Submitted:
25 March 2024
Posted:
26 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
3.1. Health Impacts and Urbanization
3.1.1. Climate, Health and the Urban Poor
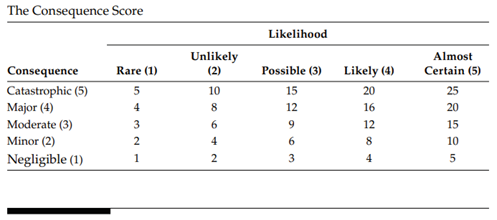
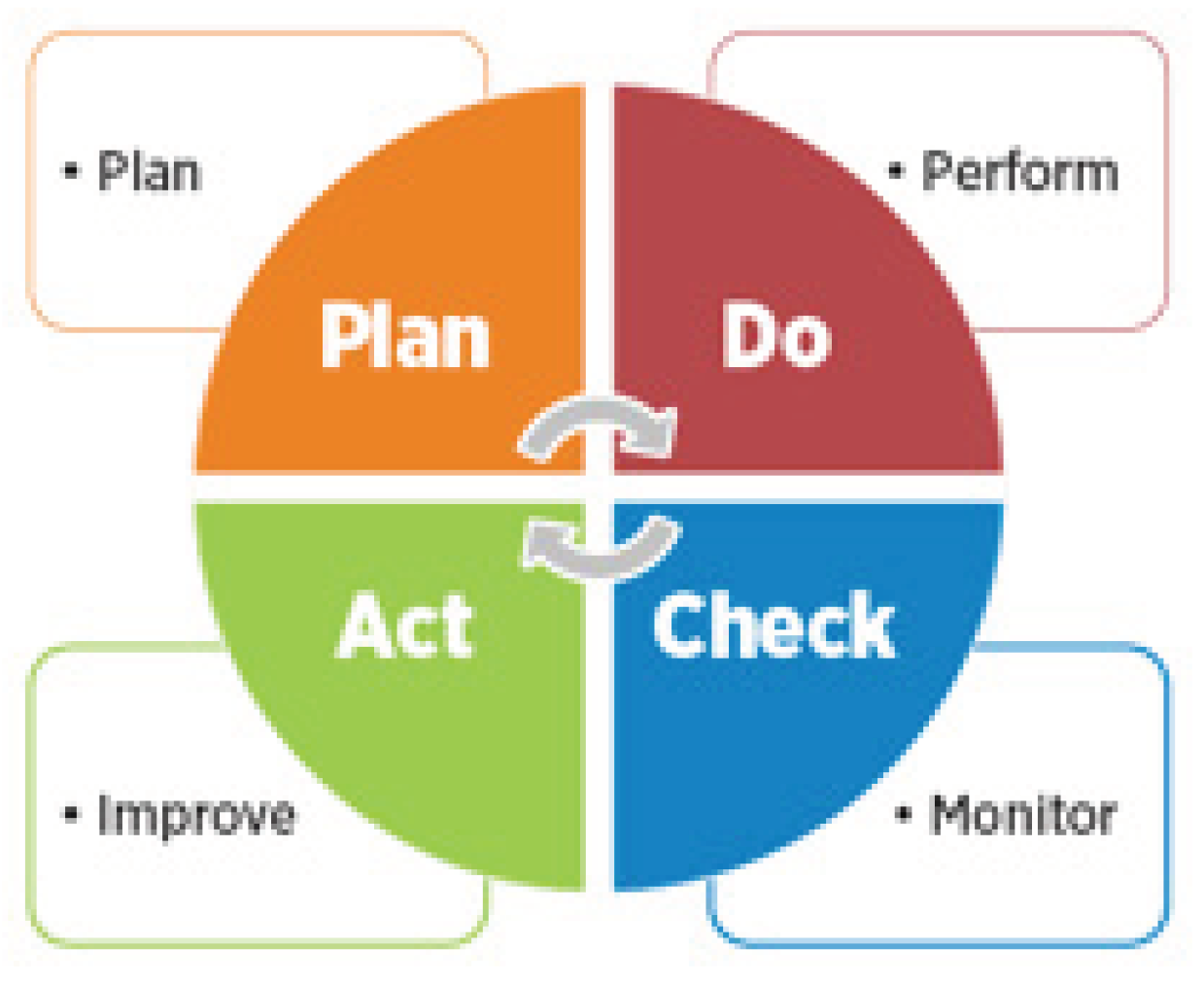
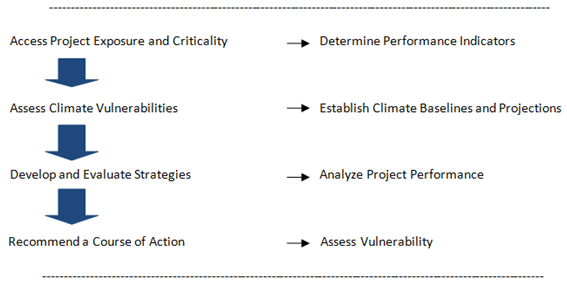
4.1. The Nexus between Climate, Health and Risk Management
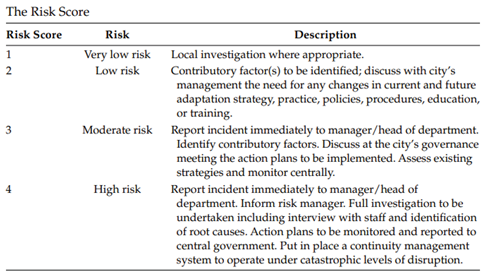
4.1. Rapid Risk Assessment for Health Care
5. Discussion
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rocha, J. , Oliveira, S., Viana, C.M., Ribeiro, A.I., Chapter 8 - Climate change and its impacts on health, environment and economy, Editor(s): Joana C. Prata, Ana Isabel Ribeiro, Teresa Rocha-Santos, One Health, Academic Press, 2022, Pages 253-279, ISBN 9780128227947. [CrossRef]
- Nadakavukaren, Anne, and Jack Caravanos. Our global environment: A health perspective. Waveland Press, 2020.
- Salimi, M.; Al-Ghamdi, S.G. Climate change impacts on critical urban infrastructure and urban resiliency strategies for the Middle East. Sustain. Cities Soc. 2019, 54, 101948. [Google Scholar] [CrossRef]
- Leichenko, Robin, and Julie A. Silva. “Climate change and poverty: vulnerability, impacts, and alleviation strategies.” Wiley Interdisciplinary Reviews: Climate Change 5, no. 4. 2014: 539-556.
- El-Sayed, A.; Kamel, M. Climatic changes and their role in emergence and re-emergence of diseases. Environ. Sci. Pollut. Res. 2020, 27, 22336–22352. [Google Scholar] [CrossRef] [PubMed]
- Ebi, Kristie L., and Jeremy J. Hess. “Health Risks Due To Climate Change: Inequity In Causes And Consequences: Study examines health risks due to climate change.” Health Affairs 39, no. 12 (2020): 2056-2062.
- Rodriguez, A. et al. Impact of climate change on health and disease in Latin America. Faculty of Medicine, Universidad Central de Venezuela. pp. 12–15. 2009.
- van der Merwe, Eduard, Matthew Clance, and Eleni Yitbarek. “Climate change and child malnutrition: a Nigerian perspective.” Food Policy 113. 2022: 102281.
- Jankowska, M.M.; Lopez-Carr, D.; Funk, C.; Husak, G.J.; Chafe, Z.A. Climate change and human health: Spatial modeling of water availability, malnutrition, and livelihoods in Mali, Africa. Appl. Geogr. 2011, 33, 4–15. [Google Scholar] [CrossRef]
- Wilbanks, T. , Steven Fernandez, G. Backus, P. Garcia, K. Jonietz, P. Kirshen, M. Savonis, W. Solecki, and L. Toole. “Climate change and infrastructure, urban systems.” In And Vulnerabilities: Technical Report for the US Department of Energy in Support of the National Climate Assessment. 2013.
- Najafi, M.R.; Zhang, Y.; Martyn, N. A flood risk assessment framework for interdependent infrastructure systems in coastal environments. Sustain. Cities Soc. 2020, 64, 102516. [Google Scholar] [CrossRef]
- Jurgilevich, A.; Räsänen, A.; Juhola, S. Assessing the dynamics of urban vulnerability to climate change: Case of Helsinki, Finland. Environ. Sci. Policy 2021, 125, 32–43. [Google Scholar] [CrossRef]
- D’amato, G.; Chong-Neto, H.J.; Ortega, O.P.M.; Vitale, C.; Ansotegui, I.; Rosario, N.; Haahtela, T.; Galan, C.; Pawankar, R.; Murrieta-Aguttes, M.; et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy 2020, 75, 2219–2228. [Google Scholar] [CrossRef]
- Caminade, C.; Kovats, S.; Rocklov, J.; Tompkins, A.M.; Morse, A.P.; Colón-González, F.J.; Stenlund, H.; Martens, P.; Lloyd, S.J. Impact of climate change on global malaria distribution. Proc. Natl. Acad. Sci. 2014, 111, 3286–3291. [Google Scholar] [CrossRef]
- Lafferty, K.D. The ecology of climate change and infectious diseases. Ecology 2009, 90, 888–900. [Google Scholar] [CrossRef]
- Gilioli, G.; Mariani, L. Sensitivity of Anopheles gambiae population dynamics to meteo-hydrological variability: a mechanistic approach. Malar. J. 2011, 10, 294–294. [Google Scholar] [CrossRef] [PubMed]
- Confalonieri, Ulisses EC, and Flávia RL Suassuna Dutra. “Climate Change and Vector Borne Diseases in Latin America.” Environmental Deterioration and Human Health: Natural and anthropogenic determinants. 2014: 315-324.
- Duval, Laetitia. “Climate Change, Vector-Borne Diseases, and Migration.” In Handbook of Labor, Human Resources and Population Economics, pp. 1-15. Cham: Springer International Publishing, 2022.
- World Health Organization [WHO]. Global Report for Research on Infectious Diseases of Poverty. World Health Organization on Behalf of the Special Programme for Research and Training in Tropical Diseases 2012. http://apps.who.int/iris/bitstream/10665 /44850/1/9789241564489_eng.pdf.
- Hallegatte, Stephane, Jun Rentschler, and Julie Rozenberg. “Adaptation principles: a guide for designing strategies for climate change adaptation and resilience.” 2020.
- Strauss, B.H.; Orton, P.M.; Bittermann, K.; Buchanan, M.K.; Gilford, D.M.; Kopp, R.E.; Kulp, S.; Massey, C.; de Moel, H.; Vinogradov, S. Economic damages from Hurricane Sandy attributable to sea level rise caused by anthropogenic climate change. Nat. Commun. 2021, 12, 1–9. [Google Scholar] [CrossRef]
- Suter, M.A.; Aagaard, K.M. Natural disasters resulting from climate change: The impact of hurricanes and flooding on perinatal outcomes. Semin. Perinatol. 2023, 47, 151840. [Google Scholar] [CrossRef] [PubMed]
- Kookana, R.S.; Drechsel, P.; Jamwal, P.; Vanderzalm, J. Urbanisation and emerging economies: Issues and potential solutions for water and food security. Sci. Total. Environ. 2020, 732, 139057. [Google Scholar] [CrossRef] [PubMed]
- Dickson, E. et al. Understanding urban risk: An approach for assessing disaster and climate risk in cities. World Bank. 2011.
- Gu, D.; Andreev, K.; Dupre, M.E. Major Trends in Population Growth Around the World. China CDC Wkly. 2021, 3, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Castells-Quintana, David, and Hugh Wenban-Smith. “Population dynamics, urbanisation without growth, and the rise of megacities.” The Journal of Development Studies 56, no. 9; 2020: 1663-1682.
- Sharifi, A.; Pathak, M.; Joshi, C.; He, B.-J. A systematic review of the health co-benefits of urban climate change adaptation. Sustain. Cities Soc. 2021, 74, 103190. [Google Scholar] [CrossRef]
- Feiden, P. Adapting to climate change: Cities and the urban poor. International Housing Coalition. 2011.
- Twinomuhangi, R.; Sseviiri, H.; Mulinde, C.; Mukwaya, P.I.; Nimusiima, A.; Kato, A.M. Perceptions and vulnerability to climate change among the urban poor in Kampala City, Uganda. Reg. Environ. Chang. 2021, 21, 1–13. [Google Scholar] [CrossRef]
- Griggs, G.; Reguero, B.G. Coastal Adaptation to Climate Change and Sea-Level Rise. Water 2021, 13, 2151. [Google Scholar] [CrossRef]
- Rose, E. A sinking world: A model framework for climate change adaptation measures in coastal cities. Vand. J. Transnat’l L.. 2020;53:367.
- Doberstein, B.; Tadgell, A.; Rutledge, A. Managed retreat for climate change adaptation in coastal megacities: A comparison of policy and practice in Manila and Vancouver. J. Environ. Manag. 2019, 253, 109753. [Google Scholar] [CrossRef]
- Dodman D, Hayward B, Pelling M, Castan Broto V, Chow W, Chu E, Dawson R, Khirfan L, McPhearson T, Prakash A, Zheng Y. Cities, Settlements and Key Infrastructure Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. 2022.
- Sharifi, A. Co-benefits and synergies between urban climate change mitigation and adaptation measures: A literature review. Sci. Total. Environ. 2020, 750, 141642. [Google Scholar] [CrossRef]
- Smiley, K.T.; Noy, I.; Wehner, M.F.; Frame, D.; Sampson, C.C.; Wing, O.E.J. Social inequalities in climate change-attributed impacts of Hurricane Harvey. Nat. Commun. 2022, 13, 1–10. [Google Scholar] [CrossRef]
- Agache, I.; Sampath, V.; Aguilera, J.; Akdis, C.A.; Akdis, M.; Barry, M.; Bouagnon, A.; Chinthrajah, S.; Collins, W.; Dulitzki, C.; et al. Climate change and global health: A call to more research and more action. Allergy 2022, 77, 1389–1407. [Google Scholar] [CrossRef] [PubMed]
- Kaczan, D.J.; Orgill-Meyer, J. The impact of climate change on migration: a synthesis of recent empirical insights. Clim. Chang. 2019, 158, 281–300. [Google Scholar] [CrossRef]
- Salm, L.; Nisbett, N.; Cramer, L.; Gillespie, S.; Thornton, P. How climate change interacts with inequity to affect nutrition. WIREs Clim. Chang. 2020, 12. [Google Scholar] [CrossRef]
- Islam, Nazrul, and John Winkel. Climate change and social inequality. 2017.
- Sam, A.G.; Abidoye, B.O.; Mashaba, S. Climate change and household welfare in sub-Saharan Africa: empirical evidence from Swaziland. Food Secur. 2020, 13, 439–455. [Google Scholar] [CrossRef]
- Halder, B.; Bandyopadhyay, J. Evaluating the impact of climate change on urban environment using geospatial technologies in the planning area of Bilaspur, India. Environ. Challenges 2021, 5, 100286. [Google Scholar] [CrossRef]
- Twinomuhangi, R.; Sseviiri, H.; Mulinde, C.; Mukwaya, P.I.; Nimusiima, A.; Kato, A.M. Perceptions and vulnerability to climate change among the urban poor in Kampala City, Uganda. Reg. Environ. Chang. 2021, 21, 1–13. [Google Scholar] [CrossRef]
- Kogo, B.K.; Kumar, L.; Koech, R. Climate change and variability in Kenya: a review of impacts on agriculture and food security. Environ. Dev. Sustain. 2020, 23, 23–43. [Google Scholar] [CrossRef]
- Holleman, Cindy, Felix Rembold, Olivier Crespo, and Valentina Conti. “The impact of climate variability and extremes on agriculture and food security-An analysis of the evidence and case studies.”. 2020.
- Wilbanks, T. , Steven Fernandez, G. Backus, P. Garcia, K. Jonietz, P. Kirshen, M. Savonis, W. Solecki, and L. Toole. “Climate change and infrastructure, urban systems.” In And Vulnerabilities: Technical Report for the US Department of Energy in Support of the National Climate Assessment. 2013.
- Allan, Richard P., Paola A. Arias, Sophie Berger, Josep G. Canadell, Christophe Cassou, Deliang Chen, Annalisa Cherchi et al. “Intergovernmental Panel on Climate Change (IPCC). Summary for Policymakers.” In Climate change 2021: The physical science basis. Contribution of working group I to the sixth assessment report of the intergovernmental panel on climate change, pp. 3-32. Cambridge University Press, 2023.
- Hughes, Sara, Eric K. Chu, and Susan G. Mason. Climate change and cities. Oxford: Oxford University Press, 2020.
- Marolla, Cesar. Climate Change Impacts on Health: The Urban Poor in the World’s Megacities. Harvard Division of Continuing Education. DASH, Harvard Library Office for Scholarly Communication. 2020.
- Marolla, C. Climate Health Risks in Megacities; Taylor & Francis Ltd: London, United Kingdom, 2016; ISBN 9781315367323. [Google Scholar]
- Almadani, B.; Aliyu, F.; Aliyu, A. Integrated Operation Centers in Smart Cities: A Humanitarian Engineering Perspective. Sustainability 2023, 15, 11101. [Google Scholar] [CrossRef]
- Owen, G. What makes climate change adaptation effective? A systematic review of the literature. Glob. Environ. Chang. 2020, 62, 102071. [Google Scholar] [CrossRef]
- Rydin, Y.; Bleahu, A.; Davies, M.; Dávila, J.D.; Friel, S.; De Grandis, G.; Groce, N.; Hallal, P.C.; Hamilton, I.; Howden-Chapman, P.; et al. Shaping cities for health: complexity and the planning of urban environments in the 21st century. Lancet 2012, 379, 2079–2108. [Google Scholar] [CrossRef] [PubMed]
- Smith, AB. 2010–2019: A landmark decade of US. billion-dollar weather and climate disasters. National Oceanic and Atmospheric Administration. 2020 Jan 8.
- Barata, M. , Ligeti, E., De Simone, G., Dickinson, T., Jack, D., Penney, J., Rahman, M., and Zimmerman, R. Climate change and human health in cities. In C. Rosenzweig, W. Solecki, S. A. Hammer, and S. Mehrotra (Eds.), Climate change and cities: First assessment report of the Urban Climate Change Research Network, 2011; pp. 183–217. Cambridge: Cambridge University Press.
- Ebi, K.L.; Semenza, J.C. Community-Based Adaptation to the Health Impacts of Climate Change. Am. J. Prev. Med. 2008, 35, 501–507. [Google Scholar] [CrossRef] [PubMed]
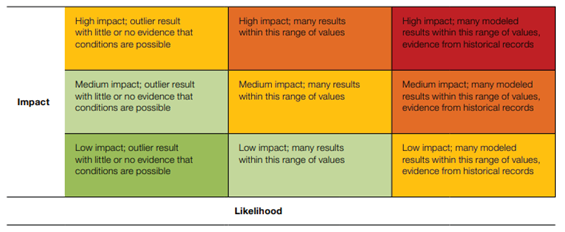
- Jones, R. N. , and Preston, B. L. Adaptation and risk management. Working Paper No. 15, Centre for Strategic Economic Studies, 2010. Victoria University, Melbourne.
- Oppenheimer, M. et al. The limits of consensus. Science, 317(5844), 1505– 1506; 2007. Retrieved from http://www.sciencemag.org/content/317/5844/1505.full.
- Moser, S.C.; Ekstrom, J.A. A framework to diagnose barriers to climate change adaptation. Proc. Natl. Acad. Sci. 2010, 107, 22026–22031. [Google Scholar] [CrossRef] [PubMed]
- Adger, W. N. Vulnerability. Global Environmental Change, 16, 268–281; 2006.
- Spickett, J.T.; Brown, H.L.; Katscherian, D. Adaptation strategies for health impacts of climate change in Western Australia: Application of a Health Impact Assessment framework. Environ. Impact Assess. Rev. 2011, 31, 297–300. [Google Scholar] [CrossRef]
- Ebi KL, Berry P, Campbell-Lendrum D, Cissé G, Hess J, Ogden N, Schnitter R. Health system adaptation to climate variability and change. Washington, DC: Global Center on Adaptation. 2019 Dec 2.
- Caldecott, B. Climate risk management (CRM) and how it relates to achieving alignment with climate outcomes (ACO). J. Sustain. Finance Invest. 2020, 12, 1167–1170. [Google Scholar] [CrossRef]
- World Bank: Climate Resilient Investment in Sub-Saharan Africa Compendium Volume – A Focus on Infrastructure Project Design in Key Sectors. 2023. World Bank. Washington D.C. The report was prepared in collaboration with Industrial Economics Inc. under the Africa Climate Resilient Investment Facility (AFRI-RES) program.
- Prats, Elena Villalobos. WHO guidance for climate-resilient and environmentally sustainable health care facilities. World Health Organization, 2020.
- Agency for Health Care and Quality, Plan-Do-Check-Act Cycle. 2022. https://digital.ahrq.
- Pojasek, R.B. Organizational Risk Management and Sustainability: A Practical Step-by Step Guide (1st ed.). 2016. CRC Press. [CrossRef]
- Kazantzidou Firtinidou D, Gkotsis I, Eftychidis G, Sfetsos A, Petrovic N, Stranjik A. Climate Related Business Continuity Model for Critical Infrastructures. Annals of Disaster Risk Sciences: ADRS. 2019 Dec 28;2(1-2):11-27.
- Ray, P.A.; Brown, C.M. Confronting Climate Uncertainty in Water Resources Planning and Project Design: The Decision Tree Framework; World Bank: Washington, DC, USA, 2015. [Google Scholar]
- Gallina, V.; Torresan, S.; Critto, A.; Sperotto, A.; Glade, T.; Marcomini, A. A review of multi-risk methodologies for natural hazards: Consequences and challenges for a climate change impact assessment. J. Environ. Manag. 2016, 168, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Izaguirre, C.; Losada, I.J.; Camus, P.; Vigh, J.L.; Stenek, V. Climate change risk to global port operations. Nat. Clim. Chang. 2021, 11, 14–20. [Google Scholar] [CrossRef]
- Gale, P.; Estrada-Peã±A, A.; Martinez, M.; Ulrich, R.; Wilson, A.; Capelli, G.; Phipps, P.; De La Torre, A.; Muã±Oz, M.; Dottori, M.; et al. The feasibility of developing a risk assessment for the impact of climate change on the emergence of Crimean-Congo haemorrhagic fever in livestock in Europe: a Review. J. Appl. Microbiol. 2009, 108, 1859–1870. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Report for Research on Infectious Diseases of Poverty. World Health Organization on Behalf of the Special Programme for Research and Training in Tropical Diseases. 2012. http://apps.who.int/iris/bitstream/10665 /44850/1/9789241564489_eng.pdf.
- Kumar, N.; Poonia, V.; Gupta, B.; Goyal, M.K. A novel framework for risk assessment and resilience of critical infrastructure towards climate change. Technol. Forecast. Soc. Chang. 2021, 165, 120532. [Google Scholar] [CrossRef]
- Cheshmehzangi, A. The City in Need. Springer Singapore; 2020.
- Sekar, L.G.; Androws, X.; Annaidasan, K.; Kumar, A.; Kannan, R.; Muthusankar, G.; Balasubramani, K. Assessment of shoreline changes and associated erosion and accretion pattern in coastal watersheds of Tamil Nadu, India. Nat. Hazards Res. 2023. [Google Scholar] [CrossRef]
- Rechel, B. , and McKee, M. Facets of public health in Europe. Maidenhead, UK: McGraw-Hill Education.2014.
- Simpson, N.P.; Mach, K.J.; Constable, A.; Hess, J.; Hogarth, R.; Howden, M.; Lawrence, J.; Lempert, R.J.; Muccione, V.; Mackey, B.; et al. A framework for complex climate change risk assessment. One Earth 2021, 4, 489–501. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).