Based on “Plantar plate disease as a part of forefoot overload syndrome: the role of MRI in detecting associated injuries”, by C. Ottonello, V. Tempesta, A. Giardino, P. Giuliani, F. Martinelli, which appeared in European Congress of Radiology, Wien, 2017, Poster Number C-3092.
1. Introduction
A plantar plate (PP), also called a plantar ligament, is a fibrocartilaginous structure found in the metatarsophalangeal (MP) joint.
PP has its proximal insertion in the metatarsal head and its distal insertion in the base of the proximal phalanx [
1], and it blends with the transverse metatarsal ligament at the MP joint, the dominant tributary of proximal plantar plate perfusion arises from the metatarsal pedicle [
2].
The plantar plates of the metatarsophalangeal joints and the intervening deep, transverse metatarsal ligaments form a continuous band of strong ligamentous tissue across the forefoot, and on the transverse section, each plantar plate is seen to be anchored to its metatarsal head by the collateral ligaments [
3].
Moreover, it is important to note that the plantar plate has attachments to other structures. The distal plantar fascial aponeurosis attaches to the proximal aspect of the plantar plates, while the deep, transverse intermetatarsal ligament connects the plantar plates of adjacent metatarsophalangeal joints along the plantar aspect of the metatarsals. Additionally, a shallow central groove on the plantar aspect of the plantar plates provides accommodation for the flexor tendons [
4,
5,
6].
PP supports the weight of the body and restricts dorsiflexion. The primary role of the plantar plate is to provide stability to the metatarsophalangeal joints II-III-IV. This is achieved through the multiple attachments and composition of the plantar plate, which consists of fibrocartilaginous tissue. Along with stability, the plantar plate also acts as a cushioning mechanism, dampening compression forces experienced during weight-bearing activities at the metatarsophalangeal joints. Furthermore, the plantar plate contributes to the resistance against tensile forces generated during the windlass effect. This occurs through the proximal attachment of the plantar fascia and subsequent dorsiflexion of the metatarsophalangeal joints. [
7,
8,
9,
10].
As reported by the study of Park J.V. et all [
2], on sixteen lower limb samples of freshly frozen human adult cadaver, different is the length of plantar plate pedicle. The plantar plate pedicle (PPD) in the metatarsophalangeal (MTP) joints was measured for its average length and width in this study. The average length and width of the PPD for all MTP joints were found to be 2.01 mm (range, 1.35–3.27 mm) and 2.08 mm (range, 0.92–3.7 mm), respectively. Specifically, in the second metatarsal, the average length and width of the PPD were measured to be 2.08 mm (range, 1.46–2.71 mm) and 2.27 mm (range, 1.53–3.38 mm), respectively. In the third metatarsal, the average length and width were 2.05 mm (range, 1.35–2.94 mm) and 2.16 mm (range, 0.92–3.7 mm), respectively. Lastly, in the fourth metatarsal, the average length and width were 1.90 mm (range, 1.42–3.27 mm) and 1.86 mm (range, 1.21–2.59 mm), respectively.
Pathologies related to the PPD, such as metatarsalgia, plantar swelling, hammertoe deformity, and subluxation of the lesser toes (particularly the second to third), can cause significant discomfort and functional impairments. Inadequate treatment of PPD pathologies can lead to long-term disability, deformities, and dysfunction. While a clinical examination is typically the first step in evaluating PPD disorders, an accurate diagnosis requires further assessment through magnetic resonance imaging (MRI). MRI allows for the evaluation of PP integrity and the assessment of potential metatarsophalangeal (MTP) joint instability, such as dorsal subluxation of the proximal phalanx, even in the absence of apparent physical trauma [
11,
12,
13,
14,
15].
In the case of a plantar plate lesion, significant improvements in symptoms are achieved after surgical treatment.
Jeffrey R. Baker et all [
16] have made a systematic Review and Meta-Analysis about plantar plate repair, a total of 12 studies with 537 plantar plate tears were included in the analysis. The collective analysis revealed a significant reduction in Visual Analog Scale (VAS) pain scores postoperatively, with a pooled mean change of -5.24 (95% CI, -6.09 to -4.39). These findings were consistent across all studies that reported VAS pain. Notably, the dorsal approach showed promising outcomes, displaying a improvement in both VAS pain scores and American Orthopaedic Foot and Ankle Society (AOFAS) scores, with relatively narrow 95% confidence intervals. The summary estimates generated for pain and function at the one-year follow-up in patients undergoing direct dorsal repair further support the predictability and effectiveness of this approach.
2. Material and Methods
2.1. Selection of Patients:
Patients were referred to our centre (Fisiocard Medical Centre, Rome, Italy) following specialist orthopaedic evaluation and standard radiographic examination of the foot. The clinical suspicion was a plantar plate lesion. The radiographic examination of the feet was always performed in our study in comparison with the dorso-plantar, latero-lateral projections and completed with the oblique projections, under load.
25 patients were recruited into our study over a two-year period, 15 positive for metatarsal pain and 10 controls. Of the 15 symptomatic patients, in 7, there was prevalent symptomatology at the II metatarsophalangeal, in 4 at the III metatarsophalangeal and in the remaining 4 cases in 2, there was prevalent sintomatology at I, and in 2 patients at the IV metatarsophalangeal.
The average age of symptomatic patients is 58.7 years, and the average age of asymptomatic patients is 59.5 years (
Table 1). The median age is about 60 years for both symptomatic and asymptomatic patients. Patients older than 80 years or younger than 35 years are not included in the sample. All patients have never undergone foot/ankle surgery, neither contraindications to performing MRI examinations.
2.2. MRI Protocol and Stress Test:
All patients underwent forefoot MRI (Atroscan C, Esaote, Genoa, Italy), operating at 0.2 T.
This low magnetic field machine is ideal for patient comfort, also having dedicated coil for ankle/foot study also allows some patient comfort, being ideal for claustrophobic patients.
All patients first performed a standard MRI examination (coronal T1 and T2-WI with fat suppression, axial and sagittal T2 WI); the examination was completed by a stress test (hyperextension toes).
“Stress test” is an easy task to perform and even affordable in terms of time-consuming (requiring only one additional T2-weighted MRI sagittal sequence FSE TR/TE 3200/90 ms) for both patients and operators.
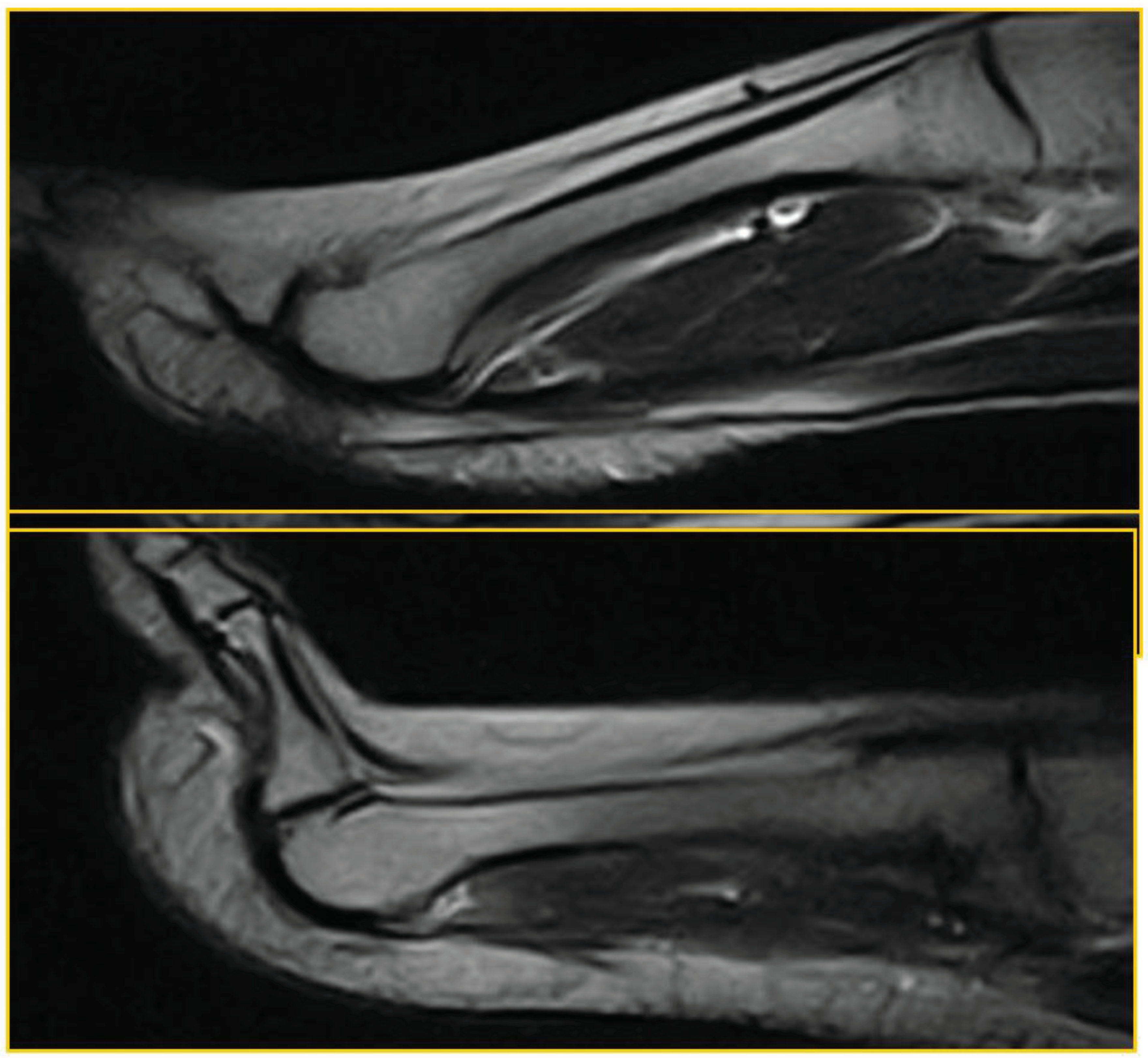
Figure 1.
standard position with joint hyperextension , “stress test”.
Figure 1.
standard position with joint hyperextension , “stress test”.
In this figure, first on the left is the standard execution of the examination, with the foot in a neutral position, then the stress test is shown, in which a forced hyperextension of the toes is achieved, placing the plantar plate itself in traction.
A 45-degree dorsiflexion stress test was then performed for approximately 2.30 minutes, the time required for completion of the sequence. No further diagnostic investigations were necessary; no patients underwent arthrography or arthro-MRI.
The examination also included an assessment of adjacent flexor tendons. Prior to treatment (surgery), all patients experiencing symptoms underwent evaluation. Consequently, the imaging characteristics accurately represented the lesions in their natural state.
The standard plantar plate appears on MRI as homogeneously hypointense due to the fibrous main component; the flexor tendon runs just inferior to the plate from which it is not always easily dissociable, which is why the MRI evaluation in suspected plantar plate lesion must be performed by a radiologist with significant experience in the field of musculoskeletal.
The examinations were performed by two operators with proven experience in the field of musculoskeletal radiology in a double-blind mode; no cases of intra-operator discordance were found. The Fisher’s Exact Test is perform for the evaluation of statistically significant results.
3. Results
We analyse the results of both symptomatic and asymptomatic patients separately.
Among symptomatic patients, 11 out of 15 individuals showed plantar plate tear or dysfunction in both the standard position and stress test. Additionally, 2 out of 15 patients exhibited plantar plate tear only on the stress test, while it was not visible in the standard position. On the other hand, 2 out of 12 patients did not display any plantar plate tear or dysfunction in either the standard position or stress test. Despite the absence of plantar plate tear in these two patients, they exhibited dorsal subluxation of the proximal phalanx during the stress test, indicating micro-instability associated with potential plantar plate failure. No tear was observed in these same two patients, although all cases of plantar plate tears identified in magnetic resonance imaging (MRI) were confirmed during surgical revision.
In the group of asymptomatic patients, 9 out of 10 individuals tested negative for plantar plate dysfunction. However, 1 out of 10 individuals demonstrated positive findings for plantar plate dysfunction, specifically dorsal subluxation observed exclusively during the stress test. No plantar plate tear was detected in this patient.
No significant flexor tendon tear was seen in all patients (
Table 2).
Some examples and pictures of the various patients will be illustrated below.
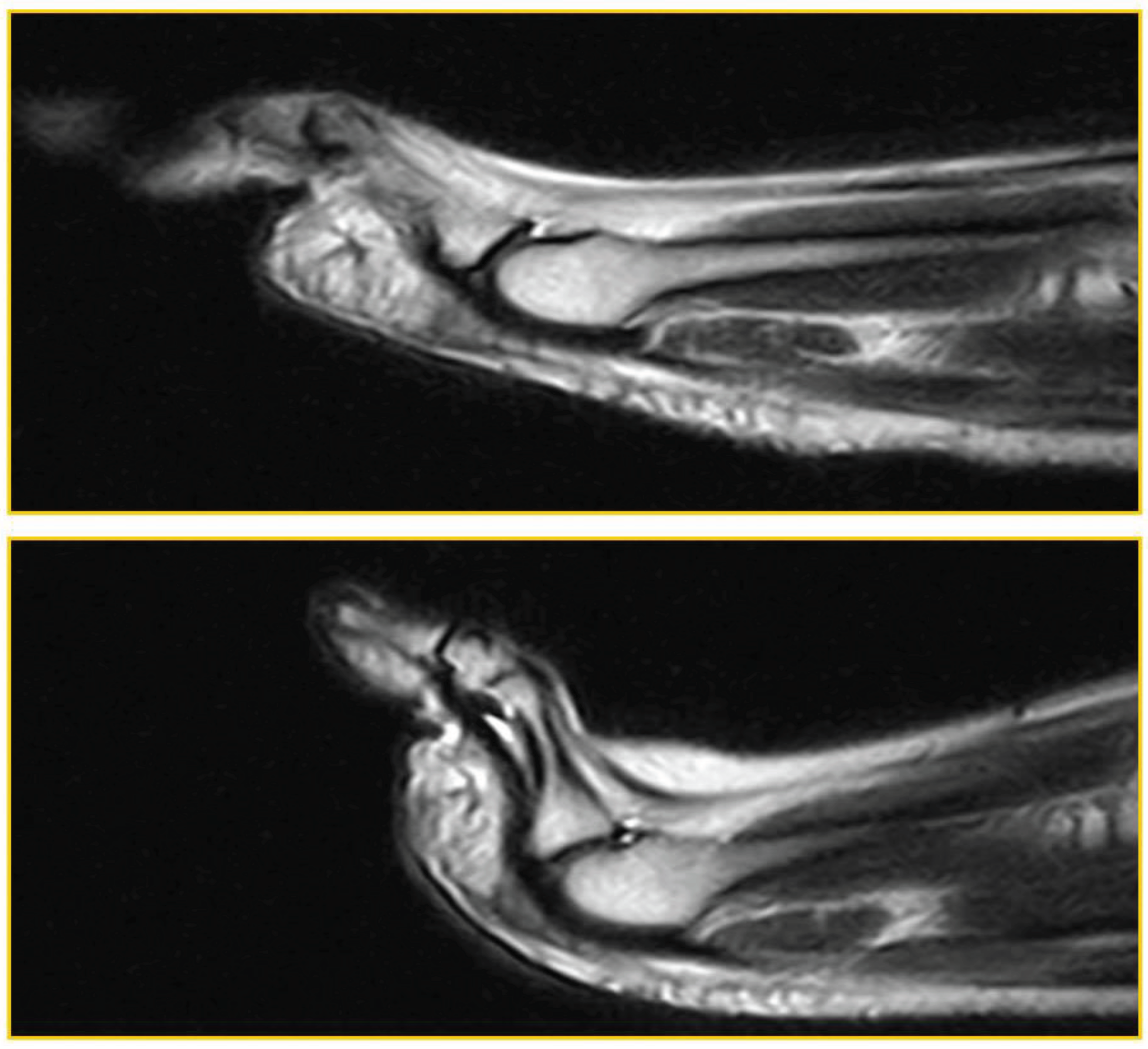
Patient 1:asymptomatic (52 years, male).True negative:Regular PP, homogeneously hypointense both in standard position and during ST (
Figure 2)
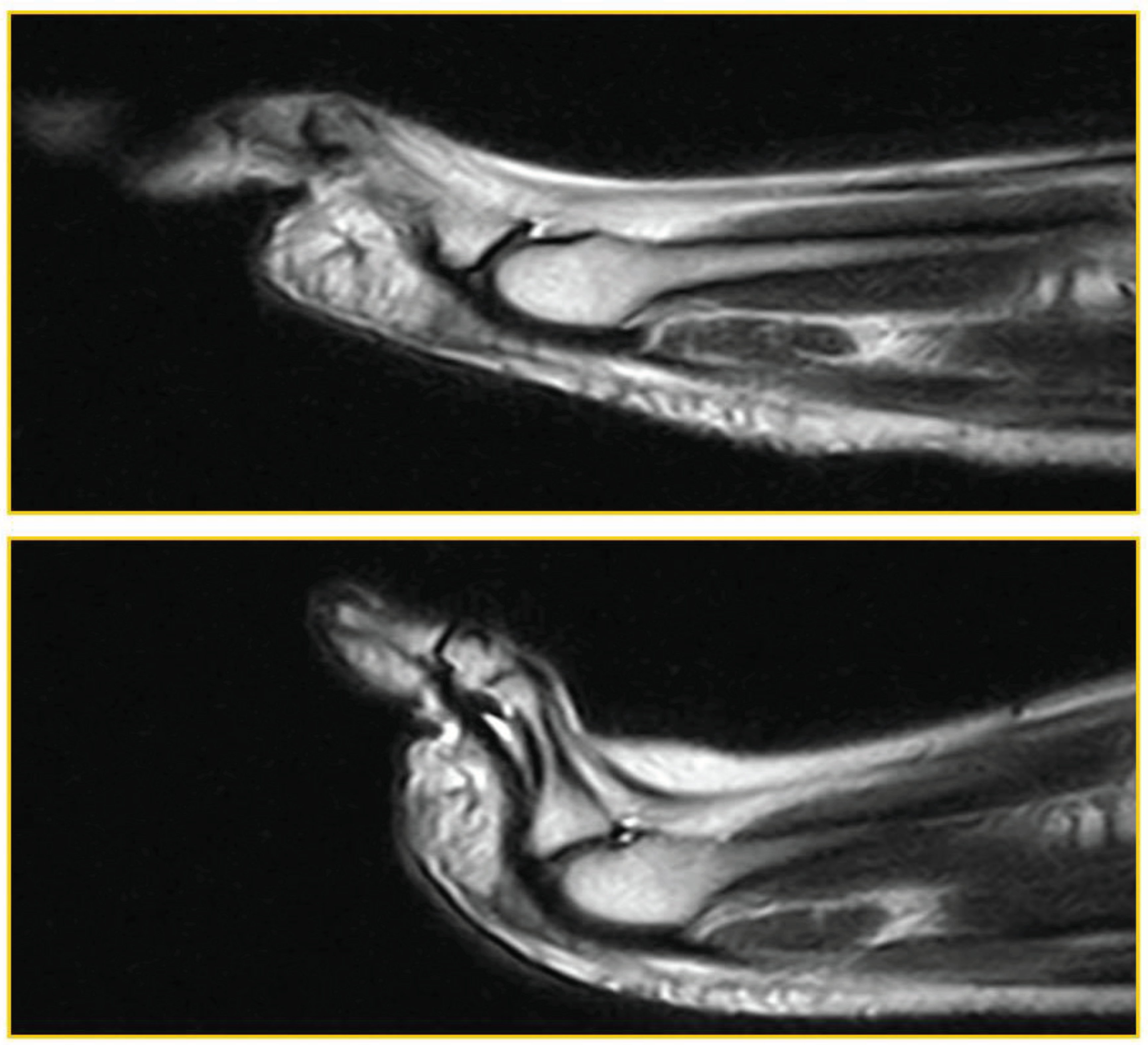
Patient 2: asymptomatic (34 years woman). False negative (laxity): MF instability (dorsal subluxation of the proximal phalanx) was demonstrated only during TS in the absence of PP tear (
Figure 3).
Patient 3: symptomatic (55-year-old woman). True positive: PP lesion visible both in standard position and during ST; dorsal subluxation is highlighted during ST (
Figure 3).
In this image, it can be seen that the lesion affects the distal portion of the plantar plate, at the insertion at the base of the proximal phalanx. There is a small interruption of the normal hypointensity of the plate itself superficialy.
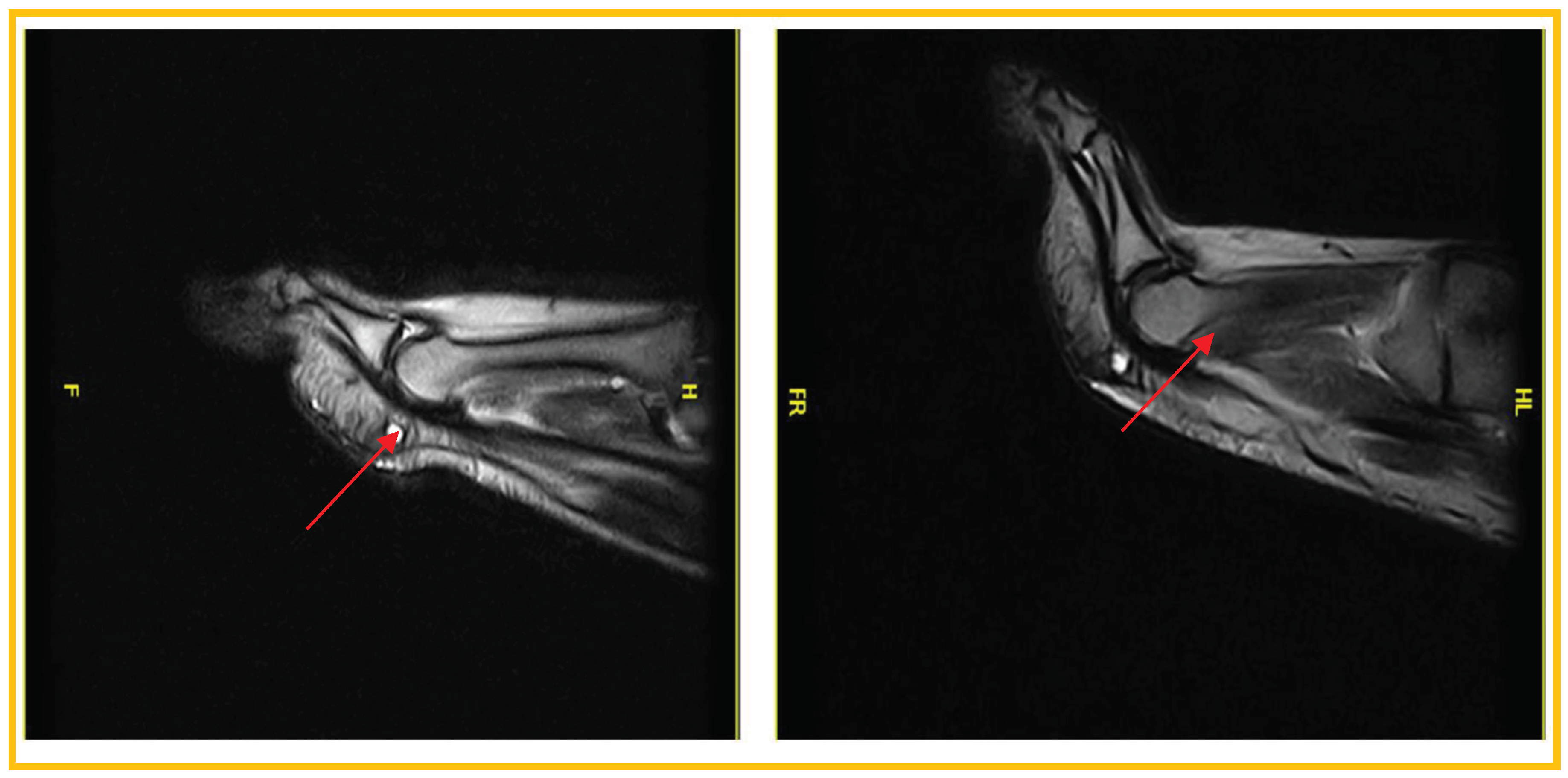
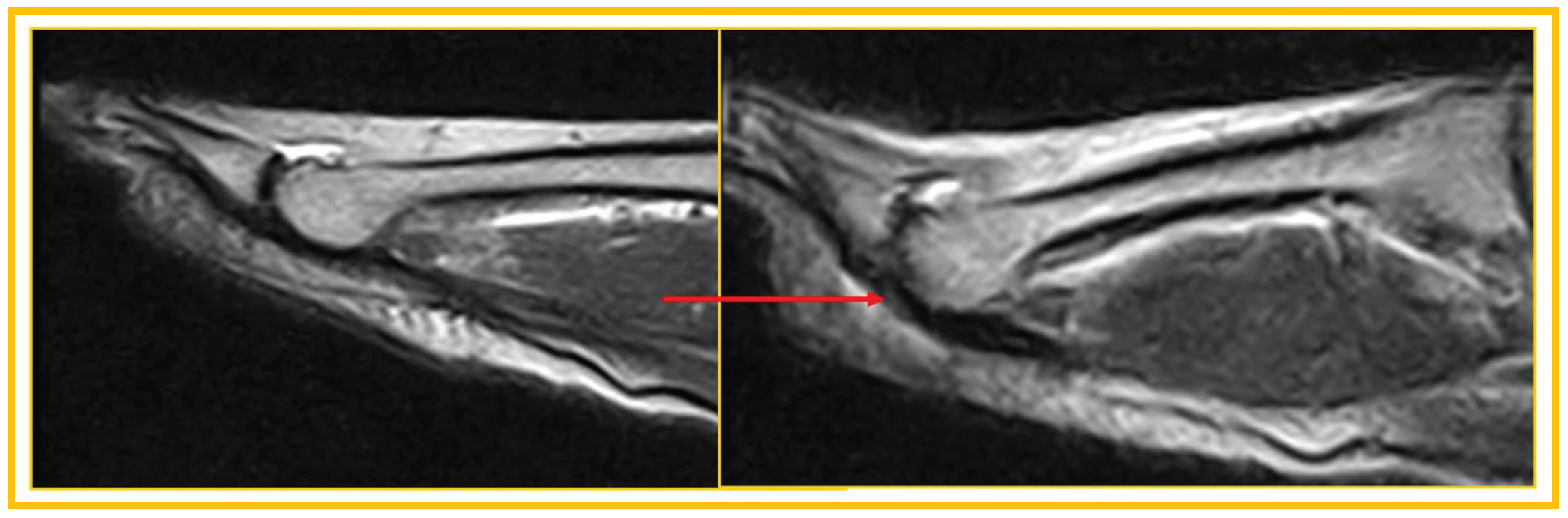
Patient 4: symptomatic (53 years, man). True positive: PP lesion visible both in standard position and during ST; dorsal subluxation is highlighted during ST (
Figure 5).
The lesion affects the distal portion of the plantar plate, at the insertion at the base of the proximal phalanx; dorsal subluxation is observed in all slices during the stress test.
Patient 5: symptomatic (59 years, woman). False negative: Joint instability; dorsal subluxation of the proximal phalanx, visible only during ST, in the absence of PP tear (
Figure 6).
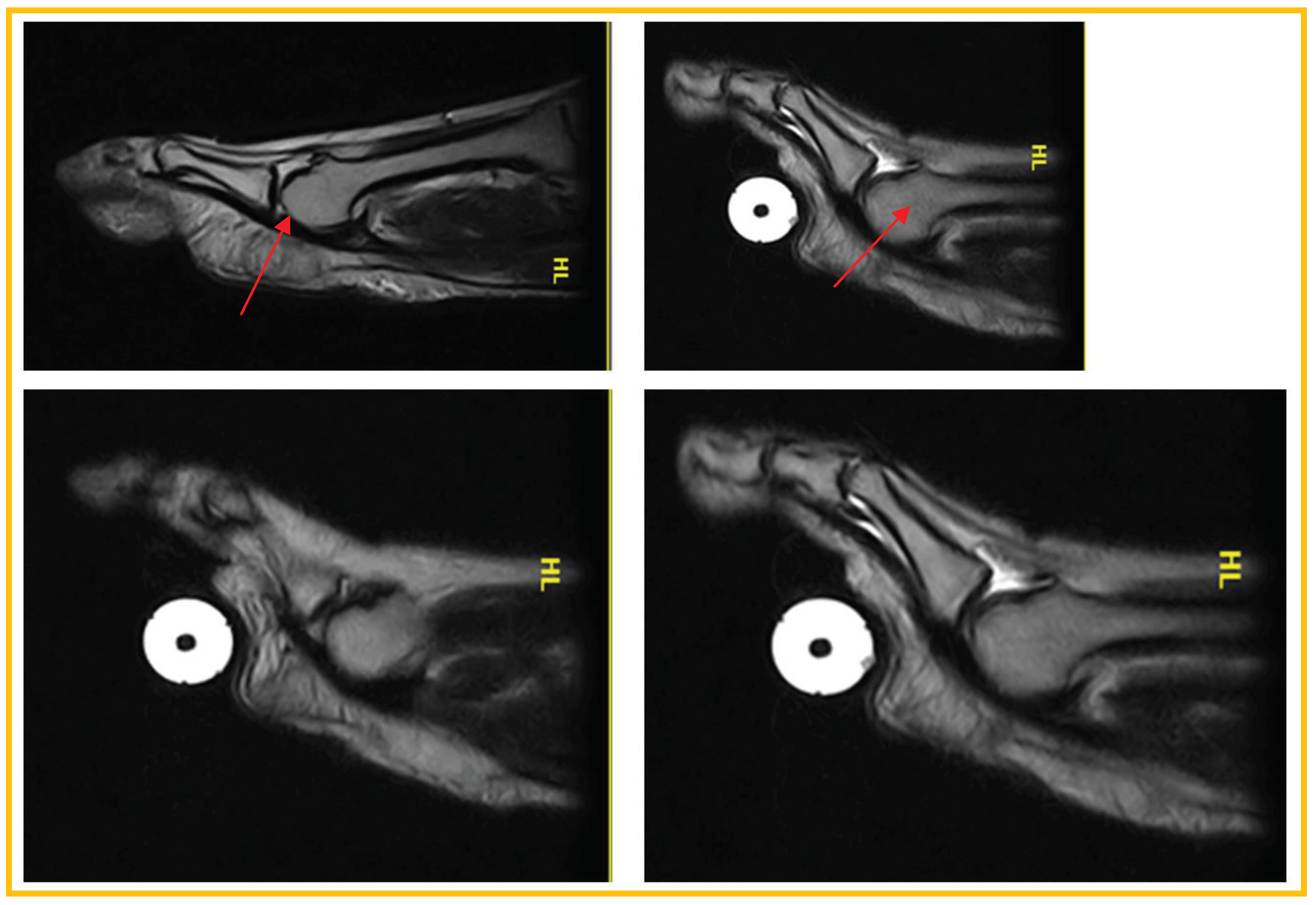
Patient 6: symptomatic (54 years,man). False negative: negative for PP lesion in standard position. The lesion becomes evident during ST (
Figure 7).
The plantar plate lesion, evident only with the stress test, affects the plantar plate at the insertion on the proximal phalanx, on the deep side.
Patient 7: symptomatic (54 years, man). False negative (laxity): Symptomatic patient, negative for PP lesion both in standard position and during ST. Laxity in the absence of a lesion was later confirmed at revision surgery (
Figure 8).
The results show that stress testing is essential for a correct diagnosis of plantar plate tear in cases where there is clinical suspicion of injury.
Standard MRI reports, in asymptomatic patients, a specificity of 100% and high VPN (90%) increased with ST (specificity and VPN equal to 100%).
In symptomatic patients, assessment of PP lesion at standard MRI reports a sensitivity of 75%, which increased to 100% with ST; sensitivity was 60% in the evaluation of MF subluxation (standard MRI), but it reached 100% with ST.
Therefore, it is important not only to identify misdiagnosed lesions but also to evaluate possible instability and dorsal subluxation of the proximal phalanx.
Also in positive patients in 2/15 (13,3%) was observed intermetatarsal space (IS) neuroma, in 2/15 (13,3%) second IS wide pericapsular fibrosis, in 2/15 (13,3%) second and third MF bursitis. In 5/15 (33,3%) were found bone lesions (1/15 second metatarsal Freiberg disease, 1/15 fifth metatarsal head stress fracture, 3/15 first MF degenerative arthritis) and in 7/15 (46,6%) flexor tendinopathy. None of these alterations were found in asymptomatic patients.
Our study’s advantage is that there was a surgical evaluation in all positive patients, which confirmed our results.
4. Discussion
Among the non-invasive methods in the diagnosis of plantar plate disease, an equally important role is played by ultrasound. Various studies and systematic reviews are available in the literature on the greater diagnostic validity of one or the other technique, often with non univocal results.
The current study conducted by Ryan J. Donegan et al. [
17] aimed to compare the diagnostic accuracy of magnetic resonance imaging (MRI) and high-resolution dynamic ultrasonography in evaluating plantar plate pathology, with surgical confirmation as the reference standard. The study included a multicenter retrospective analysis.
The findings of the study indicated that MRI had a sensitivity of 60%, specificity of 100%, positive predictive value of 100%, and negative predictive value of 33%. The overall diagnostic accuracy of MRI, compared to intraoperative findings, was 66%. On the other hand, high-resolution dynamic ultrasonography showed a sensitivity of 100%, specificity of 100%, positive predictive value of 100%, and negative predictive value of 100%. The overall diagnostic accuracy of ultrasonography, compared to intraoperative findings, was 100%. Although not statistically significant, high-resolution dynamic ultrasonography demonstrated greater accuracy than MRI in diagnosing plantar plate pathology in the lesser metatarsophalangeal joint.
Contrary to the findings of the current study, a meta-analysis conducted by Xin Duan et al. revealed different results [
18]. The meta-analysis included studies that investigated the diagnostic detection of MRI or ultrasound for plantar plate tears, with surgical criteria as the reference test. A total of seven studies, comprising 246 plantar plate tears, were included in the meta-analysis. The results of the meta-analysis indicated that MRI exhibited higher diagnostic accuracy than ultrasound for the detection of plantar plate tears. The sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio for MRI were 95%, 54%, 2.08, and 0.08, respectively. In comparison, ultrasound had a sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio of 93%, 33%, 1.20, and 0.35, respectively. The summary receiver operating characteristic curve also indicated that MRI had superior diagnostic accuracy compared to ultrasound.
Rachel H. Albright et al. [
19] conducted a systematic review and meta-analysis to assess the diagnostic accuracy of MRI and dynamic ultrasound for plantar plate injuries. The review included a thorough search of databases such as MEDLINE, CINAHL, and Clinicaltrials.gov until May 2020. The pooled sensitivity and specificity of MRI for plantar plate injuries were found to be 89% and 83%, respectively. For ultrasound, the sensitivity and specificity were 95% and 52%, respectively. Overall, MRI demonstrated superiority over ultrasound in diagnosing plantar plate injuries. However, ultrasound was more sensitive than MRI, suggesting that a negative ultrasound result would likely rule out a plantar plate injury when there is uncertainty based on a physical examination alone.
In another comparative study, Erin E. Klein et al. [
20] examined the diagnostic performance of MRI and ultrasound in 51 patients with suspected unilateral plantar plate tears specifically at the second metatarsophalangeal joint. All 51 patients were examined intraoperatively, and a total of 46 plantar plate tears were identified. The sensitivity, specificity, positive predictive value, and negative predictive value of MRI were 73.9%, 100%, 100%, and 29.4%, respectively. For ultrasound, the corresponding values were 91.5%, 25%, 91.5%, and 25%, respectively. Interestingly, MRI was able to detect four collateral ligament tears that were not identified on ultrasound. Based on these results, both MRI and ultrasound are considered suitable modalities for imaging plantar plate pathology.
It’s evident from the results available in the literature that both dynamic ultrasound and MRI play an important role in the diagnosis of plantar plate lesions, with often comparable results. Both methods, however, have limitations in identifying all plantar plate lesions.
The standard MRI examination in our study without stress test has a sensitivity rate of 75% for plantar plate lesion and 60% in the evaluation of MF subluxation.
A comparative study conducted by Sung et al. [
21] investigated the concordance between MRI findings and intraoperative results in a cohort of 45 patients (38 females and 3 males) with an average age of 52.1 years. Intraoperatively, 41 cases of plantar plate tears and 4 cases of intact ligaments were identified. The assessment of accuracy, sensitivity, specificity, positive predictive value, and negative predictive value yielded values of 96%, 95%, 100%, 100%, and 67%, respectively. Moreover, the clinical diagnosis of plantar plate injury achieved a high level of accuracy, correctly identifying the condition in 41 out of 45 patients (91%) within the study population.
Caio Nery et all [
22] in their study compared evaluation of the MTP plantar plates with arthroscopic findings in 35 patients. With the use of the standard examination, it was observed a level of precision of 88,5% in senior radiologists and a level of precision of 77,0% in less experienced radiologists.
In their study, Andrè Fukunishi Yamadà et al. [
23] conducted a comprehensive investigation into the diagnostic performance of direct and indirect MRI features for plaque lesions at radius II and III, using surgical findings as the reference standard. The study encompassed a retrospective analysis of 23 patients who presented with symptomatic instability of lesser MTP joints and had previously undergone preoperative 1.5-T MRI and subsequent surgical evaluation. A total of 45 lesser MTP joints were included in the analysis. The researchers found that the presence of pericapsular fibrosis exhibited high sensitivity (91.2%), specificity (90.9%), and accuracy (91.1%) for the diagnosis of PP tears. Furthermore, they determined that the PP-proximal phalanx distance, when a cutoff value of 0.275 cm was applied, yielded a sensitivity of 64.7%, specificity of 90.9%, and accuracy of 71.1% in the diagnosis of PP tears.
Even in MRI studies with higher levels of precision, a concordance close to 100% is never achieved. The aim of our study is to evaluate how a simple additional sequence can be a valid tool to achieve greater accuracy in the diagnosis of both plantar plate lesions and dysfunction.
Stress test would appear to significantly increase the diagnostic accuracy of MRI in the evaluation of plantar plate disease, furthermore no similar studies are yet available in the literature.
Crucially, forefoot MRI is not an operator-dependent investigation, and it provides more detail when compared with ultrasound, particularly on bone pathology.
ST is simple and quick to perform (since it is a single T2-weighted sequence) for both the operator and the patient.
When compared with arthro-MRI [
24] (after intra-articular injection of MdC, invasive), standard MRI + ST is a non-invasive and less expensive investigation that is also feasible with “dedicated” equipment.
It is interesting to analyse a scientific paper by Vanessa Dinoà et all [
25] on the difference in identifying plantar plate lesions without and with contrast-enhanced and fat-suppressed MRI.
This study examined a total of 249 contrast-enhanced forefoot MRI scans obtained from patients diagnosed with metatarsalgia between June 2012 and June 2013. The scans were reviewed by two specialized radiologists with expertise in musculoskeletal imaging. Among the patients included in the study, 59 individuals were identified as having in the plantar plate (PP); is noteworthy that 59% of these were female. Among the patients with PP tears, the majority (81.4%) had a single lesion in one of their metatarsophalangeal (MTP) joints. However, a small number of patients (7 out of 59) had a PP tear present in each foot, while 3 out of 59 patients had two PP lesions in one foot, and only 1 out of 59 patients had three lesions in one foot. Pericapsular fibrosis was observed in 70.5% of the PP lesions in pre-contrast sequences. However, for the remaining 29.5% of the lesions, the presence of the tear was only evident after the administration of a contrast agent containing gadolinium. This highlights the substantial proportion of PP lesions that became visible on MRI scans only after the administration of gadolinium.
It is true that in this case the use of contrast agents increased the diagnostic capacity of the examination, but in our opinion the cost and potential danger of using contrast agents and the contraindications to MRI examination do not allow an indication for the use of contrast agents in the diagnosis of plantar plate lesions. In our opinion, the same diagnostic step can simply be obtained with the use of the stress test, with any type of MRI machine, without the need to use high magnetic field machines, often a prerequisite in the case of arthro MRI or MRI with contrast agents.
Compared to ultrasound, MRI adds information that cannot be obtained with ultrasound, allowing, first and foremost, the study of any concomitant bone pathology (e.g. bone marrow edema). However, ultrasound can allow more reliable dynamic tests in real time. MRI study with a sectoral system makes it possible to reduce the not-inconsiderable percentage of claustrophobic patients. It should also be mentioned that there’s a small percentage of patients who cannot undergo MRI (e.g. carriers of incompatible electronic devices and ferromagnetic metal fragments in noble tissue).
In our opinion, stress testing must enter clinical practice in clinical suspicion of plantar plate lesions, as the results of our study seem to demonstrate.
The major limitation of this study is the small number of patients, and further investigation is needed to confirm our preliminary data.
5. Conclusion
Based on the data available in the literature, the standard MRI examination of plantar plate has a similar sensitivity for the identification of plantar plaque as ultrasound, with a sensitivity rate varying between 60% and 90% in the various studies.
In our study introducing the stress test, the sensitivity for both diagnosis of plantar plate lesion and in the evaluation of MF subluxation reaches 100% (a surgical evaluation was performed on all symptomatic patients for confirmation).
The aim of our study is to demonstrate how MRI with the introduction of the “stress test”, which in our opinion should become part of the normal clinical routine in patients with suspected plantar plate lesion, has a sensitivity and a negative predictive value close to 100%, thus proving to be the most suitable non-invasive diagnostic method for identifying both plantar plate lesion and plate dysfunction (dorsal subluxation), with very low health care costs and with total patient comfort (possibility of using low magnetic field MRI equipment).
A 45-degree dorsiflexion stress test was then performed for approximately 2.30 min, the time required for completion of the sequence.
If these results are confirmed by other studies in the literature, further invasive diagnostic investigations, such as arthrography or arthro-MRI, will no longer be necessary.
Ultrasound, however, has the advantage of being a noninvasive method, but comparing the results of our study with “stress test” with the data available in the literature it has lower sensitivity and negative predictive value, also it does not allow to assess the possible bone marrow edema neither the degree of concomitant arthritis.
Author Statement
The article is a recise and expanded version of a paper entitled “Plantar plate disease as a part of forefoot overload syndrome: the role of MRI in detecting associated injuries”, which was presented at European Congress of Radiology, Wien, 2017.
References
- Johnston RB 3rd, Smith J, Daniels T. The plantar plate of the lesser toes: an anatomical study in human cadavers. Foot Ankle Int. 1994, 15, 276–82. [Google Scholar] [CrossRef] [PubMed]
- Park JV, Finney FT, Singer NV, Saunders NE, Walley KC, Holmes JR, Walton DM, Talusan PG. Proximal Plantar Plate of Lesser Toe Metatarsophalangeal Joint Vascular Supply. Foot Ankle Int. 2023, 44, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Stainsby, GD. Pathological anatomy and dynamic effect of the displaced plantar plate and the importance of the integrity of the plantar plate-deep transverse metatarsal ligament tie-bar. Ann R Coll Surg Engl. 1997, 79, 58–68. [Google Scholar] [PubMed]
- McCarthy CL, Thompson GV. Ultrasound findings of plantar plate tears of the lesser metatarsophalangeal joints. Skeletal Radiol. 2021, 50, 1513–1525. [Google Scholar] [CrossRef] [PubMed]
- Bowers WH, Wolf JW Jr, Nehil JL, Bittinger S. The proximal interphalangeal joint volar plate. I. An anatomical and biomechanical study. J Hand Surg Am. 1980, 5, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Pang EQ, Yao J. Anatomy and Biomechanics of the Finger Proximal Interphalangeal Joint. Hand Clin. 2018, 34, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Hatch, DJ. Anatomy: Plantar Plate. Clin Podiatr Med Surg. 2022, 39, 411–419. [Google Scholar] [CrossRef]
- Maas NM, van der Grinten M, Bramer WM, Kleinrensink GJ. Metatarsophalangeal joint stability: a systematic review on the plantar plate of the lesser toes. J Foot Ankle Res. 2016, 9, 32. [Google Scholar] [CrossRef]
- Lee SW, Ng ZY, Fogg QA. Three-dimensional analysis of the palmar plate and collateral ligaments at the proximal interphalangeal joint. J Hand Surg Eur Vol. 2014, 39, 391–7. [Google Scholar] [CrossRef]
- Gregg J, Marks P, Silberstein M, Schneider T, Kerr J. Histologic anatomy of the lesser metatarsophalangeal joint plantar plate. Surg Radiol Anat. 2007, 29, 141–7. [Google Scholar] [CrossRef]
- Albright RH, Brooks BM, Chingre M, Klein EE, Weil LS Jr, Fleischer AE. Diagnostic accuracy of magnetic resonance imaging (MRI) versus dynamic ultrasound for plantar plate injuries: A systematic review and meta-analysis. Eur J Radiol. 2022, 152, 110315. [Google Scholar] [CrossRef]
- Mann TS, Nery CAS, Baumfeld D, Fernandes EÁ. Degenerative injuries of the metatarsophalangeal plantar plate on magnetic resonance imaging: a new perspective. Einstein (Sao Paulo). 2022, 20, eAO6543; [Google Scholar] [CrossRef]
- Nery C, Baumfeld D, Umans H, Yamada AF. MR Imaging of the Plantar Plate: Normal Anatomy, Turf Toe, and Other Injuries. Magn Reson Imaging Clin N Am. 2017, 25, 127–144. [Google Scholar] [CrossRef]
- Umans HR, Elsinger E. The plantar plate of the lesser metatarsophalangeal joints: potential for injury and role of MR imaging. Magn Reson Imaging Clin N Am. 2001, 9, 659–69. [Google Scholar] [CrossRef]
- Finney FT, Cata E, Holmes JR, Talusan PG. Anatomy and Physiology of the Lesser Metatarsophalangeal Joints. Foot Ankle Clin. 2018, 23, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Baker JR, Albright R, Jameson R, Chingre M, Klein EE, Weil L Jr, Fleischer A. Treatment of Lesser Metatarsophalangeal Joint Instability With Plantar Plate Repair: A Systematic Review and Meta-Analysis. J Foot Ankle Surg. 2022, 61, 1114–1118. [Google Scholar] [CrossRef] [PubMed]
- Donegan RJ, Stauffer A, Heaslet M, Poliskie M. Comparing Magnetic Resonance Imaging and High-Resolution Dynamic Ultrasonography for Diagnosis of Plantar Plate Pathology: A Case Series. J Foot Ankle Surg. 2017, 56, 371–374. [Google Scholar] [CrossRef]
- Duan X, Li L, Wei DQ, Liu M, Yu X, Xu Z, Long Y, Xiang Z. Role of magnetic resonance imaging versus ultrasound for detection of plantar plate tear. J Orthop Surg Res. 2017, 12, 14. [Google Scholar] [CrossRef] [PubMed]
- Albright RH, Brooks BM, Chingre M, Klein EE, Weil LS Jr, Fleischer AE. Diagnostic accuracy of magnetic resonance imaging (MRI) versus dynamic ultrasound for plantar plate injuries: A systematic review and meta-analysis. Eur J Radiol. 2022, 152, 110315. [Google Scholar] [CrossRef] [PubMed]
- Klein EE, Weil L Jr, Weil LS Sr, Knight J. Magnetic resonance imaging versus musculoskeletal ultrasound for identification and localization of plantar plate tears. Foot Ankle Spec. 2012, 5, 359–65. [Google Scholar] [CrossRef] [PubMed]
- Sung W, Weil L Jr, Weil LS Sr, Rolfes RJ. Diagnosis of plantar plate injury by magnetic resonance imaging with reference to intraoperative findings. J Foot Ankle Surg. 2012, 51, 570–4. [Google Scholar] [CrossRef] [PubMed]
- Nery C, Coughlin MJ, Baumfeld D, Mann TS, Yamada AF, Fernandes EA. MRI evaluation of the MTP plantar plates compared with arthroscopic findings: a prospective study. Foot Ankle Int. 2013, 34, 315–22. [Google Scholar] [CrossRef] [PubMed]
- Yamada AF, Crema MD, Nery C, Baumfeld D, Mann TS, Skaf AY, Fernandes ADRC. Second and Third Metatarsophalangeal Plantar Plate Tears: Diagnostic Performance of Direct and Indirect MRI Features Using Surgical Findings as the Reference Standard. AJR Am J Roentgenol. 2017, 209, W100–W108. [Google Scholar] [CrossRef]
- Yao L, Do HM, Cracchiolo A, Farahani K. Plantar plate of the foot: findings on conventional arthrography and MR imaging. AJR Am J Roentgenol. 1994, 163, 641–4. [Google Scholar] [CrossRef] [PubMed]
- Dinoá V, von Ranke F, Costa F, Marchiori E. Evaluation of lesser metatarsophalangeal joint plantar plate tears with contrast-enhanced and fat-suppressed MRI. Skeletal Radiol. 2016, 45, 635–44. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).