1. Introduction
Immunization is a cost-effective health intervention for reducing the burden of many vaccine-preventable diseases (VPD), disabilities, and deaths (1-3). Every year, more than two million children are saved through timely immunization (4), and between the years 2000 and 2015, immunization has reduced the global burden of deaths to VPDs fourfold (5). The Centres for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP) endorse the importance of timely immunization for reducing the burden of VPDs and deaths among children (6, 7).
In children, timely immunization is an important strategy for reducing the global burden of VPDs (7,8). Adherence to timely immunization in children can dramatically reduce the incidence, prevalence, and mortality of various types of VPDs (8). Timely immunization in children refers to immunizing a child within 28 or 30 days of the scheduled immunization date (8,9). However, early administration (invalid immunization) or delayed administration or missing the dose of vaccines in children indicates non-compliance with the recommended immunization schedule, which is associated with a higher risk of VPDs and even deaths (3,10-12).
Immunization non-compliance is a global concern for both developed and developing countries. This issue of immunization non-compliance is more common among underdeveloped nations (13,14). However, within a country urban-rural differences pertaining to immunization compliance also exist (15,16).
Within the South Asia region, Pakistan is the second largest country, with a human development index of 161. This HDI of 161 indicates the poor socioeconomic condition of the country. The country is still a hub of wild poliovirus (WPV) despite global eradication efforts (17). According to the Pakistan Demographic and Health Survey (PDHS) report 2017-2018, the coverage of full immunization among children in Pakistan is 66%. Of these, only 50% had received age-appropriate immunisation (18). Compared with children of middle to high socioeconomic class, more than a quarter of children from low socioeconomic class remain unimmunised (19). Children living in urban slums are underprivileged and are more susceptible to various VPDs, such as polio, measles, and enteric fever (19, 20). However, statistics about immunization coverage and appropriate immunization practices in slum areas are not yet known.
Karachi, a densely populated metropolitan city in Pakistan with a population of 14.9 million, accommodates approximately 40% slum dwellers (21). Despite the critical public health implications, there is a notable lack of comprehensive research regarding the immunization practices of slum dwellers in Karachi. To address this knowledge gap, this study investigated the paediatric immunization practices among slum dwellers in Karachi. The study focused on identifying the determinants of invalid, delayed, and missed immunizations within this specific urban demographic. Thus, this study provided a deeper understanding of the factors affecting immunization compliance in slum areas and contribute valuable insights to improve immunization programs and public health strategies in this urban context.
2. Methodology
2.1. Study Design, Setting, and Duration:
This community-based retrospective study was carried out in the urban slums of Karachi from October 2018 to August 2019. In this study, immunization data of children of urban slums aged below 2-years was extracted from their vaccination cards. The urban slums in this study were selected from six different districts of Karachi: District East, District South, District Central, District West, District Malir, and District Korangi. Each district is composed of union councils (UCs) of different size. Within each union council, many slums exist. In general, 40% of the Karachi population is composed of slum dwellers (21, 22). People living in urban slums are underprivileged, and 89% of slum dwellers are living below the poverty line (22). Thus, this study targeted slums from each UCs and district of Karachi, Pakistan.
2.2. Study Population, Sample Selection Sampling Method
This study targeted mothers of children aged less than two years from the urban slums of Karachi. The recent report of Pakistan Demographic & Health Survey (2017-2018) reported 48.6% age-appropriate immunization rate among under two-years children of urban Sindh. Considering 48.6% as the appropriate immunization practices, 95% confidence interval, and 5% margin of error, the sample size calculated was 377. The research team decided to extrapolate the sample size to triple because of concerns related to participants refusals, incomplete and/or partial responses.
For the selection of study participants, a multistage sampling technique was employed. The research team at first selected the urban slums from each district following a non-probability purposive sampling method. The non-probability purposive sampling method for the selection of slums was used because no definite information regarding the number of slums within each district of Karachi exists. In this study, the research team purposively selected each slum, and then took permission from stakeholders (union council chairman or community leaders, or religious leaders) for a household survey. Following the selection of urban slums, households and participants were selected. For the selection of participants, the 30X7 multi-stage cluster sampling technique was used. The 30X7 cluster sampling technique is a type of random sampling technique, in which the research team approaches every 7th household from each cluster. This type of sampling technique is extensively used by the Expanded Programme on Immunisation (EPI) for evaluating the vaccination program coverage and its efficacy (23). To perform the 30X7 sampling method, the research team of this study classified each slum as a cluster. From each cluster, every 7th household was approached systematically for the data collection. A pre-enrolment screening was performed for assessing the eligibility of each household.
The households were selected for data collection if they have parents/caregivers, vaccination cards, and children under two years of age. Certain households were excluded because of communication barriers, and the non-availability of community volunteers as translators. In a household where children under two years of age were not present then the next house was considered for inclusion. After eligibility determination, the research team enrolled all the parents/caregivers of all the eligible children. The research team interviewed all the enrolled parents/caregivers regarding paediatric immunization practices and assessed the vaccination status of each child from the vaccination card, which were obtained from the parents/caregiver during the household visits.
2.3. Description of Data Collection Instrument
For conducting this survey, translated version (Urdu) of a pre-validated and structured questionnaire having a reliability coefficient of 0.714 was used. This questionnaire was adapted from a study conducted by Khaliq, et al., (2017) in Karachi, Pakistan (3).
The questionnaire used in the study had seven sections, which consist of 63 questions. The first section of this questionnaire consisted of four questions, which were related to the visit information. The second and third sections of this questionnaire determined the eligibility of each participant approached for the data collection. Participants who were found eligible after the predefined screening were invited to participate in other sections of this questionnaire. A four-digit enrolment number was provided to all the respondents who consented to participate. For each ewasled participant, further information related to the sociodemographic background, immunization-related knowledge and practices, and reasons for immunization non-adherence were collected from the questions present in section four to section six. The last section of this questionnaire provides information related to the quality control and quality assurance parameters pertaining to data collection, data reviewing, and data entry.
2.4. Measurement of Study Outcome
In this study, the outcome of interest was the immunization status of children, and the immunization status of each child was calculated from the vaccine administration dates and the due date of vaccination. The vaccine administration date was the date at which the child receives a vaccination, whereas the due date of vaccination was the date at which the child has either received or has to receive the succeeding vaccination dose. The information related to vaccine administration and due date were obtained from the vaccination cards. The research team identified four different types of immunization status: valid, delayed, missed, or invalid.
If the vaccine administration date was within the window period of five days before or within 28 days of the vaccine schedule date, then it was considered a valid vaccine administration. Vaccine administration to a child five days before the recommended scheduled doses, then it is considered as invalid administration (24). The immunization was considered delayed if the difference between the vaccine schedule date and vaccine administration date exceeds more than four weeks or 28 days (25). Likewise, when the vaccination card does not show any evidence of vaccine administration irrespective of vaccine schedule date, then it is called missed vaccine administration.
2.5. Study Covariates
For assessing the determinants of immunization non-compliance, various child, maternal, paternal, household, and practices related covariates were examined. Among the children related factors, the child age, child sex, and childbirth order were included. However, for the maternal and paternal factors, the age and education of mother and father was considered separately. The household factors, include number of children delivered, family size, and place of birth. The knowledge and practice related factors included a set of questions, which assessed the knowledge and practice related to the immunization practice. The mothers who responded correctly were categorized as “Knowledgeable”, while others were classified as “Not knowledgeable”.
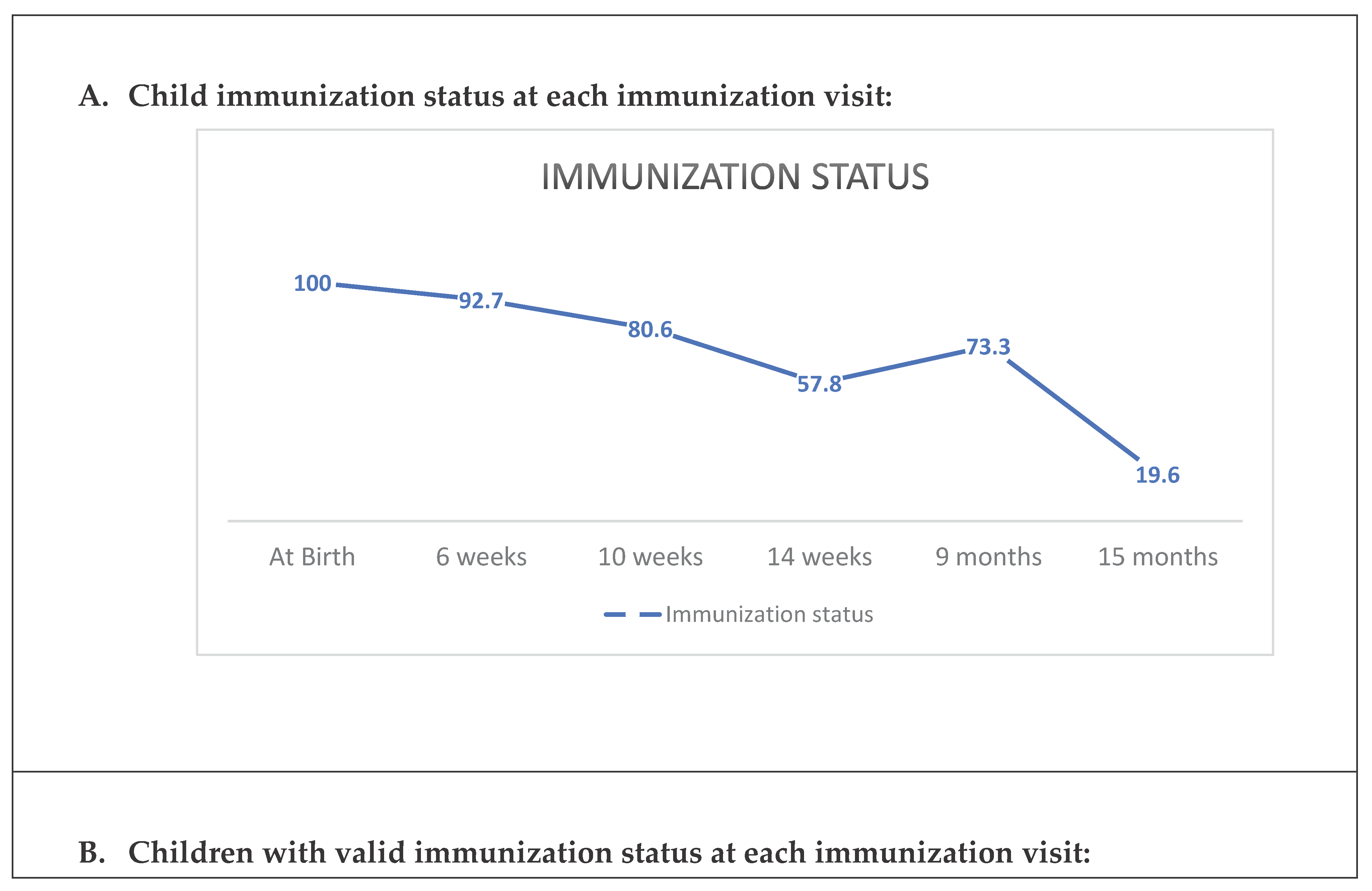
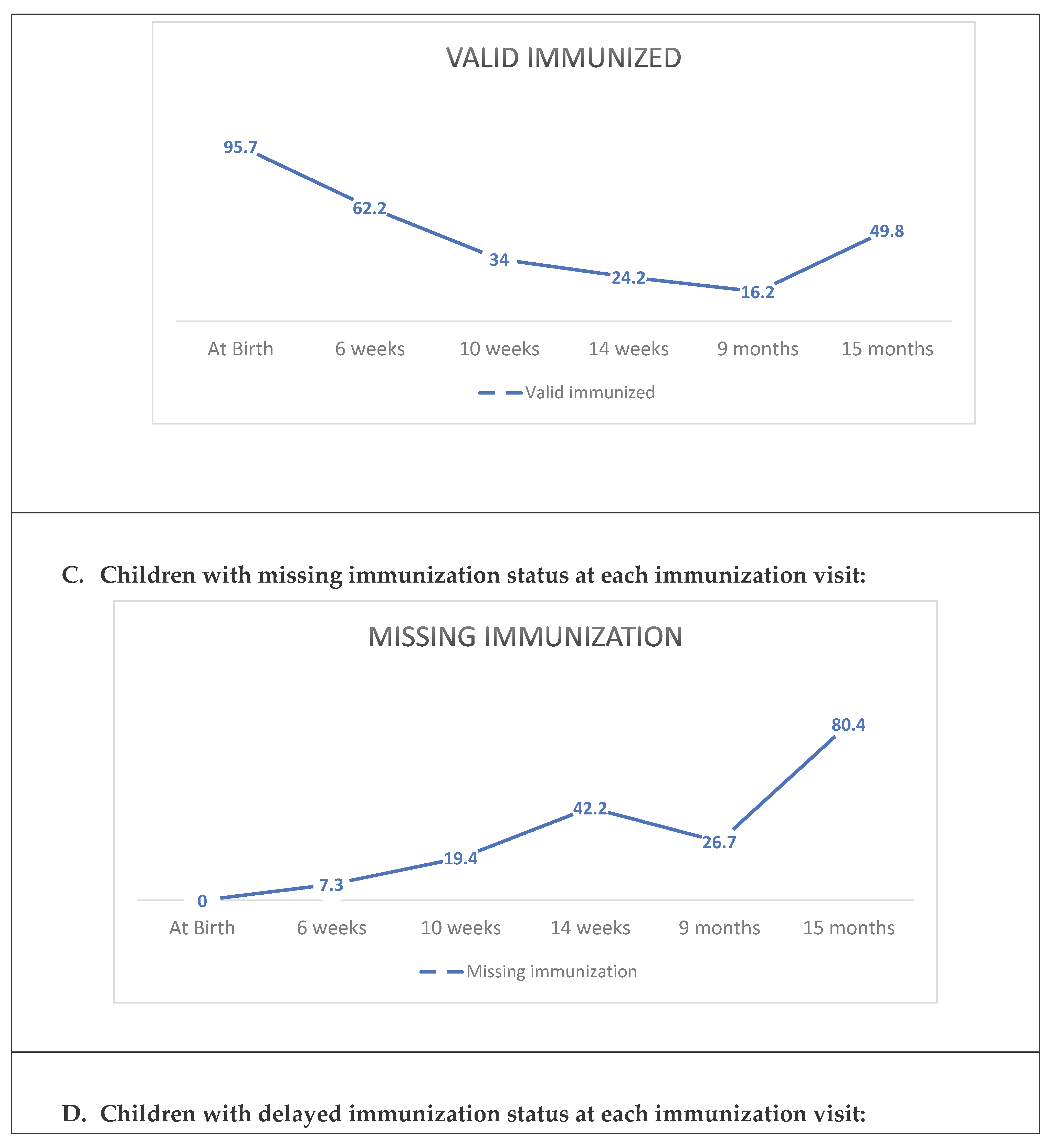
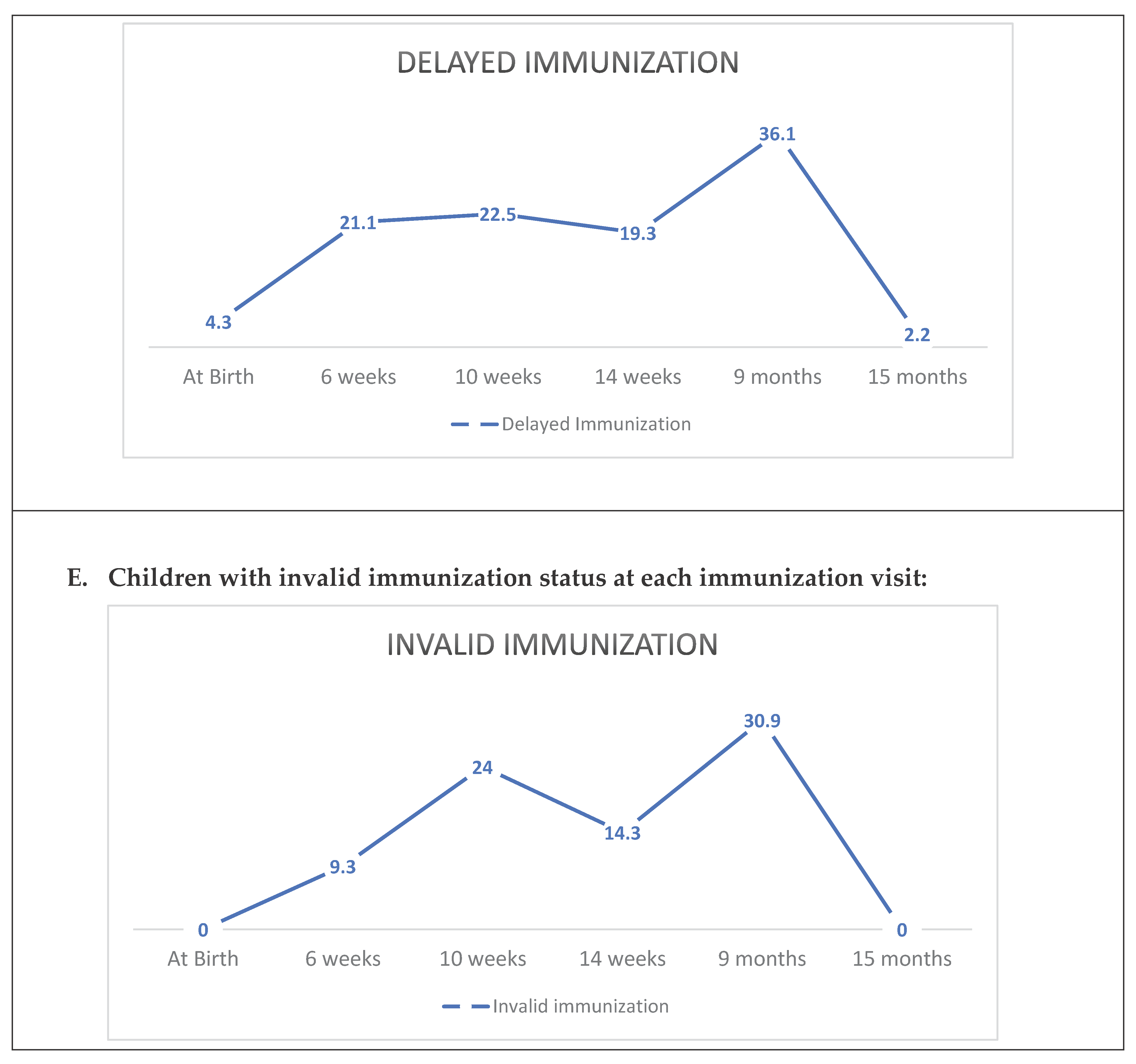
Immunization visits were assessed at six different times according to the EPI schedule of Pakistan i.e., “
at birth”, “6-weeks”, “10-weeks”, “14-weeks”, “9-months” and
“15-months”. The detail regarding these categories is presented in
Table 1.
2.6. Statistical Analysis
The data regarding the number of each study variable was assessed descriptively using Jamovi 1.2.25 software. All the categorical and continuous variables at first were assessed descriptively. Later, the distribution of each categorical and continuous variable for each category of outcome variable was assessed descriptively. The data of all the categorical variables were presented using frequency and percentage, while for the continuous variables mean and standard deviation were used for the presentation of descriptive data. In addition, the rates of full immunization, timely (valid) immunization, invalid immunization, delayed immunization, and missed immunization was calculated for the overall sample as well as at each immunization visit. Trend lines were used for illustrating the different type of immunization rates (overall and each visit).
The determinants of each type of immunization non-compliance were assessed using multinomial logistic regression. For running the multinomial logistic regression, unadjusted odds ratio (OR) and adjusted OR were calculated. A backward elimination method for calculating the adjusted ORs was used, and all the variables having a significance of over 5% were removed manually from the model. In the final model, we kept only those variables having a significance level of ≤ 0.05. The OR and 95% confidence interval for each variable were assessed to present the association of immunization status with the various predictor variables.
2.7. Ethical Consideration
The protocol of this research was approved by the Management Research Cell (MRC) of the Department of Health Management, Institute of Business Management (IoBM), Karachi, Pakistan (Approval number: MBA-MHM-16909-19). Moreover, permissions from all the stakeholders of different slums were also taken before data collection. Verbal and written consent was taken from the participating caretaker. Principals of beneficence, non-malevolence, anonymity, and equity were maintained throughout the study.
3. Results
3.1. Screening, Eligibility, and Enrolment of Study Participants
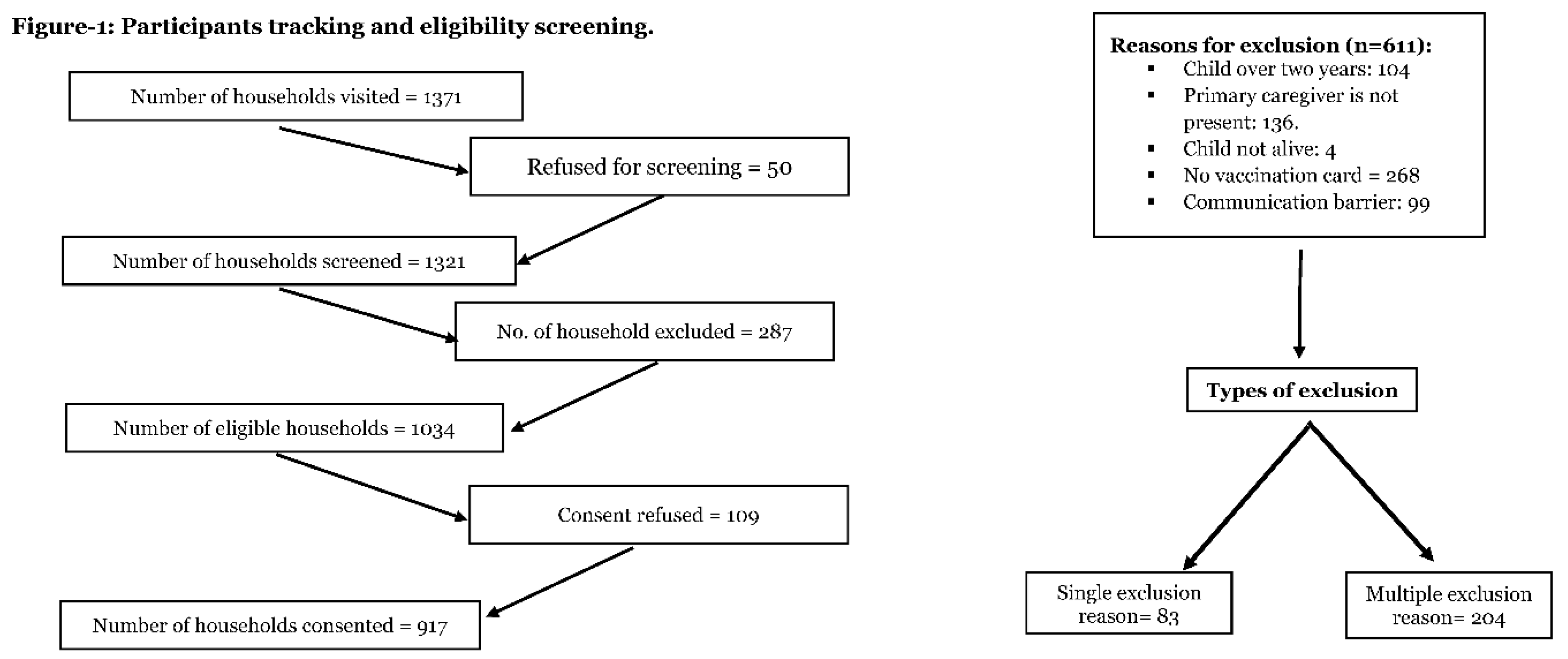
A total of 1,371 households from all six clusters were approached, of which 50 refused for screening the child. Of the remaining 1,321 households, 1,034 were eligible. Among eligible households, data of 917 households were used for analysis, while the rest was removed because of several reasons highlighted in
Figure 1.
3.2. Characteristics of Study Sample
Of 917 participants, around half of the children received vaccination on time (n=457~49.8%). There were 20.2% (n=185) children, who missed an immunization visit, while the prevalence of invalid and delayed immunized children was 12% (n=110) and 18% (n=165), respectively.
The distribution of male and female children was almost homogenous, there were 49.1% (n=450) males, and 50.9% (n=467) female. In this study, only 5% (n=46) of children had reached the age of sixth immunization visits (
Table 2).
More than half (n=498~54.3%) of the mothers had correct knowledge about the number of immunization visits during the first year of child life, while the correct knowledge about the immunization visits during the second year of their child’s life was near to a quarter (n=241~26.3%).
Different reasons for the immunization non-adherence reported in this study were lack of knowledge (n=648 ~ 71.3%), childhood illnesses (555 ~61.1%), lack of interest of decision-makers (n=534 ~58.7%), and unavailability of vaccines in the immunization centre (n=494~54.5%) (Table-2).
3.3. Infant Immunization Status for Different Immunization Visits
The highest immunization rate of 100% was reported at first visit, i.e., at birth. Similarly, the valid immunization rate of 95.7 per 100 children was observed at first visit. However, no single case of invalid and missed immunization was reported at that visit. Following the second immunization visit, this study reported a sharp decline in the immunization rate, including valid immunization rate. The immunization rate at second visit (6
th week) was 92.7 per 100 children, which decreased to 19.6 per 100 children at the sixth visit (15
th-month). Similarly, the valid immunization rate at second immunization visit was 62.2 per 100 children, which decreased to 16.2 per 100 children and 17.4 per 100 children during the 5
th and 6
th immunization visits, respectively. The decrease in the immunization rate, including valid immunization rate at each succeeding immunization visit was accompanied by an upsurge of invalid and/or delayed and/or missed immunization among children (
Figure 2).
3.4. Determinants of Invalid, Delayed, and Missed Immunization
An increase in paternal education was significantly associated to decrease the odds of invalid, delayed, and missed immunization in children. Similarly, concerns regarding the vaccines non-availability significantly reduce the odds of invalid and missed immunization but showed no association with the delayed immunization (Table-3). However, incorrect knowledge about the number of immunization visits during the first year of life, lack of knowledge about the immunization schedule, and lack of trust in the government significantly increase the odds of invalid, delayed and missed immunization (Table-3).
4. Discussion
The age-proportionate and timely immunisation are crucial for preventing the infectious diseases and promoting the health of a child. In this study, we found that invalid and delayed immunisation replaced the valid immunisation with the increase in age. The rate of valid immunisation decreased with the age of a child while the rate of missing and delayed immunisation increased with the age. The rate of valid immunisation is high at birth while the rate of delayed immunisation is hight at the age of 9 months and the missing immunisation is high at the age of 15 months. The percentage of fully immunized children for all the vaccines recommended in EPI program of Pakistan was 20% and this percentage is far lower than the finding reported by earlier studies held in other regions of Pakistan (26-28). The low percentage of fully immunized children can be attributed to the limited information on the source of data. In our study, data related to child immunisation were collected from the vaccination card of a child. However, in other studies (26,27), the data was collected from the vaccine registries or caregivers’ verbal recall. Despite the source of information, it may be important for recording child immunisation on vaccination card as clinical records may be valid than the caregivers’ or parents’ recall over the time (29).
We found in our study that inadequate knowledge about the number of immunization visits during the first year of life, lack of knowledge about the immunization schedule were significantly increased the odds of in-valid, delayed and missed immunisation. Giving inadequate information to parents regarding immunisation may be a reason for the increased odds of invalid or missed immunisation of child (30) as parents may not be aware of their child’s immunisation schedule. Similarly in a study conducted in Pakistan, it was revealed that parents having lack of knowledge about immunisation schedules or the interval between subsequent doses of vaccines were significantly positively associated with missed or delayed immunisation in children (3). However, reasons for lack of knowledge in parents were not explored in detail in our study. Therefore, it may be worth assessing parents’ knowledge about vaccination against various factors related to their socio-demographic characteristics and factors related to health services support in the future. However, the findings of our study emphasize that education regarding the importance of child immunisation, frequent awareness of child immunisation schedule is required for parents in Pakistan regardless of any circumstances.
Our study demonstrated a significant association between vaccine unavailability and immunization non-compliance. This vaccine unavailability is linked to uneven vaccine distribution and disparities in delivering community health services within a country, mirroring results from a study conducted in the United Kingdom. (31). Therefore, it is important that Pakistan health services should monitor the supply of vaccines and accessibility of vaccine doses across the mandatory immunisation periods to avoid delayed or missed immunisation to children. Further, this study has been limited to the parents and children from Karachi, Pakistan. Therefore, it may be worth assessing whether availability of vaccines an issue across other regions of Pakistan. It may be meaningful to do such assessment across other regions to identify the process of vaccine supplies and equity in accessing vaccines across the county to take nation level action to avoid inequity in health services.
Also, it is evident from global studies, that personal beliefs of parents regarding child immunisation, myths around immunisation, lack of trust on health services, and socio-economic status of a child’s family significantly influence the vaccine uptake during the first two years of a child’s life (32-34). However, we did not find associations between these factors and immunisation status of child from Karachi Pakistan. Therefore, broader research may be need across other regions of Pakistan to identify the factors related to parent’ knowledge and beliefs around child immunisation. In addition to improving the practice of health services, developing a positive attitude in parents towards child immunisation may add value to time uptake of vaccines. This may minimise the chances of delayed of missed immunisation in children from Pakistan (34,35).
4.1. Strengths and Limitations of the Study
To the best of our knowledge, this study is amongst the few studies, which examined the determinants of non-adherence to immunization and its relationship with maternal knowledge. This study provided strong evidence regarding the determinants of non-adherence to immunization because in this study the immunization status of each child was assessed through the vaccination card. Moreover, the use of a pre-validated structured questionnaire and 30X7 sampling technique for the recruitment of a large sample further strengthens the findings of this study. However, there were several limitations in this study. The data of this study were collected from the child vaccination card only at once and it was not validated from the other sources, like vaccination centres. Further some parents/caregiver did not know about the exact date of birth of their children, and many parents reported different ages of their child from the ages written on the vaccination card. Due to this reason, the relationship of child age with the immunization status was not assessed in this study. This study was limited to purposefully selected slums in Karachi Pakistan and the data was only collected from mothers who were able to communicate in the local language, while migrants from the rural and tribal areas who are unable to communicate in local language also constitute a large segment of the population. Therefore, the findings of this study cannot represent the determinants of immunization non-adherence of whole Karachi, and the whole country. Therefore, scaling further research with continuous follow-up across different regions of Pakistan and among various group of people from Pakistan may help in evaluating the real gap of valid immunisation timing among the immunized children.
4.2. Conclusion
From this study, it is evident that the proportion of timely immunized children is far less than the percentage of timely immunized children. With every subsequent immunisation visit or progression in infant age, the proportion of fully and timely immunized children decrease exponentially. Thus, vaccinating infant at right time is crucial for preventing the burden of VPDs among infants.
Author’s contribution
The idea of this research was conceived by SM, who worked on the data collection, data entry, data analysis, and results writing. The methodology of this project was written by AK, while the AZ wrote the introduction. The discussion of this research was partly written by SM, AK, and ZL. The final draft of this manuscript was reviewed and edited by ZL.
Funding
The project was self-funded by the primary researcher. All the cost related to the transportation and stationery was bear by the primary researcher. Declaration: This research was the thesis project of Ms. Saher Mukhtar Ali, who did her MBA-MHM from the Institute of Business Management (IoBM), Karachi, Pakistan, under the supervision of Dr. Asif Khaliq and Dr. Asima Zahid.
Acknowledgments
We would like to thank all the stakeholders, who provided us permission for the data collected from different slums. We also would like to thank Mr. Shahid Hussain for providing logistics support.
Conflicts of Interest
All authors declare no conflict of interest.
References
- Kazi, A.M.; Ali, M. ; K A, Kalimuddin, H. ; Zubair, K.; Kazi, A.N.; et al. Geo-spatial reporting for monitoring of household immunization coverage through mobile phones: Findings from a feasibility study. International Journal of Medical Informatics. 2017, 107, 48–55. [Google Scholar] [CrossRef]
- Manandhar, K.; Bajcharya, K.; Prajapati, R.; Shrestha, N.C. Prevalence and Predictors of Incomplete Immunization among Children Residing in the Slums of Kathmandu Valley: A Community Based Door-to-Door Survey. Kathmandu Univ Med J (KUMJ). 2018, 16, 8–13. [Google Scholar]
- Khaliq, A.; Sayed, S.A.; Hussaini, S.A.; Azam, K.; Qamar, M. Missed immunization opportunities among children under 5 years of age dwelling In Karachi city. Journal of Ayub Medical College, Abbottabad: JAMC. 2017, 29, 645. [Google Scholar] [PubMed]
- World Health Organisation. Immunisation coverage - Key facts 2020 [updated 2020, th; cited 2023 October, 5th]. Available from: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage. 15 July.
- Restrepo-Méndez, M.C.; Barros, A.J.; Wong, K.L.; Johnson, H.L.; Pariyo, G.; Wehrmeister, F.C.; et al. Missed opportunities in full immunization coverage: findings from low-and lower-middle-income countries. Global health action. 2016, 9, 30963. [Google Scholar] [CrossRef] [PubMed]
- Centres for Disease Control Prevention. Vaccine recommendations and guidelines of the ACIP: contraindications and precautions. 2017.
- Centres for Disease Control Prevention. Vaccine recommendations and guidelines of the ACIP 2015 [Available from: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/rabies.html.
- Wariri, O.; Utazi, C.E.; Okomo, U.; Sogur, M.; Murray, K.A.; Grundy, C.; Fofanna, S.; Kampmann, B. Timeliness of routine childhood vaccination among 12–35 months old children in The Gambia: Analysis of national immunisation survey data, 2019–2020. PloS one. 2023, 18, e0288741. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, S.E.; Russell, M.L.; Liu, X.C.; Simmonds, K.A.; Lorenzetti, D.L.; Sharpe, H.; Svenson, J.; Svenson, L.W. Are we speaking the same language? An argument for the consistent use of terminology and definitions for childhood vaccination indicators. Human vaccines & immunotherapeutic. 2019, 15, 740–747. [Google Scholar] [CrossRef]
- Guerra, F.A. Delays in immunization have potentially serious health consequences. Pediatric Drugs. 2007, 9, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Lochlainn, L.M.; de Gier, B.; van der Maas, N.; van Binnendijk, R.; Strebel, P.M.; Goodman, T.; de Melker, H.E.; Moss, W.J.; Hahné, S.J. Effect of measles vaccination in infants younger than 9 months on the immune response to subsequent measles vaccine doses: a systematic review and meta-analysis. The Lancet Infectious Diseases. 2019, 19, 1246–1254. [Google Scholar] [CrossRef] [PubMed]
- Borras, E.; Urbiztondo, L.; Costa, J.; Batalla, J.; Torner, N.; Plasencia, A.; Salleras, L.; Dominguez, A. ; Working Group for the Study of Measles Immunity in Children. Measles antibodies and response to vaccination in children aged less than 14 months: implications for age of vaccination. Epidemiology & Infection. 2012, 140, 1599–1606. [Google Scholar] [CrossRef]
- National Institute of Population Studies, N.P. ; Icf. Pakistan Demographic and Health Survey 2017-18. Islamabad, Pakistan: NIPS/Pakistan and ICF; 2019.
- Magambo, N.K.; Bajunirwe, F.; Bagenda, F. Geographic location of health facility and immunization program performance in Hoima district, western Uganda: a health facility level assessment. BMC Public Health. 2020, 20, 1–0. [Google Scholar] [CrossRef]
- Freeman, R.E.; Leary, C.S.; Graham, J.M.; Albers, A.N.; Wehner, B.K.; Daley, M.F.; Newcomer, S.R. Geographic proximity to immunization providers and vaccine series completion among children ages 0–24 months. Vaccine. 2023, 41, 2773–2780. [Google Scholar] [CrossRef]
- Siddique, M.; Iftikhar, S.; Dharma, V.K.; Shah, M.T.; Siddiqi, D.A.; Malik, A.A.; Chandir, S. Using geographic information system to track children and optimize immunization coverage and equity in Karachi, Pakistan. Vaccine. 2023, 41, 2922–2931. [Google Scholar] [CrossRef]
- Khaliq, A.; Elahi, A.A.; Zahid, A.; Lassi, Z.S. A survey exploring reasons behind immunization refusal among the parents and caregivers of children under two years living in urban slums of Karachi, Pakistan. International Journal of Environmental Research and Public Health. 2022, 19, 11631. [Google Scholar] [CrossRef]
- Khan, I.M.; Amber, W.; Chishti, A.L.; Hassan, K.A. Assessment of Complete Coverage of Expanded Program on Immunization in Children at Mayo Hospital Lahore, Pakistan. Journal of Islamabad Medical & Dental College. 2020, 9, 12–16. [Google Scholar] [CrossRef]
- Crocker-Buque, T.; Mindra, G.; Duncan, R.; Mounier-Jack, S. Immunization, urbanization, and slums – a systematic review of factors and interventions. BMC Public Health. 2017, 17, 556. [Google Scholar] [CrossRef] [PubMed]
- United Nation International Children's Fund. Pakistan: Key Demographic Indicators [Available from: Retrieved from: https://data.unicef.org/country/pak/ (last accessed on: , 2023). 7 March.
- Khaliq, A. ; Amreen, Jameel, N. ; Krauth, S.J. Knowledge and practices on the prevention and management of diarrhea in children under-2 years among women dwelling in urban slums of Karachi, Pakistan. Maternal and child health journal. 2022, 26, 1442–1452. [Google Scholar] [CrossRef] [PubMed]
- Shams, Z.I.; Shahid, M.; Nadeem, Z.; Naz, S.; Raheel, D.; Aftab, D.; et al. Town socio-economic status and road width determine street tree density and diversity in Karachi, Pakistan. Urban For Urban Green [Internet]. 2020, 47, 126473. [Google Scholar] [CrossRef]
- Henderson, R.H.; Sundaresan, T. Cluster sampling to assess immunization coverage: A review of experience with a simplified sampling method. Bull World Health Organ. 1982, 60, 253–260. [Google Scholar] [PubMed]
- World Health Organization. Immunization coverage cluster survey, reference manual. 2005.
- Centers for disease control and Prevention. Contraindications and Precautions [Internet]. 2023. Available from: https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.pdf.
- Riaz, A.; Husain, S.; Yousafzai, M.T.; Nisar, I.; Shaheen, F.; Mahesar, W.; et al. Reasons for non-vaccination and incomplete vaccinations among children in Pakistan. Vaccine. 2018, 36, 5288–5293. [Google Scholar] [CrossRef] [PubMed]
- Khowaja, A.R.; Zaman, U.; Feroze, A.; Rizvi, A.; Zaidi, A.K. Routine EPI coverage: subdistrict inequalities and reasons for immunization failure in a rural setting in Pakistan. Asia pacific journal of public health. 2015, 27, NP1050–NP9. [Google Scholar] [CrossRef] [PubMed]
- Qazi, U.; Malik, S.; Raza, U.A.; Saad, M.; Zeeshan, M.F.; Anwar, S. Compliance to timely vaccination in an Expanded Program on Immunization center of Pakistan. Vaccine. 2019, 37, 4618–4622. [Google Scholar] [CrossRef] [PubMed]
- Loulergue, P.; Pulcini, C.; Massin, S.; Bernhard, M.; Fonteneau, L.; Levy-Br€uhl, D.; Guthmann, J.P.; Launay, O. Validity of self-reported vaccination status among French healthcare students. Clinical Microbiology and Infection. 2014, 20, O1152–O1154. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.E.; Amlôt, R.; Weinman, J. ; Yiend Jenny, Rubin, G. J. systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017, 35, 6059–6069. [Google Scholar]
- Belt, R.V. ; Abdullah S, Mounier-Jack, S. ; Sodha, S.V.; Danielson, N.; Dadari I, Olayinka, F.; Ray, A.; Crocker-Buque, T. Improving Equity in Urban Immunization in Low- and Middle-Income Countries: A Qualitative Document Review. Vaccines. 2023, 11, 1200. [Google Scholar] [CrossRef]
- Dirirsa, K.; Makuria, M.; Mulu, E.; Deriba, B.S. Assessment of vaccination timeliness and associated factors among children in Toke Kutaye district, central Ethiopia: A Mixed study. Plos One. 2022, 17, e0262320. [Google Scholar] [CrossRef]
- Alghofaili M A, Aljuaid, S. O.; Alqahtani, N.; Alghufaili, M.; Abd-Ellatif, E.E. Factors Contributing to the Delayed Vaccination Among Children in Riyadh City, Saudi Arabia: A Cross-Sectional Study. Cureus. 2023, 15, e43188. [CrossRef]
- Alnumair, A.; Almulifi, A. Perceptions toward childhood vaccinations (side effects vs. benefits) among the parents living in Hail, Saudi Arabia. J Family Med Prim Care 2022, 11, 6285–6290. [Google Scholar] [CrossRef]
- Matta, P.; Mouallem, R.E.; Akel, M.; Hallit, S.; Khalife, M.F. Parents’ knowledge, attitude and practice towards children’s vaccination in Lebanon: role of the parent-physician communication.2000, 20, 1439.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).