1. Introduction
Posttraumatic stress disorder (PTSD) is a psychiatric condition characterized by intrusive symptoms, avoidance of stimuli associated with traumatic events, negative alterations in cognition and emotion, and changes in arousal and reactivity following exposure to one or more traumatic incidents [
1]. Individuals with PTSD typically experience involuntary intrusive trauma-related memories such as flashbacks and nightmares, yet struggle with voluntarily recalling specific details of the traumatic experience [
2,
3]. Heightened attention to trauma-related memories is often triggered by stimuli associated with threats, whereas attention to task-related stimuli tends to decrease [
4]. Memory impairments in PTSD manifest as challenges in both preserving and retrieving memories and difficulties in suppressing emotional memories [
2].
Cognitive function profiles of individuals with PTSD vary based on factors such as trauma nature, participant age, and sex. Individuals with PTSD consistently experience reduced attention and working memory [
5,
6]. Notably, among various trauma types, veterans with PTSD consistently display declines in attention, verbal memory, and learning functions, without apparent impairments in visuospatial functions [
5].
Criticism targets the excessively stringent diagnostic criteria for PTSD. Despite the high prevalence of psychological trauma, the incidence of PTSD remains relatively low [
7]. Partial PTSD, alternatively termed subthreshold or subclinical PTSD, refers to cases that partially meet yet do not fully satisfy diagnostic criteria for PTSD. This concept was first introduced in a study on Vietnamese veterans in 1992 and was later applied to community populations in 1997 [
8,
9,
10]. Although a universally agreed-upon definition of partial PTSD is lacking, partial PTSD is as prevalent as PTSD. Individuals diagnosed with partial PTSD exhibit higher rates of comorbid mental disorders [
11].
Despite the clinical significance of partial PTSD, research on the associated cognitive function profiles is notably lacking. Most studies investigating cognitive function in PTSD have focused on participants who meet the structured diagnostic criteria for PTSD [
5]. In patients with PTSD, intricate details of cognitive function profiles are closely associated with the psychopathology of PTSD and have been linked to reduced social and occupational functioning [
12]. Consequently, it is imperative to discern disease-specific cognitive function profiles, even within the context of partial PTSD.
This study aimed to address this gap by examining the results of neurocognitive function tests in individuals who experienced war-related psychological trauma, particularly those with partial PTSD (partial PTSD group), and comparing them with individuals who experienced psychological trauma yet did not meet the criteria for PTSD or partial PTSD (non-PTSD group). Furthermore, a comparative analysis of cognitive function profiles between the two groups was conducted, adjusting for potential confounding variables, such as the psychopathology of PTSD, age, depressive symptoms, education level, and other factors that may influence cognitive function and demonstrate disparities between the groups.
2. Materials and Methods
2.1. Participants
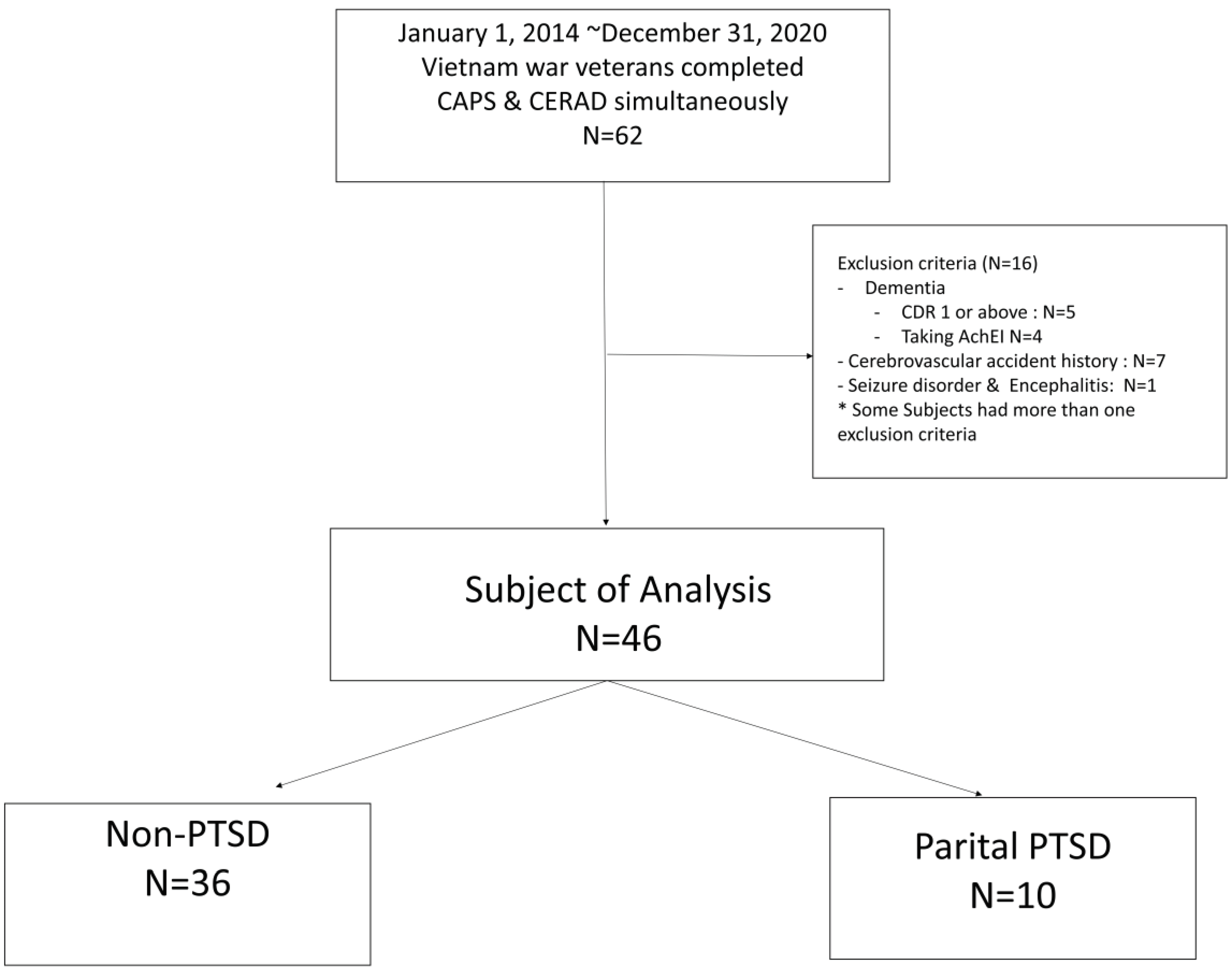
Participants were identified via a retrospective review of medical records from individuals who sought inpatient or outpatient treatment for symptoms associated with psychological trauma at the Veterans Health System Medical Center (VHSMC) between January 1, 2014, and December 31, 2020. Participants were Vietnam War veterans who underwent neurocognitive testing on the same day, which included the administration of the Clinical Administered PTSD Scale (CAPS) [
13] and the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD) [
14].
The inclusion criteria required participants to have experienced psychological trauma attributable to their involvement in the Vietnam War, as indicated in item A of the CAPS. Exclusion criteria included individuals with mental disorders resulting from general medical conditions documented during CAPS and neurocognitive testing, suspected delirium, a Clinical Dementia Rating (CDR) ≥1, and current use of acetylcholinesterase inhibitors and NMDA receptor agonists. Additionally, participants with dementia, clinically significant neurological disorders, and a history or current presence of brain damage (e.g., major vascular cerebral infarction, cerebral hemorrhage, multiple sclerosis, or epilepsy) receiving cognitive enhancement drugs corresponding to agonists were excluded.
Given the considerable time that had elapsed since testing, obtaining informed consent for this study was deemed unfeasible. Consequently, personal information was anonymized. The Institutional Review Board (IRB) waived the need for consent for research involving less than minimal risk This study was approved by the IRB of VHSMC (IRB no. 2020-07-028-001).
2.2. Clinical Evaluation
2.2.1. Clinical Administered PTSD Scale and Definition of Partial Posttraumatic Stress Disorder
The CAPS was employed to determine whether participants met the diagnostic criteria for either PTSD or partial PTSD. Participants self-reported their symptom levels over the past month using the CAPS, a structured clinical assessment tool administered by trained professionals. The CAPS consists of 30 items assessing PTSD, including 17 core symptoms, response validity, overall symptom severity, and social and occupational functioning. Each item is categorized on a scale ranging from ‘not applicable’ (0 points) to ‘most severe case’ (4 points), with 1-point intervals to assess frequency and intensity. The total scores ranged from 0 to 136 [
13]. The Korean version of CAPS, standardized by Kim et al. [
15], demonstrated excellent internal consistency with a Cronbach’s α of .93. Two versions of the CAPS exist, evaluating symptoms based on the lifetime, past month, or past week. In this study, PTSD symptoms were evaluated over the past month.
For a diagnosis of PTSD, a score of ≥1 on the frequency scale (indicating symptoms present to some extent) and ≥2 on the intensity scale (indicating symptoms of moderate severity) using the F1/I2 scoring method defined the presence of PTSD symptoms. As per diagnostic criteria, PTSD was diagnosed if participants exhibited at least one re-experiencing symptom, at least three symptoms of avoidance, and at least two symptoms of hyperarousal, persisting for one month and causing impairment [
15]. Partial PTSD was diagnosed if one or more symptoms from each category (B, C, D) of the DSM-IV PTSD diagnostic criteria were met, with symptoms persisting for at least 1 month (category E) [
9].
The Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease and the Seoul Neuropsychological Screening Battery
The Korean version of the CERAD and the Seoul Neuropsychological Screening Battery (SNSB are standardized clinical and neuropsychological assessment tools for evaluating cognitive function associated with Alzheimer’s dementia. The CERAD was developed and standardized by Lee et al. [
14] and includes the widely used Mini Mental Status Examination in Korean (MMSE-KC[J3]) for screening and assessing cognitive disorders. The MMSE-KC assesses orientation, attention, computational ability, memory registration and recall, language, and visuospatial organization.
The CERAD encompasses additional tests such as language fluency (Word Fluency Test animal/supermarket [J1]), short-version Boston Naming [J2], and visuospatial constructive behavior tests (Construction Praxis [J5]). Memory functions were evaluated using Word List Learning, Delayed Recall, Recognition (Word List Learning [J4], Delayed Recall [J6], Recognition [J7]), and Constructional Praxis Recall tests [J8]. Frontal lobe/executive functions were assessed using the Trail Making Tests A and B and the Korean-Color Word Stroop test: Word Reading/Color Reading Test.
However, the limitations of the CERAD include the absence of visual memory recognition tasks and a restricted number of tests for frontal lobe/executive function. To address these shortcomings, the Seoul Neuropsychological Screening Battery’s 2nd edition [
17] supplements the CERAD with additional tests, including the Number Memorization Test for concentration and attention, the Digit Span Test (forward, backward), the Ray Complex test for visuospatial function, and the Frontal Contrasting Program (Go/No-Go Test) for frontal lobe/executive function. Additionally, language function is assessed via comprehension and speaking tests, whereas the Clock Drawing Test evaluates visuospatial construction ability, frontal lobe/executive function, and semantic memory. Episodic and logical memories were assessed using the Story Recall Test (immediate recall, delayed recall, and recognition) of the Elderly Memory Disorder Scale [
18].
2.3. MMSE-KC
As part of the CERAD-K battery, the MMSE-KC serves as a screening tool for cognitive impairment, with its aggregate score reflecting overall cognitive function. Comprising 19 of 30 questions, the test allocated specific point values to cognitive domains: 5 points for time and place orientation, 5 for attention and calculation ability, and 6 for memory (3 points for registration and 3 for recall). Language-related components were assessed with 2 points for naming and 1 point for repetition. Additionally, the MMSE-KC evaluates command execution (3 points), space-time construction ability via the overlapping pentagon task (1 point), and understanding and judgment (2 points) [
14].
2.4. Subjective Memory Complaints Questionnaire
This questionnaire was designed to assess the subjective severity of memory impairment experienced by the individuals. It comprises 14 questions, with 4 questions dedicated to the subjective measurement of overall memory impairment and 10 questions specifically focused on evaluating the memory challenges experienced in daily life. The use of self-evaluation confers the advantage of uncovering memory issues that cannot be discerned through objective memory tests. This approach yielded crucial insights into subjective memory decline and offered valuable information that complemented objective assessments [
19].
2.5. Beck Depression Inventory
The Beck Depression Inventory (BDI) is a self-report questionnaire used to gauge the severity of depressive symptoms and encompasses 21 questions that address emotional, cognitive, motivational, physiological, and other aspects of depression [
20]. The Korean adaptation of the BDI-II used in this study was translated and validated by Seong et al. [
21].
2.6. Combat Exposure Scale
The Combat Exposure Scale (CES) is one of the most widely used tools for measuring combat-related trauma. It comprises a 7-item self-report questionnaire designed to assess exposure to diverse combat-related situations. Each item is rated on a scale of 1 to 5 points, with weights assigned based on the severity of the experience. The total score ranges from 0 to 41 points. The Korean version of the CES has demonstrated high reliability and validity, particularly among Vietnam War veterans [
22].
2.7. Alcohol Use Disorder Identification Test
The Alcohol Use Disorder Identification Test (AUDIT) is a 10-item questionnaire devised by the World Health Organization, assessing quantitative aspects of drinking, dependence, and levels of harmful drinking [
23]. The Korean version of AUDIT [
23] was employed in this study. Problematic drinking was determined in an optimization study for screening risky drinkers, where an AUDIT total score ≥10 indicated problematic drinking [
24].
2.8. Statistical Analyses
Fisher’s exact test was used for categorical variables and the Mann-Whitney test for continuous variables. A comprehensive comparison was conducted across demographic information, current psychoactive drug use, total CAPS score, BDI and CES scores, presence of problematic drinking, complaints of subjective cognitive decline, and detailed neurocognitive test results for the CERAD and SNSB between the partial PTSD and non-PTSD groups. The threshold for statistical significance was set at p <0.05. In addition, to address potential confounding factors, Quade’s analysis of covariance was applied to each test result within each area of cognitive function. Covariates included age, education level (years), BDI score, and variables that exhibited significant differences between the two groups. To mitigate the issue of multiple testing, Bonferroni correction was implemented, establishing significance at p <0.00125 (0.05/40). All statistical analyses were conducted using the Statistical Package for the Social Sciences version 21.0; IBM Corp., Armonk, NY, USA).
3. Results
3.1. Participants
Participants in this study sought hospitalization or outpatient treatment at the VHSMC for psychological trauma symptoms between January 1, 2014, and December 31, 2020. The inclusion criteria involved participation in the Vietnam War and having undergone neurocognitive testing, including the CAPS and CERAD-K, on the same day. Initially, 62 patients met these criteria; however, after applying the double-exclusion criteria, 46 participants were included in the final analysis. Following the CAPS interview, none of the subjects met the criteria for PTSD; 10 individuals were classified as having partial PTSD, and 36 were categorized as non-PTSD (
Figure 1).
Table 1 provides an overview of the demographic information, medication status, psychiatric symptoms, and CES characteristics of the partial PTSD and non-PTSD groups. The study exclusively included male participants, and no statistically significant differences were observed between the two groups regarding average age, education level, employment, marital status, combat exposure, or subjective cognitive decline (
Table 1). The proportion of individuals taking psychoactive drugs did not significantly differ between the two groups (
Supplementary Table S1).
The analysis revealed a significantly higher total CAPS score in the partial PTSD group (39.30 ± 11.14) than in the non-PTSD group (14.42 ± 9.66). BDI scores were also elevated in the partial PTSD group (non-PTSD: 27.23 ± 15.26; partial PTSD: 38.67 ± 9.19; p = 0.038). However, no statistically significant difference was observed in the rate of reported problematic drinking based on AUDIT scores between the two groups (non-PTSD: N = 8 [22.20%]; partial PTSD: N = 1 [10.00%]; p = 0.659). Similarly, the Subjective Memory Complaints Questionnaire (SMCQ) did not reveal a significant disparity in the degree of subjective cognitive decline between the non-PTSD (8.86 ± 3.56) and partial PTSD (9.40 ± 3.75) groups (p = 0.555).
3.2. Neurocognitive Function Test Results
The average completion time for the Trail Making Test B in the partial PTSD group was significantly higher than that in the non-PTSD group (non-PTSD: 212.78 ± 64.03 s; partial PTSD: 269.00 ± 62.06 s; p = 0.024) (
Table 2). Moreover, attention and calculation scores within the MMSE-KC details were significantly lower in the partial PTSD group (non-PTSD: 4.25 ± 1.32; partial PTSD: 2.90±1.91; p=0.035) than those in the non-PTSD group (
Table 3).
Detailed comparisons of neurocognitive test results, including Word Fluency Test (animal, supermarket), Short version Boston Naming Test, Word list learning, Construction Praxis, Word List Delayed recall, Word List Recognition, Constructional Praxis Recall, SNSB’s Digit Span Test (forward & backward), Rey Complex Figure Test (copy, immediate recall, delayed recall, and recognition), Go/No-Go Test, Verbal Comprehension, Verbal Repetition, Clock Drawing Test, and Story Recall Test (immediate recall, delayed recall, and recognition), did not reveal significant differences between the partial PTSD and non-PTSD groups (
Table 2). Quade’s covariance analysis, controlling for age, education level, and BDI score, also indicated no significant differences in any of the neurocognitive test items between the two groups (
Table 2).
Despite significant differences initially existed in the attention and calculation items of the MMSE-KC between the two groups before adjusting for potential confounding factors, further analysis using Quade’s covariance analysis with covariate control showed no significant differences in detailed MMSE-KC items between the partial PTSD and non-PTSD groups (
Table 2).
4. Discussion
This study aimed to discern distinctive neurocognitive functional differences associated with partial PTSD across various domains. Notably, the Trail Making Test B revealed a significant disparity in performance, indicating compromised frontal lobe and executive functions in the partial PTSD group compared with the non-PTSD group. Although the attention and calculation items of the MMSE-KC exhibited diminished performance in the partial PTSD group, subsequent adjustments for age, education level, depressive symptom severity, and Bonferroni correction for multiple testing problems demonstrated no significant differences between the two groups.
The Trail Making Test is a neuropsychological assessment tool for evaluating visual attention and task-switching abilities, specifically targeting the frontal lobe and executive functions. Trail Making Test A assesses attention, sequencing, spatiotemporal navigation, and psychomotor speed, whereas Trail Making Test B evaluates cognitive flexibility and the parameters examined in Test A [
25]. The significance of cognitive flexibility has been highlighted as a predictive factor for the severity of PTSD symptoms immediately following trauma exposure in individuals with a history of psychological trauma [
26]. Notably, our study, conducted with participants whose average age was 71.03 ± 3.29 years in the non-PTSD group and 72.20 ± 2.04 years in the partial PTSD group, more than four decades post-trauma exposure due to war participation, revealed a sustained reduction in cognitive flexibility, even in cases of chronic or delayed-onset partial PTSD.
Qureshi et al. [
6] showed that the impact of PTSD impacts attention deficits, more than twice as significantly as that of non-significant results. Studies focusing on war veterans, particularly military personnel, have shown significant results [
2]. Consistent with these findings, our study revealed a decline in attentional concentration among veterans with partial PTSD, as evidenced by the attention/calculation items of the MMSE-KC.
A meta-analysis examining major depressive disorder in individuals with PTSD demonstrated a prevalence of 52% (95% confidence interval 48–56%), exceeding the prevalence in the general population [
27]. A study on the natural history of psychological trauma in personnel mobilized for the 9/11 World Trade Center rescue operation revealed a notable increase in the diagnosis of major depressive disorder and severity of depressive symptoms among those with partial PTSD compared to those in a healthy control group [
28]. Our study aligned with these findings, indicating a significantly higher degree of depressive symptoms as measured by the BDI score in individuals with partial PTSD.
Following adjustments for depressive symptoms, age, and education level when comparing cognitive function between the two groups, this study revealed no significant differences in the detailed items of the cognitive function test. Notably, in a meta-analysis exploring the correlation between the severity of depressive symptoms and cognitive function, episodic memory, executive function, and processing speed correlate with the severity of depressive symptoms [
29]. Consistent with these findings, our study demonstrated a significant difference in depressive symptoms between the partial PTSD and non-PTSD groups, suggesting that an elevated degree of depressive symptoms in patients with partial PTSD may influence cognitive function.
The total CAPS score in the partial PTSD group, averaging 39.30 ± 11.14, was notably higher than that in the non-PTSD group, indicating a moderate level of PTSD symptoms comparable to full PTSD [
30]. Despite the high CAPS total score indicating PTSD symptoms, the partial PTSD group did not meet the DSM-IV criteria for a PTSD diagnosis. Most studies on cognitive function profiles in PTSD have focused on groups in which a PTSD diagnosis can be established via structured interviews, including CAPS [
2,
6]. Consequently, changes in cognitive function tend to be more evident when a diagnosis of PTSD is possible, whereas, in cases of partial PTSD, these changes may be less pronounced than those observed in full PTSD.
Owing to the relatively small sample size, this study employed a non-parametric test, resulting in lower test power compared to performing a parametric test and limitations in result interpretation. As a retrospective cross-sectional study, establishing a causal relationship between cognitive function and partial PTSD was challenging. Limiting inclusion to male veterans who reported combat-related psychological trauma restricted the generalizability of our findings to women and individuals with other forms of psychological trauma. Furthermore, the assessment of symptoms and cognitive function at more than 40 years post-trauma may not accurately reflect changes during the acute period immediately after trauma. This study lacked information on the psychological trauma experienced by individuals not involved in the war. Moreover, the CAPS utilized in this study was designed to screen and diagnose PTSD according to the DSM-IV criteria. Consequently, extrapolating the results of this study to the DSM-5 PTSD diagnosis and symptom evaluation has limitations. These considerations highlight the need for caution when interpreting and applying the findings of this study.
Despite these limitations, this study represents a pioneering effort to reveal the cognitive function profile associated with partial PTSD. A distinctive strength lies in the study’s focus on participants who experienced the same type of psychological trauma within a similar timeframe. This design choice is particularly significant, given that existing studies on cognitive function in PTSD have revealed varying patterns of cognitive decline depending on the type of psychological trauma [
2,
6]. Consequently, the homogeneity of trauma type and timing in this study enhanced the robustness of the findings.
This study contributes to the literature by addressing this gap. Although most studies on cognitive function in PTSD primarily focus on acute symptoms, few explore the impact of chronic or delayed onset of symptoms, and fewer extend the evaluation to more than 40 years post-psychological trauma [
6]. Therefore, this study offers valuable insights into the cognitive functions of individuals with chronic or delayed-onset symptoms long after a traumatic event.
5. Conclusions
In conclusion, this study aimed to examine the cognitive changes in individuals with partial PTSD. The findings indicated a decline in frontal lobe/executive function, mental flexibility, and attention and concentration in the partial PTSD group. However, after adjusting for depressive symptoms, education level, and age, the changes observed in the cognitive areas became non-specific, with no significant differences noted when compared with the non-PTSD group. This suggested that the alterations in cognitive function observed in patients with partial PTSD may be influenced by the presence of coexisting depressive symptoms. Future research should comprehensively explore the cognitive function profile in partial PTSD. Elucidating the relationship between trauma symptoms and cognitive function could be achieved via a large-scale prospective cohort study, thereby addressing the limitations of the small sample size and retrospective cross-sectional design of this study.
Supplementary Materials
Supplementary Table S1. Concomitant psychotropic medication.
Author Contributions
Conceptualization: Seung-Hoon Lee. Investigation: Jihye Song, Jinhee Choi, Hyung Seok So, and Hayun Choi. Methodology: Seung-Hoon Lee and Jihye Song. Project administration: Seung-Hoon Lee. Supervision: Seung-Hoon Lee. Writing—original draft: Jihye Song. Writing—review & editing: Jihye Song and Jinhee Choi, Hyung Seok So, Hayun Choi, and Seung-Hoon Lee.
Funding
This study was supported by a VHS Medical Center Research Grant from the Republic of Korea (no. VHSMC20045).
Institutional Review Board Statement
This study was approved by the IRB of VHSMC (IRB no. 2020-07-028-001).
Informed Consent Statement
Given the considerable time that had elapsed since testing, obtaining informed consent for this study was deemed unfeasible. Consequently, personal information was anonymized. The Institutional Review Board (IRB) waived the need for consent for research involving less than minimal risk.
Data Availability Statement
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Acknowledgments
This manuscript was originally written in Korean and published in the Journal of Korean Neuropsychiatric Association in 2023 May;62(2):78-85. The authors translated the manuscript into English with permission from the Journal of the Korean Neuropsychiatric Association and resubmitted it to Brain Sciences.
Conflicts of Interest
The authors claims no conflicts of interest.
References
- American Psychiatric Association. D, Association AP. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2013; p. DSM-5. [Google Scholar]
- Han, Y.-R.Y. Han, Y.-R.Y.Un J.-A.; Yun, J.; Choi, K. Posttraumatic stress disorder and cognitive Fucntioning: A literature review. J Korean Neuropsychiatr Assoc 2020, 59, 285–292. [CrossRef]
- Brewin, C.R.; Gregory, J.D.; Lipton, M.; Burgess, N. Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychol Rev 2010, 117, 210–232. [Google Scholar] [CrossRef] [PubMed]
- Pineles, S.L.; Shipherd, J.C.; Mostoufi, S.M.; Abramovitz, S.M.; Yovel, I. Attentional biases in PTSD: More evidence for interference. Behav Res Ther 2009, 47, 1050–1057. [Google Scholar] [CrossRef] [PubMed]
- Quinones, M.M.; Gallegos, A.M.; Lin, F.V.; Heffner, K. Dysregulation of inflammation, neurobiology, and cognitive function in PTSD: An integrative review. Cogn Affect Behav Neurosci 2020, 20, 455–480. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, S.U.; Long, M.E.; Bradshaw, M.R.; Pyne, J.M.; Magruder, K.M.; Kimbrell, T.; Hudson, T.J.; Jawaid, A.; Schulz, P.E.; Kunik, M.E. Does PTSD impair cognition beyond the effect of trauma? J Neuropsychiatry Clin Neurosci 2011, 23, 16–28. [Google Scholar] [CrossRef]
- Jeon, H.J.; Suh, T.; Lee, H.J.; Hahm, B.J.; Lee, J.Y.; Cho, S.J.; Lee, Y.R.; Chang, S.M.; Cho, M.J. Partial versus full PTSD in the Korean community: Prevalence, duration, correlates, comorbidity, and dysfunctions. Depress Anxiety 2007, 24, 577–585. [Google Scholar] [CrossRef]
- Mylle, J.; Maes, M. Partial posttraumatic stress disorder revisited. J Affect Disord 2004, 78, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.B.; Walker, J.R.; Hazen, A.L.; Forde, D.R. Full and partial posttraumatic stress disorder: Findings from a community survey. Am J Psychiatry 1997, 154, 1114–1119. [Google Scholar] [CrossRef]
- Weiss, D.S.; Marmar, C.R.; Schlenger, W.E.; Fairbank, J.A.; Kathleen Jordan, B.; Hough, R.L.; Kulka, R.A. The prevalence of lifetime and partial post-traumatic stress disorder in Vietnam theater veterans. J Trauma Stress 1992, 5, 365–376. [Google Scholar] [CrossRef]
- McLaughlin, K.A.; Koenen, K.C.; Friedman, M.J.; Ruscio, A.M.; Karam, E.G.; Shahly, V.; Stein, D.J.; Hill, E.D.; Petukhova, M.; Alonso, J.; et al. Subthreshold posttraumatic stress disorder in the World Health Organization world mental health surveys. Biol Psychiatry 2015, 77, 375–384. [Google Scholar] [CrossRef]
- Geuze, E.; Vermetten, E.; de Kloet, C.S.; Hijman, R.; Westenberg, H.G.J.D. Neuropsychological performance is related to current social and occupational functioning in veterans with posttraumatic stress disorder. Depress Anxiety 2009, 26, 7–15. [Google Scholar] [CrossRef]
- Blake, D.; Weathers, F.; Nagy, L.; Kaloupek, D.; Klauminzer, G.; Charney, D.; Keane, T. Clinician-Administered PTSD Scale (CAPS); Boston (MA), 1990; p. 7. [Google Scholar]
- Lee, J.H.; Lee, K.U.; Lee, D.Y.; Kim, K.W.; Jhoo, J.H.; Kim, J.H.; Lee, K.H.; Kim, S.Y.; Han, S.H.; Woo, J.I. Development of the Korean Version of the Consortium to Establish a Registry for Alzheimer’s disease Assessment Packet (CERAD-K): clinical and neuropsychological assessment batteries. J Gerontol B Psychol Sci Soc Sci 2002, 57, P47–P53. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Kim, T.Y.; Choi, J.H.; So, H.S.; Chung, M.Y.; Kim, D.S.; Bang, Y.J.; Chung, H.G. The application of the clinician administered posttraumatic stress disorder scale to identify combat related posttraumatic stress disorder. Anxiety Mood 2012, 8, 113–119. [Google Scholar]
- Morris, J.C.; Mohs, R.C.; Rogers, H. Consortium To Establish a Registry for Alzheimer’s Disease (CERAD) clinical and neuropsychological. Psychopharmacol Bull 1989, 24, 641–652. [Google Scholar]
- Ryu, H.J.; Yang, D.W. The Seoul Neuropsychological Screening Battery (SNSB) for comprehensive neuropsychological assessment. Dement Neurocogn Disord 2023, 22, 1–15. [Google Scholar] [CrossRef]
- Baek, M.J.; Kim, H.J.; Kim, S. The usefulness of the story recall test in patients with mild cognitive impairment and Alzheimer’s disease. Aging Neuropsychol Cogn 2011, 17, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Youn, J.C.; Kim, K.W.; Lee, D.Y.; Jhoo, J.H.; Lee, S.B.; Park, J.H.; Choi, E.A.; Choe, J.Y.; Jeong, J.W.; Choo, I.H.; et al. Development of the subjective memory complaints questionnaire. Dem Geriatr Cogn Disord 2009, 27, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Brown, G. Beck Depression Inventory—II. 1996, 78, 490–498. [Google Scholar]
- Sung, H.M.; Kim, J.B.; Park, Y.N.; Bai, D.S.; Lee, S.H.; Ahn, H.N. A study on the reliability and the validity of Korean version of the beck depression inventory—II (BDI–II). J Korean Soc Biol Ther Psychiatry 2008, 14, 201–212. [Google Scholar]
- Kim, D.S.; Chung, H.G.; Choi, J.H.; So, H.S.; Kim, H.J.; Go, C.M.; Kim, T.Y.; Chung, M.Y. Reliability and validity of the Korean version of the Combat Exposure Scale. Anxiety Mood 2012, 8, 106–112. [Google Scholar]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Joe, K.H.; Chai, S.H.; Park, A.; Lee, H.K.; Shin, I.H.; Min, S.H. Optimum cut-off score for screening of hazardous drinking using the Korean version of alcohol use disorder identification test (AUDIT-K). J. Korean Acad. Addict. Psychiatry 2009, 13, 34–40. [Google Scholar]
- Arnett, J.A.; Labovitz, S.S. Effect of physical layout in performance of the Trail Making Test. Psychol Assess 1995, 7, 220–221. [Google Scholar] [CrossRef]
- Ben-Zion, Z.; Fine, N.B.; Keynan, N.J.; Admon, R.; Green, N.; Halevi, M.; Fonzo, G.A.; Achituv, M.; Merin, O.; Sharon, H.; et al. Cognitive flexibility predicts PTSD symptoms: Observational and interventional studies. Front Psychiatry 2018, 9, 477. [Google Scholar] [CrossRef]
- Rytwinski, N.K.; Scur, M.D.; Feeny, N.C.; Youngstrom, E.A. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta-analysis. J Trauma Stress 2013, 26, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Cukor, J.; Wyka, K.; Jayasinghe, N.; Difede, J. The nature and course of subthreshold PTSD. J Anxiety Disord 2010, 24, 918–923. [Google Scholar] [CrossRef] [PubMed]
- McDermott, L.M.; Ebmeier, K.P. A meta-analysis of depression severity and cognitive function. J Affect Disord 2009, 119, 1–8. [Google Scholar] [CrossRef]
- Weathers, F.; Blake, D.; Krinsley, K.; Haddad, W.; Ruscio, A.; Keane, T.; Huska, J.A. Reliability and validity of the Clinician-Administered PTSD Scale. Auburn: Auburn University. 1999. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).