1. Introduction
Spondylolysis is a unilateral or bilateral defect of the pars interarticularis (or isthmus) of the vertebra, which anatomically represents the junction of pedicle, articular process and lamina [
1]. It is more frequently diagnosed in young population, especially among women, and its pathogenesis has been recognized in traumatic injuries and genetic predisposition [
2,
3,
4,
5]. In the case of adjunctive degenerative disk disease, what is a common finding with aging and in case of mechanical stress, the stability of the affected vertebra, which is is disconnected from posterior elements, can be severely injured, eventually resulting in anterior slippage [
6,
7]. This isthmic spondylolisthesis (ISL) is a dynamic scenario, since the slippage severity may progressively increase, although rarely after adolescence [
8,
9]. In 1932, Mayerding et al. have proposed a grading system for spondylolisthesis that tags as high-grade those with a slippage greater than the 50% [
10]. Low-back pain (LBP) and radiculopathies are the most reported symptoms, whereas sagittal spine deformities may worsen the clinical scenario, especially in the case of high-grade ISL (HGISL). The Spinal Deformity Study Group classification aimed to classify HGISL, and to evaluate the related spinopelvic parameters [
11]. Prolongated symptoms, non-responsiveness to conservative treatments, or neurologic deficits are accepted criteria for surgery [
2,
3,
12,
13]. Although decompression, nerve roots releasing and segmental instrumentation for promoting fusion should be always pursued, the real need for segmental deformity correction must be carefully considered [
2,
14]. Posterolateral instrumentation alone is dedicated to properly selected cases, whereas circumferential instrumentation and fusion is usually recognized as the gold standard. However, a consensus on the best surgical strategy for HGISL is still missing [
12]. Some authors have already presented their experiences in minimally invasive spine surgery (MISS) for low-grade ISL, reporting valuable clinical and radiological outcomes [
4,
5,
12,
15]. This study aimed to investigate the feasibility of a novel MISS technique for HGISL, evaluating its surgical, clinical, and radiological outcomes.
2. Materials and Methods
2.1. Study Design
This a monocentric prospective observational study on a single cohort of patients, designed and conducted according to the STROBE guidelines [
16]. The IRB approval was not requested according to the observational protocol of the present investigation.
2.2. Patient Selection
Patients referred to our neurosurgery department from January 2014 to December 2022, for HGISL of L5, grade V, VI, VII, or VII according to the SDGS classification, suffering from LBP and/or radicular symptoms, were prospectively enrolled and considered for eligibility. Oncologic diagnosis, osteoporosis, history of lumbar spine surgery, and previous traumatic injuries were considered as exclusion criteria. Full-spine x-Rays, with standard and dynamic studies, lumbosacral MRI, a ten-point itemized visual analogue scale for LBP (VAS-b) and for legs pain (VAS-1) scores, the Oswestry disability index (ODI) score, and the short form 36 physical component score (SF-36 PCS) [
17] were collected for every patient, preoperatively and during the follow-up, at 3 months, 1 year and 2 years after surgery. A specific informed consent, in agreement with the institutional guidelines, was collected from every patient.
2.3. Surgical Technique
Every procedure was performed on general anesthesia, and patients were positioned in prone neutral position. Bilateral percutaneous pedicle screws were firstly positioned under fluoroscopic guidance on L4-L5-S1, then the two lower small incisions on each side were connected. A mini-open Wiltse approach was performed bilaterally for arthrectomy, neural foramina opening, fibrous tissue removal on the pars interarticularis defect, and nerve roots neurolysis. Two expert surgeons operated on a single side each, carefully preparing the intervertebral disc space using shavers, thus allowing to progressively mobilize L5 nerve roots and to lift at the same time from both side the upper vertebral plate. At this moment, particular attention was paid to create sufficient space to insert the cage, through a huge opening of the foramen walls, but above all, trying to lift up the upper endplate and opening the disk space. To maximize the correction of the segmental deformity, a straight rod was temporarily positioned on one side, and progressively fixed for reducing the slippage and maintaining correction grade. Then a straight PLIF-shaped cage was lateral-to-medial inserted on the contralateral side. Thereafter, the temporary rod was removed and positioned on the contralateral side as described above, and a second symmetric cage was inserted from the other side to fix the vertebral body correction. A lordotic rod was finally positioned ipsilaterally to the second cage, the other straight rod was substituted with a lordotic one and the system was now locked in compression, to furtherly increase the segmental lordosis thus reducing the slip angle. Accordingly, this novel MISS technique consists in a bilateral MISS TLIF approach (bm-TLIF), and the insertion of two straight PLIF-shaped cages.
2.4. Outcomes Measurement
Intraoperative blood loss, surgical duration, and length of hospitalization were collected as surgical outcomes. Complications, VAS-b, VAS-1, ODI and SF-36 PCS scores were collected preoperatively and at every follow-up visit, as clinical outcomes. Spinopelvic parameters, slip angle and SI severity grade were measured preoperatively and at last follow-up visit, as radiological outcomes.
2.5. Statistical Analysis
Values were reported as mean ± standard deviation. The t-Student test was used to compare the quantitative continuous variables. The Fisher's exact test (2-sided) was used instead to compare the categorical variables. Statistical significance was pre-determined at an alpha of 0.05.
3. Results
3.1. Patient Data
Thirty-one patients were finally enrolled in the present study. Mean age was 29 (±7) years, the F:M ratio was 2.5:1, 9 patients were smokers and 3 suffered from diabetes type I. The DSGS deformity type was VII in 12 patients and VIII in 19 patients. All patients completed a minimum follow-up of 24 months.
3.2. Surgical and Clinical Outcomes
The mean blood loss was 250 (±150) mL, the mean surgical duration was 187 (±150) min and the mean hospitalization time was 4 (±1) days. No intraoperative complications were registered. The mean preoperative scores were VAS-b 7 (±3), VAS-1 6 (±3), ODI 55 (±23) %, and SF-36 PCS 27 (±9). At last follow-up evaluation, there was a significative improvement for every considered clinical outcome: VAS-b 2 (±2) (p=0,01), VAS-1 2 (±3) (p<0,01), ODI 14 (±12)% (p<0,01), and SF-36 PCS 44 (±17) (p=0,02). Two major complications were registered, consisting in a postoperative unilateral L5 palsy, both self-recovered within 1 year. The mean clinical follow-up was 34 months. Two patients reported a medical-resistant postoperative burning pain, referred to both legs, which resolved in one week.
3.3. Radiological Outcomes
The mean changes at last follow-up evaluation were slippage 65 (±5)% (p = 0,02), slip angle 12 (±7) degrees (p=0,01), pelvic tilt 7 (±8) degrees (p<0,01). The sagittal vertical axis (SVA) was found in the range of normality [
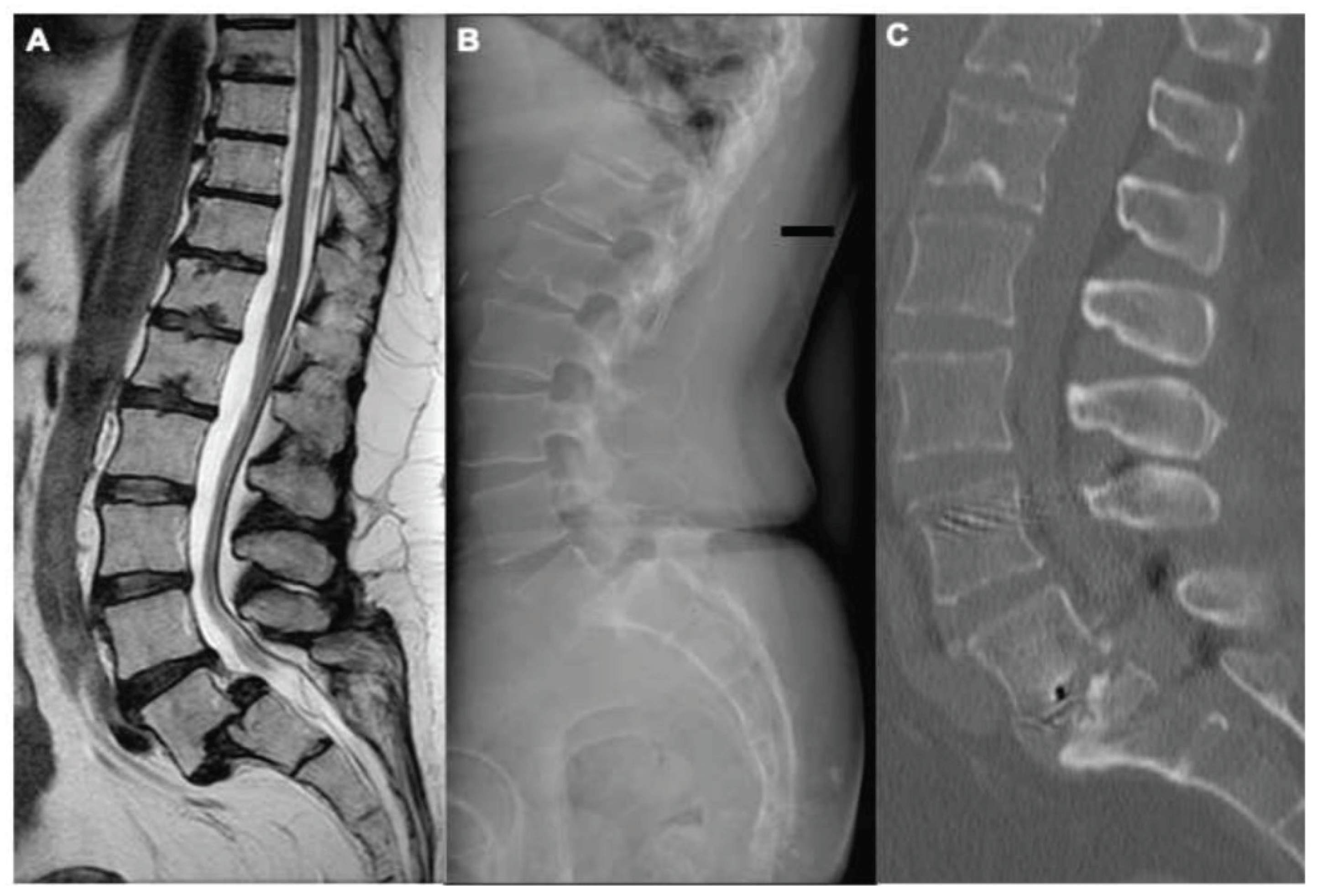
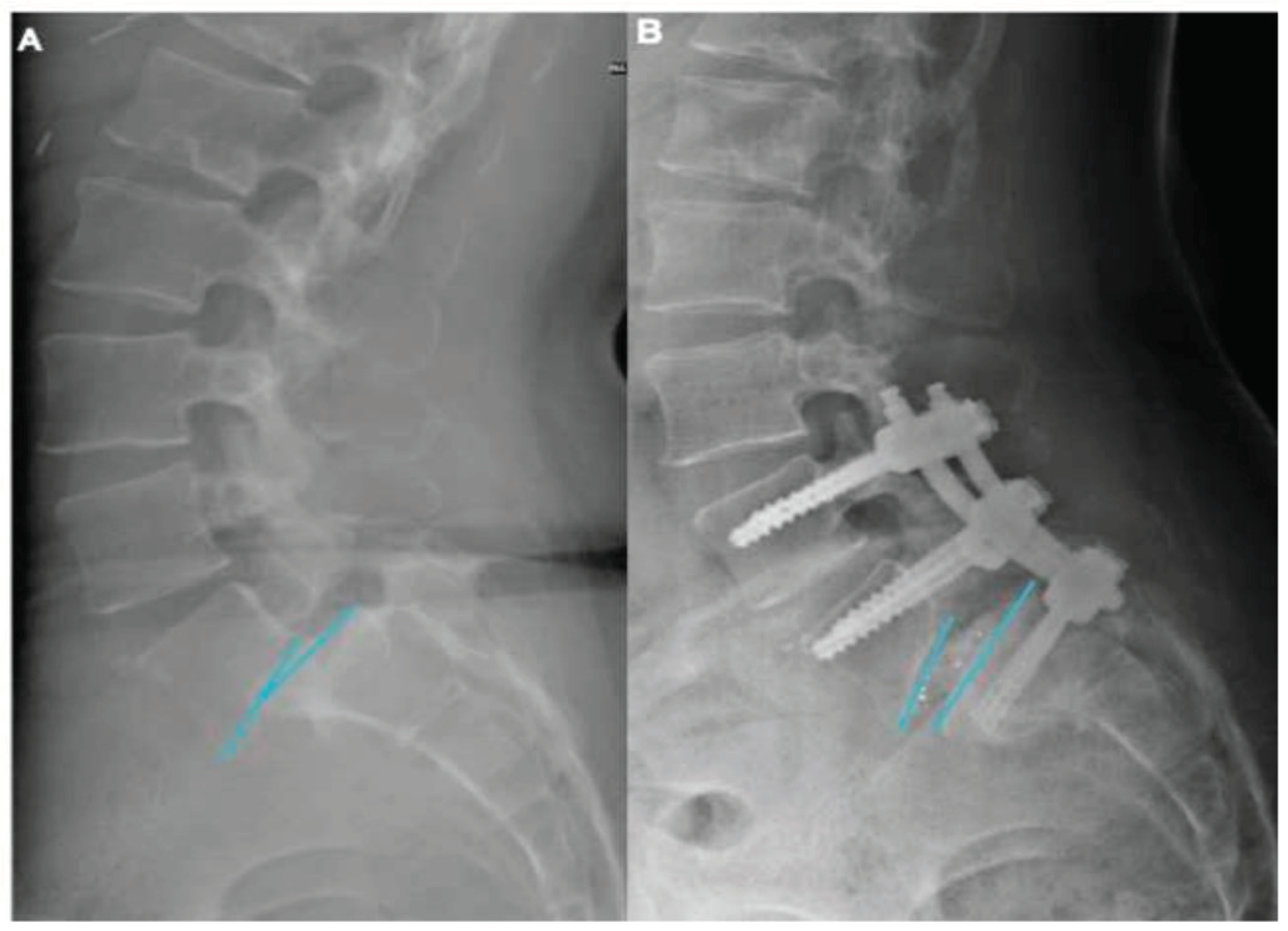
18] preoperatively and two years after surgery in all patients. No significative differences were found comparing pre- and post-operative thoracic kyphosis, lumbar lordosis, and pelvic incidence values. An illustrative case is showed in
Figure 1. The univariate analysis showed that a slip angle > 10° (
Figure 2) was the only independent factor, in our cohort of patients, in determining higher VAS-b and ODI scores (p=0,001 and p=0,03 respectively).
4. Discussion
Surgery has been progressively accepted as the treatment of choice for symptomatic patients with HGISL; however, there still are controversies about asymptomatic or poorly symptomatic patients, who can be managed also conservatively [
3,
12].
Different surgical techniques have been proposed, all recognizing decompression, nerve roots releasing and segmental fusion as primary treatment goals [
12]. The need for segmental deformity correction remains debated, thus spinopelvic parameters and global spine alignment should be carefully evaluated [
4,
19]. Indeed, according to the Marchetti and Bartolozzi classification, HGISL can be divided in low and high dysplastic, according to the severity of the bony dysplastic changes present on the L5 and S1 vertebrae and on the risk of slip progression.
In situ fixation was associated with a higher rate of slip progression, pseudarthrosis and secondary surgeries [
2]. Furthermore, modifications of spinopelvic parameters, especially PI, such in case of high dysplastic HGILS, are reported to promote slip progression [
18,
19,
20,
21].
Slippage reduction may be often achieved using pedicle screws only, however, their capability in maintaining segmental correction has been already reported as lower than circumferential instrumentations, due to the higher risk of hardware failure [
22]. Hence, the use of inter somatic cages, properly sized and positioned, may represent a key point in HGISL surgery, providing higher chances for a circumferential secondary fusion. Spinopelvic parameters restoration was associated with clinical improvement in patients with low-grade SL [
4,
14,
23]. Our results suggest that a slip angle >10° is an independent factor in determining higher VAS-b and ODI scores. Accordingly, segmental deformity correction, even partial, may provide better long-term clinical outcomes; thus, it should be always pursued in HGISL patients with spinal malalignment.
Although the evaluation of the unstable zone has been already proposed [
24], in our experience, segmental kyphosis on L5-S1 and modifications of spinopelvic parameters are critical factors to carefully evaluate to include L4 in the instrumentation system.
In the last decades, MISS procedures have been progressively adopted as a gold standard for even more degenerative [
13,
25], traumatic [
26,
27] and oncologic conditions [
28]. Furthermore, a wide gamma of instrumentation systems allows surgeons to identify case-by-case the most performing one [
29]. Previous studies have reported minimally invasive TLIF as a safe and effective technique for low-grade and high-grade SL [
5,
30,
31,
32]. A recent meta-analysis concludes that minimally invasive TLIF is associated with better surgical, clinical and radiological outcomes, while the standard open TLIF for low-grade spondylolisthesis is usually associated with shorter procedures [
33]. In 2013, Quraishi et al. firstly proposed a minimal access bilateral TLIF for HGISL, reporting a comfortable working angle for cage positioning [
5]. In our cohort of patients, bm-TLIF showed valuable surgical, clinical and radiological outcomes. The bilateral use of the Wiltse approach is related to low intraoperative blood loss and postoperative pain; it also provides an optimal working angle for inserting pedicle screw, performing atherectomy and discectomy, allowing to lateral-to-medial insert straight PLIF-shaped cages. As reported above, the possibility to work simultaneously with two symmetric approaches, using temporary roads to insert the cages for maintaining the correction grade. On the other hand, this technique requires multiple paramedian incisions, which may result in a worse aesthetic outcome, as previously proposed [
34]. Since patients operated for HGISL are mostly young women, this aspect should be carefully considered and discussed.
In case of HGISL m-TLIF may represent a challenging technique, due to the trapezoidal L5 vertebral body and a dome-shaped superior end plate of S1. The neural foramen is always horizontalized and the nerve dissection should be always conducted carefully with the aid of intraoperative microscope. Neurolysis is often difficult due to presence of tight fibrous tissue surrounding the nerve root, which is also stretched by the vertebral slippage. The insertion of the cage can be preceded by a careful smoothing of the superior S1 endplate, as well as the lift of the inferior endplate of L5.
All these technical aspects, make this procedure reserved to expert surgeons, dealing with minimally invasive procedures.
5. Limitations
Due to the low number of patients enrolled and the lack of a randomized and controlled series, properly designed clinical trials are needed to further investigate the role of bm-TLIF in HGISL management, comparing its outcomes with the standard open procedures.
6. Conclusions
The present investigation suggests that bm-TLIF, in expert hands, and selected cases, is a feasible, safe, and effective surgical strategy for HGISL, reporting valuable surgical, clinical and radiological outcomes. Properly designed clinical trials are needed to furtherly investigate its role in HGISL, compare its outcomes with standard open procedures and evaluate long-term results.
Author Contributions
Conceptualization: M.M. and Al.R. Methodology: M.M., Al.R., L.R. and An.R. Formal analysis: L.R. Data curation: S.T., S.F., A.C., A.P. and N.N. Writing—original draft preparation: M.M., Al.R; Writing—review and editing: M.M, Al.R., L.R., An.R., S.T., S.F., A.C., A.P. and N.N. Supervision, M.M., Al.R, L.R and An.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| HGISL |
High-grade isthmic spondylolisthesis |
| LBP |
Low-back pain |
| bm-TLIF |
bilateral minimally invasive TLIF |
| FU |
Follow-up |
| VAS |
Visual analogue scale |
| ODI |
Oswestry disability index |
| SF-36 |
Short-Form-36 |
| ISL |
Isthmic spondylolisthesis |
| SDSG |
Spinal Deformity Study Group |
| MISS |
Minimally invasive spine surgery |
| PLIF |
Posterior lumbar interbody fusion |
| SVA |
Sagittal vertical axis |
References
- Wiltse LL, Newman PH, Macnab I (1976) Classification of spondylolisis and spondylolisthesis. Clin Orthop Relat Res 23-29.
- Transfeldt EE, Mehbod AA (2007) Evidence-based medicine analysis of isthmic spondylolisthesis treatment including reduction versus fusion in situ for high-grade slips. Spine 32:126-129. [CrossRef]
- Xue X, Wei X, Li L (2016) Surgical Versus Nonsurgical Treatment for High-Grade Spondylolisthesis in Children and Adolescents: A Systematic Review and Meta-Analysis. Medicine (Baltimore) 95:3070. [CrossRef]
- Rajakumar DV, Hari A, Krishna M, et al (2017) Complete anatomic reduction and monosegmental fusion for lumbar spondylolisthesis of Grade II and higher: use of the minimally invasive "rocking" technique. Neurosurg Focus 43:12. [CrossRef]
- Quraishi NA, Rampersaud YR (2013) Minimal access bilateral transforminal lumbar interbody fusion for high-grade isthmic spondylolisthesis. Eur Spine J 22:1707-1713. [CrossRef]
- Beck AW, Simpson AK (2019) High-Grade Lumbar Spondylolisthesis. Neurosurg Clin NAm 30:291-298. [CrossRef]
- Miscusi M, Carnevali C, Ricciardi L, et al (2020) Histomorphology and immunohistochemical patterns in degenerative disc disease and clinical-radiological correlations: a prospective study. Eur Spine J. [CrossRef]
- Huang RP, Bohlman HH, Thompson GH, Poe-Kochert C (2003) Predictive value of pelvic incidence in progression of spondylolisthesis. Spine 28:2381-2385; discussion 2385. [CrossRef]
- Fredrickson BE, Baker D, McHolick WJ, et al (1984) The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am 66:699-707. [CrossRef]
- Koslosky E, Gendelberg D (2020) Classification in Brief: The Meyerding Classification System of Spondylolisthesis. Clin Orthop Relat Res 478:1125-1130. [CrossRef]
- Labelle H, Mac-Thiong J-M, Roussouly P (2011) Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J 20 Suppl 5:641-646. [CrossRef]
- Passias PG, Poorman CE, Yang S, et al (2015) Surgical Treatment Strategies for High-Grade Spondylolisthesis: A Systematic Review. Int J Spine Surg 9:50. [CrossRef]
- Ricciardi L, Stifano V, Sturiale CL, et al (2020) Minimally Invasive Decompression with Posterior Elements Preservation Versus Laminectomy and Fusion For Lumbar Degenerative Spondylolisthesis: A Systematic Review and Meta-Analysis of Surgical, Clinical and Radiological Outcomes. Surg Technol Int 36:.
- Fan G, Gu G, Zhu Y, et al (2016) Minimally Invasive Transforminal Lumbar Interbody Fusion for Isthmic Spondylolisthesis: In Situ Versus Reduction. World Neurosurg 90:580-587.el. [CrossRef]
- Hentenaar B, Spoor AB, de Waal Malefijt I, et al (2016) Clinical and radiological outcome of minimally invasive posterior lumbar interbody fusion in primary versus revision surgery. J Orthop Surg Res 11:2. [CrossRef]
- von Elm E, Altman DG, Egger M, et al (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE Statement: guidelines for reporting observational studies. Int J Surg 12:1495-1499. [CrossRef]
- Taft C, Karlsson J, Sullivan M (2001) Do SF-36 summary component scores accurately summarize subscale scores? Qual Life Res 10:395-404. [CrossRef]
- Le Huec JC, Thompson W, Mohsinaly Y, et al (2019) Sagittal balance of the spine. Eur Spine J 28:1889-1905. [CrossRef]
- Hresko MT, Labelle H, Roussouly P, Berthonnaud E (2007) Classification of high-grade spondylolistheses based on pelvic version and spine balance: possible rationale for reduction. Spine 32:2208-2213. [CrossRef]
- Hanson DS, Bridwell KH, Rhee JM, Lenke LG (2002) Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine 27:2026-2029. [CrossRef]
- Roussouly P, Gollogly S, Berthonnaud E, et al (2006) Sagittal alignment of the spine and pelvis in the presence of L5-s1 isthmic lysis and low-grade spondylolisthesis. Spine 31:2484-2490. [CrossRef]
- Ricciardi L, Stifano V, Proietti L, et al (2018) Intraoperative and Postoperative Segmental Lordosis Mismatch: Analysis of 3 Fusion Techniques. World Neurosurg. [CrossRef]
- Bourghli A, Aunoble S, Reebye O, Le Huec JC (2011) Correlation of clinical outcome and spinopelvic sagittal alignment after surgical treatment of low-grade isthmic spondylolisthesis. Eur Spine J 20 Suppl 5:663-668. [CrossRef]
- Lamartina C, Zavatsky JM, Petruzzi M, Specchia N (2009) Novel concepts in the evaluation and treatment of high-dysplastic spondylolisthesis. Eur Spine J 18 Suppl 1:133-142. [CrossRef]
- Miscusi M, Ramieri A, Forcato S, et al (2018) Comparison of pure lateral and oblique lateral inter-body fusion for treatment of lumbar degenerative disk disease: a multicentric cohort study. Eur Spine J27:222-228. [CrossRef]
- Trungu S, Forcato S, Bruzzaniti P, et al (2019) Minimally Invasive Surgery for the Treatment of Traumatic Monosegmental Thoracolumbar Burst Fractures: Clinical and Radiologic Outcomes of 144 Patients With a 6-year Follow-Up Comparing Two Groups With or Without Intermediate Screw. Clin Spine Surg 32:171-E176. [CrossRef]
- Cimatti M, Forcato S, Polli F, et al (2013) Pure percutaneous pedicle screw fixation without arthrodesis of 32 thoraco-lumbar fractures: clinical and radiological outcome with 36-month follow-up. Eur Spine J 22 Suppl 6:S925-932. [CrossRef]
- Miscusi M, Polli FM, Forcato S, et al (2015) Comparison of minimally invasive surgery with standard open surgery for vertebral thoracic metastases causing acute myelopathy in patients with short- or mid-term life expectancy: surgical technique and early clinical results. J Neurosurg Spine 22:518-525. [CrossRef]
- Ricciardi L, Stifano V, Rivera Perla KM, et al (2018) One center's experience with Hybrid technique for lumbar spine instrumentated surgeries: evaluation of different instrumentation systems and their management. World Neurosurg. [CrossRef]
- Kim J-S, Jung B, Lee S-H (2018) Instrumented Minimally Invasive Spinal-Transforminal Lumbar Interbody Fusion (MIS-TLIF): Minimum 5-Year Follow-Up With Clinical and Radiologic Outcomes. Clin Spine Surg 31:302-E309. [CrossRef]
- Barbagallo GMV, Piccini M, Alobaid A, et al (2014) Bilateral tubular minimally invasive surgery for low-dysplastic lumbosacral lytic spondylolisthesis (LDLLS): analysis of a series focusing on postoperative sagittal balance and review of the literature. Eur Spine J 23 Suppl 6:705-713. [CrossRef]
- Scheufler K-M, Dohmen H, Vougioukas VI (2007) Percutaneous transforminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery 60:203-212; discussion 212-213. [CrossRef]
- Qin R, Liu B, Zhou P, et al (2019) Minimally Invasive Versus Traditional Open Transforaminal Lumbar Interbody Fusion for the Treatment of Single-Level Spondylolisthesis Grades 1 and 2: A Systematic Review and Meta-Analysis. World Neurosurg 122:180-189. [CrossRef]
- Ricciardi L, Sturiale CL, Pucci R, et al (2018) Patient-oriented aesthetic outcome after lumbar spine surgery: a 1-year follow-up prospective observational study comparing minimally invasive and standard open procedures. World Neurosurg. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).