Submitted:
13 March 2024
Posted:
14 March 2024
You are already at the latest version
Abstract
Keywords:
Introduction
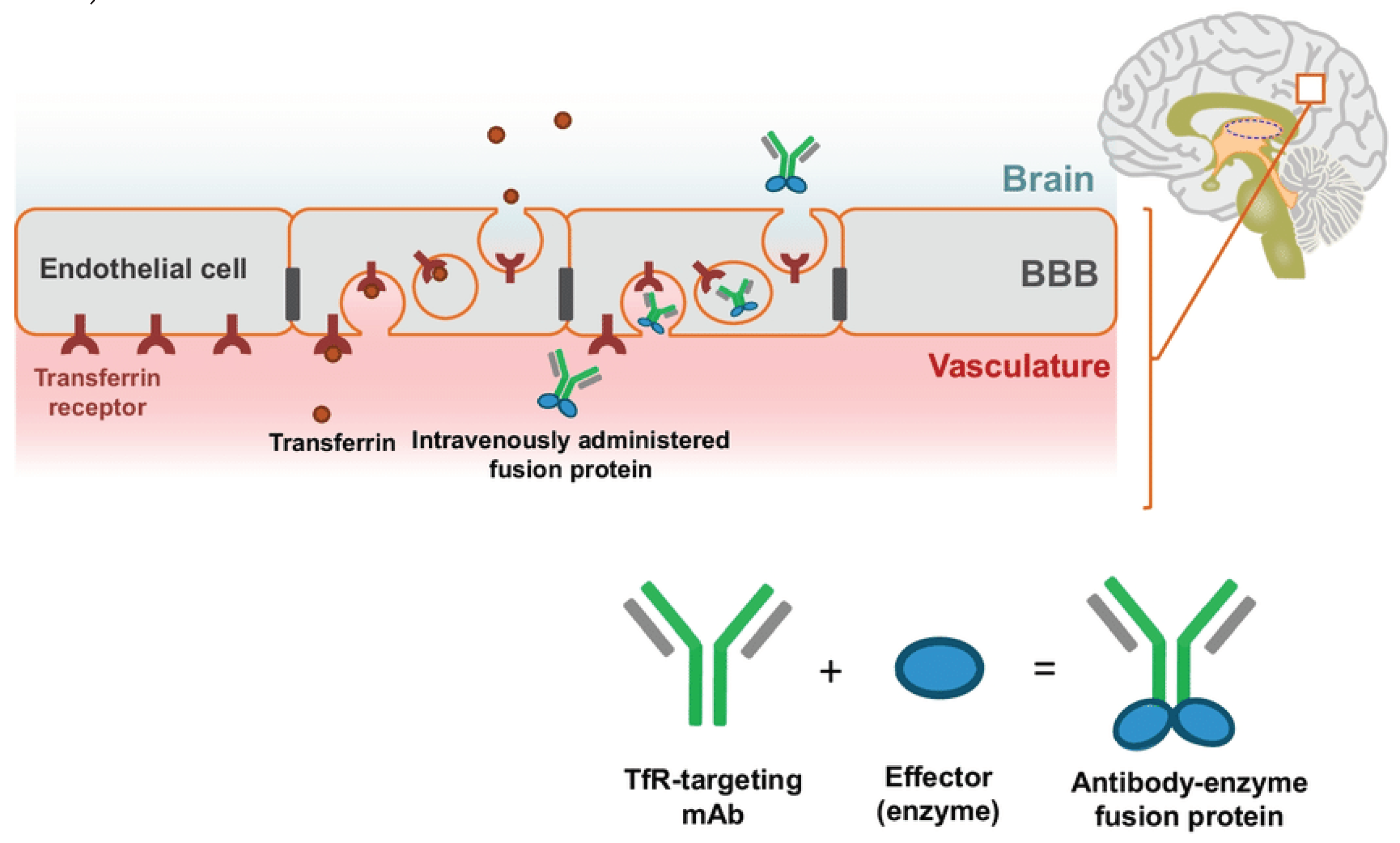
Transcytosis
mRNA-Based Transcytosis
Regulatory
Conclusions
Funding
Conflicts of Interest
Roles
References
- Goedert M. NEURODEGENERATION. Alzheimer's and Parkinson's diseases: The prion concept in relation to assembled Aβ, tau, and α-synuclein. Science. 2015;349(6248):1255555. [CrossRef]
- Bertram, L.; Tanzi, R.E. The genetic epidemiology of neurodegenerative disease. J. Clin. Investig. 2005, 115, 1449–1457. [CrossRef]
- Walsh DM, Selkoe DJ. A critical appraisal of the pathogenic protein spread hypothesis of neurodegeneration. Nat Rev Neurosci. 2016;17(4):251-60. [CrossRef]
- Makin, S. The amyloid hypothesis on trial. Nature 2018, 559, S4–S7. [CrossRef]
- Ross CA, Tabrizi SJ. Huntington's disease: from molecular pathogenesis to clinical treatment. Lancet Neurol. 2011;10(1):83-98. [CrossRef]
- Orr, H.T.; Zoghbi, H.Y. SCA1 molecular genetics: a history of a 13 year collaboration against glutamines. Hum. Mol. Genet. 2001, 10, 2307–2311. [CrossRef]
- Selkoe DJ, Hardy J. The amyloid hypothesis of Alzheimer's disease at 25 years. EMBO Mol Med. 2016;8(6):595-608. [CrossRef]
- Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, et al. Parkinson disease. Nat Rev Dis Primers. 2017;3:17013. [CrossRef]
- Foerster, B.R.; Welsh, R.C.; Feldman, E.L. 25 years of neuroimaging in amyotrophic lateral sclerosis. Nat. Rev. Neurol. 2013, 9, 513–524. [CrossRef]
- Iadanza, M.G.; Jackson, M.P.; Hewitt, E.W.; Ranson, N.A.; Radford, S.E. A new era for understanding amyloid structures and disease. Nat. Rev. Mol. Cell Biol. 2018, 19, 755–773. [CrossRef]
- Mathieu, C.; Pappu, R.V.; Taylor, J.P. Beyond aggregation: Pathological phase transitions in neurodegenerative disease. Science 2020, 370, 56–60. [CrossRef]
- Petkova AT, Leapman RD, Guo Z, Yau WM, Mattson MP, Tycko R. Self-propagating, molecular-level polymorphism in Alzheimer's beta-amyloid fibrils. Science. 2005;307(5707):262-5. [CrossRef]
- Fitzpatrick, A.W.P.; Falcon, B.; He, S.; Murzin, A.G.; Murshudov, G.; Garringer, H.J.; Crowther, R.A.; Ghetti, B.; Goedert, M.; Scheres, S.H.W. Cryo-EM structures of tau filaments from Alzheimer’s disease. Nature 2017, 547, 185–190. [CrossRef]
- Kwon, D. Rogue antibodies involved in almost one-fifth of COVID deaths. Nature 2021, 597, 162–162. [CrossRef]
- Zakariya, S.M.; Zehra, A.; Khan, R.H. Biophysical Insight into Protein Folding, Aggregate Formation and its Inhibition Strategies. Protein Pept. Lett. 2022, 29, 22–36. [CrossRef]
- Cummings, J.; Osse, A.M.L.; Cammann, D.; Powell, J.; Chen, J. Anti-Amyloid Monoclonal Antibodies for the Treatment of Alzheimer’s Disease. BioDrugs 2023, 38, 5–22. [CrossRef]
- Cummings J. Anti-Amyloid Monoclonal Antibodies are Transformative Treatments that Redefine Alzheimer's Disease Therapeutics. Drugs. 2023;83(7):569-76. [CrossRef]
- Association As. Aducanumab to Be Discontinued as an Alzheimer’s Treatment https://www.alz.org/alzheimers-dementia/treatments/aducanumab2024 [.
- Mintun, M.A.; Lo, A.C.; Evans, C.D.; Wessels, A.M.; Ardayfio, P.A.; Andersen, S.W.; Shcherbinin, S.; Sparks, J.; Sims, J.R.; Brys, M.; et al. Donanemab in Early Alzheimer’s Disease. New Engl. J. Med. 2021, 384, 1691–1704. [CrossRef]
- Post W. FDA delays Alzheimer’s drug for further review in surprise move https://www.washingtonpost.com/business/2024/03/08/eli-lilly-alzheimers-donanemab-fda/2024 [.
- Times N. A.L.S. Drug Relyvrio Fails Clinical Trial and May Be Withdrawn From the Market https://www.nytimes.com/2024/03/08/health/als-drug-relyvrio.html2024 [.
- Today PsN. Biogen Discontinues Development of Cinpanemab https://parkinsonsnewstoday.com/news/biogen-announcement-discontinue-cinpanemab-parkinsons/2024 [.
- Clinicaltrials.gov. Alzheimer’s Disease Antibody Response https://clinicaltrials.gov/search?cond=Neurological%20Disorder&aggFilters=studyType:int&term=Antibody%20Response&intr=antibody2024 [.
- Pardridge, W.M. Drug Targeting to the Brain. Pharm. Res. 2007, 24, 1733–1744. [CrossRef]
- Fortin, D.; Gendron, C.; Boudrias, M.; Garant, M. Enhanced chemotherapy delivery by intraarterial infusion and blood-brain barrier disruption in the treatment of cerebral metastasis. Cancer 2007, 109, 751–760. [CrossRef]
- Hynynen, K.; McDannold, N.; Vykhodtseva, N.; Jolesz, F.A. Noninvasive MR Imaging–guided Focal Opening of the Blood-Brain Barrier in Rabbits. Radiology 2001, 220, 640–646. [CrossRef]
- Burgess, A.; Hynynen, K. Noninvasive and Targeted Drug Delivery to the Brain Using Focused Ultrasound. ACS Chem. Neurosci. 2013, 4, 519–526. [CrossRef]
- Bradley, M.; Swindell, C.; Anthony, F.; Witman, P.; Devanesan, P.; Webb, N.; Baker, S.; Wolff, A.; Donehower, R. Tumor targeting by conjugation of DHA to paclitaxel. J. Control. Release 2001, 74, 233–236. [CrossRef]
- Moghimi, S.; Szebeni, J. Stealth liposomes and long circulating nanoparticles: critical issues in pharmacokinetics, opsonization and protein-binding properties. Prog. Lipid Res. 2003, 42, 463–478. [CrossRef]
- Dhuria, S.V.; Hanson, L.R.; Frey, W.H., 2nd. Intranasal delivery to the central nervous system: Mechanisms and experimental considerations. J. Pharm. Sci. 2010, 99, 1654–1673. [CrossRef]
- Jones, A.R.; Shusta, E.V. Blood–Brain Barrier Transport of Therapeutics via Receptor-Mediation. Pharm. Res. 2007, 24, 1759–1771. [CrossRef]
- Gao, Y.; Zhu, J.; Lu, H. Single domain antibody-based vectors in the delivery of biologics across the blood–brain barrier: a review. Drug Deliv. Transl. Res. 2020, 11, 1818–1828. [CrossRef]
- Bien-Ly, N.; Yu, Y.J.; Bumbaca, D.; Elstrott, J.; Boswell, C.A.; Zhang, Y.; Luk, W.; Lu, Y.; Dennis, M.S.; Weimer, R.M.; et al. Transferrin receptor (TfR) trafficking determines brain uptake of TfR antibody affinity variants. J. Exp. Med. 2014, 211, 233–244. [CrossRef]
- Pardridge, W.M. Drug Transport across the Blood–Brain Barrier. J. Cereb. Blood Flow Metab. 2012, 32, 1959–1972. [CrossRef]
- Zhang, Y.; Pardridge, W.M. Blood–brain barrier targeting of BDNF improves motor function in rats with middle cerebral artery occlusion. Brain Res. 2006, 1111, 227–229. [CrossRef]
- Boado RJ, Zhang Y, Zhang Y, Pardridge WM. Humanization of anti-human insulin receptor antibody for drug targeting across the human blood-brain barrier. Biotechnol Bioeng. 2007;96(2):381-91.
- Deane R, Bell RD, Sagare A, Zlokovic BV. Clearance of amyloid-beta peptide across the blood-brain barrier: implication for therapies in Alzheimer's disease. CNS Neurol Disord Drug Targets. 2009;8(1):16-30.
- Deane R, Wu Z, Sagare A, Davis J, Du Yan S, Hamm K, et al. LRP/amyloid beta-peptide interaction mediates differential brain efflux of Abeta isoforms. Neuron. 2004;43(3):333-44.
- Zlokovic, B.V. The Blood-Brain Barrier in Health and Chronic Neurodegenerative Disorders. Neuron 2008, 57, 178–201. [CrossRef]
- Pardridge WM. The blood-brain barrier: bottleneck in brain drug development. NeuroRx. 2005;2(1):3-14.
- Wilchek, M.; Bayer, E.A. The avidin-biotin complex in bioanalytical applications. Anal. Biochem. 1988, 171, 1–32. [CrossRef]
- Veronese, F.M.; Pasut, G. PEGylation, successful approach to drug delivery. Drug Discov. Today 2005, 10, 1451–1458. [CrossRef]
- Argos, P. An investigation of oligopeptides linking domains in protein tertiary structures and possible candidates for general gene fusion. J. Mol. Biol. 1990, 211, 943–958. [CrossRef]
- Carter, P.; Wells, J.A. Dissecting the catalytic triad of a serine protease. Nature 1988, 332, 564–568. [CrossRef]
- Urry, D.W. Physical Chemistry of Biological Free Energy Transduction As Demonstrated by Elastic Protein-Based Polymers. J. Phys. Chem. B 1997, 101, 11007–11028. [CrossRef]
- Arai, R.; Ueda, H.; Kitayama, A.; Kamiya, N.; Nagamune, T. Design of the linkers which effectively separate domains of a bifunctional fusion protein. Protein Eng. Des. Sel. 2001, 14, 529–532. [CrossRef]
- Huang, X.; Kong, N.; Zhang, X.; Cao, Y.; Langer, R.; Tao, W. The landscape of mRNA nanomedicine. Nat. Med. 2022, 28, 2273–2287. [CrossRef]
- Blakney, A.K.; Ip, S.; Geall, A.J. An Update on Self-Amplifying mRNA Vaccine Development. Vaccines 2021, 9, 97. [CrossRef]
- Niazi, S.K. The FDA’s New Guideline “Generally Accepted Scientific Knowledge” (GASK): An Opportunity to Expedite the Approval of Biosimilars. Pharmaceuticals 2023, 16, 1517. [CrossRef]
- Ban, W.; You, Y.; Yang, Z. Imaging Technologies for Cerebral Pharmacokinetic Studies: Progress and Perspectives. Biomedicines 2022, 10, 2447. [CrossRef]
- Marathe, P.H.; Shyu, W.C.; Humphreys, W.G. The Use of Radiolabeled Compounds for ADME Studies in Discovery and Exploratory Development. Curr. Pharm. Des. 2004, 10, 2991–3008. [CrossRef]
- Zuber C, Mitteregger G, Schuhmann N, Rey C, Knackmuss S, Rupprecht W, et al. Delivery of single-chain antibodies (scFvs) directed against the 37/67 kDa laminin receptor into mice via recombinant adeno-associated viral vectors for prion disease gene therapy. J Gen Virol. 2008;89(Pt 8):2055-61.
- Waraho-Zhmayev, D.; Meksiriporn, B.; Portnoff, A.D.; DeLisa, M.P. Optimizing recombinant antibodies for intracellular function using hitchhiker-mediated survival selection.. Protein Eng. Des. Sel. 2014, 27, 351–8. [CrossRef]
- Niazi, S.K. Non-Invasive Drug Delivery across the Blood–Brain Barrier: A Prospective Analysis. Pharmaceutics 2023, 15, 2599. [CrossRef]
- Berg, P.; Baltimore, D.; Boyer, H.W.; Cohen, S.N.; Davis, R.W.; Hogness, D.S.; Nathans, D.; Roblin, R.; Watson, J.D.; Weissman, S.; et al. Letter: Potential biohazards of recombinant DNA molecules.. 1974, 185, 303.
- Niazi, S.K. Anti-Idiotypic mRNA Vaccine to Treat Autoimmune Disorders. Vaccines 2023, 12, 9. [CrossRef]
- Niazi, S.K.; Magoola, M. mRNA and Synthesis-Based Therapeutic Proteins: A Non-Recombinant Affordable Option. Biologics 2023, 3, 355–379. [CrossRef]
- Klein, K.; Gencoglu, M.; Heisterberg, J.; Acha, V.; Stolk, P. The Global Landscape of Manufacturers of Follow-on Biologics: An Overview of Five Major Biosimilar Markets and 15 Countries. BioDrugs 2022, 37, 235–245. [CrossRef]
- Ross, E.L.; Weinberg, M.S.; Arnold, S.E. Cost-effectiveness of Aducanumab and Donanemab for Early Alzheimer Disease in the US. JAMA Neurol. 2022, 79, 478–487. [CrossRef]
- Niazi, S.K. RNA Therapeutics: A Healthcare Paradigm Shift. Biomedicines 2023, 11, 1275. [CrossRef]
- Niazi, S.K. Making COVID-19 mRNA vaccines accessible: challenges resolved. Expert Rev. Vaccines 2022, 21, 1163–1176. [CrossRef]
| Biogen withdrew Aducanumab (BLA 761178) |
| ΨACGCGGACCGCCACCCGCGCGACGACCACACGCGCCACGACCCGGACACGGACCGCCACGGCCΨAΨΨΨΨGGCACGCGACCACGCGCCACΨCGCΨΨGΨACΨΨCGCΨGGΨΨΨACGGΨCΨCGAAAGCGCΨAGΨAΨACΨΨΨΨCGCACΨAAGGCΨCGCΨACCGGGCΨCGCACCGCACGCACΨΨΨΨΨΨCGCΨCGAΨAGACCΨAACGΨAAGCGCGCΨAACGCCGCΨΨGCΨΨCGCCΨACGCCACΨGGGACCΨACGCCCGGACCACAΨACΨACGCAΨAGACCGCGGCΨΨGΨΨGGACΨΨΨGGCCACCACCGCCΨΨAAAAΨACCGΨCGΨΨΨCΨΨCΨAGGCGΨCΨGGAAAAΨAAΨACGCCACCGCCACCACΨΨΨΨΨΨCΨAΨCGCCGAAAGΨCΨACΨΨGGΨCGACGCGCCGΨΨΨΨΨΨΨCGACGGΨAΨGGCCGGACCCGGCGΨCGCGCCCGACCΨΨGΨAAGGCΨAACCGGACGACAΨAACGCΨAGACGGCCΨΨGGCGCGΨΨΨGGCGACCΨΨΨΨΨCGCCACCGCΨΨGAAAAAAΨCGCCGΨCGACGCGCGGCACGCGCCΨACCGΨGGCΨAAAAGGCGΨCGACACGGΨCGACACGGGCCCGACGCCGACGΨCGΨGGGACΨΨGGΨCAΨAAAACCGAΨAΨCGCCGCGCAAAΨΨΨACGGACΨΨΨCΨACCGCGCCCGCΨACACCGCAAACACΨΨΨGΨAΨCGΨGGΨAAAAACΨΨΨΨGGACCGCΨΨGΨΨΨCGCCΨAGCGCΨAGΨCAΨACΨΨGACGACACGGACCΨAΨΨGΨGGGCGΨΨΨGGCCACCΨACΨΨAΨAΨΨΨCΨAACGGΨAGACCGCGΨCCACGGCΨCGGΨAΨGGCACCACCGCGCGΨCGΨACCCGCCGΨΨΨCΨΨCΨAGACΨAAACCCΨΨGACGACΨΨGGΨCCGCGΨCCΨΨGΨAAAACCGΨΨΨCΨAΨΨΨΨCGΨΨΨCΨΨAAAGΨCGACAAAΨCGΨCGGGCGΨACCGΨΨΨCΨAGACGACAAAΨΨΨCΨAΨCGCGCGΨACCGAAAGACΨΨΨCACGGCGGCGCGΨACCΨACGCΨΨΨΨACAΨAGACCCGAΨACΨΨAΨACACΨGGCGCΨAAGCGΨΨGGACGCGCΨΨCCGΨGGACGGGCCΨΨCGCGGCΨGGCΨACΨΨACGΨΨΨGGCCACΨΨΨACCACGCGCGACΨCGGΨAGΨACΨΨGCGGACΨΨΨACGCΨACΨΨACCΨCGCACΨΨGΨCGCACCCGΨΨΨΨAACΨΨACGCACΨCGCGCCΨΨΨGGΨGGCΨΨCΨAACGΨAACGCΨΨΨΨAAΨACΨΨGCCGCΨΨCGCCΨACGCΨACΨCGGACCΨACCGCCGAAACACAΨAΨAACGCCCGΨΨΨACGCCGGACCACGGCCACGACCGCCΨΨΨΨGAΨAΨΨGΨΨΨΨCGCΨAΨΨGACGCΨΨCΨAΨGGGGCCΨΨCGCCCGAΨAAAACGCCACCGCCACCACΨΨΨΨΨΨΨCGCGCΨCGCΨAGACΨGGACCCΨAΨΨGGACΨΨΨCCGΨΨΨΨΨΨΨCGACGGΨAΨGGCGCCACCCGGCGΨGGCGCCCGACCΨΨGΨAAGGCΨACCCGGACGACAΨAΨΨGΨΨΨΨAAΨΨGGΨAACGGCGAAACΨACΨΨAAAAAAΨCGCΨΨCCGACGCGCGGCCCGΨCGΨΨΨΨΨΨCΨAΨCGΨCGGACACGΨΨΨGACACGΨACCCGΨCGCCGGACΨΨGGACACGCΨΨGGCΨΨGΨΨGΨΨΨCΨΨCCGAΨAAΨACCGAΨAΨGGCCGCGCAAAGCGACGGACCACCΨΨΨΨΨCCGCΨACACCGCAAACACΨΨΨGΨAGΨCΨGGCACGGCGΨCΨΨGΨGGCCGCCGΨΨΨΨΨGGGCCΨAGGCACCCGCΨΨΨΨΨGGACΨΨGCΨΨΨΨΨCΨAAΨACΨΨGACGACACGGACCΨACCGΨGGGCGΨΨΨGGCCACCΨΨCΨΨAΨACGCΨΨGACGGΨAGACCGCGCGCGCGGCΨΨGGΨACGCCACCACΨGGGCGΨΨΨCΨAΨΨΨCΨΨCGCACGCACGΨAΨΨΨΨAAGACGCGGΨCGΨCGΨCGΨAGACAAACCGΨCGΨΨGCACΨGGCΨAACGΨCGCCGΨΨGAAAACGGACAAAGCGΨCGCΨΨΨGGΨΨΨCΨAGACGACAAAGCGCΨACΨAΨGGCACACGGACCGCΨΨΨGACGΨACΨAGCGΨΨGΨGGAΨACΨΨΨΨΨAΨAGACCCGCΨΨCΨΨAΨACACΨΨΨCGCCACCCGΨΨGGACGCGΨΨΨACGΨCGΨGGΨCGΨCGGACGACCΨΨCGCACGΨGGAAAGCGGCGGGCCCGΨCGCCGΨCGCCGΨCGCCGΨCGCACGΨCGACCACCΨΨΨCGCCGCCGCCGCACCACGΨCGGCCCGGCGΨCGGACGCGGACΨCGACGCGCCGCΨCGCCGAAACGCAAAΨCGΨCGAΨACCGΨACGΨAACCCACGCGGΨCCGCGGCCCGΨΨΨCCGGACCΨΨACCCACCGCCACΨAAACCAAACΨACCGΨGGΨΨΨΨΨΨAΨAAΨAΨGGCΨAΨCGCACΨΨΨCCGGCGAAAΨGGΨAAΨCGGCGCΨAΨΨGΨCGΨΨΨΨΨGΨGGGACAΨAGACGΨCΨACΨΨGΨGGGACGCGCGCCΨΨCΨAΨGGCGCCACAΨAAΨAACGCGCGCGCΨAGCGCCGΨAACCGCGCGCGGCGCCGGGCAΨAAΨAΨACCΨACACACCCCGΨΨΨCCGΨGGΨGGCACΨGGCACΨCGΨCGCGCΨCGΨGGΨΨΨCCGGGCΨCGCACAAAGGCGACCGCGGCΨCGΨCGΨΨΨΨCGΨGGΨCGCCGCCGΨGGCGCCGCGACCCGACGGACCACΨΨΨCΨAAΨAAAAGGCCΨΨGGCCACΨGGCACΨCGACCΨΨGΨCGCCGCGCGACΨGGΨCGCCGCACGΨAΨGGAAAGGCCGCCACGACGΨCΨCGΨCGCCGGACAΨAΨCGGACΨCGΨCGCACCACΨGGCACGGCΨCGΨCGΨCGGACCCGΨGGGΨCΨGGAΨAΨAAACGΨΨGCACΨΨGGΨAΨΨΨGGCΨCGΨΨGΨGGΨΨΨCACCΨAΨΨΨGCGCACCΨΨGGCΨΨΨΨCGACGCΨAΨΨΨΨGGGΨAΨGGACGGGCGGCACGGGCCGCGGCCΨΨGACGACCCGCCGGGCΨCGCACAAAGACAAAGGCGGCΨΨΨGGCΨΨΨCΨAΨGGGACΨACΨAAΨCGGCGΨGGGGCCΨΨCACΨGGACGCACCACCACCΨACACΨCGGΨACΨΨCΨAGGCCΨΨCACΨΨΨAAAΨΨGACCAΨACACCΨACCGCACCΨΨCACGΨAΨΨGCGCΨΨΨΨGGΨΨΨGGCGCGCΨΨCΨΨGΨCAΨAΨΨGΨCGΨGGAΨAGCGCACCACΨCGCACGACΨGGCACGACGΨAGΨCCΨAACCGACΨΨGCCGΨΨΨCΨΨAΨAΨΨΨACGΨΨΨCACΨCGΨΨGΨΨΨCGCGACGGCCGCGGCΨAACΨΨΨΨΨΨGGΨAAΨCGΨΨΨCGCΨΨΨCCGGΨCGGCGCGCΨΨGGCGΨCCACAΨAΨGGGACGGCGGCΨCGGCGCΨΨCΨΨΨACΨGGΨΨΨΨΨGGΨCCACΨCGGACΨGGACGGACCACΨΨΨCCGAAAAΨAGGCΨCGCΨAΨAACGCCACCΨΨACCCΨΨΨCGΨΨGCCGGΨCGGCCΨΨΨΨGΨΨGAΨAΨΨΨΨGGΨGGGGCGGCCACGACCΨAΨCGCΨACCGΨCGAAAAAAGACAΨAΨCGΨΨΨGACΨGGCACCΨAΨΨΨΨCGGCGACCGΨCGΨCCCGΨΨGCACAAAΨCGACGΨCGCACΨACGΨACΨΨCGCGACGΨAΨΨGGΨAAΨAΨGGGΨCΨΨΨΨCGGACΨCGGACΨCGGGCCCGCCGΨCGCCGΨCGCCGΨCGCCGΨCGCΨAΨAAGΨCΨACΨGGGΨCΨCGGGCΨCGΨCGGACΨCGCGCΨCGCACCCGCΨAGCGCACΨGGΨAAΨGGACGGCGCGCΨCGGΨCΨCGΨAAΨCGΨCGAΨAGACΨΨGACCAΨAGΨCGΨCΨΨΨGGCCCGΨΨΨCGCGGCΨΨΨGACGACΨAAAΨACGCCGCΨCGΨCGGACGΨCΨCGCCGCACGGCΨCGGCGAAAΨCGCCGΨCGCCGΨCGCCGΨGGCΨAAAAΨGGGACΨGGΨAAΨCGΨCGGACGΨCGGCCΨΨCΨAAAACGCΨGGAΨAAΨAACGGΨCGΨCΨCGAΨAΨCGΨGGGGCGACΨGGAAACCGCCGCCGΨGGΨΨΨCACCΨΨΨAAΨΨΨGCGΨGGCACCGCCGCGGCΨCGCACAAAΨAAAAAGGCGGCΨCGCΨACΨΨGΨCGACΨΨΨΨCGCCGΨGGCGCΨCGCACCACACGGACGACΨΨGΨΨGAAAAΨAGGCGCGCΨΨCGCΨΨΨCACGΨCACCΨΨΨCACCΨAΨΨGCGCGACGΨCΨCGCCGΨΨGΨCGGΨCCΨΨΨCGCACΨGGCΨΨGΨCCΨAΨCGΨΨΨCΨAΨCGΨGGAΨAΨCGGACΨCGΨCGΨGGGACΨGGGACΨCGΨΨΨCGCCΨAAΨACΨΨΨΨΨGΨAΨΨΨCACAΨACGCACGCΨΨCACΨGGGΨAGΨCCCGGACΨCGΨCGGGCCACΨGGΨΨΨΨCGAAAΨΨGGCGCCGCΨΨACG |
| Lecanemab (BLA761269) |
| AΨGCGCCΨGGCGGΨGGGCGCGCΨGCΨGGΨGΨGCGCGGΨGCΨGGGCCΨGΨGCCΨGGCGGΨGCCGGAΨAAAACCGΨGCGCΨGGΨGCGCGGΨGAGCGAACAΨGAAGCGACCAAAΨGCCAGAGCΨΨΨCGCGAΨCAΨAΨGAAAAGCGΨGAΨΨCCGAGCGAΨGGCCCGAGCGΨGGCGΨGCGΨGAAAAAAGCGAGCΨAΨCΨGGAΨΨGCAΨΨCGCGCGAΨΨGCGGCGAACGAAGCGGAΨGCGGΨGACCCΨGGAΨGCGGGCCΨGGΨGΨAΨGAΨGCGΨAΨCΨGGCGCCGAACAACCΨGAAACCGGΨGGΨGGCGGAAΨΨΨΨAΨGGCAGCAAAGAAGAΨCCGCAGACCΨΨΨΨAΨΨAΨGCGGΨGGCGGΨGGΨGAAAAAAGAΨAGCGGCΨΨΨCAGAΨGAACCAGCΨGCGCGGCAAAAAAAGCΨGCCAΨACCGGCCΨGGGCCGCAGCGCGGGCΨGGAACAΨΨCCGAΨΨGGCCΨGCΨGΨAΨΨGCGAΨCΨGCCGGAACCGCGCAAACCGCΨGGAAAAAGCGGΨGGCGAACΨΨΨΨΨΨAGCGGCAGCΨGCGCGCCGΨGCGCGGAΨGGCACCGAΨΨΨΨCCGCAGCΨGΨGCCAGCΨGΨGCCCGGGCΨGCGGCΨGCAGCACCCΨGAACCAGΨAΨΨΨΨGGCΨAΨAGCGGCGCGΨΨΨAAAΨGCCΨGAAAGAΨGGCGCGGGCGAΨGΨGGCGΨΨΨGΨGAAACAΨAGCACCAΨΨΨΨΨGAAAACCΨGGCGAACAAAGCGGAΨCGCGAΨCAGΨAΨGAACΨGCΨGΨGCCΨGGAΨAACACCCGCAAACCGGΨGGAΨGAAΨAΨAAAGAΨΨGCCAΨCΨGGCGCAGGΨGCCGAGCCAΨACCGΨGGΨGGCGCGCAGCAΨGGGCGGCAAAGAAGAΨCΨGAΨΨΨGGGAACΨGCΨGAACCAGGCGCAGGAACAΨΨΨΨGGCAAAGAΨAAAAGCAAAGAAΨΨΨCAGCΨGΨΨΨAGCAGCCCGCAΨGGCAAAGAΨCΨGCΨGΨΨΨAAAGAΨAGCGCGCAΨGGCΨΨΨCΨGAAAGΨGCCGCCGCGCAΨGGAΨGCGAAAAΨGΨAΨCΨGGGCΨAΨGAAΨAΨGΨGACCGCGAΨΨCGCAACCΨGCGCGAAGGCACCΨGCCCGGAAGCGCCGACCGAΨGAAΨGCAAACCGGΨGAAAΨGGΨGCGCGCΨGAGCCAΨCAΨGAACGCCΨGAAAΨGCGAΨGAAΨGGAGCGΨGAACAGCGΨGGGCAAAAΨΨGAAΨGCGΨGAGCGCGGAAACCACCGAAGAΨΨGCAΨΨGCGAAAAΨΨAΨGAACGGCGAAGCGGAΨGCGAΨGAGCCΨGGAΨGGCGGCΨΨΨGΨGΨAΨAΨΨGCGGGCAAAΨGCGGCCΨGGΨGCCGGΨGCΨGGCGGAAAACΨAΨAACAAAAGCGAΨAACΨGCGAAGAΨACCCCGGAAGCGGGCΨAΨΨΨΨGCGGΨGGCGGΨGGΨGAAAAAAAGCGCGAGCGAΨCΨGACCΨGGGAΨAACCΨGAAAGGCAAAAAAAGCΨGCCAΨACCGCGGΨGGGCCGCACCGCGGGCΨGGAACAΨΨCCGAΨGGGCCΨGCΨGΨAΨAACAAAAΨΨAACCAΨΨGCCGCΨΨΨGAΨGAAΨΨΨΨΨΨAGCGAAGGCΨGCGCGCCGGGCAGCAAAAAAGAΨAGCAGCCΨGΨGCAAACΨGΨGCAΨGGGCAGCGGCCΨGAACCΨGΨGCGAACCGAACAACAAAGAAGGCΨAΨΨAΨGGCΨAΨACCGGCGCGΨΨΨCGCΨGCCΨGGΨGGAAAAAGGCGAΨGΨGGCGΨΨΨGΨGAAACAΨCAGACCGΨGCCGCAGAACACCGGCGGCAAAAACCCGGAΨCCGΨGGGCGAAAAACCΨGAACGAAAAAGAΨΨAΨGAACΨGCΨGΨGCCΨGGAΨGGCACCCGCAAACCGGΨGGAAGAAΨAΨGCGAACΨGCCAΨCΨGGCGCGCGCGCCGAACCAΨGCGGΨGGΨGACCCGCAAAGAΨAAAGAAGCGΨGCGΨGCAΨAAAAΨΨCΨGCGCCAGCAGCAGCAΨCΨGΨΨΨGGCAGCAACGΨGACCGAΨΨGCAGCGGCAACΨΨΨΨGCCΨGΨΨΨCGCAGCGAAACCAAAGAΨCΨGCΨGΨΨΨCGCGAΨGAΨACCGΨGΨGCCΨGGCGAAACΨGCAΨGAΨCGCAACACCΨAΨGAAAAAΨAΨCΨGGGCGAAGAAΨAΨGΨGAAAGCGGΨGGGCAACCΨGCGCAAAΨGCAGCACCAGCAGCCΨGCΨGGAAGCGΨGCACCΨΨΨCGCCGCCCGGGCAGCGGCAGCGGCAGCGGCAGCGAAGΨGCAGCΨGGΨGGAAAGCGGCGGCGGCCΨGGΨGCAGCCGGGCGGCAGCCΨGCGCCΨGAGCΨGCAGCGCGAGCGGCΨΨΨACCΨΨΨAGCAGCΨΨΨGGCAΨGCAΨΨGGGΨGCGCCAGGCGCCGGGCAAAGGCCΨGGAAΨGGGΨGGCGΨAΨAΨΨAGCAGCGGCAGCAGCACCAΨΨΨAΨΨAΨGGCGAΨACCGΨGAAAGGCCGCΨΨΨACCAΨΨAGCCGCGAΨAACGCGAAAAACAGCCΨGΨΨΨCΨGCAGAΨGAGCAGCCΨGCGCGCGGAAGAΨACCGCGGΨGΨAΨΨAΨΨGCGCGCGCGAAGGCGGCΨAΨΨAΨΨAΨGGCCGCAGCΨAΨΨAΨACCAΨGGAΨΨAΨΨGGGGCCAGGGCACCACCGΨGACCGΨGAGCAGCGCGAGCACCAAAGGCCCGAGCGΨGΨΨΨCCGCΨGGCGCCGAGCAGCAAAAGCACCAGCGGCGGCACCGCGGCGCΨGGGCΨGCCΨGGΨGAAAGAΨΨAΨΨΨΨCCGGAACCGGΨGACCGΨGAGCΨGGAACAGCGGCGCGCΨGACCAGCGGCGΨGCAΨACCΨΨΨCCGGCGGΨGCΨGCAGAGCAGCGGCCΨGΨAΨAGCCΨGAGCAGCGΨGGΨGACCGΨGCCGAGCAGCAGCCΨGGGCACCCAGACCΨAΨAΨΨΨGCAACGΨGAACCAΨAAACCGAGCAACACCAAAGΨGGAΨAAACGCGΨGGAACCGAAAAGCΨGCGAΨAAAACCCAΨACCΨGCCCGCCGΨGCCCGGCGCCGGAACΨGCΨGGGCGGCCCGAGCGΨGΨΨΨCΨGΨΨΨCCGCCGAAACCGAAAGAΨACCCΨGAΨGAΨΨAGCCGCACCCCGGAAGΨGACCΨGCGΨGGΨGGΨGGAΨGΨGAGCCAΨGAAGAΨCCGGAAGΨGAAAΨΨΨAACΨGGΨAΨGΨGGAΨGGCGΨGGAAGΨGCAΨAACGCGAAAACCAAACCGCGCGAAGAACAGΨAΨAACAGCACCΨAΨCGCGΨGGΨGAGCGΨGCΨGACCGΨGCΨGCAΨCAGGAΨΨGGCΨGAACGGCAAAGAAΨAΨAAAΨGCAAAGΨGAGCAACAAAGCGCΨGCCGGCGCCGAΨΨGAAAAAACCAΨΨAGCAAAGCGAAAGGCCAGCCGCGCGAACCGCAGGΨGΨAΨACCCΨGCCGCCGAGCCGCGAAGAAAΨGACCAAAAACCAGGΨGAGCCΨGACCΨGCCΨGGΨGAAAGGCΨΨΨΨAΨCCGAGCGAΨAΨΨGCGGΨGGAAΨGGGAAAGCAACGGCCAGCCGGAAAACAACΨAΨAAAACCACCCCGCCGGΨGCΨGGAΨAGCGAΨGGCAGCΨΨΨΨΨΨCΨGΨAΨAGCAAACΨGACCGΨGGAΨAAAAGCCGCΨGGCAGCAGGGCAACGΨGΨΨΨAGCΨGCAGCGΨGAΨGCAΨGAAGCGCΨGCAΨAACCAΨΨAΨACCCAGAAAAGCCΨGAGCCΨGAGCCCGGGCAAAGGCAGCGGCAGCGGCAGCGGCAGCGAΨGΨGGΨGAΨGACCCAGAGCCCGCΨGAGCCΨGCCGGΨGACCCCGGGCGCGCCGGCGAGCAΨΨAGCΨGCCGCAGCAGCCAGAGCAΨΨGΨGCAΨAGCAACGGCAACACCΨAΨCΨGGAAΨGGΨAΨCΨGCAGAAACCGGGCCAGAGCCCGAAACΨGCΨGAΨΨΨAΨAAAGΨGAGCAACCGCΨΨΨAGCGGCGΨGCCGGAΨCGCΨΨΨAGCGGCAGCGGCAGCGGCACCGAΨΨΨΨACCCΨGCGCAΨΨAGCCGCGΨGGAAGCGGAAGAΨGΨGGGCAΨΨΨAΨΨAΨΨGCΨΨΨCAGGGCAGCCAΨGΨGCCGCCGACCΨΨΨGGCCCGGGCACCAAACΨGGAAAΨΨAAACGCACCGΨGGCGGCGCCGAGCGΨGΨΨΨAΨΨΨΨΨCCGCCGAGCGAΨGAACAGCΨGAAAAGCGGCACCGCGAGCGΨGGΨGΨGCCΨGCΨGAACAACΨΨΨΨAΨCCGCGCGAAGCGAAAGΨGCAGΨGGAAAGΨGGAΨAACGCGCΨGCAGAGCGGCAACAGCCAGGAAAGCGΨGACCGAACAGGAΨAGCAAAGAΨAGCACCΨAΨAGCCΨGAGCAGCACCCΨGACCCΨGAGCAAAGCGGAΨΨAΨGAAAAACAΨAAAGΨGΨAΨGCGΨGCGAAGΨGACCCAΨCAGGGCCΨGAGCAGCCCGGΨGACCAAAAGCΨΨΨAACCGCGGCGAAΨGC |
| Cinpanemab (BLA pending); discontinued by Biogen |
| AΨGCGCCΨGGCGGΨGGGCGCGCΨGCΨGGΨGΨGCGCGGΨGCΨGGGCCΨGΨGCCΨGGCGGΨGCCGGAΨAAAACCGΨGCGCΨGGΨGCGCGGΨGAGCGAACAΨGAAGCGACCAAAΨGCCAGAGCΨΨΨCGCGAΨCAΨAΨGAAAAGCGΨGAΨΨCCGAGCGAΨGGCCCGAGCGΨGGCGΨGCGΨGAAAAAAGCGAGCΨAΨCΨGGAΨΨGCAΨΨCGCGCGAΨΨGCGGCGAACGAAGCGGAΨGCGGΨGACCCΨGGAΨGCGGGCCΨGGΨGΨAΨGAΨGCGΨAΨCΨGGCGCCGAACAACCΨGAAACCGGΨGGΨGGCGGAAΨΨΨΨAΨGGCAGCAAAGAAGAΨCCGCAGACCΨΨΨΨAΨΨAΨGCGGΨGGCGGΨGGΨGAAAAAAGAΨAGCGGCΨΨΨCAGAΨGAACCAGCΨGCGCGGCAAAAAAAGCΨGCCAΨACCGGCCΨGGGCCGCAGCGCGGGCΨGGAACAΨΨCCGAΨΨGGCCΨGCΨGΨAΨΨGCGAΨCΨGCCGGAACCGCGCAAACCGCΨGGAAAAAGCGGΨGGCGAACΨΨΨΨΨΨAGCGGCAGCΨGCGCGCCGΨGCGCGGAΨGGCACCGAΨΨΨΨCCGCAGCΨGΨGCCAGCΨGΨGCCCGGGCΨGCGGCΨGCAGCACCCΨGAACCAGΨAΨΨΨΨGGCΨAΨAGCGGCGCGΨΨΨAAAΨGCCΨGAAAGAΨGGCGCGGGCGAΨGΨGGCGΨΨΨGΨGAAACAΨAGCACCAΨΨΨΨΨGAAAACCΨGGCGAACAAAGCGGAΨCGCGAΨCAGΨAΨGAACΨGCΨGΨGCCΨGGAΨAACACCCGCAAACCGGΨGGAΨGAAΨAΨAAAGAΨΨGCCAΨCΨGGCGCAGGΨGCCGAGCCAΨACCGΨGGΨGGCGCGCAGCAΨGGGCGGCAAAGAAGAΨCΨGAΨΨΨGGGAACΨGCΨGAACCAGGCGCAGGAACAΨΨΨΨGGCAAAGAΨAAAAGCAAAGAAΨΨΨCAGCΨGΨΨΨAGCAGCCCGCAΨGGCAAAGAΨCΨGCΨGΨΨΨAAAGAΨAGCGCGCAΨGGCΨΨΨCΨGAAAGΨGCCGCCGCGCAΨGGAΨGCGAAAAΨGΨAΨCΨGGGCΨAΨGAAΨAΨGΨGACCGCGAΨΨCGCAACCΨGCGCGAAGGCACCΨGCCCGGAAGCGCCGACCGAΨGAAΨGCAAACCGGΨGAAAΨGGΨGCGCGCΨGAGCCAΨCAΨGAACGCCΨGAAAΨGCGAΨGAAΨGGAGCGΨGAACAGCGΨGGGCAAAAΨΨGAAΨGCGΨGAGCGCGGAAACCACCGAAGAΨΨGCAΨΨGCGAAAAΨΨAΨGAACGGCGAAGCGGAΨGCGAΨGAGCCΨGGAΨGGCGGCΨΨΨGΨGΨAΨAΨΨGCGGGCAAAΨGCGGCCΨGGΨGCCGGΨGCΨGGCGGAAAACΨAΨAACAAAAGCGAΨAACΨGCGAAGAΨACCCCGGAAGCGGGCΨAΨΨΨΨGCGGΨGGCGGΨGGΨGAAAAAAAGCGCGAGCGAΨCΨGACCΨGGGAΨAACCΨGAAAGGCAAAAAAAGCΨGCCAΨACCGCGGΨGGGCCGCACCGCGGGCΨGGAACAΨΨCCGAΨGGGCCΨGCΨGΨAΨAACAAAAΨΨAACCAΨΨGCCGCΨΨΨGAΨGAAΨΨΨΨΨΨAGCGAAGGCΨGCGCGCCGGGCAGCAAAAAAGAΨAGCAGCCΨGΨGCAAACΨGΨGCAΨGGGCAGCGGCCΨGAACCΨGΨGCGAACCGAACAACAAAGAAGGCΨAΨΨAΨGGCΨAΨACCGGCGCGΨΨΨCGCΨGCCΨGGΨGGAAAAAGGCGAΨGΨGGCGΨΨΨGΨGAAACAΨCAGACCGΨGCCGCAGAACACCGGCGGCAAAAACCCGGAΨCCGΨGGGCGAAAAACCΨGAACGAAAAAGAΨΨAΨGAACΨGCΨGΨGCCΨGGAΨGGCACCCGCAAACCGGΨGGAAGAAΨAΨGCGAACΨGCCAΨCΨGGCGCGCGCGCCGAACCAΨGCGGΨGGΨGACCCGCAAAGAΨAAAGAAGCGΨGCGΨGCAΨAAAAΨΨCΨGCGCCAGCAGCAGCAΨCΨGΨΨΨGGCAGCAACGΨGACCGAΨΨGCAGCGGCAACΨΨΨΨGCCΨGΨΨΨCGCAGCGAAACCAAAGAΨCΨGCΨGΨΨΨCGCGAΨGAΨACCGΨGΨGCCΨGGCGAAACΨGCAΨGAΨCGCAACACCΨAΨGAAAAAΨAΨCΨGGGCGAAGAAΨAΨGΨGAAAGCGGΨGGGCAACCΨGCGCAAAΨGCAGCACCAGCAGCCΨGCΨGGAAGCGΨGCACCΨΨΨCGCCGCCCGGGCAGCGGCAGCGGCAGCGGCAGCGAAGΨGCAGCΨGGΨGGAAAGCGGCGGCGGCCΨGGΨGGAACCGGGCGGCAGCCΨGCGCCΨGAGCΨGCGCGGΨGAGCGGCΨΨΨGAΨΨΨΨGAAAAAGCGΨGGAΨGAGCΨGGGΨGCGCCAGGCGCCGGGCCAGGGCCΨGCAGΨGGGΨGGCGCGCAΨΨAAAAGCACCGCGGAΨGGCGGCACCACCAGCΨAΨGCGGCGCCGGΨGGAAGGCCGCΨΨΨAΨΨAΨΨAGCCGCGAΨGAΨAGCCGCAACAΨGCΨGΨAΨCΨGCAGAΨGAACAGCCΨGAAAACCGAAGAΨACCGCGGΨGΨAΨΨAΨΨGCACCAGCGCGCAΨΨGGGGCCAGGGCACCCΨGGΨGACCGΨGAGCAGCGCGAGCACCAAAGGCCCGAGCGΨGΨΨΨCCGCΨGGCGCCGAGCAGCAAAAGCACCAGCGGCGGCACCGCGGCGCΨGGGCΨGCCΨGGΨGAAAGAΨΨAΨΨΨΨCCGGAACCGGΨGACCGΨGAGCΨGGAACAGCGGCGCGCΨGACCAGCGGCGΨGCAΨACCΨΨΨCCGGCGGΨGCΨGCAGAGCAGCGGCCΨGΨAΨAGCCΨGAGCAGCGΨGGΨGACCGΨGCCGAGCAGCAGCCΨGGGCACCCAGACCΨAΨAΨΨΨGCAACGΨGAACCAΨAAACCGAGCAACACCAAAGΨGGAΨAAACGCGΨGGAACCGAAAAGCΨGCGAΨAAAACCCAΨACCΨGCCCGCCGΨGCCCGGCGCCGGAACΨGCΨGGGCGGCCCGAGCGΨGΨΨΨCΨGΨΨΨCCGCCGAAACCGAAAGAΨACCCΨGAΨGAΨΨAGCCGCACCCCGGAAGΨGACCΨGCGΨGGΨGGΨGGAΨGΨGAGCCAΨGAAGAΨCCGGAAGΨGAAAΨΨΨAACΨGGΨAΨGΨGGAΨGGCGΨGGAAGΨGCAΨAACGCGAAAACCAAACCGCGCGAAGAACAGΨAΨAACAGCACCΨAΨCGCGΨGGΨGAGCGΨGCΨGACCGΨGCΨGCAΨCAGGAΨΨGGCΨGAACGGCAAAGAAΨAΨAAAΨGCAAAGΨGAGCAACAAAGCGCΨGCCGGCGCCGAΨΨGAAAAAACCAΨΨAGCAAAGCGAAAGGCCAGCCGCGCGAACCGCAGGΨGΨAΨACCCΨGCCGCCGAGCCGCGAAGAAAΨGACCAAAAACCAGGΨGAGCCΨGACCΨGCCΨGGΨGAAAGGCΨΨΨΨAΨCCGAGCGAΨAΨΨGCGGΨGGAAΨGGGAAAGCAACGGCCAGCCGGAAAACAACΨAΨAAAACCACCCCGCCGGΨGCΨGGAΨAGCGAΨGGCAGCΨΨΨΨΨΨCΨGΨAΨAGCAAACΨGACCGΨGGAΨAAAAGCCGCΨGGCAGCAGGGCAACGΨGΨΨΨAGCΨGCAGCGΨGAΨGCAΨGAAGCGCΨGCAΨAACCAΨΨAΨACCCAGAAAAGCCΨGAGCCΨGAGCCCGGGCGGCAGCGGCAGCGGCAGCGGCAGCAGCΨAΨGAACΨGACCCAGCCGCCGAGCGΨGAGCGΨGAGCCCGGGCCAGACCGCGCGCAΨΨACCΨGCAGCGGCGAAGCGCΨGCCGAΨGCAGΨΨΨGCGCAΨΨGGΨAΨCAGCAGCGCCCGGGCAAAGCGCCGGΨGAΨΨGΨGGΨGΨAΨAAAGAΨAGCGAACGCCCGAGCGGCGΨGCCGGAACGCΨΨΨAGCGGCAGCAGCAGCGGCACCACCGCGACCCΨGACCAΨΨACCGGCGΨGCAGGCGGAAGAΨGAAGCGGAΨΨAΨΨAΨΨGCCAGAGCCCGGAΨAGCACCAACACCΨAΨGAAGΨGΨΨΨGGCGGCGGCACCAAACΨGACCGΨGCΨGAGCCAGCCGAAAGCGGCGCCGAGCGΨGACCCΨGΨΨΨCCGCCGAGCAGCGAAGAACΨGCAGGCGAACAAAGCGACCCΨGGΨGΨGCCΨGAΨΨAGCGAΨΨΨΨΨAΨCCGGGCGCGGΨGACCGΨGGCGΨGGAAAGCGGAΨAGCAGCCCGGΨGAAAGCGGGCGΨGGAAACCACCACCCCGAGCAAACAGAGCAACAACAAAΨAΨGCGGCGAGCAGCΨAΨCΨGAGCCΨGACCCCGGAACAGΨGGAAAAGCCAΨCGCAGCΨAΨAGCΨGCCAGGΨGACCCAΨGAAGGCAGCACCGΨGGAAAAAACCGΨGGCGCCGACCGAAΨGCAGC |
| Element | Description |
| Cap (2) | A modified 5’-cap1 structure (m7G+m3'-5'-ppp-5'-Am): GA |
| 5’-UTR (52) | The 5´-untranslated region derived from human alpha-globin RNA with an optimized Kozak sequence. GAATAAACTAGTATTCTTCTGGTCCCCACAGACTCAGAGAGAACCCGCCACC |
| Signal peptide (48) | S glycoprotein signal peptide (extended leader sequence) guides translocation of the nascent polypeptide chain into the endoplasmic reticulum: ATGTTCGTGTTCCTGGTGCTGCTGCCTCTGGTGTCCAGCCAGTGTGTG |
| Coding region (n) | Codon-optimized sequence (ORF) |
| 3’-UTR (268) | The 3´ untranslated region comprises two sequence elements derived from the amino-terminal enhancer of split (AES) mRNA and the mitochondrial encoded 12S ribosomal RNA to confer RNA stability and high total protein expression: GCTAGCTGCCCCTTTCCCGTCCTGGGTACCCCGAGTCTCCCCCGACCTCGGGTCCCAGGTATGCTCCCACCTCCACCTGCCCCACTCACCACCTCTGCTAGTTCCAGACACCTCCCAAGCACGCAGCAATGCAGCTCAAAACGCTTAGCCTAGCCACACCCCCACGGGAAACAGCAGTGATTAACCTTTAGCAATAAACGAAAGTTTAACTAAGCTATACTAACCCCAGGGTTGGTCAATTTCGTGCCAGCCACACCCTGGAGCTAGC |
| poly(A) (110) | A 110-nucleotide poly(A)-tail consisting of a stretch of 30 adenosine residues, followed by a 10-nucleotide linker sequence and another 70 adenosine residues: AAAAAAAAAAAAAAAAAAAAAAAAAAAAAAGCATATGACTAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAAA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





