1. Introduction
Ovarian teratoma is the most common benign germ cell ovarian tumor (10-20%) [1]. Generally, these lesions are classified in three categories based on the constitutive elements: the first category holds tumors that have layers of detritus/cellular debris, the second characteristically presents a nodular or palm-shaped protrusion, and the last is represented by a fat-fluid level. Over the years, several cases of cystic ovarian teratomas that do not fit into the categories described above have been described, along with the presence of numerous intracystic floating balls, predominantly of fatty consistency. Mature cystic ovarian teratoma can be easily diagnosed with the help of ultrasonography, CT or MRI in situations without complications. The main drawbacks that can occur in the evolution of these lesions are represented by: ovarian torsion (the most common), rupture (1-4%), malignant transformation (1-2%), superinfection, auto-immune hemolytic anemia, hyperthyroidism (more frequently seen in ovarian goiter), carcinoid syndrome or others [1]. Following literature research, this is, to our knowledge, the first case of ruptured mature cystic ovarian teratoma with the presence of floating fatty balls.
2. Materials and Methods
This case report describes a ruptured mature cystic ovarian teratoma with the presence of floating fatty balls. For diagnosis and treatment computer tomography (CT) evaluation, magnetic resonance imaging (MRI) and surgery were performed. The CT scan was performed using a Somatom Definition Egde 128 slice scanner (Siemnes, Erlangen, Germany); both pre- and postcontrast scans were done. As for MRI evaluation, it was realized using a 1.5 T MRI scanner (Magnetom Aera, Siemens, Erlangen, Germany); this case also required pre- and post contrast sequences, including, DWI and chemical shift imaging sequences. The surgical treatment included laparatomy with left adnexectomy, peritoneal lavage and lysis of entero-enteric adhesions. A written consent for publication was obtained from the patient.
3. Case Presentation
We present the case of a 61-year-old female patient, who has been postmenopausal for about 10 years and referred to the emergency department after a minor abdominal trauma. The patient experienced diffuse abdominal pain which worsened over time. The initial blood count was unremarkable (
Table 1).
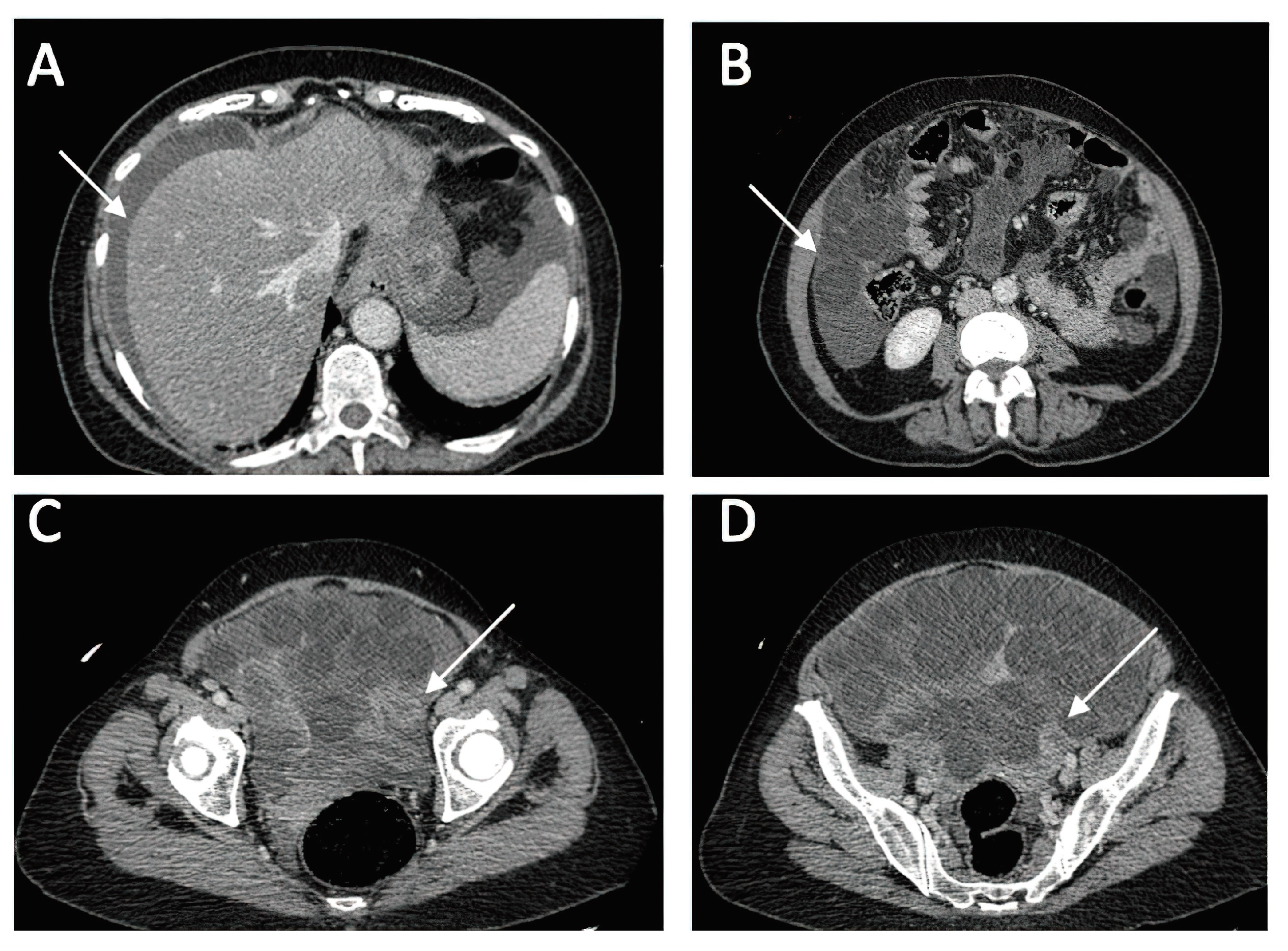
A CT investigation of the abdomen and pelvis was requested and performed. Radiology noted the presence of ascites in moderate amount, together with numerous round nodular lesions of varying sizes (between 1.5-4 cm), with no contrast uptake; the lesions were randomly distributed, with a slight prevalence for the pelvic region. However, a serpiginous lesion with intense contrast uptake was observed within the left ovary (
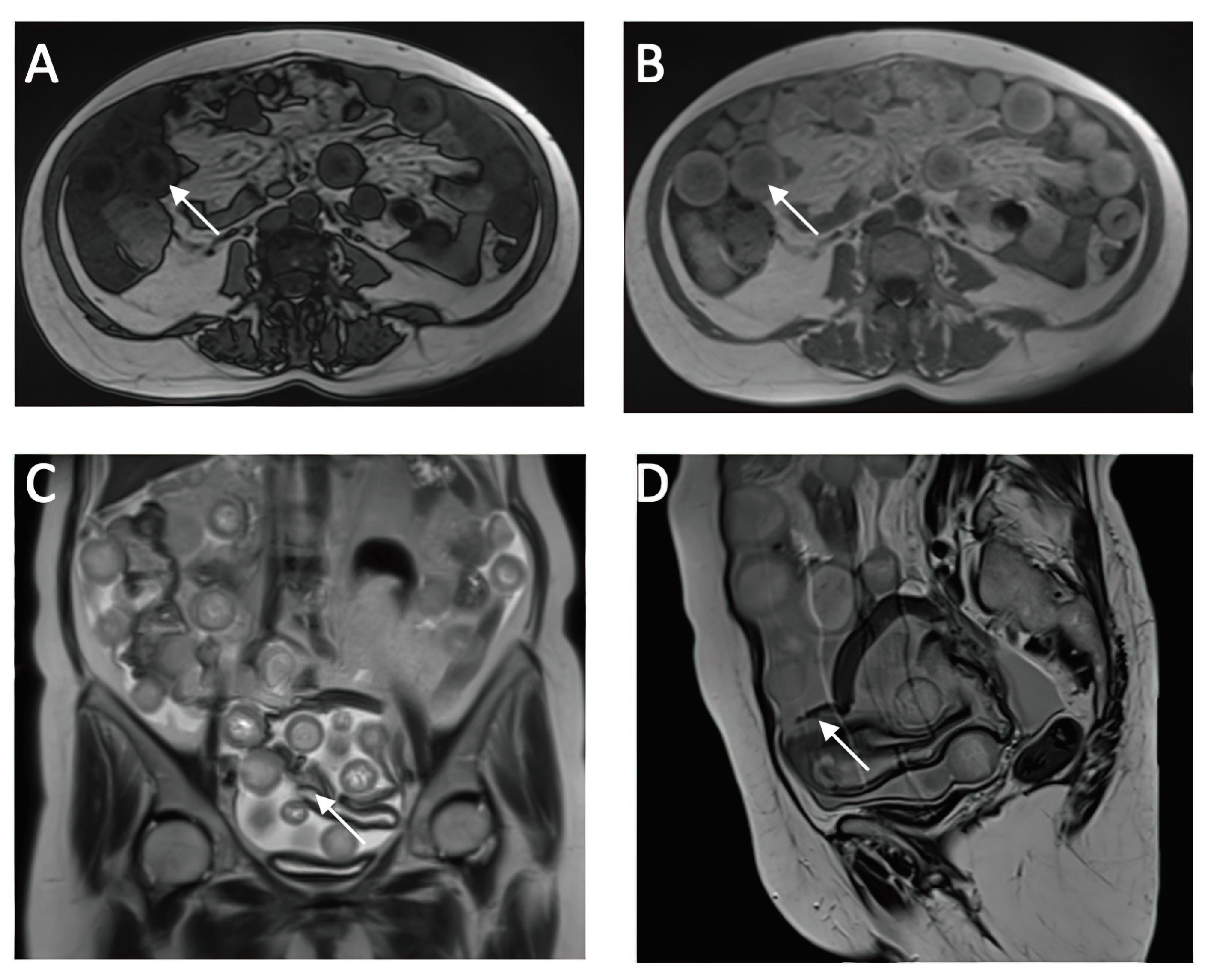
Figure 1), leading the radiologist to falsely raise the suspicion of ovarian carcinoma with peritoneal carcinomatosis. The patient was hospitalized for additional investigations and medical treatment. After several days, an abdominal and pelvic MRI was also performed (
Figure 2). Several ‘floating round bodies’ were observed throughout the whole peritoneum; the ‘floating bodies’ showed signal drop on the out-of-phase sequences suggesting fatty components. When analyzing the pelvic images, a ruptured cyst was observed across the right ovary. The diagnosis of ruptured ovarian teratoma was made and the patient underwent surgery. Left adnexectomy with peritoneal lavage and lysis of entero-enteric adhesions was performed. During the laparotomy, the peritoneal cavity was opened revealing a moderate amount of peritoneal fluid. A sample was then collected for cytologic examination. Macroscopically, the uterus had a normal appearance, with unremarkable right adnexa and left fallopian tube. As for the left ovary, a cystic mass with ruptured wall was observed. The cyst contained multiple well defined round lesions with fatty content, some of which were disseminated throughout the peritoneal cavity. The surgical findings are depicted in
Figure 3.
Eight days after the surgical intervention, the results of the histopathological ex-amination of the left ovary and peritoneal lavage samples were communicated, leading to the definitive diagnosis: mature cystic ovarian teratoma consisting of various tissues, including epidermal tissue with keratotic squamous epithelium, sebaceous and sweat glands, cartilaginous tissue, brain tissue, connective tissue covered with a cylindrical ciliated epithelium, muscle tissue, and adipose tissue. Additionally, there was an associated chronic non-specific granulomatous inflammation with multinucleated giant cells, with no signs of malignant proliferation. The postoperative evolution was favourable - the patient was discharged with a good general condition. Four months after the surgery, the patient returned to the obstetrics-gynecology clinic for evaluation, and no abnormalities were observed.
4. Discussion
Mature cystic ovarian teratoma is the most common benign ovarian neoplasm of young, fertile women. In most cases, they are asymptomatic, and unilateral (85-90%), our patient being discovered with an incidental left adnexal lesion following a minor trauma. The teratoma can associate with pelvic pain when complicated by torsion, or can be detected when it has reached a voluminous size that can be palpated. Histologi-cally, these lesions are composed of at least two of the three layers of germ cells: ecto-derm, mesoderm and endoderm. There is a histopathological difference between the two terms mentioned above, the dermoid cyst showing only ectodermal structures, while the teratoma shows both elements from ectoderm and mesoderm or endoderm. Therefore, in a teratoma we can observe elements such as: fat (in 93% of cases), mature skin (from a developmental point of view), sebaceous glands, hair follicles, sebum bags, blood, bone fragments, teeth, nails, eyes, cartilage or thyroid tissue [1]. In relation to the last element, there is a subtype of ovarian teratoma called struma ovarii which is composed entirely or almost entirely of thyroid tissue [3]. In our case, the his-topathological examination confirmed the following: epidermal tissue with keratotic squamous epithelium, sebaceous and sweat glands, cartilaginous tissue, brain tissue, connective tissue covered with a ciliated cylindrical epithelium, muscle tissue and adi-pose tissue. The mature cystic ovarian teratoma can easily be diagnosed using imaging tech-niques, due to the intra-cystic components which can be detected by ultrasound, CT, or MRI. This benign ovarian neoplasm is divided into three categories based on the com-posing elements: the first type has layers of debris/cellular remnants, the second holds a nodular protrusion or palm-like projection known as Rokitansky nodule, and the third type contains fat-fluid level. However, there is another category that does not fit into the ones previously mentioned, and is characterized by the presence of floating fatty balls inside the cyst, also known as the "floating balls" sign. This sign is consid-ered pathognomonic for benign ovarian cystic teratomas and is quite common, contra-ry to expectations [4]. These intracystic spherical lesions were first described on CT by Muramatsu et al. in 1991 [5] and later in 2000 by Otigbah et al. through ultrasound [6]. Further, we will proceed to describe mature ovarian teratomas with intra-cystic spherical ‘balls’, which are present in our case. There are few reported cases of mature cystic teratomas with multiple floating spherical masses [7]. These have been found in different locations, such as the ovary, retroperitoneum [8], and mediastinum [9], all of them with different compositions based on the mentioned region. According to Ka-wamoto et al., the appearance of multiple floating spheres within a pelvic cystic tumor has not been described in other pelvic lesions, making it a pathognomonic element for mature cystic ovarian teratomas [10]. The presence of the floating balls sign is more common in larger teratomas with a thicker wall, as they require more space to form [4]. It is speculated that the formation of spherical masses occurs through the aggrega-tion of sebum around a nidus, composed of small debris, desquamated material, or fine hair strands. Aggregation is also slightly facilitated by the peristalsis of the small intes-tine, which is in contact with the cyst wall, but it takes a long time for them to form, explaining the slow growth rate of the lesions, at approximately 1.8 mm/year [4, 10]. However, there is a case described by Donnadieu et al. [11]. where a pregnant patient had a follow-up ultrasound at 22 weeks of gestation, which revealed an ovarian cystic mass with spherical lesions inside that continued to increase in size up to 20 cm within a few weeks. This case was considered the first case of mature cystic ovarian teratoma with spherical lesions in pregnant women. On ultrasound examination, mature cystic ovarian teratoma presents as multiple hyperechogenic round structures floating in the anechoic fluid of the cyst. In some cases, it has been shown that this anechoic liquid component is more likely to be pure sebum that becomes liquid at body temperature [7]. Additionally, a study demonstrat-ed that 3D ultrasound has more benefits for the physician, compared to 2D ultrasound. Therefore, lesions appear in 3D ultrasound as spherical, globular structures, in a larger number and some adherent to each other, characteristics similar to those described macroscopically after laparotomy [12]. Due to its ability to distinguish different tissue types by their densities, even in very small amounts, CT imaging has a higher sensitivity for diagnosis compared to ul-trasound but is less recommended due to ionizing radiation risk. This type of ovarian teratoma exhibits distinct imaging characteristics, which include the presence of low-density spherical masses containing a mix of fat, debris, hair strands, and fluid. Calcifications or the dermoid plug formed from the cyst wall can also be observed. In the case of a ruptured cyst, these hypodense masses are randomly distributed in the abdomen and pelvis, predominantly in the pelvic area, surrounded by the leaked intracystic flu-id. In case of a ruptured cyst, the literature emphasizes that the fluid distributes in antidependent pockets, and may lead to chemical peritonitis. This may affect the mesen-tery and thickening of the peritoneum, closely mimicking peritoneal carcinomatosis [1, 13], as initially suspected in our case through the CT examination. Malignant trans-formation can be suggested by the enlargement of the cystic ovarian teratoma >10 cm, soft tissue plugs, and the irregular/crenelated appearance of the cyst’s wall. Although the presented teratoma was approximately 14 cm in the largest diameter, malignancy was excluded after histopathological examination. MRI is the investigation reserved for difficult-to-diagnose cases; it is extremely sensitive to fatty structures, and contrast can identify invasive solid components, mak-ing it necessary for differentiating malignant elements. It is the preferred investigation for women of childbearing age. On T1-weighted sequences, the spherical masses have a hyperintense periphery compared to the intracystic fluid, which has a hypointense center. In contrast, on T2-weighted sequences, the signal is opposed: hypointense at the periphery and hyperintense in the center. The core section consists predominantly of hair strands and soft tissues, while the main component of the globular masses is represented by fat/sebum, which appears suppressed on fat saturation sequences [12]. A characteristic sign of these lesions is the "boba sign" [14], inspired by a Taiwanese drink called bubble tea, which contains multiple tapioca pearls, having an imaging ap-pearance similar to the globular masses in mature cystic ovarian teratoma. These MRI characteristics of the globular masses were observed in our patient as well, noting that the lesions and intracystic fluid were dispersed throughout the abdomen and pelvis, indicating a complicated ruptured teratoma. In case of a suspected teratoma, the most important MRI sequence is represented by “chemical shift” imaging. Due to the fact that all spheres contain a large amount of fat, in the opposed phase images these spheres present a homogeneous signal drop-out, which makes the diagnosis straight-forward. To our knowledge, this is the first reported case of a ruptured cystic teratoma with ‘floating balls’ that has both CT and MRI imaging, making this case report an extremely useful teaching material.
5. Conclusions
This section is not mandatory, but can be added to the manuscript if the discussion is unusually long or complex.
6. Patents
This section is not mandatory, but may be added if there are patents resulting from the work reported in this manuscript.
Author Contributions
Conceptualization, D.C. and A.C.M.; methodology, D.C., D.M. and F.B.; software, I.I.; validation, N.M., C.A.-M.J. and I.-F.B.; formal analysis, M.B.; investigation, S.M.; resources, D.C.; data curation, I.I.; writing—original draft preparation, D.C. and D.M.; writing—review and editing, A.C.M. and F.B.; visualization, I.-F.B.; supervision, S.M.; project administration, D.C.; funding acquisition, A.C.M. All authors have read and agreed to the published version of the manuscript
Funding
This research received no external funding
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper
Data Availability Statement
Data are available upon request to the corresponding author
Conflicts of Interest
The authors declare no conflict of interest
References
- G. F, K. H, and N. M. e. al, “Radiopaedia.org,” [Online]. Available: https://radiopaedia.org/articles/1808. [Accessed 05 May 2023].
- G. F, “Radiopaedia.org,” [Online]. Available: https://radiopaedia.org/cases/18464. [Accessed 05 May 2023].
- K. E. M. A. e. a. Weerakkody Y, “Radiopaedia.org,” [Online]. Available: https://radiopaedia.org/articles/14478. [Accessed 05 May 2023].
- H. Sahin, A. Irmak, Akdogan, D. Ayaz, T. Karadeniz, and M. Sana, “Utility of the ‘floating ball sign’ in diagnosis of ovarian cystic teratoma,” Turk J Obstet Gynecol, vol. 16, no. 1, pp. 18-23, 2019. [CrossRef]
- M. Y, M. N, T. K, N. S, and Y. T, “CT and MR imaging of cystic ovarian teratoma with intracystic fat balls,” J Comput Assist Tomogr, vol. 15, pp. 528-529, 1991.
- O. C, T. MO, L. DG, and S. M, “Mobile globules in benign cystic teratoma of the ovary,” Br J Obstet Gynaecol, vol. 107, pp. 135-138, 2000. [CrossRef]
- J. R. Rao, Z. Shah, V. Patwardhan, V. Hanchate, H. Thakkar, and A. Garg, “Ovarian cyst teratoma,” Journal of Ultrasound in Medicine, vol. 21, pp. 687-691, 2002. [CrossRef]
- F. H, A. S, T. S, K. K, and O. K, “Hepatobiliary and pancreatic imaging: retroperitoneal mature cystic teratoma with a fat ball,” J Gastroenterol Hepatol, vol. 13, pp. 540-549, 1998.
- P. R. Hession andW. Simpson, “Mobile fatty globules in benign cystic teratoma of the mediastinum,” The British Journal of Radiology, vol. 69, pp. 186-188, 1996. [CrossRef]
- K. S, S. K, M. H, and e. al, “Multiple mobile spherules in mature cystic teratoma of the ovary,” AJR Am J Roentgenol, vol. 176, pp. 1455-1457, 2001. [CrossRef]
- A. C. Donnadieu, X. Deffieux, C. L. Ray, M. Mordefroid, R. Frydman, and H. Fernandez, “Unusual fast-growing ovarian cystic teratoma during pregnancy presenting with intracystic fat ‘floating balls’ appearance,” Fertility and Sterility, vol. 86, pp. 1758-1759, 2006. [CrossRef] [PubMed]
- N. Umesaki, A. Nagamatsu, C. Yada, and T. Tanaka, “MR and Ultrasound Imaging of Floating Globules in Mature Ovarian Cystic Teratoma,” vol. 58, pp. 130-132, 2004. [CrossRef] [PubMed]
- K. Rathod, H. Kale, R. Narlawer, J. Hardikar, V. Kulkarni, and J. Joseph, “Unusual ‘floating balls’ appearance of an ovarian cystic teratoma: Sonographic and CT findings,” Journal of Clinical Ultrasound, vol. 29, pp. 41-43, 2001. [CrossRef]
- C. A.Y., S. D.C., O. M.A. and e. al, “Boba sign: a novel sign for floating balls within a mature cystic teratoma,” Abdominal Radiology (NY), vol. 45, pp. 2931-2933, 2020. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).