Submitted:
08 March 2024
Posted:
11 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Mathematical Models
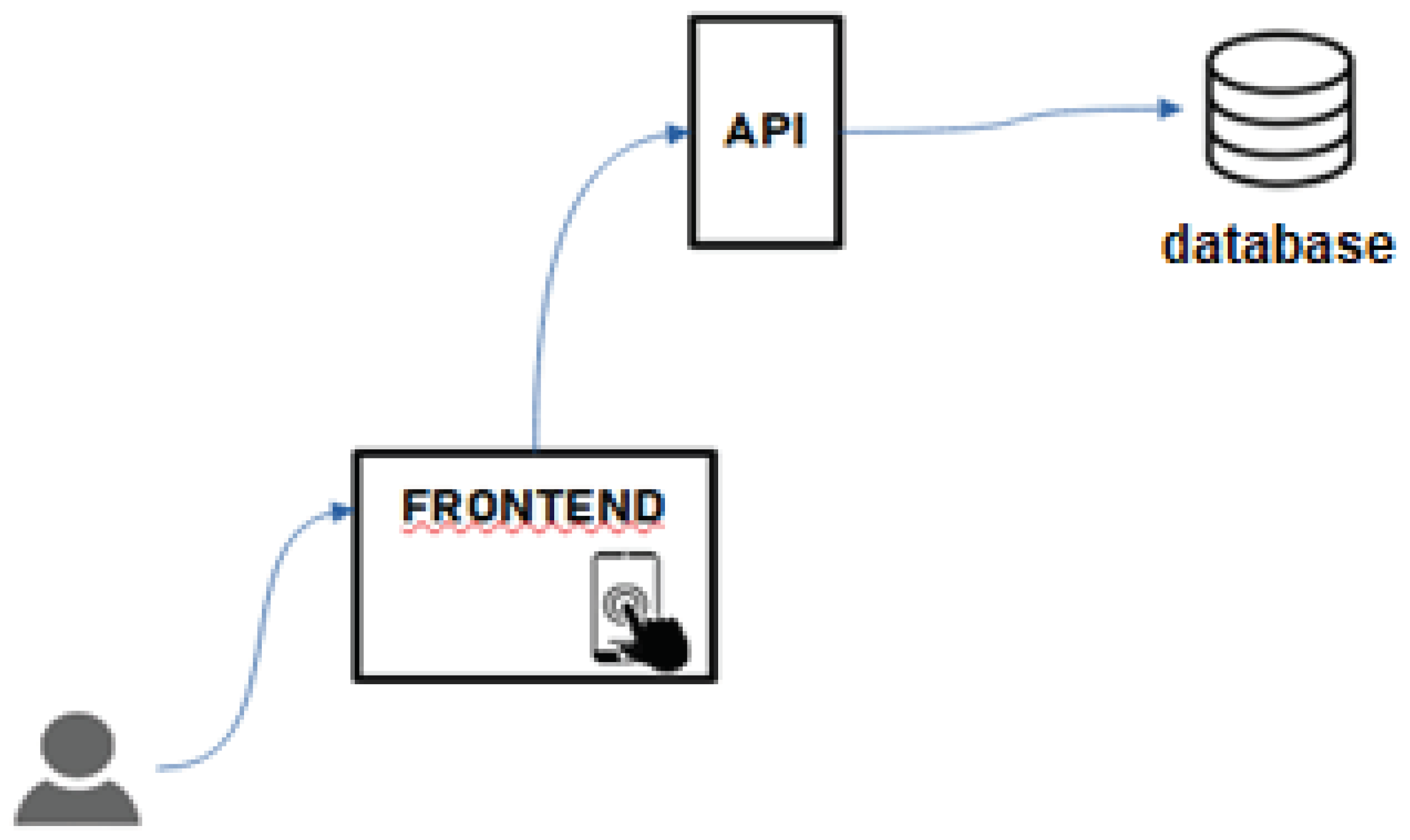
2.2. Application Development
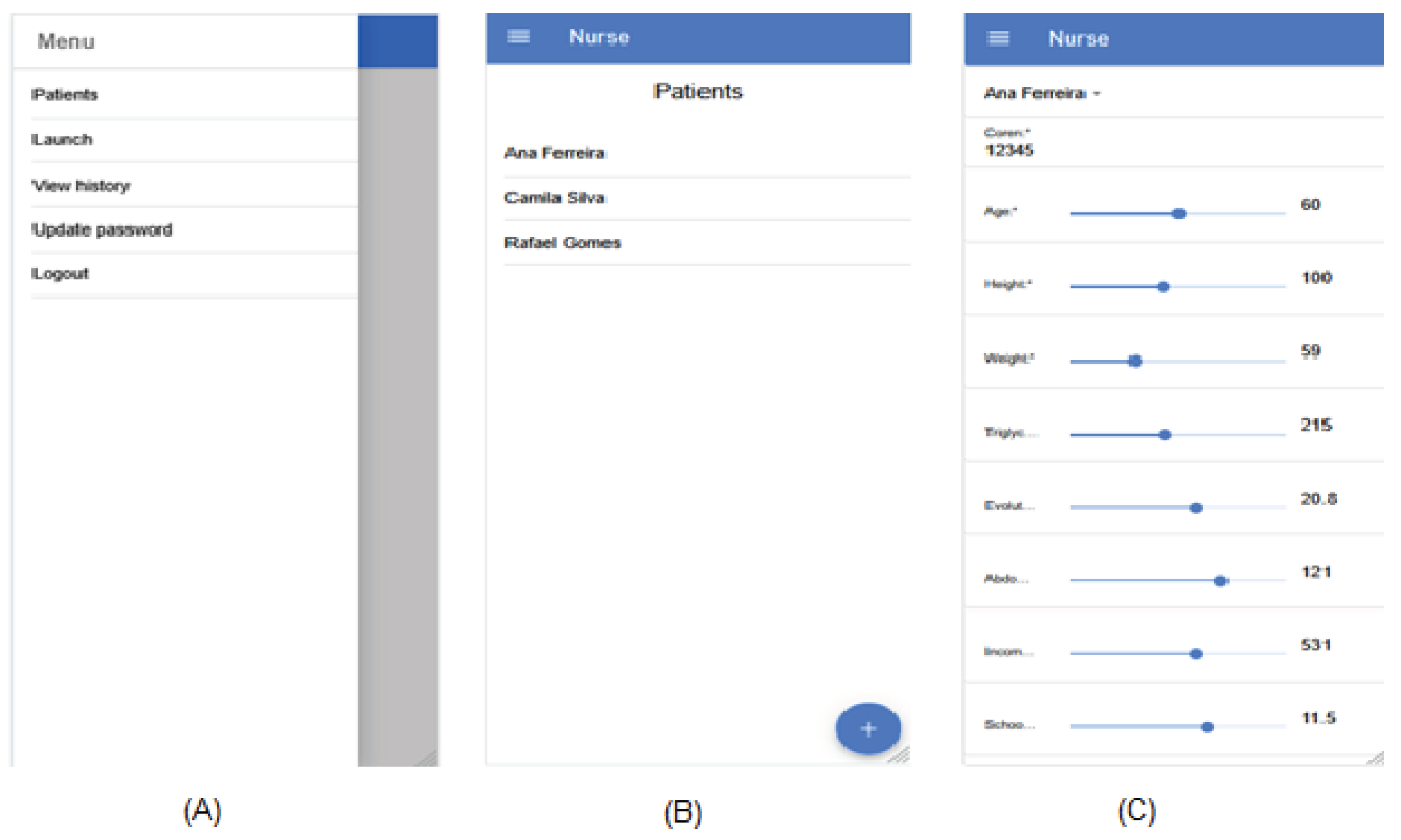
- Patients: allows nurses to view patients registered in the system, edit or delete data for a specific patient and add new patients (Figure 6B);
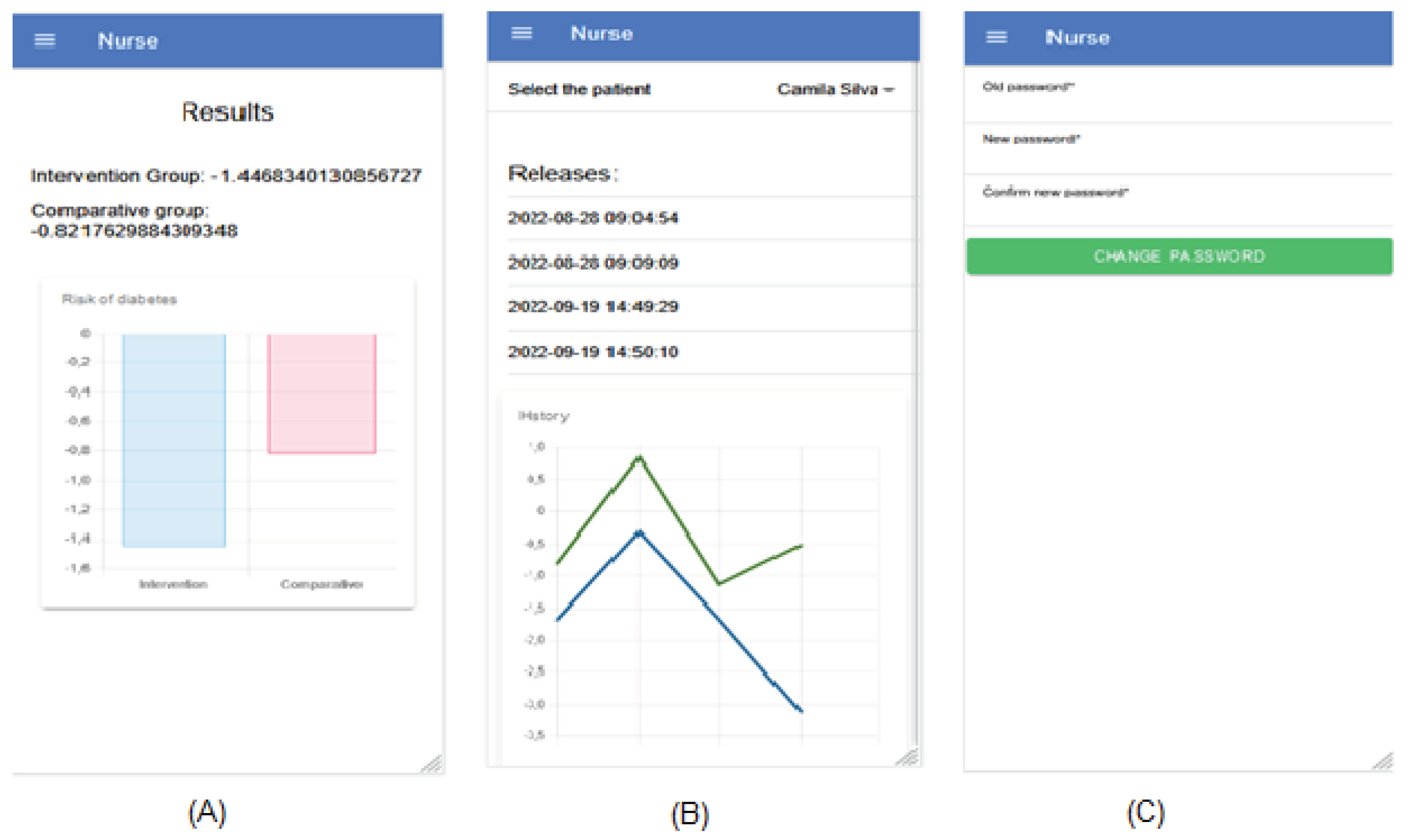
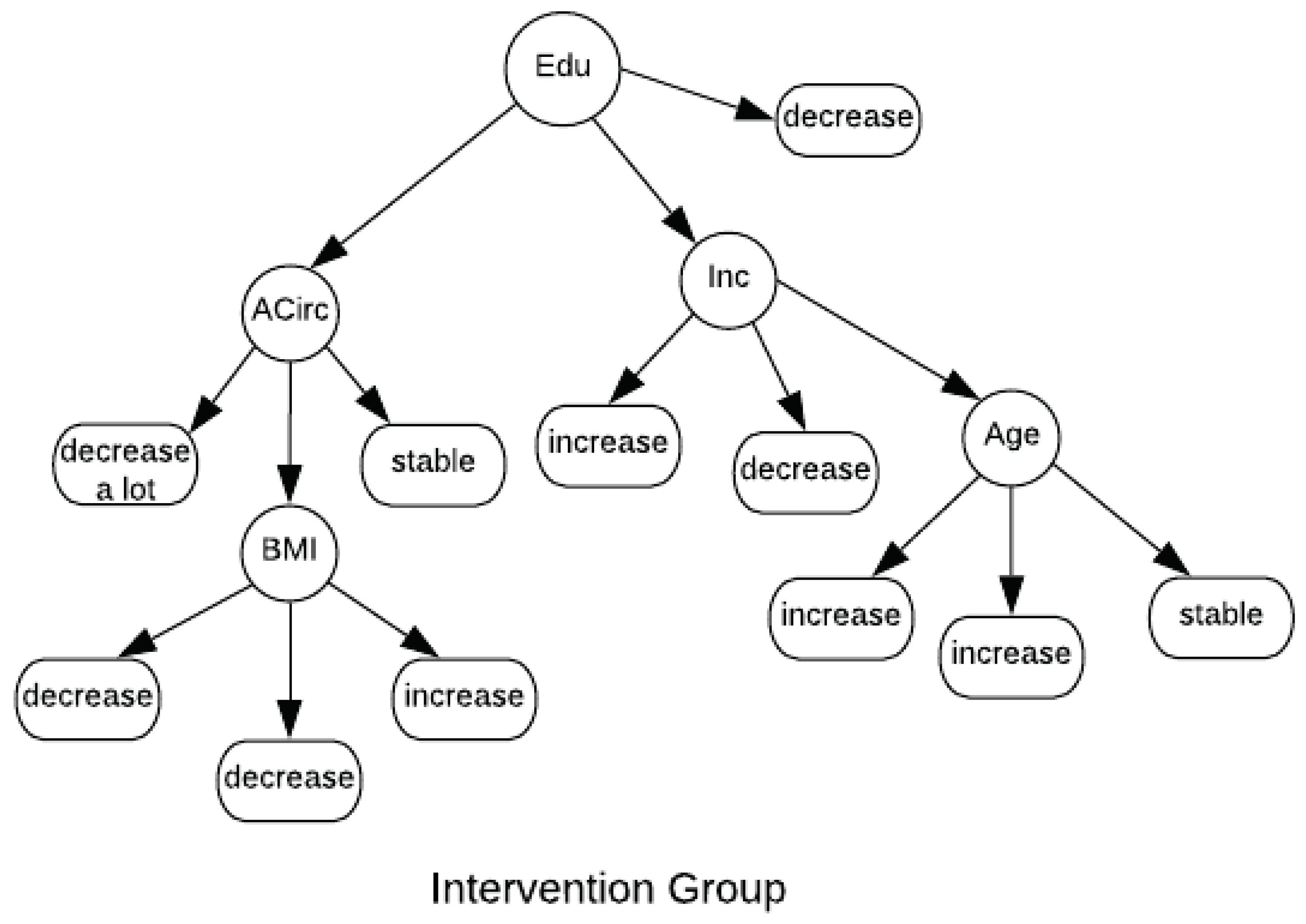
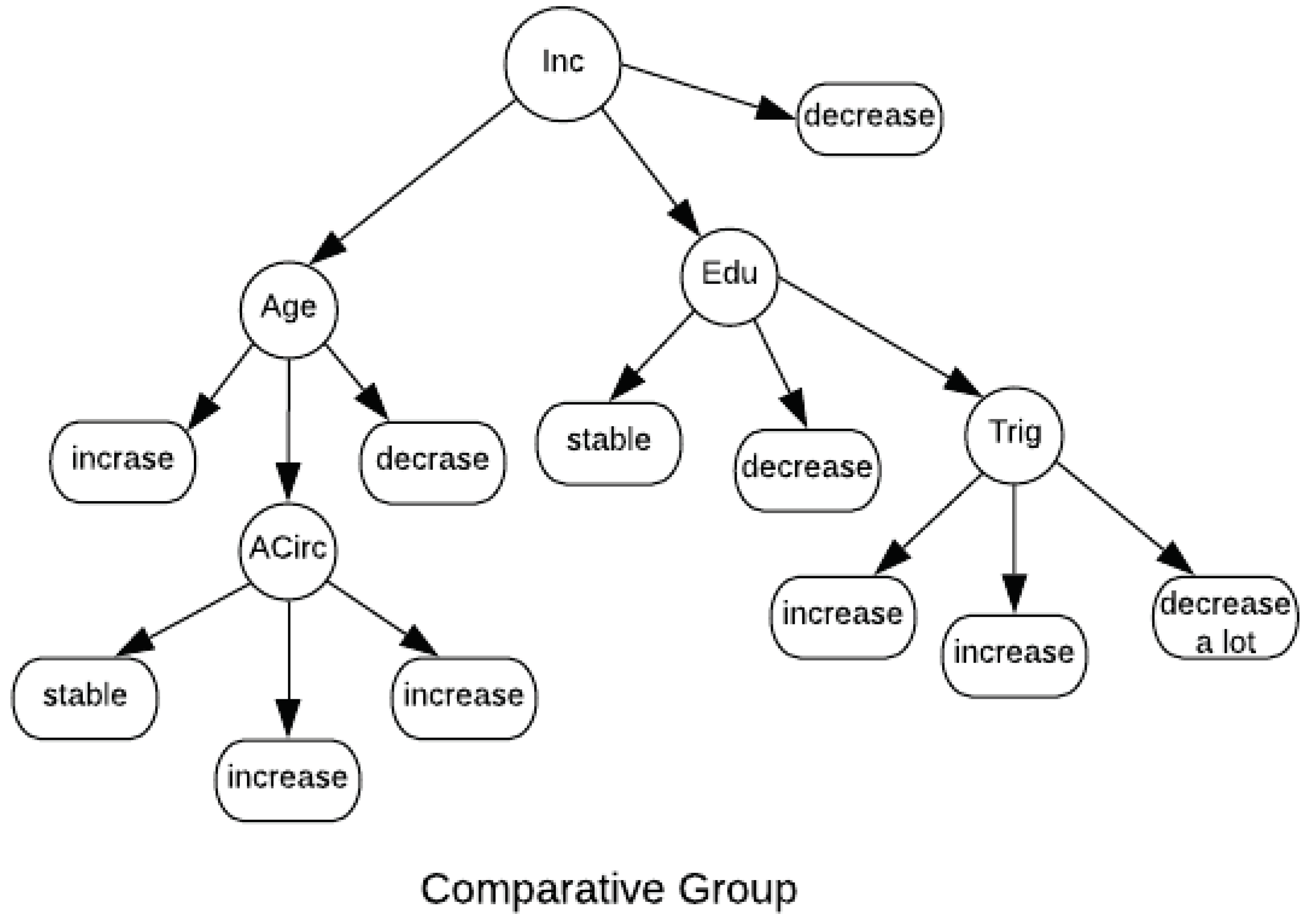
- Launch: when selecting a patient, new entries can be made (Figure 6C). To do this, data from the last entry performed for that patient is shown, providing the nurse with a view of whether the current values are higher or lower than the last time they were entered. At the end of the launch, the results obtained for the two groups are shown numerically and graphically (Figure 7A);
- View history: when selecting a patient, all entries made for him and their respective dates and times are listed (Figure 7B). Also, a line graph is presented, where each point refers to the result found in a launch, with two lines, with the blue line indicating the Intervention group and the green line the Comparative group. This enables future analyzes of the variation in results obtained that can lead to good or bad consequences for the patient’s condition;
- Update password: allows the user to change their access password whenever necessary (Figure 7C). If the user forgets their password and uses the option in Figure 5B to recover it, they will receive an email with a randomly generated password with which they can log in. Thus, with the option to update password, he can change it to a password he deems more appropriate, maintaining the security of his account.
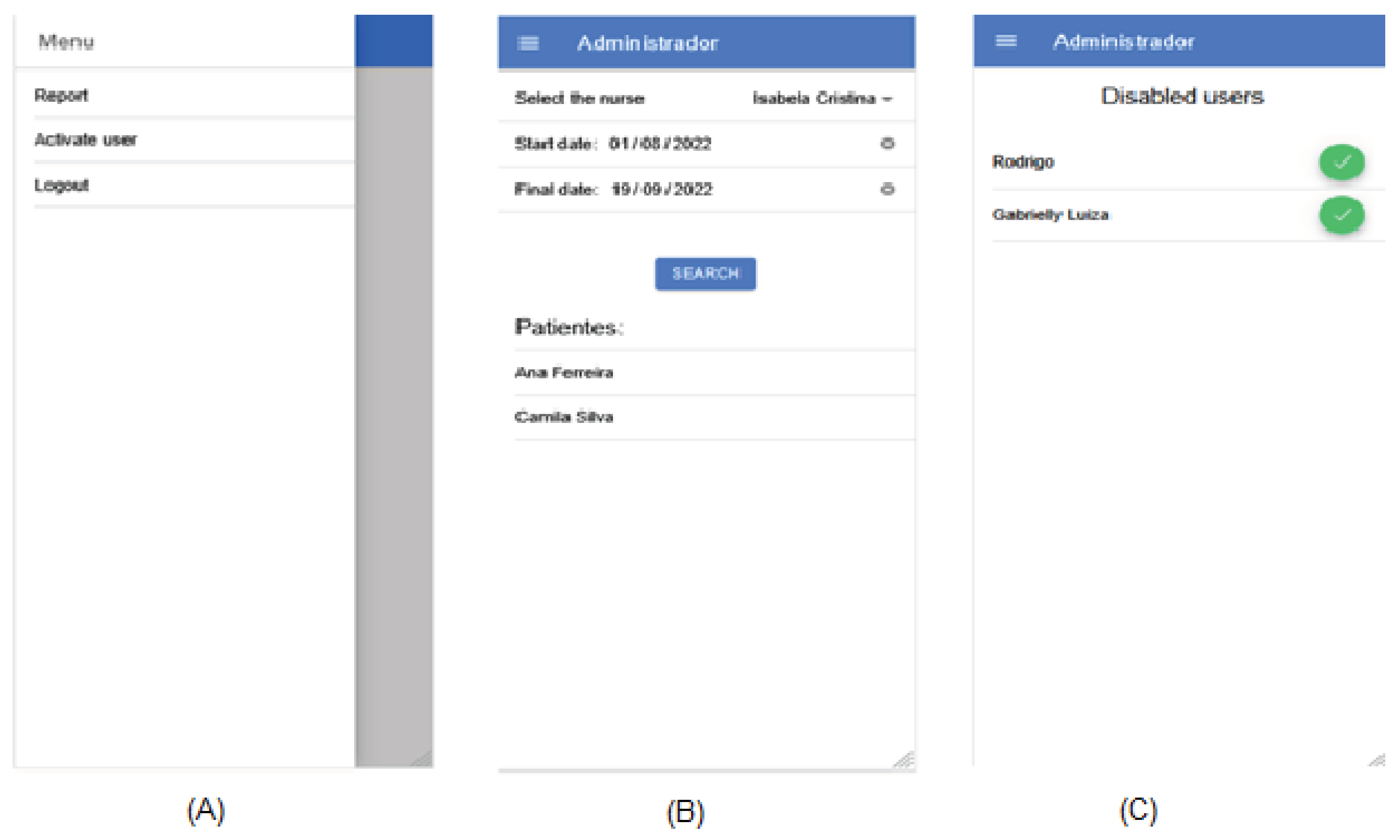
- Report: allows the administrator to view a report on which patients were seen by a specific nurse in a specified date range (Figure 8B). To do this, he selects the name of the nurse who wants to perform the search and the date range. The list of patients will then be shown. This report is useful in several analyses, such as knowing who served the most patients;
- Activate users: allows the administrator to authorize new users to access the application (Figure 8C). To do this, a list of users who have recently registered and are awaiting approval is shown. Whenever a user registers on the application, their access is not granted. It is the administrator’s role to do this, being able to control who has access to patient data and providing greater security.
3. Results and Discussion
3.1. Discussion
3.2. Self-Assessment on User Experience and Usability
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Whiting, D.R.; Guariguata, L.; Weil, C.; Shaw, J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011, 94, 311–321. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization - WHO. Diabetes. [Internet]. 2023. Available in: https://www.who.int/news-room/fact-sheets/detail/diabetes.
- American Diabetes Association - ADA. Standards of medical care in diabetes—2015 abridged for primary care providers. Clin Diabetes 2015, 33, 97. [Google Scholar] [CrossRef] [PubMed]
- Ogurtsova, K.; da Rocha Fernandes, J.D.; Huang, Y.; Linnenkamp, U.; Guariguata, L.; Cho, N.H.; et al. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017, 128, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Vêscovi, S.D.J.B.; Primo, C.C.; Sant’Anna, H.C.; Bringuete, M.E.D.O.; Rohr, R.V.; Prado, T.N.D.; et al. Aplicativo móvel para avaliação dos pés de pessoas com diabetes mellitus. Acta Paul Enferm. 2017, 30, 607–613. [Google Scholar] [CrossRef]
- Marcelo, C.A.S.; Coutinho, M.A.P.; Lara, C.R.; Paraizo, C.M.S.; Fava, S.M.C. Aplicativos móveis sobre diabetes mellitus - Revisão Narrativa. J Health Inform. 2020, 12. [Google Scholar]
- McLellan, K.C.P.; Barbalho, S.M.; Cattalini, M.; Lerario, A.C. Diabetes mellitus do tipo 2, síndrome metabólica e modificação no estilo de vida. Rev Nutr. 2007, 20, 515–524. [Google Scholar] [CrossRef]
- Bressan, G.M.; de Azevedo, B.C.F.; Souza, R.M. A Fuzzy Approach for Diabetes Mellitus Type 2 Classification. Braz Arch Biol Technol. 2020, 63, 1–11. [Google Scholar] [CrossRef]
- Castanho, R.M.. Efeito do uso do método de gerenciamento de caso sobre o controle glicêmico de pessoas com diabetes mellitus tipo 2. [Dissertação de Doutorado]. Curitiba PR: Universidade Federal do Paraná; 2013.
- Zadeh, L.A. . Conjuntos difusos. Inf Ao Controle. 1965, 8, 338–353. [Google Scholar] [CrossRef]
- Cingolani, P.; Alcala-Fdez, J. jFuzzyLogic: a robust and flexible Fuzzy-Logic inference system language implementation. In: 2012 IEEE International Conference on Fuzzy Systems. IEEE; 2012. p. 1-8.
- Marcelo, C.A.S.; Pereira Coutinho, M.A.; Lara, C.R.; Silva Paraizo, C.M.; Coelho Leite Fava, S.M. Aplicativos Móveis sobre Diabetes Mellitus - Revisão Narrativa. J Health Inform. Disponível em: https://jhi.sbis.org.br/index.php/jhi-sbis/article/view/726.. 2020, 12. [Google Scholar]
- Sousa, A.; Malveira, N.. Designing Usability and UX with UXUG-AP: Na Observational Study and an Interview with Experts. In: XVII Brazilian Symposium on Information Systems, SBSI. New York, USA: Association for Computing Machinery; 2021.
- Gomes, M.L.F.; Linhares, M.I.F.; Ferreira, C.F.; Fernandes, C.I.; Silva, M.S.; Sousa, M.A.; et al. Aplicativos móveis direcionados aos idosos para autogerenciamento do cuidado: revisão de escopo. Rev Cuidarte. 2023, 14, e2594. [Google Scholar]
- Smith-Turchyn, J.; Gravesande, J.; Agarwal, G.; Mangin, D.; Javadi, D.; Peter, J.; et al. A Healthy Lifestyle App for Older Adults with Diabetes and Hypertension: Usability Assessment. Int J Healthc Technol Manag. 2017, 16, 250–270. [Google Scholar] [CrossRef]
- Zheng, Y.; Weinger, K.; Greenberg, J.; Burke, L.E.; Sereika, S.M.; Patience, N.; et al. Actual Use of Multiple Health Monitors Among Older Adults With Diabetes: Pilot Study. JMIR Aging 2020, 3, e15995. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, S.; Waki, K.; Nannya, Y.; Nangaku, M.; Kadowaki, T.; Ohe, K. Usage Patterns of GlucoNote, a Self-Management Smartphone App, Based on ResearchKit for Patients With Type 2 Diabetes and Prediabetes. JMIR Mhealth Uhealth. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Torbjørnsen, A.; Ribu, L.; Rønnevig, M.; Grøttl, A.; Helseth, S. Users’ Acceptability of a Mobile Application for Persons with Type 2 Diabetes: A Qualitative Study. BMC Health Serv Res. 2019, 19, 641. [Google Scholar] [CrossRef] [PubMed]
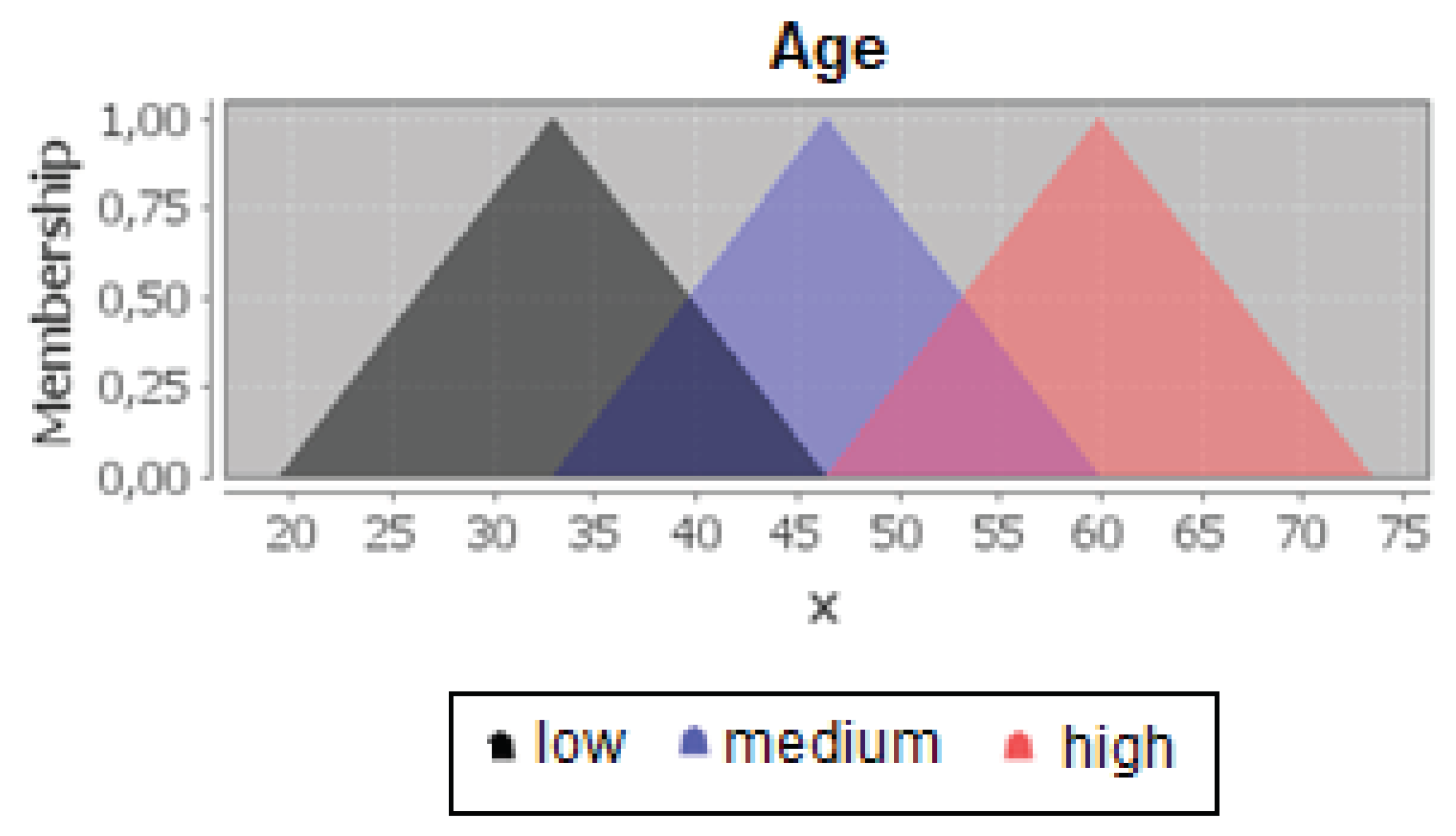

| Attribute | Low value | Medium value | High value |
|---|---|---|---|
| Age | [19,5; 33; 46,5] | [33; 46,5; 60] | [46,5; 60; 73,5] |
| Triglycerides | [-174; 47; 268,5] | [47; 268,5; 490] | [268,5; 490; 711] |
| Evolutionary Time | [-15,2; 0,20; 15,6] | [0,2; 15,6; 31] | [15,6; 31; 46,4] |
| Body Mass Index (BMI) | [3,7; 16,06; 28,4] | [16,1; 28,41; 40,8] | [28,1; 40,8; 53,1] |
| Abdominal Circumference | [45; 72; 99] | [72; 99; 126] | [99; 126; 153] |
| Income | [-400; 4.48e-05; 400] | [6,1e-05; 400; 800] | [400 ;800; 1.200] |
| Education | [-7,5; -1e-03; 7,5] | [1,1e-03; 7,5; 15] | [7,5; 15; 22,5] |
| Attribute | Low value | Medium value | High value |
|---|---|---|---|
| Age | [3; 22; 41] | [22; 41; 59,9] | [41; 60; 79] |
| Triglycerides | [-135; 45; 225] | [45; 225; 405] | [225; 405; 585] |
| Evolutionary Time | [-11.63; 0,25; 12,1] | [0,27; 12,1; 24] | [12,1; 24; 35,9] |
| Body Mass Index (BMI) | [2,2; 21,7; 41,2] | [21,7; 41,2; 60,7] | [41,2; 60,7; 80,2] |
| Abdominal Circumference | [52,8; 81; 109,2] | [81; 109,2; 137,5] | [500; 1.000; 1.500] |
| Income | [-500; -9,2e-05; 500] | [8,4e-05; 500; 1.000] | [400 ;800; 1.200] |
| Education | [-7,5; -2,6e-05; 7,5] | [6,4e-03; 7,5; 14,9] | [7,5; 15; 22,5] |
| Work | Target audience | Main goal of the application | Does it interact with healthcare professionals? |
|---|---|---|---|
| Jenna et al. (2017) | Elderly | Promote self-care and disease management | Not specified |
| Zheng et al. (2020) | Elderly | Promote self-care and disease management | Not specified |
| Yamaguchi et al. (2019) | Not specified | Promote self-care and disease management | Not specified |
| Torbjørnsen (2019) | Not specified | Promote self-care and disease management | Yes |
| DiabetesCheck | General population | Perform monitoring and prediction of diabetes risk | Yes |
| Category | Guidelines | Self-assessment |
|---|---|---|
| Requirements | Was there an exchange of information between the team and the client through interviews and/or workshops to identify key prototype requirements? | Yes. The development team, in addition to the knowledge obtained, had access to meetings with the authors of the work to identify the requirements of the application. |
| Understanding user needs | Does the prototype interface have language accessible to different user profiles: children, youth, academics, professionals, etc.? | Yes. During development, there was a concern to use vocabulary relevant to healthcare professionals impacted by the system, namely doctors and nurses. |
| Accessibility | Does the prototype allow customization of the interface to suit users with visual impairments (increased color contrast, font size)? | No. However, it is an important demand and will be incorporated into the list of requirements to be implemented in the future. |
| Ease of use | Are there standardization of elements in the prototype interface, such as buttons, icons, etc., in relation to their location? | Yes. The organization of the elements of the application interface was designed to minimize the user’s cognitive effort to find what they need. |
| Informative feedback | Are there informative feedback for the user, such as alert and error messages, loading and progress indicators, among others? | Yes. Any activity that requires extended time (such as data retrieval from the backend) is highlighted to the user through informative feedback. |
| Are the feedback informative enough for the user to understand what is happening and why? | Yes. Error and alert messages were created to use the vocabulary of the end user. | |
| Information | Are the information modularized and independent, so that the user does not need to remember other screens while performing an activity? | Yes. All the information necessary for the user to perform an activity in the application is available on the current screen. |
| Error prevention | Does the prototype protect the user from errors they might make (e.g., forgetting a required field, entering more or fewer characters than required)? | Yes. Mandatory fields are properly highlighted in the application interface. We sought to use appropriate components for each type of field. For values on a scale of 0 to 5, a selector component was used instead of requiring the user to enter the value. |
| Does the prototype use icons that suggest the action taken and hints that explain the icon and the action? | No. This is an improvement that the application interface needs to enhance user experience and usability. |
|
| Sequence of actions | Are the prototype actions reversible? | No. The current version of the application does not have the option to undo actions. However, in the case of destructive actions, the application requests user confirmation before proceeding with the action. |
| Are the action sequences organized into groups with a beginning, middle, and end? | Yes. | |
| Sense of belonging | Do the colors, icons, and styles represent the user in a way that allows the user to feel that the software was made with them in mind? | Yes. The choice of colors, icons, and other visual elements was made considering the context of the healthcare field. |
| Degree of importance | Are elements of higher importance highlighted in the prototype interface? | Yes. An example is the page titles, which are prominently positioned on the application screen (centered and with larger font size). |
| Privacy | Is it possible to control who can access certain information and when? | Yes. The application implements user authentication through profiles, so that each type of user has access to certain functions. |
| Is there an option for password recovery in the prototype, ensuring user control? | No. This functionality will be implemented in a future version of the application. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





