1. Introduction
Neck strain/sprain is the most common type of diagnosis given to motor vehicle collision (MVC) occupants treated in United States hospital emergency departments [
1]. An anatomical non-systematic review by Curotolo et al. found tissue damage from collision to the “zygopophysical joint capsules, annuli fibrosi; partial or complete ruptures of capsules, ligaments, annuli fibrosi intra-articular contusions, intra-articular fractures; and transarticular synovial joint fractures” [
2]. Conditions such as headache, neck pain (NP), myelopathy with and without neuropathic radiculopathies resulting from MVC’s frequently become chronic and debilitating. Studies have reported between 17% and 45% of injured persons have lingering dysfunction, pain, and disability at long-term follow-up [
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14].
In patients with injuries resulting from a MVC, a correlation between S-shaped, kyphotic, or hypo-lordotic cervical curve configurations and cervicogenic pain, radiculopathies, and increased rates of degenerative discs have been reported. These abnormal structural configurations are associated with multiple symptoms and worsening of prognosis [
15,
16,
17,
18,
19,
20,
21,
22,
23]. According to Nightingale et al. [
24], referring to Chen and Lui [
25] “In a column with a fixed base, buckling is evidenced by an abrupt decrease in measured compressive load with increasing deflection and moment. Snap through buckling is characterized by a visible and rapid transition from one equilibrium configuration to another.” Biomechanical investigations confirm the sagittal cervical spine exhibits ‘snap-through’ type and ‘dynamic’ buckling behavior in response to impact loads, where the complexity is related to curve configuration [
24,
26,
27,
28].
In rear-end MVC’s, during the skull translation phase, many authors have described an S-Curve (1st order buckled mode) of the cervical lordosis [
29,
30,
31,
32,
33]. Altered static cervical curvatures of patients have been previously described as buckled modes/shapes [
34] but to our knowledge no study has shown that MVC’s cause cervical curve abnormalities post-impact. Since no study has conclusively demonstrated that the MVC itself is a causation of an abnormal static cervical lordosis, we wished to investigate this possibility. Using a retrospective consecutive case series design, 41 patients were obtained where a pre-injury cervical examination and x-ray were followed by a 2nd cervical examination and x-ray after exposure to MVC. The current study’s hypothesis is that MVC exposure will cause a buckling-type of altered cervical spine alignment segmentally and globally in the sagittal cervical spine.
2. Materials and Methods
2.1. Patient Data Collection
For the current investigation, we completed a 3 center retrospective consecutive case series review of records over a 2–3-year time-period. Patients were sought where an initial neutral lateral cervical radiograph and cervical spine examination was performed followed by a repeated examination and cervical radiograph after exposure to an MVC. In addition to lateral cervical radiographs, patient records were required to have completed the numerical pain rating score (NPRS) from 0-10 (where 0 = no pain and impairment,…, 10 =severe incapacitating pain) at both examinations. Many patients also completed the neck disability index (NDI).
Our article is a retrospective review of clinical records and is except from IRB approval under section 45 CFR 46.101(b)(4). See https://www.hhs.gov/ohrp/regulations-and-policy/decision-charts-pre-2018/index.html#c5
Exclusion criteria for patients in our study were: 1) pre-existing cervical spine fractures, 2) pre-existing cervical spine surgery, 3) non-ambulatory or unable to maintain a neutral cervical posture, 4) duration between examinations of more than 1 year, and 5) failure to present to the same clinic as the primary center within 6 weeks after the MVC. Forty-one patients were identified that fit our inclusion criteria. These persons ranged in age from 8-65 years and there were 15 males and 26 females.
2.2. Cervical Circular and Elliptical Modeling
All 82 (2 sets of 41 patients) lateral cervical spine radiographs were digitized with a sonic digitizer (GP-9, from Science Accessories Corp., Shelton, CT, U.S.A.). Digitized points included: 1) the posterior hard palate, 2) the posterior portion of the foramen magnum, 3) the anterior and posterior tubercle of the atlas, and 4) all 4 vertebral body corners of C2-C7. In total, 32 combined points on the skull and cervical vertebral bodies from C1-C7 were digitized. The digitization and modeling details have been previously reported however, some details are provided here [
35].
Our circular and elliptical models extend from the posterior-superior body corner of C2 to the posterior-inferior corner of the body of C7 or to T1; the model represents the path of the posterior vertebral body coordinates between these landmarks [
35]. Vertebral body x-y coordinates were stored in a database for a computer program written in FORTRAN 77 to run on a personal computer. An original computer code performed a least-squares approximation of each person’s cervical lordosis in the shape of an ellipse or a circle. The program iterates to find a best-fit model for each person by passing ellipses and circles, in the least-squares sense, through vertebral x-y coordinates along the posterior bodies. For each person’s best-fit ellipse, the program determined semi-major (a) and semi-minor (b) axes, b/a ratio, the portion of a quadrant (between 80° and 90°), which the elliptical segment comprised and for circular models the radii of curvature is determined [
35].
2.3. Radiographic Procedures & Variables
All three clinics followed the same standardized procedure for patient positioning during exposure of the lateral cervical radiographic [
35,
36]. Each patient stood next to the x-ray bucky with the shoulder touching lightly. Tube source was 183 cm (72 inches) away from the bucky and the collimation allowed the entire cervical spine to be visualized. The patient was instructed to gently nod the head a few times with eyes closed and assume a neutral “eyes-forward” position with eyes open to prevent sway. Once the patient was still, the image was acquired. This positioning has been shown to be repeatable and reliable [
36].
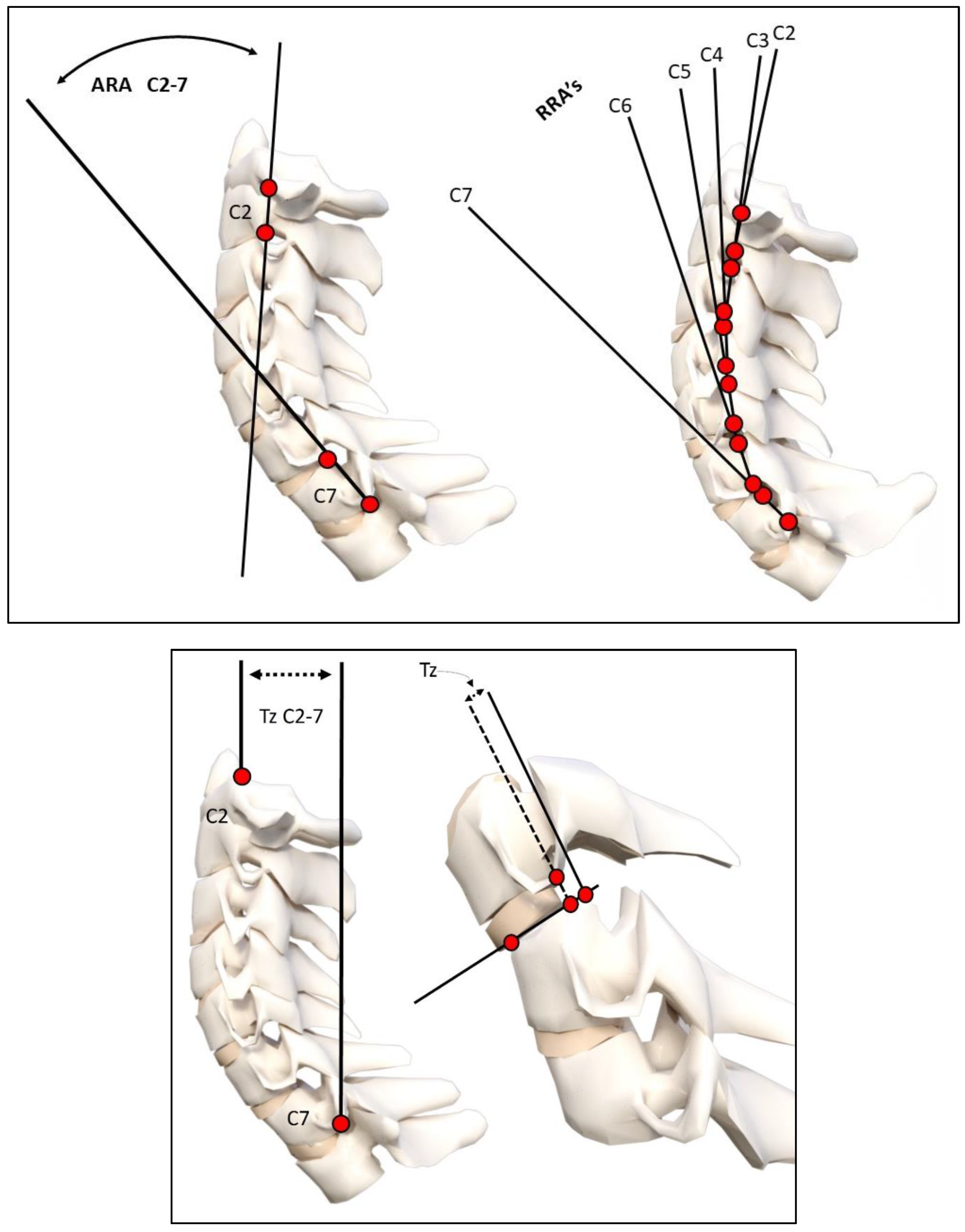
Using the digitized vertebral body x-y coordinates, sagittal cervical angular (rotations) and linear (translation) alignment variables were calculated. These variables included: 1) the intersection of posterior body lines at C2 and C7 forming a global angle of lordosis (ARA C2-C7), 2) intersection of juxtaposition posterior body lines forming relative rotation angles (RRA’s) from C2-C3 down to C6-C7, 3) a line through the posterior hard palate and the posterior foramen magnum relative to horizontal (Chamberlain’s line), 4) horizontal translation of the posterior superior vertebral body corner of C2 relative to a vertical line at the posterior inferior vertebral body corner of C7 (TzC2-C7), and 5) segmental forward and backward translations of juxta-positioned vertebra (retrolisthesis and anterolisthesis). See
Figure 1. A negative angular value indicates spinal extension or lordosis and a positive linear value indicates anterior translation. These methods of measurements have excellent examiner reliability and small error magnitudes [
37,
38].
2.4. Statistical Analysis
Descriptive statistics are presented as mean and standard deviations for all variables. Statistical comparisons of the changes in cervical modeling, radiographic alignment variables, and pain scores following exposure to a MVC were performed using a two-tailed, paired observations t-test. Patient data was initially imported into Microsoft Excel (2018 Microsoft Excel (office.microsoft.com/excel)) and statistical analysis was performed with SPSS version 29.
3. Results
3.1. Patient demographics
Patient demographics, passenger vehicle location, type of collisions, NPRS and NDI scores are presented in
Table 1. The majority of patients were in the front driver location (28/41) of the target vehicle involved in a rear-end collision (30/41). On average, patients’ pain intensity nearly doubled from a NRS of 2.7 to a 5.0 following exposure to a MVC; p < 0.001. Similarly, the NDI was available on a subset of 24 /41 (58.5%) patients and it was found to increase by a factor of two as well following exposure to the MVC (15.7% to 32.8%) indicating a change from mild to moderate impairment on the NDI.
3.2. Change in cervical curvature from MVC
The means, standard deviations, maximum and minimum values for the measured radiographic variables in the 41 patients are reported in
Table 2. An altered cervical curvature was identified following exposure to MVC and characterized by an increase in radius of circular modelling curvature, an 8° reduction (range of 40.7° loss to 5° increase) in the ARA C2-C7, and straightening / flexion of the mid cervical spine from C3-C5 (6.5° loss). In 3/41 participants a mild increase in the ARA C2-C7 was found however, the geometry was significantly altered with an increase in the radii of curvature.
Table 2 presents this data.
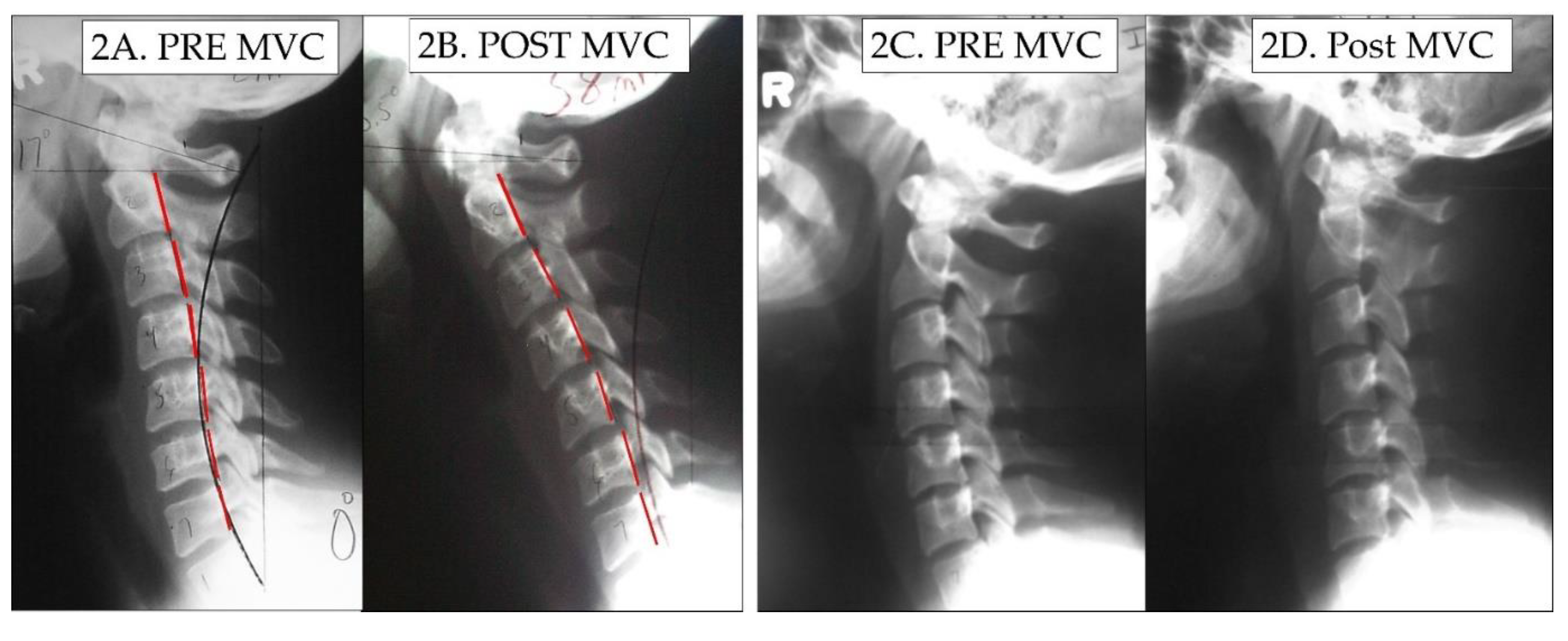
Figure 2 shows 2 female patients where the cervical curve is demonstrably altered from post MVC exposure compared to their initial lateral cervical radiographs.
3.3. Modeling results
In 2004, an average model as a piece of a circle with an angle of 34.5º between the posterior body tangents on C2 and C7 was reported [
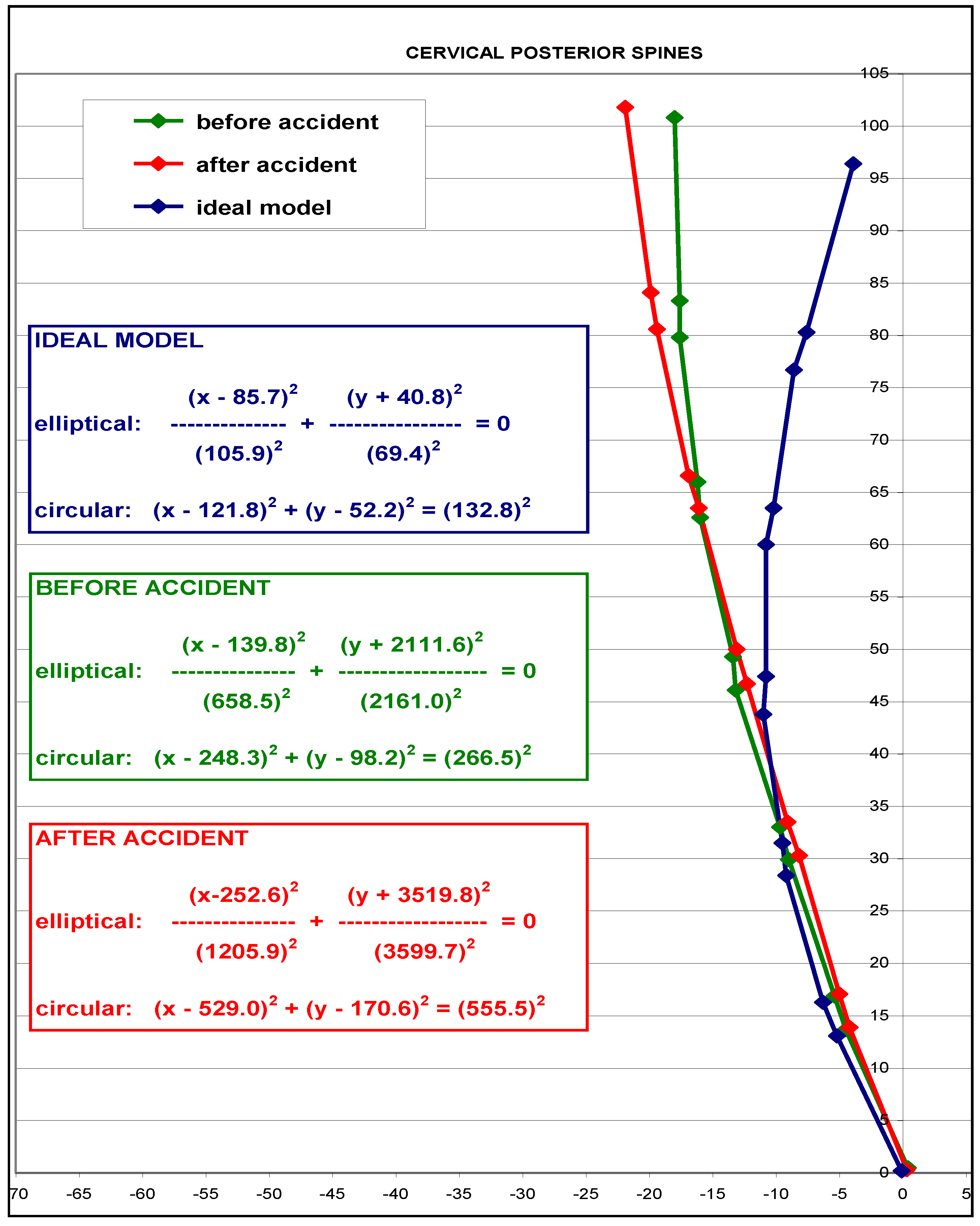
35]. This model is shown blue in
Figure 3 as a representative ‘idealized aligned model’ and is compared to the initial patient average (green model) and post MVC exposure (red model) average cervical models of the 41 participants. The averaged post MVC lateral cervical curve model approaches a 2nd order buckled mode with straightening / flexion of the mid-cervical segments C4-C6 compared to the pre-injury lateral cervical radiograph. The altered geometry is shown by the change in equation values and specifically by the increase in the radius of curvature on the before MVC vs. the after MVC model (radii of curve change from 266.5mm
2 to 555.5mm
2). Furthermore, the increase in anterior tranlsation of C2-C7 is shown in the post MVC model in
Figure 3.
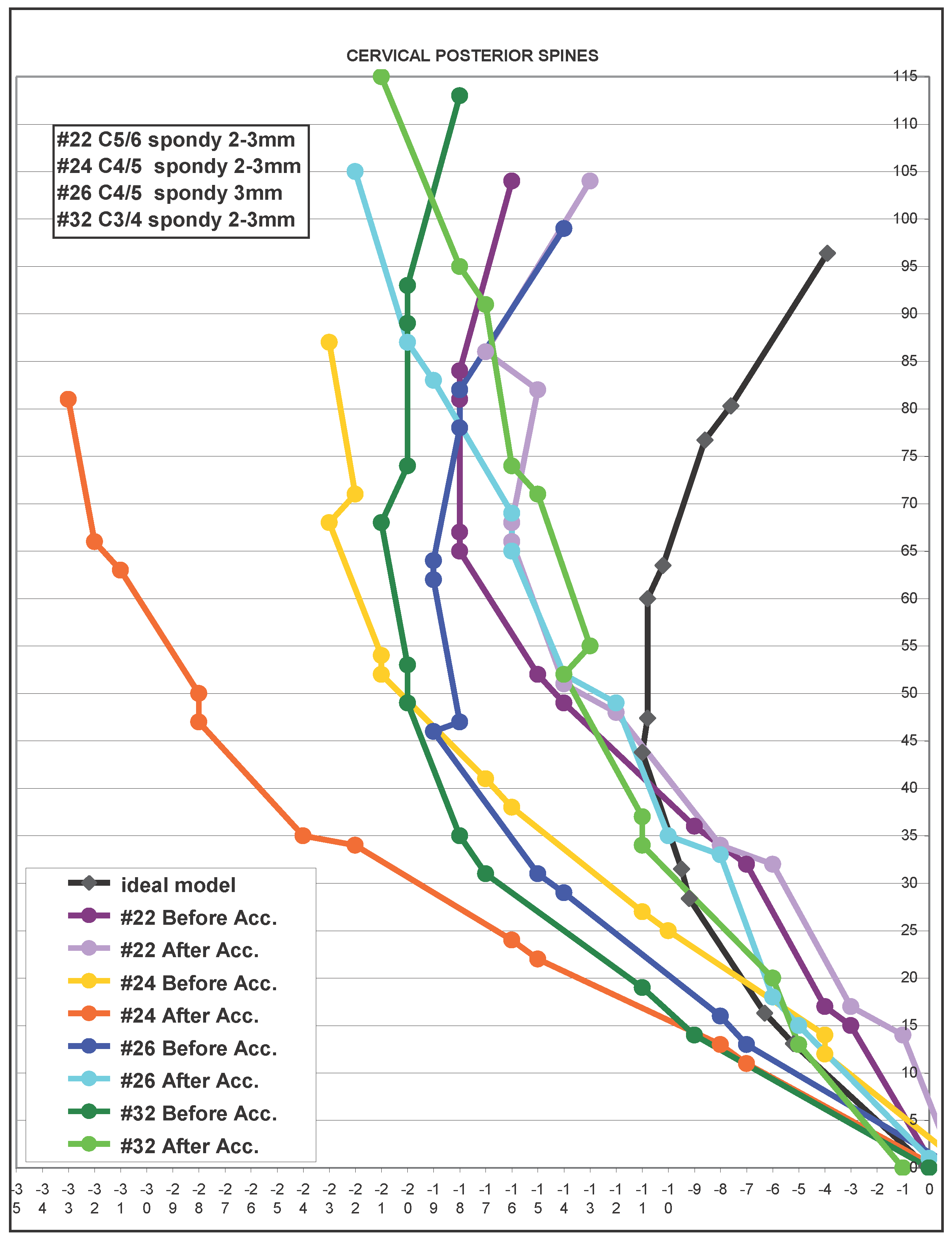
In 4/41 (10%) patients, significant segmental translations (retrolisthesis and anterolisthesis) on the post exposure MVC lateral cervical radiograph were found that were quite different in comparison to the initial pre-MVC lateral cervical radiograph. The magnitude of these segmental translations approached the limits of allowable maximum joint movement (3.5mm) before instability occurs and represents abnormal alignment suggestive of ligamentous injury.
Figure 4 presents the segmental translation of the individual segments identified on the Post MVC radiographs of these 4 patients. Each person’s model is shown pre- and post-MVC.
4. Discussion
The present study was undertaken to compare the sagittal cervical spine geometry and radiographic alignment within patients before and after exposure to a motor vehicle collision (MVC). The cervical model and radiographic alignment variables before and after MVC exposure confirm our primary hypothesis that MVC causes buckling type of alignment in the sagittal cervical spine that is noted both segmentally and globally. In our 41 participants, a general hypo-lordotic cervical curvature was identified following exposure to MVC and was characterized by an increase in radius of curvature, an approximate 8° reduction (up to 40.7° in one patient) in the ARA C2-C7, and mild kyphosis of the mid cervical spine from C3-C5 (6.5° loss). Finally, a mild increase in forward head posture was found following exposure to MVC as measured with the C2-C7 translation distance. To our knowledge, our investigation is the first study we know to report abnormal cervical curvature within a person following exposure to a MVC; however, our findings seem consistent with the general radiographic findings in MVC injured persons compared to matched control groups [
17,
18,
19,
20,
21,
22,
23,
39].
4.1. Loss of lordosis in MVC populations
Taken as a whole, the literature detailing patients involved in a MVC and those with whiplash associated disorders (WAD) indicates that hypolordosis, [
16,
17] straightened cervical curves, [
16,
17,
18,
19] S-curves, [
18,
21,
23] and kyphotic curves [
15,
18,
19,
20,
21] are risk factors for and are statistically correlated to generalized poor long-term outcomes including CNP. Data from Marshall and Tuchin [
39], for example, provides evidence that patients involved in a MVC injury have a 10° mean reduction in the C1-C7 Cobb angle of cervical lordosis compared to a control group. Complicating matters is that conflicting results have been reported whereby the relationship of altered cervical curvatures to prognostic outcomes following exposure to an MVC (both short and long-term) has been refuted [
40,
41,
42,
43]. Still, according to our review, the majority of the literature indicates that patients with injuries resulting from an MVC have a significantly greater frequency and magnitude of altered cervical curve configurations [
15,
16,
17,
18,
19,
20,
21,
23,
39]. This information implies one of two things: 1) that either patients presenting with a pre-existing abnormal cervical spine curvature are predisposed to injury of their cervical spine from the MVC event or 2) that the MVC event causes a mechanical alteration (buckling event) in the alignment of the lordotic cervical alignment leading to increased risk of injury and future pain and disability. In fact, the first of these scenarios has been preliminarily reported in the literature [
44,
45,
46] and the results of the current investigation would indicate that the second scenario also holds true.
4.2. Altered sagittal cervical geometry as a buckling type alignment
An S-shape in the cervical column can be described as the 1st order buckled mode, flexion-extension-flexion in any region as the 2nd order buckled mode, etc…, where these are increasing in complexity. During impact experiments, the cervical spine has been found to exhibit “snap-through” and dynamic type buckling behavior [
24,
26,
27,
28,
29]. The various buckled modes are the allowable shapes that the sagittal cervical curve can adopt without failure and these can be correlated to eigenvalues in solutions of nonlinear partial differential equations used to model structures [
25,
47,
48]. During exposure to a MVC the cervical spine is subjected to complex inertial loading where bending, shear, and compression loads act on the column. During the skull translation phase many authors have described an S-Curve (1st order buckled mode) of the cervical lordosis [
29,
30,
31,
32,
33]. Similarly, Matsunaga et al. [
34] described altered static cervical curvatures, including S-curves and retrolistheses, as buckled modes or shapes. The cervical spine exhibits “snap-through” and/or dynamic buckling behavior in some cases exposed to high inertial loading as in cervical acceleration-deceleration. We believe this to be a possible explanation as to why the average post MVC alignment of our population is consistent with a 2
nd order buckling alignment (extension C6-T1, flexion C4-C6, and extension C1-C4) as shown in
Figure 3 and some of our patients’ curves developed higher order buckling (3
rd order or greater as shown in selected cases in
Figure 4). Our results are in agreement with those of Kristjansson and colleagues [
21] who identified that females involved in a MVC had decreased ration of the upper vs. lower cervical lordosis with a flexion at the C4/C5 segmental level.
4.3. Pain increase post-MVC and clinical consideration
In our population, following exposure to a MVC, the average NRS pain score and neck disability index were found to nearly double; being reported as a 5/10 for the NRS. Interestingly, investigations have found that pain intensity scores following a MVC are predictive of long-term outcomes in patients with acute WAD [
2,
3,
4,
6]. A pain score of 5/10 on a NRS is considered moderate NP associated with significant disability [
2,
49]. The significance of this increase in pain cannot be understated in our population of patients. NP is one of the largest contributors to musculoskeletal global burden of disease [
49,
50,
51]. The failure to properly diagnosis neck pain and the parameters of injury can lead to increased risk of CNP due to increased mechanical stresses and strains on the nociceptive pain sensitive tissues of the spine. Increased mechanical stress and strain on internal and external spine structures, worsen ROM, strength, and worsen outcomes both short- and long-term, including degenerative changes [
2,
3,
4,
5,
6,
7,
18,
20,
51].
Trauma physicians and Emergency Room (ER) physicians should be aware of these abnormal spine parameters visualized via cervical radiography prior to considerations for differential diagnosis, and add to the decision for invasive or pharmacologic interventions, determination of referral recommendations for pharmacologic, therapeutic and/or manual treatments. Surgical referral following stabilization of triage in the ER by the ER physician must have the clinical certainty that the buckling of the cervical spine is significant enough for this type of referral. Conservative, non-invasive and non-opioid pharmacologic interventions should be considered if possible [
52,
53,
54]. Proper referral for non-invasive vs. surgical intervention could have a significant impact on the patient outcome as well as the financial burden of the injury due to the MVC.
4.4. Safety of radiography for MVC patients
Radiography is the criterion standard for spine conditions. The safety of radiography for injured patients with suspected spine conditions has been firmly established and the fear of radiography on the part of patients, physicians and others is not warranted [
55,
56,
57,
58]. Additionally, the failure to use radiography to assess the condition of the spine after injury and prior to treatment could lead to poor outcomes, including wrong diagnosis, improper treatment applications, and could increase the likelihood of future pain, dysfunction, and possible escalation of intervention including surgery [
56,
57,
58]. Lastly, regarding specific conservative care rehabilitation procedures for MVC injured patients, recent results demonstrate that the judicious usage of cervical spine radiography aids in the continued management of cervical spine disorders in patients with loss of the cervical curvature resulting from exposure to MVC [
59]. (spacing off here)
4.5. Study limitations and future recommendations
The current investigation has several limitations inherent in its design. The limitations include problems with retrospective review of records, up to a year time frame from initial examination to the 2nd examination after MVC exposure, and a limited sample size. The cervical lordosis has been found to be stable in CNP patients not undergoing treatment intervention for up to 10 years [
36,
60], and conservative treatments show long-term stability when lordosis is restored [
61]. Therefore, we doubt that the time between exams caused abnormalities on the second lateral cervical radiograph, but we cannot rule out the possibility of other non-reported injuries confounding the outcome. The limited sample size did not allow for adequate correlation between the different impact directions and consequent curve abnormality. Future investigations should compare different directions of MVC and compare the buckling shape, injuries sustained, and presenting symptoms. Additional studies should investigate the magnitude of the buckling with success of conservative and invasive treatments and outcome measure changes with long-term follow-up. Because this study involves injured patients, randomized trials with controls would be unethical and should not be considered, however, large retrospective studies of patients with spinal radiographs prior to and following MVC should be funded and undertaken.
5. Conclusions
An altered cervical curvature was identified following exposure to a MVC in 41 retrospective consecutive cases from three patient centers. The 41 patients had a prior lateral cervical radiograph for comparison to a post MVC lateral cervical radiograph. The abnormal curvature was characterized by an increase in radius of curvature, an approximate 8° reduction in C2-C7 lordosis, and mild kyphosis of the mid cervical spine, and a slight increase in anterior translation of C2-C7 sagittal balance. Ten percent of the patients developed segmental translations that approached instability limits. Overall, the modelling result of the sagittal cervical lordosis indicates that the post MVC alignment approximates a 2nd order buckling alignment indicating significant alteration in curve geometry. MVCs would appear to be a causative factor for lateral cervical curve abnormalities and as such need more attention in terms of research and rehabilitation methods in participants after exposure to a MVC. Future research should include prospective evaluation of curvature change immediately following exposure to an MVC and future modeling investigations should consider incorporating a post-crash alignment analysis to identify if change in cervical sagittal alignment might be the result of specific patient and crash characteristics. Finally, future randomized trials are needed to explore the results of cervical curve restoration in MVC injured populations to identify if this may benefit specific subgroups of patients suffering from chronic pain and impairments.
Author Contributions
Conceptualization, D.E.H.; methodology, D.E.H; data acquisition, E.A.K.; P.A.O.; J.R.F.; I.M.M.; D.E.H.; writing—original draft preparation, J.W.H. and D.E.H.; writing—review and editing, I.M.M.; D.E.H.; J.W.H.; P.A.O.; Supervision, I.M.M.; D.E.H.; funding acquisition, D.E.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Chiropractic BioPhysics, NonProfit.
Institutional Review Board Statement
Not Applicable
Informed Consent Statement
All subjects signed informed consent for evaluation and diagnostic procedures as part of their clinical evaluation at the individual providers.
Data Availability Statement
Additional pertinent data is available upon request.
Conflicts of Interest
Author E.A.K., I.M.M. declare no competing interests. J.W.H. is a compensated researcher for CBP Non-Profit, Inc. P.A.O. is a compensated consultant for Chiropractic BioPhysics, NonProfit, Inc. J.R.F. is the CEO of PostureCo, Inc. and receives compensation for the sale of PostureRay® software. D.E.H. is the CEO of Chiropractic BioPhysics® (CBP®) and provides post-graduate education to health care providers and physicians. Spine rehabilitation devices are distributed through his company. D.E.H. is the president of CBP Non-Profit, Inc., a not-for-profit spine research foundation.
References
- Quinlan, K.P.; Annest, J.L.; Myers, B.; Ryan, G.; Hill, H. Neck strains and sprains among motor vehicle occupants-United States, 2000. Accid. Anal. Prev. 2004, 36, 21–7. [Google Scholar] [CrossRef] [PubMed]
- Curatolo, M.; Bogduk, N.; Ivancic, P.C.; McLean, S.A.; Siegmund, G.P.; Winkelstein, B.A. The role of tissue damage in whiplash-associated disorders: discussion paper 1. Spine 2011, 36(25 Suppl), S309–15. [Google Scholar] [CrossRef]
- Hendriks, E.J.; Scholten-Peeters, G.G.; Van der Windt, D.A.; Neeleman-van der Steen, C.W.; Oostendorp, R.A.; Verhagen, A.P. Prognostic factors for a poor recovery in acute whiplash patients. Pain 2005, 114, 408–416. [Google Scholar] [CrossRef]
- Sterling, M.; Jull, G.; Kenardy, J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain 2006, 122, 102–108. [Google Scholar] [CrossRef]
- Rebbeck, T.; Sindhusake, D.; Cameron, I.D.; Rubin, G.; Feyer, A.M.; Walsh, J.; Gold, M.; Schofield, W.N. A prospective cohort study of health outcomes following whiplash associated disorders in an Australian population. Inj. Prev. 2006, 12, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Fundaun, J.; Kolski, M.; Baskozos, G.; Dilley, A.; Sterling, M.; Schmid, A.B. Nerve pathology and neuropathic pain after whiplash injury: a systematic review and meta-analysis. Pain. 2022, 163, e789–e811. [Google Scholar] [CrossRef] [PubMed]
- Braaf, M.M.; Rosne, R.S. Trauma of cervical spine as cause of chronic headache. J. Trauma 1975, 15, 441–446. [Google Scholar] [CrossRef]
- Nagasawa, A.; Sakakibara, T.; Takahashi, A. Roentgenographic findings of the cervical spine in tension-type headache. Headache 1993, 33, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-las-Peñas, C.; Alonso-Blanco, C.; Cuadrado, M.L. , et al. Forward head posture and neck mobility in chronic tension-type headache: a blinded, controlled study. Cephalalgia 2006, 26, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Vernon, H.; Steiman, I.; Hagino, C. Cervicogenic dysfunction in muscle contraction headache and migraine: a descriptive study. J. Manipulative Physiol. Ther. 1992, 15, 418–429. [Google Scholar]
- Ferracini, G.N.; Chaves, T.C.; Dach, F.; et al. Analysis of the cranio-cervical curvatures in subjects with migraine with and without neck pain. Physiotherapy 2017, 103, 392–399. [Google Scholar] [CrossRef]
- Buell, T.J.; Buchholz, A.L.; Quinn, J.C.; et al. Importance of sagittal alignment of the cervical spine in the management of degenerative cervical myelopathy. Neurosurg. Clin. N. Am. 2018, 29, 69–82. [Google Scholar] [CrossRef]
- Shamji, M.F.; Ames, C.P.; Smith, J.S.; et al. Myelopathy and spinal deformity: relevance of spinal alignment in planning surgical intervention for degenerative cervical myelopathy. Spine 2013, 38, S147–S148. [Google Scholar] [CrossRef]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; et al. The relationship between forward head posture and neck pain: a systematic review and meta-analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef] [PubMed]
- Casbas, L.; Chauffour, X.; Cau, J.; Bossavy, J.P.; Midy, D.; Baste, J.C.; Barret, A. Post-traumatic thoracic outlet syndromes. Ann. Vasc. Surg. 2005, 19, 25–28. [Google Scholar] [CrossRef]
- Giuliano, V.; Giuliano, C.; Pinto, F.; Scaglione, M. Soft tissue injury protocol (STIP) using motion MRI for cervical spine trauma assessment. Emergency Radiology 2004, 10, 241–245. [Google Scholar] [CrossRef]
- Giuliano, V.; Giuliano, C.; Pinto, F.; Scaglione, M. The use of flexion and extension MR in the evaluation of cervical spine trauma: initial experience in 100 trauma patients compared with 100 normal subjects. Emergency Radiology 2002, 9, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Norris, S.H.; Watt, I. The prognosis of neck injuries resulting from rear-end vehicle collisions. J. Bone Joint Surg. Br. 1983, 65, 608–611. [Google Scholar] [CrossRef]
- Zatzkin, H.R.; Kveton, F.W. Evaluation of the cervical spine in whiplash injuries. Radiology 1960, 75, 577–583. [Google Scholar] [CrossRef]
- Hohl, M. Soft-tissue injuries of the neck in automobile accidents. J Bone Joint Surg. Am. 1974, 56, 1675–1682. [Google Scholar] [CrossRef]
- Kristjansson, E.; Jonsson H., Jr. Is the Sagittal configuration of the cervical spine changed in women with chronic whiplash syndrome? A comparative computer-assisted radiographic assessment. J Manipulative Physiol. Ther. 2002, 25, 550–555. [Google Scholar] [CrossRef]
- Jackson, R. The positive findings in alleged neck injuries. Am. J. Orthop. Surg. 1964, 30, 178–87. [Google Scholar]
- Griffiths, H.J.; Olson, P.N.; Everson, L.I.; Winemiller, M. Hyperextension strain or "whiplash" injuries to the cervical spine. Skeletal Radiology 1995, 24, 263–266. [Google Scholar] [CrossRef]
- Nightingale, R.W.; Camacho, D.L.; et. al. Inertial properties and loading rates affect buckling modes and injury mechanisms in the cervical spine. J. Biomech. 2000, 33, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.F.; Lui, E.M. Structural Instability: Theory and Implementation; Elsevier: New York; pp. 4–10.
- Yoganandan, N.; Pintar, F.A.; Arnold, P.; Reinartz, J.; Cusick, J.F.; Maiman, D.J.; Sances, A. Continuous motion analysis of the head-neck complex under impact. J. Spinal Disorders 1994, 7, 420–428. [Google Scholar] [CrossRef]
- Nightingale, R.W.; McElhaney, J.H.; Richardson, W.J.; Myers, B.S. Dynamic responses of the head and cervical spine axial impact loading. J Biomech. 1996, 29, 307–318. [Google Scholar] [CrossRef]
- Nightingale, R.W.; McElhaney, J.H.; Richardson, W.J.; Best, T.M.; Myers, B.S. Experimental impact injury to the cervical spine: Relating motion of the head and the mechanism of injury. J Bone Joint Surg. Am. 1996, 78, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, M.; Kaneoka, K.; Ono, K.; Sakane, M.; Ujihashi, S.; Ochiai, N. Neck injury mechanisms during direct face impact. Spine 2006, 31, 903–908. [Google Scholar] [CrossRef]
- Garcia, T.; Ravani, B. A biomechanical evaluation of whiplash using a multi-body dynamic model. J Biomech Eng. 2003, 125, 254–265. [Google Scholar] [CrossRef] [PubMed]
- Panjabi, M.M.; Pearson, A.M.; Ito, S.; Ivancic, P.C.; Wang, J.L. Cervical spine curvature during simulated whiplash. Clin. Biom. 2004, 19, 1–9. [Google Scholar] [CrossRef]
- Garcia, T.; Ravani, B. A biomechanical evaluation of whiplash using a multi-body dynamic model. J Biomech Eng. 2003, 125, 254–265. [Google Scholar] [CrossRef] [PubMed]
- Stemper, B.D.; Yoganandan, N.; Pintar, F.A. Effects of abnormal posture on capsular ligament elongations in a computational model subjected to whiplash loading. J Biomech. 2005, 38, 1313–1323. [Google Scholar] [CrossRef]
- Matsunaga, S.; Sakou, T.; Sunahara, N.; Oonishi, T.; Maeda, S.; Nakanisi, K. Biomechanical analysis of buckling alignment of the cervical spine. Spine 1997, 22, 765–771. [Google Scholar] [CrossRef]
- Harrison, D.D.; Harrison, D.E.; Janik, T.J.; Cailliet, R.; Haas, J.W.; Ferrantelli, J.; Holland, B. Modeling of the Sagittal Cervical Spine as a Method to Discriminate Hypo-Lordosis: Results of Elliptical and Circular Modeling in 72 Asymptomatic Subjects, 52 Acute Neck Pain Subjects, and 70 Chronic Neck Pain Subjects. Spine 2004, 29, 2485–2492. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Colloca, C.J.; Betz, J.; Janik, T.J.; Holland, B. Repeatability of Posture Overtime, X-ray Positioning, and X-ray Line Drawing: An Analysis of Six Control Groups. J. Manipulative Physiol. Ther. 2003, 26, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Cailliet, R.; Troyanovich, S.J.; Janik, T.J.; Holland, B. Cobb Method or Harrison Posterior Tangent Method: Which is Better for Lateral Cervical Analysis? Spine 2000, 25, 2072–2078. [Google Scholar] [CrossRef]
- Pivotto, L.R.; Navarro, I.J.R.L.; Candotti, C.T. Radiography and photogrammetry-based methods of assessing cervical spine posture in the sagittal plane: A systematic review with meta-analysis. Gait Posture 2021, 84, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Marshall, D.L. Correlation of cervical lordosis measurement with incidence of motor vehicle accidents. J Australian Chiropractic and Osteopathy 1996, 5, 79–85. [Google Scholar]
- Matsumoto, M.; Fujimura, Y.; Suzuki, N.; Toyama, Y.; Shiga, H. Cervical curvature in acute whiplash injuries: prospective comparative study with asymptomatic subjects. Injury 1998, 29, 775–778. [Google Scholar] [CrossRef]
- Johansson, M.P.; Baann Liane, M.S.; Bendix, T.; Kasch, H.; Kongsted, A. Does cervical kyphosis relate to symptoms following whiplash injury? Man Ther. 2011, 16, 378–383. [Google Scholar] [CrossRef]
- Beltsios, M.; Savvidou, O.; Mitsiokapa, E.A.; Mavrogenis, A.F.; Kaspiris, A.; Efstathopoulos, N.; Papagelopoulos, P.J. Sagittal alignment of the cervical spine after neck injury. Eur. J. Orthop. Surg. Traumatol. 2013, 23 Suppl 1, S47–51. [Google Scholar] [CrossRef]
- Linsenmaier, U.; Deak, Z.; Krtakovska, A.; Ruschi, F.; Kammer, N.; Wirth, S.; Reiser, M.; Geyer, L. Emergency radiology: straightening of the cervical spine in MDCT after trauma--a sign of injury or normal variant? Br. J. Radiol. 2016, 89, 20150996. [Google Scholar] [CrossRef]
- Stemper, B.D.; Yoganandan, N.; Pintar, F.A. Effects of abnormal posture on capsular ligament elongations in a computational model subjected to whiplash loading. J. Biomech. 2005, 38, 1313–23. [Google Scholar] [CrossRef]
- Frechede, B.; Bertholon, N.; Saillant, G.; Lavaste, F. ; W. Skalli W. Finite element model of the human neck during omni-directional impacts. Part II: relation between cervical curvature and risk of injury, Computer Methods in Biomechanics and Biomedical Engineering, 2006, 9, 379–386. [Google Scholar] [CrossRef]
- Fréchède, B.; Bertholon, N.; Le Coz, J.Y.; Lavaste, F.; Skalli, W. Finite element model of the human neck during omni-directional impacts. Revue Européenne des Éléments 2005, 14, 463–485. [Google Scholar] [CrossRef]
- Gilmore, R. Catastrophe Theory for Scientists and Engineers; Dover Publications: New York, 1981. [Google Scholar]
- Pilkey, W.D.; Wunderlich, W. Mechanics of structures: variational and computational methods; Boca Raton; CRC Press, 1994; pp. 617–635. [Google Scholar] [CrossRef]
- Fejer, R.; Jordan, A.; Hartvigsen, J. Categorizing the severity of neck pain: establishment of cut-points for use in clinical and epidemiological research. Pain 2005, 119, 176–182. [Google Scholar] [CrossRef]
- Shin, D.W.; Shin, J.I.; Koyanagi, A.; Jacob, L.; Smith, L.; Lee, H.; Chang, Y.; Song, T.J. Global, regional, and national neck pain burden in the general population, 1990-2019: An analysis of the global burden of disease study 2019. Front Neurol. 2022, 13, 955367. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.T.; Aris, I.M.; Snyder, B.D.; Harris, M.B.; Kang, J.D.; Murray, M.; Rodriguez, E.K.; Nazarian, A. Musculoskeletal health: an ecological study assessing disease burden and research funding. Lancet Reg. Health Am. 2024, 29, 100661. [Google Scholar] [CrossRef]
- Werndle, M.C.; Myers, J.; Mortimer, A. Missed cervical spine injuries: aim for the top. Emerg Radiol. 2022, 29, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Preuss, C.V.; Kalava, A.; King, K.C. Prescription of Controlled Substances: Benefits and Risks. [Updated 2023 Apr 29]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island (FL), 2024. [Google Scholar]
- Beaudoin, F.L.; Gutman, R.; Merchant, R.C.; Clark, M.A.; Swor, R.A.; Jones, J.S.; Lee, D.C.; Peak, D.A.; Domeier, R.M.; Rathlev, N.K.; McLean, S.A. Persistent pain after motor vehicle collision: comparative effectiveness of opioids vs nonsteroidal antiinflammatory drugs prescribed from the emergency department-a propensity matched analysis. Pain. 2017, 158, 289–295. [Google Scholar] [CrossRef]
- Calabrese, E.J.; Agathokleous, E.; Giordano, J.; et al. Manhattan Project genetic studies: Flawed research discredits LNT recommendations. Environ. Pollut., 2023, 319, 120902. [Google Scholar] [CrossRef]
- Wijetunga, C.; Brady, Z.; Varma, D.K. Responsible use of advanced imaging technology. How well are risks and benefits of radiation recognised? Injury. 2018, 49, 883–884. [Google Scholar] [CrossRef]
- Oakley, P.A.; Harrison, D.E. Radiophobia: 7 Reasons Why Radiography Used in Spine and Posture Rehabilitation Should Not Be Feared or Avoided. Dose Response. 2018, 16, 1–10. [Google Scholar] [CrossRef]
- Oakley, P.A.; Harrison, D.E. X-Ray Hesitancy: Patients' Radiophobic Concerns Over Medical X-rays. Dose Response. 2020, 18, 1559325820959542. [Google Scholar] [CrossRef]
- Norton, T.C.; Oakley, P.A.; Haas, J.W.; Harrison, D.E. Positive Outcomes Following Cervical Acceleration-Deceleration (CAD) Injury Using Chiropractic BioPhysics® Methods: A Pre-Auto Injury and Post-Auto Injury Case Series. J. Clin. Med. 2023, 12, 6414. [Google Scholar] [CrossRef] [PubMed]
- Gore, D.R. Roentgenographic findings in the cervical spine in asymptomatic persons: A 10 year follow-up. Spine 2001, 26, 2463–2466. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.M.; Diab, A.A.; Harrison, D.E. The Efficacy of Cervical Lordosis Rehabilitation for Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial with 2-Year Follow-Up. J. Clin. Med. Published 2022 Nov 2. 2022, 11, 6515. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).