1. Introduction
Coronavirus disease-2019 (COVID-19) represented a major global health threat. Health Systems were easily overwhelmed [
1], The world’s real number of covid 19 deaths are far more than the published data [
2]; the WHO states, in their last report, that approximately there is an excess mortality of 66% [
3].
In April 2020, during the first and devastating wave of COVID-19, Ecuador reported 10,93 deaths per million habitants, this was one of the highest mortality rates in South America at the time [
4] and was underestimated due to limitations in data acquisition and reporting [
3].
In low resource settings the number and severity of cases resulted in high mortality due to a lack of mechanical ventilators and many other medical supplies. Prioritization of patients through Triage tools were essential to give opportunity to those who had the best chance of surviving and made easier the decision to refer them to the best equipped hospitals [
5]. Triage, using simple and economic methods were warranted to perform in any situation and specially in low-resource settings [
5].
The prediction of COVID-19 severity and the initial approach were to be established In the Prehospital field and Emergency Departments as soon as possible to optimize management.
Acute respiratory distress syndrome (ARDS) was present in up to 20% of patients with COVID-19, most of them with an urgent need of mechanical ventilation [
6,
7]
Under this scenario, the ethical and professional responsibility, forced to identify specific problems, establish protocols, evaluate individual and collective risks to face the pandemic [
8]. Without any doubt there was a huge gap between offer and demand in health care and medical supplies, creating ethical dilemmas to assign resources in the best way possible [
9], this situation became worse in low-resource countries because there is inequality to access to good quality health care systems unlike in high-income countries [
10].
In Covid-19, the main concern was the rapid respiratory decompensation that led to establishing early intubation and mechanical ventilation protocols based on the increased O2 needs. [
11,
12,
13]; recognizing the right moment to intubate is important otherwise delaying this procedure could be the cause of severe complications in short time [
14,
15,
16,
17].
Patients with clinical deterioration and significant respiratory distress needed invasive protective mechanical ventilation but there is still substantial controversy about it, Xiao Lu, et al. showed that mortality was higher in Covid-19 intubated patients compared with non-intubated [
15,
18], nevertheless some authors establish the opposite [
19,
20]. This controversy maybe impacted mortality after days or weeks of invasive mechanical ventilation [
21,
22].
The available severity scores had reported underestimation when assessing the risk of death. Fan G. et al., reported in a retrospective study the predictive performance of 7 severity scores for in-hospital mortality (A-DROP, CURB-65, PSI, SMART-COP, NEWS2, CRB-65 and qSOFA) with ROC curves. The A-DROP score shown the highest discrimination in predicting in-hospital death. The NEWS2 score is easy to use and could be helpful in emergency department, but it doesn’t reflect the severity of hypoxemia and lung injury [
23,
24]
Many score scales have been used in Emergency Departments and Intensive Care Units to estimate the severity of illness and prognosis [
25]. One of the challenges Emergency physicians confront is the precision and safety in decision-making of COVID-19 patients that should be admitted to the hospital or discharged home from the ER through the application of simple, precise, and practical scales mostly in rapid and lethal conditions like this pandemic [
26].
The Ecuadorian health system was easily overwhelmed because of the high number and the severity of covid 19 patients, emergency departments and intensive care units were overloaded in a few days and could not handle the demand. This exceptional situation motivated clinicians to use clinical scales for the evaluation and management of COVID-19 patients [
27].
The necessity of early predictors to identify the clinical condition, the indication of mechanical ventilation and the vital prognosis was of high priority during the pandemic. There are many scales, as mentioned before, that had been used but with limitations in their predictive power, complex to calculate and some with laboratory data that made impossible to use them immediately in prehospital, triage and emergency departments scenarios. Certain predictive tools like the Rox Index (RI), described by Roca [
28], which express the relation between pulse oximetry/ Inspired oxygen fraction (FiO2)/ Respiratory Rate, is a useful tool in decision-making and in the immediate therapeutic management of patients [
28,
29]. Used originally for In-patients with pneumonia with acute respiratory failure treated with High flow nasal cannula (HFNC), RI can help identify those patients with low and those with high risk for intubation [
29].
Although the predictive capacity of RI is adequate, it is not high enough to be used as the sole criterion to predict failure of the HFNC, and which patients may require Invasive mechanical ventilation (IMV). Therefore, it is important to add to this tool clinical variables or serial measurements to improve the predictive value.
The objective of the present study was to evaluate the 24-hour RI variation as a noninvasive tool in the Emergency department to define the possible outcome of covid-19 patients [
15,
16] in the pandemic scenario.
2. Materials and Methods
2.1. Study Population
Between May 1 to August 31 of 2020 a total of 204 consecutive patients were admitted to the Covid-19 treatment area in a reference second-level hospital in Quito (2850 m) altitude. Patients were admitted to the study if they had the following inclusion criteria: age 18 or older, met any of the clinical WHO criteria for Covid-19, a positive PCR-rt test, or chest CT scan result highly suspicious (CoRads 4-5) of Covid-19.
The protocol was approved by the ethics committee MSP-CZ9HGDC-2021-0700-O.
No intervention was made in this research, there is no individual identification data shown, data were obtained from the clinical records. There was no need for informed consent.
2.2. Information Collected
In 204 patients with confirmed Covid-19 infection, respiratory parameters like inspired O2 fraction, Respiratory frequency, O2 Saturation were registered, and RI calculated as the relation between O2 (Saturation/Fi O2) / Respiratory frequency, in real-time at admission and 24 hours later were calculated and registered. Other analysed variables were presence of comorbidities, radiologic and tomographic compromise, disease duration, and hospitalization time. The main outcomes were death and mechanic ventilation.
The information was prospectively collected and registered in an excel data base.
2.3. Analysis Plan:
Description of respiratory parameters was made presenting means and standard deviations of each parameter at entry and 24 hours later, differences in respiratory parameters between those whosurvived and those who deceased or those who need and did not need mechanic ventilation were tested using T-test with correction for unequal standard deviation when necessary. ROC curves analysis for each respiratory parameter and the Rox-index difference were settled to calculate under the curve AUC either to explore association with death and mechanic ventilation. Difference between entry and 24h respiratory ROX index was explored by subtracting entry minus 24h values. Cut offs for parameters were obtained by calculating the Youden index for each analysed parameter. A ROC analysis was performed to built up a logistic regression model adjusting for age, sex, presence of comorbidities and disease severity.
To analyse if the improving or waning in 24 hours RI difference, the RI scores were categorized as: >20 = normal respiratory function; 15-19 = mild respiratory deterioration; 10-14.9 = moderate respiratory deterioration; and <10 severe respiratory function deterioration. This arbitrary classification is based on normal values for Quito altitude. Logistic regression analysis was used to explore association between the change of RI using the improving status (change from a worse to better category) as basal compared with those who did not change of category, or with those who deteriorate the RI from one category to the next worse level, or with those who deteriorate more than 1 category. The logistic regression model was adjusted by age, sex, comorbidities, and radiologic severity. The results were also, explored to investigate if the change of RI category was modified by sex, age, presence or comorbidity and radiologic severity.
3. Results
3.1. Characteristics of the Population
A total of 204 patients were admitted to the Hospital with a Covid-19 diagnosis. The mean age was 57 years and 60% were male. Eighty-eight patients (43%) had comorbidities, the most frequent were hypertension and diabetes mellitus. Fever, cough, dyspnea, and malaise-myalgia were the most common symptoms. Most patients (93%) had a tomographic highly suspicious pulmonary affectation according to the imagen Co-Rads classification. Approximately one quarter of patients required mechanical ventilation, and 56 patients (27%) died (
Table 1).
3.2. Respiratory Associated Factors for Death and Mechanical Ventilation
The saturation O2 levels were statistically higher at entry and 24h later in those patients who survived than those who did not, and in those who required mechanical ventilation when compared with those who did not. Oxygen inspired fraction (FiO2) administered levels and respiratory frequency were statistically higher in deceased patients and in those requiring mechanical ventilation both at entry and after 24h. RI values were significantly higher at entry and 24 later in patients who survived and those who did not need mechanical ventilation. Difference in RI values were negative in survivors and in those who did not require mechanic ventilation. These differences were statistically higher, showing deterioration of RI, in those who did not survive and those who had mechanic ventilation (
Table 2).
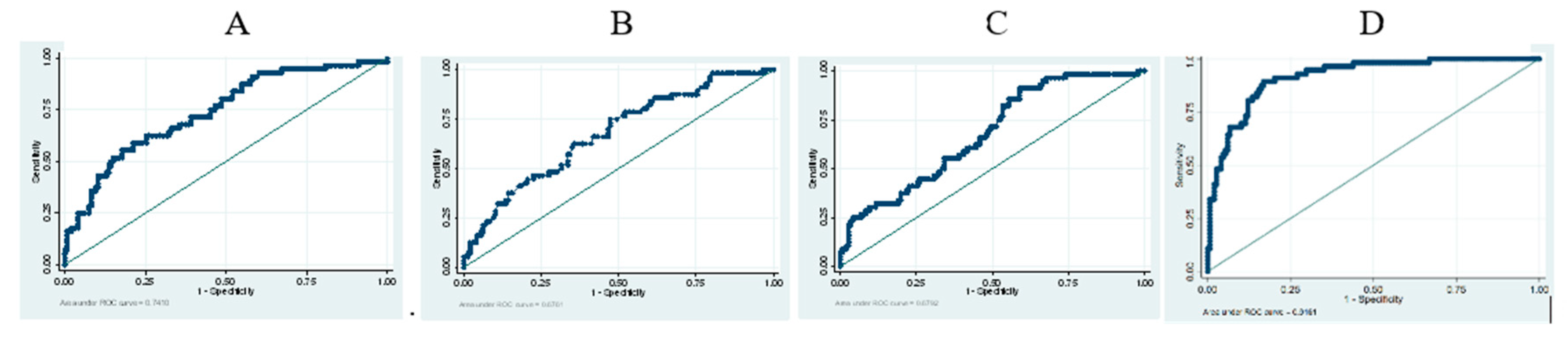
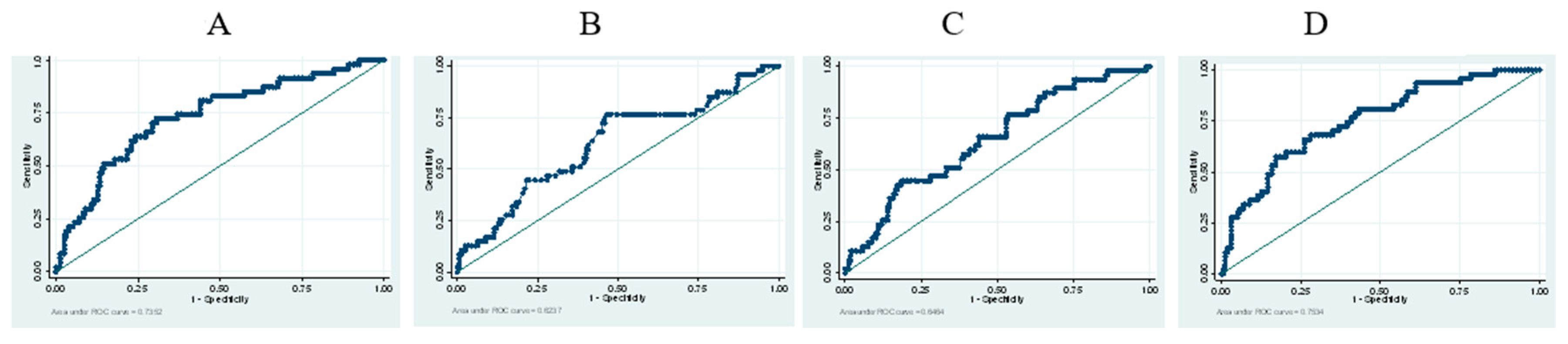
3.3. Prediction Analysis of Respiratory Parameters and Difference between RI at Entry versus 24h later for Risk of Death and Mechanical Ventilation
Difference in respiratory RI at entry versus 24h is a better predictor for death AUC 0.92 than for a mechanical ventilation predictor AUC: 0.75 (
Table 3) (
Figure 1 and
Figure 2). Each decrease in one unit of difference of RI means increasing in 48% and 16% the risk of death and mechanical ventilation respectively. Odds ratio for death risk: 1.48 (95%CI: 1.31-1.67) and for mechanical ventilation: 1.16 (95%IC: 1.1-1.23), after adjustment for age, sex, comorbidities, and severity of the disease.
3.4. Association between 24 hs Changes in Respiratory ROX Index and Death
A greater proportion of patients were admitted with moderate to severe respiratory deterioration (62%), and 24 hs later around 39% of patients were in those categories. In the same way, a minority of patients were admitted with normal respiratory function, but this increased 24 hs later (
Table 4).
The higher the deterioration in 24 hs in RI score, the higher the likelihood of death or need for mechanic support. Even, in the absence of change in the first 24 hs, there is a statistically increase in possibility of death and ventilatory support, compared with those who improve RI scores in the first 24 hs. The possibility of death and mechanical ventilation increase when the deterioration of RI is even higher. This association was independent of age, sex, disease severity and presence of comorbidities, there was no modification effect in this association due to these confounders (
Table 5).
4. Discussion
The Rox Index is a valuable tool for quick evaluation of the condition of Covid 19 patients, at admission it has a good prognostic value AUC of 78.6 to predict mortality and 76.1 for mechanical ventilation. Once stabilization and initial treatment are set up, a 24h ROX index variation became an even better prognostic tool with an AUC of 92 and 75 for mortality and mechanical ventilation respectively; this also shows that a 24h improvement in functional respiratory category is associated with survival and no need for mechanical ventilation.
In a health disaster like this pandemic [
30], conceptually, the healthcare provider’s efforts should be directed to those with the better chance to survive [
31], especially in low resource settings or countries where infrastructure is poor and access to respiratory equipment and supplies like HFNC and NIV was very difficult. As far as we have searched the literature there are few publications about the value of the RI to predict mortality or mechanical ventilation in COVID-19 patients [
32,
33]. Vega et al., establish that RI is a useful tool to guide intubation specially in moderate respiratory categories and Basoulis et al., also shows that a 12h RI is useful to predict mortality. The 24 h RI difference seems to be a good tool to differentiate between those who will survive and allows to direct resources and therapy in the right way, but maybe this is a long interval to improve or change therapeutic measures, maybe trying to calculate the RI difference in shorter periods could have a prognostic benefit for individuals.
This research was conducted in Quito, 204 consecutive patients were enrolled during the critical period of the pandemic. We identified some limitations, first this was a monocentric study, and although it was a public center patients characteristics might not be similar as in other healthcare facilities. Second Quito is a high-altitude city (2850 m) it represents a special environmental situation, the habitants of high altitude usually develop hypocapnic hypoxia and have respiratory rates higher than the sea level. The equation to calculate the RI has three components: Oxygen saturation, oxygen inspired fraction and respiratory rate, the component that keeps the same between high altitude and sea level is inspired oxygen fraction (0.21) [
34,
35], due to this we arbitrarily introduced four groups of the Rox index based on the normal parameters for Quito (
Table 4) this may become a source of bias during the analysis, as a reference Gianstefany et al., describe sea level values higher than those in Quito [
26] and are useful to contrast the data shown in our analysis, for instance the cut off for ambulatory care in Gianstefany research 26 different from 20 in our study.
We describe 4 categories that translate different stages of respiratory compromise in patients with covid-19 pneumonia, from normal to severely compromised respiratory function, if patients don’t improve the index value in 24h after implementing all the initial treatment and, even worse, if they deteriorate one or two categories (adjusted OR for deaths was 38 y 674, respectively) the outcome is worse increasing mechanical ventilation needs and mortality. The greater OR values were explained by the small numbers of analyzed patients in that category, however, even in the small numbers, the trend for association between respiratory deterioration and death or ventilator support were consistent.
Patients with Rox Index at admission superior to 20 or those who improved their Rox Index in 24h were assigned to observation or discharged for ambulatory treatment.
The in-hospital mortality was 27% (56/204) with a LOS of 7.27 days on average, the Rox index in this group deteriorated from 9.8 to 4.9 showing the rapid progress and severity of the disease. Twelve of the discharged patients died at home after being discharged from the hospital 10 of them improve the 24h Rox Index difference and only 2 deteriorated, maybe this group of patients has died because of complications of the disease but this analysis is out of the scope of this report.
5. Conclusions
Rox Index at the admission of covid 19 pneumonia patients, is an easy and quick to apply scale that has same or more accurate prediction than other scales used to predict the severity and outcome when used in Emergency departments. Interestingly, even more accurately, the 24h difference of RI has the potential to predict the outcome of patients and who benefit from intensive measures in a scenario of a healthcare disaster like this pandemic.
More research on this topic is needed to understand and take the best decisions for patients specially in low-resource settings where equipment is scarce and infrastructure is poor.
Limitations
This research is monocentric, conducted in a high-altitude city like Quito and probably introduces some bias in the analysis.
Author Contributions
Augusto Maldonado: Research Idea and design, recruitment individuals, data analysis, bibliographic search, composition, and final text revision. Pablo Endara: Research design, statistical analysis, bibliography search, composition of the final text. Patricio Abril: Bibliographic search, composition, and final text revision, recruitment individuals. Henry Carrion: Bibliographic search, composition, and final text revision. Carolina Largo: Bibliographic search, composition. Patricia Benavides: Administrative coordination, Bibliographic search, final text revision.
Conflicts of Interest
The authors declare that there is no conflict of interest in this research.
References
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA - J. Am. Med. Assoc. 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Blumenthal, D.; Fowler, E.J.; Abrams, M.; Collins, S.R. Covid-19 — Implications for the Health Care System. New Engl. J. Med. 2020, 383, 1483–1488. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global excess deaths associated with COVID-19, January 2020 - December 2021 [Internet]. WHO. 2022 [cited 2022 Jun 19]. Available from: https://www.who.int/data/stories/global-excess-deaths-associated-with-covid-19-january-2020-december-2021.
- Torres, I.; Sacoto, F. Localising an asset-based COVID-19 response in Ecuador. Lancet 2020, 395, 1339–1339. [Google Scholar] [CrossRef] [PubMed]
- Hasanin, A.; de Vasconcellos, K.; Abdulatif, M. COVID-19 in Africa: Current difficulties and future challenges considering the ACCCOS study. Anaesth. Crit. Care Pain Med. 2021, 40, 100912–100912. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Center for Systems Science and Engineering. Coronavirus COVID-19 (2019-nCoV).
- Izaguirre, M. La pandemia COVID-19 y la salud global desde la perspectiva de la bioética crítica. Anales de la Facultad de Medicina. 2021 Apr 15;81(4).
- Hidalgo MR, Copaja-Corzo C, Carrasco-Espinoza AI, Pérez-Bacigalupo DA. Asignación de recursos médicos en tiempos de COVID-19: un enfoque bioético. Revista Médica Basadrina [Internet]. 2021 Apr 30 [cited 2022 Jan 15];15(2):73–9. Available from: http://www.revistas.unjbg.edu.pe/index.php/rmb/article/view/1056.
- Okereke, M.; Ukor, N.A.; Adebisi, Y.A.; Ogunkola, I.O.; Iyagbaye, E.F.; Owhor, G.A.; Lucero-Prisno, D.E. Impact of COVID-19 on access to healthcare in low- and middle-income countries: Current evidence and future recommendations. Int. J. Heal. Plan. Manag. 2020, 36, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.C.-H.; Ho, L.T.; Cheng, J.V.; Cham, E.Y.K.; Lam, K.N. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir. Med. 2020, 8, e19–E19. [Google Scholar] [CrossRef] [PubMed]
- Dar M, Swamy L, Gavin D, Theodore A. FOCUSED REVIEWS Mechanical-Ventilation Supply and Options for the COVID-19 Pandemic Leveraging All Available Resources for a Limited Resource in a Crisis. atsjournals.org Ann Am Thorac Soc [Internet]. 2021;18(3):408–16. Available from: www.atsjournals.org.
- Meng, L.; Qiu, H.; Wan, L.; Ai, Y.; Xue, Z.; Guo, Q.; Deshpande, R.; Zhang, L.; Meng, J.; Tong, C.; et al. Intubation and Ventilation amid the COVID-19 Outbreak. Anesthesiology 2020, 132, 1317–1332. [Google Scholar] [CrossRef]
- Mohammed Sheata I, Smith SR, Kamel H, Varrassi G, Imani F, Dayani A, et al. Pulmonary Embolism and Cardiac Tamponade in Critical Care Patients with COVID-19; Telemedicine’s Role in Developing Countries: Case Reports and Literature Review. Anesth Pain Med. 2021, 11. [Google Scholar]
- Mohammadi M, Khafaee Pour Khamseh A, Varpaei HA. Invasive Airway “Intubation” in COVID-19 Patients; Statistics, Causes, and Recommendations: A Review Article. Anesth Pain Med. 2021, 11. [Google Scholar]
- Patel M, Chowdhury J, Mills N do, Marron R, Gangemi A, Dorey-Stein Z, et al. ROX Index Predicts Intubation in Patients with COVID-19 Pneumonia and Moderate to Severe Hypoxemic Respiratory Failure Receiving High Flow Nasal Therapy. medRxiv [Internet]. 2020 Jul 3 [cited 2022 Jan 15];2020.06.30.20143867. Available from: https://www.medrxiv.org/content/10.1101/2020.06.30.20143867v2.
- Roca, O.; Caralt, B.; Messika, J.; Samper, M.; Sztrymf, B.; Hernández, G.; García-De-Acilu, M.; Frat, J.-P.; Masclans, J.R.; Ricard, J.-D. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. Am. J. Respir. Crit. Care Med. 2019, 199, 1368–1376. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Zhang, M.; Qian, A.; Tang, L.; Xu, S. Lung ultrasound score in establishing the timing of intubation in COVID-19 interstitial pneumonia: A preliminary retrospective observational study. PLOS ONE 2020, 15, e0238679. [Google Scholar] [CrossRef] [PubMed]
- González, J.; Benítez, I.D.; de Gonzalo-Calvo, D.; Torres, G.; de Batlle, J.; Gómez, S.; Moncusí-Moix, A.; Carmona, P.; Santisteve, S.; Monge, A.; et al. Impact of time to intubation on mortality and pulmonary sequelae in critically ill patients with COVID-19: a prospective cohort study. Crit. Care 2022, 26, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ball, L.; Robba, C.; Herrmann, J.; Gerard, S.E.; Xin, Y.; Pigati, M.; Berardino, A.; Iannuzzi, F.; Battaglini, D.; Brunetti, I.; et al. Early versus late intubation in COVID-19 patients failing helmet CPAP: A quantitative computed tomography study. Respir. Physiol. Neurobiol. 2022, 301, 103889–103889. [Google Scholar] [CrossRef] [PubMed]
- Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Arentz, M.; Yim, E.; Klaff, L.; Lokhandwala, S.; Riedo, F.X.; Chong, M.; Lee, M. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA 2020, 323, 1612–1614. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.; Tu, C.; Zhou, F.; Liu, Z.; Wang, Y.; Song, B.; Gu, X.; Wang, Y.; Wei, Y.; Li, H.; et al. Comparison of severity scores for COVID-19 patients with pneumonia: a retrospective study. Eur. Respir. J. 2020, 56, 2002113. [Google Scholar] [CrossRef]
- Prower, E.; Grant, D.; Bisquera, A.; Breen, C.P.; Camporota, L.; Gavrilovski, M.; Pontin, M.; Douiri, A.; Glover, G.W. The ROX index has greater predictive validity than NEWS2 for deterioration in Covid-19. EClinicalMedicine 2021, 35, 100828–100828. [Google Scholar] [CrossRef] [PubMed]
- González ADR, Vázquez LV, Malmierca AB, Gómez IV, Adán AM, Santana RSD. APACHE II como predictor de mortalidad en una unidad de cuidados intensivos. Revista Cubana de Medicina Intensiva y Emergencias [Internet]. 2020 Oct 25 [cited 2022 Jan 15];19(3). Available from: http://www.revmie.sld.cu/index.php/mie/article/view/739.
- Gianstefani A, Artesiani ML, Nava S. Role of ROX Index in the first assessment of COVID-19 patients in the Emergency Department. 2020 Nov 17 [cited 2022 Jan 15]; Available from: https://www.researchsquare.com.
- Ioannidis JPA. Global perspective of COVID-19 epidemiology for a full-cycle pandemic. Eur J Clin Invest. 2020, 50, e13423. [Google Scholar] [CrossRef]
- Roca, O.; Messika, J.; Caralt, B.; García-De-Acilu, M.; Sztrymf, B.; Ricard, J.-D.; Masclans, J.R. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J. Crit. Care 2016, 35, 200–205. [Google Scholar] [CrossRef]
- Mauri, T.; Carlesso, E.; Spinelli, E.; Turrini, C.; Corte, F.D.; Russo, R.; Ricard, J.-D.; Pesenti, A.; Roca, O.; Grasselli, G. Increasing support by nasal high flow acutely modifies the ROX index in hypoxemic patients: A physiologic study. J. Crit. Care 2019, 53, 183–185. [Google Scholar] [CrossRef]
- Powell, T.; Christ, K.C.; Birkhead, G.S. Allocation of Ventilators in a Public Health Disaster. Disaster Med. Public Heal. Prep. 2008, 2, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Afolabi, MO. Public Health Disasters. In: Advancing Global Bioethics. Springer Science and Business Media B.V.; 2018. p. 1–24.
- Vega ML, Dongilli R, Olaizola G, Colaianni N, Sayat MC, Pisani L, et al. COVID-19 Pneumonia and ROX index: Time to set a new threshold for patients admitted outside the ICU. Pulmonology. 2022, 28, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Basoulis, D.; Avramopoulos, P.; Aggelara, M.; Karamanakos, G.; Voutsinas, P.-M.; Karapanou, A.; Psichogiou, M.; Samarkos, M.; Ntziora, F.; Sipsas, N.V. Validation of Sequential ROX-Index Score Beyond 12 Hours in Predicting Treatment Failure and Mortality in COVID-19 Patients Receiving Oxygen via High-Flow Nasal Cannula. Can. Respir. J. 2023, 2023, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Camayo, J.; Mejia, C.R.; Callacondo, D.; A Dawson, J.; Posso, M.; Galvan, C.A.; Davila-Arango, N.; Bravo, E.A.; Loescher, V.Y.; Padilla-Deza, M.M.; et al. Reference values for oxygen saturation from sea level to the highest human habitation in the Andes in acclimatised persons. Thorax 2017, 73, 776–778. [Google Scholar] [CrossRef]
- West, JB. High-altitude medicine. American Journal of Respiratory and Critical Care Medicine. 2012, 186, 1229–1237. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).