Submitted:
08 April 2024
Posted:
09 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Mechanism of Plant-Based in Decreasing Incidence, Morbidity, and Mortality of COVID-19
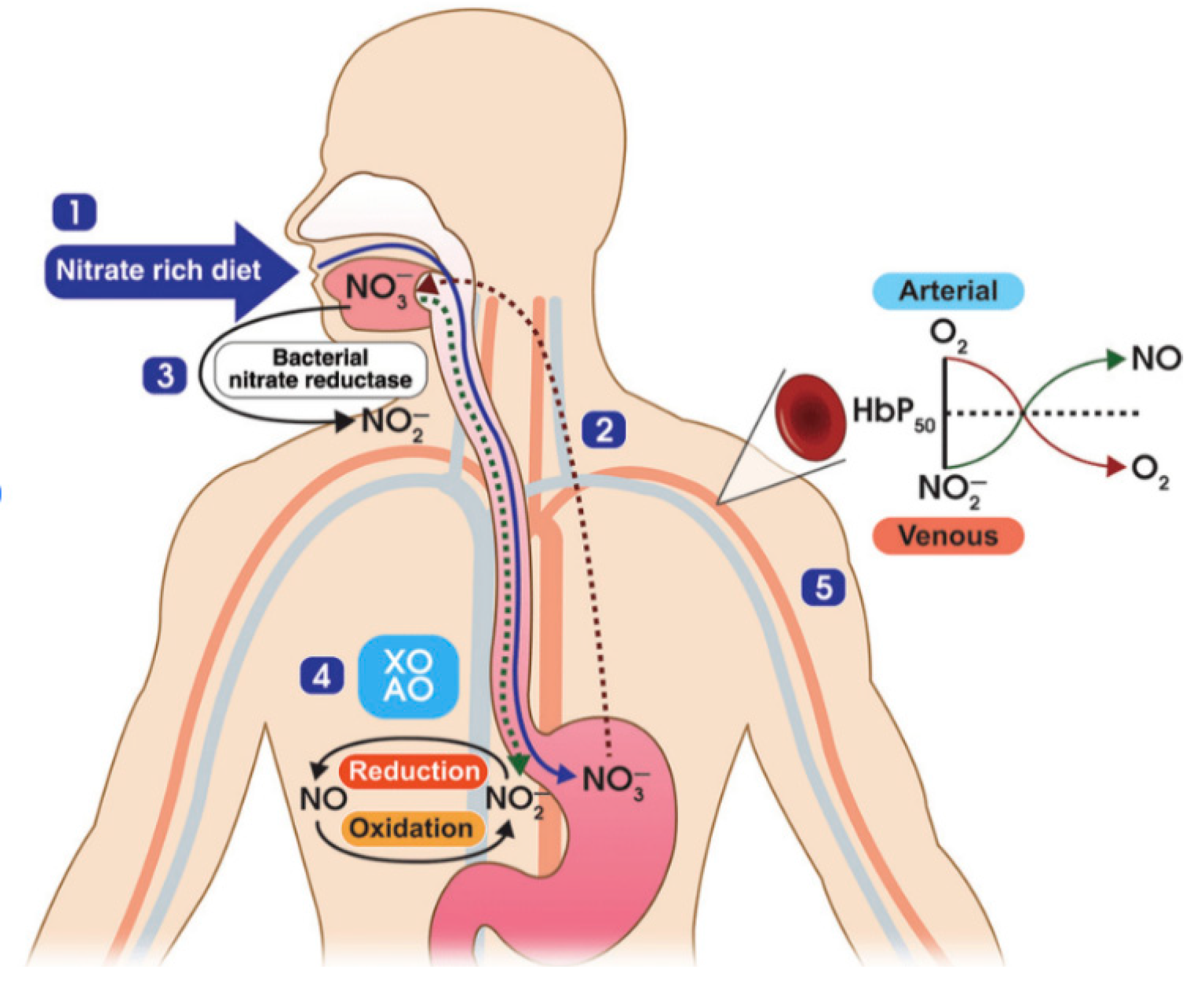
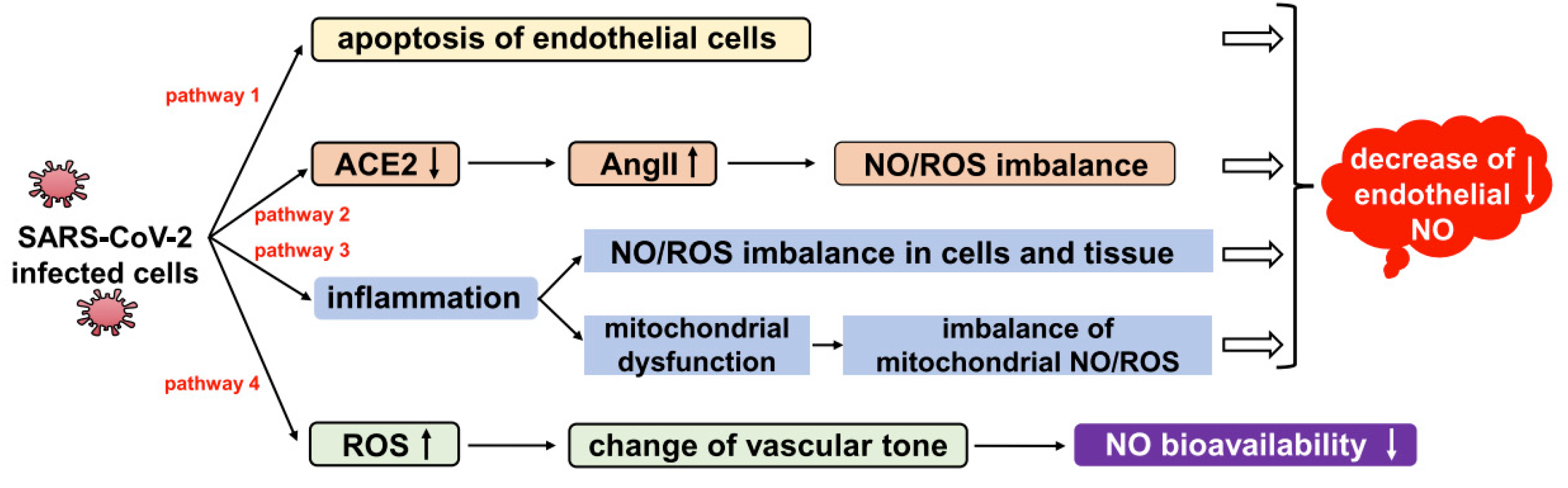
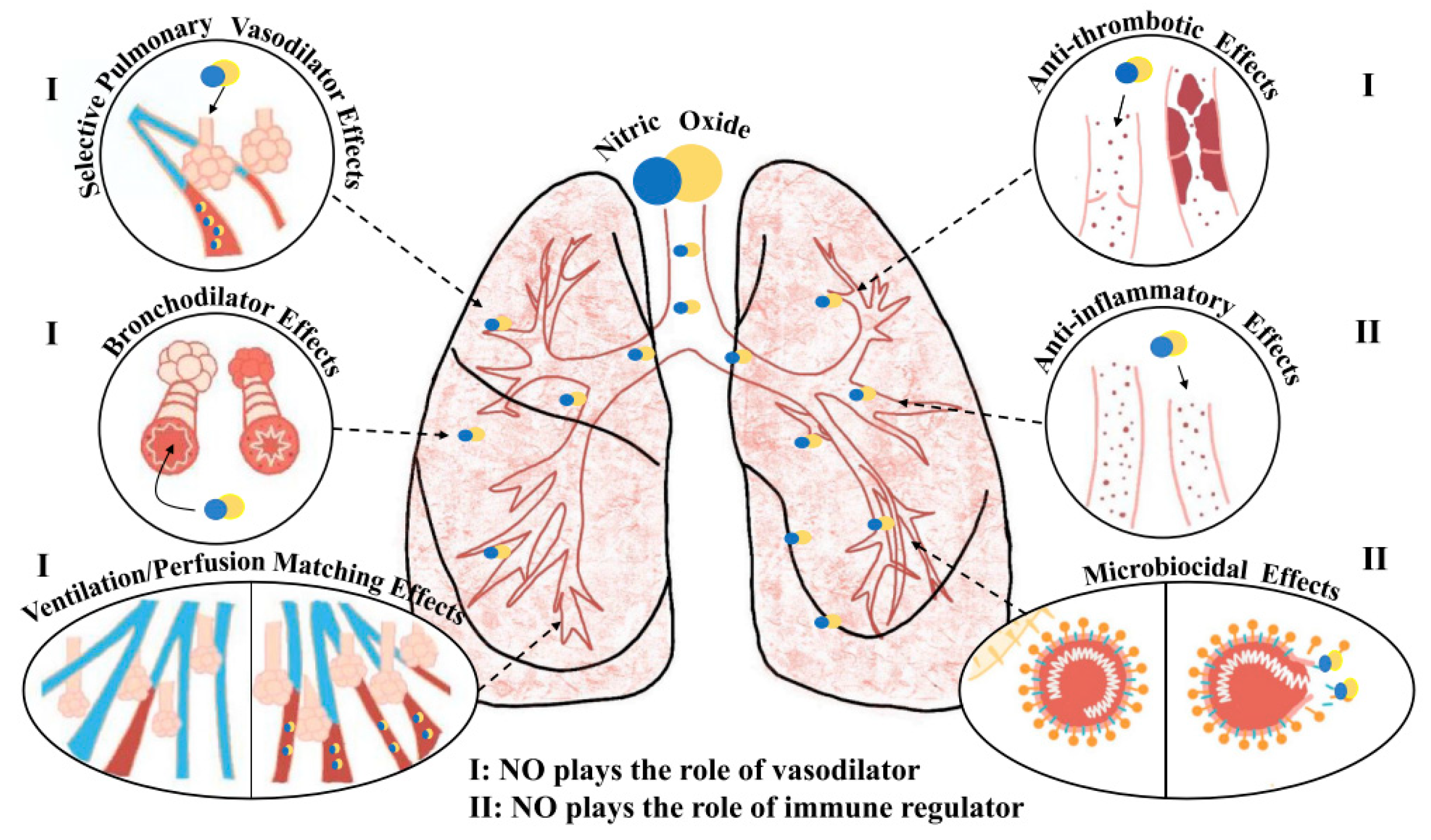
2.1. Mechanism of NO in Fighting Coronavirus
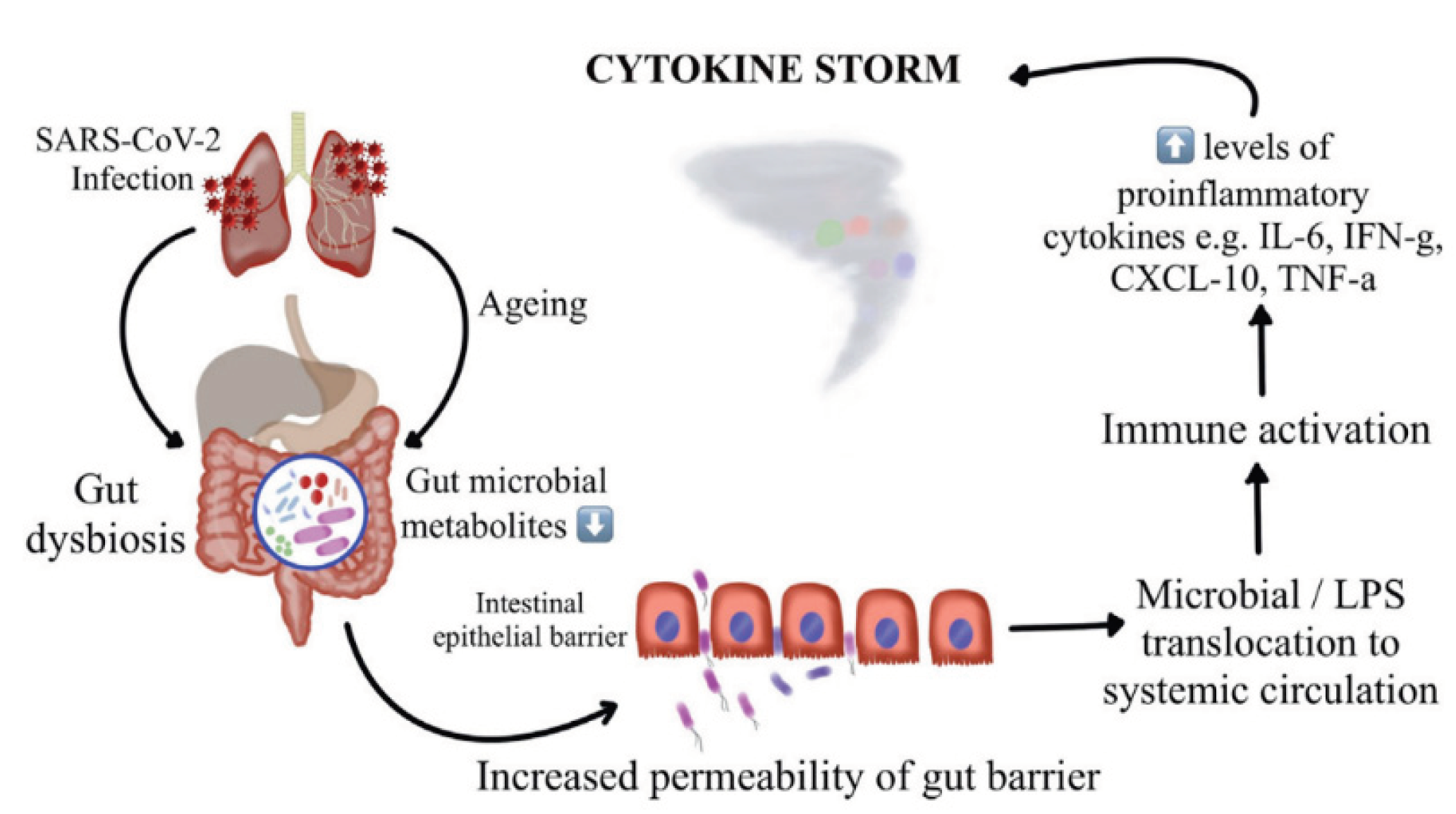
2.2. The Role of Microbiota in Coronavirus
2.3. Mechanism of Inflammation and Endothelial Dysfunction in Coronavirus
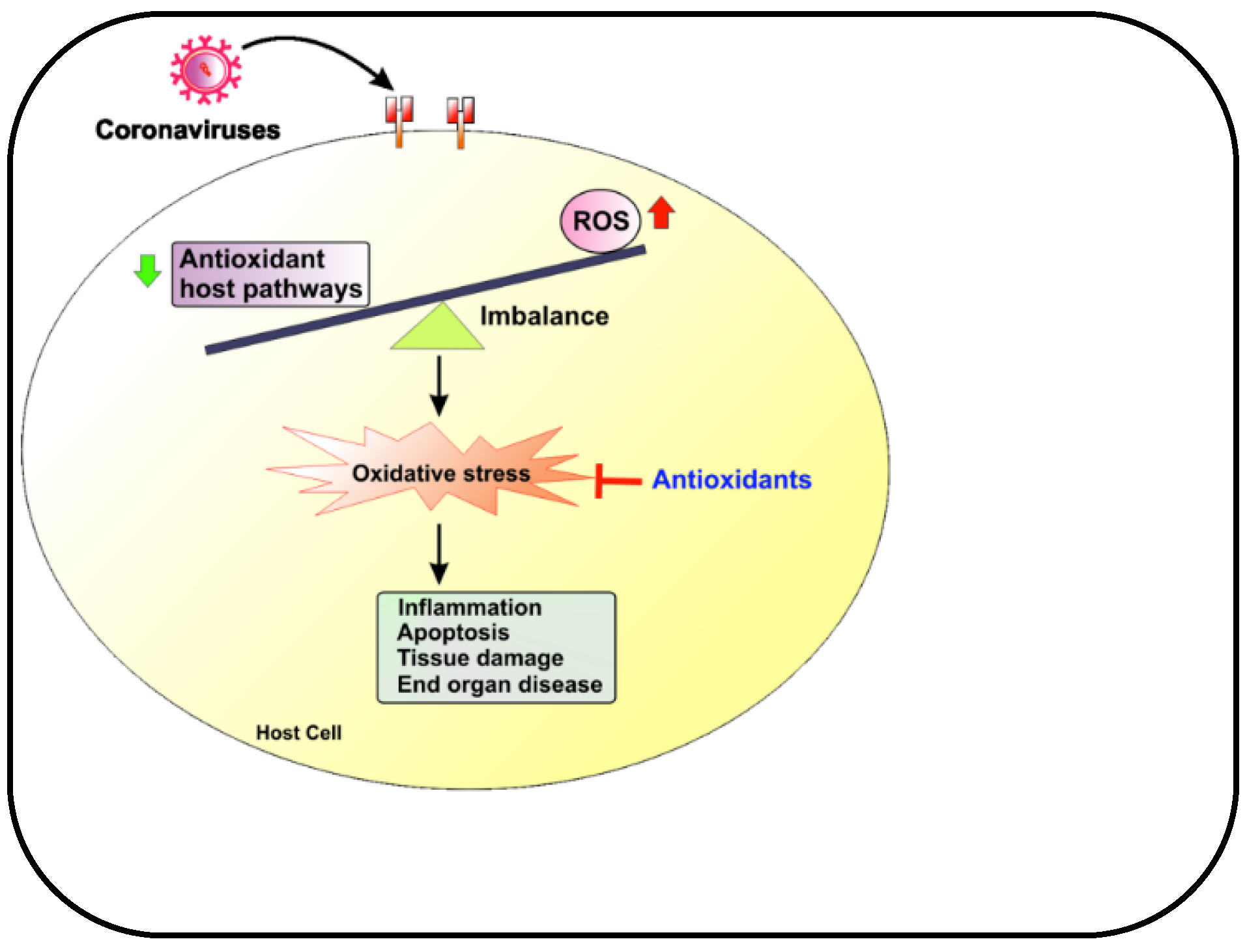
2.4. Role of Oxidative Stress in Coronavirus
2.5. The Link between Mitochondria Health and COVID-19 Severity and Mortality
2.6. Potential Benefits of Telomere Manipulation in Coronavirus Treatment
2.7. Caloric Restriction is Emerging As an Essential Factor in the Fight Against Inflammation
3. Supplements Their Significant Role in Managing COVID-19
3.1. Vitamin C
3.2. Vitamin D
3.3. Vitamin B3, Precursor of NAD+
3.4. Zinc
3.5. Copper
3.6. Selenium
3.7. Coenzyme Q10 (CoQ10)
3.8. Astaxanthin
3.9. Quercetin
3.10. Curcumin
3.11. Taurine
4. Healthy Lifestyles Their Significant Role in Managing the COVID-19 Pandemic
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wang, P.; Song, M.; Eliassen, A.H.; Wang, M.; Fung, T.T.; Clinton, S.K.; Rimm, E.B.; Hu, F.B.; Willett, W.C.; Tabung, F.K.; Giovannucci, E.L. Optimal dietary patterns for prevention of chronic disease. Nat Med. Erratum in: Nat Med. 2024. 2023, 29, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Peña-Jorquera, H.; Cid-Jofré, V.; Landaeta-Diaz, L.; et al. Plant-Based Nutrition: Exploring Health Benefits for Atherosclerosis, Chronic Diseases, and Metabolic Syndrome- A Comprehensive Review. Nutrients 2023, 15, 3244. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Rebholz, C.M.; Hedge, S.; et al. Plant-based diets, pescatarian diets and COVID-19 severity: a population-based case-control study in six countries. BMJ Nutrition, Prevention & Health. 2021, 4, e000272. [Google Scholar]
- Oboza, P.; Ogarek, N. The main causes of death in patients with COVID-19. Eur Rev Med Pharmacol Sci. 2023, 27, 2165–2172. [Google Scholar]
- Dessie, Z.G.; Zewotir, T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021, 21, 855. [Google Scholar] [CrossRef]
- Gupta, S.C.; Prasad, S.; Aggarwal, BB. Anti-inflammatory Nutraceuticals and Chronic Diseases. Advances in Experimental Medicine and Biology. 2016. [CrossRef]
- Chojnacka, K.; Skrzypczak, D.; Izydorczyk, G.; et al. Antiviral Properties of Polyphenols from Plants. Foods. 2021, 10, 2277. [Google Scholar] [CrossRef] [PubMed]
- Alesci, A.; Aragona, M.; Cicero, N.; et al. Can nutraceuticals assist treatment and improve covid-19 symptoms? Natural Product Research. [CrossRef]
- Alam, S.; Sarker, M.R.; Afrin, S. Traditional Herbal Medicines, Bioactive Metabolites, and Plant Products Against COVID-19: Update on Clinical Trials and Mechanism of Actions. Frontiers in Pharmacology 2021, 12, 671498. [Google Scholar] [CrossRef]
- Loscalzo, J.; Welch, G. Nitric Oxide and its role in cardiovascular system. Prog Cardiovasc Dis. 1995, 38, 87–104. [Google Scholar] [CrossRef]
- Cannon, R.O. , 3rd. Role of nitric oxide in cardiovascular disease: focus on the endothelium. Clin Chem. 1998, 44, 1809–1819. [Google Scholar] [CrossRef]
- Torregrossa, A.C.; Aranke, M.; Bryan, NS. Nitric Oxide and geriatrics: Implications in diagnostics and treatment of the elderly. J Geriatr Cardiol. 2011, 8, 230–242. [Google Scholar] [PubMed]
- Nikolaidis, A.; Kramer, R.; Ostojic, S. Nitric Oxide: The Missing Factor in COVID-19 Severity? Med Sci (Basel). 2022, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Flaxman, S.; Whittaker, C.; Semenova, E.; et al. Assessment of COVID-19 as the Underlying Cause of Death Among Children and Young People Aged 0 to 19 Years in the US. JAMA Netw Open. 2023, 6, e2253590. [Google Scholar] [CrossRef] [PubMed]
- Babateen, A.; Shannon, O.; Mathers, J.C.; et al. Validity and reliability of test strips for the measurement of salivary nitrite concentration with and without the use of mouthwash in healthy adults. Nitric Oxide. 2019, 91. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, J.; Ohtake, K.; Uchida, H. NO-Rich Diet for Lifestyle-Related Diseases. Nutrients. 2015, 7, 4911–4937. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, S.; Shen, X.; Glawe, J.D.; et al. Nitric Oxide and Hydrogen Sulfide Regulation of Ischemic Vascular Growth and Remodeling. Chapter in Comprehensive Physiology. 3337. [Google Scholar]
- Fang, W.; Jiang, J.; Su, L.; et al. The role of NO in COVID-19 and potential therapeutic strategies. Free Radical Biology and Medicine. 2021, 163, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Ritz, T.; Trueba, A.F.; Vogel, P.D.; et al. Exhaled nitric oxide and vascular endothelial growth factor as predictors of cold symptoms after stress. Biol Psychol. 2018, 132, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, J.S.; Aldhahir, A.M.; Al Ghamdi, S.S.; et al. Inhaled Nitric Oxide for Clinical Management of COVID-19: A Systematic Review and Meta-Analysis. Int J Environ Public Health. 2022, 19, 12803. [Google Scholar] [CrossRef]
- Mir, J.M.; Maurya, RC. Nitric oxide as a therapeutic option for COVID-19 treatment: a concise perspective. New J Chem. 2021, 45, 1774. [Google Scholar] [CrossRef]
- Wiertsema, S.P.; van Bergenhenegouwen, J.; Garssen, J.; et al. The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients. 2021, 13, 886. [Google Scholar] [CrossRef]
- Dumas, A.; Bernard, J.; Poquet, Y.; et al. The role of the lung microbiota and the gut-lung axis in respiratory infectious diseases. Cell Microbiol. 2018, 20, e12966. [Google Scholar] [CrossRef] [PubMed]
- Vijay, A.; Valdes, AM. Role of the gut microbiome in chronic diseases: a narrative review. European Journal of Clinical Nutrition. 2022, 76, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Vignesh, R.; Swathirajan, C.R. ; Tun Z-H, et al. Could Perturbation of Gut Microbiota Possibly Exacerbate the Severity of COVID-19 via Cytokine Storm? Frontiers in Immunology. 2021, 11, 607734. [Google Scholar]
- Budden, K.F.; Gellatly, S.L.; Wood, D.L.A.; et al. Emerging pathogenic links between microbiota and the gut-lung axis. Nat Rev Microbiol. 2017, 15, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Dang, A.t.; Marsland, B.J. Microbes, metabolites, and gut-lung axis. Mucosal Immunol. 2019, 12, 843–50. [Google Scholar] [CrossRef] [PubMed]
- Ramatillah, D.L.; Gan, S.-H.; Pratiwi, I. ; et al. Impact of cytokine storm on severity of COVID-19 disease in a private hospital in West Jakarta prior to vaccination. PloS One. 2022, 17, e0262438. [Google Scholar] [CrossRef] [PubMed]
- Du, R.-H.; Liang, L.-R.; Yang, C.-Q.; et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020, 56, 3. [Google Scholar] [CrossRef] [PubMed]
- Groves, H.T.; Higham, S.L.; Moffatt, M.F.; et al. Respiratory Viral Infection Alters the Gut Microbiota by Inducing Inappetence. mBio. 2020, 11, 1. [Google Scholar] [CrossRef]
- Gou, W.; Fu, Y.; Yue, L.; et al. Gut microbiota may underlie the predisposition of healthy individuals to COVID-19. MedRxiv. 2020, 22, 20076091. [Google Scholar]
- Vignesh, R.; Swathirajan, C.R.; Tun, Z.-H.; et al. Could Perturbation of Gut Microbiota Possibly Exacerbate the Severity of COVID-19 via Cytokine Storm? Frontiers in Immunology. 2021, 11, 607734. [Google Scholar] [CrossRef]
- Abadi, M.S.S.; Kodashahi, R.; Aliakbarian, M.; et al. The Association Between the Gut Microbiome and COVID-19 Severity: The Potential Role of TMAO Produced by the Gut Microbiome. Archives of Clinical Infectious Diseases. 2024, 18, e140346. [Google Scholar]
- Foster, J.A.; Baker, G.B.; Dursun, SM. The Relationship Between the Gut Microbiome- Immune System-Brain Axis and Major Depressive Disorder. Front Neurol. 2021, 12, 721126. [Google Scholar] [CrossRef] [PubMed]
- Kamo, T.; Akazawa, H.; Suda, W.; et al. Dysbiosis and compositional alterations with aging in the gut microbiota of patients with heart failure. PloS One. 2017, 12, e0174099. [Google Scholar] [CrossRef] [PubMed]
- Leeming, E.R.; Johnson, A.J.; Spector, T.D.; et al. Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients. 2019, 11, 2862. [Google Scholar] [CrossRef] [PubMed]
- Craddock, J.C.; Neale, E.P.; Peoples, G.E.; et al. Vegetarian-Based Dietary Patterns and their Relation with Inflammatory and Immune Biomarkers: A Systematic Review and Meta-Analysis. Advances in Nutrition. 2019, 10, 433–451. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, S.R.K.; Kok, C.-W.; Kunasegaran, T. ; et al. Effect of Plant-Based Diets on Gut Microbiota: A Systematic Review of Interventional Studies. Nutrients. 2023, 15, 1510. [Google Scholar] [CrossRef] [PubMed]
- Hibino, S.; Hayashida, K. Modifiable Host Factors for the Prevention and Treatment of COVID-19: Diet and Lifestyle/ Diet and Lifestyle Factors in the Prevention of COVID-19. Nutrients. 2022, 14, 1876. [Google Scholar] [CrossRef] [PubMed]
- Dovignoan, J.; Ganz, P. Role of Endothelial Dysfunction in Atherosclerosis. Circulation. 2004, 109, III–27. [Google Scholar] [CrossRef] [PubMed]
- Akinrinmade, A.O.; Obitulata-Uqwu, V.O.; Obijiofor, N.B.; et al. COVID-19 and Acute Coronary Syndrome: A Literature Review. Cureus. 2022, 14, e29747. [Google Scholar] [CrossRef]
- Margina, D.; Ungurianu, A.; Purdel, C.; et al. Chronic Inflammation in the Context of Everyday Life: Dietary Changes as Mitigating Factors. Int J Environ Res Public Health. 2020, 17, 4135. [Google Scholar] [CrossRef]
- Hojyo, S.; Uchida, M.; Tanaka, K.; et al. How COVID-19 induces cytokine storm with high mortality. Inflamm Regen. 2020, 40, 37. [Google Scholar] [CrossRef]
- Moludi, J.; Qaisar, S.A.; Alizadeh, M.; et al. The relationship between Dietary Inflammatory Index and disease severity and inflammatory status: a case-control study of COVID-19 patients. British Journal of Nutrition. 2021, 1–9. [Google Scholar] [CrossRef]
- Zhao, L.; Wirth, M.D.; Petermann-Rocha, F.; et al. Diet-Related Inflammation Is Associated with Worse COVID-19 Outcomes in the UK Biobank Cohort. Nutrients. 2023, 15, 884. [Google Scholar] [CrossRef] [PubMed]
- Paraiso, I.L.; Revel, J.S.; Stevens, JF. Potential use of polyphenols in the battle against COVID-Current Opinion in Food. Science. 2020, 32, 149–155. [Google Scholar]
- Wang, Y.; Uffelman, C.; Hill, E. The Effects of Red Meat Intake on Inflammation Biomarkers in Humans: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Curr Dev Nutr. 2022, 6 (Suppl. S1), 994. [Google Scholar] [CrossRef]
- Hofseth, L.J.; Hébert, J.R. Chapter 3- Diet and acute and chronic, systemic, low-grade inflammation. Diet, Inflammation, and Health. 2022; 85–111. [Google Scholar]
- Buck, A.N.; Vincent, H.K.; Newman, CB. Evidence-Based Dietary Practices to Improve Osteoarthritis Symptoms: An Umbrella Review. Nutrients. 2023, 15, 3050. [Google Scholar] [CrossRef] [PubMed]
- Gain, C.; Song, S.; Angtuaco, T.; et al. The role of oxidative stress in the pathogenesis of infections with coronavirus. Frontiers in Microbiology. [CrossRef]
- Li, M.; Zhu, D.; Yang, J.; et al. Clinical treatment experience in severe and critical COVID-19. Mediat Inflamm. 2021, 9924542. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.S.; Czajkowsky, DM. SARS-CoV-2 infection and oxidative stress: pathophysiology insight into thrombosis and therapeutic opportunities. Cytokine Growth Factor Rev. 2022, 63, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Gorni, D.; Finco, A. Oxidative stress in elderly population: A prevention screening study. Aging medicine. 2020, 3, 205–213. [Google Scholar] [CrossRef]
- Al-Zahrani, J. SARS-CoV-2 associated COVID-19 in geriatric population: A brief narrative review. Saudi Journal of Biological Sciences. 2021, 28, 738–743. [Google Scholar] [CrossRef]
- Macho-Gonzáles, A.; Garcimartín, A.; López-Oliva, M.E.; et al. Can Meat and Meat-Products Induce Oxidative Stress? Antioxidants. 2020, 9, 638. [Google Scholar] [CrossRef] [PubMed]
- Macho-Gonzáles, A.; Bastida, S.; Garcimartín, A.; et al. Functional Meat Products as Oxidative Stress Modulators: A Review. Advances in Nutrition. 2021, 12, 1514–1539. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrova, K.; Koelman, L.; Rodrigues, CE. Dietary patterns and biomarkers of oxidative stress and inflammation: A systematic review of observational and intervention studies. Redox Biology. 2021, 42, 101869. [Google Scholar] [CrossRef] [PubMed]
- Baghaei-Yazdi, N.; Bahmaie, M.; Abhari, FM. The Role of plant-derived natural antioxidants in reduction of oxidative stress. BioFactors. 2022, 1–23. [Google Scholar]
- Marchi, S.; Guilbaud, E.; Galluzzi, L. Mitochondrial control of inflammation. Nature Reviews Immunology. 2023, 23, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Ciccarelli, G.; Conte, S.; Cimmino, G.; et al. Mitochondrial Dysfunction: The Hidden Player in the Pathogenesis of Atherosclerosis? Int J Mol Sci. 2023, 24, 1086. [Google Scholar] [CrossRef] [PubMed]
- Shoraka, S.; Samarasinghe, A.E.; Ghaemi, A.; et al. Host mitochondria: more than an organelle in SARS-CoV-2 infection. Frontiers in Cellular and Infection Microbiology. [CrossRef]
- Junqueira, C.; Crespo, A.; Lieberman, J.; et al. FcyR-mediated SARS-CoV-2 infection of monocytes activates inflammation. Nature. 2022, 606, 576–584. [Google Scholar] [CrossRef]
- Khalil, M.; Shanmugam, H.; Abdallah, H.; et al. The Potential of the Mediterranean Diet to Improve Mitochondrial Function in Experimental Models of Obesity and Metabolic Syndrome. Nutrients. 2022, 14, 3112. [Google Scholar] [CrossRef] [PubMed]
- Pollicino, F.; Veronese, N.; Dominguez, L.; et al. Mediterranean diet and mitochondria: New findings. Experimental Gerontology. 2023, 176, 112165. [Google Scholar] [CrossRef]
- Kyriazis, I.D.; Vassi, E.; Alvanou, M.; et al. The impact of diet upon mitochondrial physiology (Review). International Journal of Molecular Medicine. 2022, 50, 135. [Google Scholar] [CrossRef]
- Ahmad, F.B.; Cisewski, J.A.; Miniño, A.; et al. Provisional Mortality Data- United States. MMWR Morb Mortal Wkly Rep. 2021, 70, 519–522. [Google Scholar] [CrossRef]
- Stokes, E.K.; Zambrano, L.D.; Anderson, K.N.; et al. Coronavirus Disease 2019 Case Surveillance—United States, January 22-May 30. MMWR Morb Mortal Wkly Rep. 2020, 69, 759–765. [Google Scholar] [CrossRef]
- Wang, Q.; Zhan, Y.; Pederson, N.L.; et al. Telomere length and all-cause mortality: a meta-analysis. Ageing Res Rev. 2018, 48, 11–20. [Google Scholar] [CrossRef]
- Sanchez-Vazquez, R.; Guío-Carrión, A.; Zapatero-Gaviria, A.; et al. Shorter telomere lengths in patients with severe COVID-19 disease. Aging (Albany NY). 2021, 13, 1–15. [Google Scholar] [CrossRef]
- Mahmoodpoor, A.; Sanale, S.; Eskandari, M.; et al. Association between leucocyte telomere length and COVID-19 severity. Egypt J Med Hum Genet. 2023, 24, 37. [Google Scholar] [CrossRef]
- Retuerto, M.; Liedó, A.; Fernandez-Varas, B.; et al. Shorter telomere length is associated with COVID-19 hospitalization and with persistence of radiographic lung abnormalities. Immunity & Ageing. 2022, 19, 38. [Google Scholar]
- Arantes dos Santos, G.; Pimenta, R.; Viana, N.I.; et al. Shorter leukocyte telomere length is associated with severity of COVID-19 infection. Biochemistry and Biophysics Reports. 2021, 27, 101056. [Google Scholar] [CrossRef]
- Aviv, A. The bullwhip effect, T-cell telomeres, and SARS-CoV-2. Lancet. 2022, 3, E715–E721. [Google Scholar] [CrossRef]
- Sepe, S.; Rossiello, F.; Cancila, V.; et al. DNA damage response at telomeres boosts the transcription of SARS-CoV-2 receptor ACE2 during aging. EMBO rep. 2022, 23, e53658. [Google Scholar] [CrossRef]
- Liu, S.; Nong, W.; Ji, L.; et al. The regulatory feedback of inflammatory signaling and telomere/telomerase complex dysfunction in chronic inflammatory disease. Experimental Gerontology. 2023, 174, 112132. [Google Scholar] [CrossRef]
- Crous-Bou, M.; Molinuevo, J.-L.; Sala-Vila, A. Plant-Rich Dietary Patterns, Plant Foods and Nutrients, and Telomere Length. Adv Nutr. 2019, 10 (Suppl. S4), S286–S303. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, S. Diet and Aging: The Role of Polyphenol-Rich Diets in Slow Down the Shortening of Telomeres: A Review. Antioxidants 2023, 12, 2086. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, E.; Epel, E. The Telomere Effect: A Revolutionary Approach to Living Younger, Healthier, Longer. Grand Central Publishing. 2017.
- Kökten, T.; Hansmannel, F.; Ndiaye, N.C.; et al. Calorie Restriction as a New Treatment of Inflammatory Diseases. Adv Nutr. 2021, 12, 1558–1570. [Google Scholar] [CrossRef] [PubMed]
- Gnoni, M.; Beas, R.; Vásques-Garagatti. Is there any role of intermittent fasting in the prevention and improving clinical outcomes of COVID-19?: intersection between inflammation, mTOR pathway, autophagy and caloric restriction. VirusDis. 2021, 32, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Martin Bagos, J.P.; Erick, M.; Matawaran, B. Predictors of Poor Glycemic Control and Increased Glucose Variability Among Admitted Moderate to Critical COVID-19 Patients with Type 2 Diabetes Mellitus: A Single Center Cross-sectional Study. J ASEAN Fed Endocr Soc. 2023, 38, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Sultan, K.; Kal, S.; Issagholian, L.; et al. The Effect of Glycemic Control on Morbidity and Mortality in Critically Ill COVID-19 Patients. Cureus 2023, 15, e47991. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Carretero, R.; Vazquez-Gomez, O.; Lopez-Lomba, M.; Gil-Prieto, R.; Gil-de-Miguel, A. Insulin Resistance and Metabolic Syndrome as Risk Factors for Hospitalization in Patients with COVID-19: Pilot Study on the Use of Machine Learning. Metab Syndr Relat Disord. 2023, 21, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Alvarado, M.; Campos-Campos, L.; Guerrero-Romero, F.; et al. The Triglycerides and Glucose Index Is an Independent Risk Factor for Acute Respiratory Distress Syndrome in Patients with Covid-Metab Syndr Relat Disord. [CrossRef]
- Horne, B.D.; May, H.T.; Muhlestein, J.B.; et al. Association of periodic fasting with lower severity of COVID-19 outcomes in the SARS-CoV-2 prevaccine era: an observational cohort from the INSPIRE registry. BMJ Nutrition, Prevention & Health. 2022, 0, eooo462. [CrossRef]
- U.S. Department of Agriculture, Agriculture Research Service, Scientific Report of the 2020 Dietary Guideline Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services, Published Accessed March 18, 2023. https://www.dietaryguidelines.gov/2020-advisory-committee-report.
- Cheng, R.Z. Can early and high intravenous dose of vitamin C prevent and treat coronavirus disease 2019 (COVID_19)? Med Drug Discov. 2020, 5, 100028. [Google Scholar] [CrossRef]
- Chen, L.; Hu, C.; Hood, M.; et al. A novel combination of vitamin, C.; curcumin and glycyrrhizin acid potentially regulates immune and inflammatory response associated with coronavirus infections: a perspective from system biology analysis. Nutrients. 2020, 12, 1193. [Google Scholar] [CrossRef]
- Marik, P.E.; Khangoora, V.; Rivera, R.; et al. Hydrocortisone, vitamin, C.; and thiamine for the treatment of severe sepsis and septic shock: a retrospective before-after study. Chest. 2017, 151, 1229–1238. [Google Scholar] [CrossRef]
- Kow, S.-K.; Hasan, S.S.; Ramachandram, D.S. The effect of vitamin C on the risk of mortality in patients with COVID-19: a systematic review and meta-analysis of randomized controlled trials. Inflammopharmacology. 2023, 18, 1–6. [Google Scholar] [CrossRef]
- Olczak-Pruc, M.; Swieczkowski, D.; Ladny, J.R.; et al. Vitamin C Supplementation for the Treatment of COVID-19: A Systematic Review and Meta-Analysis. Nutrients. 2022, 14, 4217. [Google Scholar] [CrossRef]
- Fisher, S.A.; Rahimzadeh, M.; Brierley, C.; et al. The role of vitamin D in increasing circulating T regulatory cell numbers and modulating T regulatory cell phenotypes in patients with inflammatory disease or in healthy volunteers: A systematic review. PloS One. 2019, 14, e0222313. [Google Scholar] [CrossRef]
- Gönen, M.S.; Alaylıoğlu, M.; Durcan, E.; Özdemir, Y.; Şahin, S.; Konukoğlu, D.; Nohut, O.K.; Ürkmez, S.; Küçükece, B.; Balkan, İ.İ.; et al. Rapid and Effective Vitamin D Supplementation May Present Better Clinical Outcomes in COVID-19 (SARS-CoV-2) Patients by Altering Serum INOS1, IL1B, IFNg, Cathelicidin-LL37, and ICAM1. Nutrients 2021, 13, 4047. [Google Scholar] [CrossRef]
- Giannis, D.; Ziogas, I.A.; Gianni, P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020, 127, 104362. [Google Scholar] [CrossRef]
- Mohammad, S.; Mishra, A.; Ashraf, MZ. Emerging role of Vitamin D and its associated molecules in pathways related to pathogenesis of thrombosis. Biomolecules. 2019, 9, 649. [Google Scholar] [CrossRef]
- Weir, E.K.; Thenappan, T.; Bhargaya, M.; et al. Does vitamin D deficiency increase the severity of COVID-19? Clin Med (Lond). 2020, 20, e107–e108. [Google Scholar] [CrossRef]
- D’Ecclesiis, O.; Gavioli, C.; Martinoli, C.; et al. Vitamin D and SARS Cov-2 infection, severity and mortality: A systematic review and meta-analysis. PLoS One. 2022, 17, e0268396. [Google Scholar] [CrossRef]
- Meng, J.; Li, X.; Lie, W.; et al. The role of vitamin D in the prevention and treatment of SARS-CoV-2 infection: A meta-analysis of randomized controlled trials. Clinical Nutrition. 2023, 42, 2198–2206. [Google Scholar] [CrossRef]
- Sartini, M.; Del Puente, F.; Oliva, M.; Carbone, A.; Bobbio, N.; Schinca, E.; Giribone, L.; Cristina, M.L. Preventive Vitamin D Supplementation and Risk for COVID-19 Infection: A Systematic Review and Meta-Analysis. Nutrients 2024, 16, 679. [Google Scholar] [CrossRef]
- Bogan, K.L.; Brenner, C. Nicotinic acid, nicotinamide, and nicotinamide riboside: a molecular evaluation of NAD+ precursor vitamins in human nutrition. Annu Rev Nutr. 2008, 28, 115–130. [Google Scholar] [CrossRef]
- Zheng, M.; Schultz, M.B.; Sinclair, DA. NAD+ in COVID-19 and viral infections. Trends in Immunology. 2022, 43, 283–295. [Google Scholar] [CrossRef]
- Bogan-Brown, K.; Nkrumah-Elie, Y.; Ishtiaq, Y.; et al. Potential Efficacy of Nutrient Supplements for Treatment of Prevention of COVID-19. Journal of Dietary Supplements. 2022, 19, 336–365. [Google Scholar] [CrossRef]
- Abdellatif, M.; Bugger, H.; Kroemer, G.; et al. NAD+ and Vascular Dysfunction: From Mechanisms to Therapeutic Opportunities. J Lipid Atheroscler. 2022, 11, 111–132. [Google Scholar] [CrossRef]
- Abdallah, S.B.; Mhalla, Y.; Trabelsi, I.; et al. Twice-Daily Oral Zinc in the treatment of Patients With Coronavirus Disease 2019: A Randomized Doble- Blind Controlled Trial. Clin Infect Dis. 2023, 76, 185–191. [Google Scholar] [CrossRef]
- Olczak-Pruc, M.; Szarpak, L.; Navolokina, A.; et al. The effect of zinc supplementation on the course of COVID-19- A systematic review and meta-analysis. Ann Agric Environ Med. 2022, 29, 568–574. [Google Scholar] [CrossRef]
- Francis, Z.; Book, G.; Litvin, C.; et al. The COVID-19 Pandemic and Zinc-Induced Copper Deficiency: An Important Link. Am J Med. 2022, 135, e290–e291. [Google Scholar] [CrossRef]
- Raha, S.; Mallick, R.; Basak, S.; et al. Is copper beneficial for COVID-19 patients? Med Hypotheses. 2020, 142, 109814. [Google Scholar] [CrossRef] [PubMed]
- Fakhrolmobasheri, M.; Mazaheri-Tehrani, S.; Kieliszek, M.; et al. COVID-19 and Selenium Deficiency: a Systematic Review. Biol Trace Elem Res. 2022, 200, 3945–3956. [Google Scholar] [CrossRef] [PubMed]
- Gröber, U.; Holick, MF. The coronavirus disease (COVID-19)- a supportive approach with selected micronutrients. Int J Vitam Nutr Res Int Z Vitam. Ernahrungsforschung J Int Vitaminol Nutr.
- Gullin, O.M.; Vindry, C.; Ohlmann, T.; et al. Selenium, selenoproteins and viral infection. Nutrients. 2019, 11, 2101. [Google Scholar] [CrossRef]
- Kieliszek, M.; Lipinski, B. Selenium supplementation in the prevention of coronavirus infection (COVID-19). Med Hypotheses. 2020, 143, 109878. [Google Scholar] [CrossRef]
- Dludia, P.V.; Nyambuya, T.M.; Orlando, P.; et al. The impact of coenzyme Q10 on metabolic and cardiovascular disease profiles in diabetic patients: A systematic review and meta-analysis of randomized controlled trials. Endocrinol Diabetes Metab. 2020, 3, e00118. [Google Scholar] [CrossRef]
- Alarcón-Vieco, E.; Martínez-García, I.; Sequí-Domínguez, I.; et al. Effect of coenzyme Q10 on cardiac function and survival in heart failure: an overview of systematic reviews and meta-analyses. Food Funct. 2023, 14, 6302–6311. [Google Scholar] [CrossRef]
- Jorat, M.V.; Tabrizi, R.; Kolahdooz, F.; et al. The effects of coenzyme Q10 supplementation on biomarkers of inflammation and oxidative stress in among coronary artery disease: a systematic review and meta-analysis of randomized controlled trials. Inflammopharmacology. 2019, 27, 233–248. [Google Scholar] [CrossRef]
- Sue-Ling, C.B.; Abel, W.M.; Sue-Ling, K. Coenzyme Q10 as adjunctive Therapy for Cardiovascular Disease and Hypertension: A Systematic Review. The Journal of Nutrition. 2022, 152, 1666–1674. [Google Scholar] [CrossRef]
- Hargreaves, I.R.; Mantle, D. COVID-19, Coenzyme Q10, and Selenium. Adv Exp Med Biol. 2021, 168, 1327161. [Google Scholar]
- Varnousfaderani, S.D.; Musazadeh, V.; Ghalichi, F.; et al. Alleviating effects of coenzyme Q10 supplements on biomarkers of inflammation and oxidative stress: result from an umbrella meta-analysis. Frontiers in Pharmacology. 2023, 14, 1191290. [Google Scholar] [CrossRef]
- Sumbalova, Z.; Kucharská, J.; Rausová, Z.; et al. Reduced platelet mitochondrial respiration and oxidative phosphorylation in patients with pst COVID-19 syndrome are regenerated after spa rehabilitation and targeted ubiquinol therapy. Front Mol Biosci. [CrossRef]
- Ma, B.; Lu, J.; Kang, T.; et al. Astaxanthin supplementation mildly reduced oxidative stress and inflammation biomarkers: a systematic review and meta-analysis of randomized controlled trials. Nutrition Research. 2022, 99, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Talukdar, J.; Bhadra, B.; Dattaroy, T.; et al. Potential of natural astaxanthin in alleviating the risk of cytokine storm in COVID-19. Biomed Pharmacother. 2020, 132, 110886. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi A-R, Ayazi-Nasrabadi R. Astaxanthin protective barrier and its ability to improve the health in patients with COVID-19. Iran J Microbiol. 2021, 13, 434–441.
- Cheema, H.A.; Sohail, A.; Fatima, A.; et al. Quercetin for the treatment of COVID-19 patients: A systematic review and meta-analysis. Reviews in Medical Virology. 2023, 33, e2427. [Google Scholar] [CrossRef]
- Ziaei, S.; Alimohammadi-Kamalabadi, M.; Hasani, M.; et al. The effect of quercetin supplementation on clinical outcomes in COVID-19 patients: A systematic review and meta-analysis. Food Science & Nutrition. 2023, 11, 7504–7514. [Google Scholar]
- Mrityunjaya, M.; Pavithra, V.; Neelam, R.; et al. Immune-boosting, antioxidant and anti-inflammatory food supplements targeting pathogenesis of COVID-19. Front Immunol. 2020, 11, 570122. [Google Scholar] [CrossRef]
- Smith, M.; Smith, JC. Repurposing therapeutics for COVID-19: supercomputer-based docking to the SARS-CoV-2 viral spike protein and viral spike protein-human ACE2 interface. [CrossRef]
- Khaerunnisa, S.; Kurniawan, H.; Awaluddin, R.; et al. Potential inhibitor of COVID-19 main protease (Mpro) from several medicinal plant compounds by molecular docking study. [CrossRef]
- Derosa, G.; Maffioli, P.; D’Angelo, A.; et al. A role for quercetin in coronavirus disease 2019 (COVID-19). Phytother Res. 2021, 35, 1230–1236. [Google Scholar] [CrossRef]
- Lammi, C.; Arnoldi, A. Food-derived antioxidants and COVID-19. J Food Biochem. 2021, 45, 1–6. [Google Scholar] [CrossRef]
- Hassaniazad, M.; Eftekhar, E.; Inchehsablagh, B.R.; et al. A triple-blind, placebo-controlled, randomized clinical trial to evaluate the effect of curcumin-containing nanomicelles on cellular immune responses subtypes and clinical outcome in COVID-19 patients. Phytotherapy Research. 2021, 35, 6417–6427. [Google Scholar] [CrossRef]
- Sadeghi, M.; Dehnavi, S.; Asadirad, A.; et al. Curcumin and chemokines: mechanism of action and therapeutic potential in inflammatory diseases. Inflammopharmacology. 2023, 31, 1069–1093. [Google Scholar] [CrossRef]
- Rattis, B.; Ramos, S.G.; Celles, M. Curcumin as a potential treatment for COVID-19. Frontiers in Pharmacology. 2021, 12, 675287. [Google Scholar] [CrossRef] [PubMed]
- Dourado, D.; Freire, D.T.; Pereira, D.T.; et al. Will curcumin nanosystems be the next promising antiviral alternatives in COVID-19 treatment trials? Biomedicine & Pharmacotherapy. 2021, 139, 111578. [Google Scholar]
- Manoharan, Y.; Haidas, V.; Vasanthakumar, K.C.; et al. Curcumin: A wonder drug as a preventive measure for COVID-19 management. Indian Journal of Clinical Biochemistry. 2020, 35, 373–375. [Google Scholar] [CrossRef]
- Hassaniazad, M.; Eftekhar, E.; Inchehsablagh, B.R.; et al. A triple-blind, placebo-controlled, randomized clinical trial to evaluate the effect of curcumin-containing nanomicelles on cellular immune responses subtypes and clinical outcome in COVID-19 patients. Phytotherapy Research. 2021, 35, 6417–6427. [Google Scholar] [CrossRef]
- Valizadeh, H.; Abdolmohammadi-Vahid, S.; Danshina, S.; et al. Nano-curcumin therapy, a promising method in modulating inflammatory cytokines in COVID-19 patients. International Immunopharmacology. 2020, 89, 101088. [Google Scholar] [CrossRef]
- Tahmasebi, S.; El-Esawi, M.A.; Mahmoud, Z.H.; et al. Immunomodulatory effects of nanocurcumin on Th17 cell responses in mild and severe COVID-19 patients. Journal of Cellular Physiology. 2021, 236, 5325–5338. [Google Scholar] [CrossRef]
- Chia, S.-K.; Ramachandram, D.S.; Hasan, S. S.; Hasan S. The effect of curcumin on the risk of mortality in patients with COVID-19: A systematic review and meta-analysis of randomized trials. Phytotherapy Research. 2022, 36, 3365–3368. [Google Scholar]
- Shafiee, A.; Athar, M.M.T.; Shahid, A.; et al. Curcumin for the treatment of COVID-19 patients: A meta-analysis of randomized controlled trials. Phytotherapy Research. 2023, 37, 1167–1175. [Google Scholar] [CrossRef]
- van Eijk, Larissa, E.; Offringa, et al. The Disease-Modifying Role of Taurine and Its Therapeutic Potential in Coronavirus Disease 2019 (COVID-19). Taurine 2. [CrossRef]
- Rubio-Casillas, A.; Gupta, R.C.; Redwan, E.M.; et al. Early taurine administration as a mean for halting the cytokine storm progression in COVID-19 patients. Explor Med. 2022, 3, 234–48. [Google Scholar] [CrossRef]
- Vu, T.T.; Rydland, K.J.; Achenbach, C.J.; Van Horn, L.; Cornelis, MC. Dietary Behaviors and Incident COVID-19 in the UK Biobank. Nutrients. 2021, 13, 2114. [Google Scholar] [CrossRef]
- Bousquet, J.; Anto, J.M.; Czarlewski, W.; Haahtela, T.; Fonseca, S.C.; Iaccarino, G.; Blain, H.; Vidal, A.; Sheikh, A.; Akdis, C.A.; et al. Cabbage and fermented vegetables: From death rate heterogeneity in countries to candidates for mitigation strategies of severe COVID-19. Allergy. 2021, 76, 735–750. [Google Scholar] [CrossRef]
- Gorman, S.; Weller, R. Investigating the Potential for Ultraviolet Light to Modulate Morbidity and Mortality From COVID-19: A Narrative Review and Update. Frontiers in Cardiovascular Medicine. 2020, 7. [Google Scholar] [CrossRef]
- Cherrie, M.; Clemens, T.; Colandrea, C.; Feng, Z.; Webb, D.J.; Weller, R.B.; Dibben, C. Ultraviolet A radiation and COVID-19 deaths in the USA with replication studies in England and Italy. Br J Dermatol. 2021, 185, 363–370. [Google Scholar] [CrossRef]
- Pelegrino, M.T.; Paganotti, A.; Seabra, A.B.; Weller, RB. Photochemistry of nitric oxide and S-nitrosothiols in human skin. Histochem Cell Biol. 2020, 153, 431–441. [Google Scholar] [CrossRef] [PubMed]
- Acosta-Navarro, J.C.; Dias, L.F.; Gomes de Gouveia, L.A.; et al. Vegetarian and plant-based diets associated with lower incidence of COVID-19. BMJ Nutrition, Prevention & Health, 0629. [Google Scholar]
- Soltanieh, S.; Salavatizadeh, M.; Ghazanfari, T.; et al. Plant-based diet and COVID-19 severity: results from a cross-sectional study. BMJ Nutrition, Prevention & Health, 0688. [Google Scholar]
- Kendrick, K.N.; Kim, H.; Rebholz, C.M.; et al. Plant-Base Diets and Risk of Hospitalization with Respiratory Infection: Results from the Atherosclerosis Risk in Communities (ARIC) Study. Nutrients. 2023, 15, 4265. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Barnard, ND. Can a plant-based diet help mitigate COVID-19? European Journal of Clinical Nutrition. 2022, 76, 911–912. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-Z.; Sato, T.; Sakuraba, A. Worldwide association of lifestyle-related factors and COVID-19 mortality. Annals of Medicine. 2021, 53, 1528–1533. [Google Scholar]
- Storz, M.A. Lifestyle Adjustments in Long-COVID Management: Potential Benefits of Plant-Based Diets. Current Nutrition Reports. 2021, 10, 352–363. [Google Scholar] [CrossRef]
- Lange, K.W.; Nakamura, Y. Lifestyle factors in the prevention of COVID-19. Global Health Journal 2020, 4, 146–152. [Google Scholar] [CrossRef]
- Moreb, N.A.; Albandary, A.; Jaiswal, S.; Jaiswal, A.K. Fruits and Vegetables in the Management of Underlying Conditions for COVID-19 High-Risk Groups. Foods 2021, 10, 389. [Google Scholar] [CrossRef]
- Khaleova, H.; Barnard, ND. The Role of Nutrition in COVID-19: Taking a Lesson from the 1918 H1N1 Pandemic. SAGE. 2022. http://www.sagepub.com/journalsPermissions.nav.
- Rust, P.; Ekmekcioglu. The Role of Diet and Specific Nutrients during the COVID-19 Pandemic: What Have We Learned over the Last Three Years? International Journal of Environmental Research and Public Health. 2023, 20, 5400. [Google Scholar] [CrossRef]
| Foods that reduce DII | Foods that increase DII |
|---|---|
| Red meat (steak and hamburgers) Animal products (including eggs and dairy products) Processed meat Commercial baked goods White flour (bread and noodles), white rice Deep-fried foods Sugary products Products with trans-fats Saturated fats (especially animal fats) Cholesterol (red meats, processed meats, eggs, fried foods and dairy products) |
Plant-based proteins (beans, lentils, chickpeas, edamame, hemp seeds, tofu, tempeh, and nuts) Whole grains (oatmeal, buckwheat, quinoa, pigmented rice) Starchy vegetables (sweet potatoes and beets) Seeds (flaxseeds and chia seeds) Green leafy vegetables (raw) Colorful vegetables (raw) Fruits (berries, apples, grapes, oranges, peaches, figs, bananas, and kiwi) Spices and herbs (turmeric, ginger, cumin, peppermint, cinnamon, chili, parsley, bay leaf, and basil) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





