Submitted:
25 March 2024
Posted:
26 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patients Collective
2.2. Immunohistochemical Analysis
2.3. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
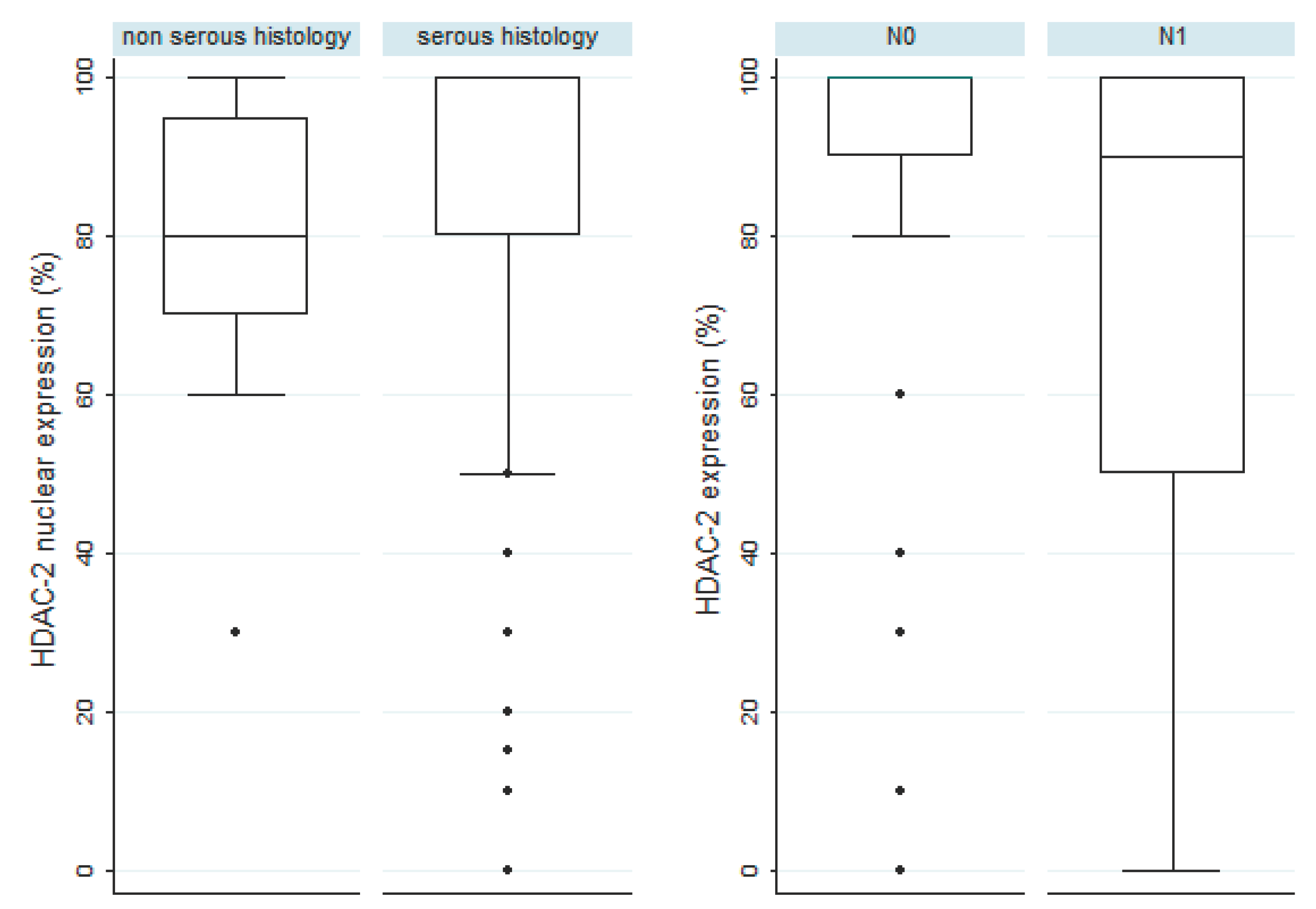
3.2. HDAC-2 Expression and Associations with Clinicopathological Characteristics
3.3. HDAC-4 Expression and Associations with Clinicopathological Characteristics
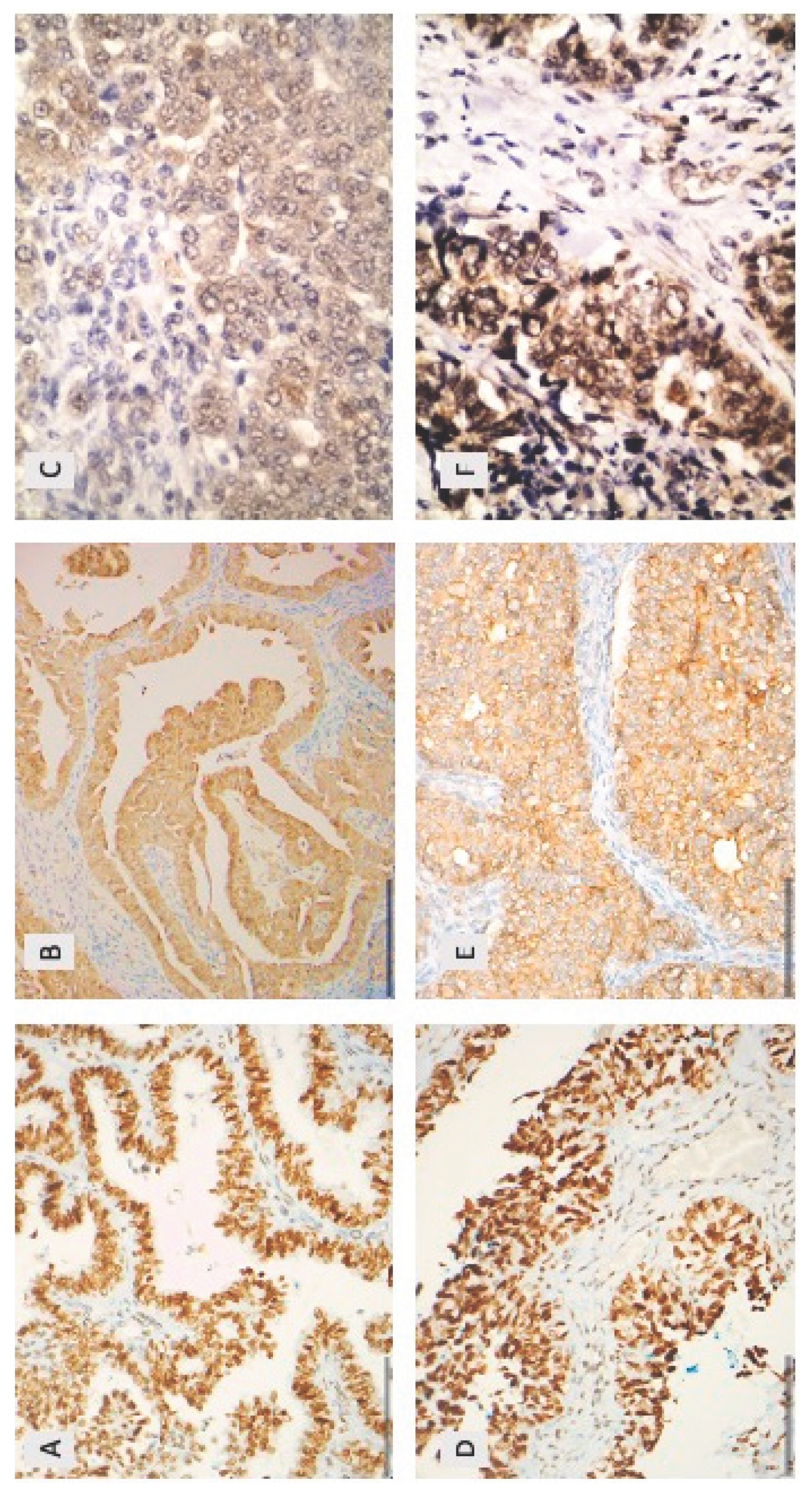
3.4. HDAC-5 Expression and Associations with Clinicopathological Characteristics
3.5. Associations between HDAC-2, HDAC-4 and HDAC-5
| Nuclear HDAC-2 | Cytoplasmic HDAC-4 | Cytoplasmic HDAC-5 | |
|---|---|---|---|
| Cytoplasmic HDAC-4 | rho=-0.09 p=0.390 | ||
| Cytoplasmic HDAC-5 | rho=-0.03 p=0.781 | rho=0.24 p=0.029* | |
| Nuclear HDAC-5 | rho=-0.03 p=0.792 | rho=0.27 p=0.012* | rho=0.5274 p<0.001* |
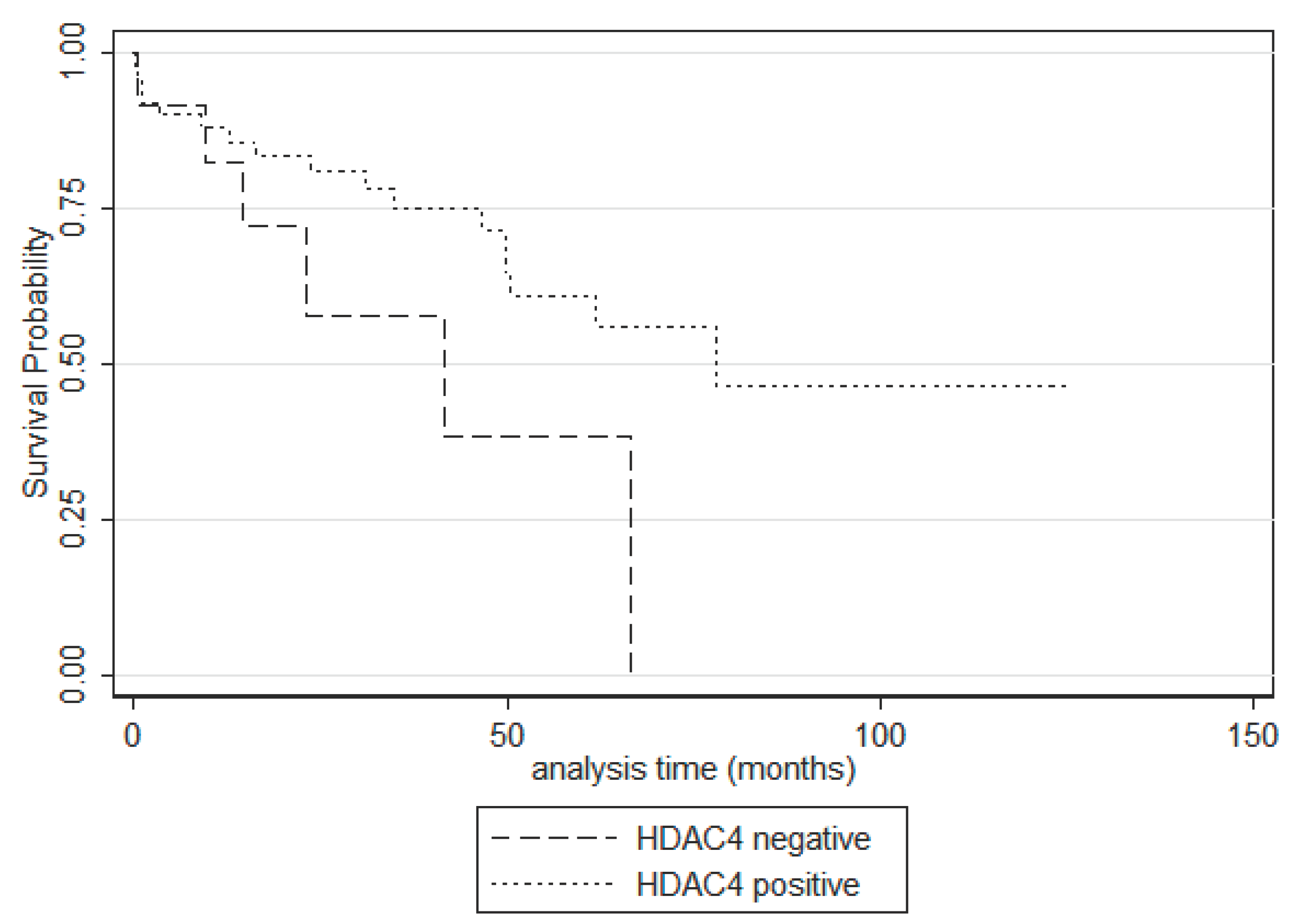
3.6. Survival Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gallinari, P.; Marco, S.D.; Jones, P.; Pallaoro, M.; Steinkühler, C. HDACs, Histone Deacetylation and Gene Transcription: From Molecular Biology to Cancer Therapeutics. Cell Res 2007, 17, 195–211. [Google Scholar] [CrossRef] [PubMed]
- Roth, S.Y.; Denu, J.M.; Allis, C.D. Histone Acetyltransferases. Annu. Rev. Biochem. 2001, 70, 81–120. [Google Scholar] [CrossRef] [PubMed]
- Marks, P. Histone Deacetylases. Current Opinion in Pharmacology 2003, 3, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Blander, G.; Guarente, L. The Sir2 Family of Protein Deacetylases. Annu. Rev. Biochem. 2004, 73, 417–435. [Google Scholar] [CrossRef] [PubMed]
- de Ruijter, A.J.M.; Gennip, A.H. van; Caron, H.N.; Kemp, S.; Kuilenburg, A.B.P. van Histone Deacetylases (HDACs): Characterization of the Classical HDAC Family. Biochemical Journal 2003, 370, 737–749. [Google Scholar] [CrossRef] [PubMed]
- Goutas, D.; Theocharis, S.; Tsourouflis, G. Unraveling the Epigenetic Role and Clinical Impact of Histone Deacetylases in Neoplasia. Diagnostics 2021, 11, 1346. [Google Scholar] [CrossRef]
- Hu, X.; Xing, W.; Zhao, R.; Tan, Y.; Wu, X.; Ao, L.; Li, Z.; Yao, M.; Yuan, M.; Guo, W.; et al. HDAC2 Inhibits EMT-Mediated Cancer Metastasis by Downregulating the Long Noncoding RNA H19 in Colorectal Cancer. J Exp Clin Cancer Res 2020, 39, 270. [Google Scholar] [CrossRef] [PubMed]
- Levidou, G.; Gajdzis, P.; Cassoux, N.; Donizy, P.; Masaoutis, C.; Gajdzis, M.; Gardrat, S.; Pergaris, A.; Danas, E.; Klijanienko, J.; et al. Histone Deacetylase (HDAC)-1, -2, -4, and -6 in Uveal Melanomas: Associations with Clinicopathological Parameters and Patients’ Survival. Cancers 2021, 13, 4763. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, A.; Horiuchi, A.; Kikuchi, N.; Hayashi, T.; Fuseya, C.; Suzuki, A.; Konishi, I.; Shiozawa, T. Type-specific Roles of Histone Deacetylase (HDAC) Overexpression in Ovarian Carcinoma: HDAC1 Enhances Cell Proliferation and HDAC3 Stimulates Cell Migration with Downregulation of E-cadherin. Intl Journal of Cancer 2010, 127, 1332–1346. [Google Scholar] [CrossRef]
- Li, Y.; Seto, E. HDACs and HDAC Inhibitors in Cancer Development and Therapy. Cold Spring Harb Perspect Med 2016, 6, a026831. [Google Scholar] [CrossRef]
- Moufarrij, S.; Dandapani, M.; Arthofer, E.; Gomez, S.; Srivastava, A.; Lopez-Acevedo, M.; Villagra, A.; Chiappinelli, K.B. Epigenetic Therapy for Ovarian Cancer: Promise and Progress. Clin Epigenet 2019, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Pouloudi, D.; Manou, M.; Sarantis, P.; Tsoukalas, N.; Tsourouflis, G.; Dana, E.; Karamouzis, M.V.; Klijanienko, J.; Theocharis, S. Clinical Significance of Histone Deacetylase (HDAC)-1, -2, -4 and -6 Expression in Salivary Gland Tumors. Diagnostics 2021, 11, 517. [Google Scholar] [CrossRef] [PubMed]
- Psilopatis, I.; Schaefer, J.I.; Arsenakis, D.; Bolovis, D.; Levidou, G. SOX11 and Epithelial-Mesenchymal Transition in Metastatic Serous Ovarian Cancer. Biomedicines 2023, 11, 2540. [Google Scholar] [CrossRef]
- Falzone, L.; Scandurra, G.; Lombardo, V.; Gattuso, G.; Lavoro, A.; Distefano, A.; Scibilia, G.; Scollo, P. A Multidisciplinary Approach Remains the Best Strategy to Improve and Strengthen the Management of Ovarian Cancer (Review). Int J Oncol 2021, 59, 53. [Google Scholar] [CrossRef] [PubMed]
- Qazi, S.; Sharma, A.; Raza, K. The Role of Epigenetic Changes in Ovarian Cancer: A Review. Indian J Gynecol Oncolog 2021, 19, 27. [Google Scholar] [CrossRef]
- Caslini, C.; Capo-chichi, C.D.; Roland, I.H.; Nicolas, E.; Yeung, A.T.; Xu, X.-X. Histone Modifications Silence the GATA Transcription Factor Genes in Ovarian Cancer. Oncogene 2006, 25, 5446–5461. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.W.Y.; Huang, Y.-W.; Hartman-Frey, C.; Kuo, C.-T.; Deatherage, D.; Qin, H.; Cheng, A.S.L.; Yan, P.S.; Davuluri, R.V.; Huang, T.H.-M.; et al. Aberrant Transforming Growth Factor Β1 Signaling and SMAD4 Nuclear Translocation Confer Epigenetic Repression of ADAM19 in Ovarian Cancer. Neoplasia 2008, 10, 908–IN2. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, A.H.M.; Afroze, S.; Osuji, G.; Kayani, S.; Colon, N.; Pantho, A.; Kuehl, T.; Pilkinton, K.; Uddin, M. Epigenetic Modifications in Ovarian Cancer: A Review. J Cancer Treat & Diagnosis 2020, 4, 17–35. [Google Scholar] [CrossRef]
- Jin, K.L.; Pak, J.H.; Park, J.-Y.; Choi, W.H.; Lee, J.-Y.; Kim, J.-H.; Nam, J.-H. Expression Profile of Histone Deacetylases 1, 2 and 3 in Ovarian Cancer Tissues. J Gynecol Oncol 2008, 19, 185. [Google Scholar] [CrossRef]
- Weichert, W.; Denkert, C.; Noske, A.; Darb-Esfahani, S.; Dietel, M.; Kalloger, S.E.; Huntsman, D.G.; Köbel, M. Expression of Class I Histone Deacetylases Indicates Poor Prognosis in Endometrioid Subtypes of Ovarian and Endometrial Carcinomas. Neoplasia 2008, 10, 1021–1027. [Google Scholar] [CrossRef]
- Shen, Y.-F.; Wei, A.-M.; Kou, Q.; Zhu, Q.-Y.; Zhang, L. Histone Deacetylase 4 Increases Progressive Epithelial Ovarian Cancer Cells via Repression of P21 on Fibrillar Collagen Matrices. Oncology Reports 2016, 35, 948–954. [Google Scholar] [CrossRef] [PubMed]
- Levinzon, L.; Madigan, M.; Nguyen, V.; Hasic, E.; Conway, M.; Cherepanoff, S. Tumour Expression of Histone Deacetylases in Uveal Melanoma. Ocul Oncol Pathol 2019, 5, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Mottet, D.; Castronovo, V. Histone Deacetylases: Target Enzymes for Cancer Therapy. Clin Exp Metastasis 2008, 25, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, M.; Nielsen, T.O. Histone Deacetylase 1 and 2 in Mesenchymal Tumors. Modern Pathology 2012, 25, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Mutze, K.; Langer, R.; Becker, K.; Ott, K.; Novotny, A.; Luber, B.; Hapfelmeier, A.; Göttlicher, M.; Höfler, H.; Keller, G. Histone Deacetylase (HDAC) 1 and 2 Expression and Chemotherapy in Gastric Cancer. Ann Surg Oncol 2010, 17, 3336–3343. [Google Scholar] [CrossRef] [PubMed]
- Giaginis, C.; Damaskos, C.; Koutsounas, I.; Zizi-Serbetzoglou, A.; Tsoukalas, N.; Patsouris, E.; Kouraklis, G.; Theocharis, S. Histone Deacetylase (HDAC)-1, −2, −4 and −6 Expression in Human Pancreatic Adenocarcinoma: Associations with Clinicopathological Parameters, Tumor Proliferative Capacity and Patients’ Survival. BMC Gastroenterol 2015, 15, 148. [Google Scholar] [CrossRef] [PubMed]
- Peng, D.; Wu, T.; Wang, J.; Huang, J.; Zheng, L.; Wang, P.; Li, J.; Wu, L.; Luo, M. microRNA-671-5p Reduces Tumorigenicity of Ovarian Cancer via Suppressing HDAC5 and HIF-1α Expression. Chemico-Biological Interactions 2022, 355, 109780. [Google Scholar] [CrossRef] [PubMed]
- Weichert, W. HDAC Expression and Clinical Prognosis in Human Malignancies. Cancer Letters 2009, 280, 168–176. [Google Scholar] [CrossRef] [PubMed]
- 2Xu, L.; Yan, X.; Wang, J.; Zhao, Y.; Liu, Q.; Fu, J.; Shi, X.; Su, J. The Roles of Histone Deacetylases in the Regulation of Ovarian Cancer Metastasis. IJMS 2023, 24, 15066. [Google Scholar] [CrossRef]
- Garrett, L.A.; Growdon, W.B.; Rueda, B.R.; Foster, R. Influence of a Novel Histone Deacetylase Inhibitor Panobinostat (LBH589) on the Growth of Ovarian Cancer. J Ovarian Res 2016, 9, 58. [Google Scholar] [CrossRef]
- Zhou, M.; Yuan, M.; Zhang, M.; Lei, C.; Aras, O.; Zhang, X.; An, F. Combining Histone Deacetylase Inhibitors (HDACis) with Other Therapies for Cancer Therapy. European Journal of Medicinal Chemistry 2021, 226, 113825. [Google Scholar] [CrossRef] [PubMed]
| Patients’ characteristics | Median value | Range |
|---|---|---|
| Age (in years) | 62 | 31-92 |
| Number of patients | Percentage | |
| Histological subtype | ||
| Serous carcinoma | 74 | 80.4% |
| Mucinous carcinoma | 3 | 3.3% |
| Endometrioid carcinoma | 5 | 5.4% |
| Clear cell carcinoma | 1 | 1.1% |
| Mixed mucinous-endometrioid carcinoma | 1 | 1.1% |
| Carcinosarcoma | 2 | 2.2% |
| Serous borderline tumor | 6 | 6.5% |
| FIGO stage | ||
| I | 27 | 30% |
| II | 10 | 11.1% |
| III | 36 | 10% |
| IV | 17 | 18.9% |
| Tumor grade | ||
| Low grade | 18 | 21%% |
| High grade | 68 | 79% |
| T-status | ||
| T1 | 29 | 32% |
| T2 | 11 | 12% |
| T3 | 50 | 56% |
| N-status | ||
| N0 | 39 | 60.9% |
| N1 | 25 | 39.1% |
| Metastasis | ||
| Metastatic cancer | 18 | 19.6% |
| Non-metastatic cancer | 74 | 80.4%% |
| Residual disease | ||
| None | 25 | 29.1%% |
| Present | 10 | 11.6% |
| Unknown | 51 | 59.3% |
| Event | ||
| Death of disease | 27/80 (follow-up: 0.1-77.9 months) | 28% |
| Censored | 53/80 (follow-up: 0.3-125.2 months) | 71% |
| Relapse | ||
| Present | 36 | 58.1% |
| Positivity rate | median | Range | |
|---|---|---|---|
| Nuclear HDAC2 | 94.4% | 100 | 0-100 |
| Cytoplasmic HDAC4 | 80,4% | 30 | 0-95 |
| Cytoplasmic HDAC5 | 28,1% | 0 | 0-55 |
| Nuclear HDAC5 | 10% | 0 | 0-45 |
| Parameter | Entire cohort | Serous carcinomas |
|---|---|---|
| Age | ||
| FIGO stage | 0.005 | 0.015 |
| T-status | 0.005 | 0.045 |
| Histological Grade | 0.368 | 0.043 |
| Serous histology | 0.060 | - |
| Presence of metastasis | 0.116 | 0.097 |
| Presence of lymph node metastasis | 0.104 | 0.175 |
| Presence of residual disease | 0.035 | 0.027 |
| HDAC-2 positivity | 0.788 | 0.802 |
| HDAC-4 positivity | 0.105 | 0.086 |
| HDAC-5 cytoplasmic positivity | 0.967 | 0.940 |
| HDAC-5 nuclear positivity | 0.324 | 0.573 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





