Submitted:
05 March 2024
Posted:
06 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
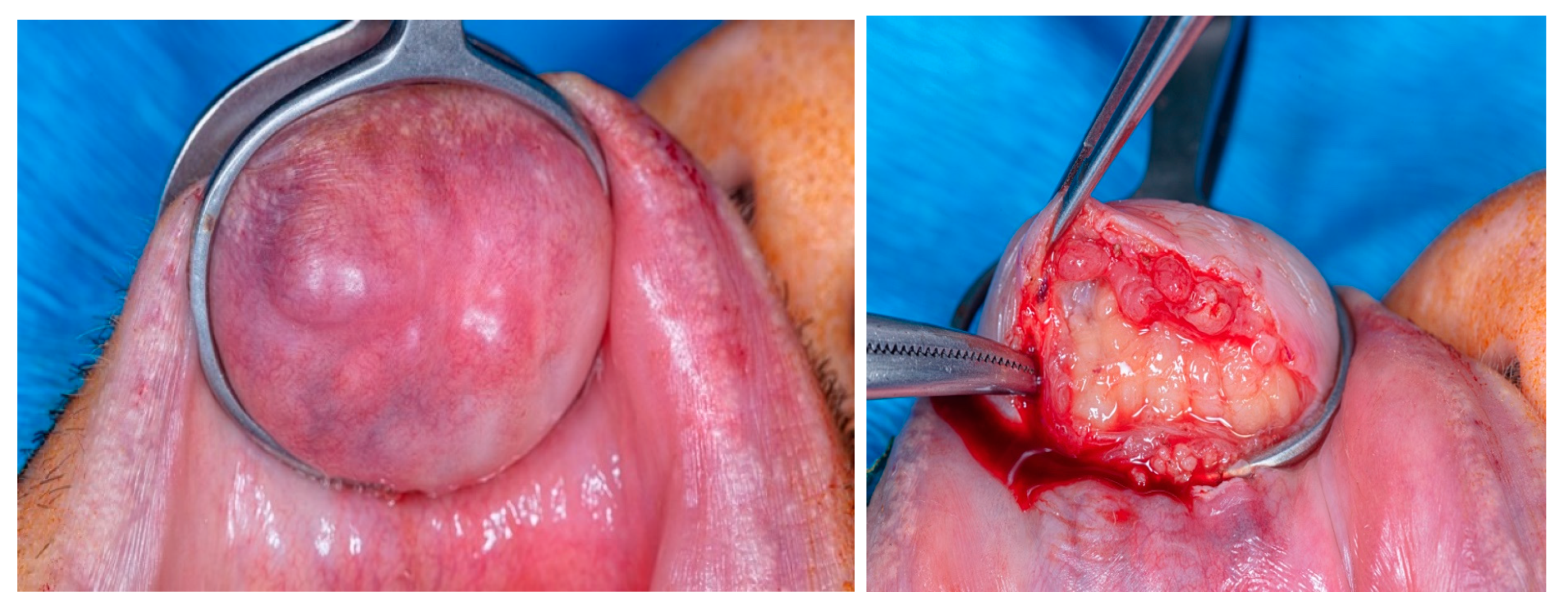
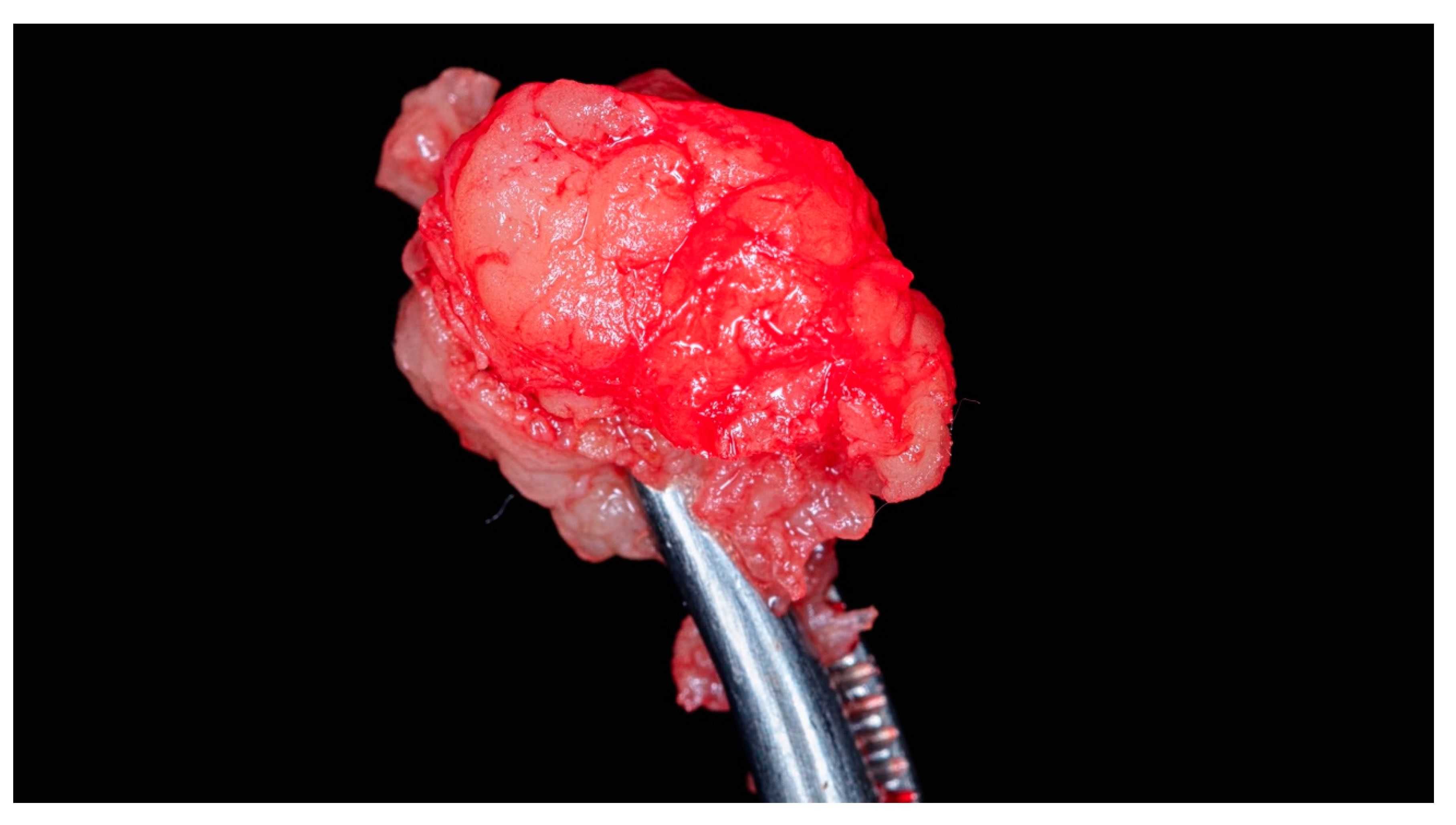
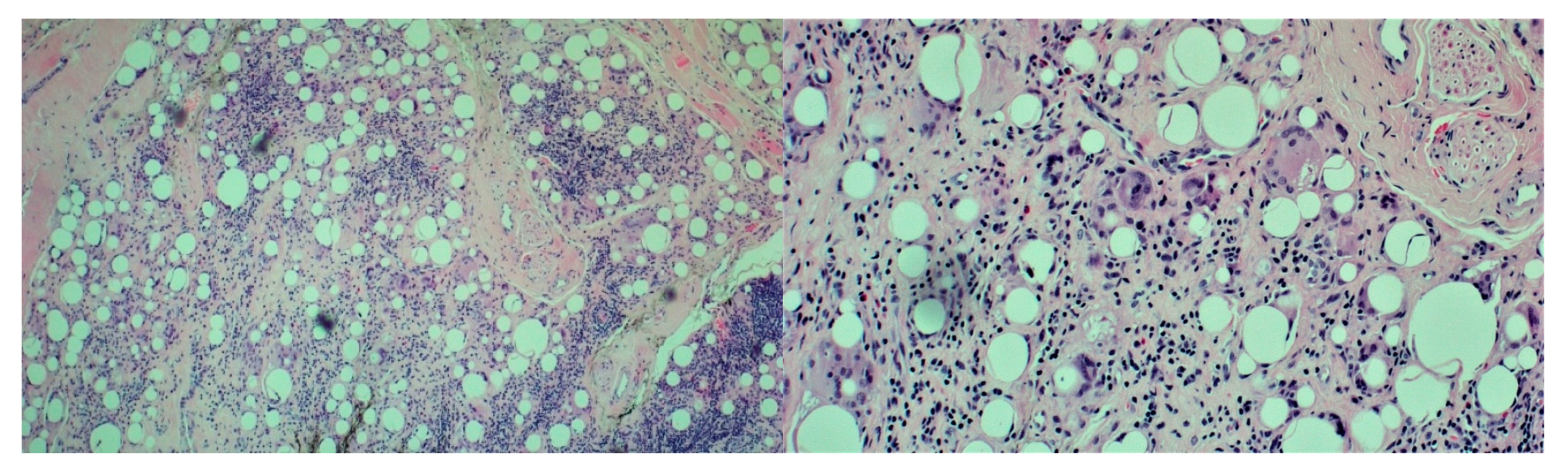
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schmidt-Westhausen, A.; Frege, J.; Reichart, P. Abscess formation after lip augmentation with silicone: case report. Int J Oral Maxillofac Surg 2004, 33(2), 198–200. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Miller, P.J. Management of lip complications. Facial Plast Surg Clin North Am 2019, 27(4), 565–570. [Google Scholar] [CrossRef] [PubMed]
- Rivkin, A.; Weinkle, S.H.; Hardas, B.; et al. Safety and effectiveness of repeat treatment with VYC-15L for lip and perioral enhancement: results from a prospective multicenter study. Aesthet Surg J 2019, 39, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Ajuz, D.; Oliveira, M.D.; Fernandes, J.C.H.; Fernandes, G.V.d.O. Facial Hemiplegia Treated with Botulinum Toxin: A Case Report. Diseases 2022, 10, 67. [Google Scholar] [CrossRef] [PubMed]
- Lemperle, G.; Morhenn, V.; Charrier, U. Human histology and persistence of various injectable filler substances for soft tissue augmentation. Aesthetic Plast Surg 2003, 27(5), 354–367. [Google Scholar] [CrossRef]
- Johl, S.S.; Burgett, R.A. Dermal filler agents: a practical review. Curr Opin Ophthalmol 2006, 17, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Clymer, M.A. Evolution in techniques: lip augmentation. Facial Plast Surg 2007, 23, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Rauso, R. 5-year study of a polyacrylamide hydrogel-based filler for rehabilitation of HIV-related facial lipoatrophy. Aesthet Surg J 2015, 35, 1021–1029. [Google Scholar] [CrossRef]
- Moscona, R.A. , Fodor, L. A retrospective study on liquid injectable silicone for lip augmentation: long -term results and patient satisfaction. J Plast Reconstr Aesthet Surg; 2010; 63, pp. 1694–1698. [Google Scholar] [CrossRef]
- Alster, T.S.; West, T.B. Human-derived and new synthetic injectable materials for soft-tissue augmentation: current status and role in cosmetic surgery. Plast Reconstr Surg 2000, 105, 2515. [Google Scholar] [CrossRef]
- Smith, K.C. Reversible versus nonreversible fillers in facial aesthetics: concerns and considerations. Dermatol Online J 2008, 14, 3. [Google Scholar] [CrossRef]
- Hirsch, R.J.; Stier, M. Complications of soft tissue augmentation. J Drugs Dermatol 2008, 7, 841–845. [Google Scholar] [PubMed]
- Salles, A.G.; Lotierzo, P.H.; Gemperli, R.; Besteiro, J.M.; Ishida, L.C.; Gimenez, R.P.; Menezes, J.; Ferreira, M.C. Complications after polymethylmethacrylate injections: report of 32 cases. Plast Reconstr Surg 2008, 121, 1811–1820. [Google Scholar] [CrossRef] [PubMed]
- Abtahinaeini, B.; Faghihi, G.; Shahmoradi, Z.; Saffaei, A. Filler migration and extensive lesions after lip augmentation: Adverse effects of polydimethylsiloxane filler. J Cosmet Dermatol 2018, 17(6), 996–999. [Google Scholar] [CrossRef] [PubMed]
- Fulton Jr, J.E.; Porumb, S.; Caruso, J.C.; Shitabata, P.K. Lip augmentation with liquid silicone. J Dermatol Surg 2005, 31, 1577–1586. [Google Scholar] [CrossRef] [PubMed]
- Pallua, N.; Wolter, T.P. A 5-year assessment of safety and aesthetic results after facial soft-tissue augmentation with polyacrylamide hydrogel (Aquamid): a prospective multicenter study of 251 patients. Plast Reconstr Surg 2010, 125, 1797–1804. [Google Scholar] [CrossRef] [PubMed]
- Hevia, O. Six-year experience using 1,000-centistoke silicone oil in 916 patients for soft-tissue augmentation in a private practice setting. Dermatol Surg 2009, 35 (Suppl 2), 1646–1652. [Google Scholar] [CrossRef] [PubMed]
- Kavoussi, H.; Ebrahimi, A. Delayed gel indurations as an adverse effect of polyacrylamide filler and its easy treatment. Dermatol Res Pract 2012, 2012, 4. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.R.; Holmes, R.E. Artecoll: a long-lasting injectable wrinkle filler material: report of a controlled, randomized, multicenter clinical trial of 251 subjects. Plast Reconstr Surg 2004, 114, 964–976. [Google Scholar] [CrossRef]
- Rauso, R.; Califano, L.; Rugge, L.; et al. Late onset complications secondary to polyacrylamide hydrogel-based filler for rehabilitation of HIV-related facial lipoatropy. Aesthet Surg J 2018, 38, N170–N174. [Google Scholar] [CrossRef]
- Salles, A.G.; Lotierzo, P.H.; Gemperli, R.; et al. Complications after polymethylmethacrylate injections: report of 32 cases. Plast Reconstr Surg 2008, 121, 1811–1820. [Google Scholar] [CrossRef]
- Park, T.H.; Seo, S.W.; Kim, J.K.; et al. Clinical experience with polymethylmethacrylate microsphere filler complications. Aesthetic Plast Surg 2012, 36, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Rauso, R.; Curinga, G.; Rusciani, A.; et al. Safety and efficacy of one-step rehabilitation of human immunodeficiency virus-related facial lipoatrophy using an injectable calcium hydroxyapatite dermal filler. Dermatol Surg 2013, 39, 1887–1894. [Google Scholar] [CrossRef] [PubMed]
- Rohrich, R.J. Advances in facial rejuvenation: botulinum toxin A, hyaluronic acid dermal fillers, and combination therapies-consensus recommendations. Plast Reconstr Surg 2008, 121, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Bergeret-Galley, C.; Latouche, X.; Illouz, Y.G. The value of a new filler material in corrective and cosmetic surgery: DermaLive and DermaDeep. Aesthetic Plast Surg 2001, 25, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Requena, C.; Izquierdo, M.J.; Navarro, M.; et al. Adverse reactions to injectable aesthetic microimplants. Am J Dermatopathol 2001, 23, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Lemperle, G.; Rullan, P.P.; Gauthier-Hazan, N. Avoiding and treating dermal filler complications. Plast Reconstr Surg 2006, 118 (Suppl. S3), 92S–107S. [Google Scholar] [CrossRef] [PubMed]
- Gladstone, H.B.; Cohen, J.L. Adverse effects when injecting facial fillers. Semin Cutan Med Surg 2007, 26, 34–39. [Google Scholar] [CrossRef]
- Broder, K.W.; Cohen, S.R. An overview of permanent and semipermanent fillers. Plast Reconstr Surg 2006, 118(3 Suppl), 7S–14S. [Google Scholar] [CrossRef]
- Sanchis-Bielsa, J.M.; Bagán, J.V.; Poveda, R.; Salvador, I. Foreign body granulomatous reactions to cosmetic fillers: a clinical study of 15 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009, 108(2), 237–241. [Google Scholar] [CrossRef]
- Lombardi, T.; Samson, J.; Plantier, F.; Husson, C.; Küffer, R. Orofacial granulomas after injection of cosmetic fillers. Histopathologic and clinical study of 11 cases. J Oral Pathol Med 2004, 33, 115–120. [Google Scholar] [CrossRef]
- Jham, B.C.; Nikitakis, N.G.; Scheper, M.A.; Papadimitriou, J.C.; Levy, B.A.; Rivera, H. Granulomatous foreign-body reaction involving oral and perioral tissues after injection of biomaterials: a series of 7 cases and review of the literature. J Oral Maxillofac Surg 2009, 67(2), 280–285. [Google Scholar] [CrossRef]
- Stolman, L.P. Human collagen reactions. Dermatol Surg 2005, 31(11Pt 2) Pt 2, 1634. [Google Scholar] [CrossRef]
- Funt, D.; Pavicic, T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clin Cosmet Investig Dermatol 2013, 6, 295–316. [Google Scholar] [CrossRef] [PubMed]
- Monheit, G.D.; Rohrich, R.J. The nature of long-term fillers and the risk of complications. Dermatol Surg 2009, 35 (Suppl 2), 1598–1604. [Google Scholar] [CrossRef]
- Trinh, L.N.; McGuigan, K.C.; Gupta, A. Delayed Granulomas as a Complication Secondary to Lip Augmentation with Dermal Fillers: A Systematic Review. Surg J (N Y) 2022, 8, e69–e79. [Google Scholar] [CrossRef] [PubMed]
- Sage, R.J.; Chaffins, M.L.; Jouba, D.J. Granulomatous foreign body reaction to hyaluronic acid: report of a case after nasolabial fold augmentation and review of management. Derm Surg 2009, 35, 1696–1700. [Google Scholar] [CrossRef] [PubMed]
- Arin, M.J.; Bäte, J.; Krieg, T.; Hunzelmann, N. Silicone granuloma of the face treated with minocycline. J Am Acad Dermatol 2005, 52(2), S53–S56. [Google Scholar] [CrossRef]
- Baumann, L.S.; Halem, M.L. Lip silicone granulomatous foreign body reaction treated with aldara (imiquimod 5%). Dermatol Surg 2003, 29(4), 429–432. [Google Scholar] [CrossRef]
- Akrish, S.; Dayan, D.; Taicher, S.; Adam, I.; Nagler, R.M. Foreign body granulomas after injection of bio-alcamid for lip augmentation. Am J Otolaryngol 2009, 30, 356–359. [Google Scholar] [CrossRef]
- Hubmer, M.G.; Hoffmann, C.; Popper, H.; Scharnagl, E. Expanded polytetrafluoroethylene threads for lip augmentation induce foreign body granulomatous reaction. Plast Reconstr Surg 1999, 103(4), 1277–1279. [Google Scholar] [CrossRef]
- Mercer, S.E.; Kleinerman, R.; Goldenberg, G.; Emanuel, P.O. Histopathologic identification of dermal filler agents. J Drugs Dermatol 2010, 9, 1072–1078. [Google Scholar] [PubMed]
- Requena, L.; Requena, C.; Christensen, L.; Zimmermann, U.S.; Kutzner, H.; Cerroni, L. Adverse reactions to injectable soft tissue fillers. J Am Acad Dermatol 2011, 64, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Conejo-Mir, J.S.; Sanz Guirado, S.; Angel Muñoz, M. Adverse granulomatous reaction to Artecoll treated by intralesional 5-fluorouracil and triamcinolone injections. Dermatol Surg 2006, 32, 1079–1082. [Google Scholar]
- Christensen, L.; Breiting, V.; Janssen, M.; Vuust, J.; Hogdall, E. Adverse reactions to injectable soft tissue permanent fillers. Aesthetic Plast Surg 2005, 29, 34–48. [Google Scholar] [CrossRef] [PubMed]
- Pasternack, F.R.; Fox, L.P.; Engler, D.E. Silicone granulomas treated with etanercept. Arch Dermatol 2005, 141(1), 13–15. [Google Scholar] [CrossRef] [PubMed]
- Kastner, S.; Gonser, P.; Paprottka, F.; et al. Removal of polyacrylamide gel (Aquamid) from the lip as a solution for late-onset complications: our 8-year experience. Aesthetic Plast Surg 2018, 42, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Fanous, N.; Brousseau, V.J.; Yoskovitch, A. The ’bikini lip reduction’: a detailed approach to hypertrophic lips. Can J Plast Surg Winter 2007, 15, 205–210. [Google Scholar] [CrossRef]
- Rauso, R.; Califano, L.; Rugge, L.; et al. Surgical lip remodeling after injection of permanent filler. Aesthet Surg J 2019, 39, 565–571. [Google Scholar] [CrossRef]
- El-Nahas, M.A.; Ghareeb, F.M. Complicated facial filler management by facelift. Menoufia Med J 2021, 33, 1347–1351. [Google Scholar]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




