Preprint
Article
Knowledge, Practice, and Infection Status of Prisoners towards Dermatophytosis: A Study in Nepal
Altmetrics
Downloads
191
Views
106
Comments
0
Submitted:
17 March 2024
Posted:
19 March 2024
You are already at the latest version
Alerts
Abstract
Background: Dermatophytosis, commonly known as tinea, poses a significant public health concern worldwide, especially in environments with poor hygiene and overcrowding, such as prisons. Despite its prevalence and impact on quality of life, there is a lack of research on the knowledge and hygiene practices regarding dermatophytosis among prisoners, particularly in Nepal.
Objective: The study aimed to assess prisoners' knowledge, hygiene practice and infection status regarding dermatophytosis in Central Prison, Nepal.
Methods: A descriptive cross-sectional study with a sample size of 184 respondents was designed to collect data using a validated pre-tested questionnaire from September 2023 to January 2024. The collected data was then analysed using IBM SPSS version 21. Knowledge and hygiene practices were measured on an eight and 11-point scale and rated as poor (≤4) and sound (>4), bad (≤6), and good (>6), respectively. Summary data were presented by descriptive, while Chi-square and logistic regression were used for inferential statistics at P < 0.05.
Results: The findings revealed moderate knowledge among prisoners regarding dermatophytosis, with significant gaps in understanding its spread and prevention. While most prisoners recognised the importance of treatment, there were misconceptions about the inevitability of contracting dermatophytosis and the role of personal hygiene.
Conclusions: Despite good knowledge levels, adherence to recommended hygiene practices was suboptimal, highlighting the need for targeted interventions. The study underscores the importance of addressing knowledge gaps, changing attitudes, and promoting hygienic practices to mitigate the burden of dermatophytosis among prisoners.
Keywords:
Subject: Medicine and Pharmacology - Other
Introduction
Dermatophytosis, also called “tinea”, is a contagious disease caused by a fungus called dermatophytes. Dermatophytes cause superficial and self-limiting infections that can be disfiguring and uncomfortable. Contact with spores, along with skin injury, high temperature, and humidity, increases the susceptibility to infection [1]. Most clinical manifestations include blistering, fissures, scales, or spots [2]. As dermatophytes thrive in warm and moist environments, the burden of some fungal diseases is more significant in regions with crowded living conditions and poor hygiene [3]. Studies have uncovered several themes, including a lack of knowledge of the disease, comprehension of its risk factors, prevention, the significance of traditional and personal beliefs, and care-seeking behaviour regarding dermatophytosis [4].
Prisons in developing countries have poor living conditions, lack of personal hygiene, sharing of personal items, and overcrowding, due to which skin diseases are pretty common among inmates [5,6]. In the prisons of Nepal, there is overcrowding, lack of primary care, and inadequate health care [7]. A study regarding the pattern of skin diseases in prisoners has been done in Nepal, and it shows that skin infections are the most common dermatological problem [6]. In the same study, the prevalence of skin problems was 27.23%. There are no skin infection prevention programs targeted towards prisoners in Nepal. In a similar study in India, despite the participants demonstrating good knowledge about the mode of spread of dermatophytosis, most of the participants still failed to implement the knowledge in maintaining personal hygiene practices [8].
Dermatophytosis patients experience psychosocial stress and challenges. A study showed significant impairment of quality of life in dermatophytosis patients, where most reported symptoms of itching, embarrassment, and self-consciousness [10]. According to a study in India, there is an urgent need to dispel myths or conventional views not backed by facts. The attitude of patients towards dermatophytosis plays a significant role in their willingness to seek medical help and adhere to prescribed treatments [4]. The study assesses prisoners’ knowledge and hygiene practices towards dermatophytosis in Central Prison, Nepal.
Methods
Using structured questionnaires, a descriptive cross-sectional study was carried out between September 2023 and January 2024 among 184 Central Prison, Nepal prisoners. Simple random sampling was used to select the participants, and the sample size was determined using Cochran’s formula:
n = Z2* p*q/e2
Where, n = sample size
Z = Level of confidence, at α= 0.05, Z=1.96 for 95% CI
p = prevalence of dermatophytosis from a previous similar study, 7.78% [5].
q = 1 - p = 1 - 0.078= 0.922
e = margin of error, 5%
Substituting, n = 111
Taking a 10% non-response rate, the final sample size was 122.
Sampling
The study purposely selected Central Prison, Nepal. The list of prisoners was obtained from the administrative record, and the required number of participants was obtained using a random number table.
Inclusion and Exclusion Criteria
The study focused on a vulnerable and high-risk population, with participation limited to prisoners who provided written consent. Research assistants also engaged with prison inmates in their dormitories to ensure respondent confidentiality. However, the study did not include individuals who were severely ill or on assignment outside the prison during the survey period.
Data Collection and Study Variables
The pre-tested standardised questionnaire used in this study consisted of three sections, filled out by the interviewer by interviewing participants:
Section A: Socio-demographic characteristics such as age, gender, level of education, marital status were included
Section B: This section included eight items on source of information, knowledge on transmission, signs and symptoms, and prevention of dermatophyte infection. Eight questions had “Yes” or “No” answers. Knowledge scores were further categorised into two categories: good knowledge and poor knowledge.
Section C: An 11-item question on general hygiene practice focusing on the general hand-washing and showering practices, undergarments drying, nail trimming, frequency of washing towels and other practices such as sharing hair-brush and clothes. They were evaluated based on responses “Yes” (given as one mark) and “No” (given as zero marks). A cut-off point using its mean value was used to categorise the scores into excellent and poor hygiene practices.
Infection Status: It was assessed based on previous diagnosis.
Data Analysis
Analysis was conducted using IBM Statistical Package for Social Sciences (SPSS) version 21.0 for Windows. Continuous variables were summarised using means and standard deviations, while categorical data were presented as proportions and percentages in summary tables and charts. The relationship between socio-demographic characteristics and relevant variables was assessed using Chi-square (χ²) and logistic regression statistics. Respondents’ knowledge of dermatophytosis was assessed on an 8-point scale, categorised as poor (≤4) or good (>4). Similarly, hygiene practices were scored on an 11-point scale and categorised as poor (≤6) or good (>6). At the same time, infection status was assessed by asking about the previous diagnosis. A p-value of less than 0.05 was considered statistically significant.
Results
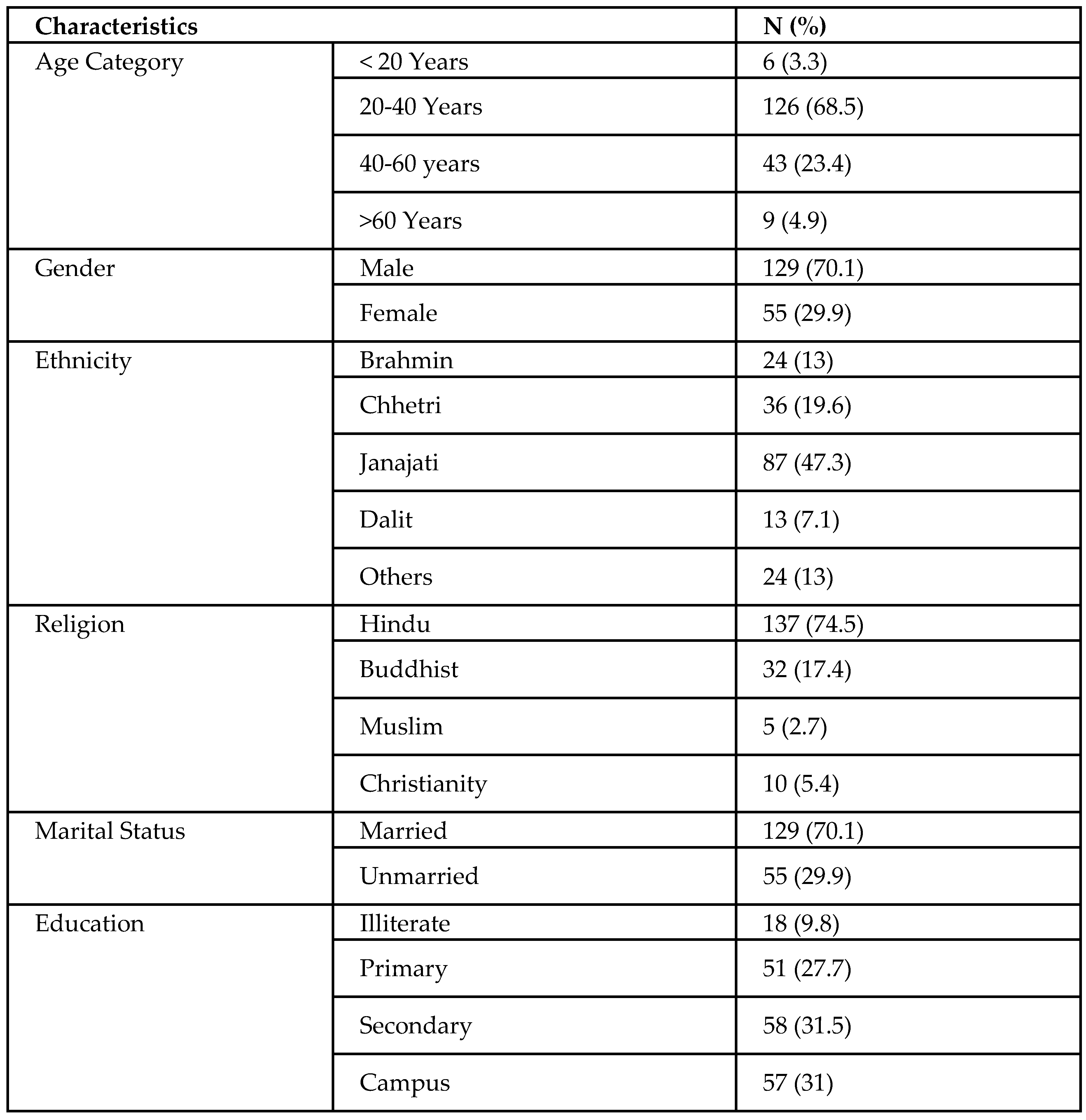
Sociodemographic Characteristics
The mean age of respondents was 35.70 years, ranging between 19 and 77. The percentage of male respondents was 70.1%, whereas 29.9% were female. In addition, more than ⅔ of respondents (70.1%) were married, and 61.5% had education equivalent to secondary level and above.
Table 1.
Socio-demographic characteristics of the study population.
 |
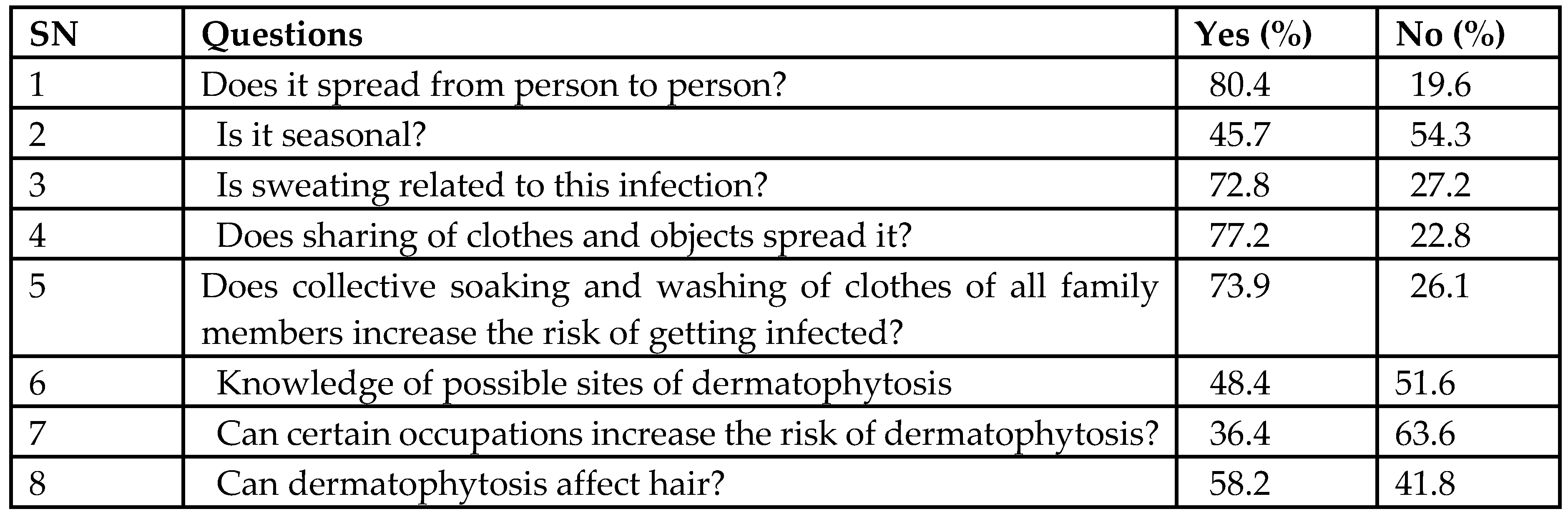
Knowledge Regarding Dermatophytosis
Assessment of prisoners’ knowledge regarding the spread of fungal infection from person to person showed that the majority (80.4%) of participants responded correctly. The study also revealed that 72.8% of prisoners reported correctly that sweating is related to infection with dermatophytosis. One-third of respondents had good knowledge regarding the spread of dermatophytosis due to collectively sharing clothes and washing. Around half of the respondents had good knowledge of the seasonal nature and possible sites of dermatophytosis infection. 63.6% of respondents did not have correct knowledge regarding occupation-related dermatophyte infection.
Table 2.
Respondents’ knowledge of dermatophytosis.
 |
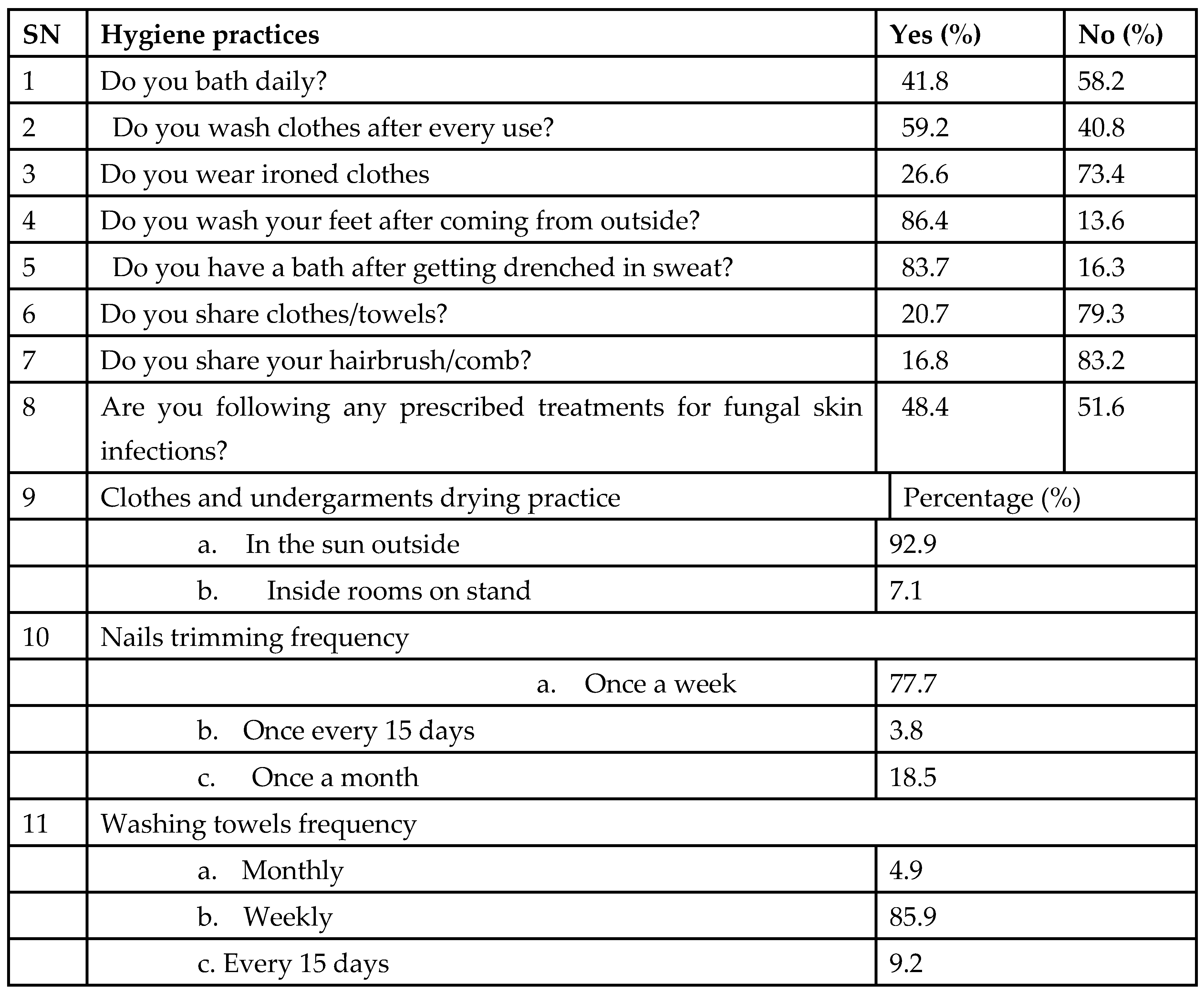
Dermatophytosis-Related Personal Hygiene Practices
About 41.8% of respondents stated that they bathed daily, 59.2% reported washing clothes after every use, and 26.6% of respondents stated that they wore ironed clothes. Most of them habitually washed their feet after coming from outside (86.4%) and bathed after getting drenched in sweat (83.7%). One-fifth of respondents shared their clothes/towels or comb. Most respondents (77.7%) reported trimming their nails weekly. A considerable proportion of the respondents (92.9%) revealed drying clothes in the sun outside. Only 7.1% reported drying clothes inside rooms. Most of them (85.9%) reported washing towels weekly.
Table 3.
Dermatophytosis-related hygiene practices.
 |
Comparison of Sociodemographic Variables and Knowledge Category
The study explored the relationship between demographic factors and knowledge levels about skin diseases, revealing several significant associations. Notably, the gender exhibited a significant association (p = 0.001), with females showing higher susceptibility than males. Furthermore, religion was significantly associated with skin disease status (p = 0.013), indicating that individuals belonging to the Hindu faith had a higher prevalence of skin diseases. Smoking status also showed a significant association (p = 0.022), with smokers exhibiting a higher risk. However, no significant associations were found between knowledge status and ethnicity, marital status, education and comorbidities category, with individuals aged 20-40 showing higher susceptibility. Gender also exhibited a notable association (p < 0.001), with females being more prone to skin diseases (B coefficient = 2.954, 95% CI [7.065, 52.134], p = 0.001). Moreover, the knowledge category demonstrated significance (p = 0.004), indicating that individuals with poor knowledge were at a higher risk (B coefficient = -1.286, 95% CI [0.115, 0.662], p = 0.004). Practice category also played a role (p = 0.009), with poor hygiene practices correlating with increased susceptibility (B coefficient = -1.171, 95% CI [0.129,0.746], p = 0.009). However, no significant associations were found between skin disease status, ethnicity, and religion.
Table 4.
Comparison of socio-demographic variables and knowledge on dermatophytosis.
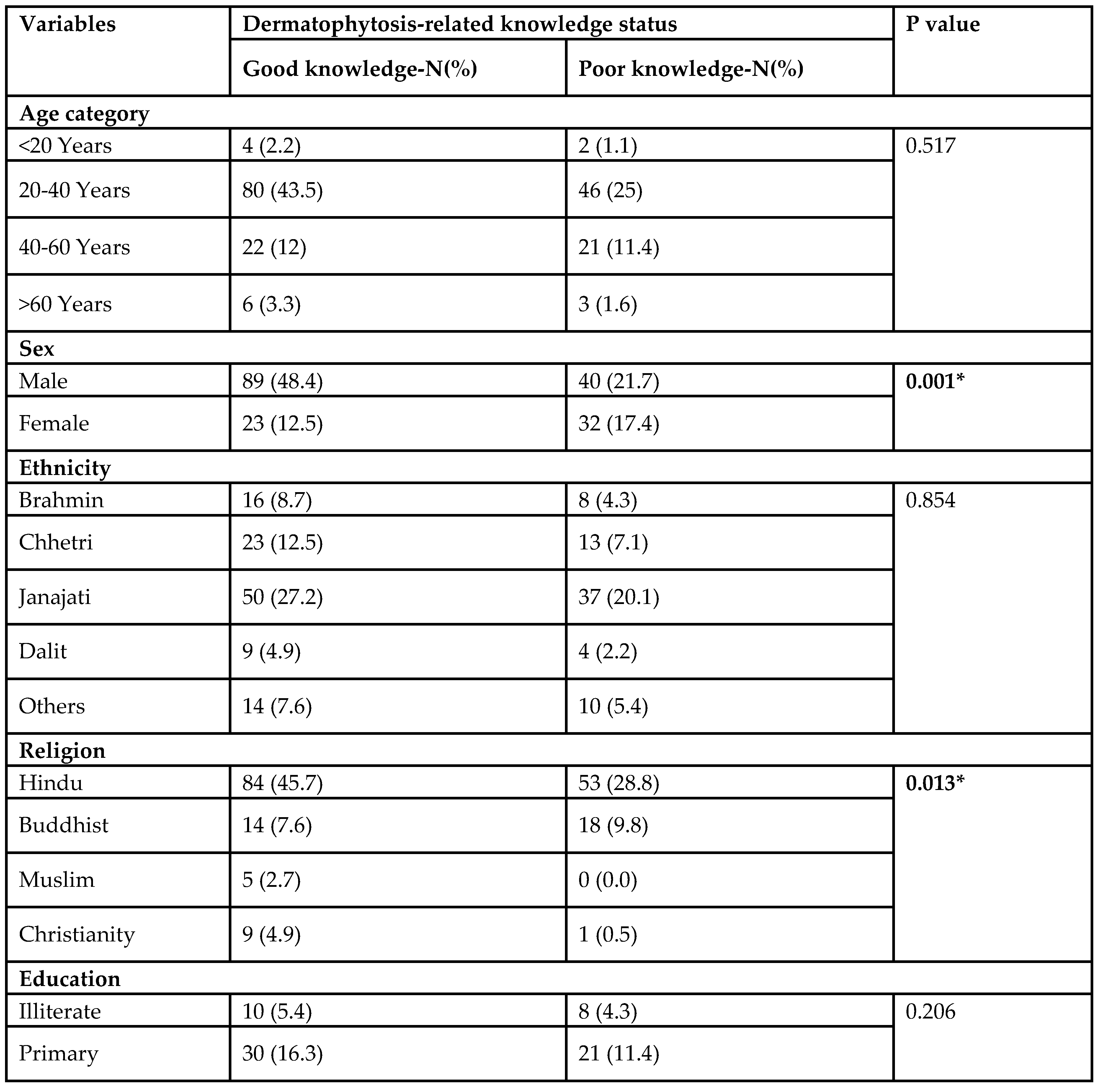 |
Table 5.
Comparison of socio-demographic variables and infection status.
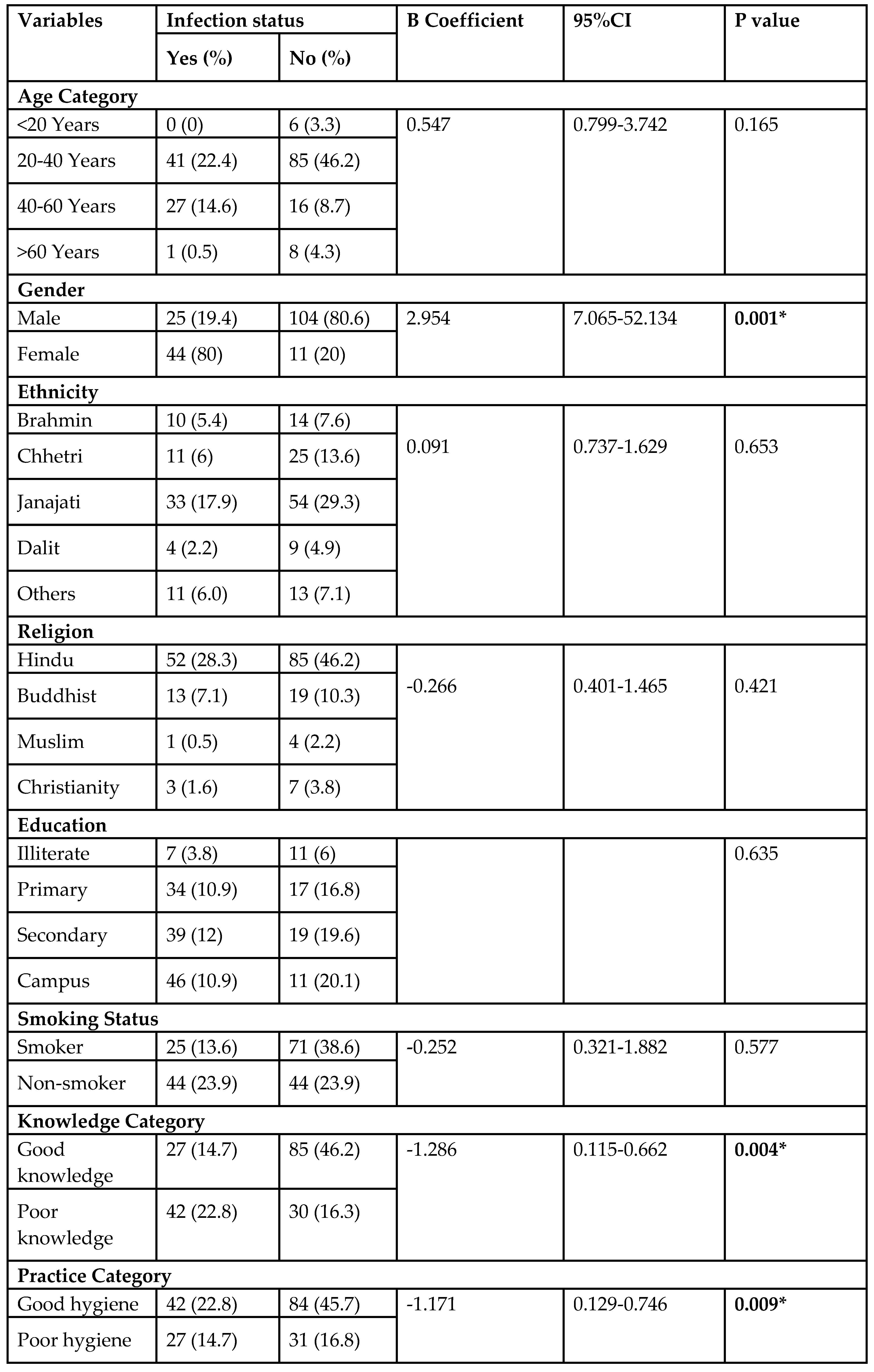 |
Discussion
The study’s findings provide valuable insights into the knowledge, infection status and hygiene practice on dermatophytosis among prisoners. The mean age of respondents was 35, which is close to that reported by Okareh et al. [15]. Younger individuals (20-40 years) demonstrated higher susceptibility to skin diseases, which could be attributed to lifestyle factors and increased exposure. The findings are from the study conducted by SK et al. and Paudel et al. [8,16]. We also report that our study had more female cases (80%) of dermatophytosis than male cases (20%). It is noted in similar studies conducted by SK et al. and Pires et al. [2,8] but not in other studies [16,17,18,19]. Individuals belonging to the Hindu faith showed a higher prevalence of skin diseases, highlighting the potential influence of cultural and religious practices on disease susceptibility. Smoking status was also found to be a significant factor, with smokers being at a higher risk, which could be attributed to the immunosuppressive effects of smoking.
Overall, the study revealed that a significant proportion of respondents (60.9%) had good knowledge regarding the spread and prevention of dermatophytosis, with the majority correctly identifying the mode of transmission and the importance of personal hygiene practices. This could be explained by 62.5% of the respondents having education up to a secondary level or more. 80% of participants knew about the spread of fungal infection from person to person, and 95% of respondents believed that treatment is necessary for dermatophytosis. It is coherent with Yamu et al. but not consistent with SK et al. 45 % had good knowledge of the seasonal nature of dermatophytosis, similar to SK et al., but differs from Yamu et al. [8,20]. However, there were also areas where knowledge gaps were evident, particularly regarding occupation-related dermatophyte infections.
The study also highlighted the importance of hygiene practices in preventing dermatophytosis. Practices such as daily bathing, washing clothes after every use, and avoiding sharing clothes/towels were associated with better knowledge levels and lower susceptibility to skin diseases. 68.5% of respondents had good hygiene practices, which might indicate satisfactory hygiene services in the prison settings. The percentage of respondents bathing daily is less than that of Yamu et al. and SK et al. It can be explained by the winter season at the time of data collection. 92.9% of respondents dried clothes in the sun, similar to Yamu et al. and SK et al. [8,20]. However, a significant proportion of respondents reported suboptimal hygiene practices, indicating the need for targeted interventions to promote better hygiene practices among this population.
Limitations
Due to the cross-sectional study design, causal inference cannot be established regarding any observed association between dependent and independent variables. The findings are also limited in generalizability to the broader population because the study was conducted on prisoners in a specific setting.
Conclusions
In conclusion, this study gives us valuable information about Nepal’s Central Prison prisoners’ dermatophytosis-related knowledge and hygiene habits. It emphasises how a person’s age, gender, degree of awareness, and cleanliness habits significantly impact their susceptibility to dermatophytosis. Specifically, males and individuals aged 20-40 years were identified as more prone to skin diseases. Moreover, poor knowledge and hygiene practices were linked to an increased dermatophytosis risk. Keeping these facts in view, it highlights the critical need for comprehensive strategies for preventing and managing dermatophytosis.
Recommendations
Based on our research findings, we suggest special educational programs on dermatophytosis prevention and treatment for prisoners in Central Prison. These programs should primarily address myths, promote hygienic practices, and encourage positive attitudes towards dermatophytosis management. In addition, routine screenings and timely medical care should be offered to prevent the disease from spreading inside the prison setting.
Funding
Universidad Continental covers the APC of this publication.
Ethical Approval
The study was approved by the Nepal Health Research Council (NHRC)’s ethical review board.
Conflict of Interest
There are no conflicts of interest.
References
- Marsella, R. Dermatophytosis. Equine Infect Dis Second Ed. 2013, 1–13. [Google Scholar]
- Pires, C.A.A.; da Cruz, N.F.S.; Lobato, A.M.; de Sousa, P.O.; Carneiro, F.R.O.; Mendes, A.M.D. Clinical, epidemiological, and therapeutic profile of dermatophytosis. An Bras Dermatol. 2014, 89, 259–64. [Google Scholar] [CrossRef] [PubMed]
- Urban, K.; Chu, S.; Scheufele, C.; Giesey, R.L.; Mehrmal, S.; Uppal, P.; et al. The global, regional, and national burden of fungal skin diseases in 195 countries and territories: A cross-sectional analysis from the Global Burden of Disease Study 2017. JAAD Int [Internet]. 2021, 2, 22–7. [Google Scholar] [CrossRef]
- An, I.; Harman, M.; Ibiloglu, I. Topical Ciclopirox Olamine 1%: Revisiting a Unique Antifungal. Indian Dermatol Online J. 2017, 10, 481–5. [Google Scholar]
- Parajuli, N.; Jonkman, M. Skin Diseases in a NEPALI Prison. Vol. 4, Journal of Chitwan Medical College. 2014. Available from: www.jcmc.cmc.edu.
- Ameen, M. Epidemiology of superficial fungal infections. Clin Dermatol. 2010, 28, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Joanne, M.D.; Hundi, G. Awareness of Risk Factors for Dermatophytoses and its impact on Quality of Life among adults in Mangalore. A Cross-sectional study. IOSR J Dent Med Sci e-ISSN [Internet]. 2018, 17, 64–70. [Google Scholar]
- S. SS, S. AK, N. AK, G. S. Study on knowledge, attitude and behaviour of patient towards dermatophytosis and importance of maintaining personal hygiene. Int J Adv Med. 2021, 8, 1560. [Google Scholar] [CrossRef]
- Joy Dhirendranath Das, Vijay Zawar, Manoj Pawar, Shrikant Kumavat, Jaya Bharati. Study of Skin Diseases in Incumbent Prison Inmates. MVP J Med Sci. 2020, 277–81. [Google Scholar]
- Ramamuthie, G.; Verma, R.K.; Appalasamy, J.; Barua, A. Awareness of risk factors for skin infections and its impact on quality of life among adults in a Malaysian City: A cross-sectional study. Trop J Pharm Res. 2015, 14, 1913–7. [Google Scholar] [CrossRef]
- Jain, S.; Kabi, S.; Swain, B. Current Trends of Dermatophytosis in Eastern Odisha. J Lab Physicians. 2020, 12, 10–4. [Google Scholar] [CrossRef]
- Mohammed, S.; Al-Jaff, B. Prevalence of dermatophytosis among Suse federal prison inmates using conventional identification methods and PCR-RFLP typing. J Zankoy Sulaimani - Part A. 2020, 22, 273–86. [Google Scholar] [CrossRef]
- Walker, S.L.; Shah, M.; Hubbard, V.G.; Pradhan, H.M.; Ghimire, M. Skin disease is common in rural Nepal: results of a point prevalence study. British Journal of Dermatology 2008, 158, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Oninla, Olumayowa A; Olasode, Olayinka A; Onayemi, Olaniyi; Ajani, Atinuke A, The Prevalence and Pattern of Skin Disorders at a University Teaching Hospital in Ile-Ife and Ilesha, Nigeria, Clinical Medicine Insights. 2014; 7.
- Okareh, O.; Okiche, C.; Aluko, O.; Omotade, O. Sanitary conditions and inmates’ knowledge and attitude towards hygiene practices in a maximum-security prison in Oyo State, Southwest Nigeria. Niger J Health Sci. 2018, 18, 15. [Google Scholar]
- Paudel, D.; Manandhar, S. Dermatophytic Infections among the Patients Attending Di Skin Hospital and Research Center at Maharajgunj Kathmandu. J Nepal Health Res Counc. 2015, 13, 226–32. [Google Scholar] [PubMed]
- Gebreeyessus, G.D.; Adem, D.B. Knowledge, Attitude, and Practice on Hygiene and Morbidity Status among Tertiary Students: The Case of Kotebe Metropolitan University, Addis Ababa, Ethiopia. J Environ Public Health. 2018, 2018, e2094621. [Google Scholar] [CrossRef] [PubMed]
- Boualem-Belmiloud, Hayati-Kadir-Shahar, Hejar-Abdulrahman. Determinants of Risk Factors On Dermatophytes Infections on Patients’ Knowledge, Attitude and Hygiene Practice Among Patients Attending Dermatology Department in A Government Hospital in Setif Province, Algeria. Malays J Med Health Sci. 2022, 206–13.
- Dsouza, M.J.; Kamath Hundi, G. Awareness of Risk Factors for Dermatophytoses and its impact on Quality of Life among adults in Mangalore. A cross-sectional study. IOSR J Dent Med Sci. 2018, 17, 64–70. [Google Scholar]
- Yamu, S.; Choudhary, D.; Aryal, S. Knowledge Attitude And Practice Regarding Superficial Fungal Infections In Dermatology Patients In Eastern Nepal. Birat J Health Sci. 2023, 8, 2096–101. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated