Submitted:
26 February 2024
Posted:
28 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Palasciano, G.; Portincasa, P.; Vinciguerra, V.; Velardi, A.; Tardi, S.; Baldassarre, G.; Albano, O. Gallstone prevalence and gallbladder volume in children and adolescents: an epidemiological ultrasonographic survey and relationship to body mass index. Am. J. Gastroenterol. 1989, 84, 1378–1382. [Google Scholar] [PubMed]
- Nomura H.; Kashiwagi S.; Hayashi J.; Kajimaya W.; Ikematsu H.; Noguchi A, et al. Prevalence of gallstone disease in general population of Okinawa, Japan. Am J Epidemiol. 1988, 128:598-605. [CrossRef]
- Wesdorp I; Bosman D.; de Graaff A.; Aronson D.; van der Blij F.; Taminiau J. Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr. 2000, 31,411-7.
- Zdanowicz K.; Daniluk J.; Lebensztejn DM.; Daniluk U. The Etiology of Cholelithiasis in Children and Adolescents-A Literature Review. Int J Mol Sci. 2022, 23, 13376. [CrossRef] [PubMed]
- Koebnick C.; Smith N.; Black MH.; Porter AH.; Richie BA.; Hudson S.; Gililland D.; Jacobsen SJ.; Longstreth GF. Pediatric obesity and gallstone disease. J Pediatr Gastroenterol Nutr. 2012, 55:328-33. [CrossRef]
- Grace, W.A.; Ransohoff, D.F. Natural history of silent gallstone: the innocent gallstone is not a myth. N. Engl. J. Med. 1982, 23, 798–800. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Park, Y.S.; Park, J.H. Cholecystectomy is feasible in children with small-sized or large numbers of gallstones and in those with persistent symptoms despite medical treatment. Pediatr. Gastroenterol. Hepatol. Nutr. 2020, 23, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Bogue, C.O.; Murphy, A.J.; Gerstle, J.T.; Moineddin, R.; Daneman, A. Risk factors, complications, and outcomes of gallstone in children. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Serdaroglu, F.; Koca, Y.S.; Saltik, F.; Koca, T.; Dereci, S.; Akcam, M.; Akcam, F.Z. Gallstones in childhood: etiology, clinical features, and prognosis. Eur. J. Gastroenterol. Hepatol. 2016, 28, 1468–1472. [Google Scholar] [CrossRef] [PubMed]
- Rocca, R.; Castellino, F.; Dapermo, F.; Masoero, G.; Sostegni, R.; Ercole, E.; et al. Therapeutic ERCP in paediatric patients. Digestive and Liver Disease 2005, 37, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.L.; Fogel, E.L.; Sherman, S.; McHenry, L.; Watkins, J.L.; Croffie, J.M.; et al. Diagnostic and therapeutic endoscopic retrograde cholangiopancreatography in children: a large series report. J. Pediatr. Gastroenterol. Nutr. 2005, 41, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Issa, H.; Al-Haddad, A.; Al-Salem, A.H. Diagnostic and therapeutic ERCP in the pediatric age group. Pediatr. Surg. Int. 2007, 23, 111–116. [Google Scholar] [CrossRef]
- Jang, J.Y.; Yoon, C.H.; Kim, K.M. Endoscopic retrograde cholangiopancreatography in pancreatic and biliary tract disease in Korean children. World J. Gastroenterol. 2010, 28, 490–495. [Google Scholar] [CrossRef]
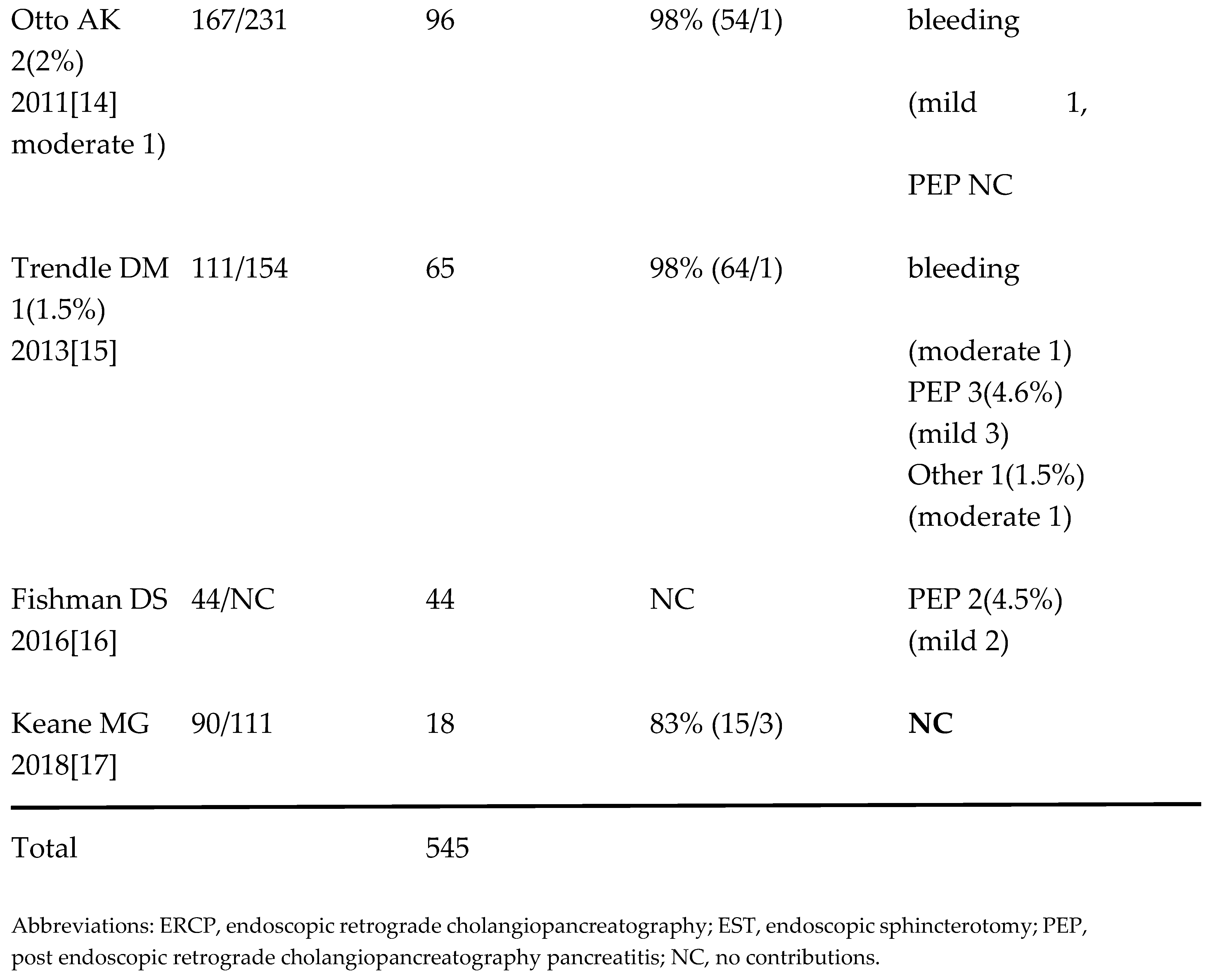
- Otto AK, Neal MD, Slivka AN, Kane TD. (2011) An appraisal of endoscopic retrograde cholangiopancreatography (ERCP) for pancreaticobiliary disease in children: our institutional experience in 231 cases. Surg Endosc 25:2536-2540. [CrossRef]
- Troendle, D.M.; Barth, B.A. ERCP can be safely and effectively performed by a pediatric gastroenterologist for choledocholithiasis in a pediatric facility. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 655–658. [Google Scholar] [CrossRef] [PubMed]
- Fishman, D.S.; Chumpitazi, B.P.; Raijman, I.; Tsai, C.M.; Smith, E.O.; et al. Endoscopic retrograde cholangiopancreatography for pediatric choledocholithiasis: assessing the need for endoscopic intervention. World J. Gastroenterol. 2016, 8, 425–432. [Google Scholar]
- Keane, M.G.; Kumar, M.; Cieplik, N.; Thorburn, D.; Johnson, G.J.; Webster, G.J.; Chapman, M.H.; Lindley, K.J.; Pereira, S.P. Paediatric pancreaticobiliary endoscopy: a 21-year experience from a tertiary hepatobiliary centre and systematic literature review. BMC Pediatr. 2018, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, M.; Atomi, Y. Does endoscopic sphincterotomy cause prolonged pancreatobiliary reflux? Am J Gastroenterol. 1999, 94, 795–798. [Google Scholar] [CrossRef]
- Gregg, J.A.; Girolami, P.D.; Carr-Locke, D.L. Effects of sphincteroplasty and endoscopic sphincterotomy on the bacteriologic characteristics of the common bile duct. Am. J. Surg. 1985, 149, 668–671. [Google Scholar] [CrossRef] [PubMed]
- Sand, J.; Airo, I.; Hiltunen, K.M.; Mattila, J. Nordback I. Changes in biliary bacteria after endoscopic cholangiography and sphincterotomy. Am. Surg. 1992, 58, 324–328. [Google Scholar]
- Weinberg, B.M.; Shindy, W.; Lo, S. Endoscopic balloon dilatation (sphincteroplasty) versus sphincterotomy for bile duct stones. Review Cochrane Database Syst Rev. 2006, 18, CD004890. [Google Scholar]
- Zhao, H.C.; He, L.; Zhou, D.C.; Geng, X.P.; Pan, F.M. Meta-analysis comparison of endoscopic papillary balloon dilatation and endoscopic sphincteropapillotomy. World J. Gastroenterol. 2013, 19, 3883–3891. [Google Scholar] [CrossRef]
- Sakai, Y.; Tsuyuguchi, T.; Sugiyama, H.; Hayashi, M.; Senoo, J.; Kusakabe, Y.; Yasui, S.; Mikata, R.; Yokosuka, O. Comparison of endoscopic papillary balloon dilatation and endoscopic sphincterotomy for bile duct stones. World J. Gastrointest Endosc. 2016, 8, 395–401. [Google Scholar] [CrossRef]
- Sato, H.; Kodama, T.; Takaaki, J.; Tatsumi, Y.; Maeda, T.; Fujita, S.; Fukui, Y.; Ogasawara, H.; Mitsufuji, S. Endoscopic papillary balloon dilatation may preserve sphincter of Oddi function after common bile duct stone management: evaluation from the viewpoint of endoscopic manometry. Gut. 1997, 41, 541–544. [Google Scholar] [CrossRef]
- Yasuda, I.; Tomita, E.; Enya, M.; Kato, T.; Moriwaki, H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001, 49, 686–691. [Google Scholar] [CrossRef]
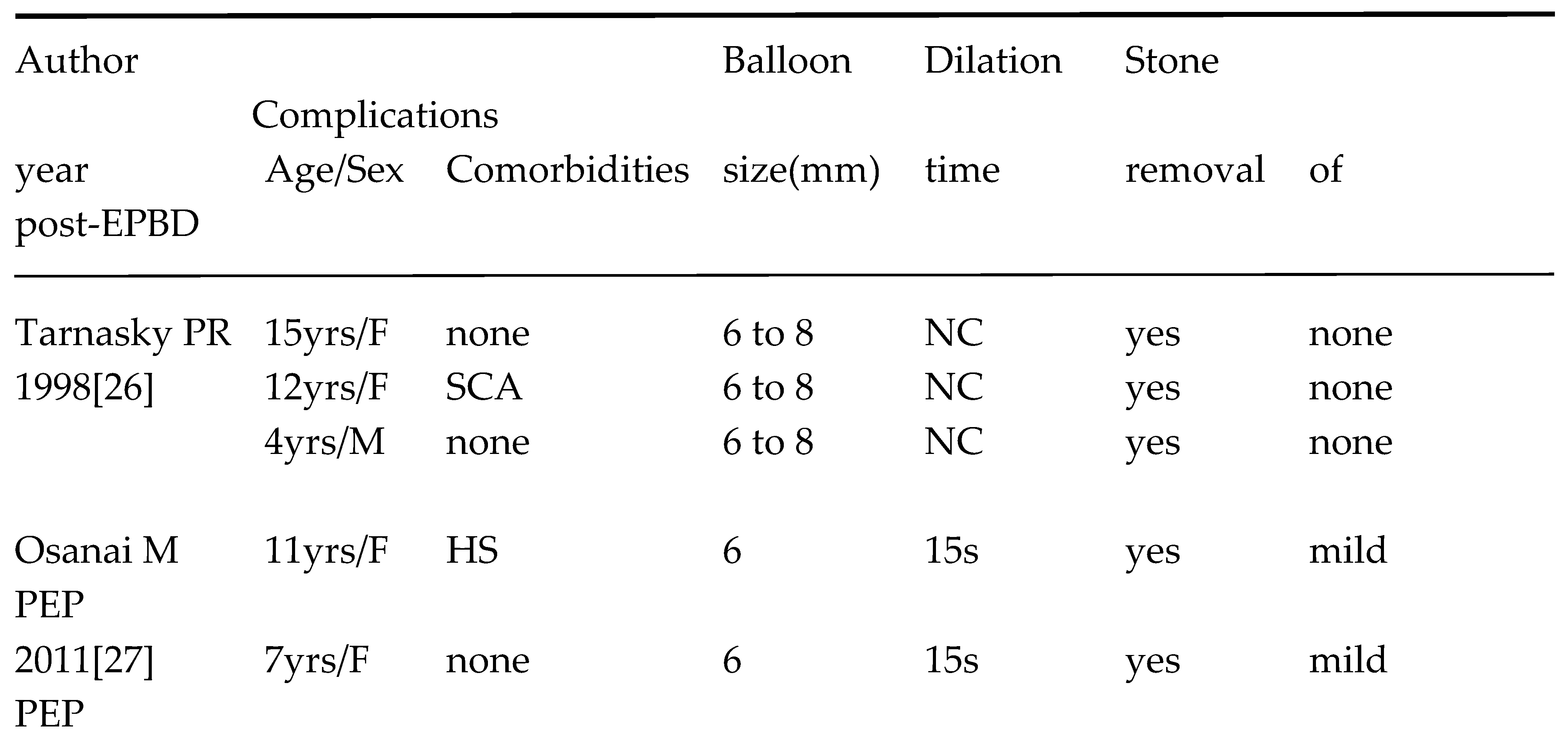
- Tarnasky, P.R.; Tagge, E.P.; Hebra, A.; Othersen, B.; Adams, D.B.; Cunningham, J.T.; Cotton, P.B.; Hawes, R.H. minimally invasive therapy for choledocholithiasis in children. Gastrointest Endosc. 1998, 47, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Osanai, M.; Maguchi, H.; Takahashi, K.; Katanuma, A.; Yane, K.; Kaneko, M.; Hashigo, S.; Katoh, S.; Harada, R.; Katoh, R.; Tanno, S. Safety and long-term outcomes of endoscopic papillary balloon dilation in children with bile duct stones. Gastrointest Endosc. 2011, 73, 619–623. [Google Scholar] [CrossRef]
- Sogo, T.; Kondo, T.; Tsunoda, T.; Murayama, A.; Komatsu, H.; Inui, A.; Fujisawa, T. Endoscopic papillary balloon dilatation for a 7-year-old girl with choledocholithiasis. Pediatr Int. 2013, 55, e1–e3. [Google Scholar] [CrossRef]
- ASGE Standards of Practice Committee. Adverse events associated with ERCP. Gastrointest Endosc. 2017, 85, 32-47.
- Cotton, P.B.; Lehman, G.; Vennes, J.; Geenen, J.E.; Russell, R.C.; Meyers, W.C.; Liguory, C.; Nickl, N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991, 37, 383–393. [Google Scholar] [CrossRef]
- Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013, 62, 102-11. [CrossRef]
- Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilatation, a possible alternative to endoscopic papillotomy. Lancet 1982; 1: 1306-7. [CrossRef]
- Disario JA, Freeman ML, Bjorkman DJ, et al. Endoscopic balloon dilatation compared with sphincterotomy for extraction of bile stones. Gastroenterol 2004; 127: 1291-9. [CrossRef]
- Manes G.; Paspatis G.; Aabakken L.; Anderloni A.; Arvanitakis M.; Ah-Soune P.; Barthet M.; Domagk D.; Dumonceau J-M, Gigot J-F; et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019, 51, 472-491. [CrossRef]
- Lou, Q.; Sun, J.; Zhang, X.; Shen, H. Successful therapeutic ERCP in a 99-day-old child with common bile duct stones: a case report and discussions on the particularities of the ERCP in children. Front Pediatr. 2020, 28, 435. [Google Scholar] [CrossRef] [PubMed]
- Zhao HC, He L, Zhou DC, Geng XP, Pan FM. Meta-analysis comparison of endoscopic papillary balloon dilatation and endoscopic sphincteropapillotomy. World J Gastroenterol. 2013, 19, 3883-91.
- Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996, 335:909-18. [CrossRef]
- Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro M, Hritz I, Mariani A, Paspatis G, Radaelli F, Lakhtakia S, Veitch AM, van Hooft JE. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020, 52:127-149. [CrossRef]
- Bae SS, Lee DW, Han J, Kim HG. Risk factor of bleeding after endoscopic sphincterotomy in average risk patients. Surg Endosc. 2019, 33:3334-3340. [CrossRef]
- Ersoz, G.; Tekesin, O.; Ozutemiz, A.O.; Gunsar, F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003, 57, 156–159. [Google Scholar] [CrossRef]
- Jang SI, Yun GW, Lee DK. Balloon dilation itself may not be a major determinant of post-endoscopic retrograde cholangiopancreatography pancreatitis. World J Gastroenterol. 2014, 20, 16913-24. [CrossRef]
- Fujisawa, T.; Kagawa, K.; Hisatomi, K.; Kubota, K.; Nakajima, A.; Matsuhashi, N. Is endoscopic papillary balloon dilatation really a risk factor for post-ERCP pancreatitis? World J Gastroenterol. 2016, 22, 5909–5916. [Google Scholar] [CrossRef]
- ASGE Standards of Practice Committee; Buxbaum JL.; Abbas Fehmi SM.; Sultan S.; Fishman DS.; Qumseya BJ.; Cortessis VK.; Schilperoort H.; Kysh L.; Matsuoka L.; Yachimski P.; et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019, 89, 1075-1105. [CrossRef]
- Wang Q, Fu L, Wu T, Ding X. The ballooning time in endoscopic papillary balloon dilation for removal of bile duct stones: A systematic review and meta-analysis. Medicine (Baltimore). 2021, 100:e24735.

 |
 |
 |
 |
 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




