Introduction
As Brunschwig A. described total pelvic exenteration (TPE) in his first report [
1]: “This procedure represents the most radical surgical attack so far described for pelvic cancer and also would appear to be among the most radical of abdominal operations that have been carried out with some measure of consistency”; TPE is considered one of the most radical surgical procedures associated with high rates of morbidity and mortality [
2]. TPE is indicated for both, locally advanced and recurrent pelvic malignancies for curative or palliative intent. The management of the recurrence disease in pelvis is a significant challenge and it must be dealt in a reference Unit with an experienced multidisciplinary team.
Gynecological and rectal cancer are the most frequent indications for this aggressive procedure. In the case of rectal cancer relapse, it might be as only an anastomotic isolated recurrence or an extensive relapse with multiorgan infiltration of adjacent organs in the pelvis [
3] or in a high percentage of the cases, this relapse could be associated to distant metastases. For this reason, a complete preoperative work up is mandatory before considering a patient as candidate for a TPE [
4]. The selection of patients for a surgical approach in rectal cancer relapse must take into consideration the prior therapy, local extension and infiltration of different organs and the presence of distant metastases. This cautious selection could improve the survival in a very selective group of patients, always done in a multidisciplinary team. For rectal cancer recurrences to achieve a R0 resection means an improvement in the survival, sometimes associated to aggressive surgeries as TPE [
5]. In order to achieve a complete cytoreduction some perioperative techniques could be used as intraoperative radiotherapy (IORT) [
6] or sometimes neoadjuvant therapy is needed [
7]. For gynecological cancers, the use of TPE offers a chance of cure reaching 50% at 5 years. In all of these patients, the external pelvic radiation has been administered and sometimes brachytherapy combined with chemotherapy too. All this group of additional treatments could reduce the burden disease and the infiltration of adjacent structures, however, they could difficult the surgical resection due to tissue inflammation or fibrosis [
8]. The use of TPE for palliation is controversial, since the associated morbidity could be considered too high for a palliative procedure, but, in experienced Units into a multidisciplinary team, it could mitigate this morbidity and to offer an improvement in the quality of life for these patients [
9]. In order to reduce the morbidity and aggression for these patients the use of minimally invasive approach help on this objective, in our study we have shown a reducing in the length of stay up to 50% comparing with open approach, however the use of this approach is still marginal [
2]. The use of this aggressive procedure must be balanced against the high rates of morbidity that this procedure has, including a possible impairment of quality of life with the use of stomas for fecal and urinary diversion.
To minimize the aggression to our patients, a minimally invasive approach could be used for TPE. The first description of LTPE was done by C. Pomel et al. in 2003 with promising results [
10]. Despite these promising results, in the largest systematic review comparing open versus laparoscopic approach, LTPE is still not a standardized procedure in most of the advanced surgical oncology units. This may be due to technical difficulties associated with multi visceral resections or perhaps, the need for a multidisciplinary collaboration through a minimally invasive approach [
2]. The mentioned systematic review included 2009 patients who underwent pelvic exenteration of which only 121 patients underwent LTPE [
2], which means that in the hugest published experience, only a 6% of patients received a minimally invasive approach for TPE.
This study aims to describe the experience with the use of laparoscopy for TPE in a heterogeneous population with different advanced pelvic malignancies for curative or palliative intent and to compare the postoperative outcomes with the open approach. Considering the paucity of studies on either laparoscopic or robotic assisted approach for TPE, this comparative study could increase the evidence about this emerging procedure.
Methods
This is a retrospective study based on a prospective database of patients who underwent TPE in our Unit from 2013 to 2023. The study was approved by the ethics committee board and no additional intervention was performed on any patient outside the clinical practice. Informed consent was not required for this analysis and all data were anonymized. All patients signed the inform consent for the surgical procedure.
Inclusion criteria for this analysis were: i) patients with pelvic malignancies (rectum, cervix or other), primary or recurrent disease, for curative or palliative intent; ii) patients who underwent TPE (open or laparoscopic). Patients who underwent posterior or anterior pelvic exenteration or those with loss of information were excluded.
The primary objective was to compare early postoperative outcomes such as length of stay and morbidity between two types of approaches (laparoscopic vs. open). Oncologic outcomes were collected but were not a study item due to the heterogeneity of oncologic diseases and the different stages (curative and palliative). Morbidity was defined as Clavien-Dindo classification [
11], with major morbidity defined as CD ≥ III.
Technical Description
LTPE was performed according to the previously reported description [
12]. Briefly, the patient was placed in the Lloyd-Davies position and 4 trocars were placed according to the needs of the surgery. Thus, the surgical procedure is as follow: release of the sigmoid colon; identification of both ureters; meso-sigmoid dissection at the root of the inferior mesenteric artery, the inferior mesenteric artery is identified and clipped using a Hem-o-lock; sigmoid section at the cut point with a mechanical stapler; dissection of both ureters, following their course to the bladder where they are sectioned; continuing with the Total Mesorectal excision to elevator muscles; bilateral parametrial dissection and uterine vessels sealing in female patients; dissection of the perivesical peritoneum and completion of cystectomy; dissection and section of the urethra using an Endo-stapler; vaginal resection is completed; before perineal time, the ileal loop is marked for urinary diversion in right iliac fossa, ureter-ileal anastomosis is performed through a periumbilical mini-laparotomy, and colostomy is allocated In the left iliac fossa; perineal time the complete amputation is performed; finally, the muscular plane of the perineum, skin and vagina is primary closed, in most of the cases V-Y major gluteus flap is not needed.
Statistical Analysis
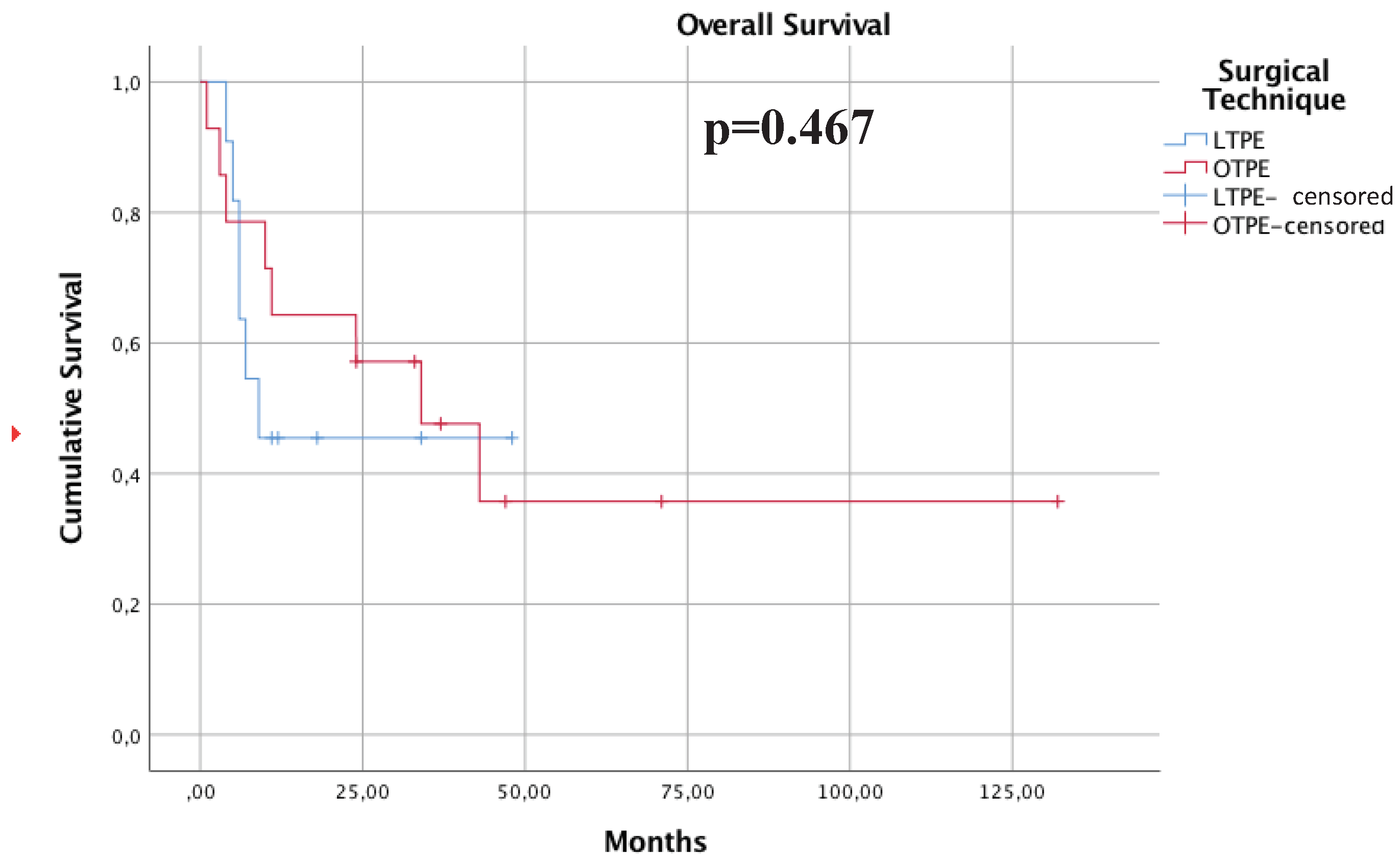
Normality criteria were tested on the cohort according to the Kolmogorov-Smirnov test. Due to a non-normal distribution, we applied the non-parametric Mann-Whitney U test for comparisons of quantitative variables and Chi-Square test for qualitative variables between LTPE and OTPE. Overall survival was estimated using the Kaplan-Meier method. Patients alive or lost to follow-up at data cut-off were censored at last contact according to this method, and the log-rank test was used for group comparisons. A p-value <0.05 was considered statistically significant. All statistical analyses were performed with SPSS version 24.0, version 3.04 (SPSS Inc., IBM Corp).
Results
A total of 19 patients who underwent surgery by a single surgeon between February 2013 and March 2023 were included in the analysis. All patients underwent total pelvic exenteration. LTPE was performed in 9/19 and OTPE in 10/19. Patient demographics varied between the two groups, with a mean age of 61.2 years for the laparoscopic approach and 53.7 years for the open approach. Only one male patient was included in the LTEP group (11%), whereas 5 male patients were included in the OTPE group (50%) (
Table 1).
The types of tumors treated by pelvic exenteration included 11 cervical (57%), 5 rectal (26%), 1 vaginal (5%), 1 sarcoma (5%), and 1 endometrial (5%) cancer. Among the 9 patients of LTEP group, there were 7 cervical (77%), 1 rectal (11%) and 1 (11%) vaginal origin. OTPE group included 4 cervical (40%), 4 rectal (40%), 1 endometrial (10%) cancer and 1 sarcoma (10%) without any case of vaginal cancer. The nature of the procedures was evaluated between both groups and showed that 89% of the total pelvic exenterations had curative intention while 11% had palliative intention. Out of 9 patients with LPE, 8 (88%) of them had curative nature while 1 (22%) had a palliative nature. OTPE group had mainly curative nature of the procedures (90%).
Complementary perioperative techniques were applied in both groups. Hyperthermic intraperitoneal chemotherapy was associated with LTPE due to a uterine leiomyosarcoma at the upper third of the cervix, which was difficult to delimit associating a high proliferative index of Ki67 (70%). In addition, one case of OTPE was treated with intraoperative radiotherapy due to a recurrence of low-grade endometrial stromal sarcoma.
Regarding surgical times, LTPE had a mean duration of 407 minutes, while OTPE had a mean duration of 367 minutes (p= 0.38). The mean length of hospital stay was reduced by up to half in LTPE (10.1 days) compared to OTPE (21.6 days) but did not reach statistical significance (p=0.26).
Surgical resection outcomes were evaluated and categorized into R0, R1, and R2. Excluding palliative surgery, LTPE showed 88.9% of R0 surgical procedures and OTPE achieved 70% R0. In terms of morbidity, major morbidity (≥grade III) was 45% in the LTPE group, without any case of death during the immediate postoperative period. Nevertheless, OTPE group had 40% (grade III/IV) with one case of death on 28
th postoperative day due to epileptic seizure caused by metastatic meningeal infiltration (
Table 1).
Survival Analysis
The median follow-up period for the entire cohort was 50 months. Kaplan–Meier survival curves are shown in
Figure 1. There were no statistical differences in overall survival (OS) between the LTPE and OTPE groups. Survival rates at the end of follow-up were 41% for the laparoscopic approach and 37% for the open approach. Despite the apparent disparity in percentages, statistical analysis revealed no significant differences (p = 0.467), suggesting that both approaches may provide similar survival outcomes.
Discussion
TPE is considered one of the most radical surgical procedures associated with high rates of morbidity and mortality [
2]. The use of minimally invasive approach for TPE remains controversial, collecting a very few studies. This retrospective and single institution study showed the feasibility of performing this procedure with similar results than open approach, improving the perioperative outcomes.
The most frequent indication for TPE is the recurrence from rectal or gynecological cancers. The management of the recurrence disease in pelvis is a significant challenge. For rectal cancer relapse the patients constitutes a very heterogenous group, they might present an anastomotic isolated recurrence or an extensive relapse with multiorgan infiltration of adjacent organs in the pelvis. This situation leads to not only an impairment in the survival but a impairment in the quality of life with untreatable pain or sepsis [
3]. Another important point is that the relapse happens in a pre-irradiated region, which makes more difficult the surgical approach or discards the treatment with another sequence of external beam radiotherapy. Additionally, the presence of local recurrence usually is associated to distant metastases making extremely difficult the complete management of these patients [
4]. The selection of patients for a surgical approach in rectal cancer relapse must take into consideration the prior therapy, local extension and infiltration of different organs and the presence of distant metastases. This cautious selection could improve the survival in very selective patients as we presented in our study, always done in a multidisciplinary team. The work up of these patients must include imaging tests to discard distant metastases as PET-CT and MRI to define the limits and the organ infiltrated by the relapse [
13]. The need of histologic confirmation is an important step before proceeding with extensive radical surgery, especially if induction chemoradiation is planned. However, sometimes the biopsy is not possible and on these situations with high suspicious of recurrence in imaging tests or PET-CT becomes reasonable the start of multimodality treatment.
For rectal cancer recurrences the complete radical resection is the key point to get the cure when a R0 is achieved, this sometimes requires aggressive surgeries as TPE, associating sometimes sacrectomies in posterior relapses [
5]. The use of this aggressive procedure must be balanced against the high rates of morbidity that this procedure has, including a possible impairment of quality of life with the use of stomas for fecal and urinary diversion. In our study we have used additional intraoperative therapies as IORT, this has demonstrated benefits to obtain a negative margin when a R1 resection is suspected. This IORT is usually used after external beam radiotherapy even one year later [
6]. The most of cases of bulky recurrences or primary rectal cancer underwent total neoadjuvant therapy including chemotherapy with FOLFOX or FOLFIRINOX following by long course of radiation [
7]. However, the worldwide experience in total pelvic exenteration using the laparoscopic approach remains scarce, being the presented study and important and comparative cohort showing benefits in the perioperative outcomes.
For gynecological cancers TPE offers a chance of cure reaching 50% at 5 years. In all of these patients external pelvic radiation has been administered and sometimes brachytherapy combined with chemotherapy. All this group of additional treatments could reduce the disease and the adjacent structures infiltrated, however, they could difficult the surgical resection due to tissue inflammation or fibrosis [
8]. Patients with cervical cancer recurrence who develop a pelvic recurrence may be candidates to TPE if a complete evaluation fails to reveal metastatic disease. In a systematic review of 21 studies of pelvic exenteration for gynecologic malignancy, resection with clear margins was achieved up to 97 percent of cases associating a postoperative mortality up to 5% [
9]. In our study most patients treated in our Unit were recurrences from cervical cancer, in other hand, two patients underwent TPE due to pelvic sepsis or uncontrollable leak or pain as palliative indication improving their quality of life instead of the diverting ostomies. The use of TPE for palliation is controversial, since the associated morbidity could be considered too high for a palliative procedure, however, in experienced Units into a multidisciplinary team could mitigate this morbidity and to offer an improvement in the quality of life for these patients [
14]. In order to reduce the morbidity and aggression for these patients the use of minimally invasive approach help on this objective, in our study we have shown a reducing in the length of stay up to 50% comparing with open approach, however the use of this approach is still marginal [
2].
TPE is still associated with a significant risk of morbidity. Therefore, careful planning and case selection are crucial to maximize survival and improve patient quality of life [
15]. In this sense, a coordinated multidisciplinary team approach can undoubtedly lead to high patient satisfaction and a reduction in short- and long-term morbidities [
16]. TPE, which removes most or all of the pelvic organs, is the only option for local control and potential cure in locally advanced colon or gynecologic cancers. However, TPE is sometimes offered in a palliative setting including patients with pelvic sepsis or uncontrollable pain due to side effects of intensive radiotherapy or local tumor progression [
15]. In our study, the included patients belong to both groups with satisfactory perioperative outcomes either by open or laparoscopic approach.
PELVEX international group aims to collect as much experience as possible about pelvic exenteration and to make recommendations, including that this procedure must be done in a reference unit wiht a multidisciplinary team to perform it. Several issues are discussed about TPE: i) type of urinary diversion, ii) use of mesh or not to cover the empty pelvis, iii) use of rectal, gracillis or gluteus flaps to cover the pelvic defect [
16].
In order to improve the perioperative outcomes for these patients, some reference units have developed the a minimally invasive approach (LTPE). To minimize the aggression to our patients, a minimally invasive approach could be used for TPE. Thus, the first description of LTPE was done by C. Pomel et al. in 2003 with promising results [
10]. Despite of these promising results in the huger systematic review to compare the open approach vs laparoscopic approach, the LTPE is not a standardized procedure in most of the advanced surgical oncology units, due to technical difficulties associated with multi-visceral resections or multidisciplinary approach by minimally invasive approach [
2]. This systematic review included 2009 patients who underwent pelvic exenteration of which only 121 patients were undergone to LTPE [
2], it means that in the hugest published experience only a 6% of patients receive a minimally invasive approach for TPE. However, robot assisted complex pelvic surgery has been proposed as a potential platform to overcome the challenges of LTPE, the use of a ‘wrist’ into the minor pelvic improve the capability of the surgeons to perform it, also robotic assisted surgery could help with the pelvic anatomical restrictions incorporating the 3-dimensions views [
2]. Robotic pelvic surgery provides enhanced views and a stable platform improving ergonomics for the operating surgeon resulting in lower conversion rates in rectal surgery. Also, robotic surgery has yet to demonstrate any clear advantage in terms of histopathological or survival outcomes for rectal and other pelvic cancers and it remains prohibitively expensive within some healthcare systems [
17]. Our study included 10 patients who underwent LTPE and showed an improvement in the perioperative outcomes associated with a reduction in the hospital stay to approximately 10 days, with similar morbidity and survival in cases of curative intent.
This study has the inherent weakness of retrospective case series studies, but the experience shown is in line with the international experience for this new technique. The findings from this study could help to improve the knowledge about this approach, considering it as an important alternative to the open approach.
In conclusion, LTPE is a feasible technique that could improve the perioperative outcomes in a very aggressive surgery with historically high morbidity condition. Maybe robotic-assisted LTPE could mitigate the difficulties of laparoscopic approach getting a more extensive acceptance for different groups worldwide.