1. Introduction
The posterior maxilla represents a clinical challenge due to anatomical limitations, alveolar bone resorption and sinus pneumatization following tooth loss in combination with type IV low-density bone [
1], factors that lead to bone deficiencies, significantly limiting the insertion of implants of desired length and diameter, besides making it difficult to achieve adequate primary stability. The lack of bone volume has been overcome by the development of different techniques and a large number of innovative surgical procedures, from short implants to pterygoid or zygomatic implants [
2,
3]. Some of these procedures have a high rate of morbidity, are delicate to perform and require advanced surgical skills by the operator. Alternatively, a less invasive procedure, the maxillary sinus floor elevation, has been widely studied by numerous clinical studies [
4,
5].
The residual bone height of the maxillary sinus determines the surgical augmentation technique. Maxillary sinus floor elevation with a lateral (lSFE) or transcrestal (tSFE) approach represents two surgical options to vertically enhance the available bone in the edentulous posterior maxilla [
6]. Both augmentation techniques are clinically effective in achieving a vertical increase in the dimension of the crest and are associated with high implant survival rates [
7,
8]. The first sinus lift procedure was described in 1976 by Tatum at the Alabama Implant Congress and published by Philip Boyne and James in 1980. It consisted of a vestibular antrostomy and filling of the cavity with autologous bone or other bone substitutes, leaving a 6-month healing period. The osteotome sinus floor elevation (OSFE) technique is a less invasive approach [
9], less time-consuming and reduces post-operative discomfort [
10] using osteotomes to increase the density of the maxillary bone by compaction and allowing the insertion of the implants with good primary stability [
11]. Later, Cosci et al. [
12] introduced an atraumatic method to perform the transcrestal technique by using a series of drills of different lengths to avoid perforation of the Schneiderian membrane during drilling. To reduce trauma and risk of membrane perforation, several techniques for the transcrestal approach have been discussed, including balloon elevation technique [
13], hydraulic sinus condensing technique [
14], trephine assisted lifting, MISE technique [
15], Kit CAS [
16]. Other advantages of the transcrestal approach are the possibility to combine in one surgical step the sinus elevation and regeneration with biomaterials along with the simultaneous insertion of the implants, and the applying a functional load earlier compared to the lateral sinus floor elevation [
17,
18]. However, the tSFE technique may present some disadvantages associated with a lower bone gain, not having a direct optical control [
19] and it is a technique that requires a minimal residual bone height to be performed [
2,
20].
Regarding this last factor, scientific literature has been evolving over the years. Initially, according to Jensen’s classification, a minimum availability of 7-9 mm of residual bone was required to perform the transcrestal technique [
21]. To date, there is sufficient scientific evidence demonstrating that the technique is safe and successful with 5 mm of residual bone high (RBH) [
20,
22,
23,
24]. However, several studies have shown that the OSFE procedure has been successfully performed in posterior maxillae with an RBH of <4 mm [
24,
25,
26]. Using this technique, the reconstruction of the posterior maxilla can be simplified and accelerated. To date, no evidence has indicated a critical threshold RBH value for the survival of implants placed with OSFE.
In order to obtain greater bone gain during sinus augmentation procedures, different graft materials mixed with or without autologous bone have been frequently used [
27,
28]. Autogenous bone grafts are considered the gold standard, owing to their maintenance of cellular and osteogenic viability [
29]. Boyne, James, and Tatum first reported the use of autogenous grafts in sinus floor elevation [
30,
31]. To reduce the volume of autogenous bone to be harvested and the morbidity of the donor area, different bone substitutes are used in sinus augmentation. Tricalcium phosphate was the first bone substitute to be successfully applied for sinus floor elevation [
32] and some studies have registered the improvement in postoperative period; limited pain and fewer complications were noted [
33]. Nevertheless, the necessity of grafting material to maintain the space for new bone formation after elevating the sinus membrane by using the crestal approach remains controversial [
29].
The most common intraoperative complication associated with maxillary sinus lift surgery is the perforation of the sinus membrane [
21]. Other surgical or post-surgical complications described in the literature were postoperative infection, nasal bleeding, oedema, and graft bone resorption [
12,
21]. To minimize the risk of Schneiderian membrane perforation, novel instruments designed specifically for sinus membrane lifting have been proposed [
34].
The study aimed to evaluate implant success and bone height variations after tSFE using the osseodensification technique (OD) combined with beta-tricalcium phosphate (β-TCP), as bone graft material and simultaneous implant placement.
2. Materials and Methods
2.1. Study Population
The study was designed as a prospective non-randomized pilot clinical trial and approved by the ethics committee of the Catholic University of Valencia San Vicente Mártir (Valencia, Spain) (Expte.UCV/2019-2020/040). All the clinical procedures were performed in full accordance with the Declaration of Helsinki 2013, version Fortaleza and CIOMS, 2002. Each patient provided written informed consent before participation. This manuscript was prepared in full accordance with Organic Law 3/2018 on the Protection of Personal Data and ensuring compliance with the regulations.
Patients were consecutively recruited and treated at the Catholic University of Valencia San Vicente Mártir from May 2020 to May 2021. Surgical procedures were performed by the students in the second year of the Master of Oral Surgery and Implantology, having all similar surgical experience, under the supervision of experienced clinical professors during the period of the study.
Inclusion criteria for patient eligibility were as follows: (i) age ≥18 years; (ii) systemic and local conditions suitable for implant placement and sinus floor elevation procedures; non-smoking patients or ≤ 10 cigarettes/day; (iii) indication for the placement of at least one implant in premolar or molar region of the maxilla with insufficient bone height (< 8 mm), without the need for horizontal bone augmentation (minimum width of 5 mm); (iv) patient willing and fully capable of complying with the study protocol; (v) minimum follow-up of one year.
Exclusion criteria were as follows: (i) any general contraindication for implant surgery (ie: uncontrolled diabetes or hypertension, acute or chronic rhinosinusitis, allergic rhinitis); (ii) Localized contraindications for implant surgery: acute or chronic infection; inflammation in the area intended for implant placement; tooth extraction tooth <3 months after surgery; (iii) Untreated periodontal disease or poor oral hygiene and non-collaborators (plaque index> 25%); (iv) Patients with an INR outside the range of between 2-4.
2.2. Statistical Analysis
To obtain the sample, consecutive non-probabilistic sampling was used, and the bone availability was studied before surgery, immediately after surgery and the final bone height at 12 months. The standard deviation was obtained from the study by Gonzalez et al. [
35]: 0.63 and the difference between the initial and final mean was 0.55. A sample size of 14 patients was estimated to ensure that the sample data came from a population with a normal distribution. To study whether the differences were statistically significant, we used comparison t-tests for related samples. Moreover, a bivariate correlation test was performed, since the sample size is small, the Spearman correlation test was used.
The statistical analysis of the data collected for the present study was performed using the SPSS 23 computer program, using a confidence level of 95% and considering statistically significant these comparison results for which the p-value obtained was less than 0.05.
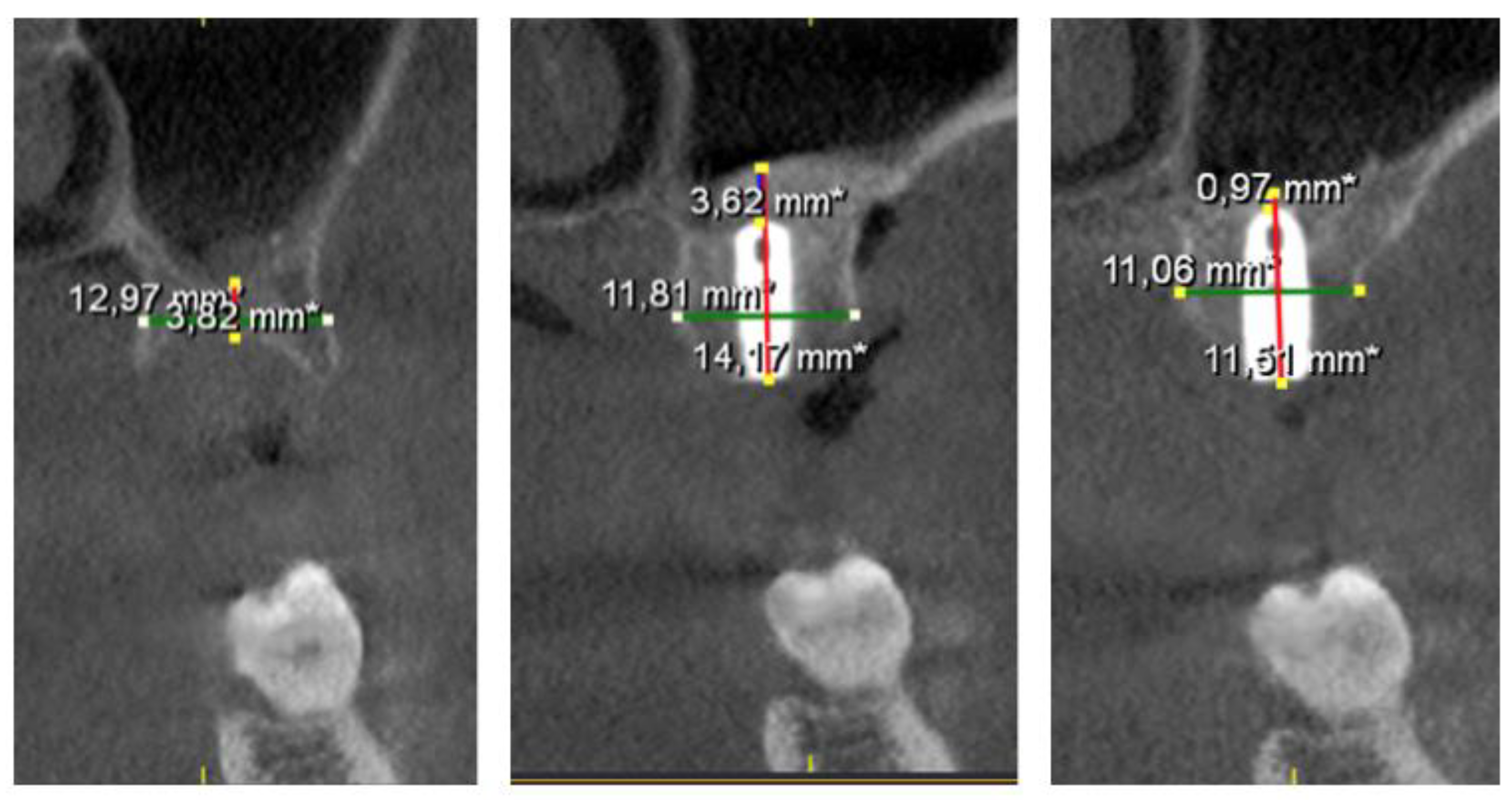
2.3. Radiographic Study
All included patients underwent a full-mouth screening; restorative, endodontic and periodontal treatments were performed as needed. For each patient, CBCT imaging was performed preoperatively (T0) and immediately after surgery (T1) underwent a cone beam computed tomography (CBCT) (Galileo system, Sirona® Germany). A preoperative CBCT T0 was taken to; identify the location of the sinus, the presence of any septum sinus, possible sinusitis, assess the alveolar-antral artery and accurately study the amount of bone available. Moreover, the bite height was registered to standardize all measurements. A second CBCT T1 was taken immediately after surgery and the third CBCT T2 was taken twelve months later (T2). Radiographic measurements of bone height and width were obtained at each stage.
2.4. Surgical Procedure
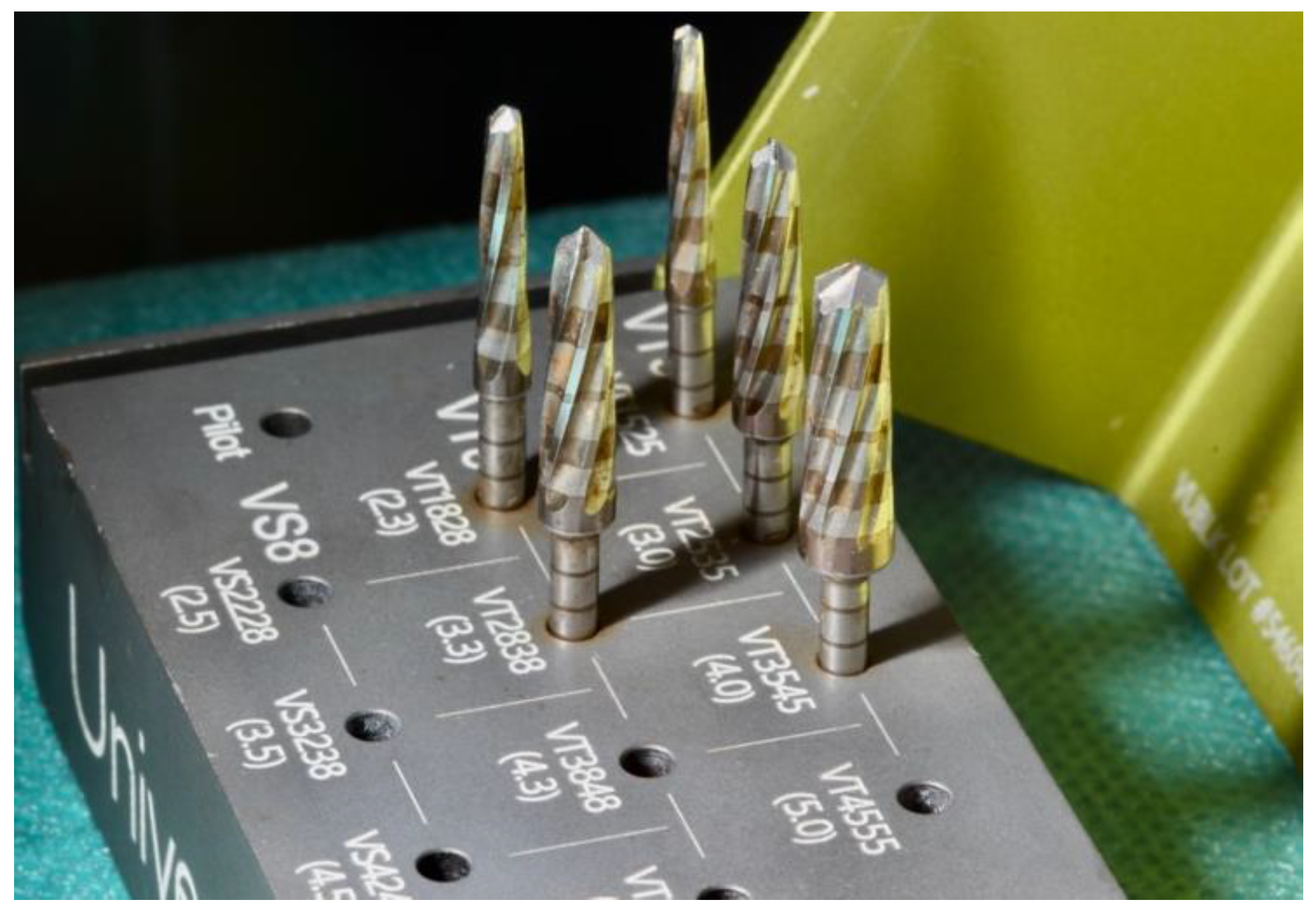
Surgical procedures were performed by second-year students of the Master of Oral Surgery and Implantology by five different clinicians, all of them with similar surgical experience, supervised by a professor expert in the OD and tSFE. After local anaesthesia (4% articaine with epinephrine 1:100.000), full-thickness flaps were reflected following a crestal incision and vertical releasing incisions if necessary. The preparation of the implant site/s was performed with Densah® burs by the Versah® system (
Figure 1), which allows the compaction of the bone by small increments and a smooth expansion of the osteotomy, alternating between VT5 and VT8 (
Figure 2) with abundant irrigation. Drills were rotated in a reversed, non-cutting direction allowing alveolar bone preservation and the increase in bone density.
Figure 1.
Densah® burs by the Versah® system.
Figure 1.
Densah® burs by the Versah® system.
Figure 2.
Decision tree for osseodensification protocol.
Figure 2.
Decision tree for osseodensification protocol.
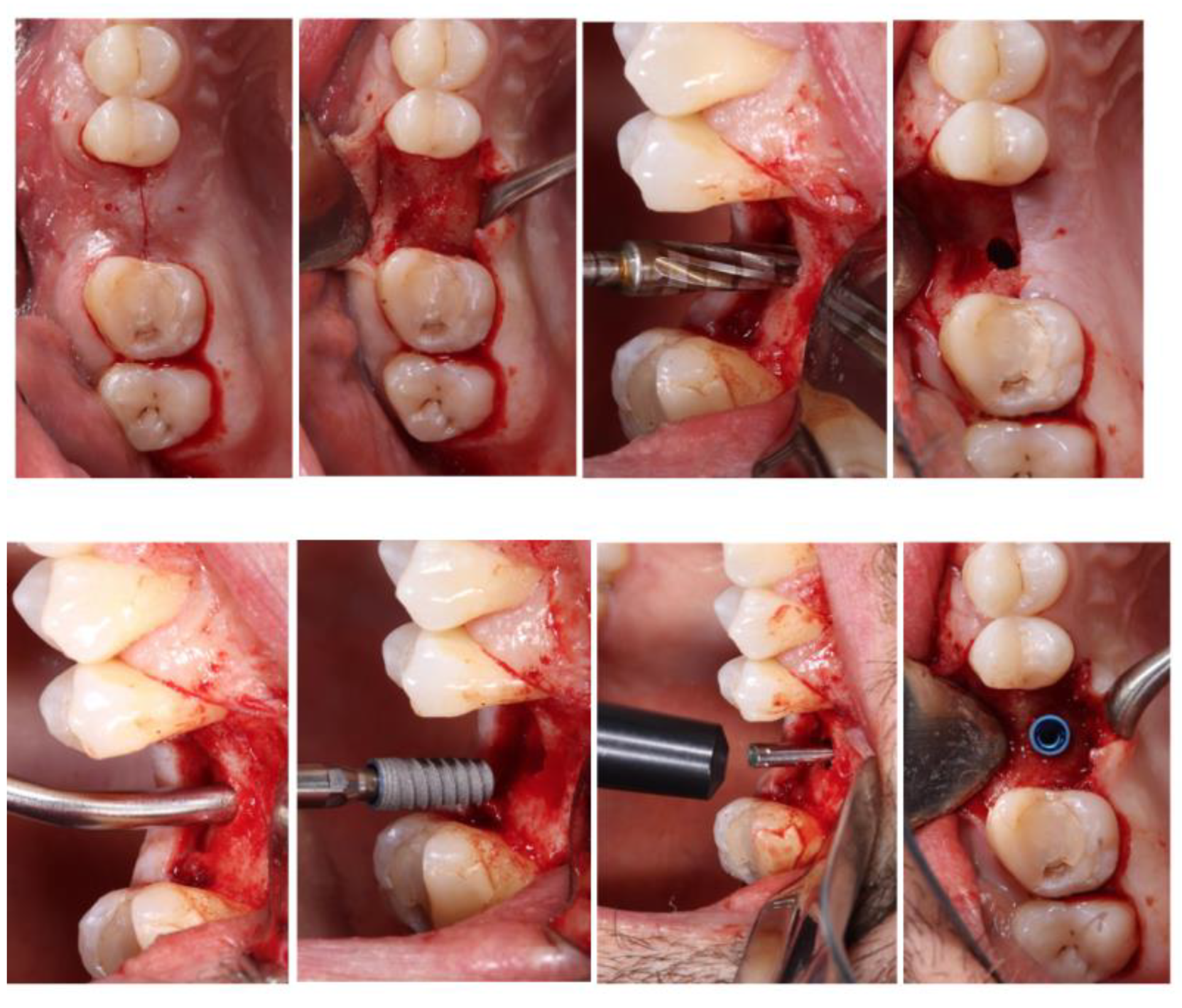
Figure 3.
Surgical procedure.
Figure 3.
Surgical procedure.
The implant site preparation was started with a pilot drill to perforate the cortical bone, and a second drill (2.0) was used to define the orientation of the implant, to the depth of 1-1.5 mm away from the sinus floor. The final diameter of the osteotomy preparation had an average diameter of between 0.5-0.7 mm less than the diameter of the implant. As grafting material, beta-tricalcium phosphate (ß-TCP) NovaBone® was applied in the alveolar bed in gel format and compacted by the last drill used to break the sinus floor, rotated in a reversed direction, at 50 rpm and without irrigation. While compacting, for each grafting injection the drilled was inserted 1-1.5 mm deeper. An attempt to standardize the quantity of graft material placed into the sinus was made using one of the package contents (i.e. about 0.25-0.50 cc). All the implants were submerged and covered with soft tissue. All implants were left submerged and primary closure of the wound was obtained.
2.5. Postoperative Care
All subjects received appropriate postoperative instructions and were prescribed Amoxicillin/Clavulanic Acid (875/125 mg for 7 days) or, if allergic to penicillin, azithromycin (500 mg for 3 days) as well as analgesics (Paracetamol 1g or Ibuprofen 400 mg every 6h if needed). The suture was removed after 15 days.
2.6. Data Collection
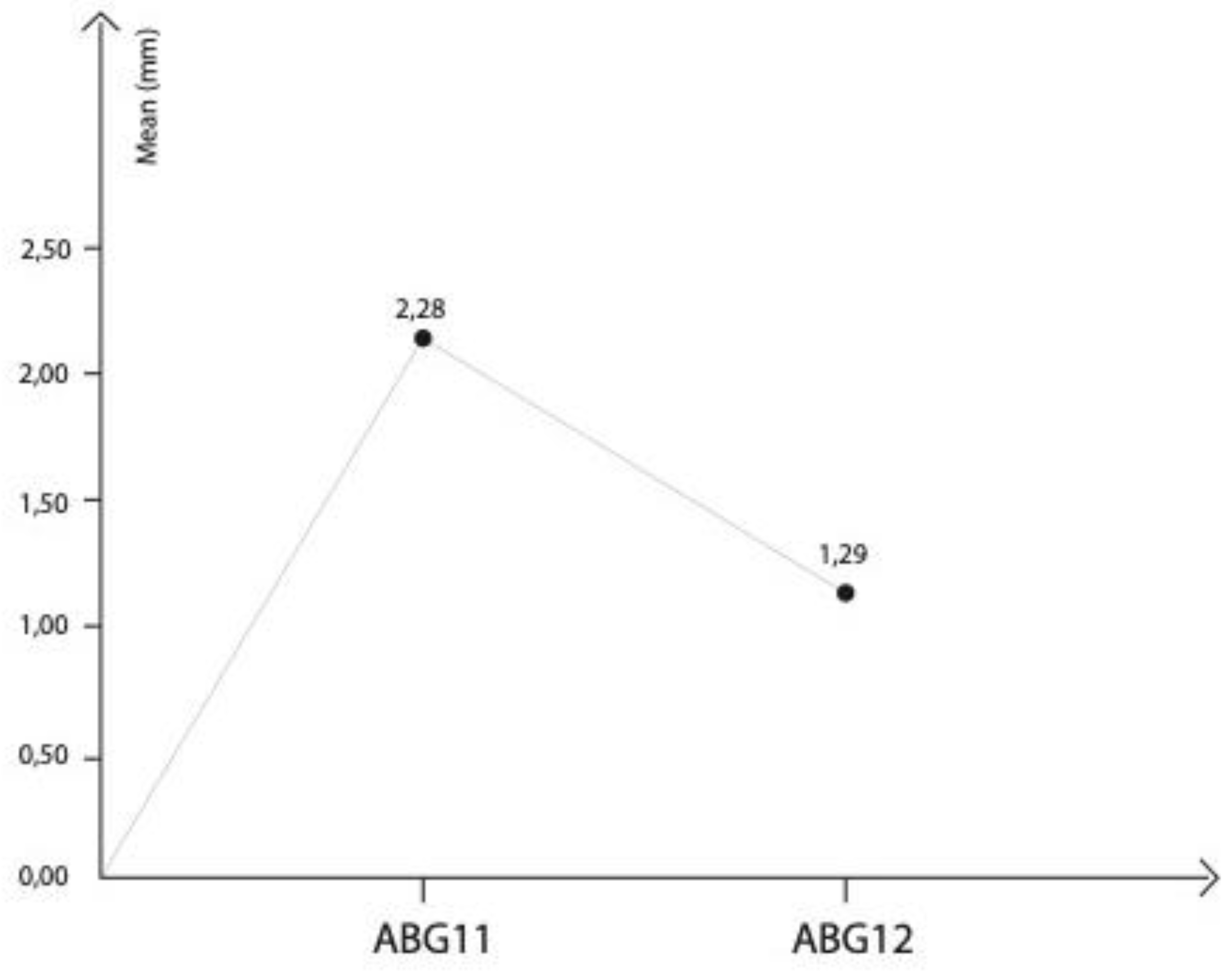
The following main variables (dependent variables) were registered: residual bone height (RBH); Apical bone gain (ABG); Residual bone width (RBW); Implant Insertion Torque (IT); Resonance Frequency Analysis (RFA). The analysis of secondary variables (independent variables) was fundamental for the evaluation of the efficacy of tSFE with OD and for determining the survival rate. Secondary variables such as age, sex, location of the implant, bone type and drilling protocol were also registered.
In the radiographic study, the following parameters were recorded: RBH: Residual bone/ available bone height, measured parallel to the implant axis, from the bone crest to the sinus floor; RBW: Residual bone width, measured in the vestibular-palatal direction; ABG: Apical bone gain. Distance from implant apex - most apical bone, measured along the axis of the implant. This value was considered as zero if the Schneiderian membrane was left in contact with the apex of the implant. All CBCT cross-sections were collected and analyzed by the same doctor and measurements were made by taking landmarks of the antagonist quadrant and adjacent structures (
Figure 4).
4. Discussion
The present study was performed to evaluate implant success and radiographic outcomes of bone height variations after tSFE performed with the OD technique [
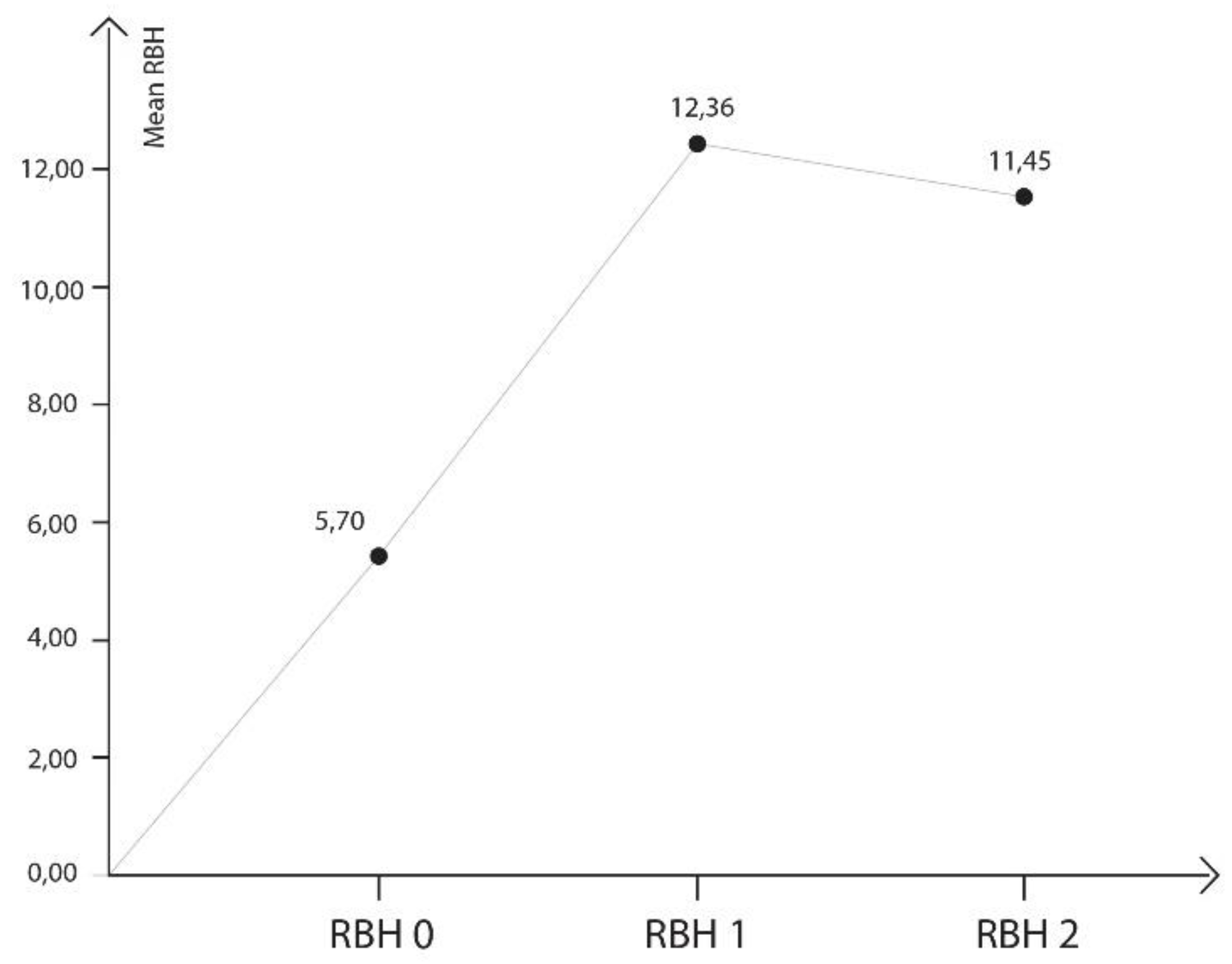
34] combined with β-TCP and simultaneous implant placement. Fourteen implants were placed in ten patients consecutively treated with tSFE using the OD technique. Radiograph measurements were performed before surgery (T0), immediately after surgery (T1) and at 12 months (T2).
The results of the study indicated (i) a 92.86 % implant success rate after a follow-up period of twelve months, (ii) that the tSFE using OD technique combined with β-TCP resulted in substantial RBH immediately after surgery and at twelve months, (iii) a graft material contraction was observed after twelve months follow-up, (iv) no correlation was observed between the bone height of the different times of the study and the primary stability.
To rehabilitate the upper posterior maxilla, maxillary sinus floor elevation with lateral or transcrestal approach represent two surgical options to vertically enhance the available bone [
6,
36]. Both augmentation techniques are clinically effective in achieving a vertical increase in crest dimension and are associated with high implant survival rates [
7,
8]. The factors that influence implant osteointegration in the posterior maxilla are bone quality, residual bone height and the primary stability of the implants, all of them related [
37,
38]. According to Wallace et al. [
39], the residual bone height is a discriminating factor between the lateral or transcrestal approach, affirming that if a residual alveolar bone of 3 mm or less is present, a lateral approach must be performed. However, protocols have not established the limits in terms of sufficient bone height for the transcrestal approach [
34]. Scientific evidence has demonstrated highly predictable results with the transcrestal approach when the available bone height was ≥ 5 mm [
20,
22,
23,
24,
34]. Moreover, several clinical studies reported high implant survival rates with a residual bone height ≤ 4 mm [
19,
23,
25,
35,
40,
41] and even with a residual bone height of 3 mm [
26,
42,
43,
44]. Gonzalez et al. [
35] compared in a multicenter study sinus augmentation with a transcrestal approach in patients with a residual bone height ≤ 4 mm (group 1) versus those with > 4 mm (group 2) of residual bone height, achieving 100% success rate in group 1 (n=35) and 98.51 % success rate in group 2 (n=67) after a mean follow up of 29.7 months.
The present study has shown that the tSFE procedure with OD and β-TCP resulted in a considerable vertical bone enhancement at twelve months follow-up. The magnitude of these results paralleled previous studies on the same technique [
34]. They evaluated the effectiveness and predictability of transcrestal elevation using osseodensification drills on 222 patients and 261 implants, obtaining favourable clinical results after a mean follow-up period of 35 months. Their records were similar to those obtained in our results: the mean residual bone height was 5.4 mm, obtaining a gain of 7 mm; in our study, the mean bone height was 5.7 mm, and a mean gain of 6.65 mm was obtained immediately after surgery and 5.75 mm at twelve months. A considerable bone gain with similar outcomes was obtained in previous investigations, where burs (CAS KIT) were used for tSFE [
19,
22]. However, when comparing the outcomes, the differences in the method for assessing radiographic measurements could lead to bias.
From the analysis of the mentioned studies, it seems that despite different approaches for sinus floor elevation, studies are heterogeneous and there is a lack of consensus in terms of indications for the different techniques.
The transcrestal sinus lift is described with the use and without the use of graft material to increase the bone height. Both variations of the technique have been described with high success rates, obtaining moderate new bone gain. The graft's volume contraction rate reported in literature ranges from 20% to 50% for both autogenous bone and bone substitutes, such as demineralized freeze-dried bone allograft (DFDBA), mineralized freeze-dried bone allograft (FDBA), and xenografts. In more recent studies, resorbable bioceramics, made of a mixture of hydroxyapatite and beta-tricalcium phosphate, have gained popularity, demonstrating bioactivity and osteoconductive properties for vertical bone augmentation of the atrophied maxilla in different histological studies [
45,
46].
In the present study, beta-tricalcium-phosphate putty was used as an alternative for the autogenous bone graft in sinus floor augmentation. A multicenter trial was performed by Better et al. [
43] with a total of 23 sinus floor elevations with a transcrestal approach. Three different flowable grafting materials were used and included an allograft putty material, an allograft gel and an alloplast consisting of a mixture of hydroxyapatite and beta-tricalcium phosphate granules in a hydrophilic polymer solution. All procedures were completed successfully, without membrane perforations and no intraoperative or postoperative adverse events were observed. Stiller et al. [
47] evaluated the clinical and osteogenetic performance of β-TCP granules (TCP-G) and β-TCP putty (TCP-P) bone graft material after sinus floor augmentation, in a split-mouth design. Obtaining excellent bone regeneration and volume stability for both materials, however, TCP-P displayed better surgical handling properties, greater bone formation as well as significantly lower grafting volume reduction values.
Based on the available literature, β-TCP seems to be a promising graft material for sinus floor augmentation, and it may lead to new bone formation and substantial enhancement of bone height [
42,
48,
49]. Nevertheless, more randomized clinical trials, with long follow-up periods and more homogenous studies in terms of the different techniques for sinus floor augmentation, are necessary to assess its long-term behaviour.
Primary stability in a dental implant is an essential factor for successful osseointegration. Surgical procedures and bone quality are some of the most common factors affecting primary stability. Achieving high insertion torque is also critical for primary stability [
50]. This study investigated approaches to improve primary stability using an osseodensification technique, which was compared to the conventional under-drilling method used for low-density bones. They affirmed the OD technique improved stability in low-density bones (based on torque and RFA measurements), which could explain our study results. When using the osseodensification technique for transcrestal sinus lift, there was no statistical evidence for an association between primary stability and the bone height available at the different times of the study. Future studies, however, are needed to confirm this consideration. This relatively new concept with a universally compatible drill has been proposed to improve bone densification and transcrestal sinus lift. This procedure has also shown better osteotomy than conventional implant drills and it allows bone expansion in different bone densities [
51]. These hypotheses we confirmed by a literature review by Pai et al. [
52], where a total of 195 articles were collected and submitted to screening using inclusion and exclusion criteria. Other authors have evaluated the medium-term success of implants placed using transcrestal sinus lift with the under-drilling protocol and investigated the relationship between the bone height and primary stability [
53]. After 106 registered patients who received 253 implants, after 5 years of follow-up, no significant differences were found in the success rate of implants placed in RBH < 4 mm and those with higher bone height. Predictable results can be achieved by under-drilling, even in atrophic alveolar crests and low bone quality. Other studies have obtained the same conclusions and support our results [
54]. Overall, our findings seem to suggest that tSFE performed with OD in association with β-TCP is an efficient surgical technique to substantially enhance the amount of bone height for implant placement with adequate primary stability, less postoperative pain, and limited surgical complications.
In terms of the clinicians' experience, although they were instructed about the sequence of surgical instruments, had a supervisor and had been involved in research protocols on the tSFE procedure and OD [
34] it may therefore be hypothesized that there were potential differences in skills as well as level of experience. Nevertheless, no information from previous studies is currently available on the impact of the operator’s experience on the outcomes of the tSFE procedure using OD technique.