J.S.; Cobley, S. Childhood obesity and its physical and psychological co-morbidities: a systematic review of Australian children and adolescents. European Journal of Pediatrics 2015, vol. 174, no. 6, pp. 715-746. [CrossRef]
- Quek, Y.H.; Tam, W. W. S.; Zhang, M. W. B.; Ho, R. C. M. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obesity Reviews 2017, vol. 18, no. 7, pp. 742–754. [CrossRef]
- Llewellyn, C. H.; Trzaskowski, M.; Plomin, R.; Wardle, J. Finding the missing heritability in pediatric obesity: the contribution of genome-wide complex trait analysis. International Journal of Obesity 2013, vol. 40, no. 10, pp. 1423–1428. [CrossRef]
- Russell-Mayhew, S.; McVey, G.; Bardick, A.; Ireland, A. Mental health, wellness, and childhood overweight/obesity. Journal of Obesity 2012, vol. 11. [CrossRef]
- Cunningham, S. A.; Kramer, M. R.; Narayan, K. MV. Incidence of Childhood Obesity in the United States. New England Journal of Medicine 2014, vol. 370, no. 5, pp. 403–411. [CrossRef]
- Pervanidou, P.; Chrousos, G. P. Stress and obesity/metabolic syndrome in childhood and adolescence. International Journal of Pediatric Obesity 2011, vol. 6, no. sup1, pp. 21–28, doi: 103109/17477166.2011.615996.
- Spear, B. A. Adolescent growth and development. Journal of the American Dietetic Association 2006, vol. 106, no. 3, pp. S23–S29. [CrossRef]
- Li, X.; Dunn, J.; Salins, D. et al. Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information. PLoS Biol 2017, vol. 15, no. 1. [CrossRef]
- Wang, Y.; Lobstein, T. Worldwide trends in childhood overweight and obesity. International Journal of Pediatric Obesity 2006, vol. 1, no. 1, pp. 11–25. [CrossRef]
- Simmonds, M.; Burch, J.; Llewellyn, A. et al. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: a systematic review and meta-analysis. Health Technology Assessment 2015, vol. 19, no. 43, pp. 1–336. [CrossRef]
- Hales, C.M.; Carroll, M. D.; Fryar, C.D.; Ogden, C. L. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8.
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. Journal of Child Psychology and Psychiatry 1997, 38, pp. 581-586. [CrossRef]
- Moretti, M. M.; Obsuth, I.; Craig, S. G.; Bartolo, T. An attachment-based intervention for parents of adolescents at risk: Mechanisms of change. Attachment & Human Development, 2015. 17(2), 119–135. [CrossRef]
- Moretti, M. M. Affect Regulation Checklist. Unpublished research measure and data. 2003. Simon Fraser University.
- Gratz, K. L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale., Journal of Psychopathology and Behavioral Assessment 2004, 26(1), 41-54. [CrossRef]
- Gross, J. J.; John, O. P. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being, Journal of Personality and Social Psychology 2003, 85(2), 348-362. [CrossRef]
- Shapiro, S. L.; Carlson, L. E.; Astin, J. A.; Freedman, B. Mechanisms of mindfulness, Journal of Clinical Psychology 2006, 62(3), 373-386. [CrossRef]
- Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html (accessed 3/2/2024).
- World Health Organization (WHO). https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index (accessed 3/2/2024).
- Kuczmarski, R. J.; Ogden, C. L.; Guo, S. S.; Grummer-Strawn, L. M.; Flegal, K. M.; Mei, Z.; Wei, R.; Curtin, L. R.; Roche, A. F.; Johnson, C. L. 2000 CDC Growth Charts for the United States: Methods and Development. Vital Health Stat 2002, 11(246).
- Chaplin, T. M.; Aldao, A. Gender differences in emotion expression in children: A meta-analytic review. Psychological Bulletin 2013, 139(4), 735-765. [CrossRef]
- Brennan, K. A.; Clark, C. L.; Shaver, P. R. Self-report measurement of adult attachment: An integrative overview. In J. A. Simpson & W. S. Rholes (Eds.), Attachment Theory and Close Relationships. New York: Guilford Press, 1998, pp. 46–76.
- Mikulincer, M.; Shaver, P. R. Attachment in Adulthood: Structure, Dynamics, and Change. New York, NY: Guilford Press, 2007.
- Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont Research Center for Children, Youth, & Families.
- Frick, P. J. Conduct Disorders and Severe Antisocial Behavior. New York, NY: Plenum Press, 1998.
- Barkley , R. A. ADHD and the Nature of Self-Control. New York, NY: Guilford Press, 1997.
- Parker, J. G.; Asher, S. R. Friendship and friendship quality in middle childhood: Links with peer group acceptance and feelings of loneliness and social dissatisfaction. Developmental Psychology 1993, 29(4), 611–621. [CrossRef]
- Eisenberg, N.; Fabes, R. A.; Spinrad, T. L. Prosocial Development, Handbook of Child Psychology: Vol. 3, Social, Emotional, and Personality Development, 6th ed, New York, NY: Wiley, 2006, pp. 646–718.
- Achenbach, T. M. (1991). Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry.
- Zahn-Waxler, C.; Klimes-Dougan, B.; Slattery, M. J. Internalizing problems of childhood and adolescence: Prospects, pitfalls, and progress in understanding the development of anxiety and depression. Development and Psychopathology 2000, 12(3), 443–466. [CrossRef]
- Frankel, L. A.; Hughes, S. O.; O'Connor, T. M.; Power, T. G.; Fisher, J. O.; Hazen, N. L. Parental Influences on Children's Self-Regulation of Energy Intake: Insights from Developmental Literature on Emotion Regulation. Journal of Obesity 2012, vol. 2012. [CrossRef]
- Rhee, K. E.; Lumeng, J. C.; Appugliese, D. P.; Kaciroti, N.; Bradley, R. H. Parenting styles and overweight status in first grade. Pediatrics 2006, vol. 117, no. 6, pp. 2047–2054. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).