Submitted:
19 March 2024
Posted:
21 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Site and Period
2.2. PALCOM Scale of the Complexity of Palliative Care Needs
2.3. Study Objectives
2.4. Inclusion Criteria
2.5. Main Outcome Variables
2.6. Descriptive Variables
2.7. Statistical Method
3. Results
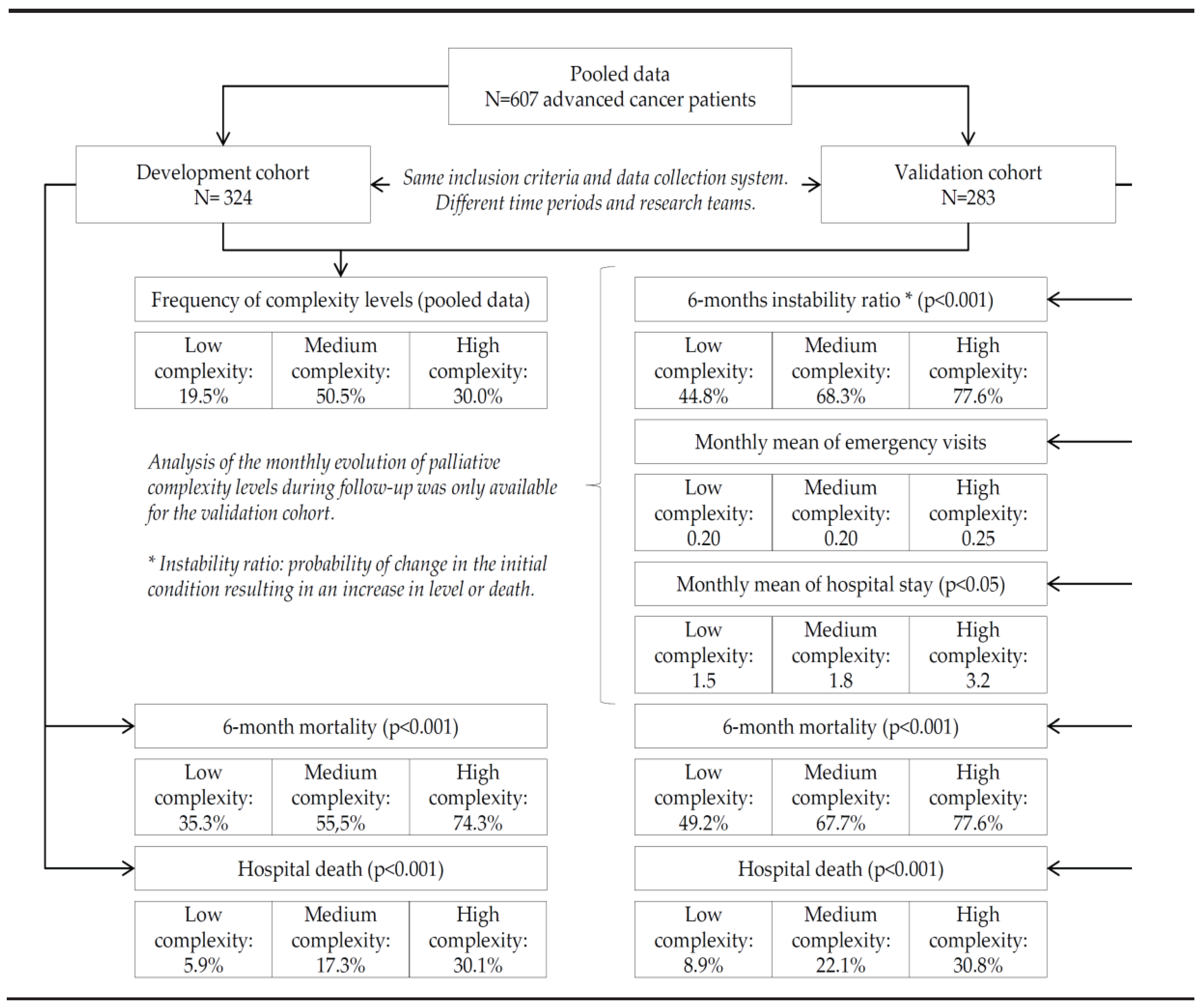
3.1. Pooled Analysis of the Two Cohorts
3.2. Evolutionary Behaviour of the Levels of Complexity (Table 4)
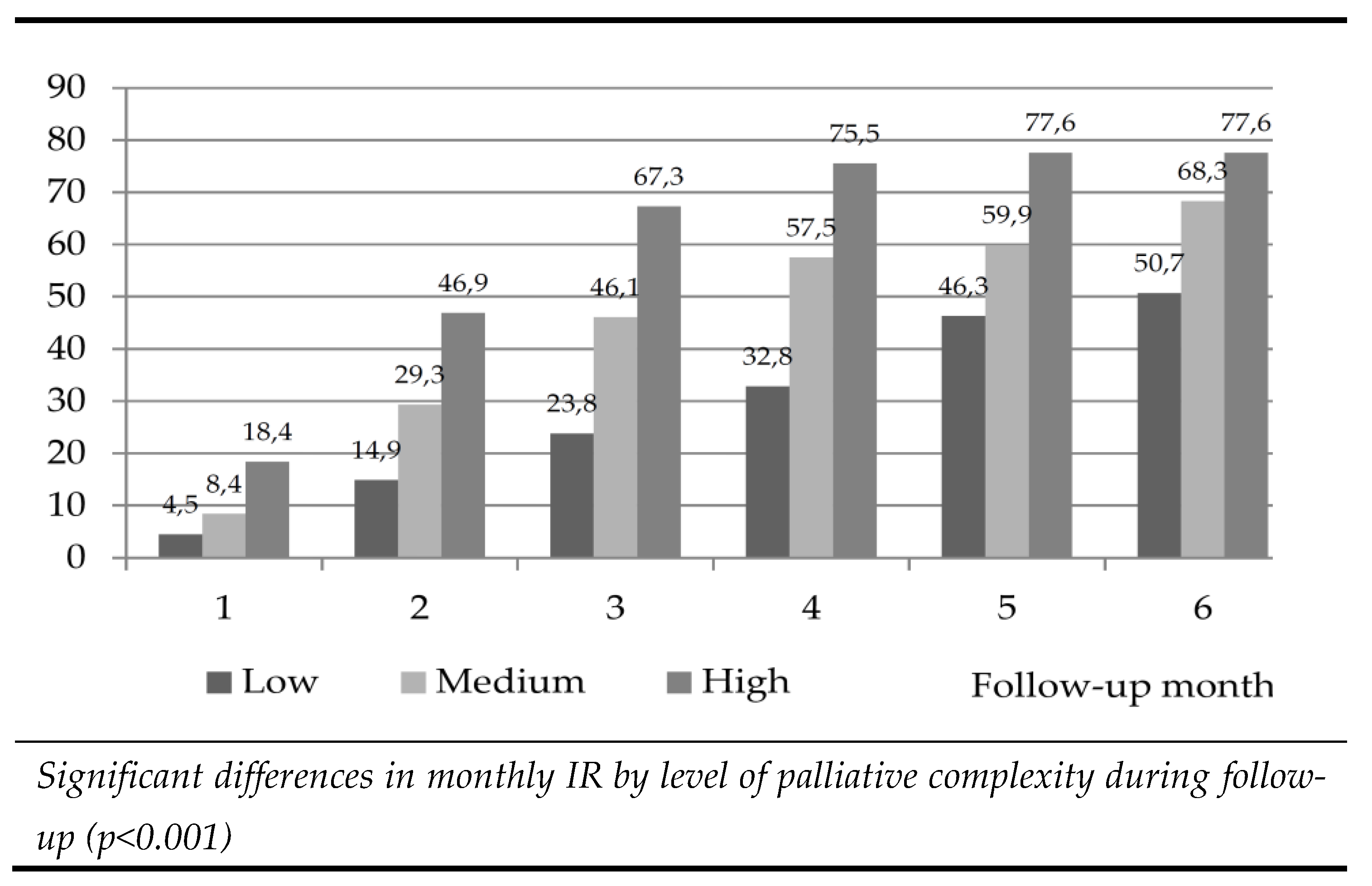
3.2.1. Instability Ratio (IR) According to the Level of PALCOM Complexity
3.2.2. Indicators of Resource Consumption According to the PALCOM Level of Complexity
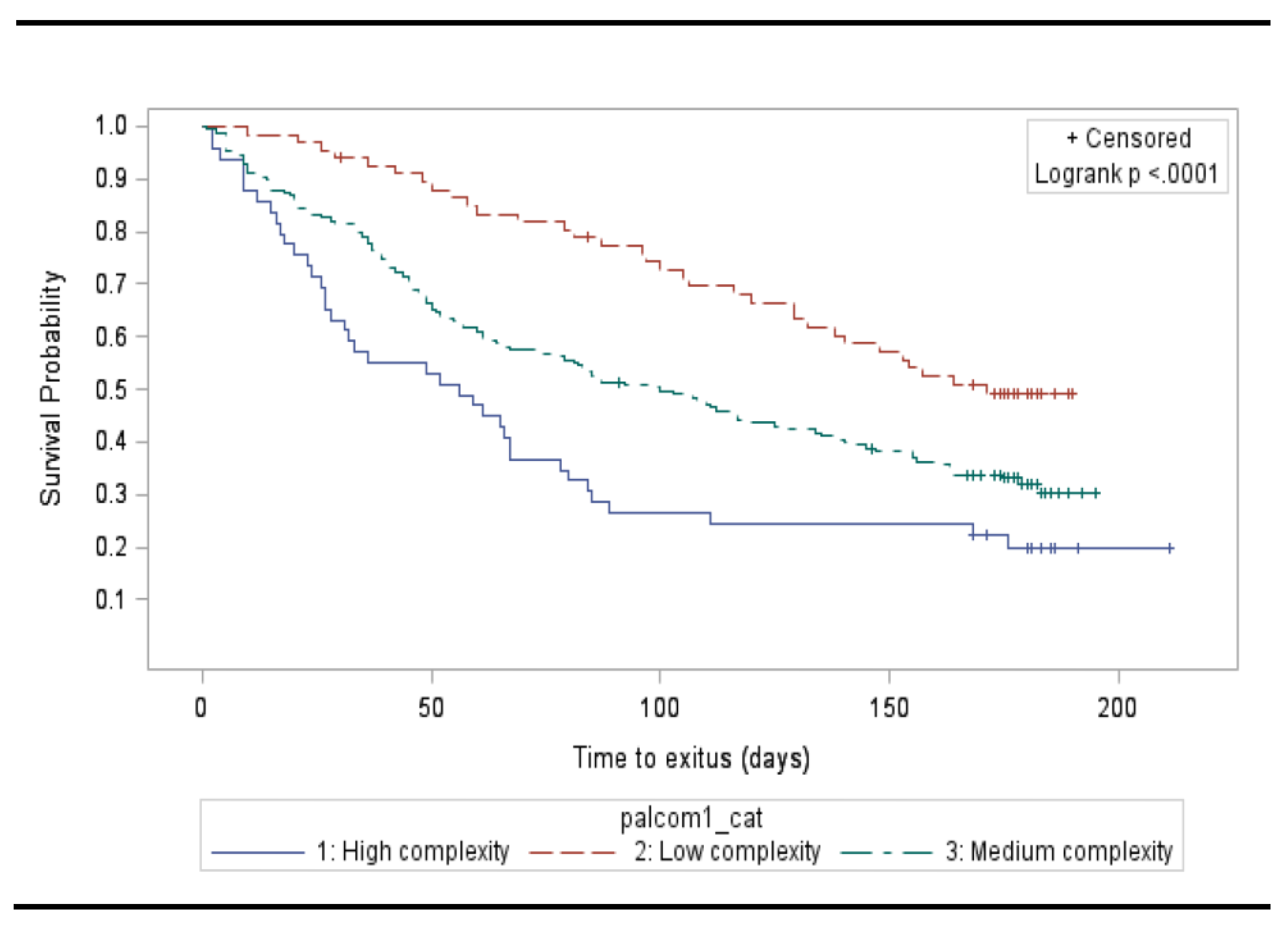
3.2.3. Survival According to the PALCOM Level of Complexity
3.3. Profiles of PALCOM Complexity
3.3.1. Profile of Low Complexity
3.3.2. Profile of Medium Complexity
3.3.3. Profile of High Complexity
4. Discussion
Study Limitations
5. Conclusions
5.1. Practical Implications
5.2. Implications for Investigation
References
- World Health Organization (WHO): Palliative Care. Accessible on Internet: https://www.who.int/ news-room/fact-sheets/detail/palliativecare (2020). Accessed January 07 2023. 07 January.
- World Health Organization. Strengthening of Palliative Care as a Component of Integrated Treatment throughout the Life Course. J. Pain Palliat. Care Pharmacother. 2014, 28, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Lakhani, S.; Scalzitti, D.A.; Padrone, L.; Martins-Welch, D. From evidence to practice: Early integration of palliative care in a comprehensive cancer center. Support Care Cancer. 2022, 31, 17. [Google Scholar] [CrossRef] [PubMed]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl,W. F.; et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Bakitas, M.A.; Tosteson, T.D.; Li, Z.; Lyons, K.D.; Hull, J.G.; Li, Z.; Dionne-Odom, J.N.; Frost, J.; Dragnev, K.H.; Hegel, M.T.; et al. Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III randomized controlled trial. J. Clin. Oncol. 2015, 33, 1438–1445. [Google Scholar] [CrossRef] [PubMed]
- Chochinov, H.M.; Kristjanson, L.J.; Breitbart, W.; McClement, S.; Hack, T.F.; Hassard, T.; Harlos, M. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: A randomised controlled trial. Lancet Oncol. 2011, 12, 753–762. [Google Scholar] [CrossRef]
- Dionne-Odom, J.N.; Azuero, A.; Lyons, K.D.; Hull, J.G.; Tosteson, T.; Li, Z.; Li, Z.; Frost, J.; Dragnev, K.H.; Akyar, I.; et al. Benefits of Early Versus Delayed Palliative Care to Informal Family Caregivers of Patients with Advanced Cancer: Outcomes from the ENABLE III Randomized Controlled Trial. J. Clin. Oncol. 2015, 33, 1446–1452. [Google Scholar] [CrossRef] [PubMed]
- Dyar, S.; Lesperance, M.; Shannon, R.; Sloan, J.; Colon-Otero, G. A nurse practitioner directed intervention improves the quality of life of patients with metastatic cancer: Results of a randomized pilot study. J. Palliat. Med. 2012, 15, 890–895. [Google Scholar] [CrossRef] [PubMed]
- Higginson, I.J.; Bausewein, C.; Reilly, C.C.; Gao, W.; Gysels, M.; Dzingina, M.; McCrone, P.; Booth, S.; Jolley, C.J.; Moxham, J. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: A randomised controlled trial. Lancet Respir. Med. 2014, 2, 979–987. [Google Scholar] [CrossRef]
- Grudzen, C.R.; Richardson, L.D.; Johnson, P.N.; Hu, M.; Wang, B.; Ortiz, J.M.; Kistler, E.A.; Chen, A.; Morrison, R.S. Emergency Department-Initiated Palliative Care in Advanced Cancer: A Randomized Clinical Trial. JAMA Oncol. 2016, 2, 591–598. [Google Scholar] [CrossRef]
- Hudson, P.; Trauer, T.; Kelly, B.; O’Connor, M.; Thomas, K.; Summers, M.; Zordan, R.; White, V. Reducing the psychological distress of family caregivers of home-based palliative care patients: Short-term effects from a randomised controlled trial. Psychooncology 2013, 22, 1987–1993. [Google Scholar] [CrossRef]
- Uitdehaag, M.J.; van Putten, P.G.; van Eijck, C.H.; Verschuur, E.M.; van der Gaast, A.; Pek, C.J.; van der Rijt, C.C.; de Man, R.A.; Steyerberg, E.W.; Laheij, R.J.; et al. Nurse-led follow-up at home vs. conventional medical outpatient clinic follow-up in patients with incurable upper gastrointestinal cancer: A randomized study. J. Pain Symptom Manag. 2014, 47, 518–530. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, C.; Swami, N.; Krzyzanowska,M. ; Hannon, B.; Leighl, N.; Oza, A.;Moore,M.; Rydall, A.; Rodin, G.; Tannock, I.; et al. Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. Lancet 2014, 383, 1721–1730. [Google Scholar] [CrossRef]
- Ferrell, B.; Sun, V.; Hurria, A.; Cristea, M.; Raz, D.J.; Kim, J.Y.; Reckamp, K.; Williams, A.C.; Borneman, T.; Uman, G.; et al. Interdisciplinary Palliative Care for Patients with Lung Cancer. J. Pain Symptom Manag. 2015, 50, 758–767. [Google Scholar] [CrossRef] [PubMed]
- Greer, J.A.; Pirl,W. F.; Jackson, V.A.; Muzikansky, A.; Lennes, I.T.; Heist, R.S.; Gallagher, E.R.; Temel, J.S. Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non-small-cell lung cancer. J. Clin. Oncol. 2012, 30, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Kaasa, S.; Loge, J.H.; Aapro, M.; Albreht, T.; Anderson, R.; Bruera, E.; Brunelli, C.; Caraceni, A.; Cervantes, A.; Currow, D.C.; et al. Integration of oncology and palliative care: A Lancet Oncology Commission. Lancet Oncol. 2018, 19, e588–e653. [Google Scholar] [CrossRef] [PubMed]
- Knaul, F.M.; Farmer, P.E.; Krakauer, E.L.; De Lima, L.; Bhadelia, A.; Kwete, X.J.; Arreola-Ornelas, H.; Gómez-Dantés, O.; Rodriguez, N.M.; Alleyne, G.A.O.; et al. Alleviating the access abyss in palliative care and pain relief—An imperative of universal health coverage: The Lancet Commission report. Lancet 2018, 391, 1391–1454. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.J.; Temin, S.; Alesi, E.R.; Abernethy, A.P.; Balboni, T.A.; Basch, E.M.; Ferrell, B.R.; Loscalzo,M. ;Meier, D.E.; Paice, J.A.; et al. American Society of Clinical Oncology provisional clinical opinion: The integration of palliative care into standard oncology care. J. Clin. Oncol. 2012, 30, 880–887. [Google Scholar] [CrossRef]
- Wood, D.E. National Comprehensive Cancer Network (NCCN) clinical practice guidelines for lung cancer screening. Thorac. Surg. Clin. 2015, 25, 185–197. [Google Scholar] [CrossRef]
- Crawford, G.B.; Dzierz˙anowski, T.; Hauser, K.; Larkin, P.; Luque-Blanco, A.; Murphy, I.; Puchalski, C.; Ripamonti, C.; on behalf of The ESMO Guidelines Committee. Care of the adult cancer patient at the end of life: ESMO Clinical Practice Guidelines. ESMO Open 2021, 6, 100225. [Google Scholar] [CrossRef]
- Ferrell, B.R.; Temel, J.S.; Temin, S.; Alesi, E.R.; Balboni, T.A.; Basch, E.M.; Firn, J.I.; Paice, J.A.; Peppercorn, J.M.; Phillips, T.; et al. Integration of Palliative Care into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2017. [CrossRef]
- Weissman, D.E.; Meier, D.E. Identifying patients in need of a palliative care assessment in the hospital setting: A consensus report from the Center to Advance Palliative Care. J. Palliat. Med. 2011, 14, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Vogt, J.; Beyer, F.; Sistermanns, J.; Kuon, J.; Kahl, C.; Alt-Epping, B.; Stevens, S.; Ahlborn, M.; George, C.; Heider, A.; et al. Symptom burden and palliative care needs of patients with incurable cancer at diagnosis and during the disease course. Oncologist 2021, 26, e1058–e1065. [Google Scholar] [CrossRef] [PubMed]
- Rodin, R.; Swami, N.; Pope, A.; Hui, D.; Hannon, B.; Le, L.W.; Zimmermann, C. Impact of early palliative care according to baseline symptom severity: Secondary analysis of a cluster-randomized controlled trial in patients with advanced cancer. Cancer Med. 2022, 11, 1869–1878. [Google Scholar] [CrossRef] [PubMed]
- Castro JA, Hannon B, Zimmermann C. Integrating Palliative Care into Oncology Care Worldwide: The Right Care in the Right Place at the Right Time. Curr Treat Options Oncol. 2023, 24, 353–372. [Google Scholar] [CrossRef]
- Hui, D.; Hannon, B.L.; Zimmermann, C.; Bruera, E. Improving patient and caregiver outcomes in oncology: Team-based, timely, and targeted palliative care. CA Cancer J. Clin. 2018, 68, 356–376. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Bruera, E. Models of Palliative Care Delivery for Patients with Cancer. J. Clin. Oncol. 2020, 38, 852–865. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Heung, Y.; Bruera, E. Timely Palliative Care: Personalizing the Process of Referral. Cancers 2022, 14, 1047. [Google Scholar] [CrossRef]
- Martin-Rosello, M.L.; Sanz-Amores, M.R.; Salvador-Comino, M.R. Instruments to evaluate complexity in end-of-life care. Curr. Opin. Support. Palliat. Care 2018, 12, 480–488. [Google Scholar] [CrossRef]
- Grant, M.; de Graaf, E.; Teunissen, S. A systematic review of classifications systems to determine complexity of patient care needs in palliative care. Palliat. Med. 2021, 35, 636–650. [Google Scholar] [CrossRef]
- Tuca, A.; Gómez-Martínez, M.; Prat, A. Predictive model of complexity in early palliative care: A cohort of advanced cancer patients (PALCOM study). Support. Care Cancer 2018, 26, 241–249. [Google Scholar] [CrossRef]
- Busquet-Duran, X.; Jiménez-Zafra, E.M.; Manresa-Domínguez, J.M.; Tura-Poma, M.; Bosch-Delarosa, O.; Moragas-Roca, A.; Padilla, M.C.G.; Moreno, S.M.; Martínez-Losada, E.; Crespo-Ramírez, S.; et al. Describing complexity in palliative home carethrough HexCom: A cross-sectional, multicenter study. J. Multidiscip. Healthc. 2020, 13, 297. [Google Scholar] [CrossRef]
- Busquet-Duran, X.; Jiménez-Zafra, E.M.; Tura-Poma, M.; Bosch-de la Rosa, O.; Moragas-Roca, A.; Martin-Moreno, S.; Martínez-Losada, E.; Crespo-Ramírez, S.; Lestón-Lado, L.; Salamero-Tura, N.; et al. Assessing Face Validity of the HexCom Model for Capturing Complexity in Clinical Practice: A Delphi Study. Healthcare 2021, 9, 165. [Google Scholar] [CrossRef]
- Busquet-Duran, X.; Moreno-Gabriel, E.; Jiménez-Zafra, E.M.; Tura-Poma, M.; Bosch-DelaRosa, O.; Moragas-Roca, A.; Martin-Moreno, S.; Martínez-Losada, E.; Crespo-Ramírez, S.; Lestón-Lado, L.; et al. Gender and Observed Complexity in Palliative Home Care: A Prospective Multicentre Study Using the HexCom Model. Int. J. Environ. Res. Public Health 2021, 18, 12307. [Google Scholar] [CrossRef] [PubMed]
- Busquet-Duran, X.; Manresa-Domínguez, J.M.; Llobera-Estrany, J.; López-García, A.I.; Moreno-Gabriel, E.; Toran-Monserrat, P. Care complexity and place of death in palliative home care. Gac Sanit. 2022, 37, 102266. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, C.E.; Klug, D.; Campos, L.; Losekann, M.V.; Nunes, T.D.S.; Cruz, R.P. Analysis of the Perroca scale in palliative care unit. Rev. ESC Enferm. USP 2018, 52, e03305. [Google Scholar]
- Green, J.; Gordon, R. The development of Version 2 of the AN-SNAP casemix classification system. Aust. Health Rev. 2007, 31 (Suppl. S1), S68–S78. [Google Scholar] [CrossRef]
- Hui, D.; Mori, M.; Watanabe, S.M.; Caraceni, A.; Strasser, F.; Saarto, T.; Cherny, N.; Glare, P.; Kaasa, S.; Bruera, E. Referral criteria for outpatient specialty palliative cancer care: An international consensus. Lancet Oncol. 2016, 17, e552–e559. [Google Scholar] [CrossRef]
- Tuca, A.; Viladot, M.; Barrera, C.; Chicote, M.; Casablancas, I.; Cruz, C.; Font, E.; Marco-Hernández, J.; Padrosa, J.; Pascual, A.; et al. Prevalence of ethical dilemmas in advanced cancer patients (secondary analysis of the PALCOM study). Support. Care Cancer 2021, 29, 3667–3675. [Google Scholar] [CrossRef]
- Tanzi, S.; Martucci, G.; Autelitano, C.; Alquati, S.; Peruselli, C.; Artioli, G. Consultations’ demand for a hospital palliative care unit: How to increase appropriateness? Implementing and evaluating a multicomponent educational intervention aimed at increase palliative care complexity perception skill. BMC Palliat. Care 2022, 21, 90. [Google Scholar]
- Comino, M.R.S.; Garcia, V.R.; López, M.A.F.; Feddersen, B.; Roselló, M.L.M.; Sanftenberg, L.; Schelling, J. Assessment of IDC-Pal as a Diagnostic Tool for Family Physicians to Identify Patients with Complex Palliative Care Needs in Germany: A Pilot Study. Gesundheitswesen 2018, 80, 871–877. [Google Scholar]
- Carrasco-Zafra, M.I.; Gómez-García, R.; Ocaña-Riola, R.; Martín-Roselló, M.L.; Blanco-Reina, E. Level of Palliative Care Complexity in Advanced Cancer Patients: A Multinomial Logistic Analysis. J. Clin. Med. 2020, 9, 1960. [Google Scholar] [CrossRef] [PubMed]
- Cerullo, G.; Videira-Silva, A.; Carrancha, M.; Rego, F.; Nunes, R. Complexity of patient care needs in palliative care: A scoping review. Ann. Palliat. Med. 2023, 12, 791–802. [Google Scholar] [CrossRef]
- Mota-Romero, E.; Tallón-Martín, B.; García-Ruiz, M.P.; Puente-Fernandez, D.; García-Caro, M.P.; Montoya-Juarez, R. Frailty, Complexity, and Priorities in the Use of Advanced Palliative Care Resources in Nursing Homes. Medicina 2021, 57, 70. [Google Scholar] [CrossRef] [PubMed]
- Busquet-Duran, X.; Esteban-Perez, M.; Manresa-Domínguez, J.M.; Moreno, S.M.; Leston-Lado, L.; Torán-Monserrat, P. Intra-rater reliability and feasibility of the HexCom advanced disease complexity assessment model. Atención Primaria 2022, 54, 102343. [Google Scholar] [CrossRef] [PubMed]
- Viladot M, Gallardo-Martínez JL, Hernandez-Rodríguez F, Izcara-Cobo J, Majó-LLopart J, Peguera-Carré M, Russinyol-Fonte G, Saavedra-Cruz K, Barrera C, Chicote M, Barreto TD, Carrera G, Cimerman J, Font E, Grafia I, Llavata L, Marco-Hernandez J, Padrosa J, Pascual A, Quera D, Zamora-Martínez C, Bozzone AM, Font C, Tuca A. Validation Study of the PALCOM Scale of Complexity of Palliative Care Needs: A Cohort Study in Advanced Cancer Patients. Cancers (Basel). 2023, 15, 4182. [Google Scholar] [CrossRef] [PubMed]
- Hui D, Bruera E. The Edmonton Symptom Assessment System 25 Years Later: Past, Present, and Future Developments. J. Pain and Symptom Management 2017, 53, 630–643. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Bruera, E. A personalized approach to assessing and managing pain in patients with cancer. J. Clin. Oncol. 2014, 32, 1640–1646. [Google Scholar] [CrossRef] [PubMed]
- Fainsinger, R.L.; Nekolaichuk, C.L. A “TNM” classification system for cancer pain: The Edmonton Classification System for Cancer Pain (ECS-CP). Support. Care Cancer 2008, 16, 547–555. [Google Scholar] [CrossRef]
- Fainsinger, R.L.; Nekolaichuk, C.L.; Lawlor, P.G.; Neumann, C.M.; Hanson, J.; Vigano, A. A multicenter study of the revised Edmonton Staging System for classifying cancer pain in advanced cancer patients. J. Pain Symptom Manag. 2005, 29, 224–237. [Google Scholar] [CrossRef]
- Tuca-Rodriguez A, Gómez-Batiste X, Espinosa-Rojas J, Martínez-Muñoz M et al. Structure, organisation and clinical outcomes in cancer patients of hospital support teams in Spain. BMJ Support Palliat Care 2012, 2(4), 356–362.
- Glouberman, S.; Zimmerman, B. Complicated and complex systems: What would successful reform of Medicare look like? Romanow Pap. 2002, 2, 21–23. [Google Scholar]
- Munday, D.F.; Johnson, S.A.; Griffiths, F.E. Complexity theory and palliative care. Palliat. Med. 2003, 17, 308–309. [Google Scholar] [CrossRef] [PubMed]
- Hodiamont F, Junger S, Leidl R, et al. Understanding complexity– the palliative care situation as a complex adaptive system. BMC Health Serv Res 2019, 19, 157. [Google Scholar]
- Quill TE, Abernethy AP. Generalist plus specialist palliative care–creating a more sustainable model. N Engl J Med. 2013, 368, 1173–1175.
- Ernecoff NC, Check D, Bannon M, Hanson LC, Dionne-Odom JN, Corbelli J, et al. Comparing Specialty and Primary Palliative Care Interventions: Analysis of a Systematic Review. J Palliat Med. 2020, 23, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Brar SSHN, Wright FC. Multidisciplinary cancer care: does it improve outcomes? Surg Oncol. 2014, 110, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Bickel KE, McNiff K, Buss MK, Kamal A, Lupu D, Abernethy AP, et al. Defining high-quality palliative care in oncology practice: An American Society of Clinical Oncology/American Academy of Hospice and Palliative Medicine Guidance Statement. J Oncol Pract. 2016, 12, e828–e838. [Google Scholar] [CrossRef] [PubMed]
- Lupu D, Quigley L, Mehfoud N, Salsberg ES. The growing demand for hospice and palliative medicine physicians: will the supply keep up? J Pain Symptom Manag. 2018, 55, 1216–1223. [Google Scholar] [CrossRef]
- Davis MP, Strasser F, Cherny N. How well is palliative care integrated into cancer care? A MASCC, ESMO, and EAPC Project. Support Care Cancer. 2015, 23, 2677–2685. [Google Scholar] [CrossRef]
- Zimmermann C, Ryan S, Hannon B, Saltman A, Rodin G, Mak E, et al. Team-based outpatient early palliative care: a complex cancer intervention. BMJ Support Palliat Care. 2019. [CrossRef]
- Zimmermann C, Buss MK, Rabow MW, Hannon B, Hui D. Should outpatient palliative care clinics in cancer centers be stand alone or embedded? J Pain Symptom Manag. 2022. [CrossRef]
| Would you be surprised if the patient died in the next 12 months? If the answer is no, the PALCOM instrument can determine the complexity of palliative care needs and allows managing the intervention of specialized Palliative Care teams. | ||||||||||
|
1. Is a high symptom burden detected? Presence of ≥5 chronic symptoms with at least a moderate intensity (Visual Analogue Scale or Numeric Ratting Scale ≥4/10) out of 10 systematically recorded symptoms: | ||||||||||
|
|
|
|
|
|
|||||
|
2. Are there any markers of difficult pain control? Any of the following characteristics can lead to potentially difficult pain: | ||||||||||
|
|
|
||||||||
|
3. Is there functional impairment? Person who requires relevant assistance for activities of daily living. (e.g. Barthel index ≤60 or Karnofsky index ≤50-60%) | ||||||||||
| 4. Any socio-familial risk factors? | ||||||||||
|
|
|
||||||||
| 5. Any ethical or existential conflict? | ||||||||||
|
|
|
||||||||
| Each of these 5 domains is scored dichotomously, 0 absence or 1 presence of any of the variables, the sum, between 0 and 5, is the total score of the PALCOM scale. | ||||||||||
|
0-1 Low complexity:Basic palliative care is recommended. Referring team to get back in contact if patient becomes more complex. In some cases, timely consultation with specialist palliative care may be needed for a comprehensive assessment or management of difficult isolated symptoms. 2-3 Medium complexity:Specialised palliative care is systematically recommended (hospital teams, home support teams or palliative care services). 4-5 High complexity:Intensive specialised palliative care is systematically recommended (teams in the hospital, support teams in the home or palliative care services). | ||||||||||
| Development cohort | Validation cohort | PALCOM pooled data | ||||
| N (%) | N (%) | p | N (%) | |||
| Total | 324 | 283 | 607 | |||
| Gender | Male | 189 (58.0) | 161 (56.9) | 0.280 | 350 (57.7) | |
| Age | (mean ±SD*) | 69 (SD±59-80) | 71 (SD±59-81) | 0.320 | 70 SD±59-80 | |
| Primary origin | ||||||
| Lung | 71 (21.9) | 64 (24.4) | 0.310 | 140 (23.1) | ||
| Colon | 38 (11.7) | 56 (19.8) | 0.290 | 94 (15.5) | ||
| Pancreas | 28 (8.6) | 18 (6.4) | 0.270 | 46 (7.6) | ||
| Breast | 22 (6.8) | 19 (6.7) | 0.190 | 41 (6.8) | ||
| Prostate | 18 (5.5) | 28 (9.9) | 0.210 | 46 (7.6) | ||
| Others | 146 (45.1) | 93 (32.8) | 0.300 | 239 (39.4) | ||
| Symptom prevalence | ||||||
| Asthenia | 299 (92.2) | 269 (95.1) | 0.210 | 568 (93.6) | ||
| Anorexia | 253 (78.1) | 226 (79.9) | 0.079 | 479 (78.9) | ||
| Pain | 245 (75.6) | 245 (86.6) | 0.100 | 490 (80.7) | ||
| Nausea | 110 (34.0) | 68 (24.0) | 0.080 | 178 (29.3) | ||
| Constipation | 202 (62.3) | 162 (57.2) | 0.110 | 364 (59.9) | ||
| Dyspnoea | 149 (45.9) | 111 (39.2) | 0.220 | 260 (42.8) | ||
| Insomnia | 191 (58.9) | 177 (62.5) | 0.180 | 368 (60.6) | ||
| Anxiety | 238 (73.4) | 184 (65.0) | 0.090 | 422 (69.5) | ||
| Sadness | 225 (69.4) | 196 (69.3) | 0.220 | 421 (69.4) | ||
| PALCOM domains | ||||||
| High symptom burden | 134 (41.3) | 136 (48.1) | 0.190 | 270 (44.5) | ||
| Refractory pain | 175 (54.0) | 166 (58.5) | 0.220 | 341 (56.2) | ||
| Karnoksky index ≤60% | 129 (39.9) | 135 (47.5) | 0.210 | 264 (43.5) | ||
| Socio-familial risk | 221 (68.3) | 184 (64.8) | 0.420 | 405 (66.7) | ||
| Existential/ethical conflicts | 59 (18.3) | 67 (23.6) | 0.080 | 126 (20.7) | ||
| PALCOM scale level | ||||||
| Low | 51 (15.8) | 67 (23.7) | 0.080 | 118 (19.5) | ||
| Medium | 139 (43.0) | 167 (59.9) | 0.780 | 306 (50.5) | ||
| High | 133 (41.2) | 49 (17.3) | 0.060 | 182 (30.0) | ||
| Development cohort | Validation cohort | Pooled data | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | 324 (53.4% of polled data) | 283 (46.6% of polled data) | 607 | |||||||||||
| Hospital inclusion | 180 (55.6) | 175 (61.8) | 355 (58.5) | |||||||||||
| Community inclusion | 144 (44.4) | 108 (38.2) | 252 (41.5) | |||||||||||
| Low | Medium | High | Low | Medium | High | Low | Medium | High | ||||||
| 51 (15.8) | 139 (43.0) | 133 (41.2) | 67 (23.7) | 167 (59.9) | 49 (17.3) | 118 (19.5) | 306 (50.5) | 182 (30.0) | ||||||
| PALCOM domains | p | p | p | |||||||||||
| High symptom burden | 20 (39.2) | 99 (71.2) | 115 (86.5) | <0.001 | 6 (8.9) | 83 (49.7) | 47 (95.5) | <0.001 | 26 (22.0) | 182 (59.4) | 162 (89.0) | <0.001 | ||
| Refractory pain | 13 (25.5) | 69 (49.6) | 93 (69.9) | <0.001 | 30 (45.7) | 93 (55.4) | 43 (87.8) | <0.001 | 43 (36.4) | 162 (52.9) | 136 (74.7) | <0.001 | ||
| Karnofsky index <60% | 17 (33.3) | 53 (38.1) | 59 (44.4) | <0.001 | 4 (5.9) | 90 (53.6) | 41 (83.7) | <0.001 | 21 (17.8) | 143 (46.7) | 100 (54.9) | <0.001 | ||
| Socio-familial risk | 33 (64.7) | 81 (58.3) | 107 (80.5) | 0.055 | 13 (19.4) | 126 (75.0) | 45 (91.8) | <0.001 | 46 (42.5) | 207 (67.6) | 152 (83.5) | <0.001 | ||
| Existential/ethical conflicts | 1 (2.0) |
25 (18.0) | 33 (24.8) | <0.001 | 4 (5.9) | 34 (20.2) | 29 (59.2) | <0.001 | 5 (4.2) | 59 (19.5) | 56 (30.8) | <0.001 | ||
| Death within 6 months | 18 (35.3) | 77 (55.4) | 99 (74.3) | <0.001 | 33 (49.2) | 114 (68.3) | 38 (77.6) | <0.001 | 51 (43.2) | 190 (62.7) | 138 (75.8) | <0.001 | ||
| Hospital death | 3 (5.9) | 24 (17.3) | 40 (30.1) | <0.001 | 6 (8.9) | 25 (22.1) | 12 (30.8) | <0.001 | 9 (7.6) | 49 (16.0) | 52 (28.6) | <0.001 | ||
| Low | Medium | High | |||||||||||
| N (%) |
Instability ratio N (cumulative %)* |
Emergency. Mean ±SD ** | Hospital days Mean ±SD * | N (%) |
Instability ratio N (cumulative %)* |
Emergency. Mean ±SD ** | Hospital days Mean ±SD * | N (%) |
Instability ratio N (cumulative %)* |
Emergency. Mean ±SD ** | Hospital days Mean ±SD * | p | |
| Baseline | 67 (23.7) | 167 (59.9) | 49 (17.3) | ||||||||||
| Month 1 | 64 (95.5) | 3 (4.5) | 0,17 ±0.4 | 1,0 ±3.1 |
153 (91.6) | 14 (8.4) | 0,22 ±0.4 |
1,5 ±4.8 |
40 (81.6) | 9 (18.4) | 0,31 ±0.5 |
2,5 ±6.7 |
* <0.001 ** NSD |
| Month 2 | 57 (85.1) | 7 (14.9) | 0,27 ±0.6 | 2,0 ±5.5 |
118 (70.7) | 35 (29.3) | 0,24 ±0.5 |
1,9 ±5.6 |
26 (53.1) | 14 (46.9) | 0,25 ±0.5 |
1,97 ±5.8 |
* <0.001 ** NSD |
| Month 3 | 51 (76.1) | 6 (23.8) | 0,20 ±0.4 | 2,2 ±5.2 |
90 (53.9) | 28 (46.1) | 0,25 ±0.5 |
2,0 ±5.5 |
16 (32.7) | 10 (67.3) | 0,26 ±0.6 |
2,09 ±6.6 |
* <0.001 ** NSD |
| Month 4 | 45 (67.2) | 6 (32.8) | 0,18 ±0.4 | 1,5 ±4.1 |
71 (42.5) | 19 (57.5) | 0,22 ±0.4 |
2,1 ±5.4 |
12 (24.5) | 4 (75.5) | 0,23 ±0.4 |
4,38 ±9.5 |
* <0.001 ** NSD |
| Month 5 | 36 (53.7) | 9 (46.3) | 0,10 ±0.3 | 1,3 ±5.1 |
67 (40.1) | 4 (59.9) | 0,23 ±0.5 |
2,0 ±5.9 |
11 (22.4) | 1 (77.6) | 0,25 ±0.6 |
2,92 ±7.9 |
* <0.001 ** NSD |
| Month 6 | 33 (49.3) | 3 (50.7) | 0,14 ±0.3 | 1,1 ±2.8 |
53 (31.7) | 14 (68.3) | 0,24 ±0.5 |
1,2 ±3.1 |
11 (22.4) | 0 (77.6) | 0,17 ±0.4 |
5,25 ±10.6 |
* <0.001 ** NSD |
| Overall 6 months | 34 (50.7) | 0,2 ±0.3 | 1,5 ±4.0 |
114 (68.3) | 0,2 ±0.5 |
1,8 ±5.0 |
38 (77.6) | 0,25 ±0.5 |
3,2 ±7.8 |
* <0.001 ** NSD |
|||
|
* Significant differences in probability of level change and mean hospitalisation days per month among levels of complexity of palliative care needs ** NSD: No significant differences in means of frequency of emergency department visits per month among levels of complexity of palliative care needs SD: standard deviation | |||||||||||||
| Level | Characteristics |
|---|---|
| Low | Involvement of 0 or 1 domains on the PALCOM scale. Low likelihood of radical change in baseline conditions in the first 3 months, at least moderate in next months. Frequency of emergency department visits similar to other levels (cancer complications or treatment toxicity). Need for hospitalisation significantly lower than other levels Survival significantly higher than other levels. |
|
|
| Medium | Involvement of 2-3 domains on the PALCOM scale. Low-moderate likelihood of radical change in baseline conditions in the first 3 months, at moderate-high in next months. Frequency of emergency department visits similar to other levels (cancer complications or treatment toxicity). Need for hospitalisation significantly higher than low complexity level. Survival significantly lower than low complexity level. |
|
|
| High | Involvement of 4-5 domains on the PALCOM scale. At least moderate likelihood of radical change in baseline conditions in the first weeks, at very high since second month of follow-up. Frequency of emergency department visits similar to other levels (cancer complications or treatment toxicity). Need for hospitalisation significantly higher than other levels Survival significantly lower than other levels. |
|
|
|
Categorisation of frequencies in this context: low<20%; moderate 21-40%; high 41-60%; very high >60%. ** Primary PC: Primary Care professionals and basic PC training. *** Secondary PC: Professionals specialised in oncology and basic training in PC. **** Tertiary PC: Professionals specialised in EPC. PC: palliative care. EPC: early palliative care | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





