1. History of Laryngoscopy
In the late 19th century, a device/tool to visualize the glottis was invented and subsequently modified by mainly ear-nose-throat (ENT) doctors, was called laryngoscope (for review, see [
1]). To acquire such glottis view, either direct or indirect, laryngoscopes served a supportive role for ENT doctors to surgically treat patients. Interestingly, laryngoscope was not used to perform intra-tracheal intubation and general anesthesia until early 20th century, first reported by Chevalier Jackson and Henry Janeway, respectively. It is worthy to mention that Janeway plays an important role in the transition phase of such laryngoscope from being as a tool used solely by the ENT specialist to a fundamental instrument by the anesthesiologist. Since then, to see the glottis and to place an insufflation tube into patient’s trachea became a clinical skill, either for airway management or clinical anesthesia.
While use of a conventional direct laryngoscope (DL) with a blade to perform tracheal intubation became popular, the airway managers immediately found occasional incidence of difficulties or failure. Several patient’s factors were identified to be associated with the likelihood of traumatized temporo-mandibular joint, mouth, or other soft tissue injuries. Those risk factors include prominent sternal region, narrow space between the incisors, reduced intraoral space, and the anteriorly positioned larynx in the patients [
2]. A new type of laryngoscope blade, among several others, was later designed to lessen the difficulty of exposing the larynx to pass an endotracheal tube [
3]. Meanwhile, several technical tips and pearls were proposed for tracheal intubation under general anesthesia, e.g., head extension, chin lift, elevating the laryngoscope and displacing the base of the tongue upward, protecting upper teeth, viewing and lifting upwards the epiglottis, visualizing the vocal cords, and finally passing the endotracheal (ET) tube. It was mentioned that such DL technique is “essentially an easy manoeuvre if simple anatomical rules are obeyed” [
3].
Unfortunately, the anatomical rules are not always obeyed for laryngoscopy. In the last few decades, several technical maneuvers were found to be helpful for direct laryngoscopy when event of difficult airway (laryngoscopy and/or intubation) was predicted or encountered. The external laryngeal manipulations, e.g., include BURP (backward, upward rightward pressure) [
4,
5,
6,
7,
8], laryngeal lift [
9], sniff positioning [
10,
11,
12,
13], and various head-neck elevation or hyperextension positions [
14,
15], were demonstrated to be beneficial for tracheal intubation. It is worthy to mention that the sniffing position does not always achieve alignment of the classical three axes (TAAT; oral/pharyngeal/laryngeal ThreeAxes Alignment Theory), e.g., in awake patients with normal airway anatomy [
16]. It has been proposed that direct laryngoscopy is inherently a three-dimensional performance [
17]. Theoretically, alignment of the three axes (oral, pharyngeal, and laryngeal) may seem ideal because it brings all anatomical structures together into one straight line for better vision. However, instead of a theory, whether in clinical practice TAAT is valid has been challenged [
18,
19].
2. A Paradigm Shift of Videolaryngoscopy
No matter the axes theories or the external laryngeal manipulations are valid and useful, the anatomical structures still limited and restrained the laryngeal visualization by the airway managers during tracheal intubation procedure. The conventional DL is definitely a difficult skill to master and heavy mental load for most medical staff, especially for those are novice practitioners or who do not perform it on a regular basis. Same true is for experienced airway managers if encountered difficult airway scenarios (e.g., obesity, limited cervical spine mobility, unstable cervical spine trauma, upper airway obstruction or bleeding, radiation fibrosis or flaps over neck region, etc.). Such difficulties may eventually cause disasters and reflected by medico-legal misadventure reports. Difficult tracheal intubation events occurred more in sicker patients, in emergency procedures, and in non-perioperative locations. It should also be noted that the “can’t intubate, can’t ventilate” and the “physiologically difficult airway” as non-anatomical reasons for emerging of clinical emergencies may occur during an endotracheal intubation. Eventually, patients’ outcomes remained poor in recent malpractice claims related to difficult tracheal intubation [
20].
Apparently, “to see is to intubate” is a prerequisite for the success of laryngoscopy which can be measured by visualization of the glottis opening, first-attempt success rate, time to complete intubation, failure rate, necessity to have assistance or changing accessary devices, complications, etc. In the real world, despite various pre-operative airway assessment parameters, DL occasionally yields expectedly or unexpectedly poor laryngeal views. When that happened, the end-results can be devastating, even if with ultimate success in airway management. To overcome such “cannot see, cannot intubate” quandary, a new VL (GlideScope
® designed by John Pacey in 2001) was made by installing a robust, high-resolution camera (charge-coupled device) embedded into a conventional laryngoscope blade. Such VL therefore is able to yield a comparable or even superior glottic view in comparison to DL [
21]. Successful intubation was generally achieved even when DL was predicted to be moderately or considerably difficult [
22].
Subsequently, it is not surprising that various kinds of the VL quickly gained global popularity as the primary intubating device in many clinical scenarios, driven by quick to learn, ease of use, positive patient outcomes, etc. Such VL was originally designed to provide an indirect view of the upper airway. Therefore, in clinically difficult airway management, it is hoping that VL improve Cormack-Lehane grade and achieve the same or a higher intubation success rate in less time and effort, compared with DL [
23]. Clinically, use of VL was observed to be associated with fewer failed attempts and complications such as hypoxaemia, whereas glottic views were improved [
24]. More important, whether VL could or should replace DL in patients with normal or difficult airways and serve as a tool for routine tracheal intubation remain a debate and requires conclusive evidence [
25,
26]. Recently, in critically ill adults undergoing tracheal intubation in the emergency room and intensive care unit, the use of VL has been demonstrated to result in more successful first-attempt intubation than DL [
27]. It should be noted that such conclusion might not be applied to airway management in the anesthetizing locations (e.g., operating rooms) or by the experienced anesthesiologists.
3. Evolution of Optic/Video Intubating Tools
The comparison between VL and DL has always been around the primary key clinical outcome parameters as first-attempt success rate, intubation time, and overall success rate. The safety outcome parameters, e.g., cardiovascular events (hypoxemia, severe hypotension, cardiac arrest, or death), esophageal intubation, dental and soft tissue injury, and aspiration, also served as the comparison indices. Although the main advantage of VL is able to provide better visualization of the glottis than DL does, both techniques may still face certain difficulties. For example, the insertion of the laryngoscopic blade into oral-pharyngeal space and advancement of the endotracheal tube/stylet unit may occasionally be awkward and failing.
The original design of VL allowed indirect laryngoscopy, better laryngeal exposure of the vocal cords and related airway structures without requiring a direct line of sight. Before the invention of the VL, the rigid fiber-optic laryngoscopy (e.g., Bullard laryngoscope™, patented for use in 1995; WuScope™, patented in 1993; UpsherScope Ultra™, patented in 1995) were also designed to provide a superb glottis visualization in rather difficult airway scenarios. Such kind of airway devices served as the rescue airway management tools when difficult airway scenarios were predicted or encountered [
28]. Unfortunately, such rescue devices generally require a significant amount of clinical experience to achieve proficiency.
Optical stylets (OS), first coined the term by Berci and Katz [
29], are rigid or semi-rigid tubular devices that fit in an endotracheal tube (ET tube) and transmit images using either fiber-optic bundles inside or a complementary metal oxide semiconductor (CMOS) video chips at the distal end of the device (for review, see [
30]). Another advanced optical intubating device was the rigid stylet invented by Pierre Bonfils in 1983 [
31]. The Bonfils endoscope was applied in a pediatric patient with difficult airway caused by Pierre-Robin syndrome. Such rigid endoscope, instead of being straight and rigid, it employed a fixed curved distal tip at the angle of 40 degrees. With this innovative design, it allowed not only better access to the anteriorly located glottis but also suitable for applying retromolar technique of tracheal intubation (for review, see [
32]).However, in contrast to flexible fiber-optic bronchoscope (FOB), the straight design of the rigid stylet was not always applicable for the cases of difficult laryngoscopy and the device itself had to be introduced with the aid of Macintosh laryngoscope for compressing the tongue base and the epiglottis (bimanual method).
4. The Styletubation
In contrast to the conventional concept of laryngoscopy, the ease of using intubating stylet (e.g., Bonfils endoscope) seems promising, either in regular/routine or expected/unexpected difficultairway scenarios. A new design of simple lighted stylet (lightwand) also was demonstrated to be clinically useful, especially when combined with laryngoscopy [
33,
34]. Although its transillumination-based design principle could not achieve the same goal as other optically-seeing intubating tools, the unique “field hockey stick” configuration of the Trachlight™ stick together with the endotracheal tube proved to be useful and practical. One of the hockey-stick examples of the stylet is the Shikani Optical Stylet (SOS; Shikani Seeing Stylet™) (
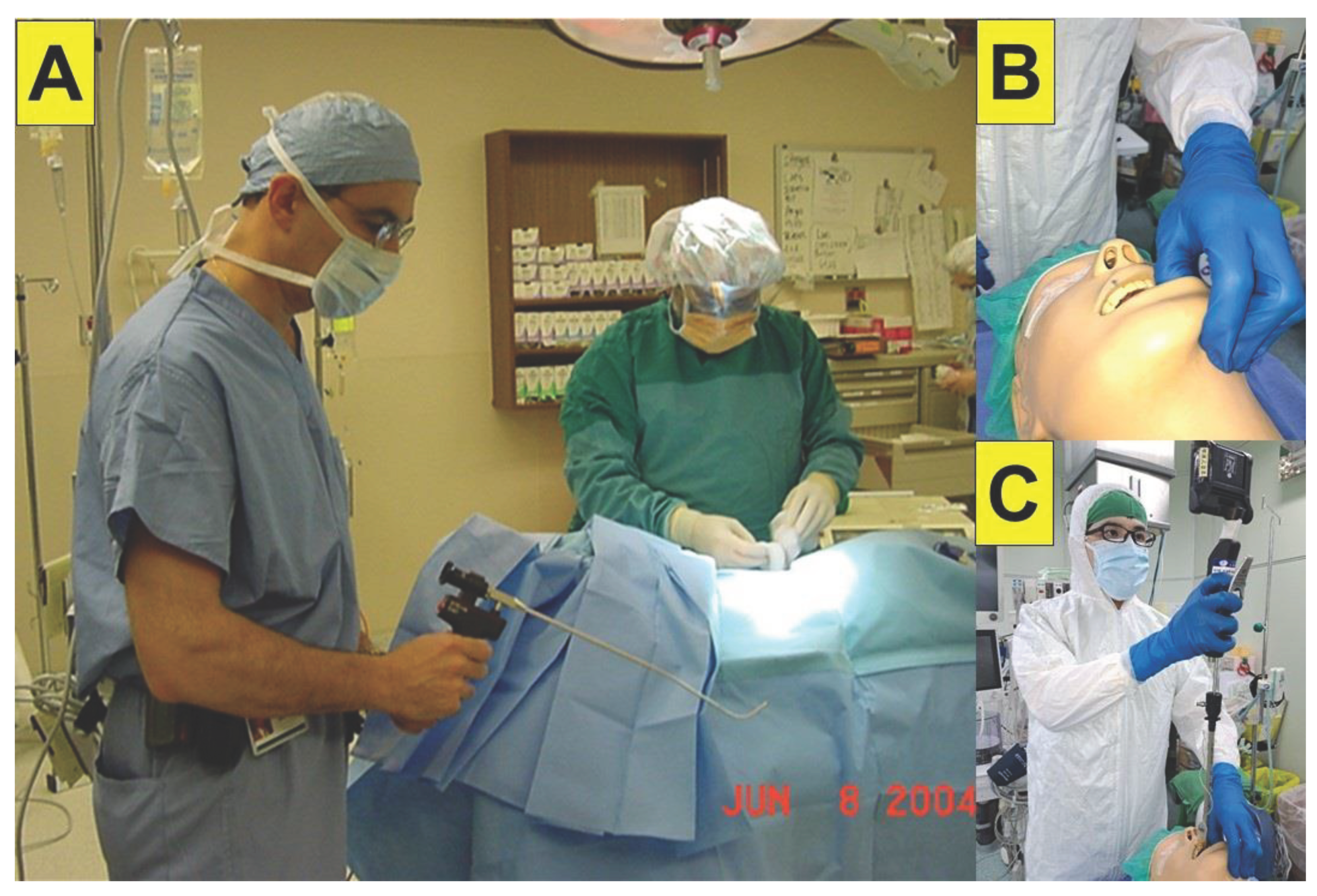
Figure 1).
The SOS (The Shikani Optical Stylet™; Clarus Medical, Minneapolis, MN, USA), invented by Alan Shikani and available since 1996, is a new generation of seeing intubating stylet that has a lens at the distal end, a fiber-optic cable inside, and connected to a camera and a video monitor. Such a design allows continuous visualization of the airway and laryngeal inlet during introduction of the ET tube into the glottis and trachea [
35]. The hockey stick design of the stylet facilitates the management of the potential difficult airway, minimizes the risk of trauma to the glottis or dentition, and allows intubation without the absolute need of the rigid laryngoscope blade to retract the base of the tongue. Another modified version of SOS is the LFS Scope
TM (Levitan First Pass Success scope; invented by Richard Levitan and manufactured by Clarus Medical (13355, 10th Ave N. Suite 110, Minneapolis, MN 55441 USA) is a short malleable semi-rigid fiberoptic stylet [
36].
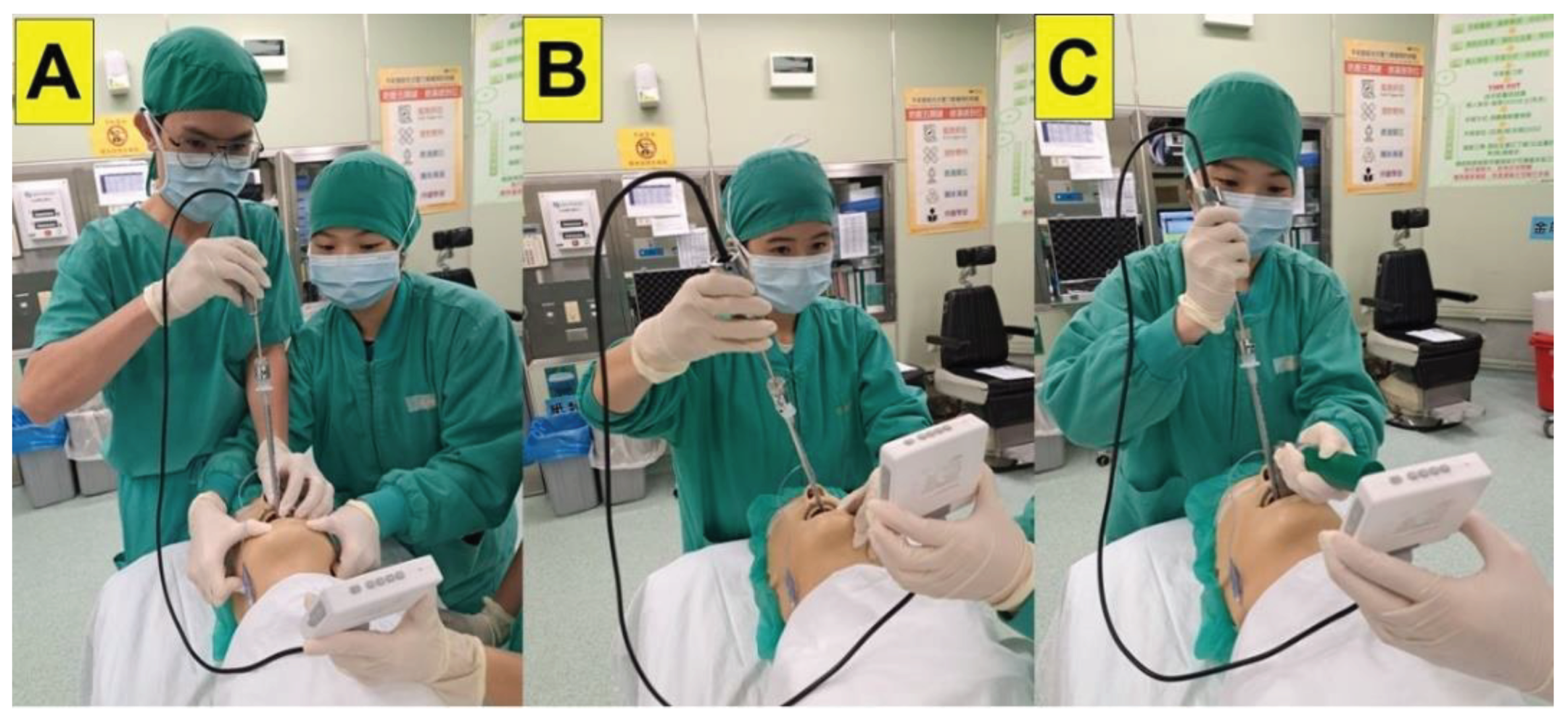
During the past two decades since the Shikani Seeing Stylet™ and its technique had been introduced, a gradual increase in adopting this intubating tool has been observed in literature. The clinical application of video-assisted intubating stylet (VS) and Shikani technique (
Figure 2) covered a broad spectrum of airway management scenarios, such as pediatric difficult airways, limited cervical spine mobility, limited mouth-opening (but still enough to accommodate an ET tube), head-neck lesions, obesity, etc [
37,
38,
39,
40,
41,
42,
43,
44]. Because operational technique of such Shikani technique with VS is sharply different form that of conventional laryngoscopy technique, we therefore coined the term “styletubation” to reflect its uniqueness and advantages (
Figure 2) [
45,
46,
47,
48]. In the following text, we will present several related issues to the styletubation technique.
5. Cases Presentation
5.1. Awake FOB or Styletubation for Emergency Tracheostomy
When appropriate, awake (oral or nasal) intubation should be considered if the difficult airway of the patient is suspected (e.g., difficult ventilation, increased risk of aspiration, short apneic tolerance, expected difficulty with emergency invasive airway rescue) [
28]. Typical examples include a huge tumor over head and neck [
49,
50] or undergoing oral maxillofacial surgery [
51]. It should be emphasized that awake FOB is still the gold standard tracheal intubation for such intractable and difficult airway scenarios, although other modified intubation modalities have been mentioned. For example, the advantageous role of VS for trans-nasal tracheal intubation has been compared with that of laryngoscopy [
52] and FOB [
53,
54]. Meanwhile, it should be noted that serious critics on trans-nasal use of VS for difficult airway have also been made [
55].
For predicted difficult airways, pre-operative trans-nasal or trans-oral endoscopic airway examination (PEAE) [
56,
57,
58], together with imaging studies, provided useful clinical information to make a plan for tracheal intubation (awake, asleep or anesthetized intubation). The FOB, among various awake tracheal intubation options, has a reasonable success rate and a favorable safety profile in cases of anticipated difficult airway management [
59]. However, difficulties (e.g., impaired glottis visualization by secretions/blood, impingement during ET tube advancement) may occur [
60,
61].
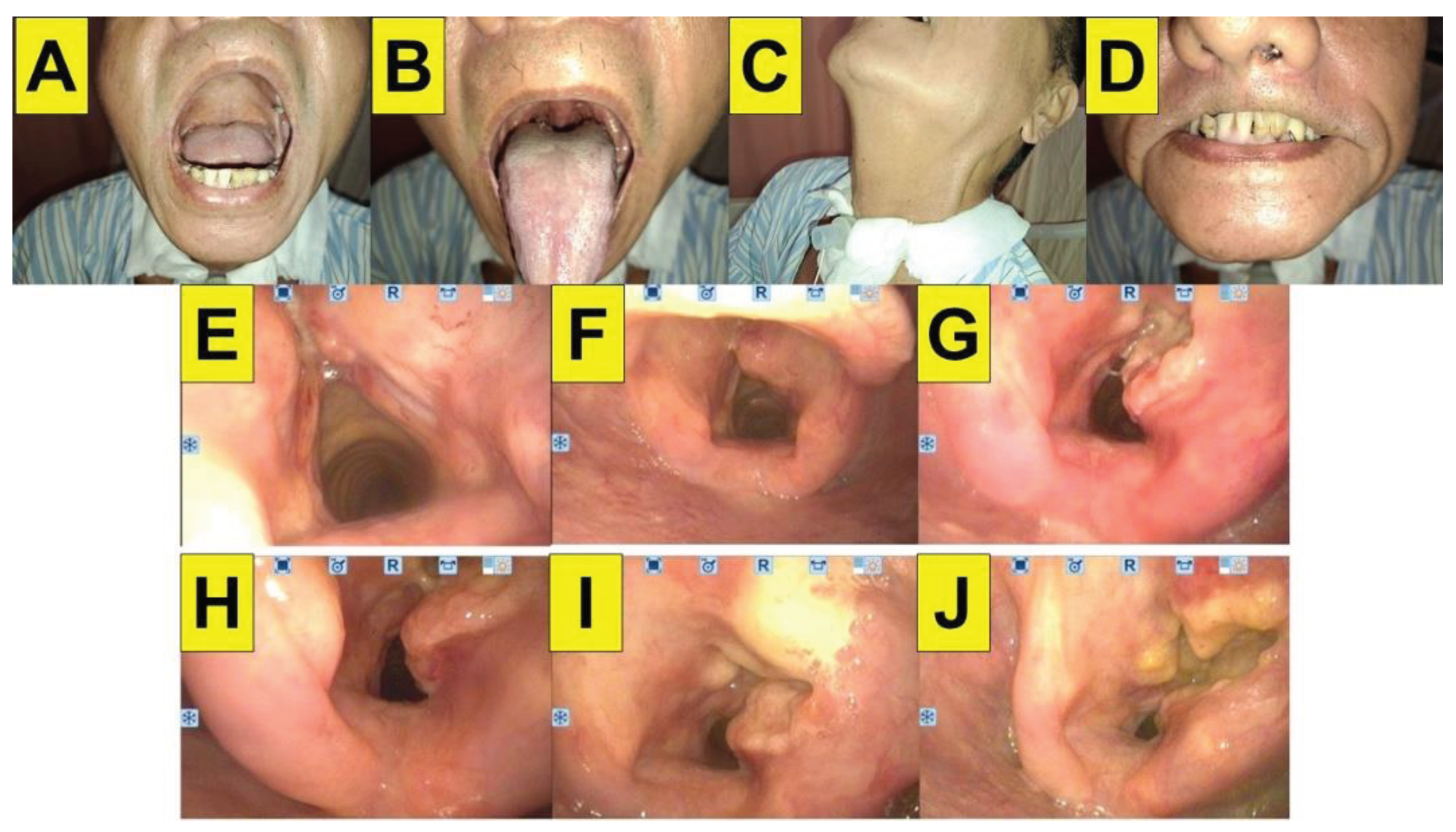
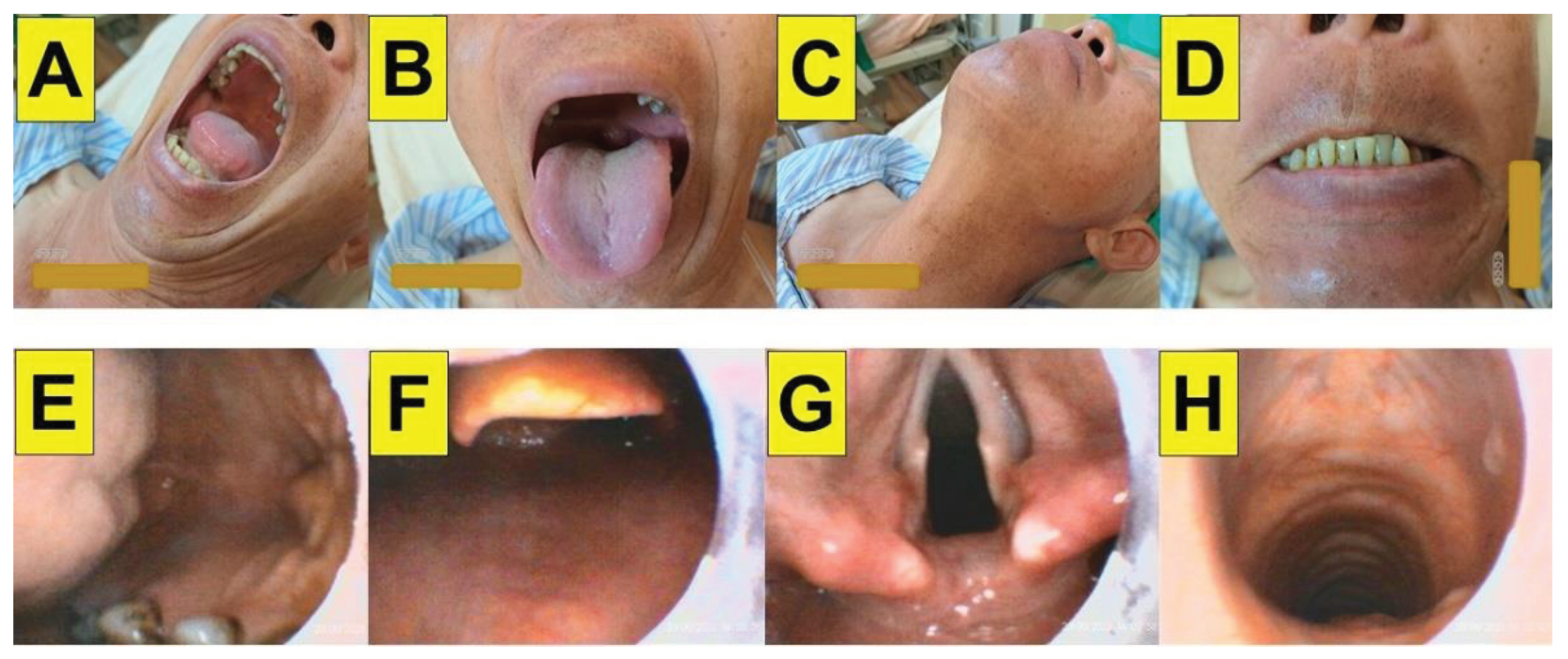
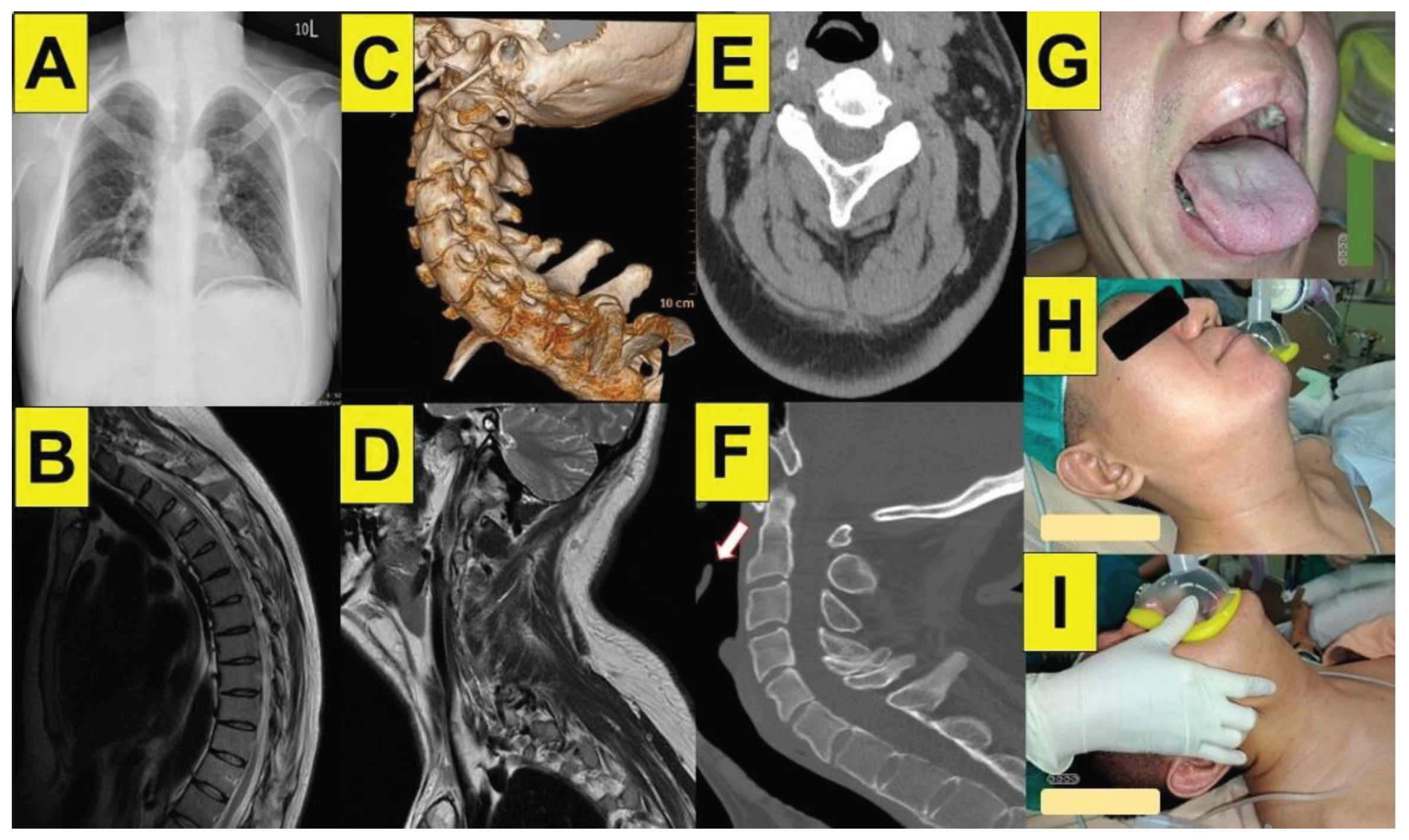
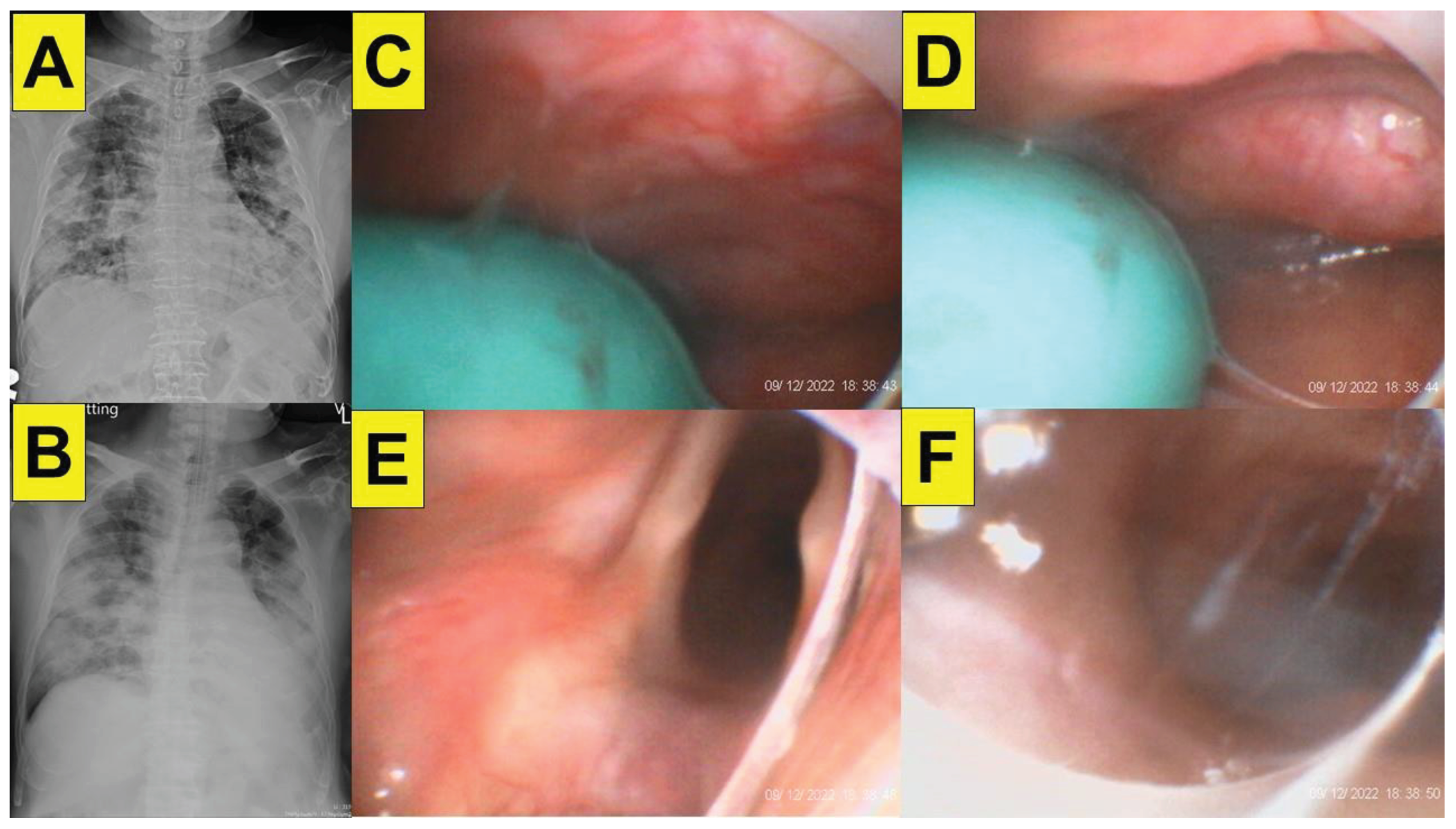
Figure 3 shows a typical case of a 60-year-old man with past history of right vocal leukoplakia and granular tumor diagnosed 8 years ago. Later diagnosis was progressive squamous cell carcinoma of the glottis–subglottic larynx (T1N0M0), with radiotherapy (6600 cGy). The MRI sequences confirmed these endoscopic findings on the vocal folds with the glottis–subglottic space reduction. The airway assessment conducted after tracheostomy shows normal by the classic predictors (i.e., mouth opening size, Mallampati score, sternomental distance, and upper lip bite test). The pre-operative nasoendoscopic images show recurrent tumor growth gradually in two years until causing dyspnea and signs of airway obstruction in the ER. To be on the safe side, the airway operator decided to perform awake nasal FOB for tracheal intubation, instead of applying styletubation. Emergent tracheostomy was performed after successful establishment of airway.
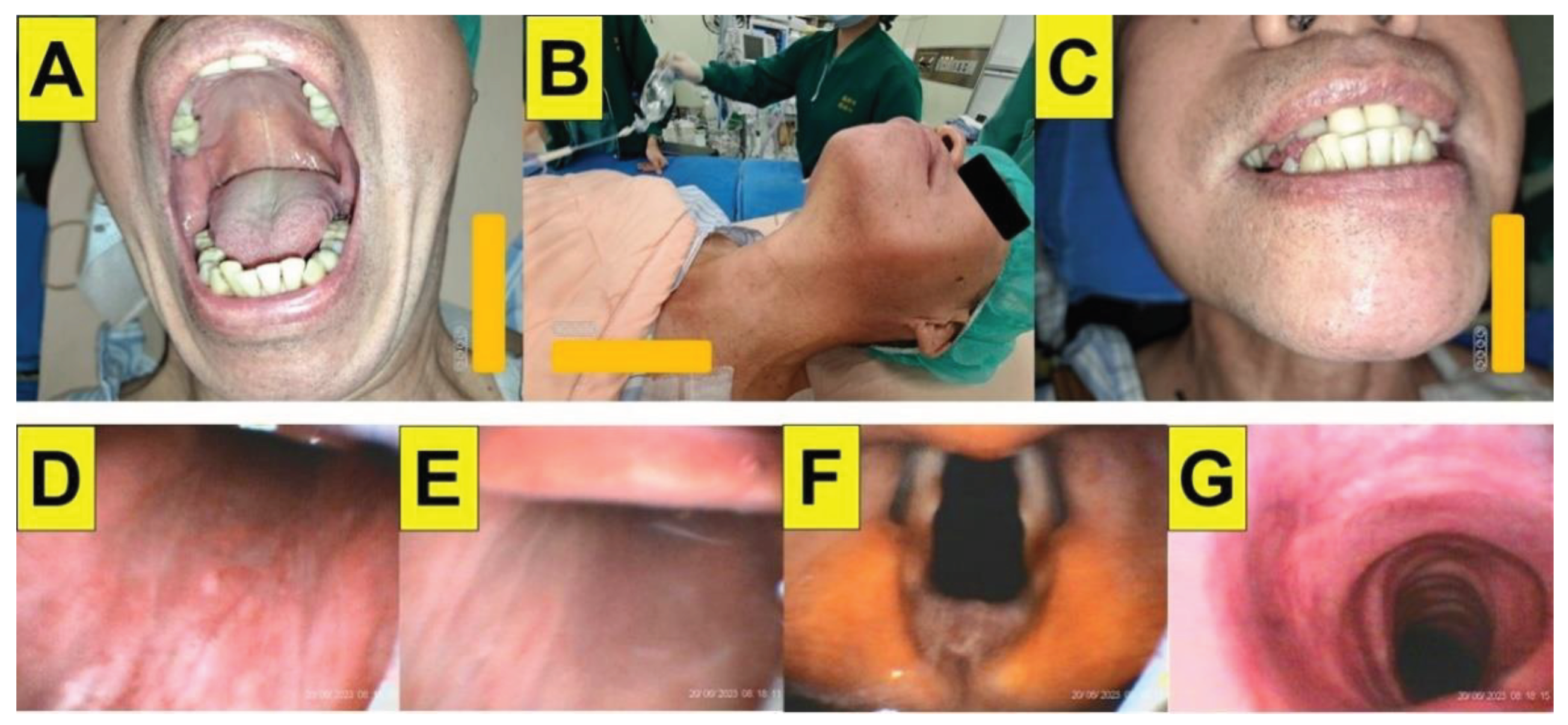
In contrast, the styletubation could be adopted as the first-line tool for tracheal intubation in certain difficult airway scenarios. Three typical cases with upper airway obstruction and dyspnea include hypopharyngeal and supraglottic carcinoma (
Figure 4). However, the styletubation technique would very much depend on the airway operator’s preference, clinical competency, and experiences. Without such self-confidence, awake FOB should be the option for tracheal intubation.
5.2. Styletubation Grading System for Tracheal Intubation
Numerous pre-operative airway evaluation methods have been used to predict whether potential difficult tracheal intubation might eventually occur in apparently normal patients [
62,
63,
64]. In addition to the traditional airway physical examinations [
65,
66,
67], several other individual physical examination findings might be predictive but do not reliably exclude the likelihood for a difficult tracheal intubation by laryngoscopy. Among them, upper lip bite test (ULBT) is reported to be an accurate individual bedside clinical assessment [
68,
69,
70,
71,
72]. Other individual tests that might be helpful to predict difficult airway, include neck circumference, cervical spine mobility, hyomental distance, thyromental distance [
73,
74,
75], sternomental distance [
76], etc. A simplified preoperative multivariate airway risk index may improve risk stratification for difficulty when laryngeal visualization is to obtain during rigid laryngoscopy (e.g., Grade IV) [
77].
While modified Mallampati classification (MMC) is an assessment to describe the relative size of the tongue base in relation to the oropharyngeal opening and space [
65,
66], it is for predicting the difficult airway by rigid laryngoscopy and not for others (e.g., FOB and styletubation). After the larynx is exposed by laryngoscopy, the degree of difficulty for glottis visualization is then described by the Cormack-Lehane classification [
78,
79]. The scoring system can predict the difficulty of advancement and insertion of ET tube into the trachea. Further, the percentage of glottic opening (POGO) scale is to assess airway visualization during endotracheal intubation by laryngoscopy and such POGO score shows good reliabilities and is able to distinguish patients with large and small degrees of partial glottic visibility [
80]. Therefore, POGO score might provide a better outcome for assessing the difference between various intubation techniques and modalities.
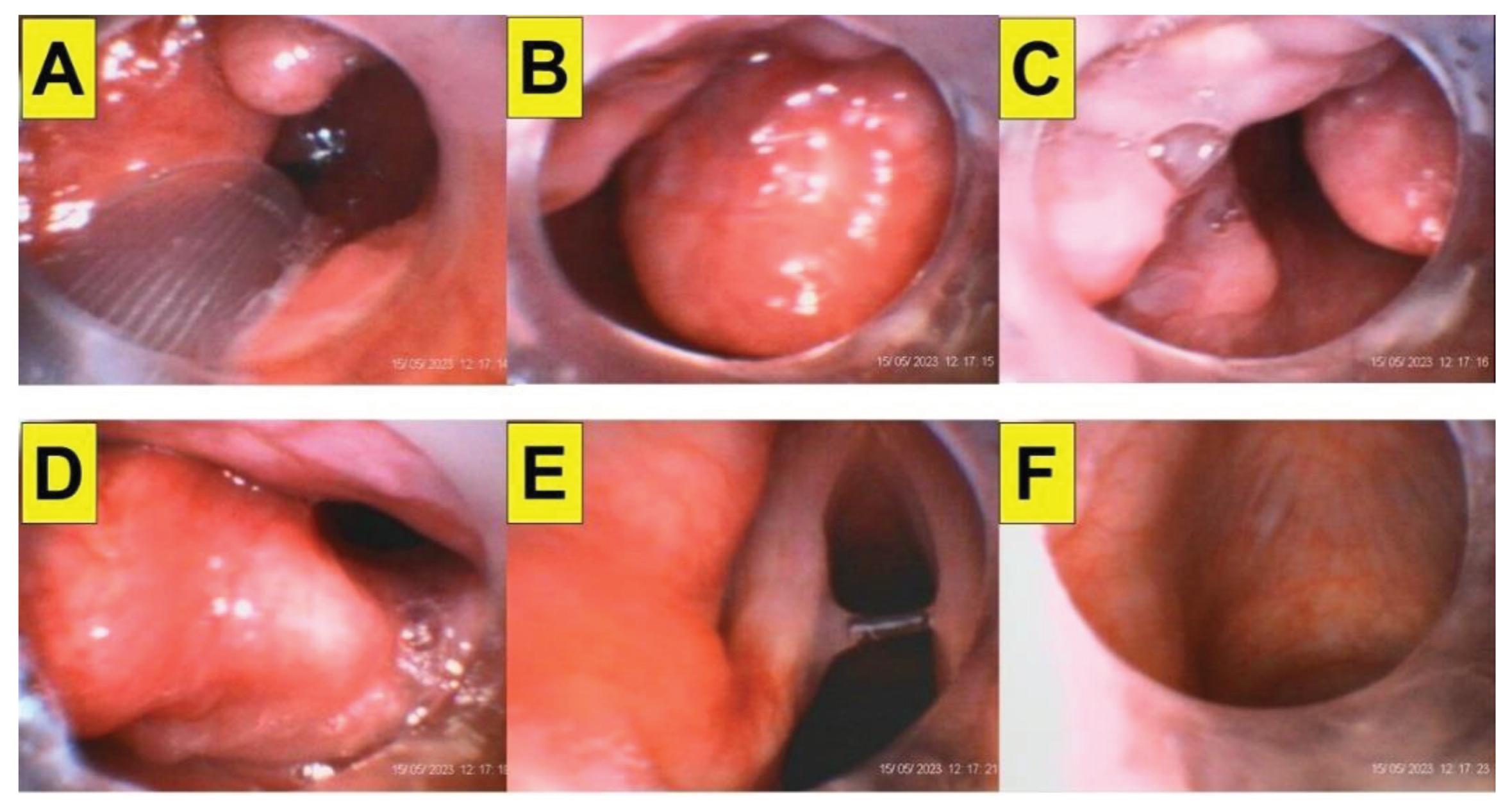
It should be stressed that “to see” (glottic visualization) and “to insert” (advancement of ET tube into trachea) are separate parts of tracheal intubation procedure. In contrast to the conventional roles of Mallampati score or Cormack-Lehane classification for laryngoscopy, the difficulty grading system of styletubation appears to be quite different. Although all the optic intubating instruments share similar difficulties (e.g., interfered by secretions, blood, vomitus, collapsed soft tissues), the main challenges for the operation of styletubation technique is the impact by the position status of patient’s epiglottis. Usually a normal shape and size of the epiglottis can easily be lifted up and pulled away from the posterior pharyngeal wall by jaw-thrust maneuver. After passing the stylet-ET tube unit under the epiglottis, a well-exposed glottis structure facilitates subsequent advancement and placement of the ET tube into trachea.
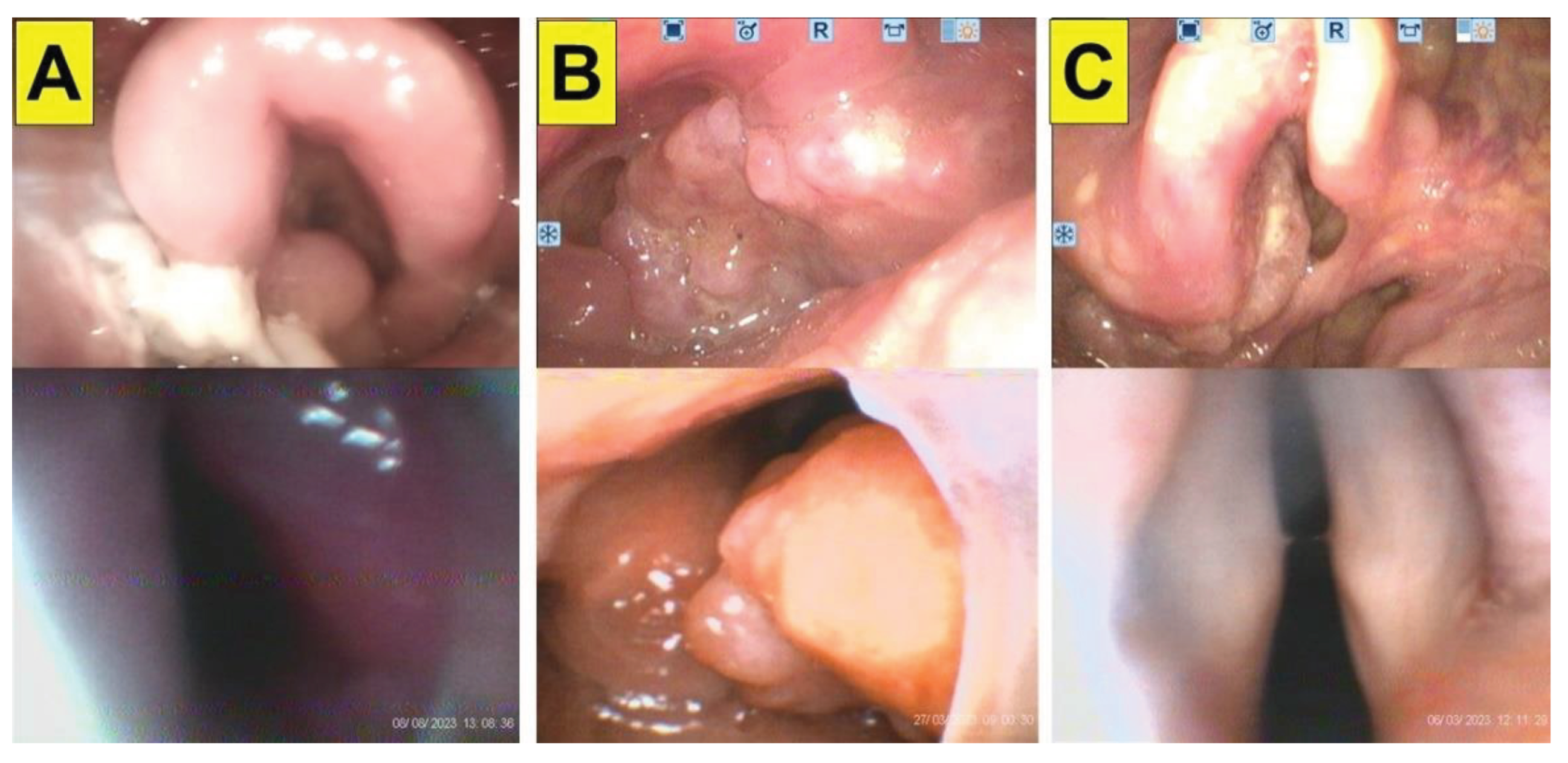
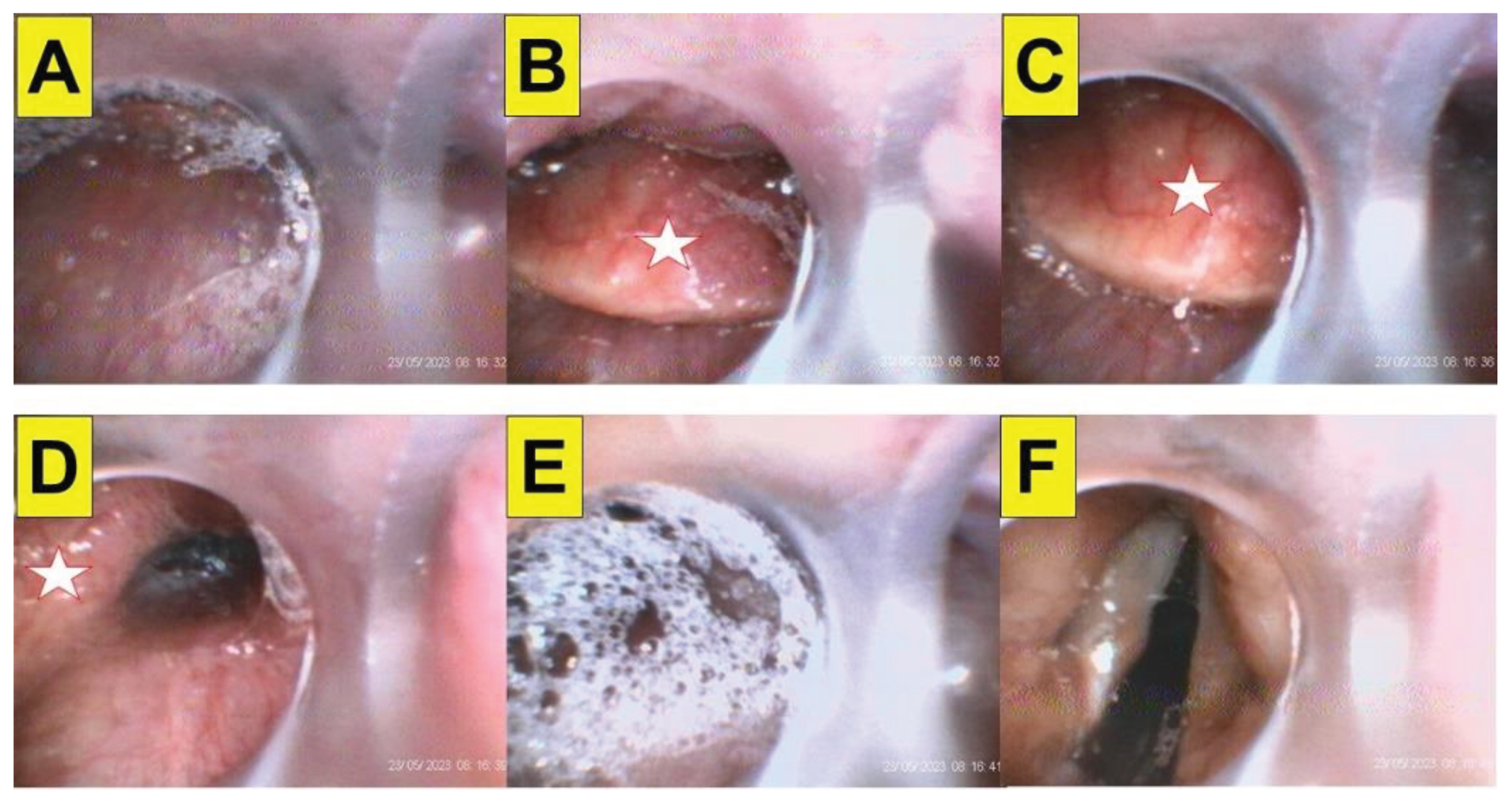
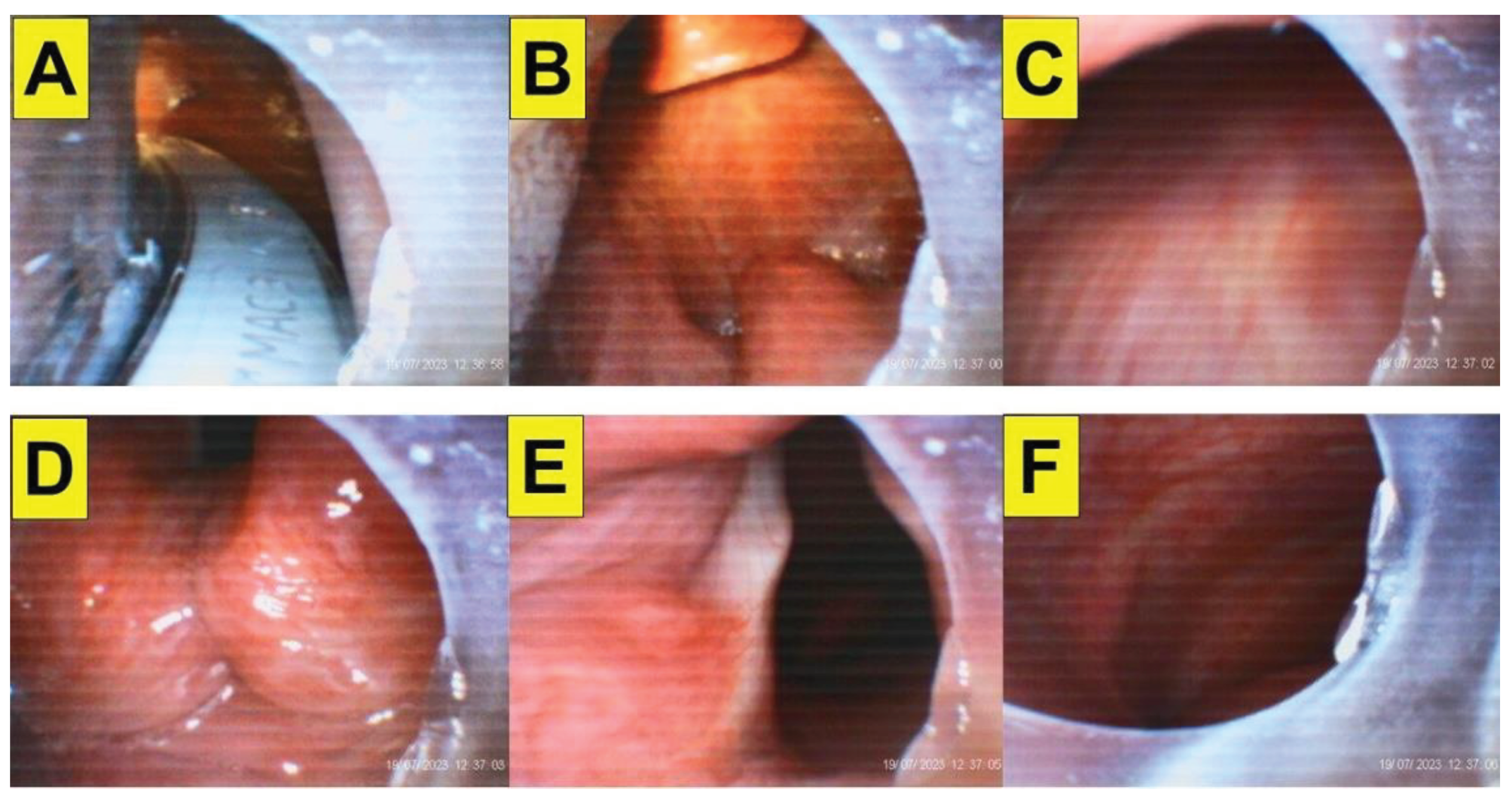
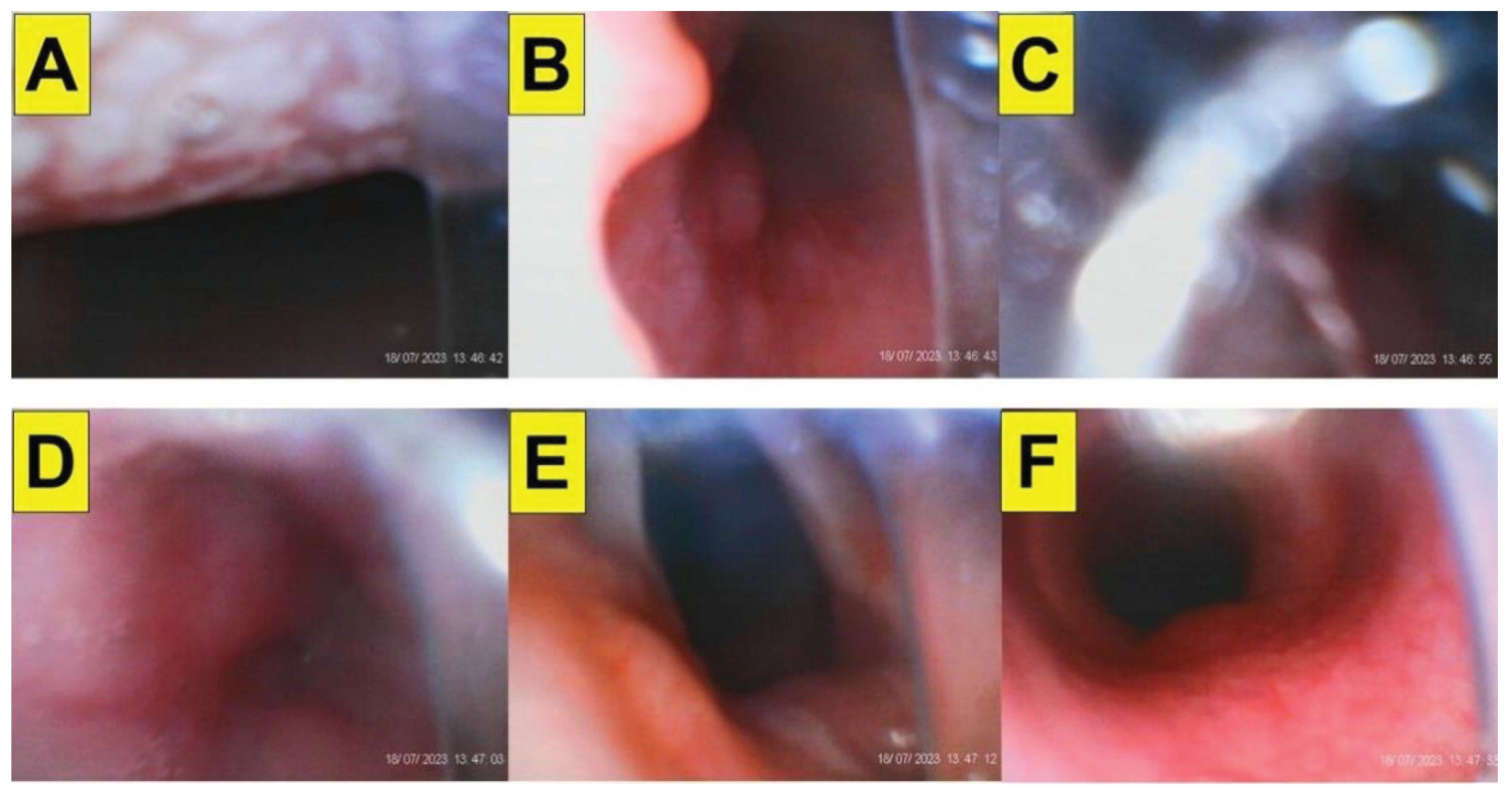
We therefore established a LQS (Luk-Qu-Shikani) grading system for such styletubation condition. The degree of difficulty performing styletubation can be categorized into three levels. The LQS grade 1 is defined as any part of the glottis structure can be seen in front of the epiglottis, usually with help of jaw thrust maneuver (
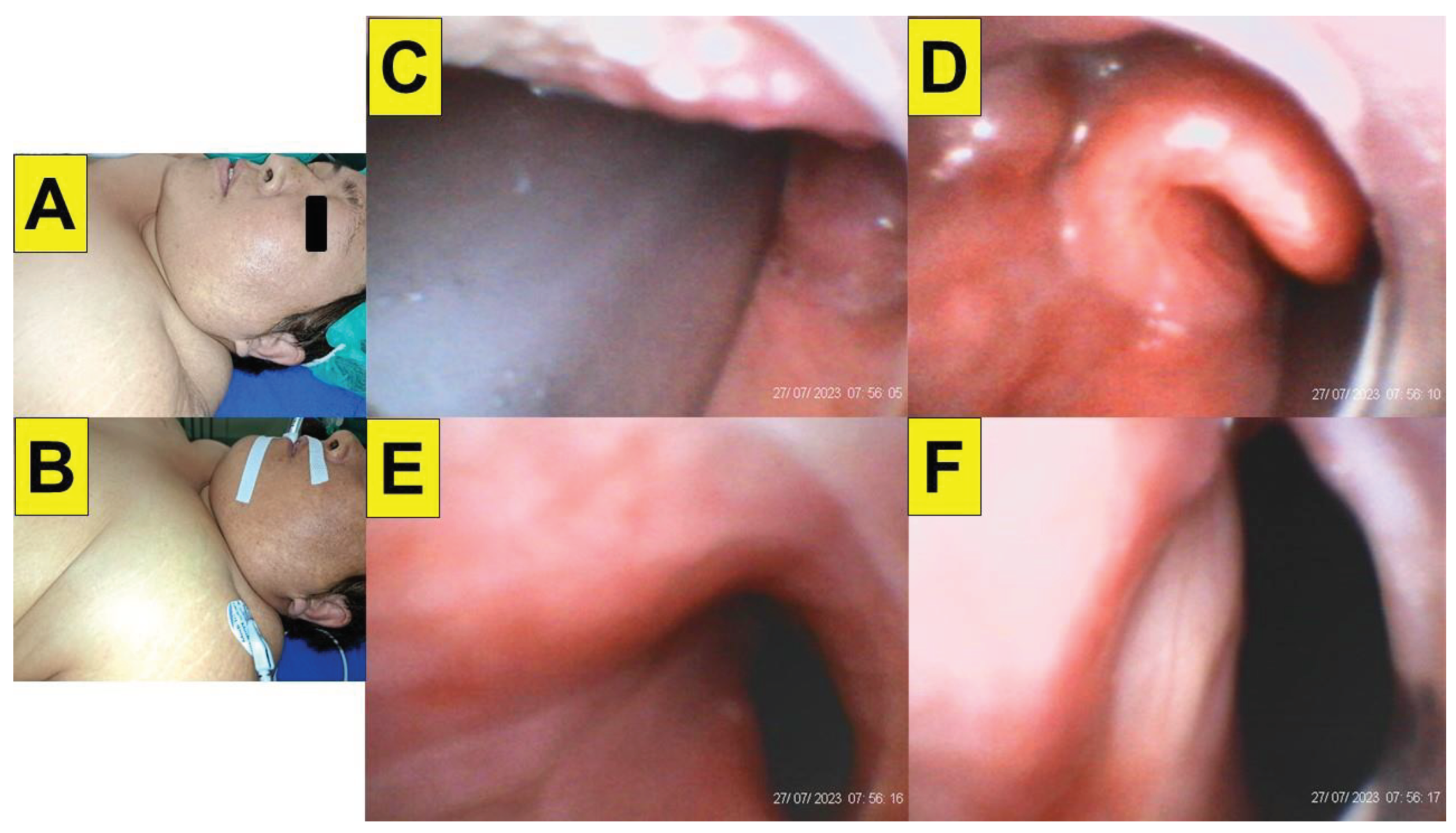
Figure 5). A trained airway operator (novice or experienced operator) can easily and smoothly perform styletubation in patients with LQS grade 1. When the epiglottis can be observed but only be lifted up a little with a marginal space beneath the epiglottis to allow the stylet-ET tube set pass through, then it is LQS grade 2 (
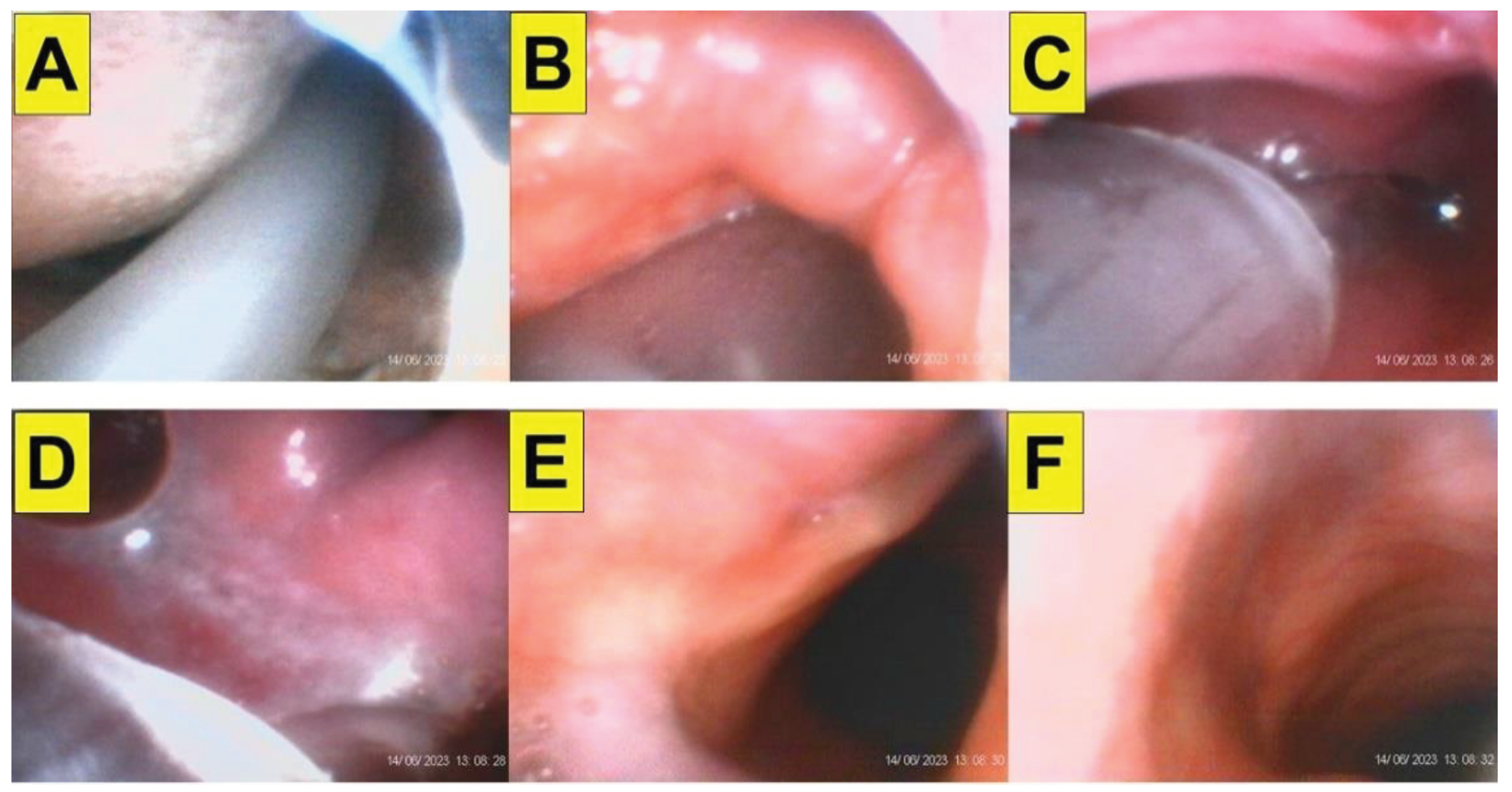
Figure 6). Usually, styletubation in patient with LQS grade 2 is not difficult. Rare but difficult, when the epiglottis can not be lifted up at all and completely dropped downward against the posterior pharyngeal wall, it is defined as the LQS grade 3 (
Figure 7). In patient with the LQS grade 3, difficult airway should be expected and need cautious efforts to operate. Usually, this rare scenario occurred in patients with certain degree of obesity, stiff neck (e.g., radiation fibrosis, status of flap reconstruction, tumor), ankylosing spondylitis, cervical spine immobility. In our experiences, the prevalence of grade 1 and grade 2 is about 65% and 35%, respectively. In anticipated difficult airway scenario, the chance to observe grade 3 is higher.
5.3. Intubating Time and Ease of Maneuverability as Outcome Parameters
In patients undergoing endotracheal intubation, it has been concluded that VL be superior to direct Macintosh DL as the former enlarges the view of glottis, shortens time to achieve intubation, facilitates intubation with easy manipulation, and causes less risk of complications. Tracheal intubation using VL has been shown to yield significantly higher intubation success rates and fewer complications than DL in patients with non-difficult airways [
81] and in particular may be useful instruments in the management of the predicted difficult airway [
82].
Although VL would be safer to employ in patients with vital requirement of hemodynamic stability, it did show longer intubation times than conventional DL [
83]. Even VL offers better glottic entrance visualization and intubation conditions, a good laryngeal view does not guarantee easy or successful tracheal tube insertion and might be VL-blade geometry-dependent [
84]. Although the time to intubate using VL is significantly dependent on operator’s experience and skills, such time is also influenced by, e.g., the angle of curvature of the stylet [
85].
In contrast to other comparators (e.g., first-pass success rate, total success rate, number of attempts, the quality of visualization, complications), “time to intubate” itself has been commonly used as a primary outcome comparator among various intubating modalities. Factors influencing such comparator include design of the device, patient’s factors, clinical scenarios, and airway operator’s skills and competency. Numerous clinical studies and meta-analyses show the comparison between Macintosh DL and various VL in normal and difficult airway scenarios [
86,
87,
88,
89]. For example, the time to intubation in normal airways with DL and VL, respectively, are 9 s and 11 s [
90]; 33 s and 34 s [
91]; 35 s and 56 s [
92]. In difficult airways, the time to intubation with DL and VL, respectively, are 38 s and 32 s [
93]; 56 s and 41s [
94]; 37 s and 14 s [
95]; 60 s and 45 s [
96]; 43 s and 45 s [
97]; 27 s ~ 50 s [
98]; 50 s and 57 s [
99]; 47 s and 38 s [
100]; 52 s and 63 s [
101]; 57 s and 45 s [
102]; 16 s and 14 s [
103]; 11 s and 73 s [
86].
In our experiences, when either experienced staff or novice trainees applied styletubation, it usually took about 5 s to 10 s (from lip to trachea) to accomplish the trachea intubation in patients with normal airway. Although it can be done in 3 s in an easy airway scenario and 30 s to 60 s for teaching purpose, we regard 10 s of such “time to intubation” be reasonable, easy, smooth, and elegant. We adhere to the tenet of “seeing around the corner” while applying the styletubation. All the signposts along the patient’s airway from mouth to trachea are encouraged to observe with styletubation technique. Even in patients with normal airway, incidental findings along patient’s airway could be observed once a while (e.g., large tonsils, laryngeal tumor, vocal polyps or cyst, tracheal tumor). In expected difficult airway, such standardized maneuverability of styletubation ensures a smooth and successful tracheal intubation.
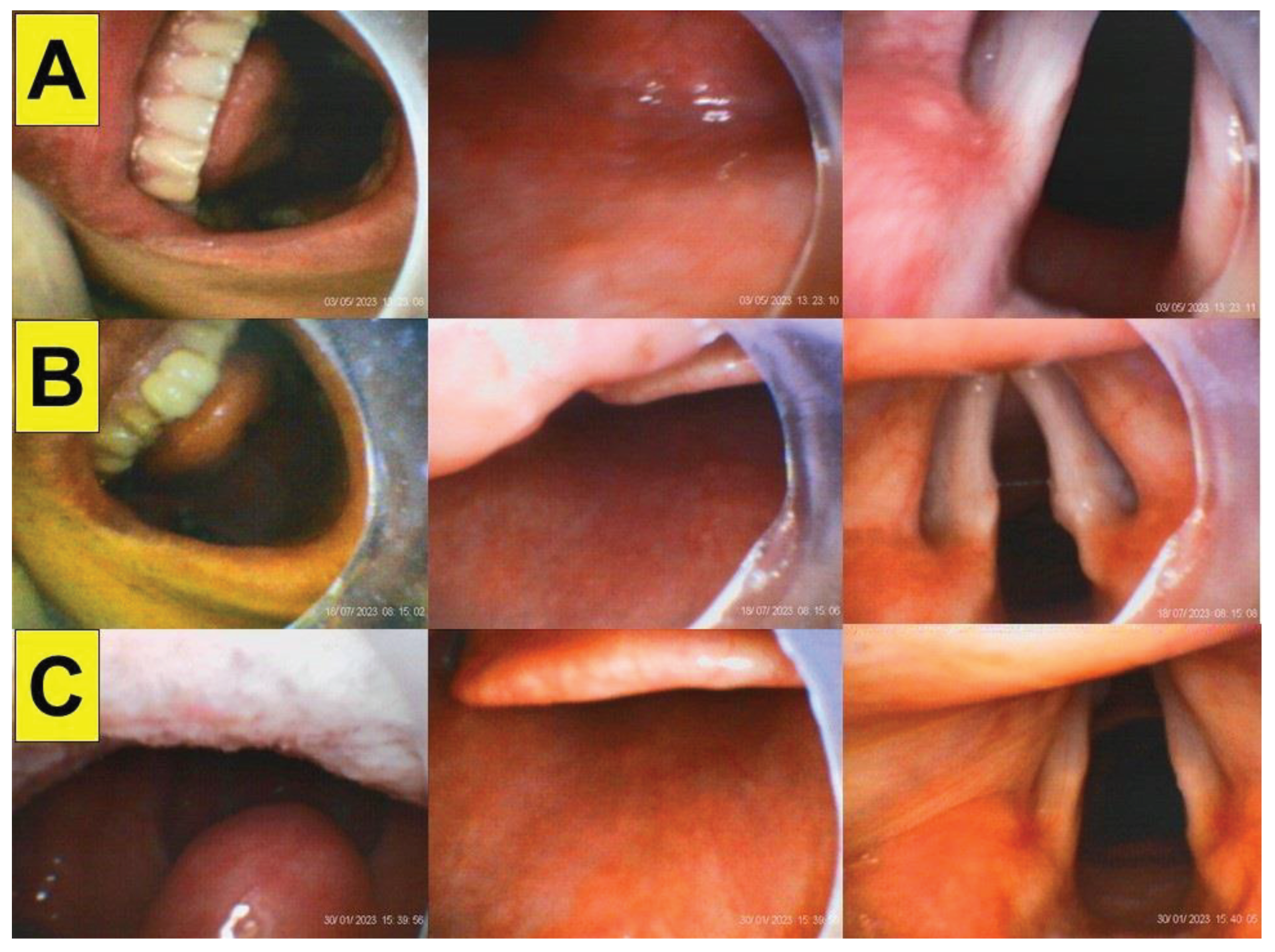
Figure 8 shows examples in three patients with time to intubation by 5 s, 7 s, and 15 s, respectively. It is worthy to mention that in our experience the first-pass successful rate is almost 100% for styletubation, while it varies widely and rather is low for DL and various VL (e.g., 86% ~ 93% [94); 70% ~ 93% [
97]; 42% ~ 72% [
92]; 37% ~ 98% [
98]; 44% ~ 90% [
99]; 85% ~ 100% [
100]; 78% ~ 67% [
101]; 92% ~ 85% [
102]; 90% ~ 85% [
103]; 26% ~ 92% [
86].)
5.4. Ankylosing Spondylitis
Among various scenarios of difficult airway management, patient’s limited cervical spine mobility is one of the tough and excruciating conditions. Patients who suffered cervical spine injuries usually are usually on immobilization device (e.g., halo ring, crowns, or vest) or cervical collar (neck brace). Other cervical spines immobilization scenarios include application of stereotactic head frame for neurosurgical procedures or practice. When laryngoscopy is on intended use under such difficult airway conditions, the airway managers often expected to encounter limited oro-pharyngeal-laryngeal exposure. Difficulty inserting the laryngoscopic blade, poor glottic visualization, or failure to orient and advance the ET tube into trachea are not uncommon.
There has been high hope for the plausible role of VL to perform better in cervical spine immobility conditions (e.g., reduced the risk of intubation failure) [
86,
104]. However, most comparative study results came from simulated scenarios (e.g., applying a cervical collar or manual in-line stabilization applied by an assistant during intubation) [
105,
106,
107] and airway mannequins models [
108,
109]. It should be stressed that VL maneuver per se may cause harm to fracture the cervical spine [
110]. It has been modeled that laryngoscopy itself might cause cervical motion and compressive strains on cervical spinal cords. The effects may exceed potentially injurious values with routine intubation forces [
111,
112]. Variables included laryngoscope-specific cervical extension, airway displacement/deformation needed for tracheal intubation, in additional to different cervical spine and airway tissue viscoelastic properties [
113]. In contrast to DL/VL, designed to improve success rate, enhance operator’s ease feeling, and reduce patient’s cervical spine movement, awake FOB is still considered as the gold-standard technique for airway management in such cases scenarios [
114,
115]. Other modalities of the intubating tools (e.g., Bonfils endoscope, lightwand) have also been studiedin this scene [
116,
117,
118,
119].
One of the examples of severe degree of limited cervical spine motion is the case of ankylosing spondylitis (AS). In few sporadic case reports, the roles of different intubating tools have been studied in patients with AS [
120,
121,
122], including combined VL with video stylet [
123]. Here, we present a case of AS undergoing corrective orthopedic spine surgery (
Figure 9). The patient has past history of ankylosing spondylitis with severe cervical hyperlordosis, and progressive thoracic kyphosis. Orthopedic operation included pedicle subtraction osteotomy (PSO), posterior instrumentation (PI), posterior lumbar interbody fusion (PLIF). His cervical mobility was severely restricted. After careful assessment was performed, we applied styletubation for tracheal intubation under standard induction of anesthesia. The time to intubationis 16 s with first-pass success (
Figure 10).
5.5. Obesity
Due to the anatomic anomalies, glottis visualization can be poor and tracheal intubation is often problematic in morbidly obese patients. Functionality and performance of VL in obese patients could be improved, e.g., better overall satisfaction score, intubation time, number of intubation attempts, and necessity of extra adjuncts [
124,
125,
126,
127,
128]. When compared to standard DL, VL required fewer intubation attempts, significantly reduced the time to secure the airway, and improved the glottic view in obese patients undergoing bariatric surgery [
97,
129].
Other intubating tools, e.g., rigid Bonfils fiberscope, when compared to VL, can be successfully used for awake intubation in morbidly obese patients when difficult airways are anticipated [
130]. In obese patients, the use of the Video Intubation Unit and VS significantly improves the visualization of the larynx, thereby improving the intubation conditions [
47,
131,
132]. Here, we demonstrate such role of styletubation in an obese patient (
Figure 11). This 42-year-old woman with a BMI 63.6 kg/m
2 underwent one anastomosis gastric bypass (OAGB). The pre-operative airway assessment showed more than acceptable for smooth trans-oral tracheal intubation after induction of anesthesia. The time to intubation was 18 s with first-pass success. The result is similar to our previous report regarding the role of styletubation in obese population [
43,
47]. It is worthy to note that ramp positioning with sniffing position and keeping patient’s neck until horizontal alignment between the sternal notch space and the external auditory meatus is helpful for laryngoscopy in obese patients [
133,
134].
5.6. Rapid Sequence Induction/Intubation
Although visualization of the vocal cords could be improved by using VL compared with direct laryngoscopy, whether better visualization consistently improves first-attempt success rate during rapid sequence oro-tracheal intubation remains to be an issue [
135,
136,
137]. Such application of VL has been studied in the settings of emergency department [
101,
138], out-of-hospital field [
139,
140,
141], intensive care units [
101], and simulated cardiopulmonary resuscitation manikin studies [
142,
143]. The inconsistent results of the role of VL are probably based on the airway operator’s training skill, experience, and clinical competency.
Cricoid pressure (CP) did not significantly improve the glottic visualization at laryngoscopy but increased the time to intubation significantly decreased the first-pass success rate [
135]. Recent large randomized clinical trial performed in patientsundergoing anesthesia with RSII failed to demonstrate the non-inferiority of the non-CP procedure in preventing pulmonary aspiration [
144]. Therefore, we routinely abandon CP (or Sellick maneuver) while applying styletubation for rapid sequence induction/intubation (RSII). Here we present a case of using styletubation for RSII (
Figure 12). This is a 59-year-old man with past history of atrial fibrillation, hypertension, ankylosing spondylitis (with stiff neck and limited cervical spine mobility), and deep vein thrombosis. He was admitted to our emergency room due to cerebellar hemorrhage and scheduled for emergent suboccipital decompressive craniectomy with intracranial pressure monitoring. Anesthetic induction agents were administered for RSII. The styletubation took only 9 s to complete with first-pass success. No CP was applied.
5.7. COVID-19 Pandemic
During the COVID-19 pandemic, the airway management strategies were developed to protect the airway managers and to provide a safe, accurate, and swift airway management of patients with COVID-19 [
145,
146,
147]. Both tools of VL and DL have been dedicated for use in patients with COVID-19, where the tracheal intubation is feasible. [
148,
149]. It is also noticed that the tracheal intubation procedure might be hampered by the personal protective equipment [
150,
151,
152,
153].
The plausible role of video-assisted intubating stylet for tracheal intubation during COVID-19 pandemicwas tested in the manikin model [
154]. In the real world, we have applied the styletubation technique for airway management in patients contracted with COVID-19 in our medical center after 2020 [
37,
40,
41,
43,
155,
156]. Here we present a case (
Figure 13) who developed bilateral pneumonia and acute respiratory distress syndrome (ARDS), congestive heart failure after he contracted COVID-19 virus during the pandemic period. He needed tracheal intubation for mechanical ventilation support in the negative-pressure isolation ward. The airway manager worn personal protective equipment (PPE) and applied styletubation technique to perform tracheal intubation. The whole procedure was smooth, swift, and accurate.
5.8. Combined VL and VS
When laryngoscopy reveals a Cormack-Lehane high grade (III or IV), certain options such as external laryngeal maneuvers (e.g., BURP), few adjuncts (gum elastic bougie, stylet) or other different airway modalities (e.g. FOB, second-generation supraglottic airway) could be applied for proper management. Not surprising, when difficult airway or repeated failure to intubate occurred, airway operators might use combined method of various airway tools [
157,
158,
159,
160,
161]. When Bonfils intubating fiberscope was applied, usually laryngoscopy (e.g., VL) was to assist to open enough airway space and to achieve the best possible laryngeal view [
162]. Such that, both views from the Bonfils scope and VL were brought together onto one single monitor. It is proposed that such combined technique can be used for difficult tracheal intubation [
163].
When optic rigid intubating stylet was designed and introduced clinically [
35], this optic stylet was proposed to use as a laryngoscopy adjunct. When the epiglottis is not seen during laryngoscopy [
164].On the other way around, laryngoscopy was found to be an adjunct to facilitate the application of VS [
42,
165,
166].
Figure 14 shows a case of applying videolaryngoscopy to facilitate styletubation and also confirmed the proper position and depth of the ET tube placement. It is worthy to mention, with such combined technique, the intubation was performed with first-pass success and smooth and swift tracheal intubation (7 s). In particular, the depth of ET tube placement by styletubation was able to be confirmed by videolaryngoscopy.
5.9. The Learning Curve
During the last two decades in Taiwan, the role of VL has been increasing in airway management and has lower rate of failed intubation in certain clinical scenarios (e.g., difficult airways) and clinical settings (e.g., operating rooms, emergency rooms, intensive care units). When compared with DL and VL, we found that styletubation appears to have satisfactory first-pass success rate, time to intubation, and rate of complications. While experienced airway operators may be skillful in various intubating tools and techniques, it is understandable that the novices (medical students, residents, non-anesthesiology trainees) might encounter difficulties during the learning and practice. Therefore, various training modules and assessment of tracheal intubation (e.g., VL and DL) for medical personnel have been reported [
167,
168,
169,
170]. Training inexperienced novice personnel with a VL, e.g., following a short teaching program, improves the success rate and time for tracheal intubation in patients with normal airways [
171] or in airway manikin with various simulated clinical scenarios [
172].
Different intubating device design itself (e.g., DL, channeled VL) may also affect novices’ learning curve (e.g., initial success rate, intubating time) [
170]. Learners’ behavior, personality, and prior experiences might also affect the learning curve and success rate of various intubating tools. In contrast to DL and VL, whether the styletubation is easier to learn by the novice trainees is not clear. Several study results show that the learning curve for novice personnel to acquire the skills of VS was quicker and steeper in real patients [
173] or airway manikins [
119,
174,
175,
176,
177]. A relatively small number of hands-on are required (less than 10 trials) to properly master such skill without causing oro-dental trauma.
Figure 15 shows a novice trainee (first-year resident of the ear-nose-throat department) operated the styletubation and resulted in first-pass success but a little bit longer intubation time (63 s). Individual differences in skill learning and competency do exist among all the trainees.
6. Time for Universal Practice of Styletubation?
The introduction of both lightwand (Trachlight™, Laerdal Medical Inc., Armonk, NY, USA) and video-assisted intubating stylet (Clarus Video System, Clarus Medical, LLC, 13355 10th Ave North, Suite 110, Minneapolis, MN 55441, USA) into Taiwan for tracheal intubation was in 2002 and 2009, respectively. Since then, the clinical experiences of applying such intubating tools were slowly built up and became known for local anesthesiologists. Since then, few clinical reports have been publishedin Taiwan and Asia [
118,
178,
179,
180,
181,
182,
183,
184,
185]. It was not until 2016 that styletubation has been universally practiced for routine tracheal intubation in Hualien Tzuchi Medical Hospital (HTZGH). It is an 1000–bed tertiary medical center in a remote region of the east coast of Taiwan. In its 18 operating rooms, all have been equipped with the VS, including Storz, UE, TuoRen, and Trachway. Also, VS has also been equipped in clinical settings outside the operating rooms, such as emergency rooms, intensive care units, and clinical competency center.
Table 1 shows the universal coverage of routine tracheal intubations conducted with styletubation. Except for teaching or other purposes, DL and VL were not routinely used any more by the anesthesia faculty staff. Excluding those who needed to undertake the nasal FOB (e.g., head/neck/oral surgery or pharyngeal/laryngeal lesions, etc.), styletubation technique is the common and routine technique universally adopted for tracheal intubation in HTZGH (
Table 1). Styletubation technique has therefore been applied for both normal and difficult airways [
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
155,
156].
Universal application of VL for routine tracheal intubationhas recently been advocated [
25,
26,
186,
187,
188,
189,
190], although some pros-cons arguments still existed [
191]. Recent clinical evidence creates a favorable argument for “universal” use of VL in anesthesia to improve efficiency, effectiveness, and safety of tracheal intubation. When VL (e.g., versus DL) was adopted as first choice for tracheal intubation in the operating rooms setting, such routine and universal use was associated with a significant lower rate of difficult airways, less use of airway rescue techniques and operator-reported difficulty [
26]. Many factors affected the controversial results of such role of VL, e.g., human factors (experiences and competency of the airway operator) [
192], patient factors (known or unexpected difficult airway), design of the devices, teaching models (simulation tools), etc.
In contrast, the role of styletubation for universal and routine tracheal intubation has never been studied or reported. A recent meta-analysis does not support the use of video-stylets as the first choice for patients with neck immobilization [
193]. Contradicted results from a meta-analysis study validated efficacy of video-stylets (and VL) for tracheal intubation in the situation of cervical spine immobilization [
194]. An airway manikin study results also support the advantageous role of video-stylet in normal airway and cervical spine immobilization scenarios [
119].
There are several limitations of the present narrative review article. In contrast to the highest level of evidence of the systematic reviews and meta-analysis, this narrative review article may still provide a new insight of the field of airway management and serve as sources of quick up-to-date reference for readers with interest in styletubation and laryngoscopy. However, our narrative review does have inherent shortcomings in terms of non-standardized and completeness of literature searching, potential human bias in the appraisal of retrieved articles, and validity and objectivity of interpretation of findings. Although we have a vast of clinical case experiences (more than 55,000 cases since 2016) of applying styletubation, we did not conduct any retrospective comparative study of styletubation against laryngoscopy. Some of the difficulties of such study design include different competency and preference of the airway operators, un-controlled clinical conditions and scenarios, completeness of medical records and airway evaluation, etc. While we presented several clinical scenarios for using styletubation in this article (e.g.,
Section 5), the sample size is small and impossible to make any statistical analysis on its significance. In fact, this clinical observational study was conducted by small group of airway operators in a single medical center. Therefore, the generalizability of the study conclusion may be limited and use and interpretation of the results should be carefully considered to avoid any unnecessary overstatement.
In conclusion, with our vast use experiences of the styletubation (in more than 55,000 patients from 2016 to 2023), we found this technique is swift (the time to intubate: from 3 s to 10 s), smooth (first-attempt success rate: 100%), safe (no airway complications), and easy (high subjective satisfaction and fast learning curve for the novice trainees) in both normal and difficult airway scenarios. We therefore propose styletubation technique can be feasibly applied as universal routine use for tracheal intubation.
Supplementary Materials
he following supporting information can be downloaded at the website of this paper posted on Preprints.org. Videos S1 (
Figure 5), Videos S2 (
Figure 6), Videos S3 (
Figure 7), Videos S4, S5, and S6 (
Figure 8), Video S7 (
Figure 10), Video S8 (
Figure 11), Video S9 (
Figure 12), Video S10 (
Figure 13), Video S11 (
Figure 14), Video S12 (
Figure 15).
Author Contributions
Conceptualization, H.-N.L., J.Z.Q.; methodology, H.-N.L.; formal analysis, H.-N.L., J.Z.Q.; investigation, H.-N.L.; resources, H.-N.L.; data curation, H.-N.L., J.Z.Q.; writing—original draft preparation, H.-N.L.; writing—review and editing, H.-N.L., J.Z.Q; visualization, H.-N.L.; supervision, H.-N.L.; project administration, H.-N.L.; funding acquisition, H.-N.L. Both authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and was approved by REC, Hualien Tzuchi Hospital (approved letter number: CR112-11).
Informed Consent Statement
Written informed consent was obtained from all patients or their legally authorized representatives.
Data Availability Statement
Not applicable.
Acknowledgments
This work was supported by Hualien Tzuchi Hospital.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Pieters, B.M.; Eindhoven, G.B.; Acott, C.; van Zundert, A.A. Pioneers of laryngoscopy: indirect, direct and video laryngoscopy. Anaesth. Intensive Care 2015, 43, 4–11. [Google Scholar] [CrossRef]
- McIntyre, J.W. Laryngoscope design and the difficult adult tracheal intubation. Can. J. Anaesth. 1989, 36, 94–98. [Google Scholar] [CrossRef]
- Macintosh, R.R. A new laryngoscope. Lancet 1943, 241, 205. [Google Scholar] [CrossRef]
- Knill, R.L. Difficult laryngoscopy made easy with a "BURP". Can. J. Anaesth. 1993, 40, 279–282. [Google Scholar] [CrossRef]
- Benumof, J.L.; Cooper, S.D. Quantitative improvement in laryngoscopic view by optimal external laryngeal manipulation. J. Clin. Anesth. 1996, 8, 136–140. [Google Scholar] [CrossRef]
- Takahata, O.; Kubota, M.; Mamiya, K.; Akama, Y.; Nozaka, T.; Matsumoto, H.; Ogawa, H. The efficacy of the "BURP" maneuver during a difficult laryngoscopy. Anesth. Analg. 1997, 84, 419–421. [Google Scholar] [CrossRef]
- Yu, T.; Wu, R.R.; Longhini, F.; Wang, B.; Wang, M.F.; Yang, F.F.; Hua, F.Z.; Yao, W.D.; Jin, X.J. The "BURP" maneuver improves the glottic view during laryngoscopy but remains a difficult procedure. J. Int. Med. Res. 2020, 48, 300060520925325. [Google Scholar] [CrossRef]
- Levitan, R.M.; Kinkle, W.C.; Levin, W.J.; Everett, W.W. Laryngeal view during laryngoscopy: a randomized trial comparing cricoid pressure, backward-upward-rightward pressure, and bimanual laryngoscopy. Ann. Emerg. Med. 2006, 47, 548–555. [Google Scholar] [CrossRef]
- Krantz, M.A.; Poulos, J.G.; Chaouki, K.; Adamek, P. The laryngeal lift: a method to facilitate endotracheal intubation. J. Clin. Anesth. 1993, 5, 297–301. [Google Scholar] [CrossRef]
- Bannister, F.B.; Macbeth, R.G. Direct laryngoscopy and tracheal intubation. Lancet 1944, 244, 651–654. [Google Scholar] [CrossRef]
- Takenaka, I.; Aoyama, K.; Iwagaki, T.; Ishimura, H.; Kadoya, T. The sniffing position provides greater occipito-atlanto-axial angulation than simple head extension: a radiological study. Can. J. Anaesth. 2007, 54, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Greenland, K.B.; Eley, V.; Edwards, M.J.; Allen, P.; Irwin, M.G. The origins of the sniffing position and the Three Axes Alignment Theory for direct laryngoscopy. Anaesth. Intensive Care 2008, 36, 23–27. [Google Scholar] [CrossRef]
- El-Orbany, M.; Woehlck, H.; Salem, M.R. Head and neck position for direct laryngoscopy. Anesth. Analg. 2011, 113, 103–109. [Google Scholar] [CrossRef]
- Levitan, R.M.; Mechem, C.C.; Ochroch, E.A.; Shofer, F.S.; Hollander, J.E. Head-elevated laryngoscopy position: improving laryngeal exposure during laryngoscopy by increasing head elevation. Ann. Emerg. Med. 2003, 41, 322–330. [Google Scholar] [CrossRef]
- Lee, L.; Weightman, W.M. Laryngoscopy force in the sniffing position compared to the extension-extension position. Anaesthesia 2008, 63, 375–378. [Google Scholar] [CrossRef] [PubMed]
- Adnet, F.; Borron, S.W.; Dumas, J.L.; Lapostolle, F.; Cupa, M.; Lapandry, C. Study of the "sniffing position" by magnetic resonance imaging. Anesthesiology 2001, 94, 83–86. [Google Scholar] [CrossRef]
- Greenland, K.B. A proposed model for direct laryngoscopy and tracheal intubation. Anaesthesia 2008, 63, 156–161. [Google Scholar] [CrossRef]
- Chou, H.C.; Wu, T.L. Rethinking the three axes alignment theory for direct laryngoscopy. Acta Anaesthesiol. Scand. 2001, 45, 261–262. [Google Scholar] [CrossRef]
- Chou, H.C.; Wu, T.L. A reconsideration of three axes alignment theory and sniffing position. Anesthesiology 2002, 97, 753–754. [Google Scholar] [CrossRef]
- Joffe, A.M.; Aziz, M.F.; Posner, K.L.; Duggan, L.V.; Mincer, S.L.; Domino, K.B. Management of difficult tracheal intubation: A closed claims analysis. Anesthesiology 2019, 131, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.M. Use of a new videolaryngoscope (GlideScope®) in the management of a difficult airway. Can. J. Anaesth. 2003, 50, 611–613. [Google Scholar] [CrossRef]
- Cooper, R.M.; Pacey, J.A.; Bishop, M.J.; McCluskey, S.A. Early clinical experience with a new videolaryngoscope (GlideScope®) in 728 patients. Can. J. Anaesth. 2005, 52, 191–198. [Google Scholar] [CrossRef]
- Niforopoulou, P.; Pantazopoulos, I.; Demestiha, T.; Koudouna, E.; Xanthos, T. Video-laryngoscopes in the adult airway management: a topical review of the literature. Acta Anaesthesiol. Scand. 2010, 54, 1050–1061. [Google Scholar] [CrossRef]
- Hansel, J.; Rogers, A.M.; Lewis, S.R.; Cook, T.M.; Smith, A.F. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation: a Cochrane systematic review and meta-analysis update. Br. J. Anaesth. 2022, 129, 612–623. [Google Scholar] [CrossRef]
- Paolini, J.B.; Donati, F.; Drolet, P. Review article: video-laryngoscopy: another tool for difficult intubation or a new paradigm in airway management? Can. J. Anaesth. 2013, 60, 184–191. [Google Scholar] [CrossRef]
- De Jong, A.; Sfara, T.; Pouzeratte, Y.; Pensier, J.; Rolle, A.; Chanques, G.; Jaber, S. Videolaryngoscopy as a first-intention technique for tracheal intubation in unselected surgical patients: a before and after observational study. Br. J. Anaesth. 2022, 129, 624–634. [Google Scholar] [CrossRef]
- Prekker, M.E.; Driver, B.E.; Trent, S.A.; Resnick-Ault, D.; Seitz, K.P.; Russell, D.W.; Gaillard, J.P.; Latimer, A.J.; Ghamande, S.A.; Gibbs, K.W.; Vonderhaar, D.J.; Whitson, M.R.; Barnes, C.R.; Walco, J.P.; Douglas, I.S.; Krishnamoorthy, V.; Dagan, A.; Bastman, J.J.; Lloyd, B.D.; Gandotra, S.; Goranson, J.K.; Mitchell, S.H.; White, H.D.; Palakshappa, J.A.; Espinera, A.; Page, D.B.; Joffe, A.; Hansen, S.J.; Hughes, C.G.; George, T.; Herbert, J.T.; Shapiro, N.I.; Schauer, S.G.; Long, B.J.; Imhoff, B.; Wang, L.; Rhoads, J.P.; Womack, K.N.; Janz, D.R.; Self, W.H.; Rice, T.W.; Ginde, A.A.; Casey, J.D.; Semler, M.W.; DEVICE Investigators and the Pragmatic Critical Care Research Group. Video versus direct laryngoscopy for tracheal intubation of critically ill adults. N. Engl. J. Med. 2023, 389, 418–429. [Google Scholar] [CrossRef]
- Apfelbaum, J.L.; Hagberg, C.A.; Connis, R.T.; Abdelmalak, B.B.; Agarkar, M.; Dutton, R.P.; Fiadjoe, J.E.; Greif, R.; Klock, P.A.; Mercier, D.; Myatra, S.N.; O’Sullivan, E.P.; Rosenblatt, W.H.; Sorbello, M.; Tung, A. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology 2022, 136, 31–81. [Google Scholar] [CrossRef]
- Berci, G.; Katz, R. Optical stylet: an aid to intubation and teaching. Ann. Otol. Rhinol. Laryngol. 1979, 88, 828–831. [Google Scholar] [CrossRef]
- Matek, J.; Kolek, F.; Klementova, O.; Michalek, P.; Vymazal, T. Optical devices in tracheal intubation-State of the art in 2020. Diagnostics 2021, 11, 575. [Google Scholar] [CrossRef]
- Bonfils, P. Difficult intubation in Pierre-Robin children, a new method: the retromolar route. Anaesthesist 1983, 32, 363–367. [Google Scholar]
- Thong, S.Y.; Wong, T.G. Clinical uses of the Bonfils Retromolar Intubation Fiberscope: a review. Anesth. Analg. 2012, 115, 855–866. [Google Scholar] [CrossRef]
- Hung, O.R.; Pytka, S.; Morris, I.; Murphy, M.; Launcelott, G.; Stevens, S.; MacKay, W.; Stewart, R.D. Clinical trial of a new lightwand device (Trachlight) to intubate the trachea. Anesthesiology 1995, 83, 509–514. [Google Scholar] [CrossRef]
- Agrò, F.; Hung, O.R.; Cataldo, R.; Carassiti, M.; Gherardi, S. Lightwand intubation using the TrachlightTM: a brief review of current knowledge. Can. J. Anaesth. 2001, 48, 592–599. [Google Scholar] [CrossRef]
- Shikani, A.H. New “seeing” stylet-scope and method for the management of the difficult airway. Otolaryngol. Head Neck Surg. 1999, 120, 113–116. [Google Scholar] [CrossRef]
- Greenland, K.B.; Liu, G.; Tan, H.; Edwards, M.; Irwin, M.G. Comparison of the Levitan FPS Scope and the single-use bougie for simulated difficult intubation in anaesthetised patients. Anaesthesia 2007, 62, 509–515. [Google Scholar] [CrossRef]
- Tsai, P.B.; Luk, H.N. Plastic sheet and video intubating stylet: A technical note. Asian J. Anesthesiol. 2021, 59, 117–121. [Google Scholar] [CrossRef]
- Tsay, P.J.; Yang, C.P.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-assisted intubating stylet technique for difficult intubation: A Case Series Report. Healthcare 2022, 10, 741. [Google Scholar] [CrossRef]
- Shih, T.L.; Koay, K.P.; Hu, C.Y.; Luk, H.N.; Qu, J.Z.; Shikani, A. The use of the Shikani video-assisted intubating stylet technique in patients with restricted neck mobility. Healthcare 2022, 10, 1688. [Google Scholar] [CrossRef]
- Yang, C.P.; Luk, H.N.; Qu, J.Z.; Shikani, A. The use of a video-assisted intubating stylet technique in a critically ill and contagious COVID-19 patient. Healthcare 2022, 10, 388. [Google Scholar] [CrossRef]
- Huang, C.H.; Su, I.M.; Jhuang, B.J.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-assisted stylet intubation with a plastic sheet barrier, a safe and simple technique for tracheal intubation of COVID-19 patients. Healthcare 2022, 10, 1105. [Google Scholar] [CrossRef]
- Jhuang, B.J.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-twin technique for airway management, combining video-intubating stylet with videolaryngoscope: A case series report and review of the literature. Healthcare 2022, 10, 2175. [Google Scholar] [CrossRef]
- Luk, H.N.; Luk, H.N.; Qu, J.Z.; Shikani, A. A paradigm shift of airway management: The role of video-assisted intubating stylet technique. In Advances in Tracheal Intubation; Lovich-Sapola, J., Ed.; IntechOpen: London, UK, 2022. [Google Scholar] [CrossRef]
- Lan, C.H.; Luk, H.N.; Qu, J.Z.; Shikani, A. An approach to improve the effectiveness of the video-assisted intubating stylet technique for tracheal intubation: A case series report. Healthcare 2023, 11, 891. [Google Scholar] [CrossRef]
- Luk, H.N.; Qu, J.Z.; Shikani, A. Styletubation: The paradigmatic role of video-assisted intubating stylet technique for routine tracheal intubation. Asian J. Anesthesiol. 2023, 61, 102–106. [Google Scholar] [CrossRef]
- Luk, H.N.; Qu, J.Z.; Shikani, A. Styletubation for routine tracheal intubation for ear-nose-throat surgical procedures. Ann. Otol. Head Neck Surg. 2023, 2, 1–13. [Google Scholar]
- Wu, B.G.; Luk, H.N.; Qu, J.Z.; Shikani, A. Styletubation in bariatric surgery: A case report. Healthcare 2023, 11, 2256. [Google Scholar] [CrossRef]
- Pan, H.-S.; Corey, T.; Luk, H.-N.; Qu, J.Z.; Shikani, A. Combined styletubation with videolaryngoscopy for tracheal intubation in patients undergoing thyroidectomy with intraoperative neuromonitoring. Anesth. Res. 2023, 1, 8–23. [Google Scholar] [CrossRef]
- Hall, C.E.; Shutt, L.E. Nasotracheal intubation for head and neck surgery. Anaesthesia 2003, 58, 249–256. [Google Scholar] [CrossRef]
- Chowdhury, N.; Cagliani, J.A.; Loyola, A.; SchianodiCola, J. Massive ameloblastoma requiring awake nasal fiberoptic intubation. Cureus 2023, 15, e40760. [Google Scholar] [CrossRef]
- Tsukamoto, M.; Hitosugi, T.; Yokoyama, T. Awake fiberoptic nasotracheal intubation for patients with difficult airway. J. Dent. Anesth. Pain Med. 2018, 18, 301–304. [Google Scholar] [CrossRef]
- Hsu, H.T.; Lin, C.H.; Tseng, K.Y.; Shen, Y.C.; Chen, C.H.; Chuang, W.M.; Cheng, K.I. Trachway in assistance of nasotracheal intubation with a preformed nasotracheal tube in patients undergoing oral maxillofacial surgery. Br. J. Anaesth. 2014, 113, 720–721. [Google Scholar] [CrossRef]
- Lee, M.C.; Tseng, K.Y.; Shen, Y.C.; Lin, C.H.; Hsu, C.W.; Hsu, H.J.; Lu, I.C.; Cheng, K.I. Nasotracheal intubation in patients with limited mouth opening: a comparison between fibreoptic intubation and the Trachway®. Anaesthesia 2016, 71, 31–38. [Google Scholar] [CrossRef]
- Cheng, T.; Wang, L.K.; Wu, H.Y.; Yang, X.D.; Zhang, X.; Jiao, L. Shikani Optical Stylet for awake nasal intubation in patients undergoing head and neck surgery. Laryngoscope 2021, 131, 319–325. [Google Scholar] [CrossRef]
- Hsieh, S.W.; Hung, K.C. Trachway® stylet: a perfect tool for nasotracheal intubation? Anaesthesia 2016, 71, 724. [Google Scholar] [CrossRef]
- Gemma, M.; Buratti, L.; Di Santo, D.; Calvi, M.R.; Ravizza, A.; Bondi, S.; Bussi, M.; Beretta, L. Pre-operative transnasal endoscopy as a predictor of difficult airway: A prospective cohort study. Eur. J. Anaesthesiol. 2020, 37, 98–104. [Google Scholar] [CrossRef]
- Sasu, P.B.; Pansa, J.I.; Stadlhofer, R.; Wünsch, V.A.; Loock, K.; Buscher, E.K.; Dankert, A.; Ozga, A.K.; Zöllner, C.; Petzoldt, M. Nasendoscopy to predict difficult videolaryngoscopy: A multivariable model development study. J. Clin. Med. 2023, 12, 3433. [Google Scholar] [CrossRef]
- Barclay-Steuart, A.; Großhennig, H.L.; Sasu, P.; Wünsch, V.A.; Stadlhofer, R.; Berger, J.; Stark, M.; Sehner, S.; Zöllner, C.; Petzoldt, M. Transnasal videoendoscopy for preoperative airway risk stratification: Development and validation of a multivariable risk prediction model. Anesth. Analg. 2023, 136, 1164–1173. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, I.; El-Boghdadly, K.; Bhagrath, R.; Hodzovic, I.; McNarry, A.F.; Mir, F.; O’Sullivan, E.P.; Patel, A.; Stacey, M.; Vaughan, D. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia 2020, 75, 509–528. [Google Scholar] [CrossRef]
- Asai, T.; Shingu, K. Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: incidence, causes and solutions. Br. J. Anaesth. 2004, 92, 870–881. [Google Scholar] [CrossRef]
- Touré, T.; Williams, S.R.; Kerouch, M.; Ruel, M. Patient factors associated with difficult flexible bronchoscopic intubation under general anesthesia: a prospective observational study. Can. J. Anaesth. 2020, 67, 706–714. [Google Scholar] [CrossRef]
- Detsky, M.E.; Jivraj, N.; Adhikari, N.K.; Friedrich, J.O.; Pinto, R.; Simel, D.L.; Wijeysundera, D.N.; Scales, D.C. Will this patient be difficult to intubate?: The rational clinical examination systematic review. JAMA 2019, 321, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.; Pace, N.L.; Lee, A.; Hovhannisyan, K.; Warenits, A.M.; Arrich, J.; Herkner, H. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst. Rev. 2018, 5, CD008874. [Google Scholar] [CrossRef]
- Roth, D.; Pace, N.L.; Lee, A.; Hovhannisyan, K.; Warenits, A.M.; Arrich, J.; Herkner, H. Bedside tests for predicting difficult airways: an abridged Cochrane diagnostic test accuracy systematic review. Anaesthesia 2019, 74, 915–928. [Google Scholar] [CrossRef]
- Mallampati, S.R. Clinical sign to predict difficult tracheal intubation (hypothesis). Can. Anaesth. Soc. J. 1983, 30, 316–317. [Google Scholar] [CrossRef]
- Mallampati, S.R.; Gatt, S.P.; Gugino, L.D.; Desai, S.P.; Waraksa, B.; Freiberger, D.; Liu, P.L. A clinical sign to predict difficult tracheal intubation: a prospective study. Can. Anaesth. Soc. J. 1985, 32, 429–434. [Google Scholar] [CrossRef]
- Samsoon, G.L.; Young, J.R. Difficult tracheal intubation: a retrospective study. Anaesthesia 1987, 42, 487–490. [Google Scholar] [CrossRef]
- Mahmoodpoor, A.; Soleimanpour, H.; Golzari, S.E.; Nejabatian, A.; Pourlak, T.; Amani, M.; Hajmohammadi, S.; Hosseinzadeh, H.; Esfanjani, R.M. Determination of the diagnostic value of the modified Mallampati score, upper lip bite test and facial angle in predicting difficult intubation: A prospective descriptive study. J. Clin. Anesth. 2017, 37, 99–102. [Google Scholar] [CrossRef]
- Kim, J.C.; Ki, Y.; Kim, J.; Ahn, S.W. Ethnic considerations in the upper lip bite test: the reliability and validity of the upper lip bite test in predicting difficult laryngoscopy in Koreans. BMC Anesthesiol. 2019, 19, 9. [Google Scholar] [CrossRef]
- Wang, L.Y.; Zhang, K.D.; Zhang, Z.H.; Zhang, D.X.; Wang, H.L.; Qi, F. Evaluation of the reliability of the upper lip bite test and the modified Mallampati test in predicting difficult intubation under direct laryngoscopy in apparently normal patients: a prospective observational clinical study. BMC Anesthesiol. 2022, 22, 314. [Google Scholar] [CrossRef]
- Kar, S.; Senapati, L.K.; Samanta, P.; Satapathy, G.C. Predictive value of modified Mallampati test and upper lip bite test concerning Cormack and Lehane’s laryngoscopy grading in the anticipation of difficult intubation: A cross-sectional study at a tertiary care hospital, Bhubaneswar, India. Cureus 2022, 14, e28754. [Google Scholar] [CrossRef]
- Moslemi, F.; Khan, Z.H.; Alizadeh, E.; Khamnian, Z.; Eftekhar, N.; Hosseini, M.S.; Mahmoodpoor, A. Upper lip bite test compared to modified Mallampati test in predicting difficult airway in obstetrics: A prospective observational study. J. Perioper. Pract. 2023, 33, 116–121. [Google Scholar] [CrossRef]
- Safavi, M.; Honarmand, A.; Zare, N. A comparison of the ratio of patient’s height to thyromental distance with the modified Mallampati and the upper lip bite test in predicting difficult laryngoscopy. Saudi J. Anaesth. 2011, 5, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Rao, K.V.N.; Dhatchinamoorthi, D.; Nandhakumar, A.; Selvarajan, N.; Akula, H.R.; Thiruvenkatarajan, V. Validity of thyromental height test as a predictor of difficult laryngoscopy: A prospective evaluation comparing modified Mallampati score, interincisor gap, thyromental distance, neck circumference, and neck extension. Indian J. Anaesth. 2018, 62, 603–608. [Google Scholar] [CrossRef]
- Chen, W.; Tian, T.; Li, X.; Jiang, T.; Xue, F. Use of the thyromental height test for prediction of difficult laryngoscopy: A systematic review and meta-analysis. J. Clin. Med. 2022, 11, 4906. [Google Scholar] [CrossRef] [PubMed]
- Amruthraju, C.M.; Sudhir, S. Rao.; Rooparani, K.; Vinay, R.; Vikas, K.N.; Deepak, T.S. The ratio of height to thyromental distance (RHTMD) and height to sternomental distance (RHSMD) as the predictive tests for difficult tracheal intubation. Cureus 2022, 14, e28734. [Google Scholar] [CrossRef]
- El-Ganzouri, A.R.; McCarthy, R.J.; Tuman, K.J.; Tanck, E.N.; Ivankovich, A.D. Preoperative airway assessment: predictive value of a multivariate risk index. Anesth. Analg. 1996, 82, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M. A new practical classification of laryngeal view. Anaesthesia 2000, 55, 274–279. [Google Scholar] [CrossRef]
- Krage, R.; van Rijn, C.; van Groeningen, D.; Loer, S.A.; Schwarte, L.A.; Schober, P. Cormack-Lehane classification revisited. Br. J. Anaesth. 2010, 105, 220–227. [Google Scholar] [CrossRef]
- Levitan, R.M.; Ochroch, E.A.; Kush, S.; Shofer, F.S.; Hollander, J.E. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad. Emerg. Med. 1998, 5, 919–923. [Google Scholar] [CrossRef]
- Liu, D.X.; Ye, Y.; Zhu, Y.H.; Li, J.; He, H.Y.; Dong, L.; Zhu, Z.Q. Intubation of non-difficult airways using video laryngoscope versus direct laryngoscope: a randomized, parallel-group study. BMC Anesthesiol. 2019, 19, 75. [Google Scholar] [CrossRef]
- Serocki, G.; Bein, B.; Scholz, J.; Dörges, V. Management of the predicted difficult airway: a comparison of conventional blade laryngoscopy with video-assisted blade laryngoscopy and the GlideScope. Eur. J. Anaesthesiol. 2010, 27, 24–30. [Google Scholar] [CrossRef]
- Misirlioglu, G.; Sen, O. Comparison of GlideScope video laryngoscopy and Macintosh laryngoscope in ear-nose and throat surgery. Ir. J. Med. Sci. 2016, 185, 729–733. [Google Scholar] [CrossRef]
- Van Zundert, A.; Maassen, R.; Lee, R.; Willems, R.; Timmerman, M.; Siemonsma, M.; Buise, M.; Wiepking, M. A Macintosh laryngoscope blade for videolaryngoscopy reduces stylet use in patients with normal airways. Anesth. Analg. 2009, 109, 825–831. [Google Scholar] [CrossRef]
- Gayathri, B.; Mani, K.; Vishak, M.; John, J.; Srinivasan, R.G.; Mirunalini, G. Factors influencing the time of intubation using C-MAC D-Blade® video laryngoscope: An observational cross-sectional study. Cureus 2023, 15, e34050. [Google Scholar] [CrossRef] [PubMed]
- Singleton, B.N.; Morris, F.K.; Yet, B.; Buggy, D.J.; Perkins, Z.B. Effectiveness of intubation devices in patients with cervical spine immobilisation: a systematic review and network meta-analysis. Br. J. Anaesth. 2021, 126, 1055–1066. [Google Scholar] [CrossRef]
- Lee, J.; Cho, Y.; Kim, W.; Choi, K.S.; Jang, B.H.; Shin, H.; Ahn, C.; Kim, J.G.; Na, M.K.; Lim, T.H.; Kim, D.W. Comparisons of videolaryngoscopes for intubation undergoing general anesthesia: Systematic review and network meta-analysis of randomized controlled trials. J. Pers. Med. 2022, 12, 363. [Google Scholar] [CrossRef]
- Hansel, J.; Rogers, A.M.; Lewis, S.R.; Cook, T.M.; Smith, A.F. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst. Rev. 2022, 4, CD011136. [Google Scholar] [CrossRef] [PubMed]
- Nedunchezhian, V.; Nedunchezhian, I.; Van Zundert, A. Clinically preferred videolaryngoscopes in airway management: An updated systematic review. Healthcare 2023, 11, 2383. [Google Scholar] [CrossRef] [PubMed]
- Amini, S.; Shakib, M. Hemodynamic changes following endotracheal intubation in patients undergoing cesarean section with general anesthesia: application of glidescope® videolaryngoscope versus direct laryngoscope. Anesth. Pain Med. 2015, 5, e21836. [Google Scholar] [CrossRef]
- Pažur, I.; Maldini, B.; Hostić, V.; Ožegić, O.; Obraz, M. Comparison of Cormack Lehane grading system and intubation difficulty score in patients intubated by D-Blade Video and direct Macintosh laryngoscope: A randomized controlled study. Acta Clin. Croat. 2016, 55, 560–564. [Google Scholar] [CrossRef]
- Al-Ghamdi, A.A.; El Tahan, M.R.; Khidr, A.M. Comparison of the Macintosh, GlideScope®, Airtraq®, and King Vision™ laryngoscopes in routine airway management. Minerva Anestesiol. 2016, 82, 1278–1287. [Google Scholar]
- Akbar, S.H.; Ooi, J.S. Comparison between C-MAC video-laryngoscope and Macintosh direct laryngoscope during cervical spine immobilization. Middle East J. Anaesthesiol. 2015, 23, 43–50. [Google Scholar]
- Lim, Y.; Yeo, S.W. A comparison of the GlideScope® with the Macintosh laryngoscope for tracheal intubation in patients with simulated difficult airway. Anaesth. Intensive Care 2005, 33, 243–247. [Google Scholar] [CrossRef]
- Ranieri, D.Jr.; Filho, S.M.; Batista, S.; do Nascimento, P.Jr. Comparison of Macintosh and Airtraq™ laryngoscopes in obese patients placed in the ramped position. Anaesthesia 2012, 67, 980–985. [Google Scholar] [CrossRef] [PubMed]
- Foulds, L.T.; McGuire, B.E.; Shippey, B.J. A randomised cross-over trial comparing the McGrath® Series 5 videolaryngoscope with the Macintosh laryngoscope in patients with cervical spine immobilisation. Anaesthesia 2016, 71, 437–442. [Google Scholar] [CrossRef]
- Yumul, R.; Elvir-Lazo, O.L.; White, P.F.; Sloninsky, A.; Kaplan, M.; Kariger, R.; Naruse, R.; Parker, N.; Pham, C.; Zhang, X.; Wender, R.H. Comparison of three video laryngoscopy devices to direct laryngoscopy for intubating obese patients: a randomized controlled trial. J. Clin. Anesth. 2016, 31, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Kleine-Brueggeney, M.; Greif, R.; Schoettker, P.; Savoldelli, G.L.; Nabecker, S.; Theiler, L.G. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: a multicentre randomized controlled trial. Br. J. Anaesth. 2016, 116, 670–679. [Google Scholar] [CrossRef]
- Kleine-Brueggeney, M.; Buttenberg, M.; Greif, R.; Nabecker, S.; Theiler, L. Evaluation of three unchannelled videolaryngoscopes and the Macintosh laryngoscope in patients with a simulated difficult airway: a randomised, controlled trial. Anaesthesia 2017, 72, 370–378. [Google Scholar] [CrossRef]
- Zhu, H.; Liu, J.; Suo, L.; Zhou, C.; Sun, Y.; Jiang, H. A randomized controlled comparison of non-channeled king vision, McGrath MAC video laryngoscope and Macintosh direct laryngoscope for nasotracheal intubation in patients with predicted difficult intubations. BMC Anesthesiol. 2019, 19, 166. [Google Scholar] [CrossRef]
- Suzuki, K.; Kusunoki, S.; Tanigawa, K.; Shime, N. Comparison of three video laryngoscopes and direct laryngoscopy for emergency endotracheal intubation: a retrospective cohort study. BMJ. Open 2019, 9, e024927. [Google Scholar] [CrossRef]
- Roh, G.U.; Kwak, H.J.; Lee, K.C.; Lee, S.Y.; Kim, J.Y. Randomized comparison of McGrath MAC videolaryngoscope, Pentax Airway Scope, and Macintosh direct laryngoscope for nasotracheal intubation in patients with manual in-line stabilization. Can. J. Anaesth. 2019, 66, 1213–1220. [Google Scholar] [CrossRef]
- Mallick, T.; Verma, A.; Jaiswal, S.; Haldar, M.; Sheikh, W.R.; Vishen, A.; Snehy, A.; Ahuja, R. Comparison of the time to successful endotracheal intubation using the Macintosh laryngoscope or KingVision video laryngoscope in the emergency department: A prospective observational study. Turk. J. Emerg. Med. 2020, 20, 22–27. [Google Scholar] [CrossRef]
- Suppan, L.; Tramèr, M.R.; Niquille, M.; Grosgurin, O.; Marti, C. Alternative intubation techniques vs Macintosh laryngoscopy in patients with cervical spine immobilization: systematic review and meta-analysis of randomized controlled trials. Br. J. Anaesth. 2016, 116, 27–36. [Google Scholar] [CrossRef]
- Robitaille, A.; Williams, S.R.; Tremblay, M.H.; Guilbert, F.; Thériault, M.; Drolet, P. Cervical spine motion during tracheal intubation with manual in-line stabilization: direct laryngoscopy versus GlideScope® videolaryngoscopy. Anesth. Analg. 2008, 106, 935–941. [Google Scholar] [CrossRef]
- Houde, B.J.; Williams, S.R.; Cadrin-Chênevert, A.; Guilbert, F.; Drolet, P. A comparison of cervical spine motion during orotracheal intubation with the Trachlight® or the flexible fiberoptic bronchoscope. Anesth. Analg. 2009, 108, 1638–1643. [Google Scholar] [CrossRef] [PubMed]
- Paik, H.; Park, H.P. Randomized crossover trial comparing cervical spine motion during tracheal intubation with a Macintosh laryngoscope versus a C-MAC D-blade videolaryngoscope in a simulated immobilized cervical spine. BMC Anesthesiol. 2020, 20, 201. [Google Scholar] [CrossRef]
- Wetsch, W.A.; Spelten, O.; Hellmich, M.; Carlitscheck, M.; Padosch, S.A.; Lier, H.; Böttiger, B.W.; Hinkelbein, J. Comparison of different video laryngoscopes for emergency intubation in a standardized airway manikin with immobilized cervical spine by experienced anaesthetists. A randomized, controlled crossover trial. Resuscitation 2012, 83, 740–745. [Google Scholar] [CrossRef] [PubMed]
- Smereka, J.; Ladny, J.R.; Naylor, A.; Ruetzler, K.; Szarpak, L. C-MAC compared with direct laryngoscopy for intubation in patients with cervical spine immobilization: A manikin trial. Am. J. Emerg. Med. 2017 35, 1142–1146. [CrossRef]
- Epaud, A.; Levesque, E.; Clariot, S. Dramatic cervical spine injury secondary to videolaryngoscopy in a patient suffering from ankylosing spondylitis. Anesthesiology 2021, 135, 495–496. [Google Scholar] [CrossRef] [PubMed]
- Gadomski, B.C.; Hindman, B.J.; Page, M.I.; Dexter, F.; Puttlitz, C.M. Intubation biomechanics: Clinical implications of computational modeling of intervertebral motion and spinal cord strain during tracheal intubation in an intact cervical spine. Anesthesiology 2021, 135, 1055–1065. [Google Scholar] [CrossRef]
- Gadomski, B.C.; Hindman, B.J.; Poland, M.J.; Page, M.I.; Dexter, F.; Puttlitz, C.M. Intubation biomechanics: Computational modeling to identify methods to minimize cervical spine motion and spinal cord strain during laryngoscopy and tracheal intubation in an intact cervical spine. J. Clin. Anesth. 2022, 81, 110909. [Google Scholar] [CrossRef]
- Hindman, B.J.; Santoni, B.G.; Puttlitz, C.M.; From, R.P.; Todd, M.M. Intubation biomechanics: laryngoscope force and cervical spine motion during intubation with Macintosh and Airtraq laryngoscopes. Anesthesiology 2014, 121, 260–271. [Google Scholar] [CrossRef]
- Rosenstock, C.V.; Thøgersen, B.; Afshari, A.; Christensen, A.L.; Eriksen, C.; Gätke, M.R. Awake fiberoptic or awake video laryngoscopic tracheal intubation in patients with anticipated difficult airway management: a randomized clinical trial. Anesthesiology 2012, 116, 1210–1216. [Google Scholar] [CrossRef]
- Yumul, R.; Elvir-Lazo, O.L.; White, P.F.; Durra, O.; Ternian, A.; Tamman, R.; Naruse, R.; Ebba, H.; Yusufali, T.; Wong, R.; Hernandez Conte, A.; Farnad, S.; Pham, C.; Wender, R.H. Comparison of the C-MAC video laryngoscope to a flexible fiberoptic scope for intubation with cervical spine immobilization. J. Clin. Anesth. 2016, 31, 46–52. [Google Scholar] [CrossRef]
- Rudolph, C.; Schneider, J.P.; Wallenborn, J.; Schaffranietz, L. Movement of the upper cervical spine during laryngoscopy: a comparison of the Bonfils intubation fibrescope and the Macintosh laryngoscope. Anaesthesia 2005, 60, 668–672. [Google Scholar] [CrossRef]
- Kim, E.; Kim, B.G.; Lim, Y.J.; Jeon, Y.T.; Hwang, J.W.; Lee, S.Y.; Park, H.P. A comparison between the conventional and the laryngoscope-assisted lightwand intubation techniques in patients with cervical immobilization: A prospective randomized study. Anesth. Analg. 2017, 125, 854–859. [Google Scholar] [CrossRef]
- Nam, K.; Lee, Y.; Park, H.P.; Chung, J.; Yoon, H.K.; Kim, T.K. Cervical spine motion during tracheal intubation using an Optiscope versus the McGrath videolaryngoscope in patients with simulated cervical immobilization: A prospective randomized crossover study. Anesth. Analg. 2019, 129, 1666–1672. [Google Scholar] [CrossRef]
- Park, J.W.; An, S.; Park, S.; Nahm, F.S.; Han, S.H.; Kim, J.H. Comparison of a new Video Intubation Stylet and McGrath® MAC video laryngoscope for intubation in an airway manikin with normal airway and cervical spine immobilization scenarios by novice personnel: A randomized crossover study. Biomed. Res. Int. 2021, 2021, 4288367. [Google Scholar] [CrossRef] [PubMed]
- Saricicek, V.; Mizrak, A.; Gul, R.; Goksu, S.; Cesur, M. GlideScope video laryngoscopy use tracheal intubation in patients with ankylosing spondylitis: a series of four cases and literature review. J. Clin. Monit. Comput. 2014, 28, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Bindra, A.; Mahajan, C.; Yadav, N. Airway management in a patient of ankylosing spondylitis with traumatic cervical spine injury. Saudi J. Anaesth. 2015, 9, 327–329. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, P.S.; Ma, H.P.; Wong, C.S.; Ong, J.R. Emergency tracheal intubation in an ankylosing spondylitis patient in a sitting position using an Airway Scope combined with face-to-face and digital intubation. J. Emerg. Med. 2018, 54, 674–677. [Google Scholar] [CrossRef]
- Chen, W.C.; Lin, S.; He, H.F. Case report: Double visualization intubation strategy for patients with ankylosing spondylitis. Front. Med. 2022, 9, 659624. [Google Scholar] [CrossRef]
- Marrel, J.; Blanc, C.; Frascarolo, P.; Magnusson, L. Videolaryngoscopy improves intubation condition in morbidly obese patients. Eur. J. Anaesthesiol. 2007, 24, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Maassen, R.; Lee, R.; Hermans, B.; Marcus, M.; van Zundert, A. A comparison of three videolaryngoscopes: the Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth. Analg. 2009, 109, 1560–1565. [Google Scholar] [CrossRef]
- Moore, A.; El-Bahrawy, A.; El-Mouallem, E.; Lattermann, R.; Hatzakorzian, R.; LiPishan, W.; Schricker, T. Videolaryngoscopy or fibreoptic bronchoscopy for awake intubation of bariatric patients with predicted difficult airways - a randomised, controlled trial. Anaesthesia 2017, 72, 538–539. [Google Scholar] [CrossRef]
- Brozek, T.; Bruthans, J.; Porizka, M.; Blaha, J.; Ulrichova, J.; Michalek, P. A randomized comparison of non-channeled GlidescopeTM Titanium versus channeled KingVisionTM videolaryngoscope for orotracheal intubation in obese patients with BMI > 35 kg·m-2. Diagnostics 2020, 10, 1024. [Google Scholar] [CrossRef]
- Gaszynski, T.; Michalek, P.; Ratajczyk, P. A prospective comparative study of laryngeal glottic view using the Vie Scope® versus standard Macintosh laryngoscope in morbidly obese patients. Ther. Clin. Risk Manag. 2023, 19, 405–411. [Google Scholar] [CrossRef]
- Ruetzler, K.; Rivas, E.; Cohen, B.; Mosteller, L.; Martin, A.; Keebler, A.; Maheshwari, K.; Steckner, K.; Wang, M.; Praveen, C.; Khanna, S.; Makarova, N.; Sessler, D.I.; Turan, A. McGrath video laryngoscope versus Macintosh direct laryngoscopy for intubation of morbidly obese patients: A randomized trial. Anesth. Analg. 2020, 131, 586–593. [Google Scholar] [CrossRef]
- Nassar, M.; Zanaty, O.M.; Ibrahim, M. Bonfils fiberscope vs GlideScope for awake intubation in morbidly obese patients with expected difficult airways. J. Clin. Anesth. 2016, 32, 101–105. [Google Scholar] [CrossRef]
- Bathory, I.; Granges, J.C.; Frascarolo, P.; Magnusson, L. Evaluation of the Video Intubation Unit in morbid obese patients. Acta Anaesthesiol. Scand. 2010, 54, 55–58. [Google Scholar] [CrossRef]
- Gaszynski, T.; Pietrzyk, M.; Szewczyk, T.; Gaszynska, E. A comparison of performance of endotracheal intubation using the Levitan FPS optical stylet or Lary-Flex videolaryngoscope in morbidly obese patients. Sci. World J. 2014, 2014, 207591. [Google Scholar] [CrossRef]
- Collins, J.S.; Lemmens, H.J.; Brodsky, J.B.; Brock-Utne, J.G.; Levitan, R.M. Laryngoscopy and morbid obesity: a comparison of the "sniff" and "ramped" positions. Obes. Surg. 2004, 14, 1171–1175. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Jang, E.A.; Hong, M.; Bae, H.B.; Kim, J. Ramped versus sniffing position in the videolaryngoscopy-guided tracheal intubation of morbidly obese patients: a prospective randomized study. Korean J. Anesthesiol. 2023, 76, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Komasawa, N.; Kido, H.; Miyazaki, Y.; Tatsumi, S.; Minami, T. Cricoid pressure impedes tracheal intubation with the Pentax-AWS Airwayscope®: a prospective randomized trial. Br. J. Anaesth. 2016, 116, 413–416. [Google Scholar] [CrossRef]
- Jiang, J.; Ma, D.; Li, B.; Yue, Y.; Xue, F. Video laryngoscopy does not improve the intubation outcomes in emergency and critical patients - a systematic review and meta-analysis of randomized controlled trials. Crit. Care 2017, 21, 288. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, S.; Maitra, S.; Baidya, D.K. A comparison between video laryngoscopy and direct laryngoscopy for endotracheal intubation in the emergency department: A meta-analysis of randomized controlled trials. J. Clin. Anesth. 2018, 47, 21–26. [Google Scholar] [CrossRef]
- Sulser, S.; Ubmann, D.; Schlaepfer, M.; Brueesch, M.; Goliasch, G.; Seifert, B.; Spahn, D.R.; Ruetzler, K. C-MAC videolaryngoscope compared with direct laryngoscopy for rapid sequence intubation in an emergency department: A randomised clinical trial. Eur. J. Anaesthesiol. 2016, 33, 943–948. [Google Scholar] [CrossRef]
- Hossfeld, B.; Frey, K.; Doerges, V.; Lampl, L.; Helm, M. Improvement in glottic visualisation by using the C-MAC PM video laryngoscope as a first-line device for out-of-hospital emergency tracheal intubation: An observational study. Eur. J. Anaesthesiol. 2015, 32, 425–431. [Google Scholar] [CrossRef]
- Macke, C.; Gralla, F.; Winkelmann, M.; Clausen, J.-D.; Haertle, M.; Krettek, C.; Omar, M. Increased first pass success with C-MAC videolaryngoscopy in prehospital endotracheal intubation—A randomized controlled trial. J. Clin. Med. 2020, 9, 2719. [Google Scholar] [CrossRef]
- Hossfeld, B.; Thierbach, S.; Allgoewer, A.; Gaessler, H.; Helm, M. First pass success of tracheal intubation using the C-MAC PM videolaryngoscope as first-line device in prehospital cardiac arrest compared with other emergencies: An observational study. Eur. J. Anaesthesiol. 2021, 38, 806–812. [Google Scholar] [CrossRef]
- Szarpak, L.; Madziala, A.; Czekajlo, M.; Smereka, J.; Kaserer, A.; Dabrowski, M.; Madziala, M.; Yakubtsevich, R.; Ladny, J.R.; Ruetzler, K. Comparison of the UEScope videolaryngoscope with the Macintosh laryngoscope during simulated cardiopulmonary resuscitation: A randomized, cross-over, multi-center manikin study. Medicine 2018, 97, e12085. [Google Scholar] [CrossRef]
- Steffen, R.; Hischier, S.; Roten, F.M.; Huber, M.; Knapp, J. Airway management during ongoing chest compressions-direct vs. video laryngoscopy. A randomised manikin study. PLoS One 2023, 18, e0281186. [Google Scholar] [CrossRef] [PubMed]
- Birenbaum, A.; Hajage, D.; Roche, S.; Ntouba, A.; Eurin, M.; Cuvillon, P.; Rohn, A.; Compere, V.; Benhamou, D.; Biais, M.; Menut, R.; Benachi, S.; Lenfant, F.; Riou, B.; IRIS Investigators Group. Effect of cricoid pressure compared with a sham procedure in the rapid sequence induction of anesthesia: The IRIS randomized clinical trial. JAMA Surg. 2019, 154, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; El-Boghdadly, K.; McGuire, B.; McNarry, A.F.; Patel, A.; Higgs, A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020, 75, 785–799. [Google Scholar] [CrossRef] [PubMed]
- Brewster, D.J.; Chrimes, N.; Do, T.B.; Fraser, K.; Groombridge, C.J.; Higgs, A.; Humar, M.J.; Leeuwenburg, T.J.; McGloughlin, S.; Newman, F.G.; Nickson, C.P.; Rehak, A.; Vokes, D.; Gatward, J.J. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med. J. Aust. 2020, 212, 472–481. [Google Scholar] [CrossRef] [PubMed]
- Foley, L.J.; Urdaneta, F.; Berkow, L.; Aziz, M.F.; Baker, P.A.; Jagannathan, N.; Rosenblatt, W.; Straker, T.M.; Wong, D.T.; Hagberg, C.A. Difficult airway management in adult Coronavirus Disease 2019 patients: Statement by the Society of Airway Management. Anesth. Analg. 2021, 133, 876–890. [Google Scholar] [CrossRef]
- Thiruvenkatarajan, V.; Wong, D.T.; Kothandan, H.; Sekhar, V.; Adhikary, S.D.; Currie, J.; Van Wijk, R.M. Airway management in the operating room and interventional suites in known or suspected COVID-19 adult patients: A practical review. Anesth. Analg. 2020, 131, 677–689. [Google Scholar] [CrossRef]
- Kim, D.S.; Jeong, D.; Park, J.E.; Lee, G.T.; Shin, T.G.; Chang, H.; Kim, T.; Lee, S.U.; Yoon, H.; Cha, W.C.; Sim, Y.J.; Park, S.Y.; Hwang, S.Y. Endotracheal intubation using C-MAC video laryngoscope vs. direct laryngoscope while wearing personal protective equipment. J. Pers. Med. 2022, 12, 1720. [Google Scholar] [CrossRef]
- Gadek, L.; Szarpak, L.; Konge, L.; Dabrowski, M.; Telecka-Gadek, D.; Maslanka, M.; Drela, W.L.; Jachowicz, M.; Iskrzycki, L.; Bialka, S.; Peacock, F.W.; Smereka, J. Direct vs. video-laryngoscopy for intubation by paramedics of simulated COVID-19 patients under cardiopulmonary resuscitation: A randomized crossover trial. J. Clin. Med. 2021, 10, 5740. [Google Scholar] [CrossRef]
- Szarpak, L.; Peacock, F.W.; Rafique, Z.; Ladny, J.R.; Nadolny, K.; Malysz, M.; Dabrowski, M.; Chirico, F.; Smereka, J. Comparison of Vie Scope® and Macintosh laryngoscopes for intubation during resuscitation by paramedics wearing personal protective equipment. Am. J. Emerg. Med. 2022, 53, 122–126. [Google Scholar] [CrossRef]
- Wieczorek, P.; Szarpak, L.; Dabrowska, A.; Pruc, M.; Navolokina, A.; Raczynski, A.; Smereka, J. A comparison of the bébé VieScope™ and direct laryngoscope for use while wearing PPE-AGP: A randomized crossover simulation trial. Children 2022, 9, 1774. [Google Scholar] [CrossRef]
- Kluj, P.; Fedorczak, A.; Fedorczak, M.; Gaszyński, T.; Kułak, C.; Wasilewski, M.; Znyk, M.; Bartczak, M.; Ratajczyk, P. Comparison of three video laryngoscopes and direct laryngoscopy for emergency endotracheal intubation while wearing PPE-AGP: A randomized, crossover, simulation trial. Healthcare 2023, 11, 884. [Google Scholar] [CrossRef]
- Wu, M.Y.; Yiang, G.T.; Ke, J.Y.; Chen, C.S.; Lin, P.C.; Chen, Y.L. Role of Trachway versus conventional modes of intubation in difficult airway management in COVID-19 setups. Emerg. Med. Int. 2021, 2021, 6614523. [Google Scholar] [CrossRef]
- Yang, Y.L.; Huang, C.H.; Luk, H.N.; Tsai, P.B. Adaptation to the plastic barrier sheet to facilitate intubation during the COVID-19 pandemic. Anesth. Analg. 2020, 131, e97–e99. [Google Scholar] [CrossRef]
- Luk, H.N.; Yang, Y.L.; Tsai, P.B. Application of plastic sheet barrier and video intubating stylet to protect tracheal intubators during Coronavirus Disease 2019 pandemic: A Taiwan experience. Cell Transplant. 2021, 30, 963689720987527. [Google Scholar] [CrossRef]
- Stacey, M.R.; Rassam, S.; Sivasankar, R.; Hall, J.E.; Latto, I.P. A comparison of direct laryngoscopy and jaw thrust to aid fibreoptic intubation. Anaesthesia 2005, 60, 445–448. [Google Scholar] [CrossRef]
- Matioc, A.A. Use of the Airtraq® with a fibreoptic bronchoscope in a difficult intubation outside the operating room. Can. J. Anaesth. 2008, 55, 561–562. [Google Scholar] [CrossRef]
- Sharma, D.; Kim, L.J.; Ghodke, B. Successful airway management with combined use of Glidescope® videolaryngoscope and fiberoptic bronchoscope in a patient with Cowden syndrome. Anesthesiology 2010, 113, 253–255. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ríos, M.A.; Nieto Serradilla, L. Combined use of an Airtraq® optical laryngoscope, Airtraq video camera, Airtraq wireless monitor, and a fibreoptic bronchoscope after failed tracheal intubation. Can. J. Anaesth. 2011, 58, 411–412. [Google Scholar] [CrossRef] [PubMed]
- Lenhardt, R.; Burkhart, M.T.; Brock, G.N.; Kanchi-Kandadai, S.; Sharma, R.; Akça, O. Is video laryngoscope-assisted flexible tracheoscope intubation feasible for patients with predicted difficult airway? A prospective, randomized clinical trial. Anesth. Analg. 2014, 118, 1259–1265. [Google Scholar] [CrossRef] [PubMed]
- Van Zundert, A.A.; Pieters, B.M. Combined technique using videolaryngoscopy and Bonfils for a difficult airway intubation. Br. J. Anaesth. 2012, 108, 327–328. [Google Scholar] [CrossRef] [PubMed]
- Pieters, B.M.; Theunissen, M.; van Zundert, A.A. Macintosh blade videolaryngoscopy combined with rigid Bonfils intubation endoscope offers a suitable alternative for patients with difficult airways. Anesth. Analg. 2018, 126, 988–994. [Google Scholar] [CrossRef] [PubMed]
- Levitan, R.M. Design rationale and intended use of a short optical stylet for routine fiberoptic augmentation of emergency laryngoscopy. Am. J. Emerg. Med. 2006, 24, 490–495. [Google Scholar] [CrossRef]
- Ma, X.; Xia, Y.M.; Fan, Q.W. Application of UE visual laryngoscope combined with Seeing Optical Stylet to tracheal intubation in obese patients. J. Shanghai Jiao Tong Univ. 2021, 41, 70–73. [Google Scholar] [CrossRef]
- Chiu, W.C.; Wu, Z.F.; Lai, M.F.; Lai, H.C. Combination use of laryngoscope, jaw thrust, and Trachway for improving difficult tracheal intubation in obese. J. Med. Sci. 2022, 42, 197–198. [Google Scholar]
- Nouruzi-Sedeh, P.; Schumann, M.; Groeben, H. Laryngoscopy via Macintosh blade versus GlideScope: success rate and time for endotracheal intubation in untrained medical personnel. Anesthesiology 2009, 110, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Gu, M.; Lian, M.; Gong, C.; Chen, L.; Li, S. The teaching order of using direct laryngoscopy first may improve the learning outcome of endotracheal incubation: A preliminary, randomized controlled trial. Medicine 2019, 98, e15624. [Google Scholar] [CrossRef]
- Ruetzler, K.; Szarpak, L.; Smereka, J.; Dabrowski, M.; Bialka, S.; Mosteller, L.; Szarpak, A.; Ludwin, K.; Wojewodzka-Zelezniakowicz, M.; Ladny, J.R. Comparison of direct and video laryngoscopes during different airway scenarios performed by experienced paramedics: A randomized cross-over manikin study. Biomed Res Int. 2020, 2020, 5382739. [Google Scholar] [CrossRef]
- Nalubola, S.; Jin, E.; Drugge, E.D.; Weber, G.; Abramowicz, A.E. Video versus direct laryngoscopy in novice intubators: A systematic review and meta-analysis. Cureus 2022, 14, e29578. [Google Scholar] [CrossRef]
- Ayoub, C.M.; Kanazi, G.E.; Al Alami, A.; Rameh, C.; El-Khatib, M.F. Tracheal intubation following training with the GlideScope® compared to direct laryngoscopy. Anaesthesia 2010, 65, 674–678. [Google Scholar] [CrossRef]
- Maharaj, C.H.; Costello, J.F.; Higgins, B.D.; Harte, B.H.; Laffey, J.G. Learning and performance of tracheal intubation by novice personnel: a comparison of the Airtraq® and Macintosh laryngoscope. Anaesthesia 2006, 61, 671–677. [Google Scholar] [CrossRef]
- Moon, Y.J.; Kim, J.; Seo, D.W.; Kim, J.W.; Jung, H.W.; Suk, E.H.; Ha, S.I.; Kim, S.H.; Kim, J.U. Endotracheal intubation by inexperienced trainees using the Clarus Video System: learning curve and orodental trauma perspectives. J. Dent. Anesth. Pain Med. 2015, 15, 207–212. [Google Scholar] [CrossRef]
- Tseng, K.Y.; Chau, S.W.; Su, M.P.; Shih, C.K.; Lu, I.C.; Cheng, K.I. A comparison of Trachway intubating stylet and Airway Scope for tracheal intubation by novice operators: a manikin study. Kaohsiung J. Med. Sci. 2012, 28, 448–451. [Google Scholar] [CrossRef]
- Hung, K.C.; Tan, P.H.; Lin, V.C.; Wang, H.K.; Chen, H.S. A comparison of the Trachway intubating stylet and the Macintosh laryngoscope in tracheal intubation: a manikin study. J. Anesth. 2013, 27, 205–210. [Google Scholar] [CrossRef]
- Ong, J.; Lee, C.L.; Huang, S.J.; Shyr, M.H. Comparison between the Trachway video intubating stylet and Macintosh laryngoscope in four simulated difficult tracheal intubations: A manikin study. Ci Ji Yi Xue Za Zhi 2016, 28, 109–112. [Google Scholar] [CrossRef]
- Pius, J.; Noppens, R.R. Learning curve and performance in simulated difficult airway for the novel C-MAC® video-stylet and C-MAC® Macintosh video laryngoscope: A prospective randomized manikin trial. PLOS One 2020, 15, e0242154. [Google Scholar] [CrossRef]
- Tsay, P.J.; Hsu, S.W.; Peng, H.C.; Wang, C.H.; Lee, S.W.; Lai, H.Y. Trachway intubating stylet for tracheal intubation in an ankylosing spondylitis patient undergoing total hip replacement under general anesthesia. Acta Anaesthesiol. Taiwan 2011, 49, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Hung, K.C. A novel modified method of using Trachway intubating stylet for awake tracheal intubation in patients with anticipated difficult airway. Acta Anaesthesiol. Taiwan 2013, 51, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.Y.; Hu, P.Y.; Lin, Y.C.; Chen, H.Y.; Chiang, F.Y.; Wu, C.W.; Dionigi, G.; Lu, I.C. Trachway video intubating stylet allows for optimization of electromyographic endotracheal tube placement for monitored thyroidectomy. Gland Surg. 2017, 6, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Ding, R.; Li, Z.; He, M.; Liu, C. Comparison of intubation of Shikani optical stylet and Clarus Video Stylet in patients with cervical spine immobilization. J. Practical Med. 2017, 24, 3933–3936. [Google Scholar]
- Xu, M.; Li, X.X.; Guo, X.Y.; Wang, J. Shikani Optical Stylet versus Macintosh laryngoscope for intubation in patients undergoing surgery for cervical spondylosis: A randomized controlled trial. Chinese Med. J. 2017, 130, 297–302. [Google Scholar] [CrossRef]
- Chen, I.W.; Chen, J.Y.; Lan, K.M.; Hung, K.C. The use of Trachway for electromyographic (EMG) tube placement. Gland Surg. 2018, 7, 244–245. [Google Scholar] [CrossRef]
- Yoon, H.K.; Lee, H.C.; Park, J.B.; Oh, H.; Park, H.P. McGrath MAC videolaryngoscope versus Optiscope video stylet for tracheal intubation in patients with manual inline cervical stabilization: A randomized trial. Anesth. Analg. 2020, 130, 870–878. [Google Scholar] [CrossRef]
- Oh, S.H.; Heo, S.K.; Cheon, S.U.; Ryu, S.A. The effects of backward, upward, rightward pressure maneuver for intubation using the OptiscopeTM: a retrospective study. Anesth. Pain Med. 2021, 16, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; Boniface, N.J.; Seller, C.; Hughes, J.; Damen, C.; MacDonald, L.; Kelly, F.E. Universal videolaryngoscopy: a structured approach to conversion to videolaryngoscopy for all intubations in an anaesthetic and intensive care department. Br. J. Anaesth. 2018, 120, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.Y. Education: the last mile to universal videolaryngoscopy. Br. J. Anaesth. 2018, 120, 1431–1432. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; Kelly, F.E.; Boniface, N.; Seller, C. Universal videolaryngoscopy: the importance of choosing the right device. Reply to ‘Cognitive re-engineering after a 15-year experience with routine videolaryngoscopy’ (Br. J. Anaesth. 2019, 122, e57–e58). Br. J. Anaesth. 2019, 122, e59–e60. [Google Scholar] [CrossRef]
- Cook, T.M.; Aziz, M.F. Has the time really come for universal videolaryngoscopy? Br. J. Anaesth. 2022, 129, 474–477. [Google Scholar] [CrossRef]
- Penketh, J.; Kelly, F.E.; Cook, T.M. Use of videolaryngoscopy as the first option for all tracheal intubations: technical benefits and a simplified algorithm for airway management. Br. J. Anaesth. 2023, 130, e425–e426. [Google Scholar] [CrossRef]
- Mirrakhimov, A.E.; Torgeson, E. Use of videolaryngoscopy as the first option for all tracheal intubations: not so fast. Comment on Br. J. Anaesth. 2022, 129, 624–634. Br. J. Anaesth. 2023, 130, e12–e13. [Google Scholar] [CrossRef]
- Pieters, B.M.A.; Maas, E.H.A.; Knape, J.T.A.; van Zundert, A.A.J. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia 2017, 72, 1532–1541. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.W.; Li, Y.Y.; Hung, K.C.; Chang, Y.J.; Chen, J.Y.; Lin, M.C.; Wang, K.F.; Lin, C.M.; Huang, P.W.; Sun, C.K. Comparison of video-stylet and conventional laryngoscope for endotracheal intubation in adults with cervical spine immobilization: A PRISMA-compliant meta-analysis. Medicine 2022, 101, e30032. [Google Scholar] [CrossRef] [PubMed]
- Hung, K.C.; Chang, Y.J.; Chen, I.W.; Lin, C.M.; Liao, S.W.; Chin, J.C.; Chen, J.Y.; Yew, M.; Sun, C.K. Comparison of video-stylet and video-laryngoscope for endotracheal intubation in adults with cervical neck immobilisation: A meta-analysis of randomised controlled trials. Anaesth. Crit. Care Pain Med. 2021, 40, 100965. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
The Shikani technique. (A): demonstration with a SOS (Shikani Seeing Stylet™). (B) jaw-thrust using a non-dominant hand, and (C) applying a video-assisted intubating stylet (Storz C-MAC® video stylet) using a dominant hand in a mannequin model.
Figure 1.
The Shikani technique. (A): demonstration with a SOS (Shikani Seeing Stylet™). (B) jaw-thrust using a non-dominant hand, and (C) applying a video-assisted intubating stylet (Storz C-MAC® video stylet) using a dominant hand in a mannequin model.
Figure 2.
Styletubation technique (video-assisted intubating stylet technique). (A) two-person method. (B) one-person with jaw-thrust method. (C) one-person with laryngoscopic assistance model. The video-assisted intubating stylet is the S-RVL Video Stylet (Sensorendo Medical Technology, Zhuhai, China). The video monitor is separated from the stylet and connected with a cable.
Figure 2.
Styletubation technique (video-assisted intubating stylet technique). (A) two-person method. (B) one-person with jaw-thrust method. (C) one-person with laryngoscopic assistance model. The video-assisted intubating stylet is the S-RVL Video Stylet (Sensorendo Medical Technology, Zhuhai, China). The video monitor is separated from the stylet and connected with a cable.
Figure 3.
Emergent tracheostomy with awake FOB technique for tracheal intubation in a patient with glottis carcinoma. The airway assessment performed after tracheostomyreveals normal by the classic predictors (A): mouth opening size; (B): Mallampati score; (C): sternomental distance; (D): upper lip bite test). A series of pre-operative nasoendoscopic images (from (E–J))show recurrent tumor growth gradually until causing dyspnea and signs of airway obstruction. Emergent tracheostomy was performed after successful establishment of airway by awake nasal FOB.
Figure 3.
Emergent tracheostomy with awake FOB technique for tracheal intubation in a patient with glottis carcinoma. The airway assessment performed after tracheostomyreveals normal by the classic predictors (A): mouth opening size; (B): Mallampati score; (C): sternomental distance; (D): upper lip bite test). A series of pre-operative nasoendoscopic images (from (E–J))show recurrent tumor growth gradually until causing dyspnea and signs of airway obstruction. Emergent tracheostomy was performed after successful establishment of airway by awake nasal FOB.
Figure 4.
Pre-operative endoscopic examination (PEAE, upper panels) and styletubation (lower panels) applied in three examples of predicted difficult airways. (A) a 60-year-old man suffered recurrent left hypopharyngeal squamous cell carcinoma with concurrent chemoradiation therapy (CCRT) one year ago. Emergent tracheostomy was performed due to dyspnea caused by soft laryngeal tissue swelling and airway compression and deviation. (B) a 65-year-old man suffered from right hypophyaryngeal squamous cell carcinoma (cT3N0M0) with CCRT. He was admitted for laryngomicrosurgery (LMS) due to dyspnea, choking, dysphagia, and body weight loss. (C) a 75-year-old man suffered from supraglottic squamous cell carcinoma (cT3N0M0) with CCRT. He underwent tracheostomy due to dyspnea and stridor.
Figure 4.
Pre-operative endoscopic examination (PEAE, upper panels) and styletubation (lower panels) applied in three examples of predicted difficult airways. (A) a 60-year-old man suffered recurrent left hypopharyngeal squamous cell carcinoma with concurrent chemoradiation therapy (CCRT) one year ago. Emergent tracheostomy was performed due to dyspnea caused by soft laryngeal tissue swelling and airway compression and deviation. (B) a 65-year-old man suffered from right hypophyaryngeal squamous cell carcinoma (cT3N0M0) with CCRT. He was admitted for laryngomicrosurgery (LMS) due to dyspnea, choking, dysphagia, and body weight loss. (C) a 75-year-old man suffered from supraglottic squamous cell carcinoma (cT3N0M0) with CCRT. He underwent tracheostomy due to dyspnea and stridor.
Figure 5.
LQS Grade 1. A 63-year-old man with a BMI 26.9 kg/m2 (height 169 cm, weight 77 kg). (A) mouth-opening with interincisor distance 5.5 cm; (B) MMC class II. (C) sternomental distance 18 cm. (D) ULBT class 1. (E) oral entrance view. (F) epiglottis view and partial glottis can been seen. (G) vocal cords view (POGO 100%). (H) tracheal rings view.
Figure 5.
LQS Grade 1. A 63-year-old man with a BMI 26.9 kg/m2 (height 169 cm, weight 77 kg). (A) mouth-opening with interincisor distance 5.5 cm; (B) MMC class II. (C) sternomental distance 18 cm. (D) ULBT class 1. (E) oral entrance view. (F) epiglottis view and partial glottis can been seen. (G) vocal cords view (POGO 100%). (H) tracheal rings view.
Figure 6.
LQS Grade 2.A 65-year-old man with a BMI 23.7 kg/m2 (height 174 cm, weight 72 kg). (A) mouth-opening with interincisor distance 5.0 cm andMMC class IV. (B) sternomental distance 17 cm. (C) ULBT class 3. (D) view of pharyngeal space. (E) epiglottis view with a narrow space against posterior pharyngeal wall. (F) vocal cords view (POGO 90%). (G) tracheal rings view.
Figure 6.
LQS Grade 2.A 65-year-old man with a BMI 23.7 kg/m2 (height 174 cm, weight 72 kg). (A) mouth-opening with interincisor distance 5.0 cm andMMC class IV. (B) sternomental distance 17 cm. (C) ULBT class 3. (D) view of pharyngeal space. (E) epiglottis view with a narrow space against posterior pharyngeal wall. (F) vocal cords view (POGO 90%). (G) tracheal rings view.
Figure 7.
LQS Grade 3.A 70-year-old man with a BMI 29.0 kg/m2 (height 167 cm, weight 81 kg); mouth-opening with interincisor distance 4.5 cm; MMC class IV; sternomental distance 16 cm; ULBT class 2. (A) pharyngeal space view. (B,C) view of epiglottis (star in white color). (D,E) view of esophageal inlet. (F) vocal cords view (POGO 100%). Epiglottis could not be lifted up by the jaw-thrust maneuver and thick and copious secretions were noted.
Figure 7.
LQS Grade 3.A 70-year-old man with a BMI 29.0 kg/m2 (height 167 cm, weight 81 kg); mouth-opening with interincisor distance 4.5 cm; MMC class IV; sternomental distance 16 cm; ULBT class 2. (A) pharyngeal space view. (B,C) view of epiglottis (star in white color). (D,E) view of esophageal inlet. (F) vocal cords view (POGO 100%). Epiglottis could not be lifted up by the jaw-thrust maneuver and thick and copious secretions were noted.
Figure 8.
Time to intubation by styletubation (from lip to trachea). Left panels: oropharyngeal view; middle panels: epiglottis view; right panels: vocal cords view.(A) a 26-year-old woman with a BMI 24.1 kg/m2 (height 155 cm, weight 58 kg); mouth-opening with interincisor distance 4.5 cm; MMC class II; sternomental distance 17 cm; ULBT class 1; LQS grade 1; POGO 100%; intubation time 5 s. (B) a 60-year-old man with a BMI 24.2 kg/m2 (height 170 cm, weight 70 kg); mouth-opening with interincisor distance 4.0 cm; MMC class II; sternomental distance 16 cm; ULBT class 1; LQS grade 2; POGO 100%; intubation time 7 s.(C) a 61-year-old man with a BMI 23.3 kg/m2 (height 167 cm, weight 65 kg); mouth-opening with interincisor distance 5.0 cm; MMC class II; sternomental distance 17 cm; ULBT class 1; LQS grade 2; POGO 100%; intubation time 15 s.
Figure 8.
Time to intubation by styletubation (from lip to trachea). Left panels: oropharyngeal view; middle panels: epiglottis view; right panels: vocal cords view.(A) a 26-year-old woman with a BMI 24.1 kg/m2 (height 155 cm, weight 58 kg); mouth-opening with interincisor distance 4.5 cm; MMC class II; sternomental distance 17 cm; ULBT class 1; LQS grade 1; POGO 100%; intubation time 5 s. (B) a 60-year-old man with a BMI 24.2 kg/m2 (height 170 cm, weight 70 kg); mouth-opening with interincisor distance 4.0 cm; MMC class II; sternomental distance 16 cm; ULBT class 1; LQS grade 2; POGO 100%; intubation time 7 s.(C) a 61-year-old man with a BMI 23.3 kg/m2 (height 167 cm, weight 65 kg); mouth-opening with interincisor distance 5.0 cm; MMC class II; sternomental distance 17 cm; ULBT class 1; LQS grade 2; POGO 100%; intubation time 15 s.
Figure 9.
Styletubation for tracheal intubation in a patient with ankylosing spondylitisand thoracic kyphosis. Pre-operative imaging studies show chest X-ray (
A), kyphosis of thoracic spines (
B), hyperlordosis of cervical spines (
C,
D,
F), view of epiglottis (
E), modified Mallampati classification III with interincisor distance 4 cm (
G); sternomental distance 13 cm (
H,
I). Cervical spine mobility is severely restricted. (same patient as in
Figure 10).
Figure 9.
Styletubation for tracheal intubation in a patient with ankylosing spondylitisand thoracic kyphosis. Pre-operative imaging studies show chest X-ray (
A), kyphosis of thoracic spines (
B), hyperlordosis of cervical spines (
C,
D,
F), view of epiglottis (
E), modified Mallampati classification III with interincisor distance 4 cm (
G); sternomental distance 13 cm (
H,
I). Cervical spine mobility is severely restricted. (same patient as in
Figure 10).
Figure 10.
Styletubation for tracheal intubation in a patient with ankylosing spondylitis, cervical hyperlordosis, and thoracic kyphosis. A 33-year-old man with a BMI 26.5 kg/m
2 (height 160 cm, weight 68 kg), mouth-opening with interincisor distance 4.0 cm; MMC class III; sternomental distance 13 cm; ULBT class 2; LQS grade 2; POGO 100%; intubation time 16 s. (
A–
C) pharyngeal view with collapsed and immobile epiglottis, LQS grade 2 based on the location status of the epiglottis. (
D,
E) visualization of the vocal cords. (
F) view of tracheal ring. (same patient as in
Figure 9).
Figure 10.
Styletubation for tracheal intubation in a patient with ankylosing spondylitis, cervical hyperlordosis, and thoracic kyphosis. A 33-year-old man with a BMI 26.5 kg/m
2 (height 160 cm, weight 68 kg), mouth-opening with interincisor distance 4.0 cm; MMC class III; sternomental distance 13 cm; ULBT class 2; LQS grade 2; POGO 100%; intubation time 16 s. (
A–
C) pharyngeal view with collapsed and immobile epiglottis, LQS grade 2 based on the location status of the epiglottis. (
D,
E) visualization of the vocal cords. (
F) view of tracheal ring. (same patient as in
Figure 9).
Figure 11.
Styletubation for tracheal intubation in an obese patient undergoing bariatric surgery. A 42-year-old woman with a BMI 63.6 kg/m2 (height 161 cm, weight 165 kg), mouth-opening with interincisor distance 5.0 cm; MMC class II; sternomental distance 16 cm; ULBT class 1; LQS grade 2; POGO 100%; intubation time 18 s. (A,B) Pre- and post-intubation. (C,D) LQS grade 2 based on the location status of the epiglottis and partial glottis visualization. (E) visualization of the vocal cords. (F) View of tracheal ring.
Figure 11.
Styletubation for tracheal intubation in an obese patient undergoing bariatric surgery. A 42-year-old woman with a BMI 63.6 kg/m2 (height 161 cm, weight 165 kg), mouth-opening with interincisor distance 5.0 cm; MMC class II; sternomental distance 16 cm; ULBT class 1; LQS grade 2; POGO 100%; intubation time 18 s. (A,B) Pre- and post-intubation. (C,D) LQS grade 2 based on the location status of the epiglottis and partial glottis visualization. (E) visualization of the vocal cords. (F) View of tracheal ring.
Figure 12.
Styletubation for rapid sequence tracheal intubation in a patient undergoing emergent neurosurgery. A 59-year-old man with a BMI 30.1 kg/m2 (height 165 cm, weight 82 kg), mouth-opening with interincisor distance 3.5 cm; MMC class III; sternomental distance 10.5 cm; ULBT class 3; LQS grade 2; POGO 100%; intubation time 9 s. (A,B) oro-pharyngeal views. (C,D) LQS grade 2 based on the location status of the epiglottis and partial glottis visualization. (E) visualization of the vocal cords. (F) View of tracheal ring.
Figure 12.
Styletubation for rapid sequence tracheal intubation in a patient undergoing emergent neurosurgery. A 59-year-old man with a BMI 30.1 kg/m2 (height 165 cm, weight 82 kg), mouth-opening with interincisor distance 3.5 cm; MMC class III; sternomental distance 10.5 cm; ULBT class 3; LQS grade 2; POGO 100%; intubation time 9 s. (A,B) oro-pharyngeal views. (C,D) LQS grade 2 based on the location status of the epiglottis and partial glottis visualization. (E) visualization of the vocal cords. (F) View of tracheal ring.
Figure 13.
Endotracheal intubation with styletubation in a patient with COVID-19. A 83-year-old man with a BMI 29.0 kg/m2 (height 153 cm, weight 68 kg). Pre-intubation airway assessment was not able to perform. LQS grade 2; POGO 100%; intubation time 12 s with first pass success. (A) chest X-ray taken before intubation. (B) chest X-ray taken after intubation. (C,D) pharyngeal views. LQS grade 2 based on the location status of the epiglottis. (E) visualization of the glottis structures. (F) View of tracheal ring.
Figure 13.
Endotracheal intubation with styletubation in a patient with COVID-19. A 83-year-old man with a BMI 29.0 kg/m2 (height 153 cm, weight 68 kg). Pre-intubation airway assessment was not able to perform. LQS grade 2; POGO 100%; intubation time 12 s with first pass success. (A) chest X-ray taken before intubation. (B) chest X-ray taken after intubation. (C,D) pharyngeal views. LQS grade 2 based on the location status of the epiglottis. (E) visualization of the glottis structures. (F) View of tracheal ring.
Figure 14.
Videolaryngoscopy-assisted styletubation. A 67-year-old man with a BMI 30.8 kg/m2 (height 161 cm, weight 80 kg); mouth-opening with interincisor distance 4.5 cm; MMC class III; sternomental distance 13 cm; ULBT class 2; LQS grade 2; POGO 100%; intubation time 7 s. (A) Videolaryngoscopic view (Cormack-Lehane grade 3, shown in the videolaryngoscopic screen). (B,C) LQS grade 2 based on the location status of the epiglottis. (D,E) visualization of the glottis structures. (F) View of tracheal ring.
Figure 14.
Videolaryngoscopy-assisted styletubation. A 67-year-old man with a BMI 30.8 kg/m2 (height 161 cm, weight 80 kg); mouth-opening with interincisor distance 4.5 cm; MMC class III; sternomental distance 13 cm; ULBT class 2; LQS grade 2; POGO 100%; intubation time 7 s. (A) Videolaryngoscopic view (Cormack-Lehane grade 3, shown in the videolaryngoscopic screen). (B,C) LQS grade 2 based on the location status of the epiglottis. (D,E) visualization of the glottis structures. (F) View of tracheal ring.
Figure 15.
A novice trainee’s first-time performance using styletubation. A 23-year-old woman with a BMI 19.8 kg/m2 (height 157 cm, weight 49 kg); mouth-opening with interincisor distance 4.0 cm; MMC class II; sternomental distance 15 cm; ULBT class 1. (A–C) views of the oro-pharyngeal space. (D) view of the pyriform recess. (E) view of the vocal cords(POGO 100%). (F) view of trachea inlet. The time to intubation is 63 s caused by tactless maneuver of the stylet, terrible sense of direction, and the obscured view by the secretions.
Figure 15.
A novice trainee’s first-time performance using styletubation. A 23-year-old woman with a BMI 19.8 kg/m2 (height 157 cm, weight 49 kg); mouth-opening with interincisor distance 4.0 cm; MMC class II; sternomental distance 15 cm; ULBT class 1. (A–C) views of the oro-pharyngeal space. (D) view of the pyriform recess. (E) view of the vocal cords(POGO 100%). (F) view of trachea inlet. The time to intubation is 63 s caused by tactless maneuver of the stylet, terrible sense of direction, and the obscured view by the secretions.
Table 1.
Use coverage of styletubation (from 2016 to 2022) in Haulien Tzu-Chi Medical Center, Hualien, Taiwan.
Table 1.
Use coverage of styletubation (from 2016 to 2022) in Haulien Tzu-Chi Medical Center, Hualien, Taiwan.
| |
2016 |
2017 |
2018 |
2019 |
2020 |
2021 |
2022 |
| Total anesthesia number |
16077 |
17831 |
17998 |
19307 |
19721 |
19244 |
19765 |
| GA number |
15339 |
16893 |
17497 |
18481 |
19009 |
18574 |
19061 |
| LMA-GA number |
5544 |
5134 |
5816 |
5902 |
5863 |
5714 |
4932 |
| ET-GA number |
5953 |
6504 |
6920 |
6966 |
7418 |
6982 |
7602 |
| |
VL |
0 |
0 |
20 |
100 |
635 |
336 |
305 |
| Styletubation |
5953 |
6504 |
6900 |
6866 |
6783 |
6646 |
7297 |
Table 2.
Comparison between videolaryngoscopy and styletubation.
Table 2.
Comparison between videolaryngoscopy and styletubation.
| |
VL |
Styletubation |
| Affordability |
Expensive (7000~10000 USD) |
Moderate (600~5000 USD) |
| Availability |
Globally |
Regionally |
| Accessibility |
Yes |
Yes |
| Maintenance |
Easy |
Easy |
| Learning curve (experienced and novice) |
Fast |
Very fast |
| Team performance |
Excellent |
Excellent |
| Rescue for difficult/failed intubation |
Practical |
Practical |
| Combined use with other tools |
With FOB |
With DL/VL/FOB |
| Use in ER, ICU, prehospital rescue by EMS |
Often |
Gradually increasing |
| View quality on video monitor |
Excellent |
Excellent |
| Required use of a laryngoscope blade |
Yes |
No |
| Required mouth opening |
Yes |
Yes |
| Required lifting force |
Yes |
No |
| Required alignment of airway axes |
Yes |
No |
| Often need external laryngeal manipulation |
Yes |
No |
| Glottic visualization |
Excellent |
Excellent |
| Difficulty inserting ET tube |
Possible |
Rare |
| Required stylet |
Possible |
No |
| Impact of collapsed epiglottis |
Heavily |
Heavily |
| Impact of secretions, blood, vomitus on the lens |
Heavily |
Heavily |
| First-attempt success rate |
High |
Perfect |
| Time to intubate |
Varied |
Fast |
| See-around the corner of the airway structures |
Yes |
Yes |
| Esophageal intubation incidence |
Possible |
Very rare |
| Autonomic stimulation |
Very much |
Mild |
| Airway-related complications |
Quite often |
Very rare |
| Suitable for awake intubation |
Yes |
Yes |
| Operator’s subjective satisfaction |
High |
Extremely high |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).