Submitted:
20 February 2024
Posted:
21 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Coating of Medical Devices
2.1. Deposition of Antimicrobial Films
2.2. Deposition of Biocompatible and Adhesive Coatings
3. Plasma as a Therapeutic Intervention
3.1. Direct Application of Plasma to Tissue
3.2. Combinations of Plasma with Traditional Pharmaceuticals
3.3. Interactions of Plasma with Liquids
4. Decontamination of Unwanted Pharmaceutical Active Ingredients
5. Conclusions
References
- E. J. Gildersleeve and R. Vaßen, ‘Thermally Sprayed Functional Coatings and Multilayers: A Selection of Historical Applications and Potential Pathways for Future Innovation’, J. Therm. Spray Technol., vol. 32, no. 4, pp. 778–817, Apr. 2023. [CrossRef]
- J. R. Hollahan, ‘Rare gas plasma polymerization of benzene at −196°C’, Makromol. Chem., vol. 154, no. 1, pp. 303–308, 1972. [CrossRef]
- H. Yasuda, Plasma Polymerization. Orlando: Academic Press, 1985.
- H. O. Pierson, Handbook of Chemical Vapour Deposition. New York: Noyes Publication, 1999.
- A. M. Wróbel, A. Walkiewicz-Pietrzykowska, J. E. Klemberg-Sapieha, Y. Nakanishi, T. Aoki, and Y. Hatanaka, ‘Remote Hydrogen Plasma Chemical Vapor Deposition from (Dimethylsilyl)(trimethylsilyl)methane. 1. Kinetics of the Process; Chemical and Morphological Structure of Deposited Silicon−Carbon Films’, Chem. Mater., vol. 15, no. 8, pp. 1749–1756, Apr. 2003. [CrossRef]
- G. P. Lopez and B. D. Ratner, Plasma Polymerization and Plasma Interactions with Polymeric Materials: Proceedings of the Symposium on Plasma Polymerization and Plasma Interactions with Polymeric Materials, Held at the ACS 199th National Meeting in Boston, Massachusetts, April 1990. Wiley, 1990.
- L. M. Han, K. Rajeshwar, and R. B. Timmons, ‘Film Chemistry Control and Electrochemical Properties of Pulsed Plasma Polymerized Ferrocene and Vinylferrocene’, Langmuir, vol. 13, no. 22, pp. 5941–5950, Oct. 1997. [CrossRef]
- M. E. Ryan, A. M. Hynes, and J. P. S. Badyal, ‘Pulsed Plasma Polymerization of Maleic Anhydride’, Chem. Mater., vol. 8, no. 1, pp. 37–42, Jan. 1996. [CrossRef]
- S. R. Coulson, I. S. Woodward, J. P. S. Badyal, S. A. Brewer, and C. Willis, ‘Plasmachemical Functionalization of Solid Surfaces with Low Surface Energy Perfluorocarbon Chains’, Langmuir, vol. 16, no. 15, pp. 6287–6293, Jul. 2000. [CrossRef]
- P. A. F. Herbert, L. O’Neill, and J. Jaroszyńska-Wolińska, ‘Soft Plasma Polymerization of Gas State Precursors from an Atmospheric Pressure Corona Plasma Discharge’, Chem. Mater., vol. 21, no. 19, pp. 4401–4407, Oct. 2009. [CrossRef]
- L. J. Ward, W. C. E. Schofield, J. P. S. Badyal, A. J. Goodwin, and P. J. Merlin, ‘Atmospheric Pressure Plasma Deposition of Structurally Well-Defined Polyacrylic Acid Films’, Chem. Mater., vol. 15, no. 7, pp. 1466–1469, Apr. 2003. [CrossRef]
- L. J. Ward, W. C. E. Schofield, J. P. S. Badyal, A. J. Goodwin, and P. J. Merlin, ‘Atmospheric Pressure Glow Discharge Deposition of Polysiloxane and SiOx Films’, Langmuir, vol. 19, no. 6, pp. 2110–2114, Mar. 2003. [CrossRef]
- M. Tatoulian, F. Arefi-Khonsari, and J.-P. Borra, ‘Deposition of Organic Coatings at Atmospheric Pressure from Liquid Precursors’, Plasma Process. Polym., vol. 4, no. 4, pp. 360–369, 2007. [CrossRef]
- L.-A. O’Hare, L. O’Neill, and A. J. Goodwin, ‘Anti-microbial coatings by agent entrapment in coatings deposited via atmospheric pressure plasma liquid deposition’, Surf. Interface Anal., vol. 38, no. 11, pp. 1519–1524, 2006. [CrossRef]
- D. Pignatelli et al., ‘Plasma assisted deposition of free-standing nanofilms for biomedical applications’, Plasma Process. Polym., vol. 13, no. 12, pp. 1224–1229, 2016. [CrossRef]
- P. Heyse, M. B. J. Roeffaers, S. Paulussen, J. Hofkens, P. A. Jacobs, and B. F. Sels, ‘Protein Immobilization Using Atmospheric-Pressure Dielectric-Barrier Discharges: A Route to a Straightforward Manufacture of Bioactive Films’, Plasma Process. Polym., vol. 5, no. 2, pp. 186–191, 2008. [CrossRef]
- G. Da Ponte, E. Sardella, F. Fanelli, S. Paulussen, and P. Favia, ‘Atmospheric Pressure Plasma Deposition of Poly Lactic Acid-Like Coatings with Embedded Elastin’, Plasma Process. Polym., vol. 11, no. 4, pp. 345–352, 2014. [CrossRef]
- S. Malinowski, P. A. F. Herbert, J. Rogalski, and J. Jaroszyńska-Wolińska, ‘Laccase Enzyme Polymerization by Soft Plasma Jet for Durable Bioactive Coatings’, Polymers, vol. 10, no. 5, Art. no. 5, May 2018. [CrossRef]
- A. Los, D. Ziuzina, D. Boehm, P. Bourke, and E. Al, ‘Efficacy of Cold Plasma for Direct Deposition of Antibiotics as a Novel Approach for Localized Delivery and Retention of Effect’, Dec. 2019. [CrossRef]
- D. O’sullivan, H. McArdle, J.-A. O’Reilly, R. J. O’Kennedy, R. Forster, and L. O’Neill, ‘Plasma deposition of collagen for cell-culture applications’, Plasma Process. Polym., vol. 17, no. 3, p. 1900147, 2020. [CrossRef]
- ‘Global Medical Device Coating Market Size Analysis Report’. Accessed: Jan. 09, 2024. [Online]. Available: https://www.bccresearch.com/market-research/healthcare/medical-device-coatings-report.html.
- A. Dao et al., ‘Antibacterial Plasma Polymer Coatings on 3D Materials for Orthopedic Applications’, Adv. Mater. Interfaces, vol. n/a, no. n/a, p. 2300063. [CrossRef]
- T. Egghe, R. Morent, R. Hoogenboom, and N. D. Geyter, ‘Substrate-independent and widely applicable deposition of antibacterial coatings’, Trends Biotechnol., vol. 41, no. 1, pp. 63–76, Jan. 2023. [CrossRef]
- R. Q. Baculi, G. M. Malapit, and L. E. Abayao, ‘Atmospheric pressure plasma deposition of silver nanoparticles on bark fabric for bacterial growth inhibition’, J. Text. Inst., vol. 114, no. 1, pp. 142–150, Jan. 2023. [CrossRef]
- A. Loesch-Zhang, A. Geissler, and M. Biesalski, ‘Plasma polymerization of biogenic precursors’, Plasma Process. Polym., vol. 20, no. 10, p. e2300016, 2023. [CrossRef]
- K. Prasad, S. Sasi, J. Weerasinghe, I. Levchenko, and K. Bazaka, ‘Enhanced Antimicrobial Activity through Synergistic Effects of Cold Atmospheric Plasma and Plant Secondary Metabolites: Opportunities and Challenges’, Molecules, vol. 28, no. 22, Art. no. 22, Jan. 2023. [CrossRef]
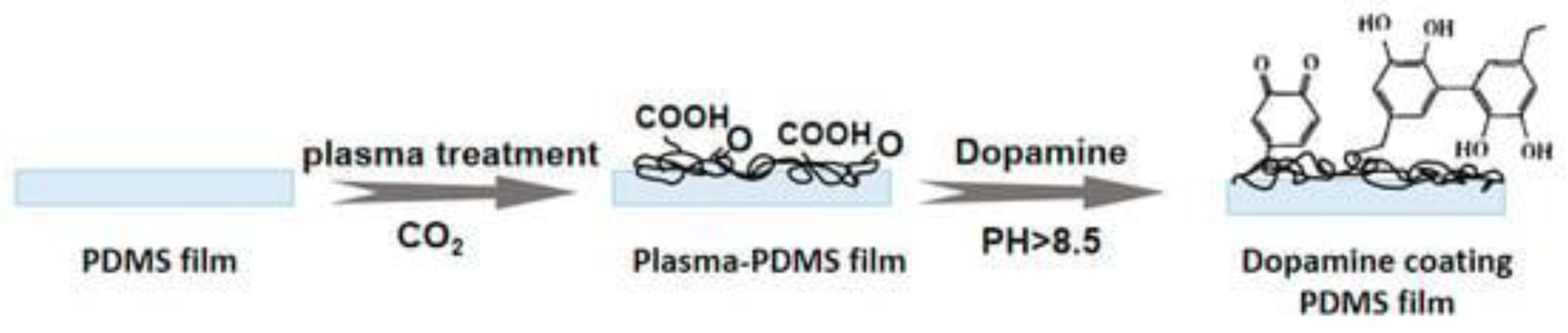
- M. Lu, L. Ding, T. Zhong, and Z. Dai, ‘Improving Hydrophilicity and Adhesion of PDMS through Dopamine Modification Assisted by Carbon Dioxide Plasma’, Coatings, vol. 13, no. 1, Art. no. 1, Jan. 2023. [CrossRef]
- Y. Zhang, T. Yang, B. Li, and J. Li, ‘Surface modifications of zirconia with plasma pretreatment and polydopamine coating to enhance the bond strength and durability between zirconia and titanium’, Dent. Mater. J., vol. 42, no. 3, pp. 449–457, 2023. [CrossRef]
- X. Saitaer et al., ‘Polydopamine-Inspired Surface Modification of Polypropylene Hernia Mesh Devices via Cold Oxygen Plasma: Antibacterial and Drug Release Properties’, Coatings, vol. 9, no. 3, Art. no. 3, Mar. 2019. [CrossRef]
- T.-L. Su, T.-P. Chen, and J. Liang, ‘Green in-situ synthesis of silver coated textiles for wide hygiene and healthcare applications’, Colloids Surf. Physicochem. Eng. Asp., vol. 657, p. 130506, Jan. 2023. [CrossRef]
- T. Gallingani et al., ‘A new strategy to prevent biofilm and clot formation in medical devices: The use of atmospheric non-thermal plasma assisted deposition of silver-based nanostructured coatings’, PLOS ONE, vol. 18, no. 2, p. e0282059, Feb. 2023. [CrossRef]
- G. T. L. Teixeira et al., ‘Exploring the functionalization of Ti-6Al-4V alloy with the novel antimicrobial peptide JIChis-2 via plasma polymerization’, Biofouling, vol. 39, no. 1, pp. 47–63, Jan. 2023. [CrossRef]
- A. Vesel, ‘Deposition of Chitosan on Plasma-Treated Polymers—A Review’, Polymers, vol. 15, no. 5, Art. no. 5, Jan. 2023. [CrossRef]
- K.-N. Ho, L.-W. Chen, T.-F. Kuo, K.-S. Chen, S.-Y. Lee, and S.-F. Wang, ‘Surface modification of zirconia ceramics through cold plasma treatment and the graft polymerization of biomolecules’, J. Dent. Sci., vol. 18, no. 1, pp. 73–80, Jan. 2023. [CrossRef]
- M. da Silva Bullmann et al., ‘Eucalyptus globulus essential oil thin film polymerized by cold plasma on Ti6Al4V: Sterilization effect, antibacterial activity, adhesion, and viability of mesenchymal stem cells’, Plasma Process. Polym., vol. 20, no. 11, p. e2300075, 2023. [CrossRef]
- M.-R. Kayaian and M. J. Hawker, ‘Using 1,8-cineole plasma with both pulsed and continuous depositions to modify commercially available wound dressing materials’, Biointerphases, vol. 18, no. 5, p. 051002, Oct. 2023. [CrossRef]
- H. N. B. Marzoug et al., ‘Eucalyptus oleosa Essential Oils: Chemical Composition and Antimicrobial and Antioxidant Activities of the Oils from Different Plant Parts (Stems, Leaves, Flowers and Fruits)’, Molecules, vol. 16, no. 2, Art. no. 2, Feb. 2011. [CrossRef]
- D. Sakthi Kumar et al., ‘Electrical and optical properties of plasma polymerized eucalyptus oil films’, J. Appl. Polym. Sci., vol. 90, no. 4, pp. 1102–1107, 2003. [CrossRef]
- A. Masood, N. Ahmed, M. F. M. Razip Wee, A. Patra, E. Mahmoudi, and K. S. Siow, ‘Atmospheric Pressure Plasma Polymerisation of D-Limonene and Its Antimicrobial Activity’, Polymers, vol. 15, no. 2, Art. no. 2, Jan. 2023. [CrossRef]
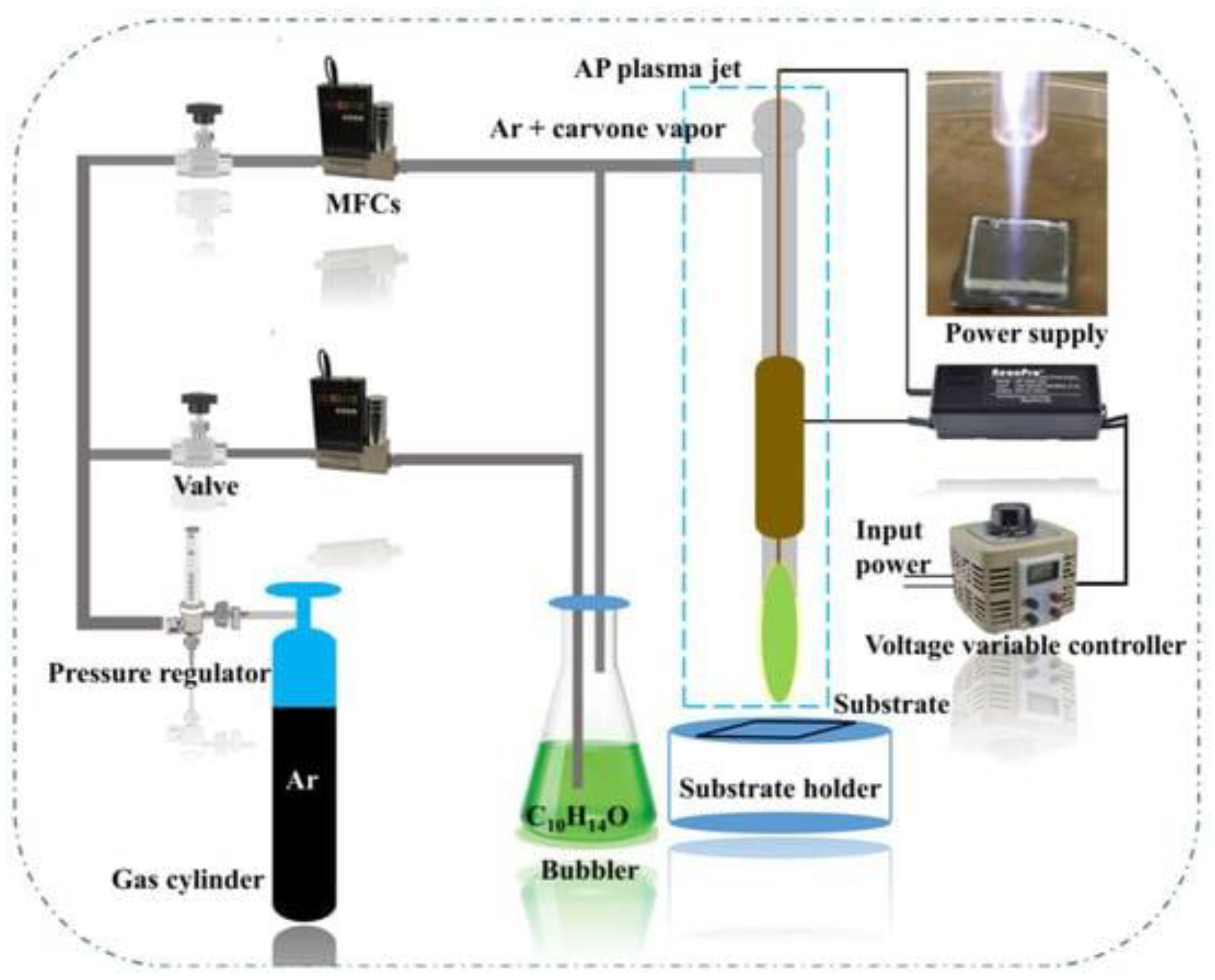
- A. Masood, N. Ahmed, F. Shahid, M. F. Mohd Razip Wee, A. Patra, and K. S. Siow, ‘Atmospheric Pressure Plasma Polymerization of Carvone: A Promising Approach for Antimicrobial Coatings’, Coatings, vol. 13, no. 6, Art. no. 6, Jun. 2023. [CrossRef]
- I. N. Amirrah et al., ‘Plasma-Polymerised Antibacterial Coating of Ovine Tendon Collagen Type I (OTC) Crosslinked with Genipin (GNP) and Dehydrothermal-Crosslinked (DHT) as a Cutaneous Substitute for Wound Healing’, Materials, vol. 16, no. 7, Art. no. 7, Jan. 2023. [CrossRef]
- E. O. M. Ruiz et al., ‘Cold plasma copolymer with antimicrobial activity deposited on three different substrates’, Polímeros, vol. 33, p. e20230038, Dec. 2023. [CrossRef]
- H. Shabani, A. Dezhpour, S. Jafari, M. J. M. Moghaddam, and M. Nilkar, ‘Antimicrobial activity of cold atmospheric-pressure argon plasma combined with chicory (Cichorium intybus L.) extract against P. aeruginosa and E. coli biofilms’, Sci. Rep., vol. 13, no. 1, Art. no. 1, Jun. 2023. [CrossRef]
- M. S. Hosseini et al., ‘Synthesis and evaluation of modified lens using plasma treatment containing timolol-maleate loaded lauric acid-decorated chitosan-alginate nanoparticles for glaucoma’, J. Biomater. Sci. Polym. Ed., vol. 34, no. 13, pp. 1793–1812, Sep. 2023. [CrossRef]
- E. Wulandari et al., ‘Nanoscale iodophoric poly(vinyl amide) coatings for the complexation and release of iodine for antimicrobial surfaces’, Appl. Surf. Sci., vol. 641, p. 158422, Dec. 2023. [CrossRef]
- A. Machková et al., ‘Silver nanoparticles with plasma-polymerized hexamethyldisiloxane coating on 3D printed substrates are non-cytotoxic and effective against respiratory pathogens’, Front. Microbiol., vol. 14, p. 1217617, Aug. 2023. [CrossRef]
- X. L. Strudwick, J. D. Whittle, A. J. Cowin, and L. E. Smith, ‘Plasma-Functionalised Dressings for Enhanced Wound Healing’, Int. J. Mol. Sci., vol. 24, no. 1, Art. no. 1, Jan. 2023. [CrossRef]
- B. Rout and P.-L. Girard-Lauriault, ‘Cell Attachment and Laminin Immobilization on Hydrogels Coated by Plasma Deposited Nitrogen, Oxygen or Sulfur Based Organic Thin Films’, Plasma Chem. Plasma Process., vol. 43, no. 3, pp. 709–736, May 2023. [CrossRef]
- A. O. Solovieva, N. A. Sitnikova, V. V. Nimaev, E. A. Koroleva, and A. M. Manakhov, ‘PRP of T2DM Patient Immobilized on PCL Nanofibers Stimulate Endothelial Cells Proliferation’, Int. J. Mol. Sci., vol. 24, no. 9, Art. no. 9, Jan. 2023. [CrossRef]
- L. M. Aung et al., ‘Functionalization of zirconia ceramic with fibronectin proteins enhanced bioactivity and osteogenic response of osteoblast-like cells’, Front. Bioeng. Biotechnol., vol. 11, 2023, Accessed: Jan. 04, 2024. [Online]. Available: https://www.frontiersin.org/articles/10.3389/fbioe.2023.1159639. [CrossRef]
- D. Le, J. Pan, and H. Xing, ‘The Cell Adhesion and Proliferation Enhancement Impact of Low-Temperature Atmospheric Pressure Plasma-Polymerized Heptylamine on the Surface of Ti6Al4V Alloy’, Materials, vol. 16, no. 19, Art. no. 19, Jan. 2023. [CrossRef]
- S. J. Mills et al., ‘Delivery of multipotent adult progenitor cells via a functionalized plasma polymerized surface accelerates healing of murine diabetic wounds’, Front. Bioeng. Biotechnol., vol. 11, p. 1213021, Aug. 2023. [CrossRef]
- G. Laghi et al., ‘Control strategies for atmospheric pressure plasma polymerization of fluorinated silane thin films with antiadhesive properties’, Plasma Process. Polym., vol. 20, no. 4, p. 2200194, 2023. [CrossRef]
- T. de los Arcos et al., ‘PECVD and PEALD on polymer substrates (Part II): Understanding and tuning of barrier and membrane properties of thin films’. arXiv, Jun. 26, 2023. [CrossRef]
- Š. Kelarová et al., ‘Influence of the argon ratio on the structure and properties of thin films prepared using PECVD in TMSAc/Ar mixtures’, Vacuum, vol. 207, p. 111634, Jan. 2023. [CrossRef]
- S. R. Coulson, I. S. Woodward, J. P. S. Badyal, S. A. Brewer, and C. Willis, ‘Ultralow Surface Energy Plasma Polymer Films’, Chem. Mater., vol. 12, no. 7, pp. 2031–2038, Jul. 2000. [CrossRef]
- N. Burmeister et al., ‘Zwitterionic surface modification of polyethylene via atmospheric plasma-induced polymerization of (vinylbenzyl-)sulfobetaine and evaluation of antifouling properties’, Colloids Surf. B Biointerfaces, vol. 224, p. 113195, Apr. 2023. [CrossRef]
- G. Newman et al., ‘Challenge of material haemocompatibility for microfluidic blood-contacting applications’, Front. Bioeng. Biotechnol., vol. 11, p. 1249753, Aug. 2023. [CrossRef]
- R. Brandenburg, K. H. Becker, and K.-D. Weltmann, ‘Barrier Discharges in Science and Technology Since 2003: A Tribute and Update’, Plasma Chem. Plasma Process., vol. 43, no. 6, pp. 1303–1334, Nov. 2023. [CrossRef]
- H. Yu, Y. Yu, C. Li, and L. Feng, ‘Surface Preparation and Cytocompatibility of Three-Dimensional Printed Fully Degraded Coronary Stents Using the Plasma Polymerization Technology’, Sci. Adv. Mater., vol. 15, no. 1, pp. 67–78, Jan. 2023. [CrossRef]
- H. Rezaei, A. A. Matin, and M. Mohammadnejad, ‘Cold atmospheric plasma treated 3D printed polylactic acid film; application in thin film solid phase microextraction of anticancer drugs’, Talanta, vol. 266, p. 125064, Jan. 2024. [CrossRef]
- R. Chakraborty, A. G. Anoop, A. Thakur, G. C. Mohanta, and P. Kumar, ‘Strategies To Modify the Surface and Bulk Properties of 3D-Printed Solid Scaffolds for Tissue Engineering Applications’, ACS Omega, vol. 8, no. 6, pp. 5139–5156, Feb. 2023. [CrossRef]
- M. Cámara-Torres, P. Fucile, R. Sinha, C. Mota, and L. Moroni, ‘Boosting bone regeneration using augmented melt-extruded additive-manufactured scaffolds’, Int. Mater. Rev., vol. 68, no. 7, pp. 755–785, Oct. 2023. [CrossRef]
- O. Lotz, D. R. McKenzie, M. M. Bilek, and B. Akhavan, ‘Biofunctionalized 3D printed structures for biomedical applications: A critical review of recent advances and future prospects’, Prog. Mater. Sci., vol. 137, p. 101124, Aug. 2023. [CrossRef]
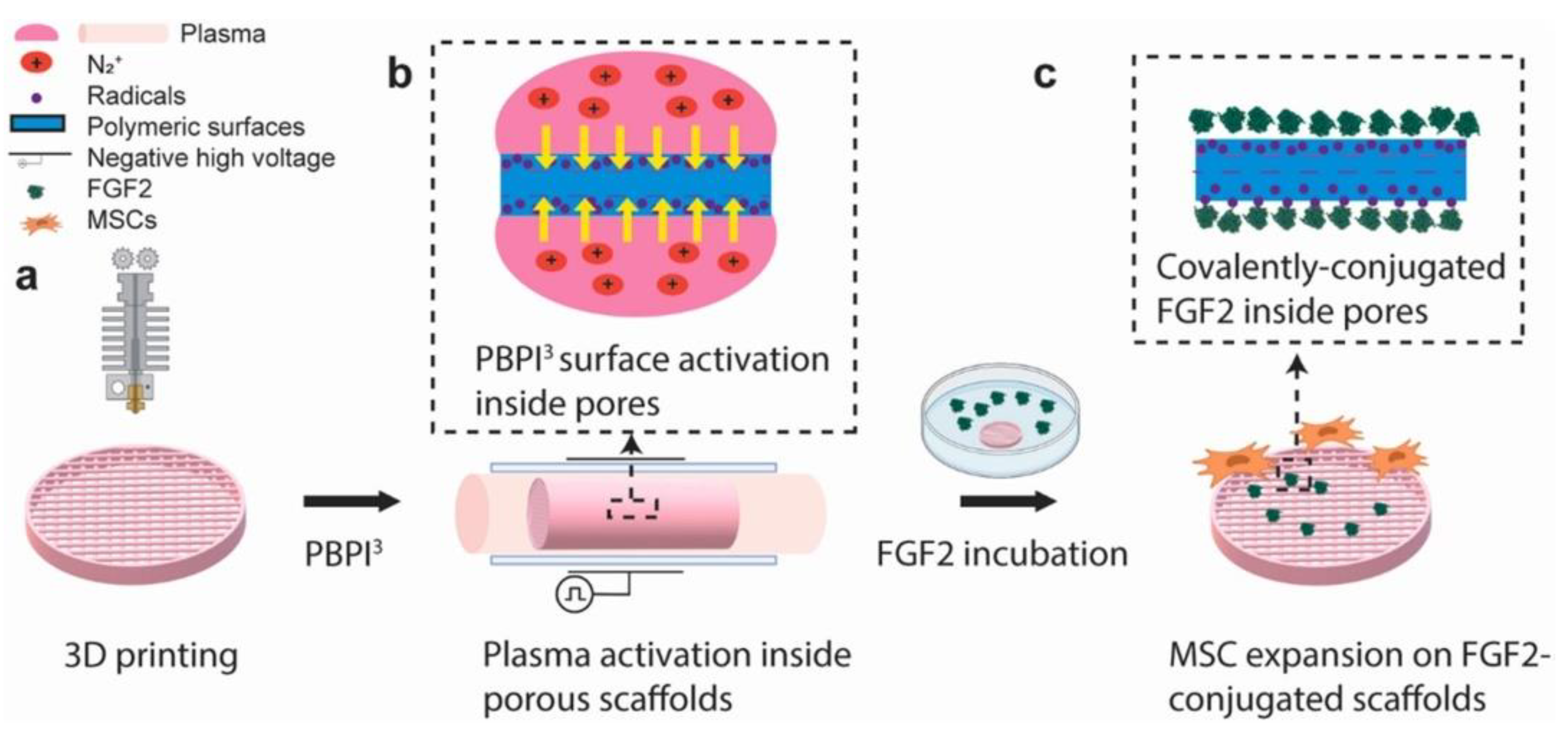
- A. Zhang et al., ‘A cost-effective and enhanced mesenchymal stem cell expansion platform with internal plasma-activated biofunctional interfaces’, Mater. Today Bio, vol. 22, p. 100727, Oct. 2023. [CrossRef]
- L. Miri, S. Irani, M. Pezeshki-Modaress, H. Daemi, and S. M. Atyabi, ‘Guiding mesenchymal stem cells differentiation into chondrocytes using sulfated alginate/cold atmospheric plasma modified polycaprolactone nanofibrous scaffold’, Polym. Bull., vol. 80, no. 8, pp. 8845–8860, Aug. 2023. [CrossRef]
- Z. Wang, F. Wen, and M. S. K. Chong, ‘Surface Modification of Tissue Engineering Scaffolds’, in Polymeric Biomaterials for Tissue Regeneration: From Surface/Interface Design to 3D Constructs, C. Gao, Ed., Singapore: Springer Nature, 2023, pp. 227–264. [CrossRef]
- M. Asadian et al., ‘The role of plasma-induced surface chemistry on polycaprolactone nanofibers to direct chondrogenic differentiation of human mesenchymal stem cells’, J. Biomed. Mater. Res. A, vol. 112, no. 2, pp. 210–230, 2024. [CrossRef]
- S. Aliakbarshirazi, R. Ghobeira, T. Egghe, N. De Geyter, H. Declercq, and R. Morent, ‘New plasma-assisted polymerization/activation route leading to a high density primary amine silanization of PCL/PLGA nanofibers for biomedical applications’, Appl. Surf. Sci., vol. 640, p. 158380, Dec. 2023. [CrossRef]
- S. Seemann et al., ‘Response of Osteoblasts on Amine-Based Nanocoatings Correlates with the Amino Group Density’, Molecules, vol. 28, no. 18, Art. no. 18, Jan. 2023. [CrossRef]
- R. C. Costa et al., ‘The race for the optimal antimicrobial surface: perspectives and challenges related to plasma electrolytic oxidation coating for titanium-based implants’, Adv. Colloid Interface Sci., vol. 311, p. 102805, Jan. 2023. [CrossRef]
- A. Fattah-alhosseini and M. Molaei, ‘A review of functionalizing plasma electrolytic oxidation (PEO) coatings on titanium substrates with laser surface treatments’, Appl. Surf. Sci. Adv., vol. 18, p. 100506, Dec. 2023. [CrossRef]
- L. Moreno et al., ‘Ciprofloxacin Release and Corrosion Behaviour of a Hybrid PEO/PCL Coating on Mg3Zn0.4Ca Alloy’, J. Funct. Biomater., vol. 14, no. 2, Art. no. 2, Feb. 2023. [CrossRef]
- S. Farshid, M. Kharaziha, and M. Atapour, ‘A self-healing and bioactive coating based on duplex plasma electrolytic oxidation/polydopamine on AZ91 alloy for bone implants’, J. Magnes. Alloys, vol. 11, no. 2, pp. 592–606, Feb. 2023. [CrossRef]
- R. Wang et al., ‘Cancer-targeting carbon quantum dots synthesized by plasma electrochemical method for red-light-activated photodynamic therapy’, Plasma Process. Polym., vol. n/a, no. n/a, p. e2300174. [CrossRef]
- N. K. Kaushik, S. Bekeschus, H. Tanaka, A. Lin, and E. H. Choi, ‘Plasma Medicine Technologies’, Appl. Sci., vol. 11, no. 10, Art. no. 10, Jan. 2021. [CrossRef]
- M. Laroussi, ‘Plasma Medicine: A Brief Introduction’, Plasma, vol. 1, no. 1, Art. no. 1, Sep. 2018. [CrossRef]
- M. Lotfi, M. Khani, and B. Shokri, ‘A Review of Cold Atmospheric Plasma Applications in Dermatology and Aesthetics’, Plasma Med., vol. 13, no. 1, 2023. [CrossRef]
- S. Chupradit et al., ‘Recent advances in cold atmospheric plasma (CAP) for breast cancer therapy’, Cell Biol. Int., vol. 47, no. 2, pp. 327–340, 2023. [CrossRef]
- N. Gelbrich et al., ‘Medical gas plasma augments bladder cancer cell toxicity in preclinical models and patient-derived tumor tissues’, J. Adv. Res., vol. 47, pp. 209–223, May 2023. [CrossRef]
- F. Nejat, K. Jadidi, S. Eghtedari, and N. Nabavi, ‘Sublimation of Benign Conjunctival Nevi Using Plasma-Assisted Noninvasive Surgery: A Clinical Case Series’, Iran. J. Med. Sci., vol. 48, no. 1, pp. 85–90, Jan. 2023. [CrossRef]
- J. M. Jung et al., ‘Cold Plasma Treatment Promotes Full-thickness Healing of Skin Wounds in Murine Models’, Int. J. Low. Extrem. Wounds, vol. 22, no. 1, pp. 77–84, Mar. 2023. [CrossRef]
- Y. Lee et al., ‘An Atmospheric Plasma Jet Induces Expression of Wound Healing Genes in Progressive Burn Wounds in a Comb Burn Rat Model: A Pilot Study’, J. Burn Care Res., vol. 44, no. 3, pp. 685–692, May 2023. [CrossRef]
- M. Bagheri, M. von Kohout, A. Zoric, P. C. Fuchs, J. L. Schiefer, and C. Opländer, ‘Can Cold Atmospheric Plasma Be Used for Infection Control in Burns? A Preclinical Evaluation’, Biomedicines, vol. 11, no. 5, Art. no. 5, May 2023. [CrossRef]
- H. Zhang, C. Zhang, and Q. Han, ‘Mechanisms of bacterial inhibition and tolerance around cold atmospheric plasma’, Appl. Microbiol. Biotechnol., vol. 107, no. 17, pp. 5301–5316, Sep. 2023. [CrossRef]
- S. Das et al., ‘Antimicrobial Efficacy of Argon Cold Atmospheric Pressure Plasma Jet on Clinical Isolates of Multidrug-Resistant ESKAPE Bacteria’, IEEE Trans. Radiat. Plasma Med. Sci., vol. 7, no. 4, pp. 421–428, Apr. 2023. [CrossRef]
- S. Hu et al., ‘Simultaneous removal of antibiotic-resistant Escherichia coli and its resistance genes by dielectric barrier discharge plasma’, Environ. Res., vol. 231, p. 116163, Aug. 2023. [CrossRef]
- A. Algammal, H. F. Hetta, M. Mabrok, and P. Behzadi, ‘Editorial: Emerging multidrug-resistant bacterial pathogens “superbugs”: A rising public health threat’, Front. Microbiol., vol. 14, p. 1135614, Feb. 2023. [CrossRef]
- N. Abu Rached, S. Kley, M. Storck, T. Meyer, and M. Stücker, ‘Cold Plasma Therapy in Chronic Wounds—A Multicenter, Randomized Controlled Clinical Trial (Plasma on Chronic Wounds for Epidermal Regeneration Study): Preliminary Results’, J. Clin. Med., vol. 12, no. 15, Art. no. 15, Jan. 2023. [CrossRef]
- M. Li et al., ‘Basic research and clinical exploration of cold atmospheric plasma for skin wounds’, Bioeng. Transl. Med., vol. 8, no. 5, p. e10550, 2023. [CrossRef]
- Y. Li et al., ‘Plasma-activated ethanol solution and it’s decontamination effect’, High Volt., vol. 8, no. 4, pp. 833–840, 2023. [CrossRef]
- J.-A. Maybin et al., ‘Cold atmospheric pressure plasma-antibiotic synergy in Pseudomonas aeruginosa biofilms is mediated via oxidative stress response’, Biofilm, vol. 5, p. 100122, Dec. 2023. [CrossRef]
- L. Han, S. Patil, D. Boehm, V. Milosavljević, P. J. Cullen, and P. Bourke, ‘Mechanisms of Inactivation by High-Voltage Atmospheric Cold Plasma Differ for Escherichia coli and Staphylococcus aureus’, Appl. Environ. Microbiol., vol. 82, no. 2, pp. 450–458, Jan. 2016. [CrossRef]
- D. Ziuzina, D. Boehm, S. Patil, P. J. Cullen, and P. Bourke, ‘Cold Plasma Inactivation of Bacterial Biofilms and Reduction of Quorum Sensing Regulated Virulence Factors’, PLOS ONE, vol. 10, no. 9, p. e0138209, Sep. 2015. [CrossRef]
- M. Ahmadi et al., ‘Cold Physical Plasma-Mediated Fenretinide Prodrug Activation Confers Additive Cytotoxicity in Epithelial Cells’, Antioxidants, vol. 12, no. 6, Art. no. 6, Jun. 2023. [CrossRef]
- B. Pinheiro Lopes, L. O’Neill, P. Bourke, and D. Boehm, ‘Combined Effect of Plasma-Activated Water and Topotecan in Glioblastoma Cells’, Cancers, vol. 15, no. 19, Art. no. 19, Jan. 2023. [CrossRef]
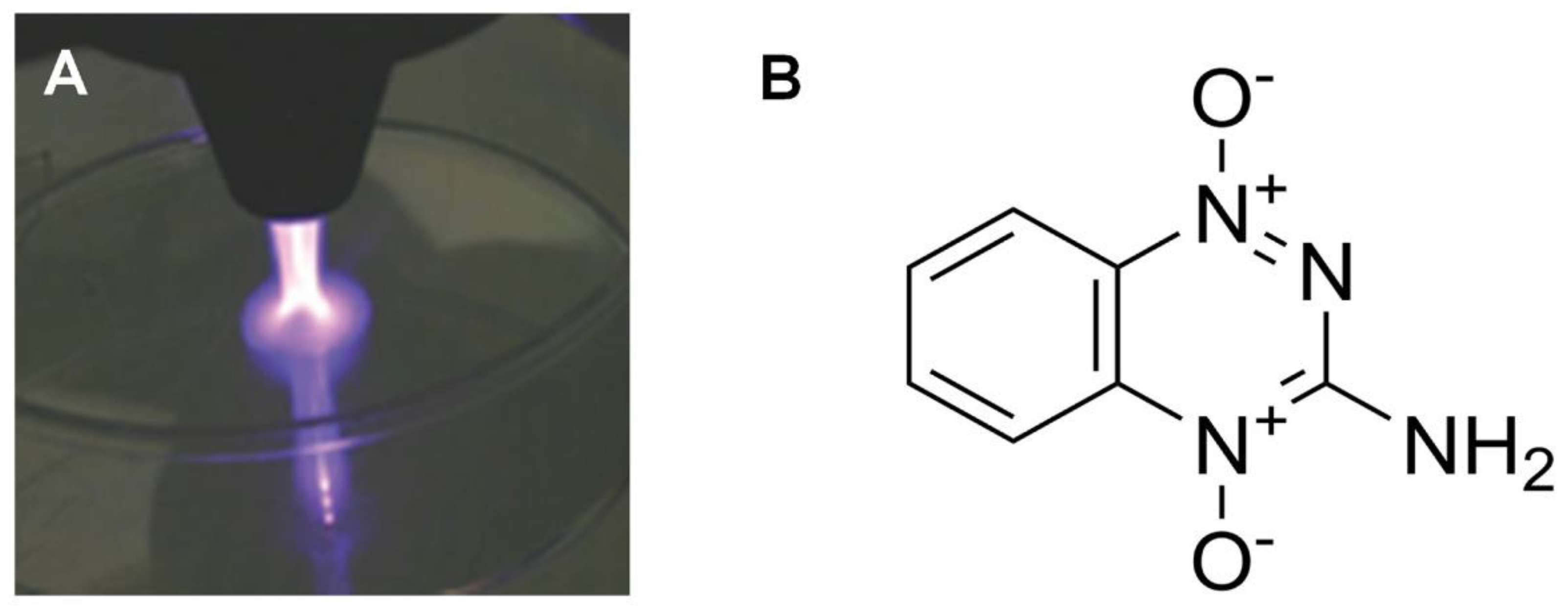
- M. Yehl et al., ‘The Development of Nonthermal Plasma and Tirapazamine as a Novel Combination Therapy to Treat Melanoma In Situ’, Cells, vol. 12, no. 16, Art. no. 16, Jan. 2023. [CrossRef]
- T. Pavlik et al., ‘The Role of Autophagy and Apoptosis in the Combined Action of Plasma-Treated Saline, Doxorubicin, and Medroxyprogesterone Acetate on K562 Myeloid Leukaemia Cells’, Int. J. Mol. Sci., vol. 24, no. 6, Art. no. 6, Jan. 2023. [CrossRef]
- A. Dezhpour, H. Ghafouri, S. Jafari, and M. Nilkar, ‘Effects of cold atmospheric-pressure plasma in combination with doxorubicin drug against breast cancer cells in vitro and in vivo’, Free Radic. Biol. Med., vol. 209, pp. 202–210, Nov. 2023. [CrossRef]
- V. Kniazeva, D. Tzerkovsky, Ö. Baysal, A. Kornev, E. Roslyakov, and S. Kostevitch, ‘Adjuvant composite cold atmospheric plasma therapy increases antitumoral effect of doxorubicin hydrochloride’, Front. Oncol., vol. 13, 2023, Accessed: Jan. 05, 2024. [Online]. Available: https://www.frontiersin.org/articles/10.3389/fonc.2023.1171042. [CrossRef]
- Y. Wang et al., ‘Cold atmospheric plasma sensitizes head and neck cancer to chemotherapy and immune checkpoint blockade therapy’, Redox Biol., vol. 69, p. 102991, Feb. 2024. [CrossRef]
- C. Yan et al., ‘Cold atmospheric plasma sensitizes melanoma cells to targeted therapy agents in vitro’, J. Biophotonics, vol. n/a, no. n/a, p. e202300356. [CrossRef]
- T. Pavlik, N. Kostukova, M. Pavlova, N. Gusein-Zade, and N. Shimanovskii, ‘Modulation of the Effect of Doxorubicin and Medroxyprogesterone Acetate on Cytokine and Oxidant Activity of Human Leukocytes by Hanksâ Cold Plasma-Treated Solution’, Plasma Med., vol. 13, no. 1, 2023. [CrossRef]
- D. Murillo, C. Huergo, B. Gallego, R. Rodríguez, and J. Tornín, ‘Exploring the Use of Cold Atmospheric Plasma to Overcome Drug Resistance in Cancer’, Biomedicines, vol. 11, no. 1, Art. no. 1, Jan. 2023. [CrossRef]
- D. Tian, Y. Lv, L. Nie, X. Li, J. Liu, and X. Lu, ‘Comparative study of touchable plasma devices on transdermal drug delivery’, Plasma Process. Polym., vol. 20, no. 9, p. e2200216, 2023. [CrossRef]
- E. Wu, L. Nie, D. Liu, X. Lu, and K. (Ken) Ostrikov, ‘Plasma poration: Transdermal electric fields, conduction currents, and reactive species transport’, Free Radic. Biol. Med., vol. 198, pp. 109–117, Mar. 2023. [CrossRef]
- P. R. Sreedevi and K. Suresh, ‘Cold atmospheric plasma mediated cell membrane permeation and gene delivery-empirical interventions and pertinence’, Adv. Colloid Interface Sci., vol. 320, p. 102989, Oct. 2023. [CrossRef]
- V. Vijayarangan et al., ‘Boost of cosmetic active ingredient penetration triggered and controlled by the delivery of kHz plasma jet on human skin explants’, Front. Phys., vol. 11, 2023, Accessed: Jan. 05, 2024. [Online]. Available: https://www.frontiersin.org/articles/10.3389/fphy.2023.1173349. [CrossRef]
- T. Fang, X. Cao, B. Shen, Z. Chen, and G. Chen, ‘Injectable cold atmospheric plasma-activated immunotherapeutic hydrogel for enhanced cancer treatment’, Biomaterials, vol. 300, p. 122189, Sep. 2023. [CrossRef]
- L. Huang et al., ‘Bactericidal effects of plasma-activated saline prepared by surface dielectric barrier discharge with different dielectric layers and working gases’, Plasma Process. Polym., vol. 20, no. 1, p. 2200110, 2023. [CrossRef]
- M. Hummert, P. Leenders, A. Mellmann, K. Becker, and T. Kuczius, ‘Generation of Plasma-Activated Fluids for Successful Disinfection of Pseudomonas aeruginosa in Liquid Environments and Determination of Microbial Damage’, Plasma, vol. 6, no. 4, Art. no. 4, Dec. 2023. [CrossRef]
- J. Lin, D. Liu, J. Zhang, R. Zhou, M. Rong, and K. (Ken) Ostrikov, ‘Insights into reactivity and bactericidal effects of water activated by He and Ar plasma jets’, Plasma Process. Polym., vol. 20, no. 4, p. 2200173, 2023. [CrossRef]
- T. von Woedtke, G. Gabriel, U. E. Schaible, and S. Bekeschus, ‘Oral SARS-CoV-2 reduction by local treatment: A plasma technology application?’, Plasma Process. Polym., vol. 20, no. 3, p. 2200196, 2023. [CrossRef]
- H. Wang, C. Liu, Y. Wu, M. A. Bashir, C. Shao, and Q. Huang, ‘Application of NaCl in Cold Atmospheric Plasma Jet and Plasma-Activated Solution to Enhance Virus Inactivation’, Plasma Med., vol. 13, no. 2, 2023. [CrossRef]
- V. Armenise et al., ‘The effect of different cold atmospheric plasma sources and treatment modalities on the generation of reactive oxygen and nitrogen species in water’, Plasma Process. Polym., vol. 20, no. 4, p. 2200182, 2023. [CrossRef]
- M. Shaji, A. Rabinovich, M. Surace, C. Sales, and A. Fridman, ‘Physical Properties of Plasma-Activated Water’, Plasma, vol. 6, no. 1, Art. no. 1, Mar. 2023. [CrossRef]
- K. S. Wong, N. S. L. Chew, M. Low, and M. K. Tan, ‘Plasma-Activated Water: Physicochemical Properties, Generation Techniques, and Applications’, Processes, vol. 11, no. 7, Art. no. 7, Jul. 2023. [CrossRef]
- Z. Liu et al., ‘Controlling plasma-activated solution chemistry for targeted cancer cell death’, Plasma Process. Polym., vol. 20, no. 10, p. e2300029, 2023. [CrossRef]
- Z. Zhou, H. Li, Z. Qi, and D. Liu, ‘Biological and Chemical Reactivities of Plasma-Activated Water Prepared at Different Temperatures’, Plasma Chem. Plasma Process., Aug. 2023. [CrossRef]
- R. Zhou, T. Zhang, and R. Zhou, ‘Pulsed Discharges for Water Activation and Plasma-Activated Water Production’, in Pulsed Discharge Plasmas: Characteristics and Applications, T. Shao and C. Zhang, Eds., in Springer Series in Plasma Science and Technology. , Singapore: Springer Nature, 2023, pp. 325–347. [CrossRef]
- V. Veronico et al., ‘Anticancer Effects of Plasma-Treated Water Solutions from Clinically Approved Infusion Liquids Supplemented with Organic Molecules’, ACS Omega, vol. 8, no. 37, pp. 33723–33736, Sep. 2023. [CrossRef]
- H. Xu et al., ‘Enhancement of the drug sensitization of cancer cells by plasma-activated saline’, Plasma Process. Polym., vol. 20, no. 9, p. e2300001, 2023. [CrossRef]
- S. Xu et al., ‘Anticancer effects of DBD plasma-activated saline within different discharge modes’, J. Phys. Appl. Phys., vol. 56, no. 34, p. 345205, May 2023. [CrossRef]
- K. Kutasi, L. Bencs, Z. Tóth, and S. Milošević, ‘The role of metals in the deposition of long-lived reactive oxygen and nitrogen species into the plasma-activated liquids’, Plasma Process. Polym., vol. 20, no. 3, p. 2200143, 2023. [CrossRef]
- L. Guo et al., ‘Inactivation effects of the mist nebulized with plasma-activated air on Pseudomonas aeruginosa through the simulated respiratory tract’, Plasma Process. Polym., vol. 20, no. 9, p. e2200204, 2023. [CrossRef]
- H. Saadawy et al., ‘Treatment of hepatocellular carcinoma with in situ generated plasma-activated air-driven water mist’, Plasma Process. Polym., vol. 20, no. 9, p. e2200234, 2023. [CrossRef]
- A. Chakraborty et al., ‘Pharmaceuticals and Personal Care Products as Emerging Environmental Contaminants: Prevalence, Toxicity, and Remedial Approaches’, ACS Chem. Health Saf., vol. 30, no. 6, pp. 362–388, Nov. 2023. [CrossRef]
- A. L. V. Cubas, A. R. de A. Dutra, T. C. Alves, R. T. Bianchet, A. A. Rambo, and N. A. Debacher, ‘Evaluation of antimicrobial sensitivity to tetracycline exposed to non-thermal plasma’, Quím. Nova, vol. 46, pp. 236–240, May 2023. [CrossRef]
- F. LU, J. ZHOU, and Z. WU, ‘Degradation of antibiotic contaminants from water by gas–liquid underwater discharge plasma’, Plasma Sci. Technol., vol. 25, no. 3, p. 035506, Jan. 2023. [CrossRef]
- M. El Shaer et al., ‘Antibiotics Degradation and Bacteria Inactivation in Water by Cold Atmospheric Plasma Discharges Above and Below Water Surface’, Plasma Chem. Plasma Process., vol. 40, no. 4, pp. 971–983, Jul. 2020. [CrossRef]
- M. Magureanu et al., ‘Degradation of antibiotics in water by non-thermal plasma treatment’, Water Res., vol. 45, no. 11, pp. 3407–3416, May 2011. [CrossRef]
- D. Terefinko et al., ‘Removal of clinically significant antibiotics from aqueous solutions by applying unique high-throughput continuous-flow plasma pencil and plasma brush systems’, Chem. Eng. J., vol. 452, p. 139415, Jan. 2023. [CrossRef]
- C. Liang, C. Fang, H. Wang, M. A. Bashir, and Q. Huang, ‘Removal of Ampicillin Using Cold Atmospheric-Pressure Plasma Jet and Its Plasma-Activated Water’, Plasma Med., vol. 13, no. 2, 2023. [CrossRef]
- F. Bilea et al., ‘Removal of a mixture of antibiotics in water using nonthermal plasma’, Plasma Process. Polym., vol. 20, no. 8, p. 2300020, 2023. [CrossRef]
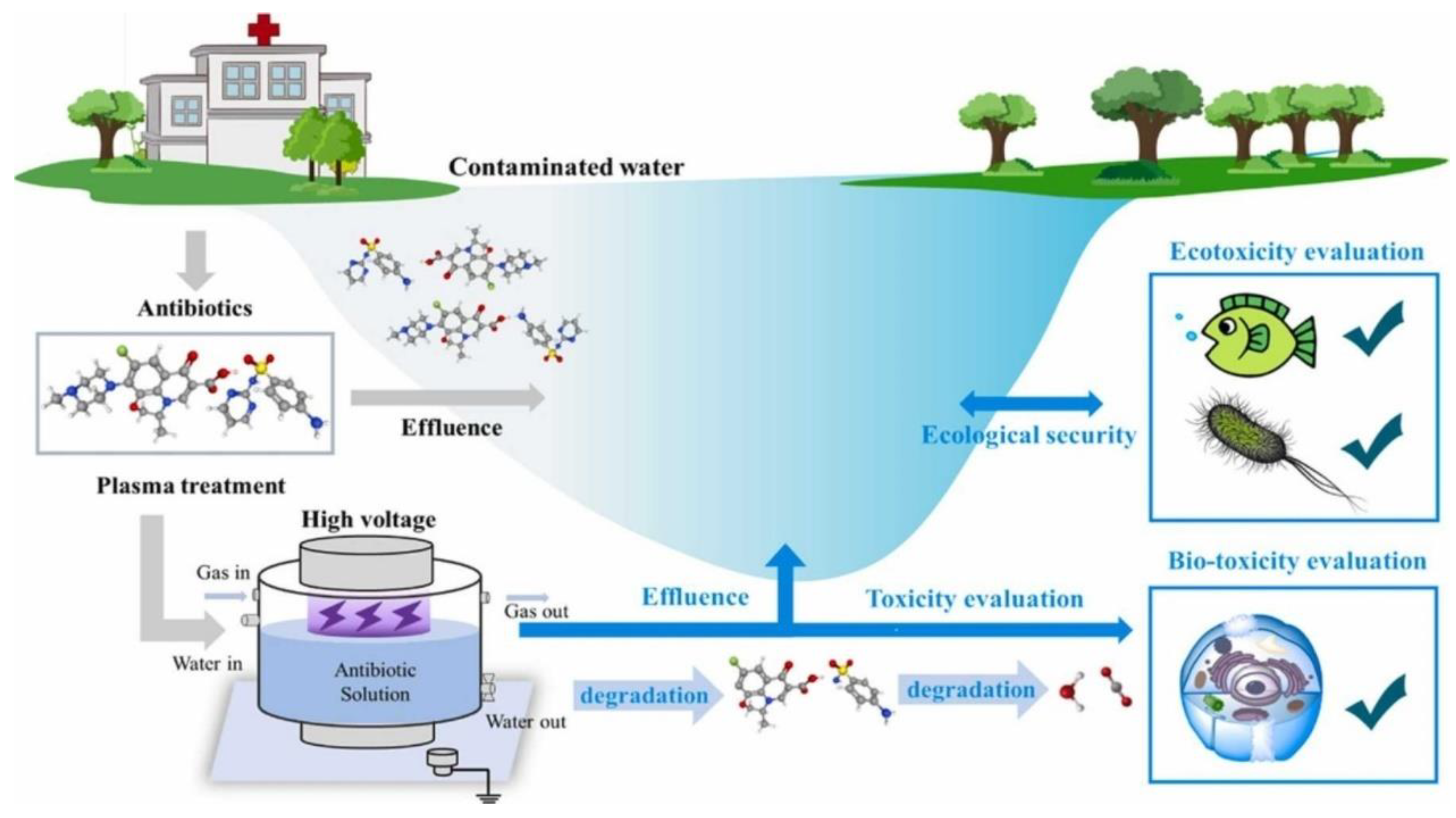
- S. HU et al., ‘Degradation of sulfamethoxazole in water by dielectric barrier discharge plasma jet: influencing parameters, degradation pathway, toxicity evaluation’, Plasma Sci. Technol., vol. 25, no. 3, p. 035510, Jan. 2023. [CrossRef]
- C. Fang, C. Shao, S. Wang, Y. Wu, C. Liu, and Q. Huang, ‘Simultaneous removal of levofloxacin and sulfadiazine in water by dielectric barrier discharge (DBD) plasma: Enhanced performance and degradation mechanism’, Process Saf. Environ. Prot., vol. 171, pp. 459–469, Mar. 2023. [CrossRef]
- N. Nandy, A. Pasupathi, Y. Subramaniam, and S. Nachimuthu, ‘Eliminating ciprofloxacin antibiotic contamination from water with a novel submerged thermal plasma technology’, Chemosphere, vol. 326, p. 138470, Jun. 2023. [CrossRef]
- T. B. M. Mosaka, J. O. Unuofin, M. O. Daramola, C. Tizaoui, and S. A. Iwarere, ‘Inactivation of antibiotic-resistant bacteria and antibiotic-resistance genes in wastewater streams: Current challenges and future perspectives’, Front. Microbiol., vol. 13, 2023, Accessed: Jan. 05, 2024. [Online]. Available: https://www.frontiersin.org/articles/10.3389/fmicb.2022.1100102. [CrossRef]
- T. Shen et al., ‘Introduction of oxygen vacancy to Bi2Mn4O10 supported by nickel foam for 1O2 dominated metronidazole degradation under dielectric barrier discharge plasma’, Appl. Catal. B Environ., vol. 328, p. 122518, Jul. 2023. [CrossRef]
- C. Sarangapani et al., ‘Degradation kinetics of cold plasma-treated antibiotics and their antimicrobial activity’, Sci. Rep., vol. 9, no. 1, Art. no. 1, Mar. 2019. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




