Submitted:
06 March 2024
Posted:
07 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
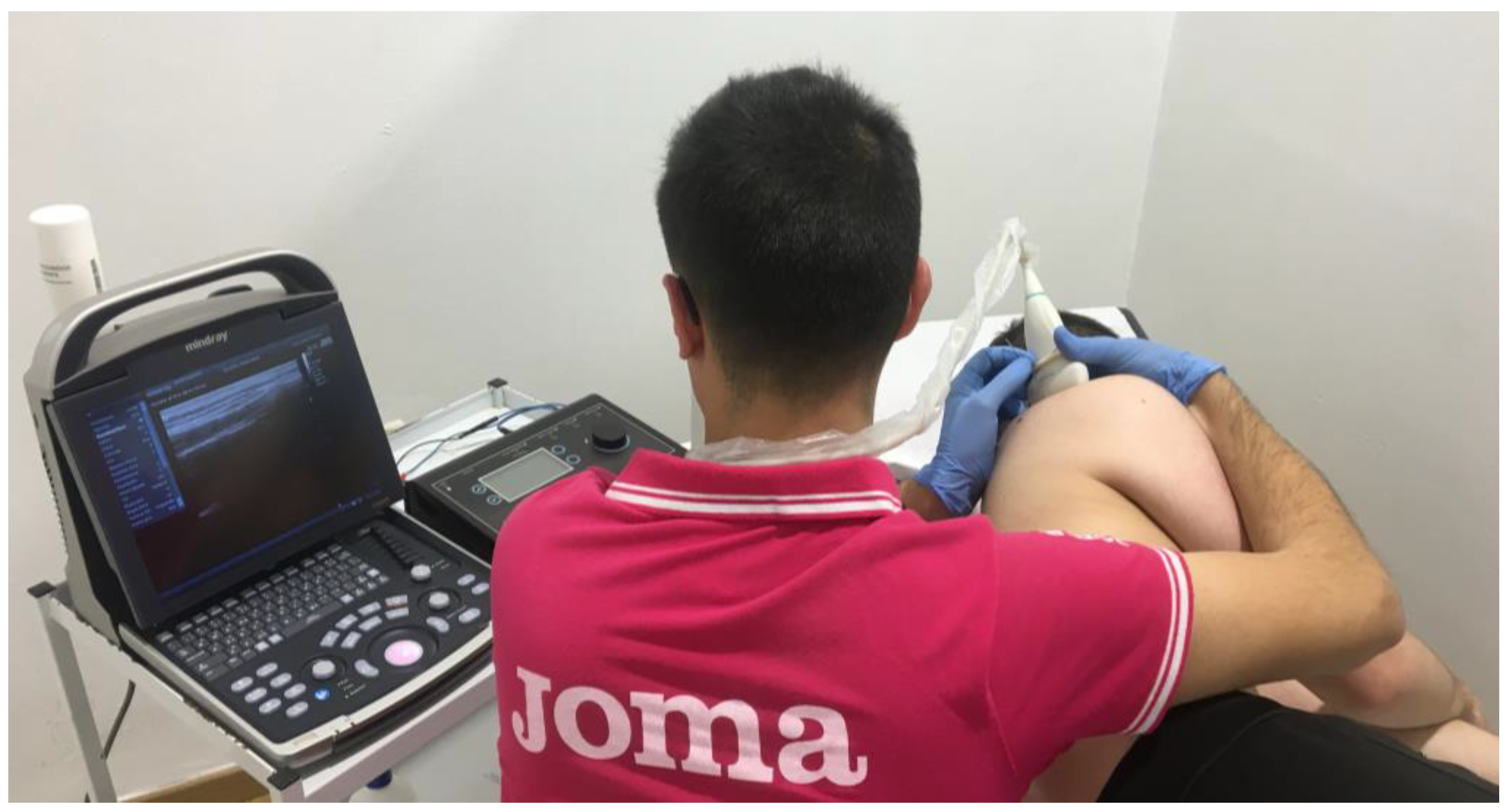
2. Materials and Methods
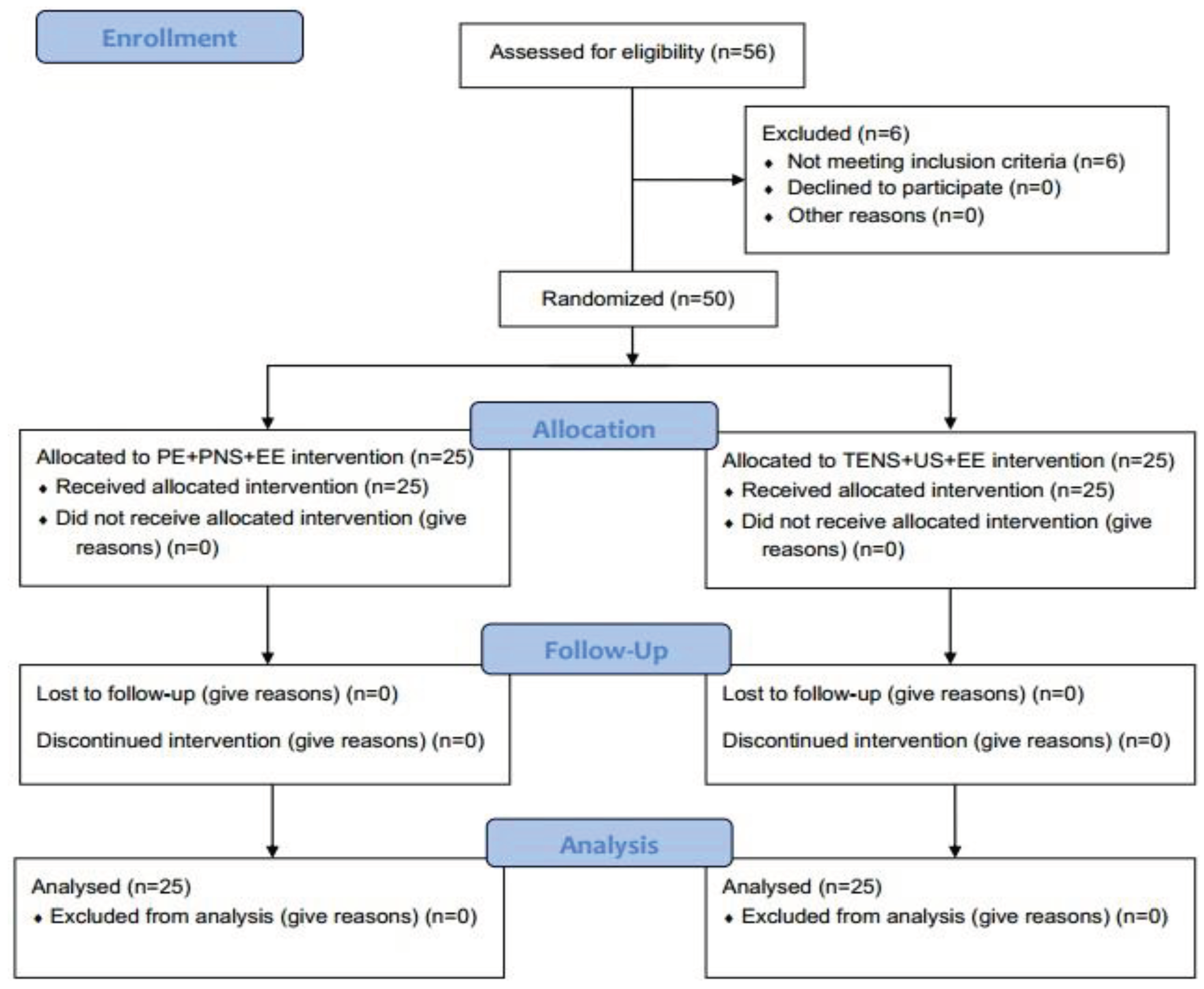
2.1. Study Design
2.2. Participants
2.3. Sample Size Calculation, Randomization and Blinding
2.4. Statistical Analysis
2.5. Outcomes Measurements
2.6. Interventions
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lipman, K.; Wang, C.; Ting, K.; Soo, C.; Zheng, Z. Tendinopathy: injury, repair, and current exploration. Drug Des. Devel. Ther. 2018, 12, 591–603. [Google Scholar] [CrossRef]
- Millar, N.L.; Silbernagel, K.G.; Thorborg, K.; Kirwan, P.D.; Galatz, L.M.; Abrams, G.D.; Murrell, G.A.C.; McInnes, I.B.; Rodeo, S.A. Tendinopathy. Nat. Rev. Dis. Prim. 2021, 7. [Google Scholar] [CrossRef]
- Andarawis-Puri, N.; Flatow, E.L. Promoting effective tendon healing and remodeling. J. Orthop. Res. 2018, 36, 3115–3124. [Google Scholar] [CrossRef]
- Joyce, D.; Robinson, K. Sport Science of Injury. In NSCA’s Essentials of Sport Science; French, D., Torres Ronda, L., Eds.; Human Kinetics Publishers Inc.: Champaign, 2022; ISBN 978-1-4925-9335-5. [Google Scholar]
- Chianca, V.; Albano, D.; Messina, C.; Midiri, F.; Mauri, G.; Aliprandi, A.; Catapano, M.; Pescatori, L.C.; Monaco, C.G.; Gitto, S.; et al. Rotator cuff calcific tendinopathy: from diagnosis to treatment. Acta Biomed. 2018, 89, 186–196. [Google Scholar] [CrossRef]
- Engebretsen, K.; Grotle, M.; Bautz-Holter, E.; Ekeberg, O.M.; Brox, J.I. Determinants of the Shoulder Pain and Disability Index in patients with subacromial shoulder pain. J. Rehabil. Med. 2010, 42, 499–505. [Google Scholar] [CrossRef]
- Doiron-Cadrin, P.; Lafrance, S.; Saulnier, M.; Cournoyer, É.; Roy, J.S.; Dyer, J.O.; Frémont, P.; Dionne, C.; MacDermid, J.C.; Tousignant, M.; et al. Shoulder Rotator Cuff Disorders: A Systematic Review of Clinical Practice Guidelines and Semantic Analyses of Recommendations. Arch. Phys. Med. Rehabil. 2020, 101, 1233–1242. [Google Scholar] [CrossRef]
- Lewis, J.S. Rotator cuff tendinopathy. Br. J. Sports Med. 2009, 43, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Osborne, J.D.; Gowda, A.L.; Wiater, B.; Wiater, J.M. Rotator cuff rehabilitation: Current theories and practice. Phys. Sportsmed. 2016, 44, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Littlewood, C.; Bateman, M.; Connor, C.; Gibson, J.; Horsley, I.; Jaggi, A.; Jones, V.; Meakins, A.; Scott, M. Physiotherapists’ recommendations for examination and treatment of rotator cuff related shoulder pain: A consensus exercise. Physiother. Pract. Res. 2019, 40, 87–94. [Google Scholar] [CrossRef]
- Arias-Buría, J.L.; Truyols-Domínguez, S.; Valero-Alcaide, R.; Salom-Moreno, J.; Atín-Arratibel, M.A.; Fernández-De-Las-Peñas, C. Ultrasound-Guided Percutaneous Electrolysis and Eccentric Exercises for Subacromial Pain Syndrome: A Randomized Clinical Trial. Evidence-based Complement. Altern. Med. 2015, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Huguet, M.; Góngora-Rodríguez, J.; Rodríguez-Huguet, P.; Ibañez-Vera, A.J.; Rodríguez-Almagro, D.; Martín-Valero, R.; Díaz-Fernández, Á.; Lomas-Vega, R. Effectiveness of Percutaneous Electrolysis in Supraspinatus Tendinopathy: A Single-Blinded Randomized Controlled Trial. J. Clin. Med. 2020, 9, 1837. [Google Scholar] [CrossRef] [PubMed]
- Valera-Garrido, F.; Minaya-Muñoz, F. Concepto y fundamentos de la electrolisis percutánea musculoesquelética (EPM). In Electrolisis percutánea musculoesquelética. Tendón y bursa; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, 2021; pp. 3–24. ISBN 978-84-9113-016-1. [Google Scholar]
- Minaya-Muñoz, F.; Valera-Garrido, F. Neuromodulación percutánea ecoguiada. In Fisioterapia invasiva; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, 2017; pp. 283–294. [Google Scholar]
- Sánchez-Ibáñez, J.; Colmena, C.; Benabent, J.; García-Herreros, S.; Valles, S.-L. New Technique in Tendon Sport Recovery. Percutaneous Electrolysis Intratissue (EPI®). Int. J. Phys. Med. Rehabil. 2013, 1, 1000113, http://dx.doi.org/10.4172/jpmr.1000113. [Google Scholar]
- Valera-Garrido, F.; Minaya-Muñoz, F.; Sánchez-Ibáñez, J.M.; García-Palencia, P.; Valderrama-Canales, F.; Medina-Mirapeix, F.; Polidori, F. Comparison of the Acute Inflammatory Response and Proliferation of Dry Needling and Electrolysis Percutaneous Intratissue (EPI®) in Healthy Rat Achilles Tendons. Br. J. Sports Med. 2013, 47, 29–30. [Google Scholar] [CrossRef]
- García-Bermejo, P.; De-La-Cruz-Torres, B.; Naranjo-Orellana, J.; Albornoz-Cabello, M. Autonomic Responses to Ultrasound-Guided Percutaneous Needle Electrolysis: Effect of Needle Puncture or Electrical Current? J. Altern. Complement. Med. 2018, 24, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Huguet, M.; Góngora-Rodríguez, J.; Lomas-Vega, R.; Martín-Valero, R.; Díaz-Fernández, Á.; Obrero-Gaitán, E.; Ibáñez-Vera, A.J.; Rodríguez-Almagro, D. Percutaneous Electrolysis in the Treatment of Lateral Epicondylalgia: A Single-Blind Randomized Controlled Trial. J. Clin. Med. 2020, 9, 2068. [Google Scholar] [CrossRef]
- Macías-Hernández, S.I.; Pérez-Ramírez, L.E. Fortalecimiento excéntrico en tendinopatías del manguito de los rotadores asociadas a pinzamiento subacromial. Evidencia actual. Cir. Cir. 2015, 83, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Dejaco, B.; Habets, B.; van Loon, C.; van Grinsven, S.; van Cingel, R. Eccentric versus conventional exercise therapy in patients with rotator cuff tendinopathy: a randomized, single blinded, clinical trial. Knee Surgery, Sport. Traumatol. Arthrosc. 2017, 25, 2051–2059. [Google Scholar] [CrossRef]
- Malliaras, P.; Johnston, R.; Street, G.; Littlewood, C.; Bennell, K.; Haines, T.; Buchbinder, R. The Efficacy of Higher Versus Lower Dose Exercise in Rotator Cuff Tendinopathy: A Systematic Review of Randomized Controlled Trials. Arch. Phys. Med. Rehabil. 2020, 101, 1822–1834. [Google Scholar] [CrossRef]
- Heron, S.; Woby, S.; Thompson, D. Comparison of three types of exercise in the treatment of rotator cuff tendinopathy/shoulder impingement syndrome: A randomized controlled trial. Physiotherapy 2017, 103. [Google Scholar] [CrossRef]
- Martinoli, C.; Beggs, I.; Bianchi, S.; Bueno, A.; Cohen, M.; Court-payen, M.; Grainger, A.; Kainberger, F.; Klauser, A.; Mcnally, E.; et al. Musculoskeletal ultrasound: technical guidelines. Insights Imaging 2010, 1, 99–141. [Google Scholar] [CrossRef]
- Jacobson, J.A. Shoulder US: anatomy, technique, and scanning pitfalls. Radiology 2011, 260, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Sheehan, S.E.; Orwin, J.F.; Lee, K.S. Comprehensive Shoulder US Examination: A Standardized Approach with Multimodality Correlation for Common Shoulder Disease. Radiogr. a Rev. Publ. Radiol. Soc. North Am. Inc 2016, 36, 1606–1627. [Google Scholar] [CrossRef] [PubMed]
- Kinsella, R.; Cowan, S.M.; Watson, L.; Pizzari, T. A comparison of isometric, isotonic concentric and isotonic eccentric exercises in the physiotherapy management of subacromial pain syndrome/rotator cuff tendinopathy: Study protocol for a pilot randomised controlled trial. Pilot Feasibility Stud. 2017, 3. [Google Scholar] [CrossRef] [PubMed]
- Thong, I.S.K.; Jensen, M.P.; Miró, J.; Tan, G. The validity of pain intensity measures: What do the NRS, VAS, VRS, and FPS-R measure? Scand. J. Pain 2018, 18, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.; Anwer, S.; Iqbal, A.; Iqbal, Z. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res 2018, 11, 851–856. [Google Scholar] [CrossRef]
- Beshay, N.; Lam, P.H.; Murrell, G.A.C. Assessing the Reliability of Shoulder Strength Measurement: Hand-Held versus Fixed Dynamometry. Shoulder Elb. 2011, 3, 244–251. [Google Scholar] [CrossRef]
- Holt, K.L.; Raper, D.P.; Boettcher, C.E.; Waddington, G.S.; Drew, M.K. Hand-held dynamometry strength measures for internal and external rotation demonstrate superior reliability, lower minimal detectable change and higher correlation to isokinetic dynamometry than externally-fixed dynamometry of the shoulder. Phys. Ther. Sport 2016, 21, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, L.; Oestergaard, L.G.; van Tulder, M.; Petersen, A.K. Measurement Properties of Isokinetic Dynamometry for Assessment of Shoulder Muscle Strength: A Systematic Review. Arch. Phys. Med. Rehabil. 2021, 102, 510–520. [Google Scholar] [CrossRef]
- Guzmán-Muñoz, E.; Méndez-Rebolledo, G. Electromiografía en las Ciencias de la Rehabilitación. Salud Uninorte 2018, 34, 753–765. [Google Scholar] [CrossRef]
- Sethi, K.; Noohu, M.M. Scapular muscles strengthening on pain, functional outcome and muscle activity in chronic lateral epicondylalgia. J. Orthop. Sci. 2018, 23, 777–782. [Google Scholar] [CrossRef]
- Valera-Garrido, F.; Minaya-Muñoz, F. Evaluación, descripción y guía ecográfica en la aplicación de la electrolisis percutánea en las tendinopatías y lesiones bursales. In Electrolisis percutánea musculoesquelética. Tendón y bursa; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, 2021; pp. 71–88. [Google Scholar]
- Valera-Garrido, F.; Minaya-Muñoz, F. Procedimientos invasivos ecoguiados en fisioterapia. In Fisioterapia invasiva; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, 2017; pp. 215–246. [Google Scholar]
- Papatheodorou, A.; Ellinas, P.; Takis, F.; Tsanis, A.; Maris, I.; Batakis, N. US of the shoulder: Rotator cuff and non-rotator cuff disorders. Radiographics 2006, 26. [Google Scholar] [CrossRef] [PubMed]
- Del-Castillo-González, F. Diagnóstico ecográfico. In Lesiones músculo-tendinosas en el medio deportivo; Del-Castillo-Campos, M.J., Ramos-Álvarez, J.J., Polo-Portes, C., Eds.; Dirección General de Juventud y Deportes. Consejería de Educación, Juventud y Deporte. Comunidad de Madrid: Madrid, 2017; pp. 74–82. [Google Scholar]
- Hervás, M.T.; Navarro Collado, M.J.; Peiró, S.; Rodrigo Pérez, J.L.; López Matéu, P.; Martínez Tello, I. Versión Española del cuestionario DASH. Adaptación transcultural, fiabilidad, validez y sensibilidad a los cambios. Med. Clin. (Barc). 2006, 127, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Torres-Lacomba, M.; Sánchez-Sánchez, B.; Prieto-Gómez, V.; Pacheco-da-Costa, S.; Yuste-Sánchez, M.J.; Navarro-Brazález, B.; Gutiérrez-Ortega, C. Spanish cultural adaptation and validation of the shoulder pain and disability index, and the oxford shoulder score after breast cancer surgery. Health Qual. Life Outcomes 2015, 13. [Google Scholar] [CrossRef]
- Valera-Garrido, F.; Minaya-Muñoz, F. Electrolisis percutánea en tendón y bursa. Metodología de aplicación. In Electrolisis percutánea musculoesquelética. Tendón y bursa; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, 2021; pp. 45–70. ISBN 978-84-9113-016-1. [Google Scholar]
- Valera-Garrido, F.; Minaya-Muñoz, F.; Pereira-Barbosa, M. Electrolisis percutánea ecoguiada en el manguito rotador. In Electrolisis percutánea musculoesquelética. Tendón y bursa; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, 2021; pp. 107–130. [Google Scholar]
- De-Miguel-Valtierra, L.; Salom-Moreno, J.; Fernández-de-las-Peñas, C.; Cleland, J.A.; Arias-Buría, J.L. Ultrasound-Guided Application of Percutaneous Electrolysis as an Adjunct to Exercise and Manual Therapy for Subacromial Pain Syndrome: A Randomized Clinical Trial. J. Pain 2018, 19, 1201–1210. [Google Scholar] [CrossRef]
- Maya-Martín, J.; Albornoz-Cabello, M. Estimulación eléctrica transcutánea. In Electroestimulación transcutánea y neuromuscular, y neuromodulación; Albornoz-Cabello, M., Maya-Martín, J., Eds.; Elsevier: Barcelona, 2021; pp. 1–76. ISBN 978-84-9113-606-4. [Google Scholar]
- Lin, M.L.; Chiu, H.W.; Shih, Z.M.; Lee, P.Y.; Li, P.Z.; Guo, C.H.; Luo, Y.J.; Lin, S.C.; Lin, K.Y.; Hsu, Y.M.; et al. Two transcutaneous stimulation techniques in shoulder pain: Transcutaneous Pulsed Radiofrequency (TPRF) versus transcutaneous electrical nerve stimulation (TENS): A comparative pilot study. Pain Res. Manag. 2019, 2019. [Google Scholar] [CrossRef]
- Gunay Ucurum, S.; Kaya, D.O.; Kayali, Y.; Askin, A.; Tekindal, M.A. Comparison of different electrotherapy methods and exercise therapy in shoulder impingement syndrome: A prospective randomized controlled trial. Acta Orthop. Traumatol. Turc. 2018, 52, 249–255. [Google Scholar] [CrossRef]
- Desmeules, F.; Boudreault, J.; Dionne, C.E.; Frémont, P.; Lowry, V.; MacDermid, J.C.; Roy, J.-S. Efficacy of exercise therapy in workers with rotator cuff tendinopathy: a systematic review. J. Occup. Health 2016, 58, 15-0103-RA. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Green, S.; Mrocki, M.A.; Surace, S.J.; Deitch, J.; Mcbain, B.; Lyttle, N.; Buchbinder, R. Electrotherapy modalities for rotator cuff disease. Cochrane Database Syst. Rev. 2016, 2016. [Google Scholar] [CrossRef]
- Balci, T.O.; Turk, A.C.; Sahin, F.; Kotevoglu, N.; Kuran, B. Efficacy of therapeutic ultrasound in treatment of adhesive capsulitis: A prospective double blind placebo-controlled randomized trial. J. Back Musculoskelet. Rehabil. 2018, 31, 955–961. [Google Scholar] [CrossRef]
- Cook, J.L.; Purdam, C.R. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br. J. Sports Med. 2009, 43, 409–416. [Google Scholar] [CrossRef]
- Rio, E.; Moseley, L.; Purdam, C.; Samiric, T.; Kidgell, D.; Pearce, A.J.; Jaberzadeh, S.; Cook, J. The pain of tendinopathy: physiological or pathophysiological? Sports Med. 2014, 44, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Rio, E.; Kidgell, D.; Lorimer Moseley, G.; Gaida, J.; Docking, S.; Purdam, C.; Cook, J. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. Br. J. Sports Med. 2016, 50, 209–215. [Google Scholar] [CrossRef]
- Calderón-Díez, L.; Sánchez-Sánchez, J.L.; Sánchez-Ibáñez, J.M.; Belón-Pérez, P. Percutaneous Electrolysis (EPI®), a Promising Technology in the Treatment of Insertional Patellar Tendinopathy in Soccer Players. 2023, 24–31, https://doi.org/10.1007/978-3-031-22356-3_3/COVER. [Google Scholar]
- Margalef, R.; Minaya-Muñoz, F.; Valera-Garrido, F.; Bosque, M.; Santafé, M.M. Changes in pH as a result of galvanic currents used in percutaneous needle electrolysis. Rev. Fisioter. Invasiva / J. Invasive Tech. Phys. Ther. 2020, 03, 006–006. [Google Scholar] [CrossRef]
- Peñín-Franch, A.; García-Vidal, J.A.; Martínez, C.M.; Escolar-Reina, P.; Martínez-Ojeda, R.M.; Gómez, A.I.; Bueno, J.M.; Minaya-Muñoz, F.; Valera-Garrido, F.; Medina-Mirapeix, F.; et al. Galvanic current activates the NLRP3 inflammasome to promote Type I collagen production in tendon. Elife 2022, 11, e73675. [Google Scholar] [CrossRef] [PubMed]
- Peñín-Franch, A.; García-Vidal, J.A.; Escolar-Reina, P.; Medina-Mirapeix, F.; Pelegrín-Vivancos, P. Electrolisis e inflamación. Bases biológicas de la electrolisis percutánea. In Electrolisis percutánea musculoesquelética. Tendón y bursa; Valera-Garrido, F., Minaya-Muñoz, F., Eds.; Elsevier: Barcelona, 2021; pp. 25–32. ISBN 978-84-9113-016-1. [Google Scholar]
- Sánchez-Sánchez, J.L.; Calderón-Díez, L.; Herrero-Turrión, J.; Méndez-Sánchez, R.; Arias-Buría, J.L.; Fernández-De-Las-Peñas, C. Changes in Gene Expression Associated with Collagen Regeneration and Remodeling of Extracellular Matrix after Percutaneous Electrolysis on Collagenase-Induced Achilles Tendinopathy in an Experimental Animal Model: A Pilot Study. J. Clin. Med. 2020, 9, 3316. [Google Scholar] [CrossRef]
- Albornoz-Cabello, M.; Castro-Sánchez, A.M. Neuromodulación periférica transcutánea. In Electroestimulación transcutánea y neuromuscular, y neuromodulación; Albornoz-Cabello, M., Maya-Martín, J., Eds.; Elsevier: Barcelona, 2021; pp. 171–196. ISBN 978-84-9113-606-4. [Google Scholar]
- Wilson, R.D.; Harris, M.A.; Gunzler, D.D.; Bennett, M.E.; Chae, J. Percutaneous peripheral nerve stimulation for chronic pain in subacromial impingement syndrome: A case series. Neuromodulation 2014, 17, 771–776. [Google Scholar] [CrossRef]
- Shi, L.L.; Freehill, M.T.; Yannopoulos, P.; Warner, J.J.P. Suprascapular nerve: is it important in cuff pathology? Adv. Orthop. 2012, 2012, 1–6. [Google Scholar] [CrossRef]
- Wu, W.T.; Chen, L.R.; Chang, H.C.; Chang, K.V.; Özçakar, L. Quantitative Ultrasonographic Analysis of Changes of the Suprascapular Nerve in the Aging Population With Shoulder Pain. Front. Bioeng. Biotechnol. 2021, 9, 640747. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, C.; Kwak, J.M.; Jung, H. won; Kholinne, E.; Jeon, I.H. Suprascapular nerve neuropathy leads to supraspinatus tendon degeneration. J. Orthop. Sci. 2020, 25, 588–594. [Google Scholar] [CrossRef]
- Nakanishi, Y.; Okada, T.; Takeuchi, N.; Kozono, N.; Senju, T.; Nakayama, K.; Nakashima, Y. Histological evaluation of tendon formation using a scaffold-free three-dimensional-bioprinted construct of human dermal fibroblasts under in vitro static tensile culture. Regen. Ther. 2019, 11, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Alfredson, H.; Ljung, B.O.; Thorsen, K.; Lorentzon, R. In vivo investigation of ECRB tendons with microdialysis technique--no signs of inflammation but high amounts of glutamate in tennis elbow. Acta Orthop. Scand. 2000, 71, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Croteau, F.; Robbins, S.M.; Pearsall, D. Hand-Held Shoulder Strength Measures Correlate With Isokinetic Dynamometry in Elite Water Polo Players. J. Sport Rehabil. 2021, 30, 1233–1236. [Google Scholar] [CrossRef] [PubMed]
- Boudreau, N.; Gaudreault, N.; Roy, J.S.; Bédard, S.; Balg, F. The addition of glenohumeral adductor coactivation to a rotator Cuff exercise program for rotator Cuff tendinopathy: A single-blind randomized controlled trial. J. Orthop. Sports Phys. Ther. 2019, 49, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.L.; Khan, K.M.; Maffulli, N.; Purdam, C. Overuse tendinosis, not tendinitis part 2: applying the new approach to patellar tendinopathy. Phys. Sportsmed. 2000, 28, 31–46. [Google Scholar] [CrossRef]
- Maenhout, A.G.; Mahieu, N.N.; De Muynck, M.; De Wilde, L.F.; Cools, A.M. Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surg Sport. Traumatol Arthrosc 2013, 21, 1158–1167. [Google Scholar] [CrossRef]


| ALL (50) | PE+PNS+EE (16) | TENS+US+EE (16) | ||||||
|---|---|---|---|---|---|---|---|---|
| CATEGORICAL | Frequency | % | Frequency | % | Frequency | % | p | |
| Sex | Male | 36 | 72.0 | 19 | 76.0 | 17 | 68.0 | 0.529 |
| Female | 14 | 28.0 | 6 | 24.0 | 8 | 32.0 | ||
| Hipo-echogenicity | Yes | 43 | 86.0 | 22 | 88.0 | 21 | 84.0 | 0.684 |
| No | 7 | 14.0 | 3 | 12.0 | 4 | 16.0 | ||
| Thickness | Yes | 47 | 94.0 | 24 | 96.0 | 23 | 92.0 | 0.552 |
| No | 3 | 6.0 | 1 | 4.0 | 2 | 8.0 | ||
| Hypervascularization | Yes | 47 | 94.0 | 23 | 92.0 | 24 | 96.0 | 0.552 |
| No | 3 | 6.0 | 2 | 8.0 | 1 | 4.0 | ||
| Affected side | Right | 34 | 68.0 | 16 | 64.0 | 18 | 72.0 | 0.544 |
| Left | 16 | 32.0 | 9 | 36.0 | 7 | 28.0 | ||
| Dominant hand | Right | 47 | 94.0 | 24 | 96.0 | 23 | 92.0 | 0.552 |
| Left | 3 | 6.0 | 1 | 4.0 | 2 | 8.0 | ||
| CONTINUOUS | Mean | SD | Mean | SD | Mean | SD | p | |
| Age | 44.24 | 11.80 | 44.36 | 13.36 | 44.12 | 10.29 | 0.944 | |
| Weight | 82.08 | 11.44 | 83.88 | 7.50 | 80.28 | 14.28 | 0.270 | |
| Height | 1.74 | 0.07 | 1.74 | 0.07 | 1.74 | 0.07 | 0.752 | |
| BMI | 27.17 | 4.10 | 27.66 | 2.81 | 26.68 | 5.09 | 0.402 | |
| NPRS | 7.24 | 1.36 | 7.56 | 1.26 | 6.92 | 1.41 | 0.097 | |
| DASH | 54.50 | 19.40 | 62.16 | 15.86 | 46.84 | 19.86 | 0.004 | |
| % DASH | 45.42 | 16.16 | 51.80 | 13.22 | 39.03 | 16.55 | 0.004 | |
| SPADI | 69.32 | 18.75 | 71.24 | 17.50 | 67.40 | 20.09 | 0.475 | |
| % SPADI | 53.32 | 14.42 | 54.80 | 13.46 | 51.85 | 15.46 | 0.475 | |
| Abduction strength | 8.45 | 1.42 | 8.56 | 1.74 | 8.34 | 1.03 | 0.590 | |
| Internal rotation strength | 8.55 | 1.42 | 8.70 | 1.68 | 8.41 | 1.12 | 0.480 | |
| External rotation strength | 8.40 | 1.39 | 8.42 | 1.54 | 8.38 | 1.26 | 0.920 | |
| Supraspinatus EMS | 168.31 | 89.32 | 162.73 | 104.37 | 173.88 | 73.01 | 0.663 | |
| Upper trapezius EMS | 391.98 | 165.12 | 400.94 | 173.91 | 383.02 | 158.92 | 0.705 | |
| VARIABLE | Post-treatment | 12 weeks follow-up | 24 weeks follow-up | |||||
|---|---|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | Frequency | % | |||
| Hipo-echogenicity | PE+PNS+EE | Yes | 20 | 80.0 | 16 | 64.0 | 9 | 36.0 |
| No | 5 | 20.0 | 9 | 36.0 | 16 | 64.0 | ||
| TENS+US+EE | Yes | 23 | 92.0 | 22 | 88.0 | 19 | 76.0 | |
| No | 2 | 8.0 | 3 | 12.0 | 6 | 24.0 | ||
| Thickness | PE+PNS+EE | Yes | 19 | 76.0 | 9 | 36.0 | 3 | 12.0 |
| No | 6 | 24.0 | 16 | 64.0 | 22 | 88.0 | ||
| TENS+US+EE | No | 23 | 92.0 | 21 | 84.0 | 16 | 64.0 | |
| No | 2 | 8.0 | 4 | 16.0 | 9 | 36.0 | ||
| Hypervascularization | PE+PNS+EE | Yes | 13 | 52.0 | 8 | 32.0 | 2 | 8.0 |
| No | 12 | 48.0 | 17 | 68.0 | 23 | 92.0 | ||
| TENS+US+EE | Yes | 23 | 92.0 | 20 | 80.0 | 14 | 56.0 | |
| No | 2 | 8.0 | 5 | 20.0 | 11 | 44.0 | ||
| VARIABLE | F | p | η2 | POTENCIA |
|---|---|---|---|---|
| NPRS | 17.684** | 0.000 | 0.536 | 1.000 |
| DASH | 22.962** | 0.000 | 0.600 | 1.000 |
| % DASH | 22.962** | 0.000 | 0.600 | 1.000 |
| SPADI | 21.328** | 0.000 | 0.582 | 1.000 |
| % SPADI | 21.328** | 0.000 | 0.582 | 1.000 |
| Abduction strength | 6.086* | 0.001 | 0.284 | 0.945 |
| Internal rotation strength | 3.754* | 0.017 | 0.197 | 0.777 |
| External rotation strength | 8.340** | 0.000 | 0.352 | 0.988 |
| Supraspinatus EMS | 17.443** | 0.000 | 0.532 | 1.000 |
| Upper trapezius EMS | 5.703* | 0.002 | 0.271 | 0.929 |
| Post-treatment | 12 weeks follow-up | 24 weeks follow-up | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VARIABLE | Within-Group Change Score |
Between-Groups Change Score | Effect Size |
Within-Group Change Score | Between-Groups Change Score | Effect Size | Within-Group Change Score | Between-Groups Change Score | Effect Size | |||||||
| Mean dif. |
p | Mean dif. |
p | d | Mean dif. |
p | Mean dif. |
p | d | Mean dif. |
p | Mean dif. |
p | d | ||
| NPRS | PE+PNS+EE | -5.48 | 0.000** | -2.96 | 0.000** | 1.527 | -6.22 | 0.000** | -2.74 | 0.000** | -1.39 | -6.60 | 0.000** | -3.08 | 0.000** | -1.857 |
| TENS+US+EE | -2.52 | 0.000** | -3.48 | 0.000** | -3.52 | 0.000** | ||||||||||
| DASH | PE+PNS+EE | -48.16 | 0.000** | -33.16 | 0.000** | 2.117 | -55.12 | 0.000** | -36.56 | 0.000** | -2.358 | -57.20 | 0.000** | -37.44 | 0.000** | -2.374 |
| TENS+US+EE | -15.00 | 0.000** | -18.56 | 0.000** | -19.76 | 0.000** | ||||||||||
| % DASH | PE+PNS+EE | -40.13 | 0.000** | -27.63 | 0.000** | 2.116 | -45.93 | 0.000** | -30.47 | 0.000** | -2.357 | -47.67 | 0.000** | -31.20 | 0.000** | -2.348 |
| TENS+US+EE | -12.50 | 0.000** | -15.47 | 0.000** | -16.47 | 0.000** | ||||||||||
| SPADI | PE+PNS+EE | -52.84 | 0.000** | -30.96 | 0.000** | 2.016 | -61.04 | 0.000** | -33.64 | 0.000** | -2.02 | -63.96 | 0.000** | -35.36 | 0.000** | -2.133 |
| TENS+US+EE | -21.88 | 0.000** | -27.40 | 0.000** | -28.60 | 0.000** | ||||||||||
| % SPADI | PE+PNS+EE | 40.65 | 0.000** | -23.82 | 0.000** | 2.016 | -46.95 | 0.000** | -25.88 | 0.000** | -2.02 | -49.20 | 0.000** | -27.20 | 0.000** | -2.132 |
| TENS+US+EE | 16.83 | 0.000** | -21.08 | 0.000** | -22.00 | 0.000** | ||||||||||
| Abduction strength | PE+PNS+EE | 1.42 | 0.000** | 0.74 | 0.000** | 1.132 | 1.81 | 0.000** | 0.83 | 0.000** | 1.169 | 2.18 | 0.000** | 1.10 | 0.000** | 1.178 |
| TENS+US+EE | 0.68 | 0.000** | 0.98 | 0.000** | 1.09 | 0.000** | ||||||||||
| Internal rotation strength | PE+PNS+EE | 1.10 | 0.000** | 0.32 | 0.030* | 0.637 | 1.60 | 0.000** | 0.56 | 0.002** | 0.911 | 1.82 | 0.000** | 0.66 | 0.004** | 0.868 |
| TENS+US+EE | 0.78 | 0.000** | 1.04 | 0.000** | 1.16 | 0.000** | ||||||||||
| External rotation strength | PE+PNS+EE | 1.40 | 0.000** | 0.58 | 0.000** | 1.065 | 1.87 | 0.000** | 0.81 | 0.000** | 1.193 | 2.22 | 0.000** | 1.02 | 0.000** | 1.408 |
| TENS+US+EE | 0.82 | 0.000** | 1.06 | 0.000** | 1.20 | 0.000** | ||||||||||
| Supraspinatus EMS | PE+PNS+EE | 85.36 | 0.000** | 67.82 | 0.000** | 1.890 | 127.57 | 0.000** | 96.16 | 0.000** | 1.958 | 155.67 | 0.000** | 122.21 | 0.000** | 1.881 |
| TENS+US+EE | 17.54 | 0.000** | 31.40 | 0.000** | 33.46 | 0.000** | ||||||||||
| Upper trapezius EMS |
PE+PNS+EE | -136.96 | 0.000** | -71.05 | 0.016* | 0.710 | -167.15 | 0.000** | -95.92 | 0.003** | -0.883 | 155.67 | 0.000** | -78.50 | 0.015* | -1.719 |
| TENS+US+EE | -65.91 | 0.000** | -71.23 | 0.000** | -88.81 | 0.000** | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





