1. Introduction
There are many clinical tools for preoperative assessment of difficult intubation and no matter how detailed assessment may be, there is still a significant number of unanticipated airway difficulties. This is why there is still a need to provide further studies in order to define more precise and accurate parameters and tests to timely predict serious complications [
1,
2,
3].
Preoperative airway assessment is even more difficult in ENT surgery, and especially laryngology, where an anesthesiologist is faced with morphological changes on airway itself. There are multiple practice situations where not a single prediction assessment tool, which is useful in other surgical fields, can effectively be used in ENT surgery. Therefore, there is a need to develop specific assessment tools for ENT surgery and laryngology.
In the year of 1998, Arne et al. developed and validated a single index for prediction of difficult airway for both general and ENT surgery and provided a universal cut-off value [
4,
5]. Since ENT surgery has a broad spectrum of head and neck pathologies, we tested the accuracy of this score in patients who had laryngeal lesions and masses.
With the development of medical engineering, there is an emerging trend to use modern means of visualization and diagnostics [
6,
7,
8,
9]. Expert consensus on difficult airway assessment recommended in 2023. that transnasal endoscopy can be used for preoperative assessment of patients with periglottic lesions or abnormal airway structures [
6]. Since laryngeal pathology is very specific, we have tested the accuracy of a combination of flexible laryngoscopy with ARNE score.
2. Materials and Methods
We have included a total of 100 patients in this prospective pilot clinical study. All the included patients were scheduled for microscopic laryngeal surgery at the Clinic for Otorhinolaryngology, University Clinical Center in Nis, in the period from June to November 2023. Inclusion criteria were: diagnosis of a vocal cord change, planned general endotracheal anesthesia, age over 18 years and the absence of a tracheostomy. Exclusion criteria were: patients younger than 18 years, presence of a tracheostomy cannula, patients’ refusal to participate in our research, inability to understand and/or sign an informed consent and urgent surgical interventions.
All the included patients were informed about our research and signed an informed consent. Clinical examination was performed a day before surgery by an anesthesiologist and a specially designed questionnaire was filled. Among other general and clinical data, this questionnaire contained the data needed to calculate the ARNE score. The data needed for ARNE score calculation are provided in the Table 1. Total possible points are 48, however, according to authors recommendations, 11 points are used as a cut-off value. Therefore, all the patients who have a total score above 11 were considered to have potentially difficult intubation.
Table 1.
Calculation of ARNE score.
Table 1.
Calculation of ARNE score.
| Risk factors |
|
Points |
| Previous knowledge of difficult intubation |
No
Yes |
0
10 |
| Pathologies associated with difficult intubation |
No
Yes |
0
5 |
| Clinical symptoms of airway pathology |
No
Yes |
0
3 |
| Inter-incisor gap (IIG) and mandible luxation (ML) |
IIG≥5 cm ili ML˃0
3.5 cm˂IIG˂5 cm i ML=0
IIG˂3.5 cm i ML˂0 |
0
3
13 |
| Thyromental distance |
≥6.5 cm
˂6.5 cm |
0
4 |
| Maximal range of head and neck movement |
˃100°
90°±10°
˂80° |
0
2
5 |
| Mallampati’s modified test |
Class 1
Class 2
Class 3
Class 4 |
0
2
6
8 |
| TOTAL POSSIBLE |
|
48 |
All the included risk factors were measured according to previous relevant recommendations and everyday clinical practice. The following pathologies were considered to be associated with difficult intubation: malformations in the facial area, acromegaly, cervical spondylosis with limited neck mobility, atlanto-occipital joint diseases, respiratory tract tumors and stiff joint syndrome. All the included patients had a score of 5 since one of the inclusion criteria was change on the vocal cords. Clinical symptoms of airway pathology were defined as one of the following: dyspoea, dysphonia, dysphagia and sleep apnea syndrome.
Each patient was clinically examined by an ENT surgeon and flexible laryngoscopy was performed. Before the surgery, the ENT surgeon was asked to declare the airway as difficult or not according to seen pathology and previous experience.
Difficulty of intubation was assessed according to clinically accepted intubation difficulty scale (IDS). Parameters needed to calculate IDS score are provided in the Table 2. We have considered the following as alternative techniques: repositioning of the patient, changing of the laryngoscope blade, change of endotracheal tube size, use of bougie or fiberoptic bronchoscope.
Table 1.
Calculation of IDS score.
Table 1.
Calculation of IDS score.
| Parameter |
Score |
| Number of attempts˃1 |
Every additional attempt adds 1 point |
| Number of operators˃1 |
Every additional operator adds 1 point |
| Number of alternative techniques |
Seach alternative technique adds 1 point |
| Cormack-Lehane grade |
Grade 1=0 points
Grade 2=1 points
Grade 3=2 points
Grade 4=3 points |
| Lifting force required |
Normal=0 points
Increased=1 points |
| Laryngeal pressure |
No=0 points
Yes=1 points |
| Vocal cords mobility |
Adbuction=0 points
Adduction=1 points |
The statistical significance was calculated using Mann Whitney U test. We have used binary statistic regression to predict the outcome and combine different parameters. The area under the curve (AUC) was determined with the aim of defining the cut-off value of statistically significant scale parameters. P value below 0.05 was considered a statistically significant result. All results were statistically processed in the program SPSS10.0 (Statistical Package for the Social Sciences, Chicago, IL, USA) for Windows.
The study was approved by the Ethical Committee of Medical School, University in Niš, Niš, Serbia and by the Ethical Committee of the University Clinical Center of Niš, Niš. Serbia.
3. Results
The mean age of included patients was 60.31±31 years, with 37% of female and 63% of male patients. A total of 33 patients (33%) had difficult intubation according to IDS score with 4% of patients who were not possible to intubate with any alternative technique due to changes on the vocal cords and surgical airway was established.
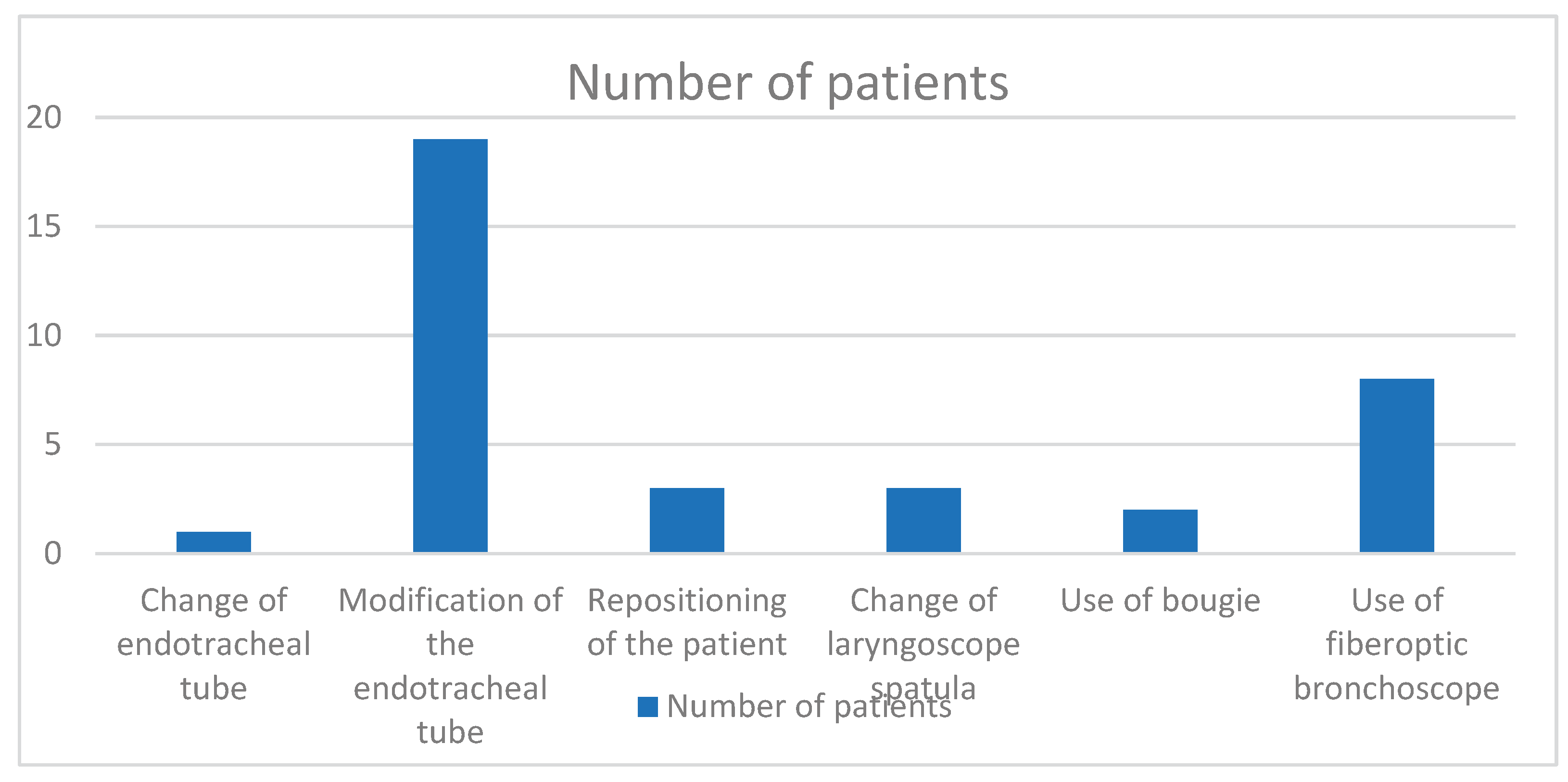
There was a need to use alternative intubation techniques in 30 patients out of which 26 (88.66%) were difficult to intubate, according to IDS score. Details about types of used alternative techniques are provided on the
Figure 1, with a reference that there were two or more techniques used in several patients.
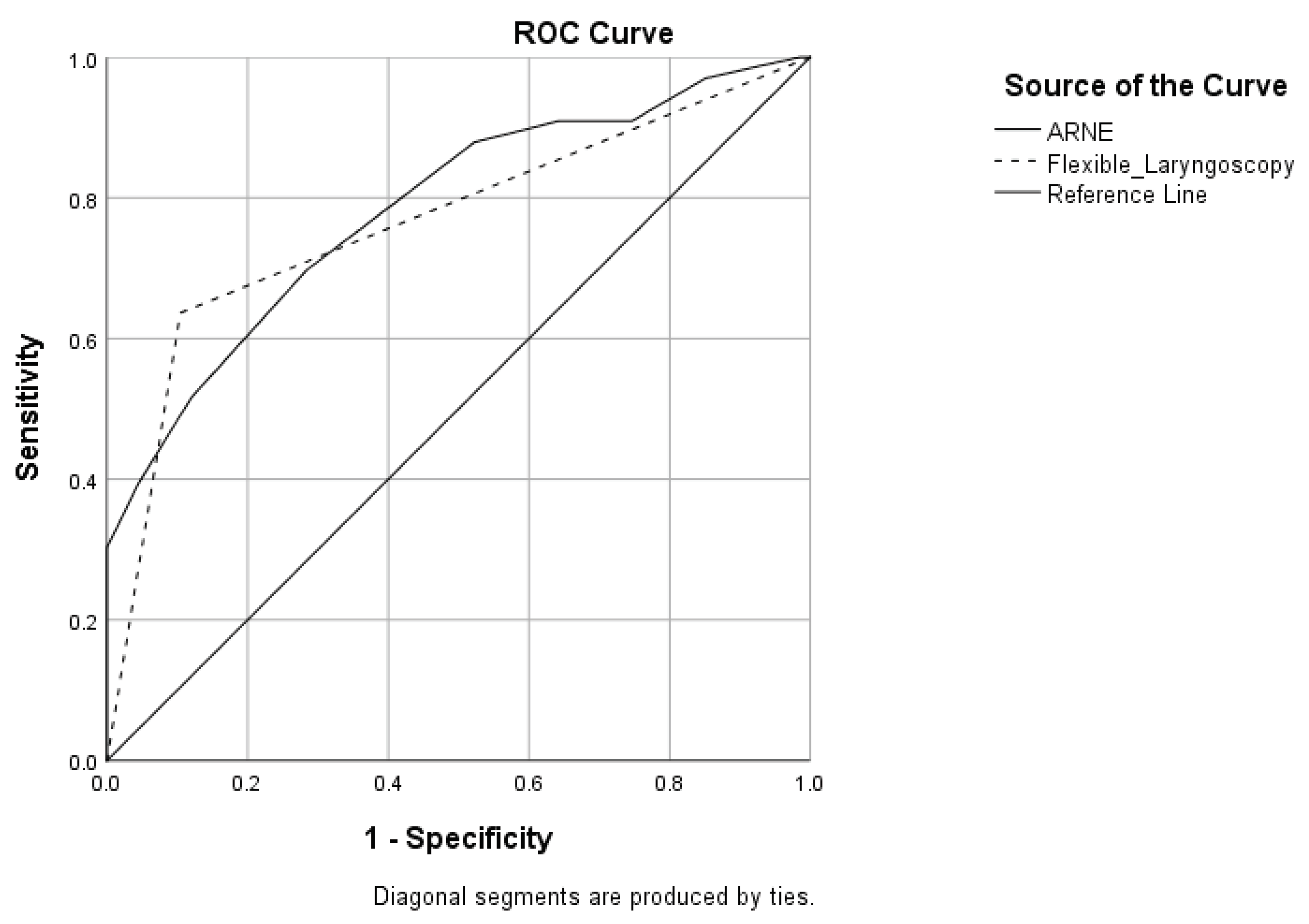
After calculating IDS score we have divided patients into two groups, the difficult intubation (DI) and normal intubation (NI) group. Then we have calculated ARNE score for each patient according to data provided in Table 1 and ARNE score showed to be an accurate score for predicting difficult intubation in laryngology with P<0.0001 and AUC curve 0.784 (P<0.0001, 95% CI 0.685-0.884) (
Figure 2). It is important to signify that as much as 85% had one or more clinical symptoms of airway pathology. As an independent parameter flexible laryngoscopy showed to be accurate with P<0.0001 and AUC curve 0.766 (P<0.0001, 95% CI 0.657-0.875) (
Figure 2).
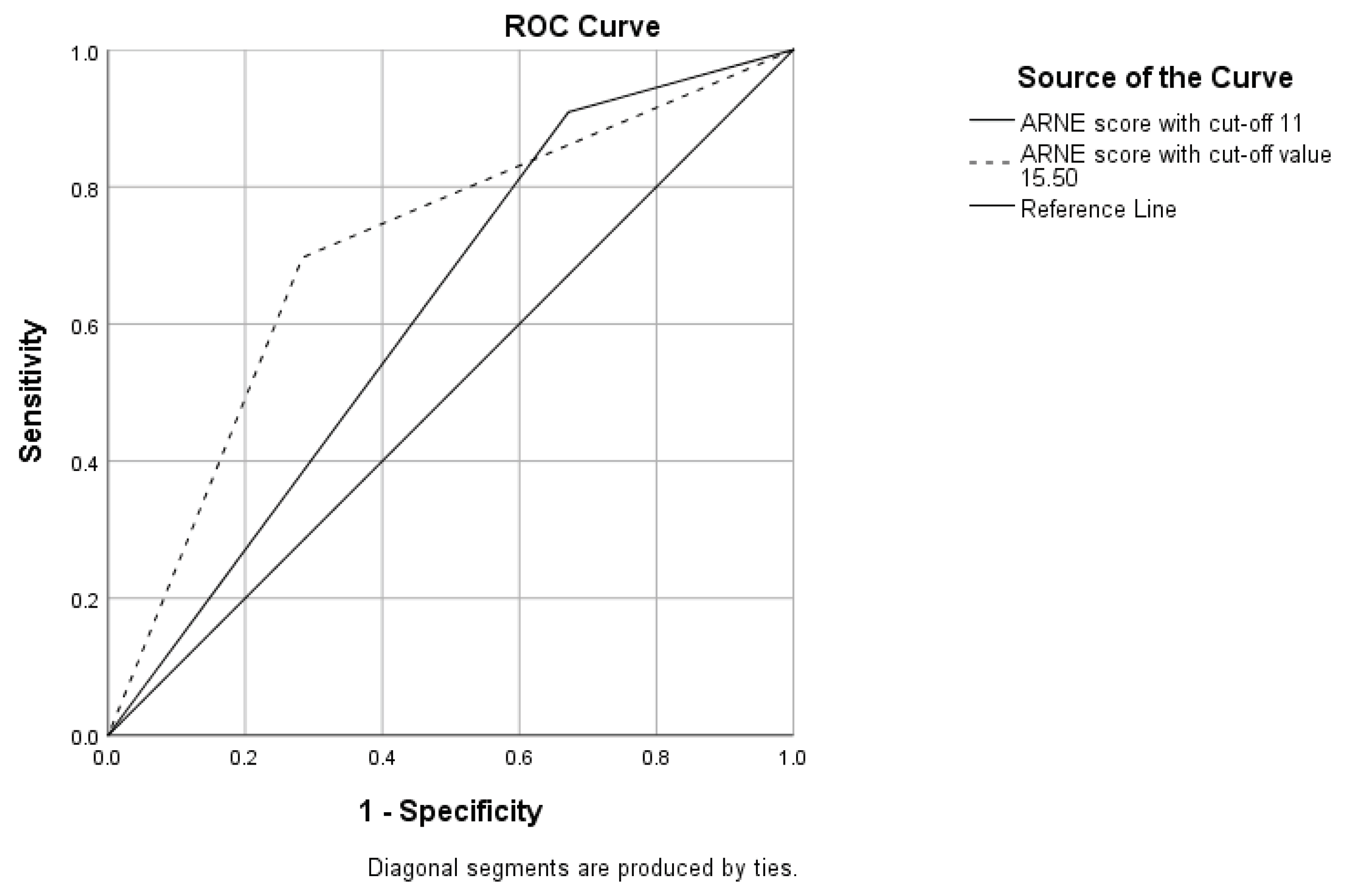
We used a recommended cut-off value to divide patients in two groups, above and below total score of 11 and as much as 75% were defined as „difficult to intubate“. This model retained statistical significance of P<0.010, however lost statistical significance in C statistics with AUC 0.619 (P=0.054, 95% CI 0.517-0.730). We have then defined a new cut-off value of 15.50, according to AUC ROC curve results, with sensitivity of 69.7% and specificity of 71.6%. When we divided the patients in two groups according to new cut-off value, the new statistical model improved with P<0.0001 and AUC 0.707 (P=0.001, 95% CI 0.596-0.817) (
Figure 3). Also, this cut-off value predicted difficult intubation in 42% of the patients.
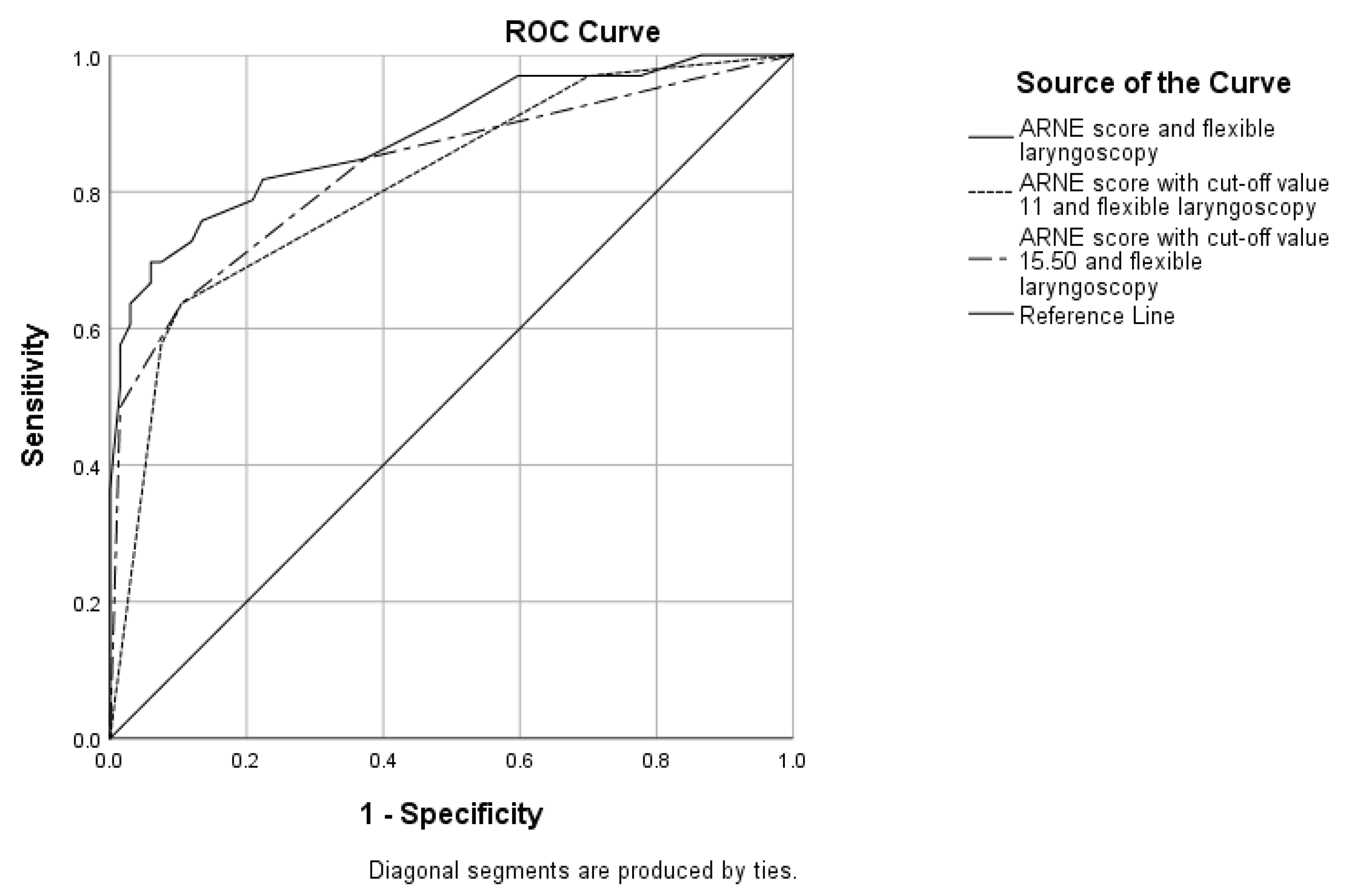
Since flexible laryngoscopy is routinely used in laryngology and this pathology is extremely specific we have combined flexible laryngoscopy with ARNE score and ARNE score with recommended and new cut-off values. Results are provided in
Figure 4.
4. Discussion
The percent of difficult intubations in our study is 33% which is higher than in other studies (10-12). This can be explained by the fact that all the included patients had tumors on laryngeal level and in some cases made endotracheal intubation more difficult (13). This statement is confirmed by the data provided by Barclay-Steuart et al. who had an incidence of predicted difficult intubations of 24.7% in patients with pharyngolaryngeal lesions (14). Also, the number of impossible intubations in our study was high with 4% of patients whose airway was surgically established. Research show that in our county there is a high number of patients who present with advanced disease and that the median lost time is 8.77 months beginning from the first symptoms to diagnosis (15, 16). Treatment outcome and survival rates depend on established stage of disease, also these patients are harder to intubate since they present with a high rate stridor and a greater airway obstruction (11, 17, 18). Tasli et al. reported an incidence of 3.3% of impossible intubations in ENT patients, which correlates with out results (19).
There is a great need for an accurate score in ENT and especially laryngeal surgery. There are no official recommendations and research in this field are rare while generally used parameters and tests of difficult intubation prediction are not accurate in ENT surgery (20, 21). The score provided by Arne et al. is presented as specific for both general and ENT surgeries, however, specificity of laryngeal pathology implicated that this score may not be completely accurate. We can see that ARNE score alone can not be used independently as a completely accurate prediction score with AUC 0.784. Also, when the recommended cut-off value of 11 is provided, AUC is statictically insignificant and falls to 0.619, with 75% of patients predicted as difficult to intubate. One of the reasons for this can be found in the fact that all the included patients had maximum points for the risk factor named „Pathologies associated with difficult intubation“ and as much as 85% of patients had a maximum points for „Clinical symptoms of airway pathology“. Also, there is a great limitation in our research when it comes to the risk factor „Previous knowledge of difficult intubation“. There are no official data about previous difficult intubations in our country and many times patients are not informed about the existence of difficult airway.
According to AUC ROC curve, we have recommended a new cut-off value of 15.50, which improves AUC to 0.707 and brings back the statistical significance to the model. However, with this result, ARNE score still can not be considered to be independently accurate in the preoperative settings. This bring us to the problem what is the right mean to distinct real difficult intubation in laryngeal pathology.
As previously mentioned, there is a growing tendency to use modern diagnostic and visual technologies in patients when there is a predicted high risk for difficult intubation. There is special need for their use in laryngology since airway pathology can severely compromise endotracheal intubation (6, 22, 23).
When added to ARNE score without cut-off values and with recommended and new cut-off values, flexible laryngoscopy improves the prediction with AUC respectively: 0.882, 0.813 and 0.833. Flexible laryngoscopy, together with other visual technology, has improved difficult intubation prediction in other studies (8, 24). This implicates the neccessity of multidisciplinary preoperative assessment of airway in laryngology, which is also confirmed by other authors in, mostly, case reports (25-27).
When it comes to flexible laryngoscopy, there is a neccessity of surgical subjective assessment of airway difficulty. There is a developed Tasli classification of transnasal flexible laryngoscopy, however, this can not be applied to laryngeal tumor pathology since this classification is mostly based on normal airway and is simmilar to Cormack-Lehane gradation (19).
There is a neccessity for further research with the aim of developing accurate tests and scores for prediction of difficult airway in laryngology. These models would have to include modern visual diagnostic technology and surgical assessment.
5. Conclusions
ARNE score can not be used as an independent predictor in difficult airway prediction in patients with laryngeal pathology. It is recommended to use flexible laryngoscopy and use multidisciplinary approach in difficult airway prediction. Also, universally recommended cut-off value of 11 can not be effectively used in laryngology and a new cut-off value of 15.50 is recommended.
Author Contributions
All authors contributed to the study conception and design. Study design was performed by Danica Marković, Milan Stanković, Vesna Marjanović and Maja Šurbatović. Material preparation, data collection and analysis were performed by Danica Marković, Milan Stanković, Dušan Milisavljević and Biljana Stošić. The first draft of the manuscript was written by Danica Marković, review and editing was done by Milan Stanković, Maja Šurbatović, Vesna Marjanović and Biljana Stošić and all authors commented on previous versions of the manuscript. Supervision was done by Milan Stanković. All authors read and approved the final manuscript.
Funding
Please add: This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of MEDICAL SCHOOL, UNIVERSITY IN NIŠ, NIŠ, SERBIA (protocol code 22-6600/2-2 and 08.06.2023.) by the Ethics Committee of UNIVERSITY CLINICAL CENTER IN NIŠ, NIŠ, SERBIA (protocol code 13235/6 and 11.05.2023.)
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on demand.
Acknowledgments
We thank Primarius Tatjana Kovačević, MD, PhD, Dragana Mitrović, MD, Toma Kovačević, MD, Tanja Cvetković, Senior OT techinican and Darko Djordjević, Senior OT techinican, for their valuable assistance considering data collection.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ellard, L; Wong, D. T. Preoperative Airway Evaluation. Curr Anesthesiol Rep. 2020, 10, 19–27. [Google Scholar] [CrossRef]
- Apfelbaum. J.L.; Hagberg, C.A.; Connis, R.T.; Abdelmalak, B.B.; Agarkar, M. et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022, 136, 31–81. [Google Scholar] [CrossRef]
- Trambadia DN, Yadav P, A S. Preoperative Assessment to Predict Difficult Airway Using Multiple Screening Tests. Cureus. 2023, 15, e46868. [Google Scholar]
- Arné, J.; Descoins, P.; Fusciardi, J.; Ingrand, P.; Ferrier, B.; Boudigues, D.; Ariès, J. Preoperative assessment for difficult intubation in general and ENT surgery: predictive value of a clinical multivariate risk index. Br J Anaesth. 1998, 80, 140–6. [Google Scholar] [CrossRef]
- Descoins, P.; Arné, J.; Bresard, D.; Ariès, J.; Fusciardi, J. Proposal for a new multifactor screening score of difficult intubation in ORL and stomatognathic surgery: preliminary study. Ann Fr Anesth Reanim. 1994, 13, 195–200. [Google Scholar] [CrossRef]
- Xia, M.; Ma, W.; Zuo, M.; Deng, X.; Xue, F.; Battaglini, D.; et al. Expert consensus on difficult airway assessment. Hepatobiliary Surg Nutr. 2023, 12, 545–66. [Google Scholar] [CrossRef] [PubMed]
- Burgess, M.B.; Schauer, S.G.; Hood, R.L.; De Lorenzo, R.A. The Difficult Airway Redefined. PDM. 2022, 37, 723–6. [Google Scholar] [CrossRef] [PubMed]
- Gemma, M.; Buratti, L.; Di Santo, D.; Calvi, M.R.; Ravizza, A.; Bondi, S.; et al. Pre-operative transnasal endoscopy as a predictor of difficult airway: A prospective cohort study. EJA. 2020, 37, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Altun, D.; Kara, H.; Bozbora, E.; Ali, A.; Dinç, T.; Sonmez, S.; et al. The Role of Indirect Laryngoscopy, Clinical and Ultrasonographic Assessment in Prediction of Difficult Airway. Laryngoscope 2021, 131, E555-60. [Google Scholar] [CrossRef] [PubMed]
- Tuzuner-Oncul, A.M.; Kucukyavuz, Z. Prevalence and Prediction of Difficult Intubation in Maxillofacial Surgery Patients. J Oral Maxillofac Surg. 2008, 66, 1652–8. [Google Scholar] [CrossRef] [PubMed]
- Jayaraj, A.K.; Siddiqui, N.; Abdelghany, S.M.O.; et al. Management of difficult and failed intubation in the general surgical population: a historical cohort study in a tertiary care centre. Can J Anesth/J Can Anesth. 2022, 69, 427–37. [Google Scholar] [CrossRef]
- Adnet, F.; Racine, S.X.; Borron, S.W.; Clemessy, J.L.; Fournier, J.L.; Lapostolle, L.; et al. A survey of tracheal intubation difficulty in the operating room: a prospective observational study. Anesthesiologica Scandinavica. 2001, 45, 327–32. [Google Scholar] [CrossRef]
- Brenner, M.J.; Cramer, J.D.; McGrath, B.A. et al. Oral Intubation Attempts in Patients With a Laryngectomy: A Significant Safety Threat. Otolaryngol Head Neck Surg 2021, 164, 1040–3. [Google Scholar] [CrossRef]
- Barclay-Steuart, A.; Großhennig, H.L.; Sasu, P.; Wünsch, V.A.; Stadlhofer, R.; Berger, J. et al. Transnasal Videoendoscopy for Preoperative Airway Risk Stratification: Development and Validation of a Multivariable Risk Prediction Model. Anesth Analg 2023, 136, 1164–73. [Google Scholar] [CrossRef]
- Dragicevic, D.; Anđelic, B. M.; Jovic, R.; Kljajic, V.; Vlaski, L.; Savovic, S. Clinical stage of laryngeal carcinoma and lost time at the moment of diagnosis with 15-year-long interval. Are there any changes? J BUON. 2019, 24, 2499–505. [Google Scholar]
- Čanković. M.; Tešić, M.; Jevtić, M.; Stevanović, D.; Jovanović, M.B.; Kostić, D. et al. Predictors of health-related quality of life in Serbian patients with head and neck cancer. Med Oral Patol Oral Cir Bucal. 2022, 27, e340–50. [Google Scholar]
- Jovic, R.; Miladinov-Mikov, M.; Canji, K.; Mitrovic, S. Some epidemiological characteristics of laryngeal cancer in the province of Vojvodina from 1985-1996. Archive of Oncology. 2001, 9, 17–9. [Google Scholar]
- Mason, R.A.; Fielder, C.P. The obstructed airway in head and neck surgery. Anaesthesia. 1999, 54, 625–8. [Google Scholar] [CrossRef] [PubMed]
- Tasli, H.; Karaman, N.E.; Isler, D.; Subasi, B. A Predictor of Difficult Airway: The Tasli Classification in Transnasal Flexible Laryngoscopy. Journal of Voice. 2023, 37, 945–50. [Google Scholar] [CrossRef]
- Li, W.X.; Wang, D.D.; Li, X.; Li, W.X.; Han, Y.; Cai, Y.R. Risk factors for difficult mask ventilation and difficult intubation among patients undergoing pharyngeal and laryngeal surgery. Helyon. 2023, 9, e14408. [Google Scholar] [CrossRef]
- Kumar, A.; Kumar Gupta, A.; Singh Rathore, V.; Kanwar Shekhawat, K. Assessing risk factors for challenging intubation in ENT surgeries: a preoperative evaluation approach. Int J Life Sci Biotechnol Pharma Res. 2023, 12, 464–8. [Google Scholar]
- Ottoveggio, G.; Verro, B.; Lapi, M.; Tarantino, F.; Beccia, G.; Saraniti, C. Difficult intubation in ENT patient: Simultaneous videolaryngoscopy with flexible bronchoscopy. A combined approach. Case report. Int J Surg Case Rep 2024, 116, 109345. [Google Scholar] [CrossRef]
- Daggupati, H.; Maurya, I.; Singh, R.D.; Ravishankar, M. Development of a scoring system for predicting difficult intubation using ultrasonography. Indian J Anaesth. 2020, 64, 187–92. [Google Scholar]
- Narula, S.; Mann, D.S.; Sadana, N.; Vasan, N.R. Evaluating the utility of pre-operative airway assessment for intubation management in difficult airway patients. J Laryngol Otol. 2020, 134, 909–16. [Google Scholar] [CrossRef]
- Hofmeyr, R.; Llewellyn, R.; Fagan, J.J. Multidisciplinary difficult airway challenges: Perioperative management of glottic and supraglottic tumors. Oper Tech Otolayngol Head Neck Surg. 2020, 31, 120–7. [Google Scholar] [CrossRef]
- Pandian, V.; Ghazi, T.U.; He, M.Q, et al. Multidisciplinary Difficult Airway Team Characteristics, Airway Securement Success, and Clinical Outcomes: A Systematic Review. Ann Otol Rhinol Laryngol. 2023, 132, 938–54. [Google Scholar] [CrossRef] [PubMed]
- McAvoy, J.; Ewing, T.; Nekhendzy, V. The value of preoperative endoscopic airway examination in complex airway management of a patient with supraglottic cancer. JoHNA 2019, 3, e19. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).