1. Introduction
The number of revision total hip arthroplasty (rTHAs) procedures is predicted to dramatically increase in a short time with rates over 50% [
1,
2]. Additionally, the risk of a second revision procedure after rTHA reaches 19% according to recent studies [
3,
4]. The main cause for THA failure is aseptic loosening of the implant on the acetabular side which is often associated to severe bone defects[
5,
6]. The accurate assessment of the bone loss and remaining bone stock is essential to plan the revision surgery procedure and choose the appropriate implant design, therefore classifying acetabular defects remain a major issue. In the current medical practice, classification schemes of acetabular bone defects mostly rely on traditional radiographs, which can provide a solely 2-dimension image of a more complex anatomy [
7,
8,
9,
10,
11,
12]. One of the most common, the Paprosky classification, is based on the analysis of the implant migration and the remaining radiological anatomical landmarks and provides different indications for surgical reconstruction according to the severity and localization of bone defects [
7,
13]. However, different authors reported low reliability and reproducibility due to a lack of accuracy of standard radiographs analysis and the need for subjective evaluation of bone defects features [
14,
15,
16].
CT (computed tomography) scans offer a more accurate 3-dimension view, showing anatomical structures that otherwise would be covered by the overlap of the metal implant in plain radiographs[
17]. With the rise of modern 3D modelling software, CT images can be elaborated and used to recreate tridimensional anatomical replicas of the patients’ anatomy[
18,
19,
20].
In this scenario of advanced imaging techniques, different studies proposed new methodologies for the assessment of acetabular bone defect based on 3D models. Zhang et al. proposed a new system that relies on a qualitative analysis of acetabular bone defects on 3D models of the pelvis, without a quantitative assessment, focusing on the integrity of the supporting structures to achieve sufficient implant fixation[
21]. The system needed a subjective estimation of the bone loss, and they reported excellent reliability and reproducibility when compared to x-rays. Recently, Meynen et al. used 3D models to analyze the accuracy of the Acetabular Defect Classification (ADC), a qualitative classification originally elaborated by Wirtz et al.[
22,
23]. On 3D-CT imaging with statistical shape models, bone loss volume was quantified, and this analytical defect information were used by the raters to classify defects, resulting in doubling the intra- and inter-rater reliability and in upscaling of acetabular defect classification when compared to standard radiographs[
24].
The first attempts for a reliable and precise methodology for a computerized volumetric quantification of acetabular bone loss, was the Total radial Acetabular Bone Loss (TrABL) by Gelaude et al. who developed an advanced CT-based image processing 3D anatomical reconstruction [
25]. The output of the analysis consisted in a ratio and a graphical spatial representation of the bone defect in the lateral view of the acetabulum. The methodology offered precise information in terms of volume of bone loss and spatial localization around the acetabulum but did not provide indications about the residual structural support of the remaining bone stock. Therefore, the authors suggested its use as a support for complex revision case and preexisting classification systems [
25].
Similarly, Hettich et al. validated an analytic method of acetabular bone loss pointing out the opportunity of quantifying the volume of acetabular bone defects using statistical shape models and dividing the acetabulum in 4 different anatomical sectors according to the main structural areas of the acetabulum (anterior wall and column, the posterior wall and column, the superior dome, and the medial wall) [
26]. Later in another study, the authors applied the methodology on 50 cases, where the bone loss was expressed as a percentage of decrease bone volume on the different sectors of the acetabulum and added a qualitative analysis that described the morphology of the most common defects [
27].
The methodologies previously described, focused on the analysis of the bone defects in terms of bone volume loss. This quantitative assessment, although objective and reliable, do not offer an overall intuitive comprehension of the extent and severity of the defect. Moreover, providing only a visual output of the lateral view of the acetabulum makes difficult to understand the morphology and extension of the defect and, the integrity of the main structural areas. This could potentially limit the use of these methodology in the daily clinical practice when the surgeon is called to identify the implant design according to residual supportive bone surfaces and consequently its fixation points.
In this study, we aim to describe a method of quantitative assessment of acetabular defects based on CT-scan 3D models that allow both an objective quantification and a visual output of the defect in the three 3 different planes: the axial, sagittal, and coronal planes. The methodology relies on the analysis of the residual bone stock of each main structural area of the acetabulum expressed as sectors, quantifying the ratio of bone surface loss compared to the healthy hemipelvis.
2. Material and Methods
The methodology was retrospectively applied on CT scans specimens of six patients selected from the data set of our institution. We included specimens of patients who underwent to THA revision surgery for aseptic loosening and were diagnosed with acetabular bone defects, with a contralateral healthy native hemipelvis. The CT scans were visually analyzed, and the acetabular defects were classified by two senior surgeons (AC and GM), according to the Paprosky Classification [
13] (
Table 1).
The provision of the CT-scans was approved by the teaching hospital ethic committee (Prot. PG/2021/9935).
The methodology consisted of three phases: (1)
pre-processing and mirroring, (2)
views and sector definition, and (3)
analysis (
Figure 1). The pre-processing included CT-scan acquisition, segmentation of bone structures and metal implants, and the mirroring of the healthy hemipelvis on a solid model of the pathological hemipelvis. In the
views and sector definition phase, three different planes were identified corresponding to a frontal view, a sagittal section view and an axial section view of the acetabulum. 4 different sectors corresponding to the main structural acetabular areas were identified on native pelvis and pathological pelvis. In the
analysis phase, measurements of bone loss in terms of areas of bone stock lost compared to the native acetabulum were made.
2.1. Pre-Processing and Mirroring
CT scans of the specimens included in the study were performed with a 3 mm slice thickness and a pixel size of 0.80 mm. During the acquisition, a preliminary metal artifacts protocol was applied using a MAR software (Smart Metal Artifact Reduction, GE Healthcare).
Digital Imaging and Communications in Medicine (DICOM) files of CT scans of the pelvises were imported into Mimics Innovation Suite 3D modelling software (version 23.0, Materialise, Leuven, Belgium). A single trained operator, GM, performed the further steps under clinical supervision of a senior surgeon, AC. Reduce scattering protocol was applied for residual metal artifact noise. Bony parts and metal implants were manually segmented obtaining three-dimensional separate objects of the two hemipelvis. Thresholding was manually edited to preserve both cortical and cancellous bone. After post-processing with filling techniques, smooth factor of 0.70 mm, and wrap factor of 1.0 mm, the 3D objects were exported as standard triangulation language (STL) mesh and processed in 3-Matic software (Materialise, Leuven, Belgium).
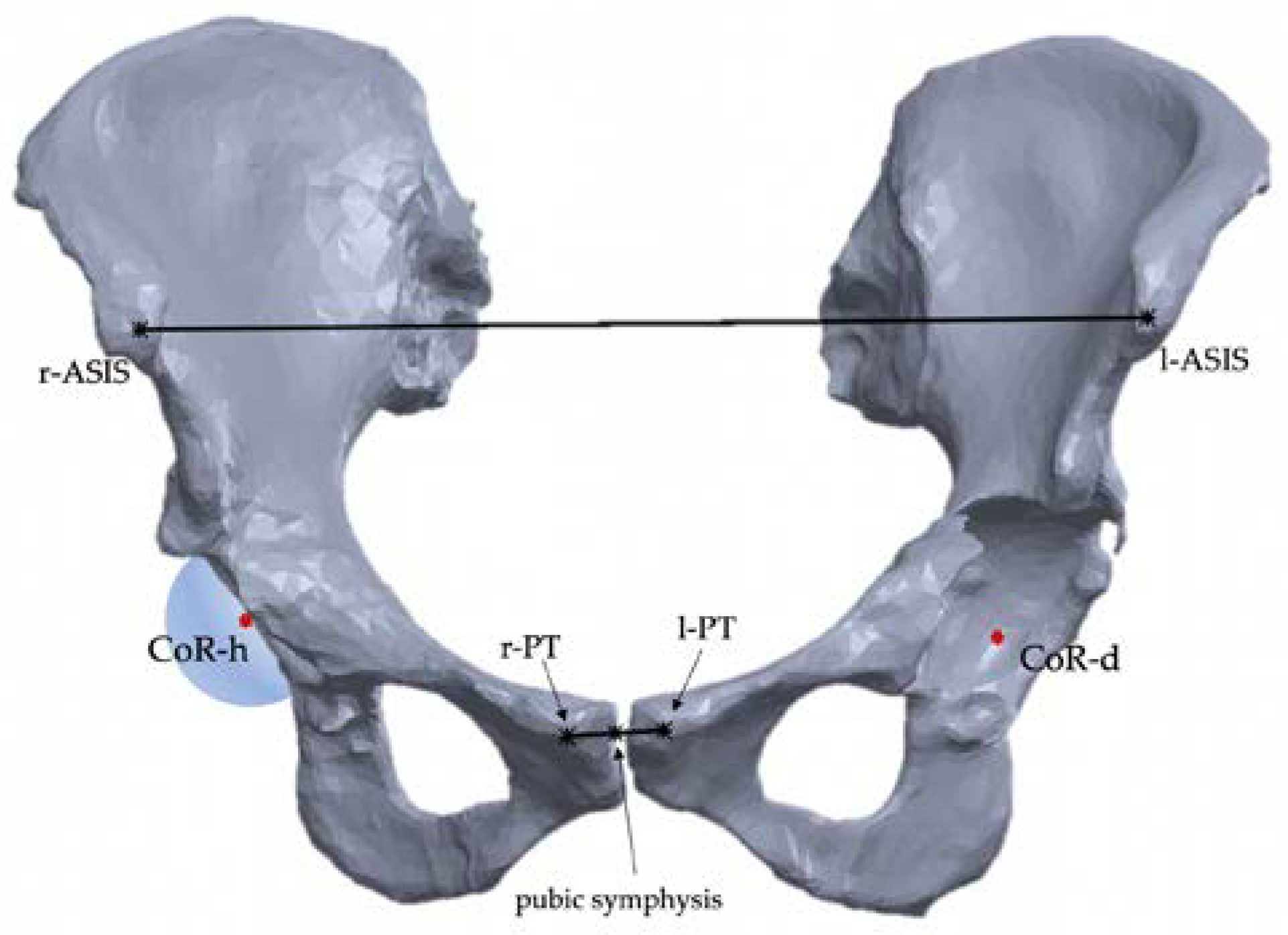
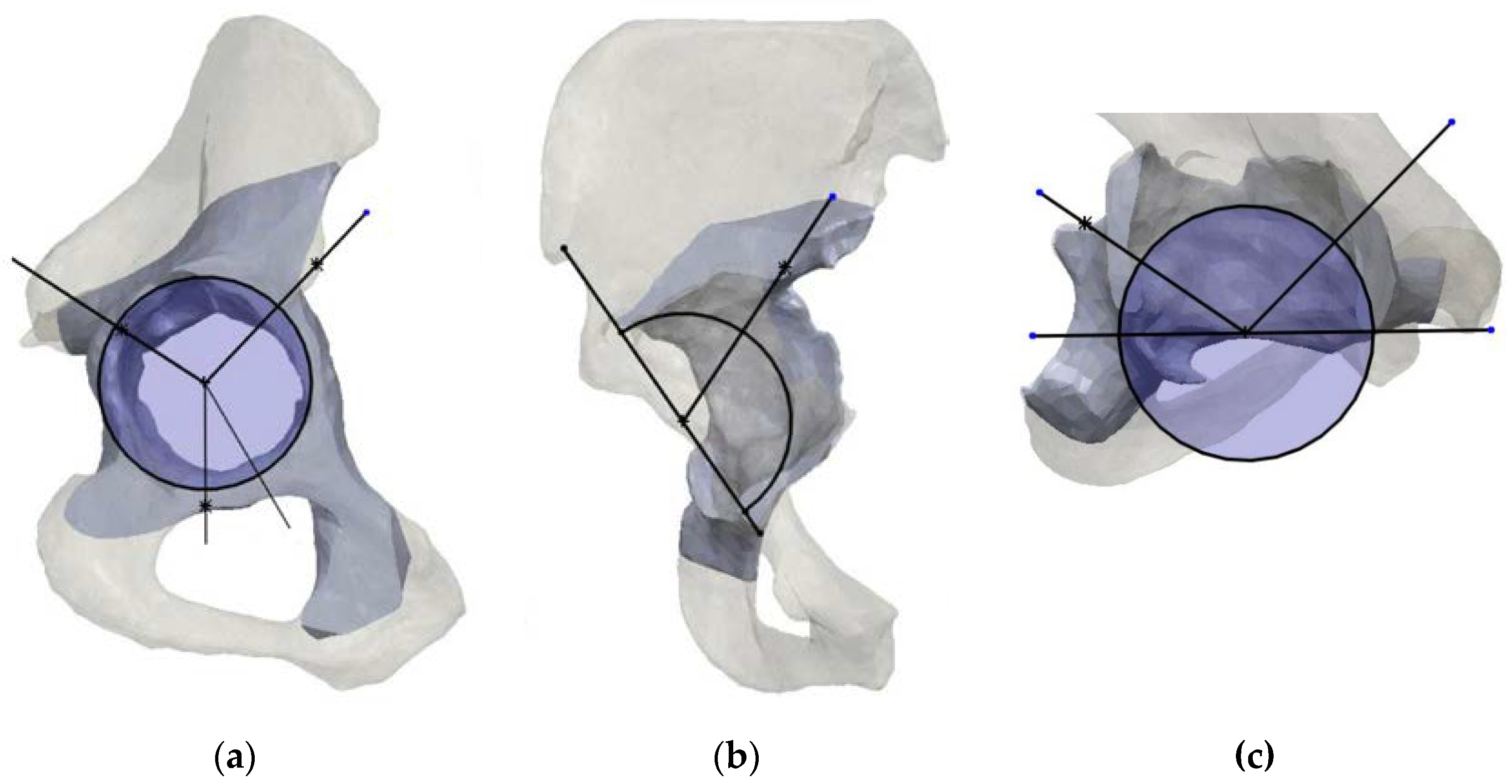
After mesh correction, a sphere was fitted lying on the acetabulum surface to identify the center of rotation of the native hip. Considering that the disrupted anatomy of the pathological hemipelvis could not allow to precisely identify the hip center of rotation, using the
mirroring tool the native hemipelvis was mirrored on the pathological side and so it was the native hip center of rotation (CoR), which represent a pivoting reference landmark for the classification system (
Figure 1)
2.2. Planes and Sectors Definition
In this phase, the acetabulum anatomical supporting structures, the posterior and anterior column, the superior dome, and medial wall were identified as 4 different sectors according to their clinical relevancy.
Starting on the healthy hemipelvis, the sectors were defined on 3 different planes: a frontal plane, a sagittal plane, and an axial plane, orthogonal to each other.
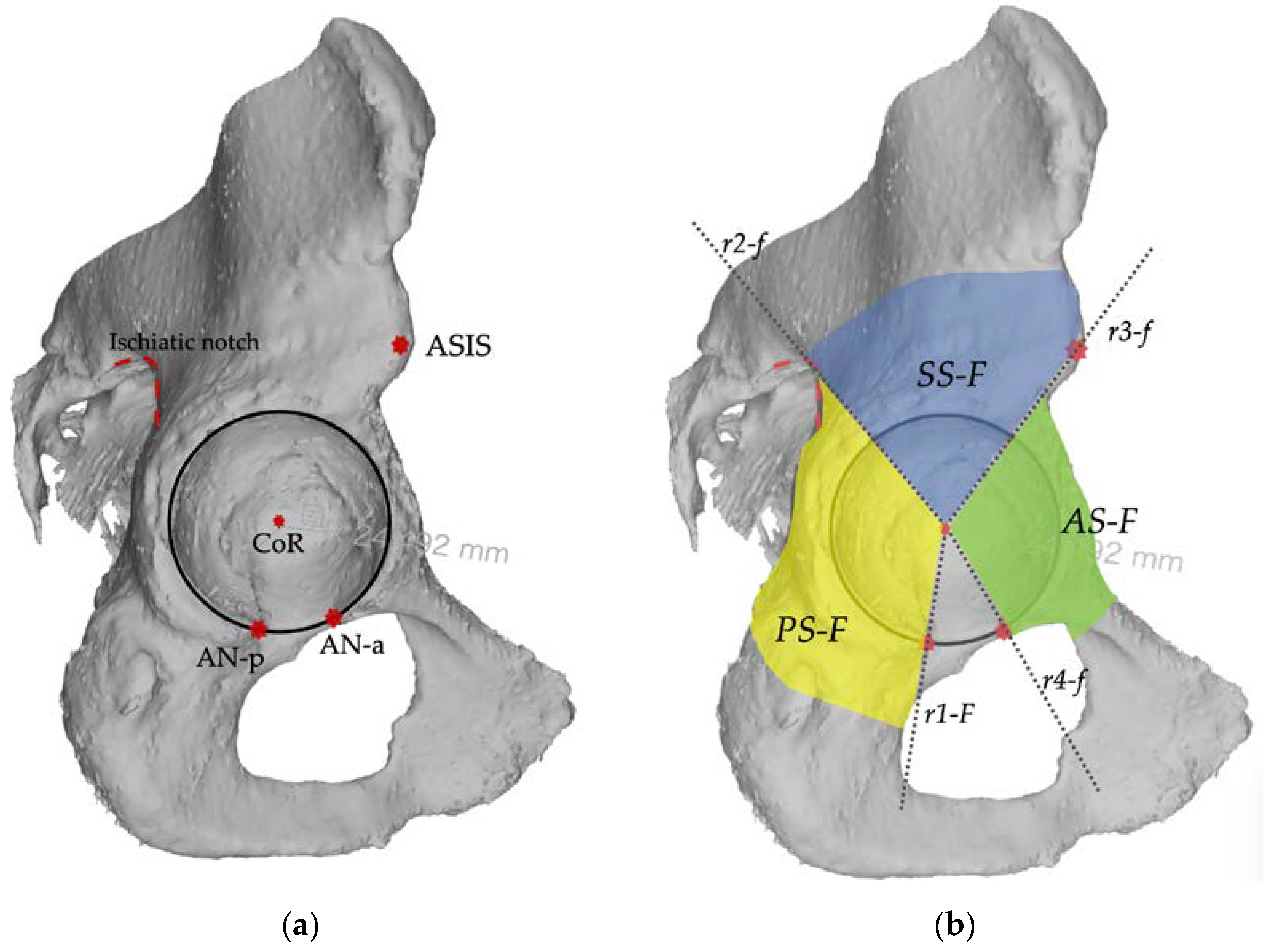
The frontal plane corresponded to the lateral anatomical view of the acetabulum and was defined by the acetabular rim border. In this plane, 3 sectors are identified including respectively the posterior column, the superior dome, and the anterior column. The posterior sector (PS-F) is defined by a line (r1-F) drawn caudally from the center of rotation to the projection of anterior aspect of the acetabular notch, by a line (r2-f) drawn cranially from the center of rotation (CoR) towards the projection of the ischiatic notch. The anterior sector (AS-F) is defined by a line (r3-F) drawn cranially from the center of rotation towards the projection of the anterior superior iliac spine (ASIS), a line (r4-F) drawn caudally from the center of rotation towards the projection of the posterior aspect of the acetabular notch. The superior sector (SS-F) is defined by line r2-F, line r3-F.
Figure 2.
Landmarks and sectors construction on the frontal plane (a) In the frontal plane view the landmarks for sectors description are identified: the acetabular rim (black circle), the Center of Rotation (CoR), the Anterior Superior Iliac Spine, the ischiatic notch (red dotted line), and the anterior and posterior aspect of acetabular notch (AN-p, AN-a); (b) In the frontal view four reference lines (r1-F, r2-F, r3-F, r4-F) are used to describe three sectors: the posterior (PS-F), the superior (SS-F) and the anterior (AS-F).
Figure 2.
Landmarks and sectors construction on the frontal plane (a) In the frontal plane view the landmarks for sectors description are identified: the acetabular rim (black circle), the Center of Rotation (CoR), the Anterior Superior Iliac Spine, the ischiatic notch (red dotted line), and the anterior and posterior aspect of acetabular notch (AN-p, AN-a); (b) In the frontal view four reference lines (r1-F, r2-F, r3-F, r4-F) are used to describe three sectors: the posterior (PS-F), the superior (SS-F) and the anterior (AS-F).
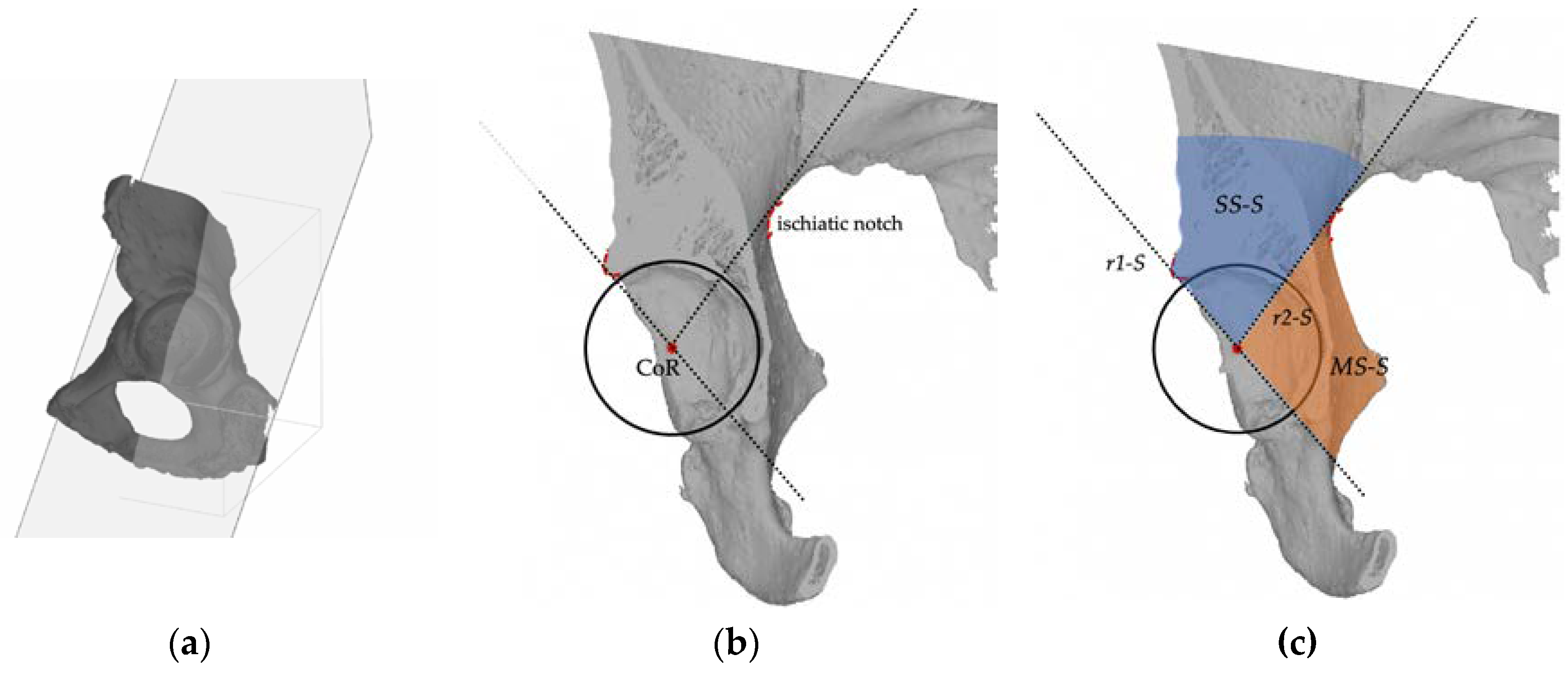
The sagittal plane is orthogonal to the frontal plane and lies on a straight line connecting the CoR and the 18 o’clock and 12 o’clock position around the acetabular rim as reference landmarks and crosses the medial wall and the acetabular superior dome. In this plane, 2 sectors are identified. The superior sector (SS-S) is defined by a line (r1-S) drawn from the center of rotation to the projection of the superior aspect of the acetabular rim, and by a line (r2-S) drawn posteriorly from the center of rotation (CoR) towards the projection of the ischiatic notch. The medial sector (MS-S) is defined by r2-S line and the caudal extension of r1-S line.
Figure 3.
(a) the sagittal plane crosses the acetabulum at 18 o’clock and 12 o’clock position (b) In the sagittal plane view the landmarks for sectors description are the acetabular rim (black circle), the Center of Rotation (CoR), the ischiatic notch (red dotted line), and the superior anterior margin of acetabular rim (red dotted line); (c) In the axial view two reference lines (r1-S, r2-S) are used to describe two sectors: the superior (SS-S), and the medial (MS-S).
Figure 3.
(a) the sagittal plane crosses the acetabulum at 18 o’clock and 12 o’clock position (b) In the sagittal plane view the landmarks for sectors description are the acetabular rim (black circle), the Center of Rotation (CoR), the ischiatic notch (red dotted line), and the superior anterior margin of acetabular rim (red dotted line); (c) In the axial view two reference lines (r1-S, r2-S) are used to describe two sectors: the superior (SS-S), and the medial (MS-S).
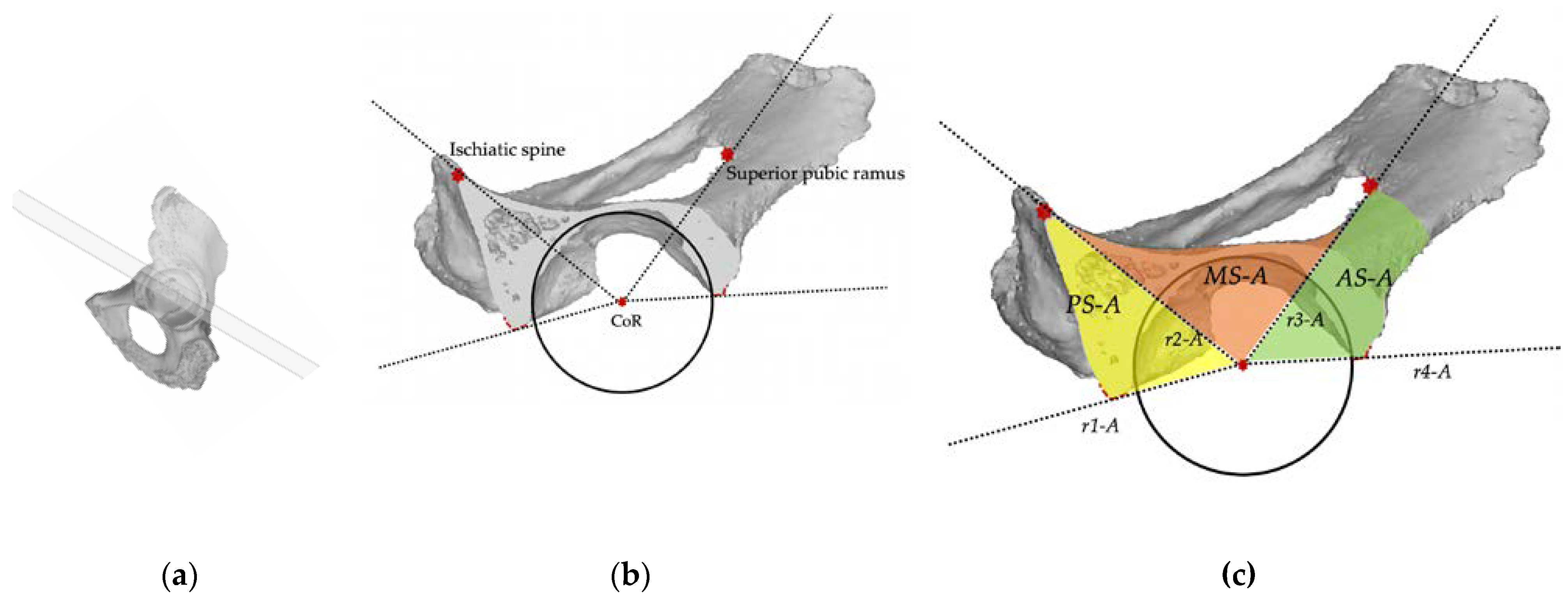
The axial plane is orthogonal to the sagittal plane and lies on a straight line connecting the CoR and the 09 o’clock and 15 o’clock position around the acetabular rim and crosses the posterior column, the medial wall, and anterior column. In this plane, 3 sectors are identified. The posterior sector (PS-A) is defined by a line (r1-A) drawn posteriorly from the center of rotation to the posterior acetabular rim, and other line (r2-A) drawn from the center of rotation (CoR) towards the projection of the posterior part of the superior pubic ramus connecting to the obturator foramen. The anterior sector (AS-A) is defined between a line (r3-A) drawn from the center of rotation towards the projection of the ischiatic spine (IS) and a line (r4-A) drawn from the center of rotation to the anterior acetabular rim. The medial sector (MS-A) is defined by line r2-A, line r3-A.
Figure 4.
(a) the axial plane crosses the acetabulum at the 09 o’clock and 15 o’clock position (b) In the sagittal plane view the landmarks for sectors description are the acetabular rim (black circle), the Center of Rotation (CoR), the ischiatic spine, and the anterior and posterior margin of acetabular rim (red dotted lines), and the the posterior part of the superior pubic ramus; (c) In the axial view four reference lines (r1-A, r2-A, r3-A, r4-A) are used to describe tree sectors: the posterior (PS-A), the medial (MS-A) and the anterior (AS-A).
Figure 4.
(a) the axial plane crosses the acetabulum at the 09 o’clock and 15 o’clock position (b) In the sagittal plane view the landmarks for sectors description are the acetabular rim (black circle), the Center of Rotation (CoR), the ischiatic spine, and the anterior and posterior margin of acetabular rim (red dotted lines), and the the posterior part of the superior pubic ramus; (c) In the axial view four reference lines (r1-A, r2-A, r3-A, r4-A) are used to describe tree sectors: the posterior (PS-A), the medial (MS-A) and the anterior (AS-A).
On the pathological side, the procedure is repeated using the mirrored native hip center of rotation as pivotal reference point and the remaining anatomical landmarks, as shown in
Figure 5.
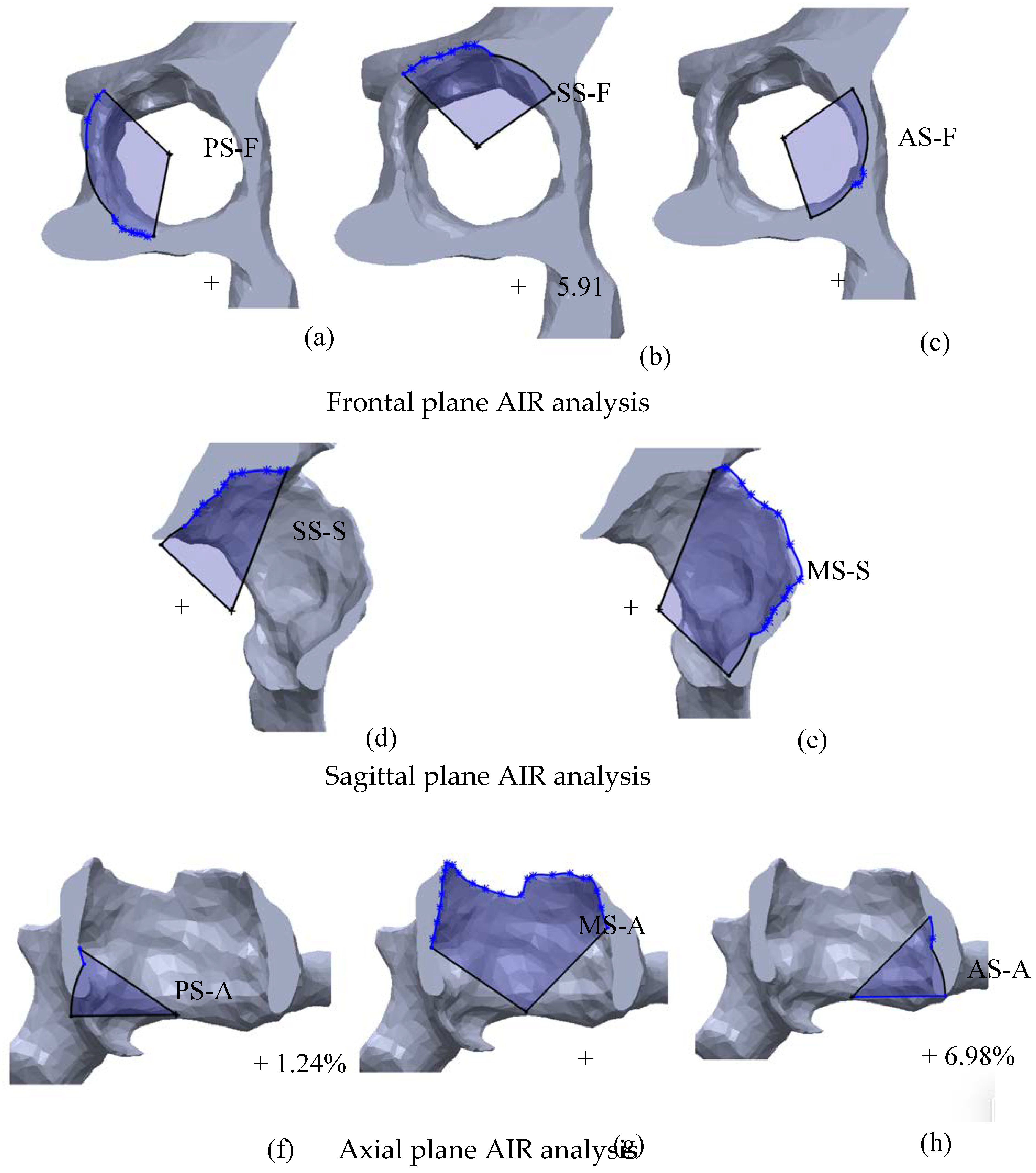
2.3. Analysis
In this phase, the different sectors are transformed in polygons using the acetabular rim as the third side of the polygon. The same procedure is repeated on the pathological side using the furthest borders of the bone defect as the third side. The areas of the sectors are then measured (mm
2), and the bone defect entity is expressed as the percentual increase of the defected sector area (
Adef) as compared to the corresponding healthy sector (
Anat), using this equation (
Figure 6):
Conversely, the percentual increase of the area represents the amount of bone loss occurred in a sector. Defects are then categorized in minimal, moderate, severe, massive according to the of area increase ratio (
AIR) values detected in each sector (
Table 2). The grading in minimal, moderate, severe, and massive was inspired by clinical consideration derived by most used classification systems [
8,
10,
13]and the thresholds as similarly proposed by Gelaude and Hettlich [
25,
26].
3. Results
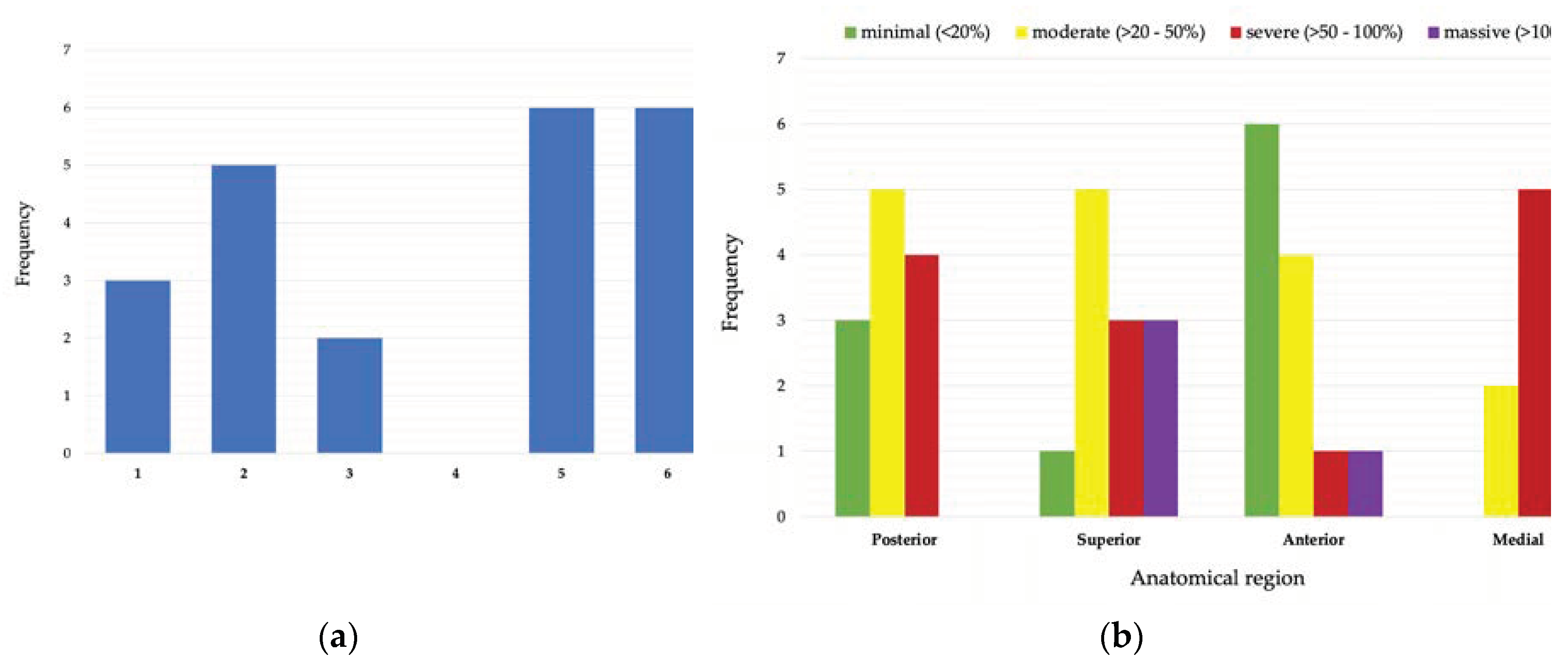
3.1. Quantitative Defect Assessment
The suggested method was applied on six exemplary specimens (
Table 3).
Acetabular rim diameters of the native hemipelvis ranged from 52 to 66 mm. Area Increase Ratio (AIR) between the native hemi-pelvis and the pathological hemi-pelvis was calculated for each sector; for a total of 48 single analysis. Minimal defects; ranging from 0 to +17,75% of AIR; were found in 11/48 (22.91%) sectors analyzed; while a moderate defect (range; +28.61% – +49.20%, AIR) was detected in 15/48 (31.25%) sectors. Severe defects (range; +109,02– +91.30%, AIR) was found in 13/48 (27,08%) sectors analyzed; while massive defects (range; +50.75 – +171.35%, AIR) were identified only in 9/48 (18.75%) sectors. Minimal defects were mostly localized in the anterior sectors (6/11; 54.54%). Most severe defects affected the posterior; superior and medial sectors (12/13; 92.30%). Massive defects were most likely located in superior and medial sectors (8/9; 88.88%). Only in one case a massive defect involved an anterior sector (
Figure 7)
3.2. Qualitative Defect Assessment
Specimen 1 and 3, showed a IIC Paprosky type that describe an acetabular defect with a distorted rim but intact supportive columns, and an all-medial migration of the implant. Similarly, the AIR analysis showed minimal defect for anterior and posterior sectors and a severe to massive defects in the medial sector. Additionally, in specimen 1, the sagittal plane showed a severe defect in the superior sector which wasn’t visible in the solely frontal analysis. This highlight that the analysis on two planes for each sector, is crucial to better understanding the defect’s morphology, extension, and severity. Specimen 2 and 6, showed a IIIB Paprosky type defect which is characterized by superior migration of the implant and severe posterior and medial osteolysis, with bone loss spanning from 9 o’clock to 5 o’clock position. AIR analysis showed, as well, massive defects located in superior and medial sectors and moderate to severe in the posterior sectors. In Specimen 4, a IIA Paprosky type, were found as expected only minimal and moderate AIR defects. Specimen 5 was classified as IIIA Paprosky type, which implies a severe superior migration of the implant and severe ischial and medial with bone loss 10 o’clock to 2 o’clock position.
4. Discussion
Paprosky classification represent the most common and recognized scheme, first offering a practical surgical algorithm that rely on the qualitative assessment of the integrity of the main supportive anatomical structure of the acetabulum[
13]. As the other most used acetabular defects classification systems, it relies on 2D radiographs, with poor results in terms of reliability and accuracy between preoperative planning and intraoperative findings[
14,
15,
16]. The development of modern diagnostic and tridimensional reconstruction techniques inspired different authors to use 3D models to anticipate the intraoperative reality and consequently develop new quantitative and reproducible classification methods[
20,
21,
24,
27]. Significant efforts were made to switch from a qualitative evaluation to a quantitative estimation of the bone defects. First, Gelaude et al, validated a methodology for the quantification of acetabular defects that relies on the volumetric analysis of bone loss and provides a schematic visual output of the defected acetabulum [
25]. Then, Hettlich et al. proposed a similar volumetric analysis adding an anatomic visual output of the lateral view of the acetabulum and identified different anatomical sectors. They highlighted the need for spatial information aside the volumetric value of bone loss, to assess the integrity of the main supporting structure of the acetabulum[
26]. Conversely, the solely visualization in the lateral view of the acetabulum do not offer an overall display of the morphology and extension of the defect, the most likely have erratic shapes, width and depth. Nevertheless, these methodologies showed the potential of 3D models analysis to improve the existing classification schemes as reported by Meynen et al. [
24].
Starting from these premises, we elaborated a methodology aiming to provide a quantitative assessment of acetabular defects associated to a visualization of the structural anatomical area of the acetabulum, in the three planes of the space. The methodology is based on the quantitative analysis of bone defects, expressed as the area of bone loss detected in the four main anatomical sectors of the acetabulum, first measured on a plane corresponding to the lateral anatomic view of the acetabulum (the frontal plane) and then two additional planes crossing the acetabulum (the sagittal and axial plane). In the frontal plane we analyzed the integrity of the acetabular rim and surrounding structures (posterior column, superior dome, and anterior column). The sagittal plane was meant to offer a comprehensive cross view of the superior dome and the supero-lateral or medial extension of the defect and integrity of the medial wall. The axial plane crosses the acetabulum at its equatorial level and shows the integrity of the mid part of the posterior and anterior column, and the medial wall. The reference landmarks we used to determine the sectors, were manually detected, and easily reproducible in both sides of all the specimens, allowing to border the sectors even when severe bone loss occurred.
We believe that the comparison of defected sector’s area to the healthy corresponding, using the raw square millimeter measure could be not efficient in representing the impact of a determined defect among acetabula of different dimensions. Therefore, the quantitative value was expressed as a Ratio of the Area Increase (AIR), and then graded in in minimal, moderate, severe, and massive to describe and scale different defect types according to patient-specific anatomy. The grading system was inspired by the most used classification systems, with the aim to offer an intuitive and feasible tool for clinical application[
8,
9,
10,
12,
13].
In our preliminary analysis, we found a majority of moderate and severe defected sectors (28/48, 58.3%) in the posterior and superior sectors. Minimal defects were found specially in anterior sectors (6/11, 54.5%) while massive defects mostly involved superior and medial sectors (8/9, 88.8%). This prevalence of moderate-severe defects was consistent with the severity of Paprosky types detected, all II and III types. Moreover, there was a visual correlation within the morphology of Paprosky types and AIR defects. Accordingly, AIR severe defects were found in posterior, superior and medial sectors. Interestlingly, completely different AIR gradings can coexist in the same hemipelvis: while a sector can massively be affected by bone loss another sector can be completely intact, suggesting that the methodology seem able to comprehensively describe the features of a defect acetabulum.
The proposed methodology has several limitations. First, we described the methodology only on specimens with a contralateral healthy hemipelvis, using “a mirroring technique”. In the future, the procedure will be applied to specimens with both defected hemipelvis with the support of statistical shape models (SSMs) as described by other authors[
22,
26]. The second limitation is the manual processing of the 3D models for metal artefacts reduction, segmentation, and landmarks identification. To be clinically feasible and to improve the accuracy of the method, some of these steps should be automated even with the support of artificial intelligence (AI). Third, the small number of specimens did not allow to validate the methodology, so further studies with larger samples are needed.
We believe that the main novelty and strength of our methodology is the change of focus from measuring the volume of bone loss to measuring the area of bone loss. Through the Area Increase Ratio (AIR), we described the defect as a “missing supporting surface”, offering a visual perception of morphology, location, and extent of the defect on three different spatial planes.
Nevertheless, the methodology needs to be validated in terms of accuracy and reliability. Further analysis could enhance the definition of defect categories and the grading system, especially for massive defects, as in the case of a multiple revision procedures or in the setting post-traumatic defects and oncologic surgery. Using SSMs technology, the methodology could be merged in 3D CT-based planning software for preoperative surgical decision making and support the development of new treatment algorithms including patient-specific surgical strategies.
Author Contributions
Conceptualization, G.M. and A.C.1; methodology, G.M; software, G.M.; validation, A.C.1, A.C.2 and G.M.; formal analysis, G.M.; investigation, A.C.; resources, A.C.; data curation, G.M.; writing—original draft preparation, G.M.; writing—review and editing, A.C.; visualization, G.M., A.C.1, A.C.2; supervision, A.C.1. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Cagliari State University (Prot. PG/2021/9935).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
We encourage all authors of articles published in MDPI journals to share their research data. In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Where no new data were created, or where data is unavailable due to privacy or ethical restrictions, a statement is still required. Suggested Data Availability Statements are available in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics.
Acknowledgments
not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Schwartz, A.M.; Farley, K.X.; Guild, G.N.; Bradbury, T.L. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2030. The Journal of Arthroplasty 2020, 35, S79–S85. [Google Scholar] [CrossRef]
- Erivan, R.; Villatte, G.; Dartus, J.; Reina, N.; Descamps, S.; Boisgard, S. Progression and Projection for Hip Surgery in France, 2008-2070: Epidemiologic Study with Trend and Projection Analysis. Orthopaedics & Traumatology: Surgery & Research 2019, 105, 1227–1235. [Google Scholar] [CrossRef]
- Yu, S.; Saleh, H.; Bolz, N.; Buza, J.; Iorio, R.; Rathod, P.A.; Schwarzkopf, R.; Deshmukh, A.J. Re-Revision Total Hip Arthroplasty: Epidemiology and Factors Associated with Outcomes. Journal of Clinical Orthopaedics and Trauma 2020, 11, 43–46. [Google Scholar] [CrossRef]
- Shichman, I.; Askew, N.; Habibi, A.; Nherera, L.; Macaulay, W.; Seyler, T.; Schwarzkopf, R. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2040-2060. Arthroplasty Today 2023, 21, 101152. [Google Scholar] [CrossRef] [PubMed]
- Marongiu, G.; Podda, D.; Mastio, M.; Capone, A. Long-Term Results of Isolated Acetabular Revisions with Reinforcement Rings: A 10- to 15-Year Follow-Up. HIP International 2019, 29, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Gu, J.; Zhou, Y. Primary Total Hip Arthroplasty Failure: Aseptic Loosening Remains the Most Common Cause of Revision. Am J Transl Res 2022, 14, 7080–7089. [Google Scholar] [PubMed]
- Paprosky, W.G.; Perona, P.G.; Lawrence, J.M. Acetabular Defect Classification and Surgical Reconstruction in Revision Arthroplasty. The Journal of Arthroplasty 1994, 9, 33–44. [Google Scholar] [CrossRef] [PubMed]
- D’Antonio, J.A.; Capello, W.N.; Borden, L.S.; Bargar, W.L.; Bierbaum, B.F.; Boettcher, W.G.; Steinberg, M.E.; Stulberg, S.D.; Wedge, J.H. Classification and Management of Acetabular Abnormalities in Total Hip Arthroplasty. Clin Orthop Relat Res 1989, 126–137. [Google Scholar] [CrossRef]
- Gross, A.E.; Allan, D.G.; Catre, M.; Garbuz, D.S.; Stockley, I. Bone Grafts in Hip Replacement Surgery. The Pelvic Side. Orthop Clin North Am 1993, 24, 679–695. [Google Scholar] [CrossRef]
- Saleh, K.J.; Holtzman, J.; Gafni, A.; Saleh, L.; Jaroszynski, G.; Wong, P.; Woodgate, I.; Davis, A.; Gross, A.E. Development, Test Reliability and Validation of a Classification for Revision Hip Arthroplasty. J. Orthop. Res. 2001, 19, 50–56. [Google Scholar] [CrossRef]
- Engh, C.A.; Glassman, A.H.; Griffin, W.L.; Mayer, J.G. Results of Cementless Revision for Failed Cemented Total Hip Arthroplasty. Clin Orthop Relat Res 1988, 91–110. [Google Scholar] [CrossRef]
- Gustilo, R.B.; Pasternak, H.S. Revision Total Hip Arthroplasty with Titanium Ingrowth Prosthesis and Bone Grafting for Failed Cemented Femoral Component Loosening. Clin Orthop Relat Res 1988, 111–119. [Google Scholar] [CrossRef]
- Paprosky, W.G.; Perona, P.G.; Lawrence, J.M. Acetabular Defect Classification and Surgical Reconstruction in Revision Arthroplasty. A 6-Year Follow-up Evaluation. J Arthroplasty 1994, 9, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Hofstaetter, J.G.; Sullivan, T.; Costi, K.; Howie, D.W.; Solomon, L.B. Validity and Reliability of the Paprosky Acetabular Defect Classification. Clin Orthop Relat Res 2013, 471, 2259–2265. [Google Scholar] [CrossRef]
- Gozzard, C.; Blom, A.; Taylor, A.; Smith, E.; Learmonth, I. A Comparison of the Reliability and Validity of Bone Stock Loss Classification Systems Used for Revision Hip Surgery. The Journal of Arthroplasty 2003, 18, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Gu, A.; Adriani, M.; Malahias, M.-A.; Fassihi, S.C.; Nocon, A.A.; Bostrom, M.P.; Sculco, P.K. Reliability and Validity of Acetabular and Femoral Bone Loss Classification Systems in Total Hip Arthroplasty: A Systematic Review. HSS Jrnl 2020, 16, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Horas, K.; Arnholdt, J.; Steinert, A.F.; Hoberg, M.; Rudert, M.; Holzapfel, B.M. Acetabular Defect Classification in Times of 3D Imaging and Patient-Specific Treatment Protocols. Orthopäde 2017, 46, 168–178. [Google Scholar] [CrossRef]
- Marongiu, G.; Prost, R.; Capone, A. A New Diagnostic Approach for Periprosthetic Acetabular Fractures Based on 3D Modeling: A Study Protocol. Diagnostics 2019, 10, 15. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos-Vaquinhas, A.; López-Torres, I.I.; Matas-Diez, J.A.; Calvo-Haro, J.A.; Vaquero, J.; Sanz-Ruiz, P. Improvement of Surgical Time and Functional Results after Do-It-Yourself 3D-Printed Model Preoperative Planning in Acetabular Defects Paprosky IIA-IIIB. Orthopaedics & Traumatology: Surgery & Research 2022, 108, 103277. [Google Scholar] [CrossRef]
- Zhang, J.; Liu, X.; Zeng, Y.; Zhai, Z.; Mao, Y.; Yu, D.; Wang, L.; Yan, M.; Zhu, Z.; Li, H. Comparison of 3D Printing Rapid Prototyping Technology with Traditional Radiographs in Evaluating Acetabular Defects in Revision Hip Arthroplasty: A Prospective and Consecutive Study. Orthopaedic Surgery 2021, 13, 1773–1780. [Google Scholar] [CrossRef]
- Zhang, J.; Hu, Y.; Ying, H.; Mao, Y.; Zhu, Z.; Li, H. Reliability and Validity Test of a Novel Three-Dimensional Acetabular Bone Defect Classification System Aided with Additive Manufacturing. BMC Musculoskelet Disord 2022, 23, 432. [Google Scholar] [CrossRef] [PubMed]
- Meynen, A.; Vles, G.; Zadpoor, A.A.; Mulier, M.; Scheys, L. The Morphological Variation of Acetabular Defects in Revision Total Hip Arthroplasty—A Statistical Shape Modeling Approach. Journal Orthopaedic Research 2021, 39, 2419–2427. [Google Scholar] [CrossRef] [PubMed]
- Wirtz, D.C.; Jaenisch, M.; Osterhaus, T.A.; Gathen, M.; Wimmer, M.; Randau, T.M.; Schildberg, F.A.; Rössler, P.P. Acetabular Defects in Revision Hip Arthroplasty: A Therapy-Oriented Classification. Arch Orthop Trauma Surg 2020, 140, 815–825. [Google Scholar] [CrossRef] [PubMed]
- Meynen, A.; Vles, G.; Roussot, M.; Van Eemeren, A.; Wafa, H.; Mulier, M.; Scheys, L. Advanced Quantitative 3D Imaging Improves the Reliability of the Classification of Acetabular Defects. Arch Orthop Trauma Surg 2022, 143, 1611–1617. [Google Scholar] [CrossRef] [PubMed]
- Gelaude, F.; Clijmans, T.; Delport, H. Quantitative Computerized Assessment of the Degree of Acetabular Bone Deficiency: Total Radial Acetabular Bone Loss (TrABL). Advances in Orthopedics 2011, 2011, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hettich, G.; Schierjott, R.A.; Ramm, H.; Graichen, H.; Jansson, V.; Rudert, M.; Traina, F.; Grupp, T.M. Method for Quantitative Assessment of Acetabular Bone Defects. Journal Orthopaedic Research 2019, 37, 181–189. [Google Scholar] [CrossRef]
- Schierjott, R.A.; Hettich, G.; Graichen, H.; Jansson, V.; Rudert, M.; Traina, F.; Weber, P.; Grupp, T.M. Quantitative Assessment of Acetabular Bone Defects: A Study of 50 Computed Tomography Data Sets. PLoS ONE 2019, 14, e0222511. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).