Submitted:
27 March 2024
Posted:
01 April 2024
You are already at the latest version
Abstract
Keywords:
Introduction
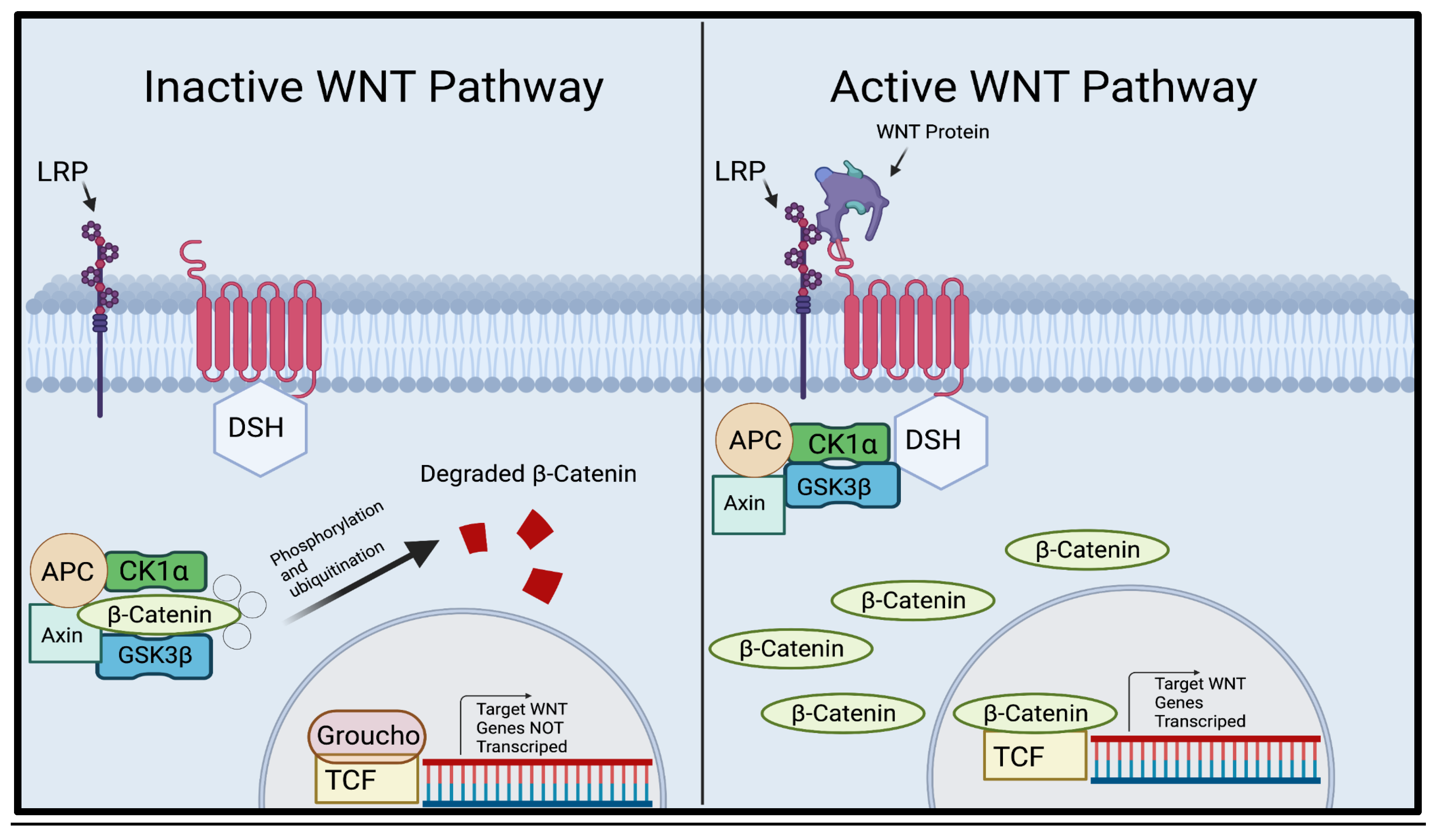
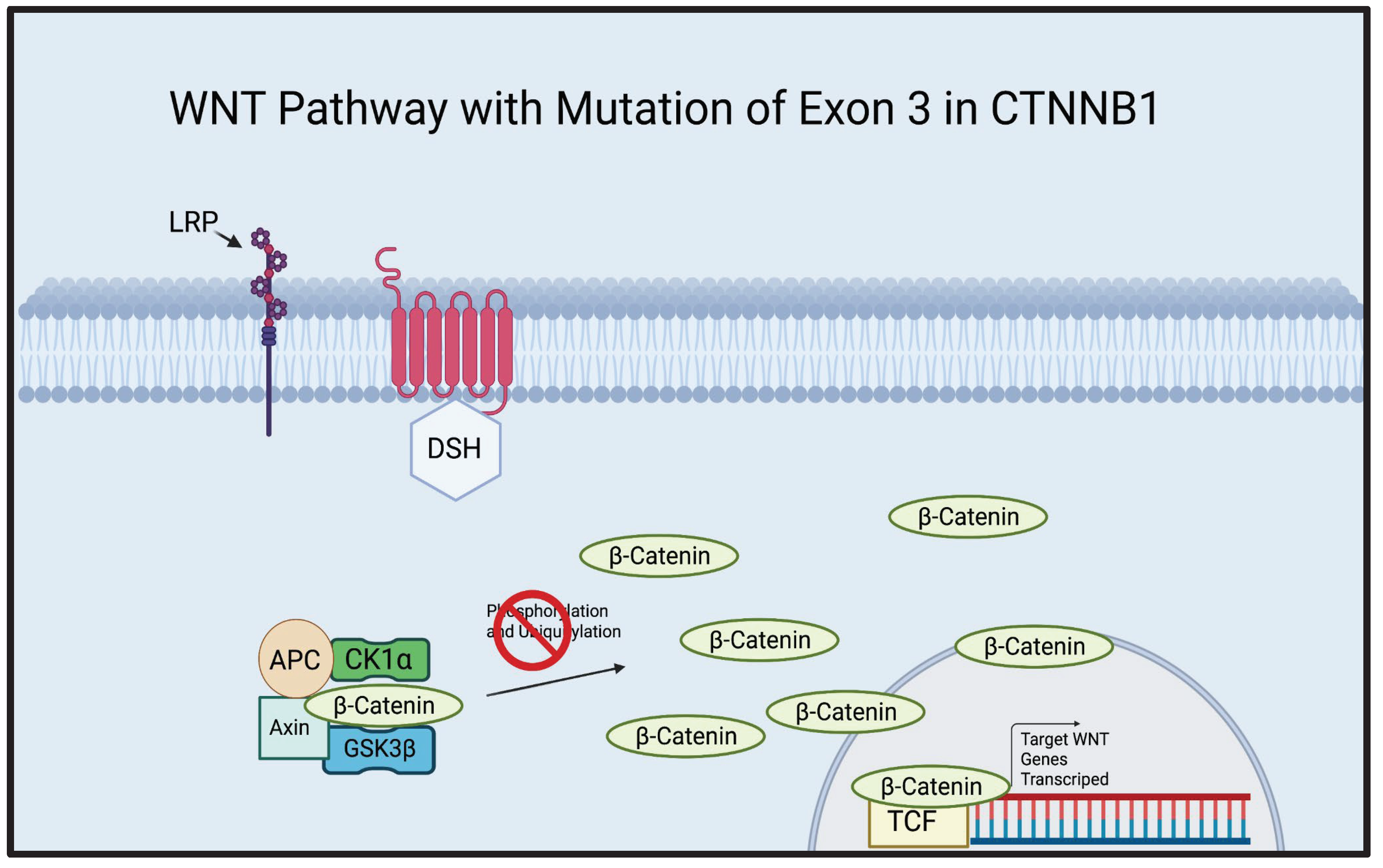
β-Catenin, WNT Pathway, and the Cause of Adamaninomatous Craniopharyngioma
RNAi Therapy in Treatments of ACP
sHRNA
siRNA
CRISPR
Discussion
Conclusion
References
- Karavitaki, N., Cudlip, S., Adams, C. B. T. & Wass, J. A. H. Craniopharyngiomas. Endocr. Rev. 27, 371–397 (2006). [CrossRef]
- Dandurand, C., Sepehry, A. A., Asadi Lari, M. H., Akagami, R. & Gooderham, P. Adult Craniopharyngioma: Case Series, Systematic Review, and Meta-Analysis. Neurosurgery 83, 631 (2018). [CrossRef]
- Muller, H. L. Childhood craniopharyngioma. Recent advances in diagnosis, treatment and follow-up. Horm. Res. 69 (2008). [CrossRef]
- Müller, H. L. The Diagnosis and Treatment of Craniopharyngioma. Jinko Mondai Kenkyusho. Nenpo 110, 753–766 (2020). [CrossRef]
- Bunin, G. R. et al. The descriptive epidemiology of craniopharyngioma. J. Neurosurg. 89, 547–551 (1998). [CrossRef]
- Olsson, D. S., Andersson, E., Bryngelsson, I.-L., Nilsson, A. G. & Johannsson, G. Excess Mortality and Morbidity in Patients with Craniopharyngioma, Especially in Patients with Childhood Onset: A Population-Based Study in Sweden. J. Clin. Endocrinol. Metab. 100, 467–474 (2015). [CrossRef]
- Momin, A. A. et al. Descriptive epidemiology of craniopharyngiomas in the United States. Pituitary 24, (2021) . [CrossRef]
- Brastianos, P. et al. GE-05 * EXOME SEQUENCING REVEALS BRAF MUTATIONS IN PAPILLARY CRANIOPHARYNGIOMAS. Neuro-Oncology vol. 16 v97–v97 (2014). [CrossRef]
- He, J. et al. Characterization of novel CTNNB1 mutation in Craniopharyngioma by whole-genome sequencing. Mol. Cancer 20 (2021). [CrossRef]
- Martinez-Barbera, J. P. Molecular and cellular pathogenesis of adamantinomatous craniopharyngioma. Neuropathology and Applied Neurobiology vol. 41 721–732 (2015). [CrossRef]
- Sekine, S. et al. Craniopharyngiomas of adamantinomatous type harbor beta-catenin gene mutations. Am. J. Pathol. 161 (2002). [CrossRef]
- Gaston-Massuet, C. et al. Increased Wingless (Wnt) signaling in pituitary progenitor/stem cells gives rise to pituitary tumors in mice and humans. Proc. Natl. Acad. Sci. U. S. A. 108, 11482–11487 (2011) . [CrossRef]
- Duff, J. et al. Long-term outcomes for surgically resected craniopharyngiomas. Neurosurgery 46, (2000). [CrossRef]
- Karavitaki, N. et al. Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clinical Endocrinology vol. 62 397–409 (2005) . [CrossRef]
- Zapata-Benavides, P. et al. shRNA-WT1 Potentiates Anticancer Effects of Gemcitabine and Cisplatin Against B16F10 Lung Metastases In Vitro and In Vivo. In Vivo 33, (2019). [CrossRef]
- Stripp, D. C. H. et al. Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. International Journal of Radiation Oncology*Biology*Physics vol. 58 714–720 . [CrossRef]
- Fahlbusch, R., Honegger, J., Paulus, W., Huk, W. & Buchfelder, M. Surgical treatment of craniopharyngiomas: experience with 168 patients. Journal of Neurosurgery vol. 90 237–250 (1999). [CrossRef]
- Kalapurakal, J. A., Goldman, S., Hsieh, Y. C., Tomita, T. & Marymont, M. H. Clinical outcome in children with craniopharyngioma treated with primary surgery and radiotherapy deferred until relapse. Med. Pediatr. Oncol. 40, (2003). [CrossRef]
- Huelsken, J. & Behrens, J. The Wnt signalling pathway. Journal of Cell Science vol. 115 3977–3978 (2002). [CrossRef]
- Logan, C. Y. & Nusse, R. The Wnt signaling pathway in development and disease. Annu. Rev. Cell Dev. Biol. 20, (2004). [CrossRef]
- Gao, C. et al. Exon 3 mutations of CTNNB1 drive tumorigenesis: a review. Oncotarget 9, 5492 (2018). [CrossRef]
- Tatsumi, N. et al. Wilms’ tumor gene WT1-shRNA as a potent apoptosis-inducing agent for solid tumors. International Journal of Oncology (2008). [CrossRef]
- Hwang, J.-E. et al. Intravenous KITENIN shRNA Injection Suppresses Hepatic Metastasis and Recurrence of Colon Cancer in an Orthotopic Mouse Model. J. Korean Med. Sci. 26, 1439–1445 (2011). [CrossRef]
- Kijima, N. et al. Wilms’ Tumor 1 Is Involved in Tumorigenicity of Glioblastoma by Regulating Cell Proliferation and Apoptosis. Anticancer Res. 34, 61–67 (2014).
- Hu, B. et al. Therapeutic siRNA: state of the art. Signal Transduction and Targeted Therapy 5, 1–25 (2020). [CrossRef]
- Rao, D. D., Vorhies, J. S., Senzer, N. & Nemunaitis, J. siRNA vs. shRNA: similarities and differences. Adv. Drug Deliv. Rev. 61, (2009). [CrossRef]
- Moore, C. B., Guthrie, E. H., Huang, M. T.-H. & Taxman, D. J. Short Hairpin RNA (shRNA): Design, Delivery, and Assessment of Gene Knockdown. Methods Mol. Biol. 629, 141 (2010). [CrossRef]
- Zhang, F., Chen, A., Chen, J., Yu, T. & Guo, F. SiRNA-mediated silencing of beta-catenin suppresses invasion and chemosensitivity to doxorubicin in MG-63 osteosarcoma cells. Asian Pac. J. Cancer Prev. 12, 239–245 (2011).
- siRNA-Mediated β-Catenin Knockdown in Human Hepatoma Cells Results in Decreased Growth and Survival. Neoplasia 9, 951–959 (2007). [CrossRef]
- Ledford, H. CRISPR, the disruptor. Nature Publishing Group UK (2015). [CrossRef]
- Katti, A., Diaz, B. J., Caragine, C. M., Sanjana, N. E. & Dow, L. E. CRISPR in cancer biology and therapy. Nat. Rev. Cancer 22, 259–279 (2022). [CrossRef]
- Zhuang, C. et al. Engineered CRISPR/Cas13d Sensing hTERT Selectively Inhibits the Progression of Bladder Cancer. Front Mol Biosci 8, 646412 (2021). [CrossRef]
- Transl. [CrossRef]
- Goschzik, T. et al. Genomic Alterations of Adamantinomatous and Papillary Craniopharyngioma. J. Neuropathol. Exp. Neurol. 76, 126–134 (2017). [CrossRef]
- Qi, L., Xing, L. N., Wei, X. & Song, S. G. Effects of VEGF suppression by small hairpin RNA interference combined with radiotherapy on the growth of cervical cancer. Genet. Mol. Res. 13, (2014). [CrossRef]
- Rao, D. D., Senzer, N., Cleary, M. A. & Nemunaitis, J. Comparative assessment of siRNA and shRNA off target effects: what is slowing clinical development. Cancer Gene Ther. 16, 807–809 (2009). [CrossRef]
- Baek, S. T. et al. Off-target effect of doublecortin family shRNA on neuronal migration associated with endogenous microRNA dysregulation. Neuron 82, 1255–1262 (2014). [CrossRef]
- Jazbinšek, S. et al. Prevalence of Endocrine and Metabolic Comorbidities in a National Cohort of Patients with Craniopharyngioma. HRP 93, 46–57 (2020). [CrossRef]
- Mahfouz, M. M., Piatek, A. & Stewart, C. N., Jr. Genome engineering via TALENs and CRISPR/Cas9 systems: challenges and perspectives. Plant Biotechnol. J. 12, 1006–1014 (2014). [CrossRef]
- Gaj, T., Gersbach, C. A. & Barbas, C. F. ZFN, TALEN, and CRISPR/Cas-based methods for genome engineering. Trends Biotechnol. 31, (2013). [CrossRef]
- Doudna, J. A. & Charpentier, E. Genome editing. The new frontier of genome engineering with CRISPR-Cas9. Science 346, (2014). [CrossRef]
- Kevles, D. J. Eugenics and human rights. BMJ 319, 435–438 (1999). [CrossRef]
- Brokowski, C. & Adli, M. CRISPR Ethics: Moral Considerations for Applications of a Powerful Tool. J. Mol. Biol. 431, (2019). [CrossRef]
- Zhang, D. et al. Genome editing with the CRISPR-Cas system: an art, ethics and global regulatory perspective. Plant Biotechnol. J. 18, (2020). [CrossRef]
- Ebina, H., Misawa, N., Kanemura, Y. & Koyanagi, Y. Harnessing the CRISPR/Cas9 system to disrupt latent HIV-1 provirus. Sci. Rep. 3, 1–7 (2013). [CrossRef]
- Zhen, S. et al. In vitro and in vivo growth suppression of human papillomavirus 16-positive cervical cancer cells by CRISPR/Cas9. Biochem. Biophys. Res. Commun. 450, 1422–1426 (2014). [CrossRef]
- Targeted Disruption of V600E-Mutant BRAF Gene by CRISPR-Cpf1. Molecular Therapy - Nucleic Acids 8, 450–458 (2017). [CrossRef]
- Zeng, G. et al. ; Sirna-mediated beta-catenin knockdown in human hepatoma cells results in decreased growth and survival. Neoplasia (New York, N.Y.). [CrossRef]
- Moon, Randall T. “Wnt/β-Catenin Pathway | Science's STKE.” Wnt/β-Catenin Pathway. Science Signaling. https://www.science.org/doi/10.1126/stke.2712005cm1 (2005).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



