Key Points
Palmitoylethanolamide (PEA) is largely prescribed in neuropathic pain patients
Data on its clinical use have never been extensively reviewed
This review aims to analyze existing data on the site of action, pharmacodynamics, and pharmacokinetics, on the occasion of the introduction into the market of a new formulation, EquiPEA®, which is suggested as an innovative potentiality to solve some of the pharmacokinetics existing problems.
1. Introduction
Chronic neuropathic pain is a prevalent and incapacitating illness that poses a significant problem in the field of medical treatments, impacting a substantial number of individuals globally [
1]. Based on recent figures provided by the International Association for the Study of Pain (IASP), it has been determined that neuropathic pain affects roughly 7-10% of the global population [
2]. This prevalence leads to a significant proportion of chronic pain instances. Most of this phenomenon is observed across a wide range of demographic categories, affecting individuals regardless of age, gender, or financial background. Neuropathic pain incurs a significant economic burden, including direct healthcare expenditures, reduced productivity, and the societal impact of impaired quality of life [
3]. Consequently, there is an urgent need to develop novel and well-tolerated therapeutic interventions.
In the pursuit of efficacious and lasting resolutions to this widespread health problem, Palmitoylethanolamide (PEA) has been suggested as a notable contender [
4]. The ascent of PEA as an active molecule in treating neuropathic pain may be attributed to its unique mechanisms of action and the accumulation of clinical evidence supporting its efficacy [
5]. The multidimensional nature of its pain modulation efficacy has attracted attention, presenting a divergence from conventional analgesics that may exhibit limited effectiveness and unwanted adverse reactions.
Looking at the scientific literature, a comprehensive review of this molecule is missing. In light of this context, this narrative review aims to offer a thorough examination of the trajectory of PEA, encompassing its initial discovery, elucidation of its mechanisms of action, and its current standing as a benchmark in managing chronic neuropathic pain. By engaging in this endeavor, we aim to contribute to the continuing scholarly conversation surrounding treatment approaches that mitigate the personal distress experienced by patients and tackle the broader societal and economic ramifications associated with chronic pure neuropathic and/or mixed pain.
2. Methodology
This study utilizes a thorough descriptive thematic analysis to understand the role of PEA in managing chronic neuropathic pain. The study's approach places significant importance on adhering to the Scale for Assessment of Narrative Review Articles (SANRA) standard [
6].
2.1. Eligibility Criteria
Accepted papers need to fall into the category of peer-reviewed empirical or prospective papers. Furthermore, the study topic needed to be focused on PEA and its role in chronic neuropathic pain management. The accepted types of studies included original articles, reviews, case series, case reports, or letters to the editor. For all of them, the full text was requested.
Conversely, studies were excluded if they failed to meet the relevance criteria to the designated topic, lacked adequate reporting of objectives and conclusions, or did not provide full-text access. These criteria were applied systematically to ensure the selection of papers closely aligned with the objectives and focus of the study.
2.2. Information Sources and Search
To ensure a complete literature study, the methodology for information retrieval in the research on "Palmitoylethanolamide (PEA) Involvement in Chronic Neuropathic Pain Management" included a comprehensive search across multiple databases. The search began with creating databases and ended with the most recent update as of 2010-2023. PubMed was one of the key databases used in this search. The search strategy's Medical Subject Headings (MeSH) terms were chosen to capture the substance of the investigation, with an emphasis on "Palmitoylethanolamide," "Chronic Neuropathic Pain," and related terms. The Boolean operators "AND" and "OR" were used to refine and improve the search's specificity. The primary search term was "Palmitoylethanolamide AND Chronic Neuropathic Pain". To encompass all relevant literature, this basic search phrase was expanded to include synonymous terms, variants, and alternative formulations; e.g., the search query was supplemented with phrases like "neuropathic pain management" and "PEA treatment". Scopus, Embase, PsycINFO, and Web of Science were checked in addition to PubMed to ensure a more extensive coverage. Each database's search tactics were adjusted to its unique features and indexing terms while remaining consistent with the broader study objective. References from identified publications and reviews were thoroughly examined to uncover potential supplementary sources.
2.3. Selection Process
The abstract and title screenings and full-text assessments were performed against the qualifying criteria by two independent authors (CC and DF), following pilot screenings with over 80% agreement, which were monitored by the primary author (GV). Any disagreements were settled through consensus or with the assistance of the lead author.
2.4. Data Charting and Items
The study team created a coding scheme to guide the extraction of formal data items. The primary data extractor (CC) was in charge of obtaining elements such as publication type, sources, geographies addressed, and the objectives and main findings of the selected literature. Another author (GF) independently checked 5% of the retrieved data to guarantee accuracy and dependability. The entire method, from extraction to synthesis, followed the research team's planned coding structure and recommendations.
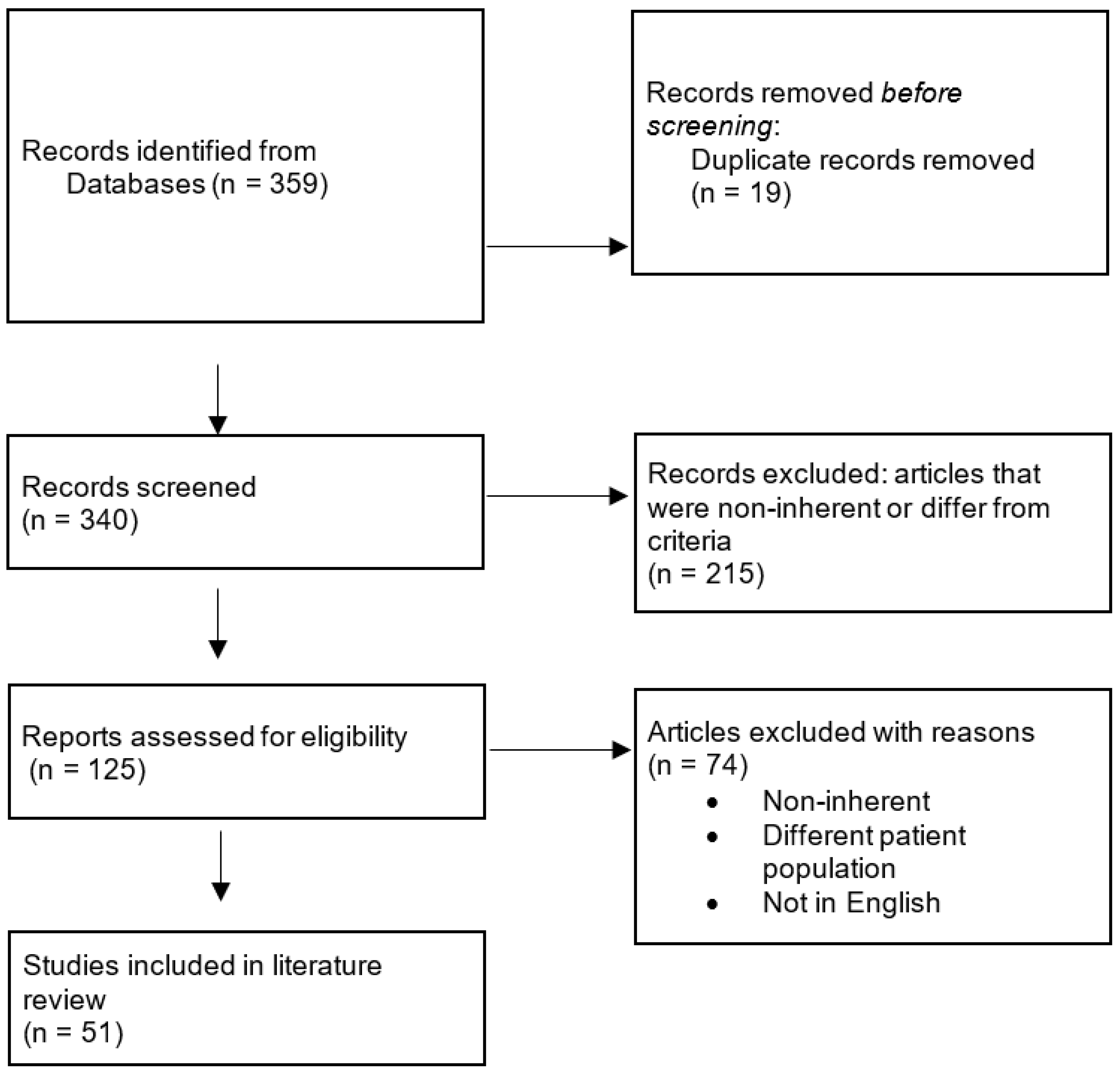
A flowchart was used to incorporate a visual depiction of the article selection process within the paper, providing readers with a clear picture of the methodical approach to article inclusion (Figure 1). The independent extractions, including formal data items and content quotations, were paired following comparison and consistency. This methodological rigor ensured the data charting process's dependability and accuracy in clarifying the role of PEA in chronic neuropathic pain management.
Figure 1.
Flowchart of selected manuscript.
Figure 1.
Flowchart of selected manuscript.
3. Synthesis of the Results Simple Descriptive Data
After the literature search, a comprehensive examination resulted in the selection of 51 studies. This diverse collection of studies collectively informs the exploration of PEA's potential involvement in chronic neuropathic pain management, offering a broad and nuanced perspective on the multifaceted aspects of this subject.
3.1. Quality Assessment Following SANRA Assessment
The outcomes of the SANRA were documented in
Table S1 (Supplementary Material). All 156 assessments, comprising evaluations from three raters across 51 manuscripts, were included in the subsequent statistical analysis. The mean cumulative score for all 51 manuscripts amounted to 6.28 points. Notably, the highest scores were assigned to item 1 (Justification of the article’s importance for the readership) with a mean of 1.17, and item 2 (Statement of concrete aims or formulation of questions) with a mean of 1.17. Conversely, items 3, 4, 5 and 6 garnered the lowest scores, exhibiting means of 0.92, 1.01, 0.96 and 1.05, respectively.
4. Evolution of PEA: A historical analysis
PEA, a fatty acid amide known for its anti-inflammatory and analgesic effects, has significantly evolved from its initial discovery to its present recognition as a therapeutic component for managing chronic neuropathic pain. A comprehensive examination of the historical development of PEA provides significant insights into the scientific advancements, pivotal discoveries, and transformative shifts in thinking that have influenced its progression throughout its existence [
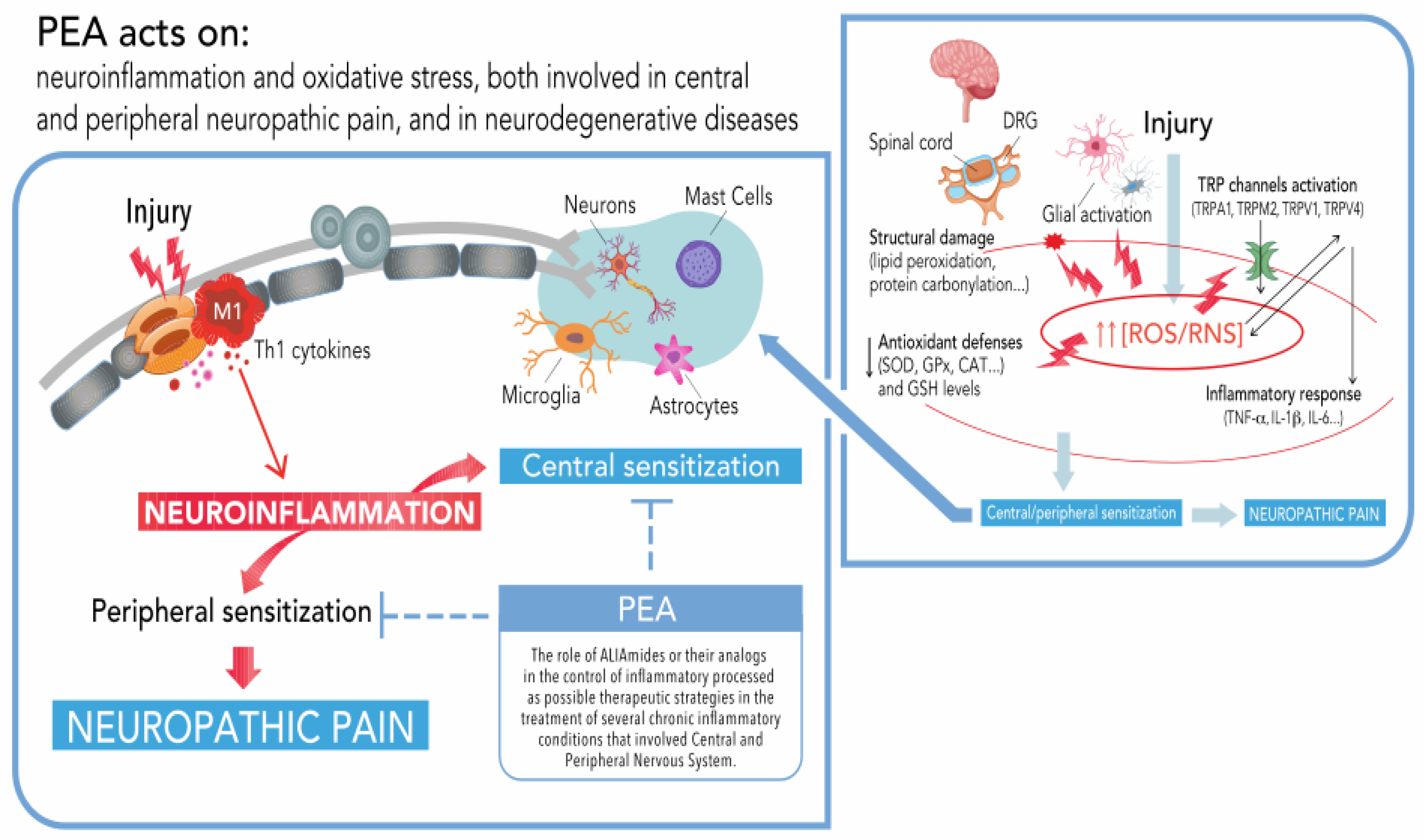
7]. In
Figure 2 we have tried to summarize what has been suggested until now about its effects. The following paragraphs provide a basis for comprehending the improvements achieved in utilizing the therapeutic capabilities of PEA.
4.1. Discovery and Early Investigations
The narrative of PEA commences during the mid-20th century when researchers investigating the pharmacological characteristics of egg yolk unexpectedly encountered this substance of natural origin [
8]. Initially regarded as a biochemical anomaly, the therapeutic implications of PEA remained largely unexplored for a long time. The discovery of the anti-inflammatory characteristics of PEA and its role in modifying the endocannabinoid system occurred in the late 1990s, as researchers began to publish data related to its effects [
9]. The preliminary inquiries established the foundation for comprehending the anti-inflammatory and analgesic actions of PEA, namely its connections with cannabinoid receptors and its function in alleviating neuroinflammation [
10,
11,
12]
4.2. Clinical Validation and Therapeutic Potential
The progression from being a mere object of scientific interest in the laboratory to being utilized in clinical settings is a significant milestone in developing PEA. The efficacy of PEA in various neuropathic pain syndromes was validated by implementing clinical trials, providing evidence of the analgesic properties of PEA [
11]. The researchers emphasized its safety and tolerability. Some also focused on the effectiveness of PEA expanded beyond its suggested generic application in treating neuropathic pain, and included a broader range of disorders [
12]. The growing body of evidence spurred a reassessment of the therapeutic potential of PEA, resulting in its acknowledgment as an interesting active molecule in the management of chronic neuropathic pain.
4.3. Mechanistic Insights and Neuroprotective Dimensions
Deeper research gradually unfolded the mechanisms of action of PEA. Exploring PEA's capacity to interact with cannabinoid type 2 (CB2) and regulate mast cell activation has emerged as a central area of focus, revealing its intricate but specific mechanism for modulating pain [
12]. PEA interaction is not limited to CB2 but also addresses the CB1, in its antinociceptive action [
13]. Moreover, research has offered valuable information regarding the neuroprotective attributes of PEA [
14] (
Figure 3). These studies have elucidated its potential to modulate mechanisms implicated in neurodegenerative processes. This demonstrated development broadened the scope of PEA beyond the mere management of symptoms, suggesting its promise in addressing the fundamental pathophysiological mechanisms associated with persistent neuropathic pain [
15].
4.4. Comparative Analysis and Progress in Pain Management
One crucial element in the advancement of PEA pertains to its comparison with conventional therapy. Comparative investigations, suggesting that PEA’s diverse modes of action provide benefits, have yielded significant findings about its relative effectiveness and safety about conventional analgesics [
16,
17]. The advancements in pain management by utilizing PEA extend beyond its direct analgesic properties [
18]. The importance of PEA in providing an option that effectively balances efficacy and safety is indicative of the progression of treatment approaches in response to the opioid pandemic [
18].
4.5. Challenges and Future Directions
Although clinical data supports the therapeutic usefulness of this molecule, it is necessary to conduct additional comprehensive and well-structured trials to solidify its significance. Further investigation is needed to explore the ideal dose regimens, potential interactions with other drugs, and long-term consequences [
19]. Moreover, a more comprehensive understanding of the mechanisms underlying PEA could facilitate the advancement of innovative formulations or combination medicines to augment its therapeutic efficacy [
20].
Upon examining the historical trajectory of PEA, it becomes clear that its development has consistently advanced from being a molecule of biochemical interest to a useful component in managing chronic neuropathic pain [
21]. The significance of PEA in the developing field of pain treatment is underscored by the success achieved in exploiting its therapeutic potential. Affording to the various obstacles and potential advantages that lay in the therapy path, the ongoing development of PEA presents a progressively unfolding narrative [
22].
5. Pharmacodynamics of PEA: Unraveling Molecular and Cellular Targets
PEA has attracted considerable interest due to its diverse pharmacological effects, notably in treating chronic neuropathic pain [
23]. Comprehending the pharmacodynamics of PEA necessitates a comprehensive examination of its multifaceted interactions with many molecular and cellular targets and the ensuing biological mechanisms that form the basis of its therapeutic efficacy [
24]. A detailed examination would elucidate the complex pathways by which PEA affects physiological processes, providing valuable insights into its potential applications.
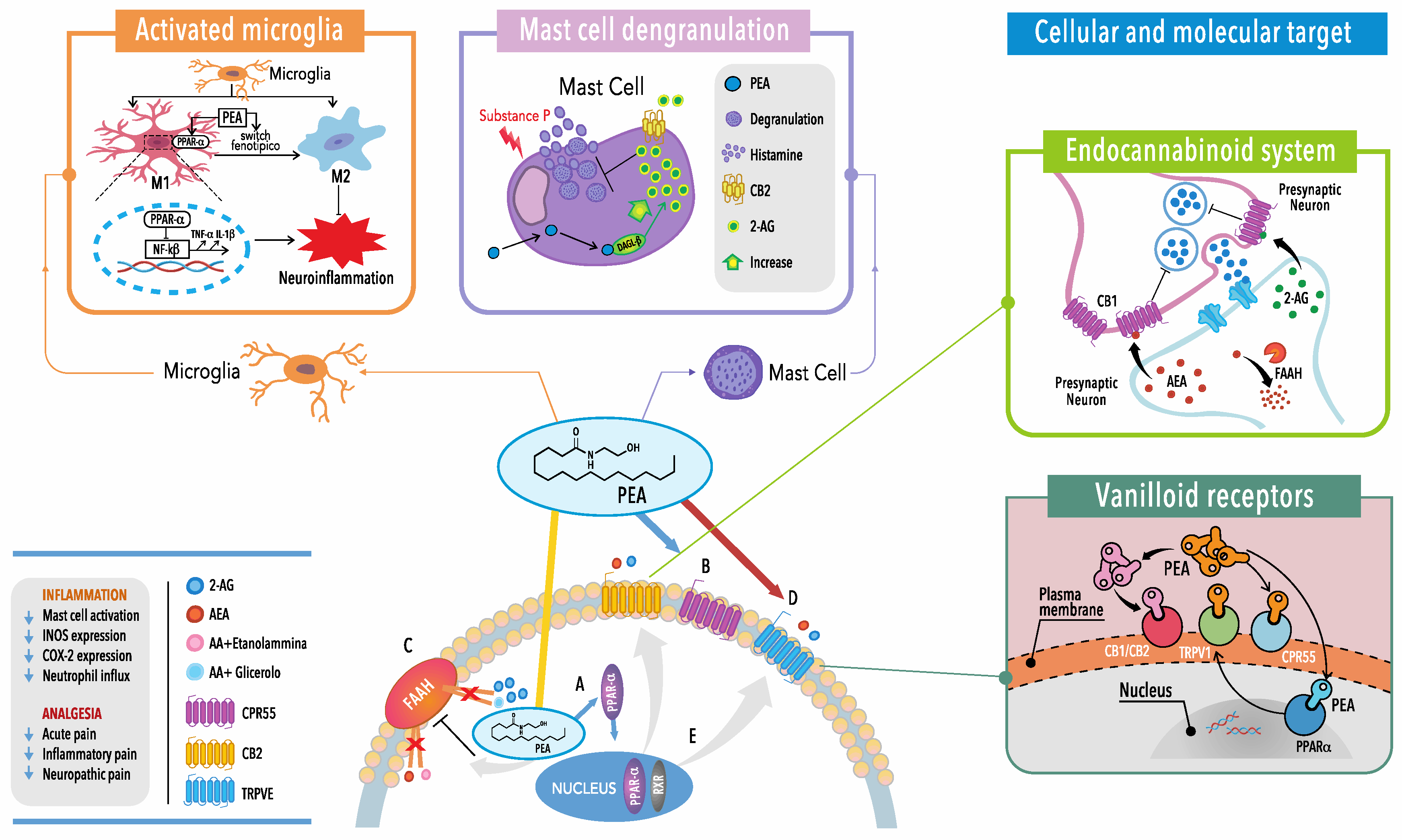
5.1. Molecular Targets: Engaging the Endocannabinoid System
The interaction between PEA and the endocannabinoid system (ECS) is a key focus in the field of pharmacodynamics at present. However, the role of PEA is controversial and still debated since it binds to CB1 and CB2 cannabinoid receptors, with very low or negligible affinity, suggesting possible indirect mechanisms [
13,
25]. An ‘entourage hypothesis’, stating that the effects of PEA are due to enhancement of the ECS, has been also proposed. Indeed, it has been shown that PEA is able to increase the number of CB2 receptors on inflammatory cells through a mechanism involving peroxisome proliferator-activated receptor alpha (PPAR-𝛼) [
25]. The expression of these receptors is highly prevalent in immune cells and tissues closely linked to inflammation, establishing a biological basis for the anti-inflammatory effects of PEA. Besides CB receptors, PEA exhibits molecular versatility since it is able to interact with other elements of the ECS, including the transient receptor potential vanilloid type-1 (TRPV1) channels [
23]. The complex interplay within the ECS constitutes the fundamental basis of the pharmacodynamics of PEA.
5.2. Cellular targets: Modulating Mast Cells and Glial Cells
The influence of PEA extends beyond the ECS to include mast cells, which are significant contributors to the immunological and inflammatory processes. PEA exerts its effects by stabilizing the membranes of mast cells, thereby reducing the release of pro-inflammatory mediators [
24]. The effectiveness of PEA in controlling disorders characterized by neuroinflammation, such as neuropathic pain, can be attributed to its anti-inflammatory properties. Moreover, the actions of PEA on glial cells, specifically microglia and astrocytes in the central nervous system, underscore its influence on neuroinflammatory mechanisms [
26]. The involvement of dysregulated activation of glial cells has been identified in chronic pain syndromes. The capacity of PEA to control these cells highlights its potential to address the neuroinflammatory aspect of neuropathic pain. Using these cellular interactions, PEA coordinates a complex response beyond simply alleviating symptoms [
24].
5.3. Biological Functions: Anti-Inflammatory and Analgesic Actions
As mentioned above, the anti-inflammatory effects of PEA have been also associated with PPAR-a activation [
24]. PPAR-𝛼 is well known for its role in lipid metabolism. It regulates transcriptional programs responsible for the development of inflammation through mechanisms directly related to the proinflammatory transcription factors, NF-𝜅Band AP1. Pharmacological studies have demonstrated that PPAR-𝛼 agonists are efficacious in rodent models of inflammatory and autoimmune diseases, and a neuropathic pain model in which the PPAR-𝛼 has been genetically deleted, showed a loss of PEA effectiveness, thus suggesting that PEA may act as PPAR-𝛼 agonist [
24].
As already shown, the molecular and cellular interactions of PEA result in a range of biological functions, primarily characterized by its anti-inflammatory and analgesic properties. PEA exerts a significant anti-inflammatory effect by suppressing immunological responses and inhibiting the release of inflammatory mediators [
27]. The aforementioned anti-inflammatory characteristics are especially relevant in cases of chronic pain, as neuroinflammation plays a role in the persistence of pain signals. The analgesic benefits of PEA are derived from its ability to modulate pain pathways at several levels [
27]. Its analgesic efficacy is further enhanced by its ability to attenuate neuroinflammation through its activities on glial and mast cells. Using an integrated approach in pain modulation highlights the potential of PEA as a viable therapeutic agent that specifically targets the molecular mechanisms associated with chronic neuropathic pain [
28].
5.4. Beyond Pain Management: Neuroprotective and Homeostatic Roles
Although PEA is mainly appreciated for its effectiveness in pain management, its pharmacodynamics suggest that it may have wider neuroprotective and homeostatic functions. According to existing literature, PEA may have a role in maintaining neuronal integrity and function [
29]. Through its intervention in neuroinflammatory processes and potential influence on neurotrophic factors, the activities of PEA extend beyond mere symptom control to effectively address the fundamental pathophysiology of neurodegenerative diseases. Furthermore, the impact of PEA on homeostasis encompasses metabolic processes, as evidenced by research suggesting its possible involvement in lipid metabolism and energy regulation [
30]. This observation implies a wider-reaching systemic influence, which presents opportunities for investigating the potential applications of PEA in metabolic illnesses and situations when maintaining physiological balance is of utmost importance [
31].
Although the pharmacodynamics of PEA show promise, obstacles still need to be addressed. Therefore, further research is required to enhance our comprehension and improve treatment results, especially on the intimate molecular mechanisms of receptors involved in pain perception. Careful consideration is necessary when evaluating the appropriate dose regimens, potential interactions with other drugs, and the impact of specific patient characteristics on the pharmacological response to PEA [
25]. Potential avenues for future research involve exploring the molecular complexities of the interactions of PEA within distinct cellular populations, thereby elucidating more refined mechanisms of its biological activity. Furthermore, exploring potential synergistic effects with other therapeutic agents can augment the overall effectiveness of interventions based on PEA [
32].
6. PEA Pharmacokinetics: Evolving Approaches to Enhance Absorption and Bioavailability
The investigation and analysis of the pharmacokinetics of PEA have garnered much attention and examination, particularly about its administration via the oral route [
33]. The effectiveness of PEA relies on its absorption and bioavailability due to its inherent features as a naturally occurring fatty acid amide [
34]. Over time, researchers have encountered several obstacles in their efforts to maximize these essential elements to achieve the most favorable treatment results [
32]. The investigation into the evolutionary patterns of the pharmacokinetics of PEA provides insights into the novel approaches utilized to address challenges related to absorption, helping to improve the amount of drug available in the systemic circulation.
6.1. The Challenge of Absorption
The investigation into the pharmacokinetics of PEA commenced upon the realization that its absorption was a notable obstacle. Due to its lipophilic nature, PEA encounters challenges in terms of solubility and subsequent absorption throughout the gastrointestinal tract [
33]. The initial efforts to administer the drug orally were impeded by inadequate absorption rates, which directly affected the drug's bioavailability and, consequently, its therapeutic effectiveness.
6.2. Evolution of Formulations
To tackle the absorption issue, researchers created formulations that could augment the solubility and bioavailability of PEA. Over time, various techniques have been utilized, and the development of micronized PEA has emerged as a significant breakthrough [
35]. The micronization process entails reducing particle size to increase the exposed surface area and boost solubility [
30]. The utilization of micronized PEA formulations has demonstrated enhanced absorption, hence allowing its systemic circulation after oral ingestion.
Liposomal formulations have emerged as a viable route in advancing the pharmacokinetics of PEA. Liposomes are lipid-derived vesicles that serve as carriers for the encapsulation of PEA, potentially enhancing its solubility and safeguarding it from destruction [
36]. These formulations aim to improve absorption and extend the compound's duration in the bloodstream, maximizing its therapeutic efficacy.
6.3. Nanotechnology and PEA Delivery
Absorption is not the only factor that determines the bioavailability of a drug [
32]. Several other aspects have an impact, including metabolism and excretion. This highlights the need to acquire a complete understanding of the pharmacokinetic profile of PEA.
The field of nanotechnology has witnessed significant progress in recent times, leading to a notable surge in innovation in the delivery of PEA. Nanoparticle-based formulations, such as nanoemulsions and polymeric nanoparticles, possess distinct advantages in drug encapsulation and targeted delivery [
37]. The utilization of nanotechnology in delivering PEA is evidence of the continuous endeavors to optimize its pharmacokinetic characteristics, hence augmenting its therapeutic efficacy. Its primary objective is to enhance the solubility and stability of PEA, potentially addressing certain obstacles commonly encountered with conventional formulations.
6.4. Combination with Substances Promoting Absorption
6.4.1. Equisetum Arvense L.
Extracts of Equisetum Arvense are well known for their anti-inflammatory properties [
38], and also for topical application [
39]. They are also used to increase the absorption of other drugs [
40]. For these reasons, PEA has been combined with Equisetum Arvense in a new oral formulation and branded as EquiPEA
® [
41].
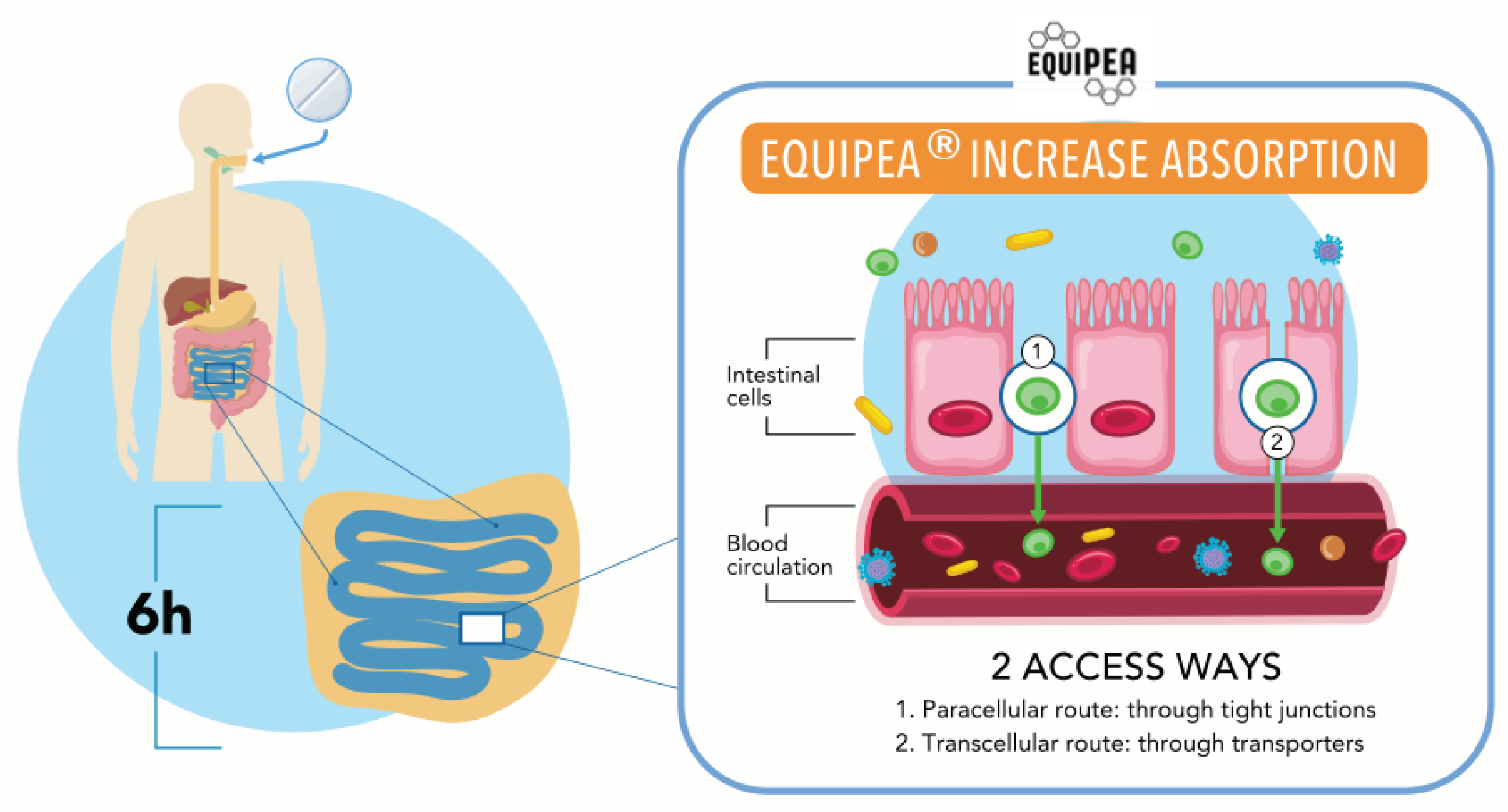
6.4.2. EquiPEA®
The EquiPEA
® patent strategically tackles the bioavailability limitations inherent in previous PEA formulations. EquiPEA
® aims to improve absorption and therapeutic efficacy by offering significant innovations in formulation design [
41]. Transepithelial electrical resistance (TEER), apparent permeability coefficient (Papp) values and tight junction (TJ) activity were evaluated to document the absorption of EquiPEA
®. The results revealed that EquiPEA
® has a better absorption profile than PEA-um because it can cross the transcellular pathway (enterocyte) and the paracellular pathway (TJ). This is important considering that the intestinal absorption phase is closely related to the transit in the small intestine, which is usually 6 hours, confirming an improvement in bioavailability and suggesting a synergistic effect of the combination of PEA and Equisetum Arvense (
Figure 4). The focused delivery mechanism of EquiPEA
® overcomes the limitations associated with PEA dispersion throughout the body, allowing for targeted transport to specific tissues and cells [
41]. Its interaction with receptors implicated in anti-inflammatory, antioxidant, and analgesic pathways is improved by this focused method addressed to increase the bioavailability, hence improving therapeutic accuracy [
41]. The patent also underlines the critical variables of action stability and persistence. EquiPEA
®, which focuses on the degradation of PEA within the human body, seems to provide a more dependable and long-lasting therapeutic option than standard PEA formulations [
41].
6.4.3. EquiPEA® vs. PEA-um
Improved bioavailability and customized administration strategy of EquiPEA
® lead to its significant anti-inflammatory effect, specifically targeting immune cells and modulating inflammatory pathways [
41]. The future clinical comparison with PEA-um will determine whether EquiPEA
® has greater anti-inflammatory characteristics, potentially offering breakthroughs in treating chronic inflammation-related disorders [
42]. Future research will determine whether the customized delivery strategy of EquiPEA
® results in greater antioxidant benefits, especially important in neurological and neurodegenerative illnesses where oxidative stress plays a key role [
43]. The targeted delivery mechanism and stability modifications of EquiPEA
® aim to optimize its analgesic characteristics, perhaps providing better and longer pain relief than traditional PEA formulations. Future comparative clinical studies will clarify whether EquiPEA
® may provide analgesic efficacy breakthroughs, particularly in chronic pain conditions. The clinical value of the EquiPEA
® patent is in its potential to provide more tailored approaches to PEA therapy. While scalability, cost-effectiveness, and future clinical validation are significant roadblocks, the comparative study with PEA-um will give critical insights into its efficacy. EquiPEA
®, if proven superior, could change PEA-based therapeutics by providing a potent and precise alternative for patients suffering from inflammation, oxidative stress consequences, and chronic pain. In conclusion, the EquiPEA
® patent might mark a considerable step forward in overcoming the problems associated with traditional PEA formulations absorption. Its potential impact on clinical practice and patient outcomes is still being investigated as research advances.
6.5. Clinical Implications and Patient Outcomes
For patients affected by chronic neuropathic or mixed pain, the optimization of the pharmacokinetics of PEA has a crucial role in attaining enduring pain relief and enhancing the overall quality of life. When clinicians are managing PEA therapy, they must consider not only the prescribed dosage schedules but also the particular formulation utilized [
42]. Enhanced absorption and bioavailability of formulations can lead to increased predictability and effectiveness of therapeutic effects [
41]. The selection of a specific formulation can substantially impact the initiation and duration of therapeutic effects, which are crucial considerations in customizing treatment strategies to meet the unique requirements of each patient [
44].
The dynamic nature of the pharmacokinetics of PEA is closely intertwined with regulatory factors. As innovative formulations and delivery systems continue to emerge, regulatory agencies must adjust their evaluation processes to assess these advancements' safety and efficacy [
45]. Acknowledging PEA as a prominent active molecule in managing persistent neuropathic pain highlights the significance of adapting regulatory frameworks to accommodate advancing pharmacokinetic approaches. Moving forward, it is anticipated that there will be more breakthroughs in the pharmacokinetics of PEA driven by progress in pharmaceutical technology and a more comprehensive comprehension of the compound's physiological interactions [
46]. The utilization of combination medicines that exploit the synergistic effects between PEA and other drugs presents promising opportunities for improving therapeutic outcomes while simultaneously reducing adverse effects [
47]. For instance, the combined administration of PEA and non-steroidal anti-inflammatory drugs (NSAIDs) can result in heightened pain alleviation, indicating a possible synergistic interplay for improved pain control [
48]. This partnership demonstrates the potential to enhance treatment regimens by utilizing the synergistic advantages of PEA in conjunction with conventional analgesics.
Subsequent investigations could focus on optimizing the delivery of PEA, encompassing not just its oral administration but also alternative routes, including transdermal and intravenous delivery, thereby investigating more possibilities for its effective administration [
49]. It is imperative to comprehend the influence of various formulations on the pharmacokinetics of PEA in heterogeneous patient cohorts, encompassing individuals with comorbidities or differing degrees of inflammation. This knowledge would be pivotal in customizing therapeutic strategies.
7. Neuropathic pain
7.1. Peripheral Neuropathic Pain
Peripheral neuropathic pain results, in general, from peripheral nerve injury that causes abnormal signaling and increased sensitivity. PEA's therapeutic efficacy in treating peripheral neuropathic pain is mainly attributed to its capacity to regulate immune responses, reduce neuroinflammation, and interact with crucial molecular targets [
50]. PEA demonstrates significant anti-inflammatory properties, fundamental in peripheral neuropathic pain, where inflammation plays a central role [
16]. Through its interaction with mast cells, PEA can stabilize cellular membranes and effectively suppress the production of pro-inflammatory mediators. The anti-inflammatory mechanism of action facilitates the resolution of neuroinflammatory processes, hence mitigating pain hypersensitivity [
51]. The immunomodulatory characteristics of PEA have a broader impact on other immune cells and mast cells. The engagement of PEA with CB2 receptors on immune cells plays a crucial role in regulating the immune response, effectively maintaining a balanced inflammatory environment [
52]. The management of immunological dysregulation is of particular significance in disorders such as diabetic neuropathy and post-herpetic neuralgia. In an animal model of oxaliplatin-induced neuropathy, a complex panel of pharmacodynamic targets may account for the different pharmacological effects [
53]. Indeed, PEA can increase the antioxidant defense reducing oxidative stress, a characteristic feature of oxaliplatin neurotoxicity strongly related to pain. Moreover, the activation of PPAR-α has a pivotal role in PEA-mediated pain relief and PEA modulation of microglial cells [
53]. The activity of PEA on immune cells has a role in regulating pain signaling and maintaining immunological balance, as well as in models of osteoarthritic pain [
54].
7.2. Central Neuropathic Pain: Navigating the Neural Landscape
Central neuropathic pain (CNP) is closely linked to peripheral neuropathic pain, as both disorders are characterized by abnormal communication in the nervous system [
50]. PEA, known for its ability to protect the nervous system and reduce inflammation, is a possible treatment option. Research indicates that controlling neuroinflammation by PEA may help alleviate peripheral neuropathic pain and reduce central sensitization in chronic neuropathic pain [
16]. PEA's dual action makes it a good option for total relief of neuropathic pain by targeting interconnected pathways in the central and peripheral nervous systems [
50]. CNP, which originates from injury within the neurosensorial system, poses unique difficulties. The therapeutic efficacy of PEA in significant neuropathic pain is distinguished by its impact on glial cells, neuroinflammatory mechanisms, and the modulation of pain pathways within the central nervous system (CNS) [
55]. The therapeutic effectiveness of PEA in central neuropathic pain is significantly influenced by its effects on glial cells, particularly microglia and astrocytes. The maintenance of chronic pain states is associated with dysregulated activation of glial cells [
50]. The capacity of PEA to decrease the activation of glial cells mitigates neuroinflammation, disrupting the process of central sensitization and offering therapeutic benefits in situations like spinal cord injury or multiple sclerosis [
56].
In addition to its immediate analgesic benefits, PEA demonstrates neuroprotective qualities relevant to the central neuropathic pain framework. Research findings indicate that PEA may promote the survival and proper functioning of neurons, potentially alleviating the neurodegenerative effects commonly observed in chronic pain situations within the central nervous system [
51]. The modulation of pain pathways inside the CNS by PEA entails interactions with different mechanisms, including TRPV1 channels. PEA has a role in the modulation of pain signals by affecting the activity of TRPV1 [
52]. This mechanism of action provides relief in situations where nociceptive input is amplified due to central sensitization.
7.3. Clinical Evidence: From Bench to Bedside
The therapeutic potential of PEA in treating both peripheral and central neuropathic pain is supported by an expanding body of clinical evidence. Many experiments and studies have been conducted to examine the effectiveness of PEA in various neuropathic pain syndromes, yielding valuable insights into its clinical applicability [
52]. The efficacy of PEA in the management of diabetic neuropathy, which is a prevalent form of peripheral neuropathy, has been suggested [
32]. This publication has documented positive outcomes in terms of pain scores, nerve function, and quality of life among persons with diabetic neuropathy who received supplementation with PEA [
32].
The capacity of PEA to alleviate pain hypersensitivity and inflammation related to nerve injury has been emphasized in preclinical investigations [
57]. Within the domain of central neuropathic pain, specifically in disorders such as multiple sclerosis (MS), PEA has demonstrated potential. Improvements in pain scores and quality of life among individuals with MS who were administered PEA supplementation have been reported [
3,
58]. These findings indicate the possibility of PEA as a supplementary treatment for peripheral and central neuropathic pain linked to neurological illnesses.
8. Neuroinflammation and PEA: A Common Thread
PEA has been identified as a versatile drug with potential therapeutic efficacy in various CNS disorders consequent to neuroinflammation. The multiple modes of action exhibited by PEA render it an intriguing contender for addressing a range of illnesses that impact the CNS [
59]. We will try to examine the scientific underpinnings and clinical substantiation of the involvement of PEA in each of these central nervous system disorders.
Neuroinflammation is prevalent in numerous neurological illnesses. It assumes a crucial part in the development and advancement of various conditions, including dementia, Parkinson's disease, Alzheimer's disease, amyotrophic lateral sclerosis (ALS), and multiple sclerosis [
59]. PEA with its mentioned capacity to regulate immunological responses and mitigate neuroinflammatory processes may play a role in the reduction of neuroinflammation.
8.1. Dementia
Dementia represents a substantial worldwide health concern due to its manifestation of cognitive deterioration and memory impairment. The involvement of neuroinflammation has been identified in the advancement of different types of dementia [
5,
60]. A clinical study has suggested that the supplementation of PEA could provide advantages in the context of disorders connected to dementia [
60]. This research has documented enhancements in cognitive performance and a decrease in neuroinflammation among persons diagnosed with vascular dementia and Alzheimer's disease. Further studies would be very helpful.
8.2. Alzheimer's Disease
Alzheimer's disease is intricately associated with neuroinflammation, defined by forming beta-amyloid plaques and neurofibrillary tangles [
61]. The potential of PEA to modify inflammation and perhaps interfere in neurodegenerative processes has garnered significant interest in the field of Alzheimer's research. The clinical data is still limited, but recent research indicates that PEA might play a role in safeguarding neuronal integrity and cognitive function in models of Alzheimer's disease [
61]. Additional investigation is necessary to fully comprehend the extent of PEA's potential in Alzheimer's treatments.
8.3. Parkinson's Disease
Parkinson's disease is a neurodegenerative disorder that is characterized by the progressive loss of dopaminergic neurons [
22]. The pathophysiology of this illness involves neuroinflammatory processes, which have a role in the development and manifestation of motor symptoms [
22]. PEA would be a promising candidate for supplementary therapy in the treatment of Parkinson's disease. Studies suggest that PEA may demonstrate neuroprotective properties in experimental models of Parkinson's disease [
62,
63]. While clinical research in this particular domain is still developing, preclinical findings indicate potential in targeting neuroinflammatory mechanisms linked to Parkinson's disease.
8.4. Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis (ALS) is associated with neuroinflammation, which is recognized as a contributing factor [
64]. PEA may have potential opportunities for addressing the inflammatory environment linked to ALS [
63]. The investigation of PEA's involvement in ALS within clinical studies is currently constrained, while studies indicate that PEA might demonstrate neuroprotective properties in ALS models [
64]. Research conducted on human populations is essential for determining the possible clinical usefulness in ALS patients.
8.5. Multiple Sclerosis
Multiple sclerosis (MS), an autoimmune demyelinating illness, is characterized by the presence of neuroinflammation as a prominent aspect. PEA might be a compelling option for treating neuroinflammation in MS [
65]. The findings of previous investigations indicate that PEA could serve as a therapeutic intervention for MS [
66]. These studies propose that PEA exhibits advantageous effects by diminishing neuroinflammation and safeguarding neurological function. Clinical investigation is needed to achieve a thorough comprehension of the role of PEA in the management of MS.
PEA has demonstrated in animal experiments its versatility and potential in effectively addressing a range of CNS diseases. The compound's ability to reduce inflammation, protect neurons, and modulate the immune system makes it a potential option for regulating the complex mechanisms involved in neurodegenerative and inflammatory conditions [
67]. Although the clinical landscape is still evolving, the available preclinical evidence and initial clinical observations indicate that PEA shows the potential to enhance outcomes for individuals affected by illnesses such as dementia, Parkinson's disease, Alzheimer's disease, ALS, and MS [
68]. The comprehensive investigation, examination of innovative compositions, and enhanced comprehension of individual patient variables are crucial in fully harnessing the therapeutic capabilities of PEA in the wide range of CNS disorders [
69,
70].
9. Conclusion
In conclusion, PEA is a natural product variously studied as supplementary pharmacological therapy in several clinical conditions. It has shown significant anti-inflammatory and neuroprotective properties. To the best of our knowledge, this is the most extensive narrative review on the molecule.
EquiPEA®, recently introduced in the market, might represent an advancement in tackling key obstacles related to the pharmacokinetics of conventional PEA formulations. EquiPEA® is addressed to enhancing the bioavailability, hence the efficacy of PEA therapy as an anti-inflammatory, antioxidant, and analgesic by reducing concerns related to bioavailability, targeted delivery, and stability. However, direct comparative clinical evaluations with PEA-um and other pharmaceutical preparations are necessary to understand the level of innovation brought into the field of PEA-based medicines. At the moment, this novel compound seems to represent an effective therapeutical opportunity for patients suffering from illnesses defined by chronic inflammation, oxidative stress, and pain. It exhibits considerable translational potential in personalized medicine, offering promising prospects for implementing tailored techniques in PEA therapy. This aligns with the ongoing paradigm shift towards personalized medicine. EquiPEA® would increase the clinical usefulness of PEA therapy across a range of central nervous system and inflammatory illnesses. The data present in the literature at the moment represent a promising route for further investigation.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Table S1. SANRA Score for quality assessment of the selected studies.
Acknowledgments
The authors are grateful to the Paolo Procacci Foundation for the support of the project. A warm gratitude goes also to Dr Samiullah Dahri for the support in the literature search, and to Dr Mahima Khatri and Dr Satesh Kumar for the analysis of the selected publications following the SANRA guidelines, and the preparation of Table S1 (Supplemental Material).
Conflicts of Interest
GV declares relationships as a component of the speakers’ bureau, consultant and member of advisory boards of: Abbott International; Berlin-Chemie; Dompé Farmaceutici (Italy); Epitech Group (Italy); Grünenthal; Inomed (Italy); Menarini Africa and Middle East (Abu Dhabi); Menarini Asia-Pacific (Singapore); Menarini Central America (Guatemala); Menarini International; L. Molteni & C. Dei Fratelli Alitti (Italy); Shionogi, Takeda (Italy); Viatris (Italy); Zambon (Italy). His laboratory has received research grants from CNR (Italy), Dompé Farmaceutici (Italy); Epitech Group (Italy); Fondazione Maugeri (Italy), Pfizer (Italy). DF declares relationships during the past 2 years as a conference speaker, member of advisory boards or consultant for the following pharmaceutical companies: Abiogen Pharma (Italy); Alfasigma (Italy); Angelini Industries (Italy); Bayer Italia (Italy); Grünenthal Italia (Italy); Lundbeck Italia (Italy); L. Molteni & C. Dei Fratelli Alitti (Italy); SPA (Italy); Sandoz (Italy); Viatris (Italy); Zambon (Italy). The other authors do not have conflict of interest to declare.
References
- Kritikou P, Vadalouca A, Rekatsina M, Varrassi G, Siafaka I. The Diagnostic Odyssey of Patients with Chronic Neuropathic Pain-Expert Opinion of Greek Pain Specialists. Clin Pract. 2023;13(1):166-176. [CrossRef]
- Di Stefano G, Di Lionardo A, Di Pietro G, Truini A. Neuropathic Pain Related to Peripheral Neuropathies According to the IASP Grading System Criteria. Brain Sci. 2020;11(1):1. [CrossRef]
- Landolfo E, Cutuli D, Petrosini L, Caltagirone C. Effects of Palmitoylethanolamide on Neurodegenerative Diseases: A Review from Rodents to Humans. Biomolecules. 2022 May 5;12(5):667. [CrossRef]
- Lang-Illievich K, Klivinyi C, Lasser C, Brenna CTA, Szilagyi IS, Bornemann-Cimenti H. Palmitoylethanolamide in the Treatment of Chronic Pain: A Systematic Review and Meta-Analysis of Double-Blind Randomized Controlled Trials. Nutrients. 2023;15(6):1350. [CrossRef]
- Assogna M, Di Lorenzo F, Martorana A, Koch G. Synaptic Effects of Palmitoylethanolamide in Neurodegenerative Disorders. Biomolecules. 2022;12(8):1161. [CrossRef]
- Baethge C, Goldbeck-Wood S, Mertens S. SANRA-a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4:5. [CrossRef]
- Petrosino S, Schiano Moriello A. Palmitoylethanolamide: A Nutritional Approach to Keep Neuroinflammation within Physiological Boundaries-A Systematic Review. Int J Mol Sci. 2020;21(24):9526. [CrossRef]
- Lang-Illievich K, Klivinyi C, Rumpold-Seitlinger G, Dorn C, Bornemann-Cimenti H. The Effect of Palmitoylethanolamide on Pain Intensity, Central and Peripheral Sensitization, and Pain Modulation in Healthy Volunteers-A Randomized, Double-Blinded, Placebo-Controlled Crossover Trial. Nutrients. 2022;14(19):4084. [CrossRef]
- D'Amico R, Impellizzeri D, Cuzzocrea S, Di Paola R. ALIAmides Update: Palmitoylethanolamide and Its Formulations on Management of Peripheral Neuropathic Pain. Int J Mol Sci. 2020;21(15):5330. [CrossRef]
- Petrosino S, Di Marzo V. The pharmacology of palmitoylethanolamide and first data on the therapeutic efficacy of some of its new formulations. Br J Pharmacol. 2017;174(11):1349-1365. [CrossRef]
- Gatti A, Lazzari M, Gianfelice V, Di Paolo A, Sabato E, Sabato AF. Palmitoylethanolamide in the treatment of chronic pain caused by different etiopathogenesis. Pain Med. 2012;13(9):1121-30. [CrossRef]
- Lambert DM, Vandevoorde S, Diependaele G, Govaerts SJ, Robert AR. Anticonvulsant activity of N-palmitoylethanolamide, a putative endocannabinoid, in mice. Epilepsia. 2001;42(3):321-7. [CrossRef]
- Romero TR, Resende LC, Guzzo LS, Duarte ID. CB1 and CB2 cannabinoid receptor agonists induce peripheral antinociception by activation of the endogenous noradrenergic system. Anesth Analg. 2013;116(2):463-72. [CrossRef]
- Esposito E, Impellizzeri D, Mazzon E, Paterniti I, Cuzzocrea S. Neuroprotective activities of palmitoylethanolamide in an animal model of Parkinson's disease. PLoS One. 2012;7(8):e41880. [CrossRef]
- Schmitz A, Anselme C, Ravallec M, Rebuf C, Simon JC, Gatti JL, Poirié M. The cellular immune response of the pea aphid to foreign intrusion and symbiotic challenge. PLoS One. 2012;7(7):e42114. [CrossRef]
- Paladini A, Fusco M, Cenacchi T, Schievano C, Piroli A, Varrassi G. Palmitoylethanolamide, a Special Food for Medical Purposes, in the Treatment of Chronic Pain: A Pooled Data Meta-analysis. Pain Physician. 2016;19(2):11-24. [PubMed]
- Passavanti MB, Alfieri A, Pace MC, Pota V, Sansone P, Piccinno G, Barbarisi M, Aurilio C, Fiore M. Clinical applications of palmitoylethanolamide in pain management: protocol for a scoping review. Syst Rev. 2019;8(1):9. [CrossRef]
- Varrassi G, Fusco M, Skaper SD, Battelli D, Zis P, Coaccioli S, Pace MC, Paladini A. A Pharmacological Rationale to Reduce the Incidence of Opioid Induced Tolerance and Hyperalgesia: A Review. Pain Ther. 2018;7(1):59-75. [CrossRef]
- D'Aloia A, Molteni L, Gullo F, Bresciani E, Artusa V, Rizzi L, Ceriani M, Meanti R, Lecchi M, Coco S, Costa B, Torsello A. Palmitoylethanolamide Modulation of Microglia Activation: Characterization of Mechanisms of Action and Implication for Its Neuroprotective Effects. Int J Mol Sci. 2021;22(6):3054. [CrossRef]
- Skaper SD, Facci L, Giusti P. Glia and mast cells as targets for palmitoylethanolamide, an anti-inflammatory and neuroprotective lipid mediator. Mol Neurobiol. 2013;48(2):340-52. [CrossRef]
- De Icco R, Greco R, Demartini C, Vergobbi P, Zanaboni A, Tumelero E, Reggiani A, Realini N, Sances G, Grillo V, Allena M, Tassorelli C. Spinal nociceptive sensitization and plasma palmitoylethanolamide levels during experimentally induced migraine attacks. Pain. 2021;162(9):2376-2385. [CrossRef]
- Brotini S, Schievano C, Guidi L. Ultra-micronized Palmitoylethanolamide: An Efficacious Adjuvant Therapy for Parkinson's Disease. CNS Neurol Disord Drug Targets. 2017;16(6):705-713. [CrossRef]
- Cristiano C, Avagliano C, Cuozzo M, Liguori FM, Calignano A, Russo R. The Beneficial Effects of Ultramicronized Palmitoylethanolamide in the Management of Neuropathic Pain and Associated Mood Disorders Induced by Paclitaxel in Mice. Biomolecules. 2022 Aug 20;12(8):1155. [CrossRef]
- Di Cesare Mannelli L, D'Agostino G, Pacini A, Russo R, Zanardelli M, Ghelardini C, Calignano A. Palmitoylethanolamide is a disease-modifying agent in peripheral neuropathy: pain relief and neuroprotection share a PPAR-alpha-mediated mechanism. Mediators Inflamm. 2013;2013:328797. [CrossRef]
- Guida F, Luongo L, Boccella S, Giordano ME, Romano R, Bellini G, Manzo I, Furiano A, Rizzo A, Imperatore R, Iannotti FA, D'Aniello E, Piscitelli F, Sca Rossi F, Cristino L, Di Marzo V, de Novellis V, Maione S. Palmitoylethanolamide induces microglia changes associated with increased migration and phagocytic activity: involvement of the CB2 receptor. Sci Rep. 2017;7(1):375. [CrossRef]
- Noce A, Albanese M, Marrone G, Di Lauro M, Pietroboni Zaitseva A, Palazzetti D, Guerriero C, Paolino A, Pizzenti G, Di Daniele F, Romani A, D'Agostini C, Magrini A, Mercuri NB, Di Daniele N. Ultramicronized Palmitoylethanolamide (um-PEA): A New Possible Adjuvant Treatment in COVID-19 patients. Pharmaceuticals (Basel). 2021;14(4):336. [CrossRef]
- Scuteri D, Guida F, Boccella S, Palazzo E, Maione S, Rodríguez-Landa JF, Martínez-Mota L, Tonin P, Bagetta G, Corasaniti MT. Effects of Palmitoylethanolamide (PEA) on Nociceptive, Musculoskeletal and Neuropathic Pain: Systematic Review and Meta-Analysis of Clinical Evidence. Pharmaceutics. 2022;14(8):1672. [CrossRef]
- Seol TK, Lee W, Park S, Kim KN, Kim TY, Oh YN, Jun JH. Effect of palmitoylethanolamide on inflammatory and neuropathic pain in rats. Korean J Anesthesiol. 2017;70(5):561-566. [CrossRef]
- Kamper, D. Palmitoylethanolamide (PEA) in the treatment of neuropathic pain: a case study. Nutr Health. 2022;28(2):265-269. [CrossRef]
- De Luca P, Camaioni A, Marra P, Salzano G, Carriere G, Ricciardi L, Pucci R, Montemurro N, Brenner MJ, Di Stadio A. Effect of Ultra-Micronized Palmitoylethanolamide and Luteolin on Olfaction and Memory in Patients with Long COVID: Results of a Longitudinal Study. Cells. 2022;11(16):2552. [CrossRef]
- Pieralice S, Vari R, Minutolo A, Maurizi AR, Fioriti E, Napoli N, Pozzilli P, Manfrini S, Maddaloni E. Biomarkers of response to alpha-lipoic acid ± palmitoiletanolamide treatment in patients with diabetes and symptoms of peripheral neuropathy. Endocrine. 2019;66(2):178-184. [CrossRef]
- Schifilliti C, Cucinotta L, Fedele V, Ingegnosi C, Luca S, Leotta C. Micronized palmitoylethanolamide reduces the symptoms of neuropathic pain in diabetic patients. Pain Res Treat. 2014;2014:849623. [CrossRef]
- Rankin L, Fowler CJ. The Basal Pharmacology of Palmitoylethanolamide. Int J Mol Sci. 2020;21(21):7942. [CrossRef]
- Bettoni I, Comelli F, Colombo A, Bonfanti P, Costa B. Non-neuronal cell modulation relieves neuropathic pain: efficacy of the endogenous lipid palmitoylethanolamide. CNS Neurol Disord Drug Targets. 2013 Feb 1;12(1):34-44. [CrossRef]
- Impellizzeri D, Bruschetta G, Cordaro M, Crupi R, Siracusa R, Esposito E, Cuzzocrea S. Micronized/ultramicronized palmitoylethanolamide displays superior oral efficacy compared to nonmicronized palmitoylethanolamide in a rat model of inflammatory pain. J Neuroinflammation. 2014 Aug 28;11:136. [CrossRef]
- Keppel Hesselink JM, Kopsky DJ. Palmitoylethanolamide, a neutraceutical, in nerve compression syndromes: efficacy and safety in sciatic pain and carpal tunnel syndrome. J Pain Res. 2015 Oct 23;8:729-34. [CrossRef]
- Puglia C, Blasi P, Ostacolo C, Sommella E, Bucolo C, Platania CBM, Romano GL, Geraci F, Drago F, Santonocito D, Albertini B, Campiglia P, Puglisi G, Pignatello R. Innovative Nanoparticles Enhance N-Palmitoylethanolamide Intraocular Delivery. Front Pharmacol. 2018 Mar 28;9:285. [CrossRef]
- Cetojević-Simin DD, Canadanović-Brunet JM, Bogdanović GM, Djilas SM, Cetković GS, Tumbas VT, Stojiljković BT. Antioxidative and antiproliferative activities of different horsetail (Equisetum arvense L.) extracts. J Med Food. 2010;13(2):452-9. [CrossRef]
- Asgharikhatooni A, Bani S, Hasanpoor S, Mohammad Alizade S, Javadzadeh Y. The effect of equisetum arvense (horse tail) ointment on wound healing and pain intensity after episiotomy: a randomized placebo-controlled trial. Iran Red Crescent Med J. 2015;17(3):e25637. [CrossRef]
- Boqué N, Valls RM, Pedret A, Puiggrós F, Arola L, Solà R. Relative absorption of silicon from different formulations of dietary supplements: a pilot randomized, double-blind, crossover post-prandial study. Sci Rep. 2021;11(1):16479. [CrossRef]
- Ruga S, Galla R, Ferrari S, Invernizzi M, Uberti F. Novel Approach to the Treatment of Neuropathic Pain Using a Combination with Palmitoylethanolamide and Equisetum arvense L. in an In Vitro Study. Int J Mol Sci. 2023;24(6):5503. [CrossRef]
- Ardizzone A, Fusco R, Casili G, Lanza M, Impellizzeri D, Esposito E, Cuzzocrea S. Effect of Ultra-Micronized-Palmitoylethanolamide and Acetyl-l-Carnitine on Experimental Model of Inflammatory Pain. Int J Mol Sci. 2021;22(4):1967. [CrossRef]
- Rekatsina M, Paladini A, Piroli A, Zis P, Pergolizzi JV, Varrassi G. Pathophysiology and Therapeutic Perspectives of Oxidative Stress and Neurodegenerative Diseases: A Narrative Review. Adv Ther. 2020;37(1):113-139. [CrossRef]
- Esposito E, Cuzzocrea S. Palmitoylethanolamide in homeostatic and traumatic central nervous system injuries. CNS Neurol Disord Drug Targets. 2013;12(1):55-61. [CrossRef]
- Kriek, R. Palmitoylethanolamide: problems regarding micronization, ultra-micronization and additives. Inflammopharmacology. 2014;22(3):195-8. [CrossRef]
- Silva M, Martins D, Charrua A, Piscitelli F, Tavares I, Morgado C, Di Marzo V. Endovanilloid control of pain modulation by the rostroventromedial medulla in an animal model of diabetic neuropathy. Neuropharmacology. 2016;107:49-57. [CrossRef]
- Wallace VC, Segerdahl AR, Lambert DM, Vandevoorde S, Blackbeard J, Pheby T, Hasnie F, Rice AS. The effect of the palmitoylethanolamide analogue, palmitoylallylamide (L-29) on pain behaviour in rodent models of neuropathy. Br J Pharmacol. 2007;151(7):1117-28. [CrossRef]
- Indraccolo U, Favilli A, Dell'Anna A, Di Francesco A, Dionisi B, Giugliano E, Murina F, Stocco E. Looking for Responders among Women with Chronic Pelvic Pain Treated with a Comicronized Formulation of Micronized Palmitoylethanolamide and Polydatin. Biomed Res Int. 2022;2022:8620077. [CrossRef]
- Maghfour J, Rietcheck H, Szeto MD, Rundle CW, Sivesind TE, Dellavalle RP, Lio P, Dunnick CA, Fernandez J, Yardley H. Tolerability profile of topical cannabidiol and palmitoylethanolamide: a compilation of single-centre randomized evaluator-blinded clinical and in vitro studies in normal skin. Clin Exp Dermatol. 2021;46(8):1518-1529. [CrossRef]
- Lama A, Pirozzi C, Severi I, Morgese MG, Senzacqua M, Annunziata C, Comella F, Del Piano F, Schiavone S, Petrosino S, Mollica MP, Diano S, Trabace L, Calignano A, Giordano A, Mattace Raso G, Meli R. Palmitoylethanolamide dampens neuroinflammation and anxiety-like behavior in obese mice. Brain Behav Immun. 2022;102:110-123. [CrossRef]
- Luongo L, Guida F, Boccella S, Bellini G, Gatta L, Rossi F, de Novellis V, Maione S. Palmitoylethanolamide reduces formalin-induced neuropathic-like behaviour through spinal glial/microglial phenotypical changes in mice. CNS Neurol Disord Drug Targets. 2013;12(1):45-54. [CrossRef]
- Hesselink JM, Hekker TA. Therapeutic utility of palmitoylethanolamide in the treatment of neuropathic pain associated with various pathological conditions: a case series. J Pain Res. 2012;5:437-42. [CrossRef]
- Di Cesare Mannelli L, Pacini A, Corti F, Boccella S, Luongo L, Esposito E, Cuzzocrea S, Maione S, Calignano A, Ghelardini C. Antineuropathic profile of N-palmitoylethanolamine in a rat model of oxaliplatin-induced neurotoxicity. PLoS One. 2015;10(6):e0128080. [CrossRef]
- Britti D, Crupi R, Impellizzeri D, Gugliandolo E, Fusco R, Schievano C, Morittu VM, Evangelista M, Di Paola R, Cuzzocrea S. A novel composite formulation of palmitoylethanolamide and quercetin decreases inflammation and relieves pain in inflammatory and osteoarthritic pain models. BMC Vet Res. 2017;13(1):229. [CrossRef]
- Petrosino S, Schiano Moriello A, Verde R, Allarà M, Imperatore R, Ligresti A, Mahmoud AM, Peritore AF, Iannotti FA, Di Marzo V. Palmitoylethanolamide counteracts substance P-induced mast cell activation in vitro by stimulating diacylglycerol lipase activity. J Neuroinflammation. 2019;16(1):274. [CrossRef]
- Keith JM, Jones WM, Pierce JM, Seierstad M, Palmer JA, Webb M, Karbarz MJ, Scott BP, Wilson SJ, Luo L, Wennerholm ML, Chang L, Brown SM, Rizzolio M, Rynberg R, Chaplan SR, Breitenbucher JG. Heteroarylureas with spirocyclic diamine cores as inhibitors of fatty acid amide hydrolase. Bioorg Med Chem Lett. 2014;24(3):737-41. [CrossRef]
- Gugliandolo E, D'amico R, Cordaro M, Fusco R, Siracusa R, Crupi R, Impellizzeri D, Cuzzocrea S, Di Paola R. Effect of PEA-OXA on neuropathic pain and functional recovery after sciatic nerve crush. J Neuroinflammation. 2018;15(1):264. [CrossRef]
- Valenza M, Facchinetti R, Steardo L, Scuderi C. Palmitoylethanolamide and White Matter Lesions: Evidence for Therapeutic Implications. Biomolecules. 2022;12(9):1191. [CrossRef]
- Ajenikoko MK, Ajagbe AO, Onigbinde OA, Okesina AA, Tijani AA. Review of Alzheimer's disease drugs and their relationship with neuron-glia interaction. IBRO Neurosci Rep. 2022;14:64-76. [CrossRef]
- Colizzi M, Bortoletto R, Colli C, Bonomo E, Pagliaro D, Maso E, Di Gennaro G, Balestrieri M. Therapeutic effect of palmitoylethanolamide in cognitive decline: A systematic review and preliminary meta-analysis of preclinical and clinical evidence. Front Psychiatry. 2022;13:1038122. [CrossRef]
- Crupi R, Navarra M, Cuzzocrea S, Esposito E. The Association of Palmitoylethanolamide with Luteolin Decreases Neuroinflammation and Stimulates Autophagy in Parkinson's Disease Model. CNS Neurol Disord Drug Targets. 2015;14(10):1350-65. [CrossRef]
- Cordaro M, Cuzzocrea S, Crupi R. An Update of Palmitoylethanolamide and Luteolin Effects in Preclinical and Clinical Studies of Neuroinflammatory Events. Antioxidants (Basel). 2020 Mar 5;9(3):216. [CrossRef]
- Siracusa R, Paterniti I, Impellizzeri D, Cordaro M, Crupi R, Navarra M, Cuzzocrea S, Esposito E. The Association of Palmitoylethanolamide with Luteolin Decreases Neuroinflammation and Stimulates Autophagy in Parkinson's Disease Model. CNS Neurol Disord Drug Targets. 2015;14(10):1350-65. [CrossRef]
- Clemente, S. Amyotrophic lateral sclerosis treatment with ultramicronized palmitoylethanolamide: a case report. CNS Neurol Disord Drug Targets. 2012;11(7):933-6. [CrossRef]
- Zimmermann T, Bartsch JC, Beer A, Lomazzo E, Guggenhuber S, Lange MD, Bindila L, Pape HC, Lutz B. Impaired anandamide/palmitoylethanolamide signaling in hippocampal glutamatergic neurons alters synaptic plasticity, learning, and emotional responses. Neuropsychopharmacology. 2019;44(8):1377-1388. [CrossRef]
- Orefice NS, Alhouayek M, Carotenuto A, Montella S, Barbato F, Comelli A, Calignano A, Muccioli GG, Orefice G. Oral Palmitoylethanolamide Treatment Is Associated with Reduced Cutaneous Adverse Effects of Interferon-β1a and Circulating Proinflammatory Cytokines in Relapsing-Remitting Multiple Sclerosis. Neurotherapeutics. 2016;13(2):428-38. [CrossRef]
- Bellanti F, Bukke VN, Moola A, Villani R, Scuderi C, Steardo L, Palombelli G, Canese R, Beggiato S, Altamura M, Vendemiale G, Serviddio G, Cassano T. Effects of Ultramicronized Palmitoylethanolamide on Mitochondrial Bioenergetics, Cerebral Metabolism, and Glutamatergic Transmission: An Integrated Approach in a Triple Transgenic Mouse Model of Alzheimer's Disease. Front Aging Neurosci. 2022;14:890855. [CrossRef]
- Mattace Raso G, Russo R, Calignano A, Meli R. Palmitoylethanolamide in CNS health and disease. Pharmacol Res. 2014;86:32-41. [CrossRef]
- Di Filippo M, Pini LA, Pelliccioli GP, Calabresi P, Sarchielli P. Abnormalities in the cerebrospinal fluid levels of endocannabinoids in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2008 Nov;79(11):1224-9. [CrossRef]
- Jean-Gilles L, Feng S, Tench CR, Chapman V, Kendall DA, Barrett DA, Constantinescu CS. Plasma endocannabinoid levels in multiple sclerosis. J Neurol Sci. 2009 Dec 15;287(1-2):212-5. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).