1. Introduction
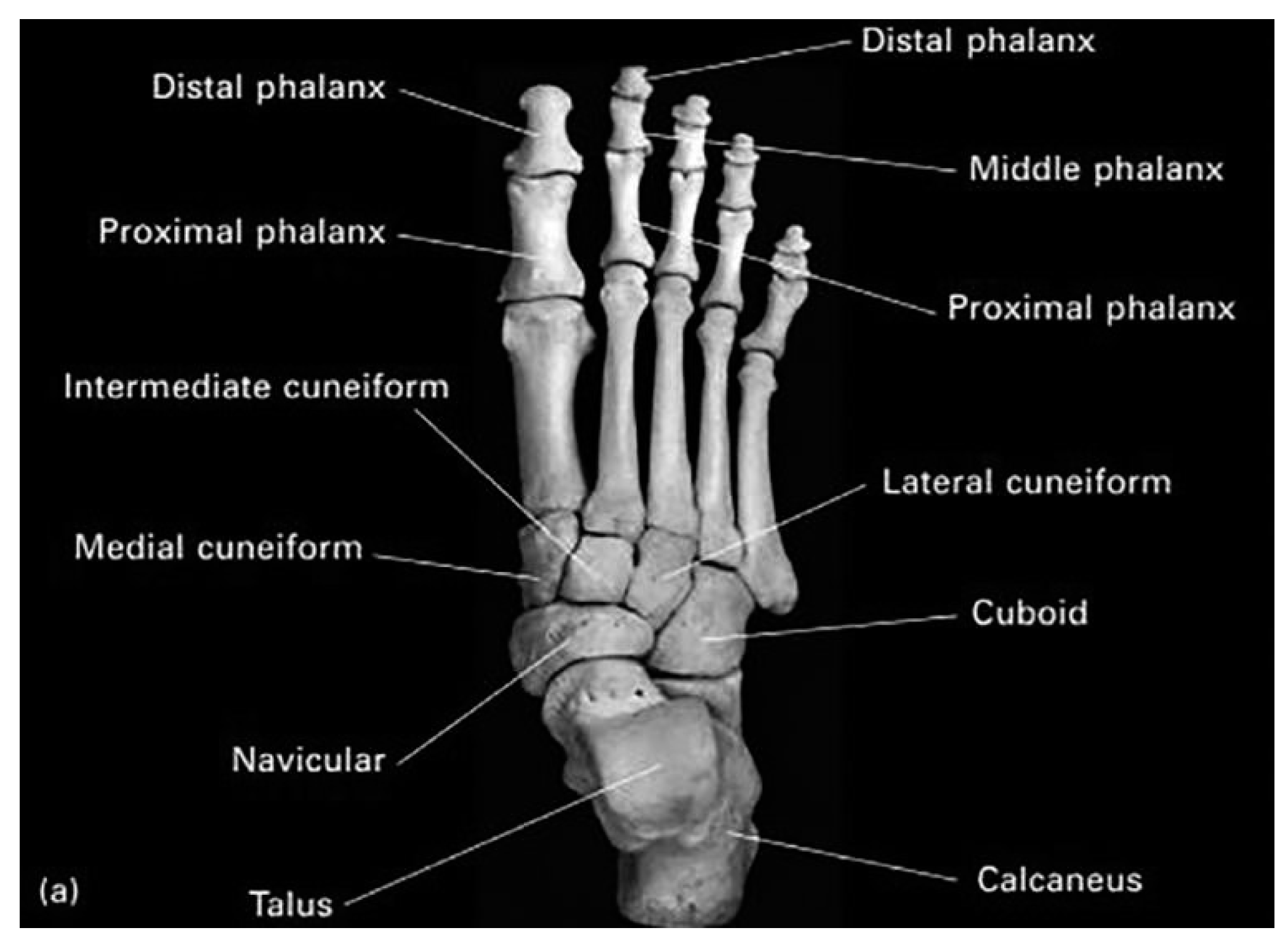
The human foot is a complex structure composed of 26 bones, 33 joints, 107 ligaments and 19 muscles. One of the main joints of the foot is the metatarsophalangeal (MTP) joint, which connects the metatarsal bones (the middle bones of the foot) to the phalanges (the bones of the toes). They allow: Flexion, Extension, abduction, adduction, and circumduction. This joint play a major role in the stance phase of the gait cycle [
1].
Figure 1.
Anatomy of right foot bones (Superior view) [
2].
Figure 1.
Anatomy of right foot bones (Superior view) [
2].
There are various reasons why one might need to use an implant of the metatarso phalangeal joint, including conditions like advanced rheumatoid arthritis, hallux rigidus, and bone infections or amputations that causes joint locking. However, for this study, it’s focalized in the use of the implant of the MTP joint for malignant tumors affecting this part.
Figure 2.
X-ray of left foot showing abnormal ossification around 3
rd MTP Joint [
3].
Figure 2.
X-ray of left foot showing abnormal ossification around 3
rd MTP Joint [
3].
These tumors can cause significant damage and pain with locking the joint. In such cases, an implant can aid in restoring the lost function and mobility to the impacted area, enabling patients to lead more normal lives and to regain their normal activities. Understanding the use of an implant for malignant bone tumors can help improve the care and outcomes for patients dealing with these conditions.
A malignant bone tumor of the metatarsal phalangeal bone is a type of cancerous growth that occurs in the bones of the foot, specifically in the joint between the metatarsal and the phalangeal bone [
4]. It can arise from a variety of tissues and can be classified as primary or metastatic.
The most common bone tumors in this area are osteosarcoma, chondrosarcoma, and Ewing's sarcoma. Osteosarcoma is the most common type of bone cancer in general and is characterized by the production of abnormal bone tissue with stiff joint [
5]. Chondrosarcoma, on the other hand, is a cancer of the cartilage, that begins in the bones and sometimes occur in the soft tissues near bones with locking the joint [
4,
5]. Ewing's sarcoma typically affects children and young adults with a peak incidence at 15 years of age. [
6].
Symptoms of these tumors can include increasing pain, swelling near the bone, bone injury or bone break for no clear reason, and stiffness in the affected joint [
4,
5].
Treatment for malignant bone tumors of the metatarsal phalangeal bone typically involves a combination of surgery, chemotherapy, and radiation therapy. The specific treatment plan will depend on the type and stage of the cancer, as well as other individual factors such as age and general health [
7].
3D printing is revolutionary since it allows the creation of precise, customizable structures, releasing up an ocean of possibilities in various sectors, particularly healthcare. The use of this method makes it possible to produce customized medical equipment that can be adapted to the specific needs of patients, which is an innovative feature that was not achievable with conventional production techniques.
In traumatology, modeling and 3D printing are crucial since they give medical professionals a greater knowledge of complicated injuries and more accuracy during surgery. It enhances preoperative planning by allowing precise three-dimensional imagery of severe injuries. Moreover, it makes it easier to create personalized implants, cutting guides, and fixation plates, all of which have the potential to enhance patient outcomes by enhancing fit and precision during surgery [
8,
9].
Medical applications of three-dimensional (3D) printing technology are increasing, and 3D-printed implants have demonstrated high accuracy and customizability and achieved good clinical performance in repair and orthopedic reconstruction [
9].
In this perspective, this paper proposes a personalized (on measure) implant design methodology to replace the MTP lesions caused by the tumor disease, in order to enable patients to recover their technical skills. To do so, it was proceeded to the exploitation of 2D
CT images to perform a 3D reconstruction that allows to model the implant prototype. Subsequently, a feasibility study on 3D printing using new materials was carried out comparing two high-performance 3D printers, the Next 5100 and the Volumic Stream 30 Ultra, in order to implement our method and print the designed prototype.
2. Related Works
The exploration of a titanium metatarsophalangeal implant is enriched by an expansive array of contributions from the orthopedics and traumatology research community. These pivotal works are bound by a central thread - the employment of ground-breaking materials and technologies for surgical implants. At the forefront, a comprehensive examination of the HAPY pyrocarbon spherical metatarsophalangeal implant is laid out in the study by Martin Schramm et al. [
10]. The focus on biocompatibility, wear resistance, and the mimicry of natural joint function in their work profoundly dictates the selection of titanium for the implant. Drawing from this, a revolutionary methodology proposed by Btihal El Ghali et al. offers a greater depth of comprehension [
11]. The 3D reconstruction of CT scan images, adopted for the fabrication of a patient-specific lunate implant, sets an exemplary model for the design of the metatarsophalangeal implant. Subsequently, Srikong Chandhanarat et al. present an illustrative application of these technologies, exploring a case of a fifth toe giant cell tumor treated using a 3D printed proximal phalangeal prosthesis [
12]. Their triumphant narrative endorses the patient-oriented methodology and hints at the potential for augmented functional outcomes with 3D printed implants. Advancing from this point, further profundity is added to the comprehension of 3D printing's potential by the research conducted by L Xu et al. [
13]. The intricate process they adopted for amending bone defects with 3D-printed personalized prostheses following metacarpal giant cell tumor resection imparts valuable knowledge into related procedures, spanning from preoperative planning and imaging to virtual modeling and 3D printing. Parallelly, Mina Zare et al. extend the discourse from titanium towards the domain of silicone-based biomaterials [
14]. Their investigation into strategies to enhance the performance of these materials, inclusive of antimicrobial tactics, surface modification techniques, and the integration of nanomaterials, nurtures the imagination for future implant innovations. An essential cornerstone of this research is the grasp of surgical outcomes. In this context, the prospective clinical and biomechanical analysis of feet post the first metatarsophalangeal (MTP) joint replacement by R. A. Rajan et al. offers valuable teachings [
15]. Their approach mirrors the importance placed on comprehensive evaluations in surgical interventions. Conclusively, a case report by Jiangang Cheng et al. circles back to underscore the choice of titanium as the material for the implant [
16]. This documents the repair of distal fibular and lateral malleolus defects utilizing an individualized 3D-printed titanium alloy prosthesis. Through the synthesis of these individual threads of research, a rounded understanding emerges. This understanding has informed the design, execution, and evaluation of the titanium metatarsophalangeal implant under discussion. These integrated findings, theories, and case studies light up the path ahead for this field of research.
3. Materials and Methods
Table 1.
3D design software comparison.
Table 1.
3D design software comparison.
| Softwares |
Functionalities |
Accessibitity |
Disadvantages |
Operatingsystem |
Rating |
| Blender |
3D modeling, Sculpting, Texturing, Animation, Simulation.. Free and Open source Cross-Platform Compatibility Versatility and functionality |
free |
Complex Interface Limited CAD features Lack of customer service |
Windows macOS Linux |
8,5/10 |
| Solidworks |
3D modeling, Simulation, Visualization, Design automation.. Intuitive interface Interoperability Powerful simulation tools |
Paying |
Price Hardware demands Complexity Large files |
Windows |
9,5/10 |
| Cinema 4D |
|
Paying |
|
Windows MacOs |
8/10 |
| 3D Slicer |
Open Source for image analysis 3D reconstruction, 3D Modeling, Image segmentation |
Free |
|
Compatible with most operating systems |
9,5/10 |
| Materialise Mimics |
Image processing, 3D segmentation, 3D visualization, 3D model export, High quality 3D models Biomedical focus Strong support and documentation |
Paying |
|
Compatible with most operating systems |
9,5/10 |
Table Edu4.0
d’Anatomage
|
Proprietary software for the realization, image dissection, virtual reality, manual segmentation High quality 3D reconstruction Offers a library of real patient case studies |
Paying |
|
Windows of the anatomy table |
9/10 |
| Meshmixer |
|
Free |
|
Windows MacOs |
9,5/10 |
3.1. CT Image Acquisition
All Computerized Tomography (CT) images used for this study were taken at the Cheikh Zaid International University Hospital of a normal patient's foot, then they were analyzed and reviewed by 4 radiologists using (Somatom Def AS, Siemens Healthineers, Germany). The main scanning parameters were as follow: Tube voltage: 120 kV, pitch factor 1⁄4 0.3–1.5 mm, recon matrix 1⁄4 512 x 512, slice thickness 1⁄4 1 mm. During the session, the patient lies supine with the foot in a neutral position, which is usually accomplished by asking the patient to stand their foot flat on the scanner bed.
3.2. Comparative Study of Design Software
In this section we present a comparison analysis that involves a benchmarking of six of the most efficient 3D modeling and reconstruction software, each was evaluated according to several requirements, including accessibility, open-source compatibility, and general quality.
We chose the top four performers with the highest marks using a 10-point rating methodology for the evaluation procedure. It has led us to choose Table Edu 4.0, Materialise Mimics, SolidWorks and Meshmixer as the most efficient ones that meets our needs and expectations.
3.2.1. Blender
Blender is an open source, 3D modeling, animation and rendering software, widely used in the film, video game, animation and creative arts industry. It offers a full range of tools for modeling, texturing, lighting, animation and rendering virtual 3D objects and environments. One of the key features of Blender is its 3D modeling capabilities. It provides a versatile set of tools for creating 3D models using various techniques like polygonal modeling, sculpting, and procedural modeling. Artists and designers can shape and manipulate objects with precision and creativity [
17].
3.2.2. Cinema 4D
Cinema 4D is a commercial modelling, animation and 3D rendering software developed by the German company Maxon Computer GmbH. It is generously used in the film, television and design industries to create 3D graphics, specific effects, animations and CG images. One of the notable features of Cinema 4D is its intuitive and user-friendly interface, making it accessible to both beginners and experienced 3D artists. [
18].
3.2.3. Table EDU 4.0 (Anatomage)
Figure 3.
Anatomage table.
Figure 3.
Anatomage table.
Anatomage created the software platform Table Edu 4.0, which offers interactive tools for anatomy and medical education. It is intended for use in classrooms, labs, and other instructional environments. It’s a proprietary software for the realization, image dissection, virtual reality and manual segmentation that offers an immersive and fascinating approach to manipulate, dissect, manually segment, and explore anatomical structures by virtual reality with high quality 3D reconstruction [
19].
3.2.4. 3D SLICER
3D Slicer is a free, open-source software for visualization, processing, segmentation, registration, and analysis of medical, biomedical, and other 3D images and meshes; and planning and navigating image-guided procedures. The primary purpose of 3D Slicer is to process and analyze medical imaging data, such as MRI, and CT scans to extract meaningful information for diagnosis, research, and treatment planning. It offers a comprehensive set of tools for image segmentation, allowing users to delineate anatomical structures and regions of interest within the medical images. This software's benefits include the ability to estimate distances and do 3D reconstructions from 2D pictures obtained using several medical energy modalities [
19].
3.2.5. Materialise Mimics
Materialise Mimics is a 3D image processing, design and modeling software that allows users to import and process medical imaging data such as CT or MRI scans. Due to its capability to create high-quality 3D models of medical pictures, it is often used in the medical field. It is the best option for a variety of medical applications, including surgical planning, patient-specific implant design, and medical research, thanks to its sophisticated tools and algorithms and interaction with 3D printing software [
20].
3.2.6. SolidWorks
SolidWorks is a CAD (Computer Aided Design) software used to create 3D models for design, engineering, and manufacturing purposes. Users of SolidWorks may convert 2D sketches into 3D models, which gives them the ability to edit designs in three dimensions for improved comprehension and communication among design team members. In the medical profession, it is used for the design and modeling of medical equipment including implants, prostheses, and surgical tools as well as for simulating human anatomy and analyzing the mechanics and structure of bones and tissue [
21].
3.2.7. Meshmixer
Meshmixer is a software program developed by Autodesk, a leading software company specializing in 3D design, engineering, and entertainment software. He is often involved in the 3D printing process to adjust and repair 3D models, integrate different models, or provide supports for printing. The program offers a wide range of features, including adding texture, smoothing rough areas, and hollowing out models to save on printing material. In general, it is an effective, adaptable, and simple tool for 3D modeling and printing [
22].
3.3. Comparative Study of Biomaterials (Benchmark)
The table below serves as a benchmark comparison between the top five most frequently applied materials in the field of implants. Each of the materials on the list has a special combination of advantages and weaknesses that make it suitable for a variety of implant devices and patient requirements. The table evaluates each material based on a number of factors, including its strength, durability, weight, cost, and comfort, by also considering the surgical outcomes and patient satisfaction associated with each material.
Table 2.
Advantages and weaknesses of biomaterials.
Table 2.
Advantages and weaknesses of biomaterials.
| Biomaterials |
Advantages |
Weaknesses |
| Stainless steel |
|
|
| Polyethylene |
|
▪ Degradation ▪ Its rigid nature ▪ Damage to the surface |
| Cobalt alloys |
|
|
| Titanium and Titanium alloys |
|
|
| Polymer |
|
|
3.4. 3D Printers
3.4.1. Volumic Stream 30 Ultra
The Volumic Stream 30 Ultra is a high-performance desktop 3D printer for experts and advanced users. This printer has a maximum resolution of 50 microns, which enables it to create high-quality products. Additionally, it has a filament detecting system that recognizes breaks in the filament and has a restart printing functionality in case of a power interruption. It comes with Wi-Fi and USB connections, which makes it easier to transmit printing data [
23].
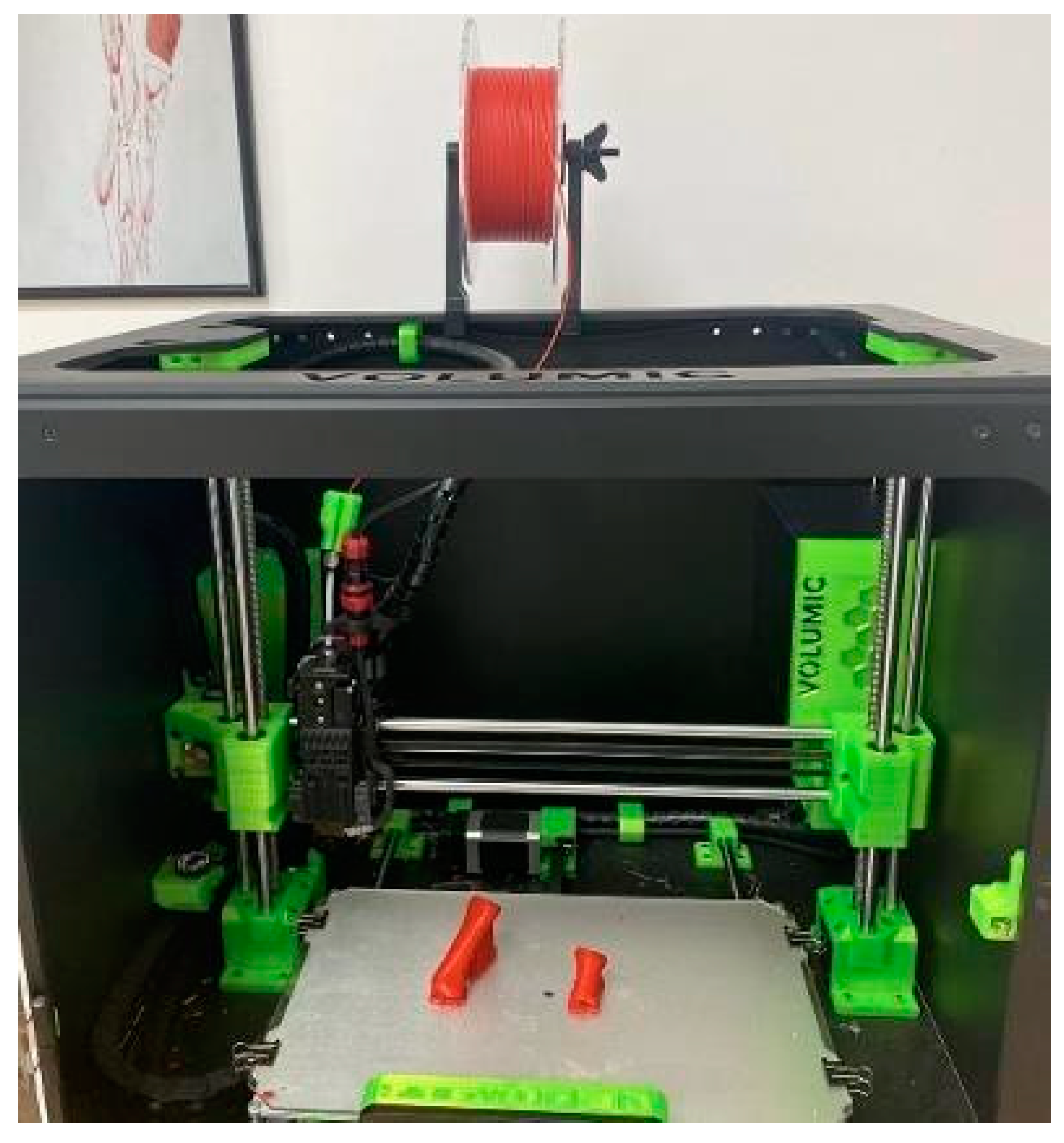
Figure 4.
Volumic Stream 30 Ultra 3D printer.
Figure 4.
Volumic Stream 30 Ultra 3D printer.
3.4.2. Next Dent 5100
The Next Dent 5100 is a professional-grade 3D printer designed primarily for dental applications. It’s one of the first dental 3D printers employs biocompatible materials to create high-quality, patient-specific dental implants, prosthesis, and models. With a touchscreen interface and simple software, it is also simple to operate and makes print preparation and maintenance simple. The printer also has automated calibration and a selfdiagnosis mechanism to make sure it is always operating at its best. By applying a unique process called Laser Stereolithography (LSL), it can produce dental models with incredibly detailed features and precise measurements. This technology builds up the model from the bottom up by selectively curing the resin liquid with a laser layer by layer [
24].
Figure 5.
NextDent 5100 3D printer.
Figure 5.
NextDent 5100 3D printer.
4. Experiments and Results
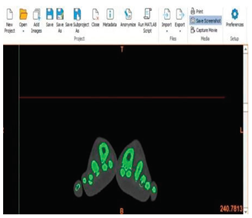
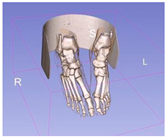
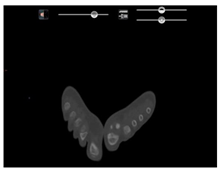
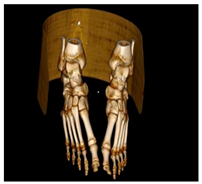
4.1. 3D Reconstruction of the Whole Foot
This comparative review presents an exploration of foot segmentation capabilities using three distinct software programs. Each software's unique capabilities and results are examined and highlighted through the lens of both 2D imaging and 3D reconstruction. Screenshots depicting the exact segmentation outputs achieved by each software program allow for a visual comparison, serving as a tangible testament to their respective efficacies and accuracies. This approach facilitates a comprehensive understanding of the strengths and nuances of each software, paving the way for an informed decision when choosing the best tool for specific needs in foot segmentation.
Table 3.
3D reconstructions of foot.
Following this, we will embark on a detailed comparative analysis, scrutinizing the individual performance and capabilities of these tools, to ascertain their strengths and potential limitations.
Firstly, with regards to the 3D Slicer software, it demonstrates considerable capabilities in creating 3D reconstructions of the foot. While the overall results are laudable, it occasionally misses a few intricate details, indicating minor inconsistencies in precision. However, these small shortcomings do not significantly detract from its overall usefulness, affirming 3D Slicer's reputation as a reliable tool in the realm of medical imaging and 3D reconstruction.
Next, we consider Materialise Mimics. This software distinguishes itself with extraordinary precision and accuracy in creating 3D foot reconstructions. Its ability to accurately capture minute details of foot anatomy allows it to produce a top-notch 3D model. An outstanding feature that enhances Materialise Mimics' appeal is its capability to promptly export the restructured model into an STL file, ideally suited for 3D printing. This function increases operational efficiency, making it a highly effective tool.
Lastly, the Table Edu 4.0 version. This software delivers impressive results in terms of 3D foot reconstruction, perfectly replicating delicate anatomical details. However, it faces a significant limitation in its inability to export the reconstructed model into a 3D printable STL format. This limitation reduces the software's adaptability, restricting its application primarily to the Anatomage Table environment and limiting its usefulness in situations requiring physical models.
4.2. 3D Printing of the Bone
4.2.1. Using Volumic Stream 30 Ultra
The Volumic Stream 30 Ultra's 3D printing of a bone model. The printing process utilized a thermoplastic polymer called PLA filament and took a total of 1 hour and 11 minutes to complete. The printer features a heated print bed, which helps in maintaining the optimal temperature for the PLA filament to adhere properly.
Additionally, the printer is equipped with an extruder, a device responsible for feeding the PLA filament into the printer. The filament is melted and extruded through a nozzle onto the print bed, where it cools down and solidifies to form the initial layer of the bone model. This technique is repeated layer by layer until the entire bone model is finished.
Figure 6.
3D Printed bone using PLA.
Figure 6.
3D Printed bone using PLA.
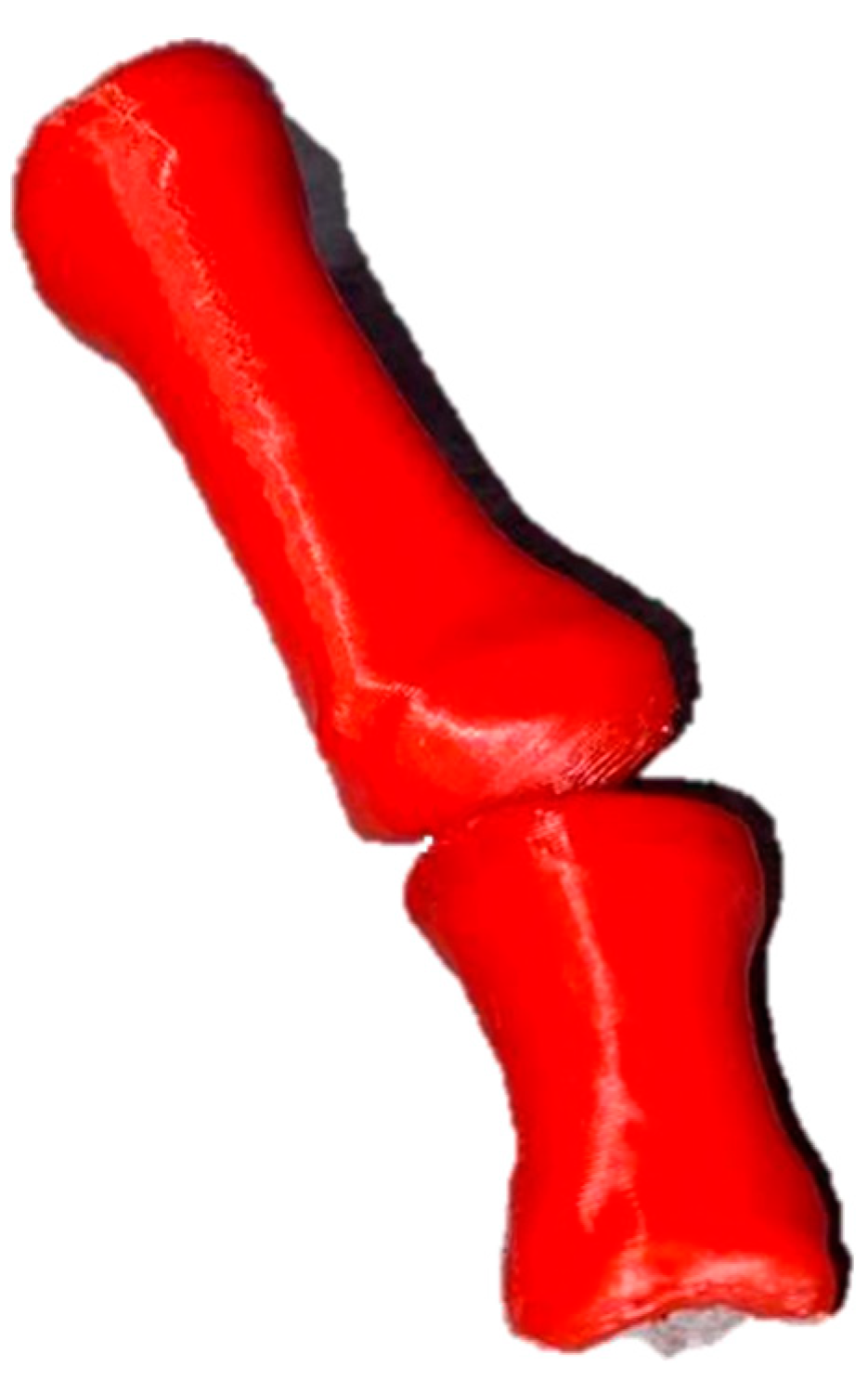
4.2.2. Using Next Dent 5100
The printing process of this particular printer utilizes digital light processing (DLP) technology, where layers of resin liquid are solidified using UV light. To begin the process, a digital 3D volume of the bone is inputted into the printer's software. The bone model is then printed layer by layer, following the instructions from the digital 3D volume and using the DLP technique to cure the resin. Each layer is added on top of the previous one, gradually constructing the bone model. The entire printing process took approximately one hour to complete. Throughout this time, the printer continuously solidified the resin layers, bringing the bone model to its final form.
Figure 7.
3D printed bone using resin.
Figure 7.
3D printed bone using resin.
4.3. 3D Printing of the Hollowed Bones
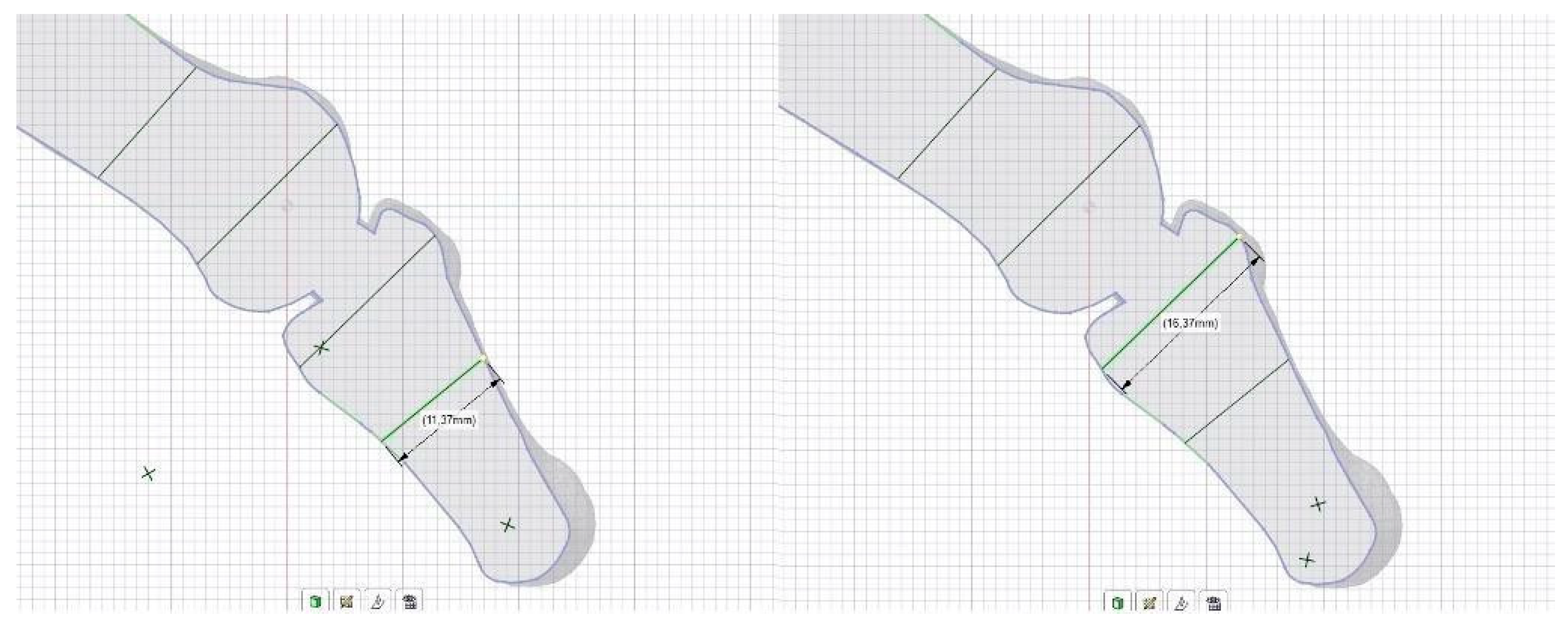
4.3.1. Dimensions of the Removed Part of the Bones
The following set of images exemplify the quantified measurements of the bone volume extracted in preparation for the implantation in this specific case. These illustrations offer an extensive portrayal of the mandatory alterations made to the existing osseous structure, thereby facilitating an accurate fitting of the implant element. This specific volumetric assessment underscores the crucial nature of meticulous planning and precise execution in ensuring the success of implant surgeries. In this particular case, it further illuminates the amount of bone removal required to accommodate the implant optimally.
Figure 8.
Dimensions of the phalangeal part.
Figure 8.
Dimensions of the phalangeal part.
In this particular case, the images reveal precise measurements of the phalangeal bone section set for removal to accommodate the implant insertion. The head of the phalanx, which is the rounded topmost part of the bone, measures 16.37mm, signifying a substantial removal requirement to ensure a successful implant fit. Meanwhile, the upper part of the phalanx, often referred to as the base, measures 11.37mm.
Figure 9.
Dimensions of the metatarsal part.
Figure 9.
Dimensions of the metatarsal part.
On the other hand, the images provide specific measurements of the metatarsal bone portion designated for removal to make way for the implant. The head of the metatarsal bone, the distal rounded part, measures 17.09mm, indicating a significant volume for extraction to accommodate the implant device. The superior or upper section of the metatarsal, referred to as the base, is found to measure 12.68mm.
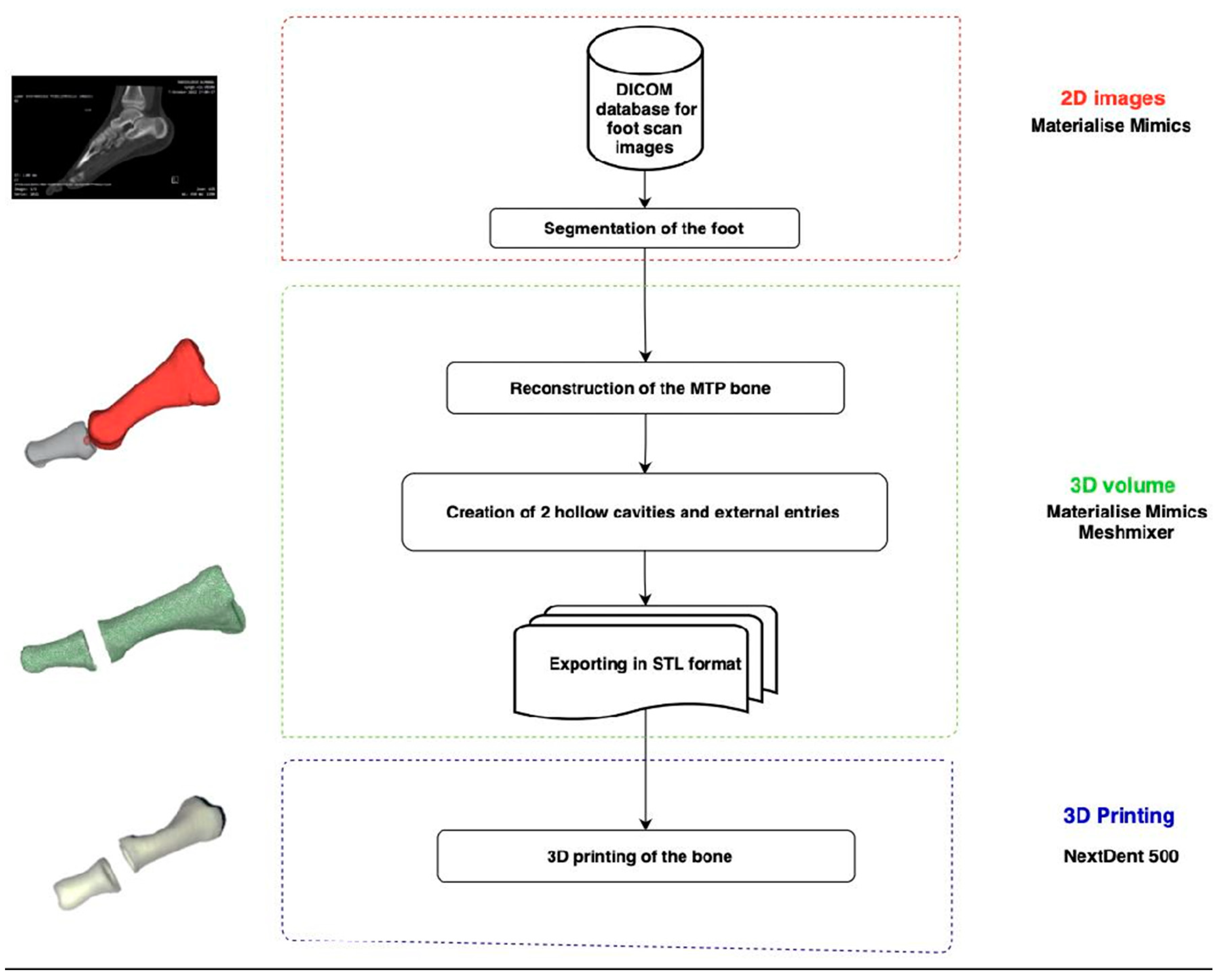
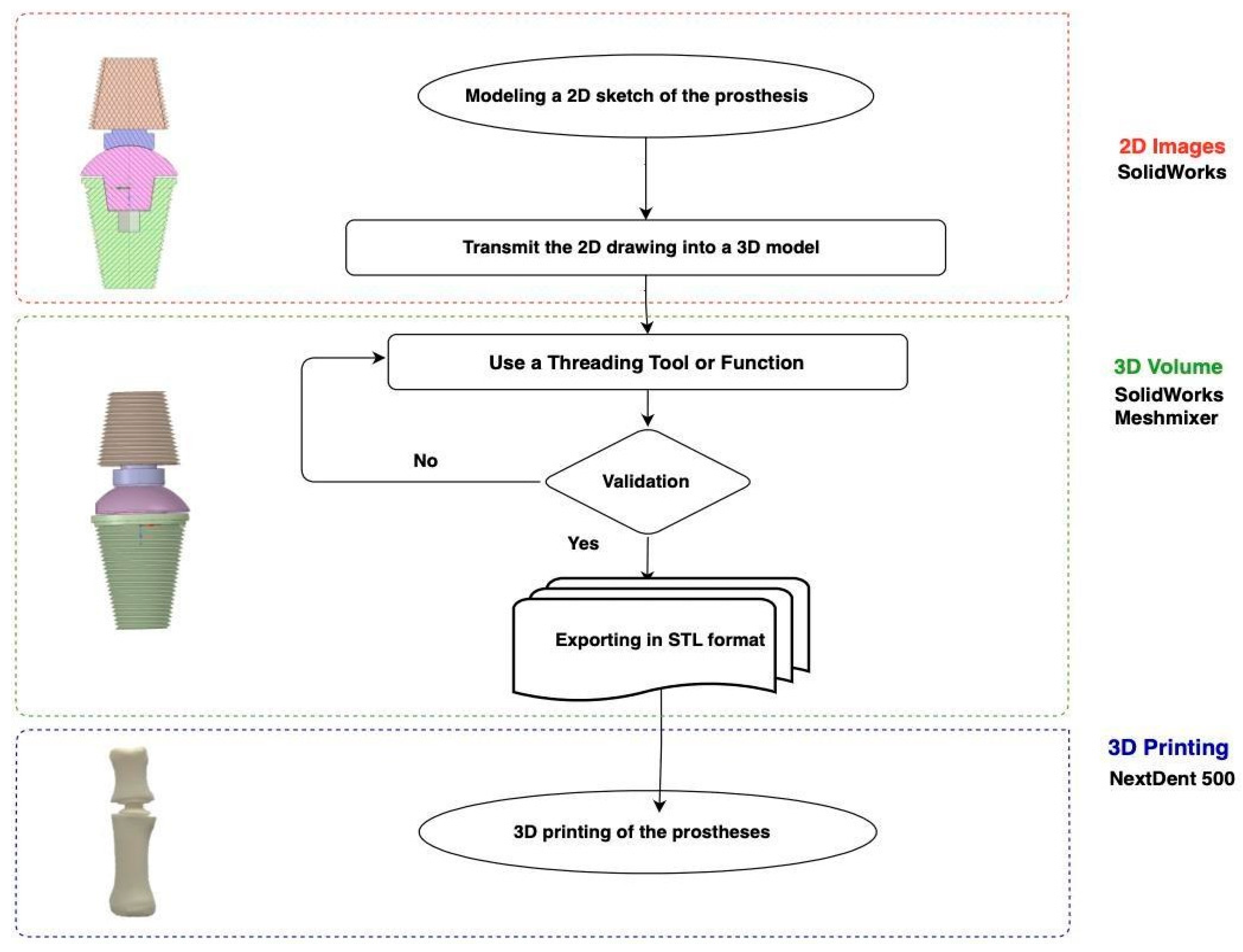
4.3.2. Flowchart of the 3D Printing of the Hollowed Bones
The following flowchart defines the steps taken to create a 3D reconstruction of the metatarsophalangeal hollowed bones to receive the implant. Firstly, the collection of 2D scan images of the patient's foot, which are usually stored in DICOM format. After being collected, these images are uploaded into the Materialise Mimics software. This specialized software is used for processing the DICOM images and plays a crucial role in the next step: the 3D segmentation of the whole foot. This software is able to offer a more thorough and accurate representation of the patient's anatomy by converting 2D images into a 3D structure. After the reconstruction, the metatarsophalangeal bones is then reconstructed and then exported as an STL file. The next phase involves threading, cleaning, and refining the model with another 3D modeling software called Meshmixer, by creating threads, removing unnecessary surfaces and refining the bones for more accurate definition, which improves the precision of the model, guaranteeing it is ready to receive the implant. The finishing step in this approach is the 3D printing of the bones with cavities, a Next Dent 3D printer is used in this instance.
Figure 10.
Flowchart of the hollowed bones.
Figure 10.
Flowchart of the hollowed bones.
4.4. Modeling the Implant
3D reconstruction is the process of creating a three-dimensional model or representation of an object or scene from two-dimensional data. Several sources, including images, medical imaging scans, laser scanning, and structured light scanning, can provide this data. Image capture, data preprocessing, feature recognition and matching, camera calibration, triangulation, and surface reconstruction are the typical stages in the 3D reconstruction process [
25]. In order to identify the elements required to create the implant, after the segmentation of the whole foot we reconstructed the bones with the chosen software Materialise Mimics, then we created a 2D model sketch composed of 4 pieces using a CAD program which was SolidWorks, by following the lead of toes and fingers implants models that already existed. The same software is used to transfer the finished 2D drawing in 3D, after that we check if the dimensions and proportions are accurate and consistent with the specifications of the implant. Once the 3D model has been created, it must be edited and refined in preparation for 3D printing. We used Meshmixer to do so, which enables us to alter the 3D model while preserving the size and shape of the implant by deleting extraneous components or decreasing the mesh's density.
Figure 11.
2D sketch of the implant.
Figure 11.
2D sketch of the implant.
Figure 12.
3D model of the implant.
Figure 12.
3D model of the implant.
4.5. Components of the Implant and Its Functionalities
The following table illustrates the four separate components of the implant item, each accompanied by an image and a description of its individual functionalities. The accompanying descriptions clarify each component’s specific roles and how they contribute to the implant device’s overall functionality, while the accompanying pictures give each part a clear visual representation. This table representation provides a thorough knowledge of the construction and use of the implant, highlighting the significance and purpose of each part within the overall system.
Table 4.
components of the implant.
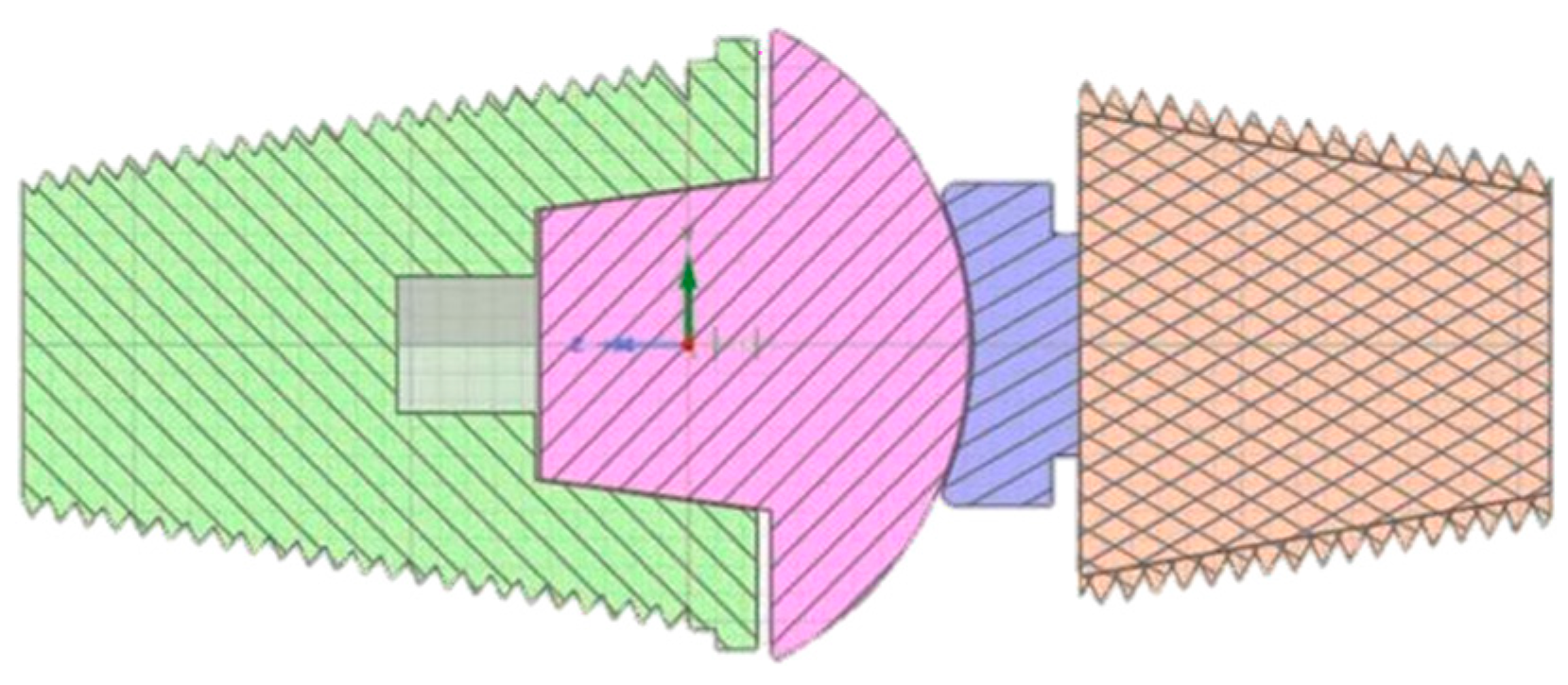
4.6. 3D Printing of the Implant
The creation of the implant joint involved a complex and intricate 3D printing process that consisted of four distinct parts. Specifically, two of these parts were specifically designed to replace the removed sections of both the metatarsal and phalangeal bones. The intention behind these components was to accurately replicate the missing bone segments and restore the structural integrity of the foot. The remaining two components served a crucial role in connecting the replaced bone parts and facilitating mobility between them. These linking components were carefully engineered to ensure smooth movement and enable the implant to function as closely as possible to the natural joint structure. The successful integration of these four components was vital to the overall functionality and effectiveness of the implant joint, as it aimed to restore not only the physical appearance but also the functional abilities of the foot.
Figure 13.
Printed prototype inside the bone.
Figure 13.
Printed prototype inside the bone.
4.7. Flowchart of the Implant Creation Steps
The second flowchart was produced to summarize the phases to develop an implant for the metatarsophalangeal joint using 3D modeling and printing. At first, models that have previously been made, like those of the metacarpophalangeal joints from the hand, served as sources of inspiration. The first essential step is to perform a 2D sketch modeling of the implant inspired by these models. For this purpose, the SolidWorks software was used due to its tools making it easy for this task. The sketch is then converted into a 3D model with the help of the same software. During this transition, the 3D volume of the previously segmented bones from the first flowchart serves as a basis. To achieve the maximum degree of accuracy and details in the implant model, the 3D model is next threaded, modified and further enhanced for better precision using the Meshmixer software once again.
After the 3D model has been validated, and for now, the 3D printer Next Dent 5100 was employed to print out the implant using resin. Yet, our future perspective is to boost the quality of our work by 3D printing this implant with the chosen biomaterial which is titanium.
Figure 14.
Flowchart of the implant creation steps.
Figure 14.
Flowchart of the implant creation steps.
5. Discussion
5.1. Software Selection
Materialise Mimics proved to be an excellent choice and was quite successful in this project. It offered a variety of options that really aided and improved this work's efficiency.
The user-friendly interface of Materialise Mimics was one of its noticeable benefits, especially for beginners. The software offered intuitive tutorials on their website, which really helped in quickly picking up its functionalities and applying them effectively.
SolidWorks has been crucial to the accomplishment of our project. We were given a suite of thorough tools by this potent 3D modeling program, which helped us plan, simulate, and evaluate our project with remarkable accuracy and efficiency. Complex models could be easily created using its user-friendly interface, and its sophisticated simulation tools allowed us to project how our design would perform in the real world and make the required modifications. The collaborative features of SolidWorks also facilitated effective team coordination, enabling us to work together smoothly, irrespective of distance. Overall, SolidWorks superior features and capabilities really aided in the successful completion of our project.
Meshmixer has proven to be highly helpful and pleasing for our needs in creating the implant. We have been able to modify and enhance our 3D models with amazing accuracy and flexibility because to its extensive toolkit. We were able to build and refine the implant with a high level of anatomical accuracy because to the software's capacity to sculpt, mix, and change meshes, assuring a secure fit for the user.
5.2. Printing Material’s Selection
After a thorough analysis of the benchmark study mentioned before, it was decided that titanium and its alloys are the best materials for joint implant as they offer the best combination of biocompatibility, durability, and osseointegration properties. When compared to other biomaterials, titanium and its alloys are quite pricey, but the long-term advantages of employing this material can justify the initial expense. The final choice of the material was based on the analysis of various factors, including mechanical properties, biocompatibility, and long-term stability, that were listed in the benchmark developed before.
However, due to the existing restrictions on its availability, it was decided that the application of this biomaterial would be a future prospect for this project, and it was decided to work with the two available options (PLA and resin material) to get an idea of the real-life outcome of the implant.
Both biomaterials met the initial requirements for the first step which was printing the bones, though there was an obvious difference between the PLA and the resin material in terms of performance and quality. The resin showed more definition and accuracy than the PLA material, that’s why only the resin material was chosen in the following step: the printing of the implant.
5.3. Specialized Implant
Our specialized created implant is an individual solution customized specifically for each individual situation. We won't start the modeling process over from scratch for each new example to achieve this result. We will simply measure and edit the piece's essential geometric characteristics using the 2D photos from the foot scanner, which will then be updated in the program to provide us with the final outcome. This considerably speeds up the design process while yet guaranteeing a precise and unique fit for each user.
Looking towards the future, the possibility to extend this customized implant approach to include any affected bone within the body is indeed an exciting prospect for our project. Our methodology's capacity to scale and adapt creates a broad framework that may be used to treat a wide variety of bone problems.
This implies that a wider range of therapeutic options and life-improving benefits may be available. Patients with a variety of bone disorders, not simply those in need of a metatarsophalangeal implant, could profit from a customized treatment plan created to meet their particular requirements. The ability to design unique implant to fit a variety of bones may enable faster integration and adaption owing to the specific fit, as well as more successful therapy and recovery.
5.4. Model Verification
Three radiology and traumatology specialists were given the final report to offer us their feedback. According to their professional analysis, everyone agreed that the results was excellent and showed a flawless and realistic outcome. These specialists validated the complete procedures that were taken to obtain such outcome, including diagnosing the disorders that resulted the locked joint and the requirement for using such an implant, in addition to acknowledging the effectiveness of the implant. They also agreed that titanium should be used as the preferred biomaterial and that this implant should be made in two pieces to allow full mobility and natural movement. Overall, their approval confirmed the meticulous procedures done in this implant development.
6. Conclusion
This work explores the creation of a customized implant for the metatarsophalangeal bones, using one of the main applications of 3D printing in the medical industry. This development aims to help people suffering from conditions affecting this joint, such as diseases or abnormalities by offering them this custom implant. The article describes how a set of tools and software is used to create a 3D model from a patient's 2D medical imaging data. Then, using various procedures, this model is carefully refined and optimized for printing. Once the model has been correctly manufactured, it can replace the functionality of the MTP joint so that the foot can function normally again.
References
- MacGregor, Robert, and Doug W. Byerly. "Anatomy, Bony Pelvis and Lower Limb, Foot Bones." (2020).
- L.K. Chan, The anatomy of the human foot, in: A. Luximon (Ed.), Handb. Footwear Des. Manuf., second edi, Woodhead Publishing, 2021: pp. 3−28.
- Batra AV, Sullivan JO (2018) A Rare Case of Benign Osteochondromatous Lesion beneath the 3rdMetatarsophalangeal Joint. J Orthop Res Physiother 4: 038. [CrossRef]
- Kokubu, Yasuhiko, et al. "Postoperative clinical and functional outcomes in patients with tumor and tumor-like lesion of foot and ankle." Journal of Foot and Ankle Research 15.1 (2022): 75. 3. Scott Litin, M.D. “Mayo Clinic Family Health Book” 5th edition (2021). [CrossRef]
- Ferguson, Jason L., and Sean P. Turner. "Bone cancer: diagnosis and treatment principles." American family physician98.4 (2018): 205-213.
- Riggi, Nicolò, Mario L. Suvà, and Ivan Stamenkovic. "Ewing’s sarcoma." New England Journal of Medicine 384.2 (2021): 154-164.
- Board, PDQ Pediatric Treatment Editorial. "Ewing Sarcoma Treatment (PDQ®)." PDQ Cancer Information Summaries [Internet]. National Cancer Institute (US), 2021.
- Wang, Yitian, et al. "The functional outcomes and complications of different reconstruction methods for Giant cell tumor of the distal radius: comparison of Osteoarticular allograft and three-dimensional-printed prosthesis." BMC Musculoskeletal Disorders21.1 (2020): 1-15. [CrossRef]
- Gan, Fengping, et al. "Treatment of giant cell tumor of bone around knee joint with three-dimensional printing personalized prosthesis." Zhongguo xiu fu Chong Jian wai ke za zhi= Zhongguo Xiufu Chongjian Waike Zazhi= Chinese Journal of Reparative and Reconstructive Surgery 34.6 (2020): 751-755. [CrossRef]
- SCHRAMM, Martin, MAESTRO, Michel, et DECROOCQ, Lauryl. Implant métatarso phalangien sphérique en pyrocarbone HAPY®: note de technique. Revue de Chirurgie Orthopédique et Traumatologique, 2021, vol. 107, no 5, p. 583-586. [CrossRef]
- EL GHALI, Btihal, EL MIDAOUI, Omar, EL GHALI, Mohamed Ayman, et al. Modeling and Implementation of a Lunate Implant Based on 3D Reconstruction of CT Scan Images. In : 2021 Fifth International Conference On Intelligent Computing in Data Sciences (ICDS). IEEE, 2021. p. 1-7.
- Giant cell tumor CHANDHANAYINGYONG, Chandhanarat, SRIKONG, Korakod, PUNCREOBUTR, Chedtha, et al. Three-dimensional printed, proximal phalangeal prosthesis with metatarsophalangeal joint arthroplasty for the treatment of a giant cell tumor of the fifth toe: The first case report. International Journal of Surgery Case Reports, 2020, vol. 73, p. 84-89. [CrossRef]
- Xu L, Qin H, Cheng Z, Jiang WB, Tan J, Luo X, Huang W. 3D-printed personalised prostheses for bone defect repair and reconstruction following resection of metacarpal giant cell tumours. Ann Transl Med. 2021 Sep;9(18):1421. [CrossRef]
- ZARE, Mina, GHOMI, Erfan Rezvani, VENKATRAMAN, Prabhuraj D., et al. Silicone-based biomaterials for biomedical applications: antimicrobial strategies and 3D printing technologies. Journal of Applied Polymer Science, 2021, vol. 138, no 38, p. 50969. [CrossRef]
- RAJAN, R. A., KERR, M., EVANS, H., et al. A prospective clinical and biomechanical analysis of feet following first metatarsophalangeal joint replacement. Gait & Posture, 2021, vol. 89, p. 211-216. [CrossRef]
- CHENG, Jiangang, GAO, Yang, LONG, Zhuoyu, et al. Repair of distal fibular and lateral malleolus defects with individualized 3D-printed titanium alloy prosthesis: The first case report from China. International Journal of Surgery Case Reports, 2022, vol. 94, p. 107057. [CrossRef]
- Sazzad, F., Goh, J.H., Ong, Z.X. et al. Three dimensional modeling of atrioventricular valves provides predictive guides for optimal choice of prosthesis. Sci Rep 12, 7432 (2022). [CrossRef]
- DUMITRESCU, Gean-Carlos Nicholas, and Patricia Isabela BRAILEANU. "Custom Prosthetic Finger Device Using 3D Printable PA11 CF Powder." The Annals of “Dunarea de Jos” University of Galati. Fascicle IX, Metallurgy and Materials Science 46.1 (2023): 33-36.Cinema 4D official. [CrossRef]
- FARAHAT, Zineb, HASNI, Mouad, MEGDICHE, Kawtar, et al.Comparative Study of DICOM Files Handling Software’s: Study Based on the Anatomage Table. In : Innovation in Information Systems and Technologies to Support Learning Research: Proceedings of EMENA-ISTL 2019 3. Springer International Publishing, (2020). p. 390-399.
- ASIF, Muhammad Khan, NAMBIAR, Phrabhakaran, KHAN, Iqra Muhammad, et al. Enhancing the three-dimensional visualization of a foreign object using Mimics software. Radiology case reports, 2019, vol. 14, no 12, p. 1545-1549. [CrossRef]
- Bratovanov, Nikolay. "Robot modeling, motion simulation and off-line programming based on SolidWorks API." 2019 Third IEEE International Conference on Robotic Computing (IRC). IEEE, 2019.
- YUNGA, Alexis David Armijos, CORTE, Nicole Adriana Juela, OCAMPO, Fabiana Valentina Pesantez, et al. Comparative study of reliability in three software meshmixer, 3d slicer and nemocast of the intercanine and intermolar spaces of digital models. World Journal of Advanced Research and Reviews, 2023, vol. 17, no 1, p. 1040-1045. [CrossRef]
- Paramasivam, V., G. Singh, and S. Santhanakrishnan. "3D printing of human anatomical models for preoperative surgical planning." Procedia Manufacturing 48 (2020): 684-690.Volumic stream 30 ultra official website. [CrossRef]
- GIORDANO, Geoff. 3D Printing the Future of Healthcare: Additive manufacturing, or 3D printing, is fast-tracking developments in the medical device industry. Plastics Engineering, 2019, vol. 75, no 6, p. 14-17.
- Phang, J.T.S., Lim, K.H. & Chiong, R.C.W. Un examen des techniques de reconstruction tridimensionnelle. Multimed Tools Appl 80, 17879–17891 (2021).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).